A Detailed Report on Nursing Care Strategies for COPD Patients
VerifiedAdded on 2020/03/23
|14
|3349
|44
Report
AI Summary
This report delves into the comprehensive nursing care required for patients diagnosed with Chronic Obstructive Pulmonary Disease (COPD). It begins with an introduction to COPD, its increasing prevalence, and its impact on global health, followed by an examination of the disease's complexity, chronicity, and associated comorbidities, such as diabetes and cardiovascular diseases. The report then analyzes a case study of a COPD patient, highlighting the interrelation of various factors affecting patient well-being, including physical and mental health, and the challenges faced by healthcare providers. Furthermore, it provides an in-depth understanding of COPD's pathophysiology, including airway inflammation, structural changes, and mucociliary dysfunction. The core of the report focuses on nursing interventions, encompassing nursing diagnoses, care goals, rationales, and expected outcomes, and it details interventions for dyspnea, ineffective airway clearance, and the risk of infection. The report also emphasizes the importance of health coaching, self-management strategies, patient empowerment, and advocacy, and it highlights the role of registered nurses in providing comprehensive care, including collaboration with other healthcare professionals. The report concludes by summarizing key aspects of COPD care and emphasizing the need for a multidisciplinary approach to improve patient outcomes.

Running head: NURSING CARE FOR COPD
Nursing Care for COPD
Name of the student:
Name of the university:
Author note:
Nursing Care for COPD
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING CARE FOR COPD
Table of Contents
Introduction: 2
Nursing intervention for COPD: 5
Health coaching, self-management, empowerment and advocacy: 10
Collaboration by registered nurse: 11
Conclusion: 12
References: 13
Table of Contents
Introduction: 2
Nursing intervention for COPD: 5
Health coaching, self-management, empowerment and advocacy: 10
Collaboration by registered nurse: 11
Conclusion: 12
References: 13
2NURSING CARE FOR COPD
Introduction:
The health care industry has advanced considerably in the past few decades and what used to
be an incurable morbidity, taking hundreds of lives; now there are different treatment options for
it. However, it also needs to be considered that despite all the technological revolution in the
health care industry, there still is a number of emerging public health concerns that mortality
rates are increasing rapidly (Lisspers et al., 2014). One of the most common of these health
priorities can be considered the chronic obstructive pulmonary disorder that targets more than
34% of the global population and this particular health disorder contributes to a large proportion
of mortality to the health care sector.
Chronic obstructive pulmonary disorder or COPD is a respiratory disease which can be
characterized by the blocked respiratory airways, shortness of breath and excessive sputum or
cough production. The patient suffering with COPD can be cared for optimally if a
multidisciplinary team having different experts belonging to different care sectors; ho can
address differential care needs of the patient. This assignment will attempt to evaluate all aspects
associated with caring for a patient suffering with COPD taking the help of a case study.
Interrelationship of complexity, chronicity and co-morbidity in healthcare
COPD is the chronic illness and is associated with various comorbidities such as diabetes
mellitus, cardiac disease, osteoporosis, hypertension, muscle weakness and other psychological
disorders (Mellado et al., 2016). Chronicity of the illness refers to the condition that is difficult to
be cured. Comorbidities are the medical condition that are associated and occur together with the
main illness. These comorbidities add to the complexity of the chronic disease. COPD is the
Introduction:
The health care industry has advanced considerably in the past few decades and what used to
be an incurable morbidity, taking hundreds of lives; now there are different treatment options for
it. However, it also needs to be considered that despite all the technological revolution in the
health care industry, there still is a number of emerging public health concerns that mortality
rates are increasing rapidly (Lisspers et al., 2014). One of the most common of these health
priorities can be considered the chronic obstructive pulmonary disorder that targets more than
34% of the global population and this particular health disorder contributes to a large proportion
of mortality to the health care sector.
Chronic obstructive pulmonary disorder or COPD is a respiratory disease which can be
characterized by the blocked respiratory airways, shortness of breath and excessive sputum or
cough production. The patient suffering with COPD can be cared for optimally if a
multidisciplinary team having different experts belonging to different care sectors; ho can
address differential care needs of the patient. This assignment will attempt to evaluate all aspects
associated with caring for a patient suffering with COPD taking the help of a case study.
Interrelationship of complexity, chronicity and co-morbidity in healthcare
COPD is the chronic illness and is associated with various comorbidities such as diabetes
mellitus, cardiac disease, osteoporosis, hypertension, muscle weakness and other psychological
disorders (Mellado et al., 2016). Chronicity of the illness refers to the condition that is difficult to
be cured. Comorbidities are the medical condition that are associated and occur together with the
main illness. These comorbidities add to the complexity of the chronic disease. COPD is the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING CARE FOR COPD
complex disease, as the patient had to cope up with various other comorbidities, which increases
the length of the hospital study and exacerbation of COPD symptoms (Donner et al., 2017).
Therefore, it mandates the need of more than one drug to fight the comorbidities along with
COPD. Risk factors such as smoking, medication interaction, aging and lack of treatment of
comorbidities add to the complexity of the comorbidities and outcomes in the patients with
COPD. The complexity of the presentation of the symptoms makes it challenging for the
clinicians to mage the chronic disease (De Lucas-Ramos et al., 2017). Thus, the complexity,
chronicity and the comorbidity is interrelated in the health care and this concept must be clear to
the health care providers to rightly handle the upcoming challenges.
In the given study, Angela (COPD patient) was presented to her GP with increasing shortness
of breath, increased sputum production, which has changed to dark yellow with green staining.
Her condition is worsening daily. She is feeling unwell since several days. Her SaO2 is 84% on
room air, temperature 38.4 C, She is significantly dyspnoeic, struggling to say more than 5 words
without a breath. Her pulse is 104bpm and her BP remains elevated at 162/102mmHg. Due to
inadequate intake of the medication, her symptoms have exacerbated. Consequently, she had to
increase her antibiotics, nebulisers and oxygen therapy to maintain SpO2 above 92%. Due to
hospitalisation, her mental well-being is affected. She is more upset due to burden of illness,
inconvenience caused to her family, and at unable to care for daughters. Thus, chronic illness and
associated comorbidities makes treatment more complex that ultimately affected both the
physical and mental wellbeing.
Pathophysiology of COPD
COPD is characterised by airway inflammation, structural changes in the airway and
mucociliary dysfunction. As a consequent of exposure to the inhaled irritants such as polluted
complex disease, as the patient had to cope up with various other comorbidities, which increases
the length of the hospital study and exacerbation of COPD symptoms (Donner et al., 2017).
Therefore, it mandates the need of more than one drug to fight the comorbidities along with
COPD. Risk factors such as smoking, medication interaction, aging and lack of treatment of
comorbidities add to the complexity of the comorbidities and outcomes in the patients with
COPD. The complexity of the presentation of the symptoms makes it challenging for the
clinicians to mage the chronic disease (De Lucas-Ramos et al., 2017). Thus, the complexity,
chronicity and the comorbidity is interrelated in the health care and this concept must be clear to
the health care providers to rightly handle the upcoming challenges.
In the given study, Angela (COPD patient) was presented to her GP with increasing shortness
of breath, increased sputum production, which has changed to dark yellow with green staining.
Her condition is worsening daily. She is feeling unwell since several days. Her SaO2 is 84% on
room air, temperature 38.4 C, She is significantly dyspnoeic, struggling to say more than 5 words
without a breath. Her pulse is 104bpm and her BP remains elevated at 162/102mmHg. Due to
inadequate intake of the medication, her symptoms have exacerbated. Consequently, she had to
increase her antibiotics, nebulisers and oxygen therapy to maintain SpO2 above 92%. Due to
hospitalisation, her mental well-being is affected. She is more upset due to burden of illness,
inconvenience caused to her family, and at unable to care for daughters. Thus, chronic illness and
associated comorbidities makes treatment more complex that ultimately affected both the
physical and mental wellbeing.
Pathophysiology of COPD
COPD is characterised by airway inflammation, structural changes in the airway and
mucociliary dysfunction. As a consequent of exposure to the inhaled irritants such as polluted
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING CARE FOR COPD
air, tobacco smoke a chronic inflammation of the airway and lung tissues occurs along with the
inflammation in the blood vessels (Celli, 2014). When the irritants are inhaled, it stimulates the
lymphocytes, neutrophils, CD8+ T-lymphocytes, and other inflammatory cells such as
macrophages, and B cells. These stimulated cells are activated to trigger a cascade (Celli, 2014).
Firstly, the inflammatory mediators are released such as interferon gamma, tumour necrosis
factor alpha, C-reactive protein, and interleukins (IL-1, IL-6, IL-8). These mediators can sustain
the inflammatory process. They induce range of systemic effects and leads to tissue damage
(Rodríguez-Roisin, 2014).
Secondly, the chronic illness leads to various structural changes in the lugs that limit the
airflow. The airway inflammation remain associated with the COPD due to airway remodelling.
The narrowing of the airway is caused by the peribronchial fibrosis, over multiplication of the
epithelial cells of the airways, damage of the airway and build-up of the scar tissues (Mitchell,
2015). This results in the loss of lung tissue elasticity. It is caused by the damage of the
structures that support alveoli. It results in collapse of small airways on exhalation. It causes
trapped air in the lungs and impedes airflow. This reduces the lung capacity (Pouwels et al.,
2017).
Thirdly, the mucous glands are enlarged by smoking and consequent inflammation. These
glands line the lung airway and upon enlargement, it leads to goblet cell metaplasia. Ultimately,
the region is filled with mucous secreting cells. COPD inflammation damages the mucociliary
transport system that cleans the airway mucus. Eventually mucous is accumulated in the airways
that blocks and worsen the airflow (Rogers, 2014).
The pathophysiology of COPD detailed above can be related with the case study. Angela
experiences dyspnoea and shortness of breath. Dyspnoea results due to airflow obstruction and
air, tobacco smoke a chronic inflammation of the airway and lung tissues occurs along with the
inflammation in the blood vessels (Celli, 2014). When the irritants are inhaled, it stimulates the
lymphocytes, neutrophils, CD8+ T-lymphocytes, and other inflammatory cells such as
macrophages, and B cells. These stimulated cells are activated to trigger a cascade (Celli, 2014).
Firstly, the inflammatory mediators are released such as interferon gamma, tumour necrosis
factor alpha, C-reactive protein, and interleukins (IL-1, IL-6, IL-8). These mediators can sustain
the inflammatory process. They induce range of systemic effects and leads to tissue damage
(Rodríguez-Roisin, 2014).
Secondly, the chronic illness leads to various structural changes in the lugs that limit the
airflow. The airway inflammation remain associated with the COPD due to airway remodelling.
The narrowing of the airway is caused by the peribronchial fibrosis, over multiplication of the
epithelial cells of the airways, damage of the airway and build-up of the scar tissues (Mitchell,
2015). This results in the loss of lung tissue elasticity. It is caused by the damage of the
structures that support alveoli. It results in collapse of small airways on exhalation. It causes
trapped air in the lungs and impedes airflow. This reduces the lung capacity (Pouwels et al.,
2017).
Thirdly, the mucous glands are enlarged by smoking and consequent inflammation. These
glands line the lung airway and upon enlargement, it leads to goblet cell metaplasia. Ultimately,
the region is filled with mucous secreting cells. COPD inflammation damages the mucociliary
transport system that cleans the airway mucus. Eventually mucous is accumulated in the airways
that blocks and worsen the airflow (Rogers, 2014).
The pathophysiology of COPD detailed above can be related with the case study. Angela
experiences dyspnoea and shortness of breath. Dyspnoea results due to airflow obstruction and
5NURSING CARE FOR COPD
exertion. The damage caused to lungs makes it hard to breath as the airflow is limited. It takes
more efforts to make air travel. The breathing irritants may have damaged the tiny air sacs within
the lungs. Therefore, the COPD patients develop emphysema. The shortness of breath is also
related to irritants and mucous that cause swelling and inflammation. In case of Angela,
shortness of breath can also be the sign of flare up or exacerbation. It may be also be caused by
the infections, Flu or pneumonia (Mitchell, 2015). The elevated blood pressure in Angela can be
related with the pulmonary hypertension due to arteries that transfer blood to lungs. It forces a
patient to breath faster (Rodríguez-Roisin, 2014).
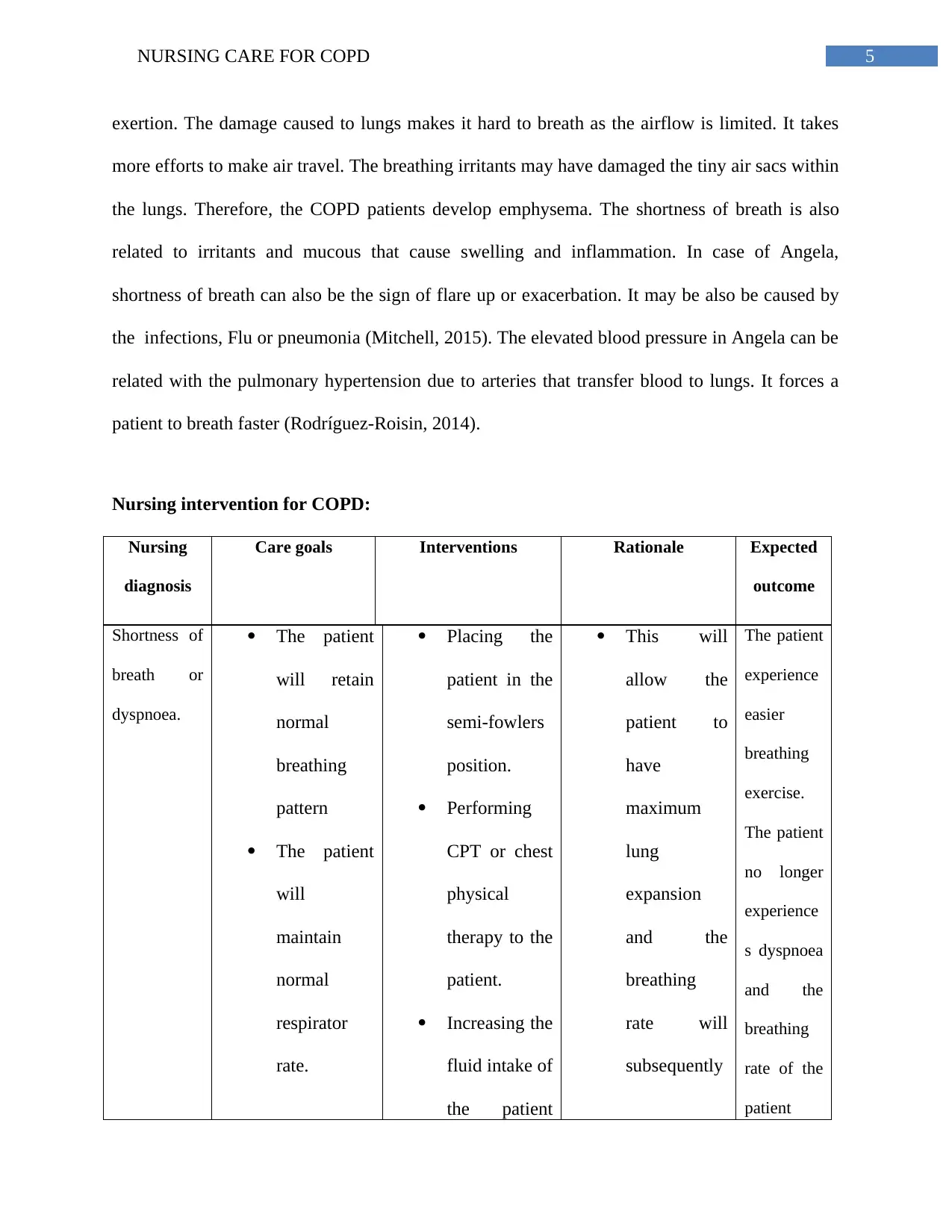
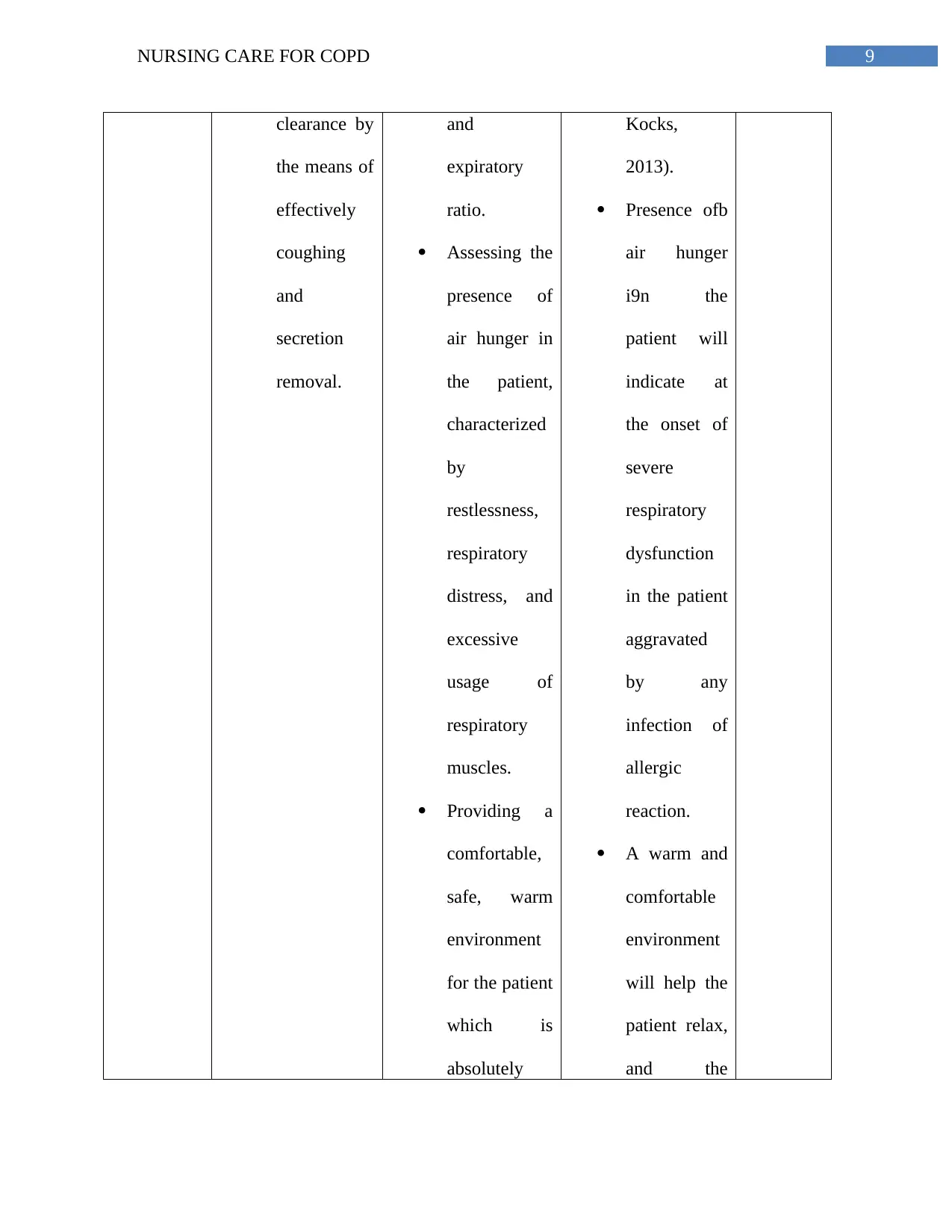
Nursing intervention for COPD:
Nursing
diagnosis
Care goals Interventions Rationale Expected
outcome
Shortness of
breath or
dyspnoea.
The patient
will retain
normal
breathing
pattern
The patient
will
maintain
normal
respirator
rate.
Placing the
patient in the
semi-fowlers
position.
Performing
CPT or chest
physical
therapy to the
patient.
Increasing the
fluid intake of
the patient
This will
allow the
patient to
have
maximum
lung
expansion
and the
breathing
rate will
subsequently
The patient
experience
easier
breathing
exercise.
The patient
no longer
experience
s dyspnoea
and the
breathing
rate of the
patient
exertion. The damage caused to lungs makes it hard to breath as the airflow is limited. It takes
more efforts to make air travel. The breathing irritants may have damaged the tiny air sacs within
the lungs. Therefore, the COPD patients develop emphysema. The shortness of breath is also
related to irritants and mucous that cause swelling and inflammation. In case of Angela,
shortness of breath can also be the sign of flare up or exacerbation. It may be also be caused by
the infections, Flu or pneumonia (Mitchell, 2015). The elevated blood pressure in Angela can be
related with the pulmonary hypertension due to arteries that transfer blood to lungs. It forces a
patient to breath faster (Rodríguez-Roisin, 2014).
Nursing intervention for COPD:
Nursing
diagnosis
Care goals Interventions Rationale Expected
outcome
Shortness of
breath or
dyspnoea.
The patient
will retain
normal
breathing
pattern
The patient
will
maintain
normal
respirator
rate.
Placing the
patient in the
semi-fowlers
position.
Performing
CPT or chest
physical
therapy to the
patient.
Increasing the
fluid intake of
the patient
This will
allow the
patient to
have
maximum
lung
expansion
and the
breathing
rate will
subsequently
The patient
experience
easier
breathing
exercise.
The patient
no longer
experience
s dyspnoea
and the
breathing
rate of the
patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING CARE FOR COPD
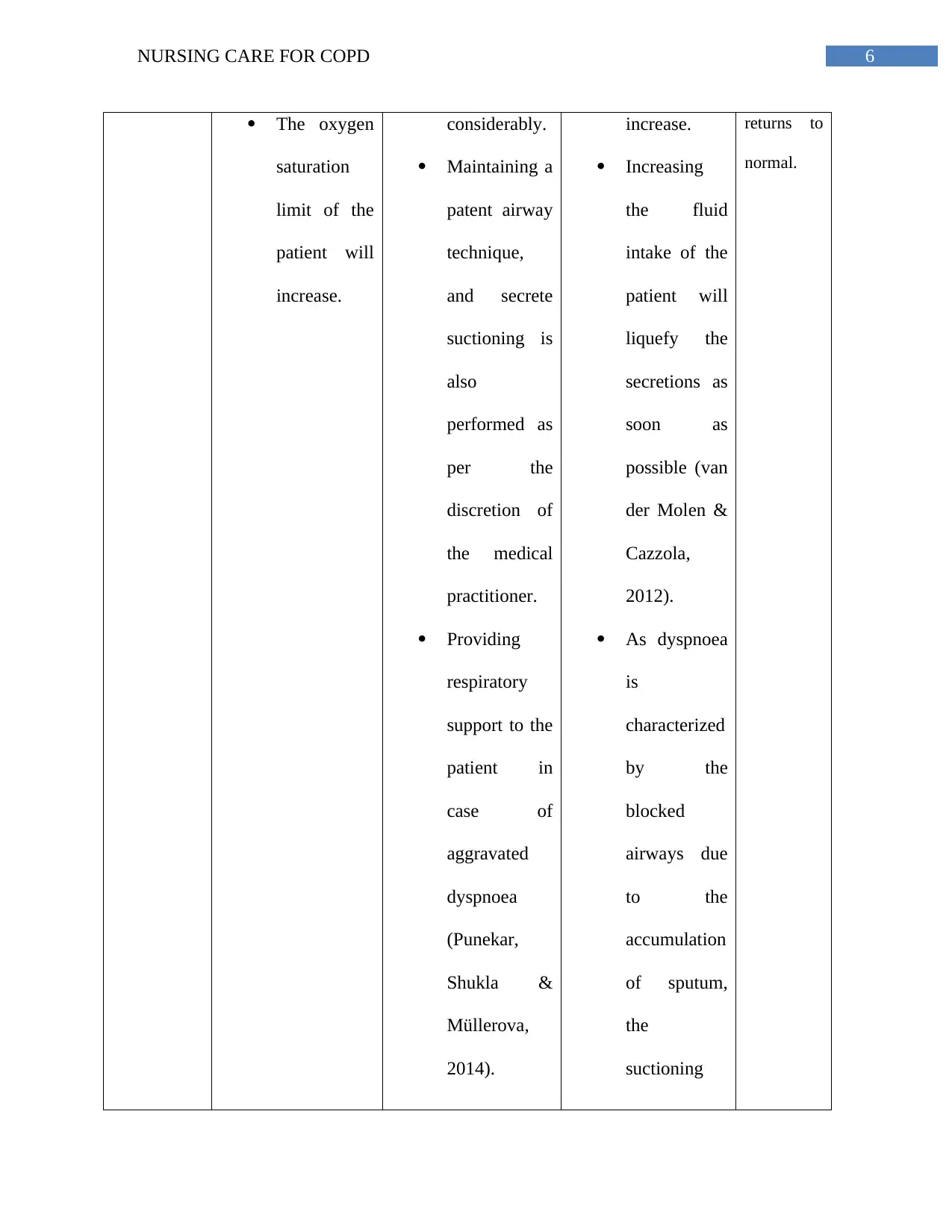
The oxygen
saturation
limit of the
patient will
increase.
considerably.
Maintaining a
patent airway
technique,
and secrete
suctioning is
also
performed as
per the
discretion of
the medical
practitioner.
Providing
respiratory
support to the
patient in
case of
aggravated
dyspnoea
(Punekar,
Shukla &
Müllerova,
2014).
increase.
Increasing
the fluid
intake of the
patient will
liquefy the
secretions as
soon as
possible (van
der Molen &
Cazzola,
2012).
As dyspnoea
is
characterized
by the
blocked
airways due
to the
accumulation
of sputum,
the
suctioning
returns to
normal.
The oxygen
saturation
limit of the
patient will
increase.
considerably.
Maintaining a
patent airway
technique,
and secrete
suctioning is
also
performed as
per the
discretion of
the medical
practitioner.
Providing
respiratory
support to the
patient in
case of
aggravated
dyspnoea
(Punekar,
Shukla &
Müllerova,
2014).
increase.
Increasing
the fluid
intake of the
patient will
liquefy the
secretions as
soon as
possible (van
der Molen &
Cazzola,
2012).
As dyspnoea
is
characterized
by the
blocked
airways due
to the
accumulation
of sputum,
the
suctioning
returns to
normal.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING CARE FOR COPD
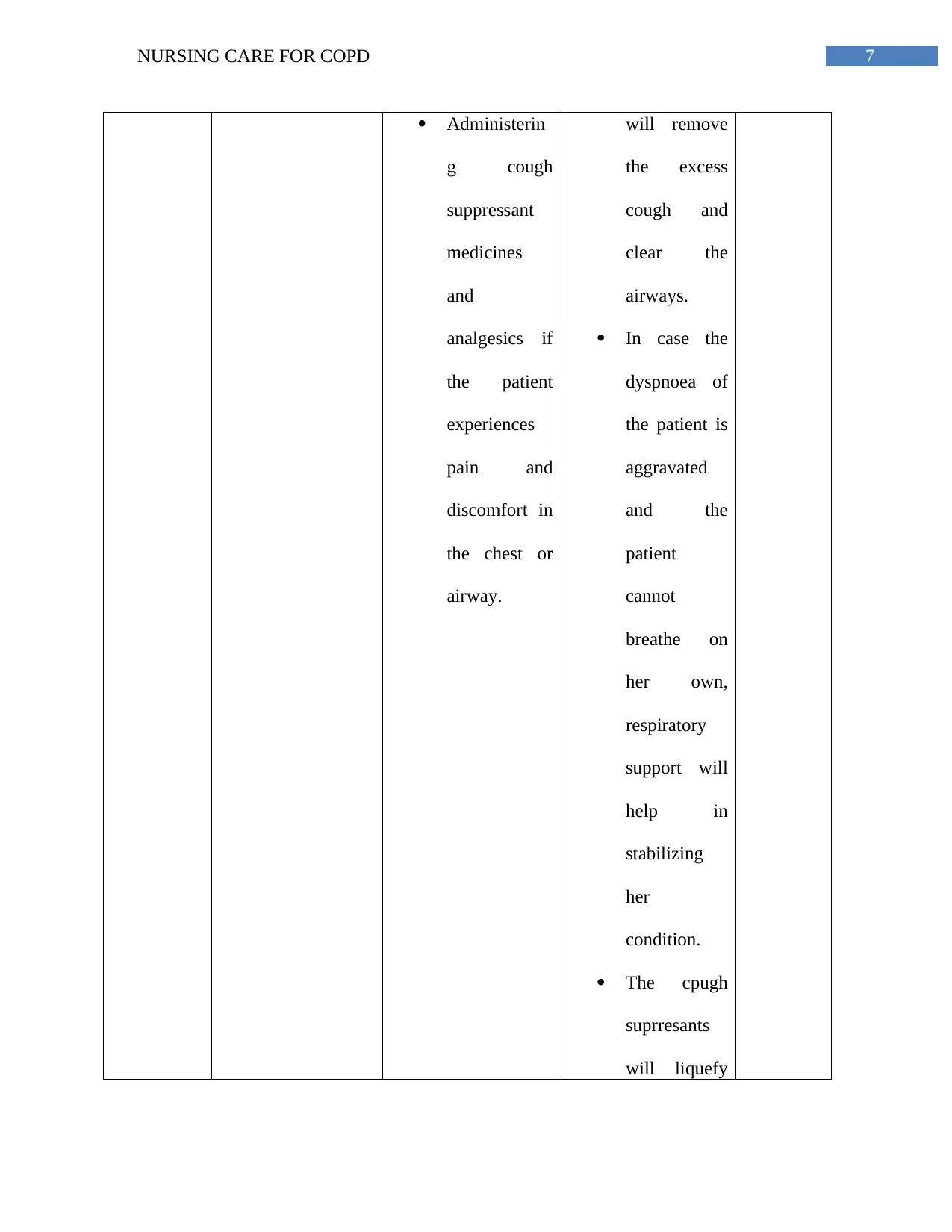
Administerin
g cough
suppressant
medicines
and
analgesics if
the patient
experiences
pain and
discomfort in
the chest or
airway.
will remove
the excess
cough and
clear the
airways.
In case the
dyspnoea of
the patient is
aggravated
and the
patient
cannot
breathe on
her own,
respiratory
support will
help in
stabilizing
her
condition.
The cpugh
suprresants
will liquefy
Administerin
g cough
suppressant
medicines
and
analgesics if
the patient
experiences
pain and
discomfort in
the chest or
airway.
will remove
the excess
cough and
clear the
airways.
In case the
dyspnoea of
the patient is
aggravated
and the
patient
cannot
breathe on
her own,
respiratory
support will
help in
stabilizing
her
condition.
The cpugh
suprresants
will liquefy
8NURSING CARE FOR COPD
the
accumulated
cough and
the mild
analgesics
will help the
patent feel
comfortable.
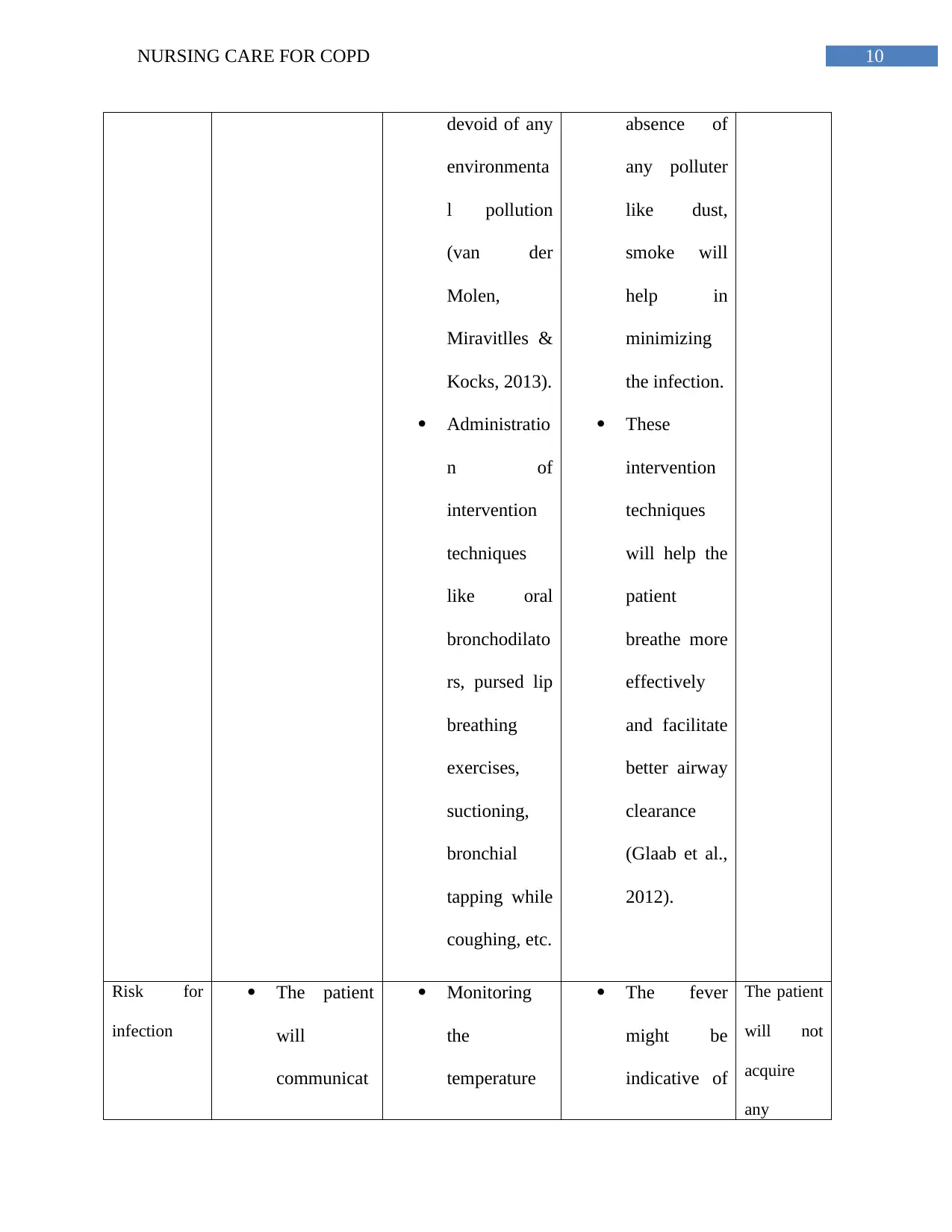
Ineffective
airway
clearance
Maintaining
the airway
patency of
the patient
with the
breathing
sounds
getting
clearer.
Demonstrati
ng breathing
interventions
to the patient
to improve
airway
Auscultation
of the
breathing
sounds of the
patient
checking for
wheezes,
crackles or
rhonchi.
Assessment
of respiratory
rate taking
into accounts
both the
inspiratory
It will
indicate if
the patient is
expressing
any
indication of
bronchospas
m.
It will assess
whether the
patient has
tachypnea
(van der
Molen,
Miravitlles &
The airway
of the
pati9ent
will be
effectively
cleared.
The patient
will face
no
difficulties
in maintain
normal
breathing
pattern.
the
accumulated
cough and
the mild
analgesics
will help the
patent feel
comfortable.
Ineffective
airway
clearance
Maintaining
the airway
patency of
the patient
with the
breathing
sounds
getting
clearer.
Demonstrati
ng breathing
interventions
to the patient
to improve
airway
Auscultation
of the
breathing
sounds of the
patient
checking for
wheezes,
crackles or
rhonchi.
Assessment
of respiratory
rate taking
into accounts
both the
inspiratory
It will
indicate if
the patient is
expressing
any
indication of
bronchospas
m.
It will assess
whether the
patient has
tachypnea
(van der
Molen,
Miravitlles &
The airway
of the
pati9ent
will be
effectively
cleared.
The patient
will face
no
difficulties
in maintain
normal
breathing
pattern.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING CARE FOR COPD
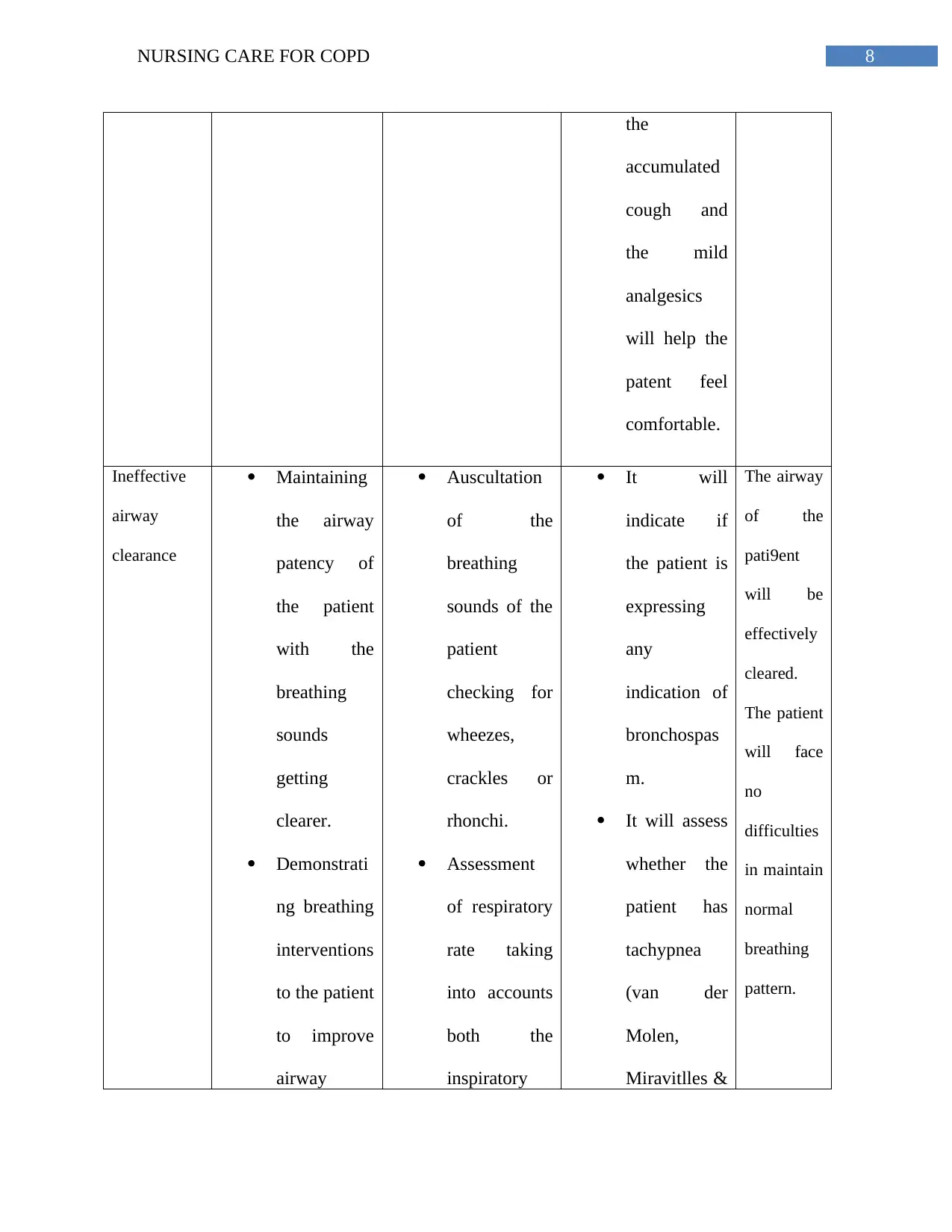
clearance by
the means of
effectively
coughing
and
secretion
removal.
and
expiratory
ratio.
Assessing the
presence of
air hunger in
the patient,
characterized
by
restlessness,
respiratory
distress, and
excessive
usage of
respiratory
muscles.
Providing a
comfortable,
safe, warm
environment
for the patient
which is
absolutely
Kocks,
2013).
Presence ofb
air hunger
i9n the
patient will
indicate at
the onset of
severe
respiratory
dysfunction
in the patient
aggravated
by any
infection of
allergic
reaction.
A warm and
comfortable
environment
will help the
patient relax,
and the
clearance by
the means of
effectively
coughing
and
secretion
removal.
and
expiratory
ratio.
Assessing the
presence of
air hunger in
the patient,
characterized
by
restlessness,
respiratory
distress, and
excessive
usage of
respiratory
muscles.
Providing a
comfortable,
safe, warm
environment
for the patient
which is
absolutely
Kocks,
2013).
Presence ofb
air hunger
i9n the
patient will
indicate at
the onset of
severe
respiratory
dysfunction
in the patient
aggravated
by any
infection of
allergic
reaction.
A warm and
comfortable
environment
will help the
patient relax,
and the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING CARE FOR COPD
devoid of any
environmenta
l pollution
(van der
Molen,
Miravitlles &
Kocks, 2013).
Administratio
n of
intervention
techniques
like oral
bronchodilato
rs, pursed lip
breathing
exercises,
suctioning,
bronchial
tapping while
coughing, etc.
absence of
any polluter
like dust,
smoke will
help in
minimizing
the infection.
These
intervention
techniques
will help the
patient
breathe more
effectively
and facilitate
better airway
clearance
(Glaab et al.,
2012).
Risk for
infection
The patient
will
communicat
Monitoring
the
temperature
The fever
might be
indicative of
The patient
will not
acquire
any
devoid of any
environmenta
l pollution
(van der
Molen,
Miravitlles &
Kocks, 2013).
Administratio
n of
intervention
techniques
like oral
bronchodilato
rs, pursed lip
breathing
exercises,
suctioning,
bronchial
tapping while
coughing, etc.
absence of
any polluter
like dust,
smoke will
help in
minimizing
the infection.
These
intervention
techniques
will help the
patient
breathe more
effectively
and facilitate
better airway
clearance
(Glaab et al.,
2012).
Risk for
infection
The patient
will
communicat
Monitoring
the
temperature
The fever
might be
indicative of
The patient
will not
acquire
any
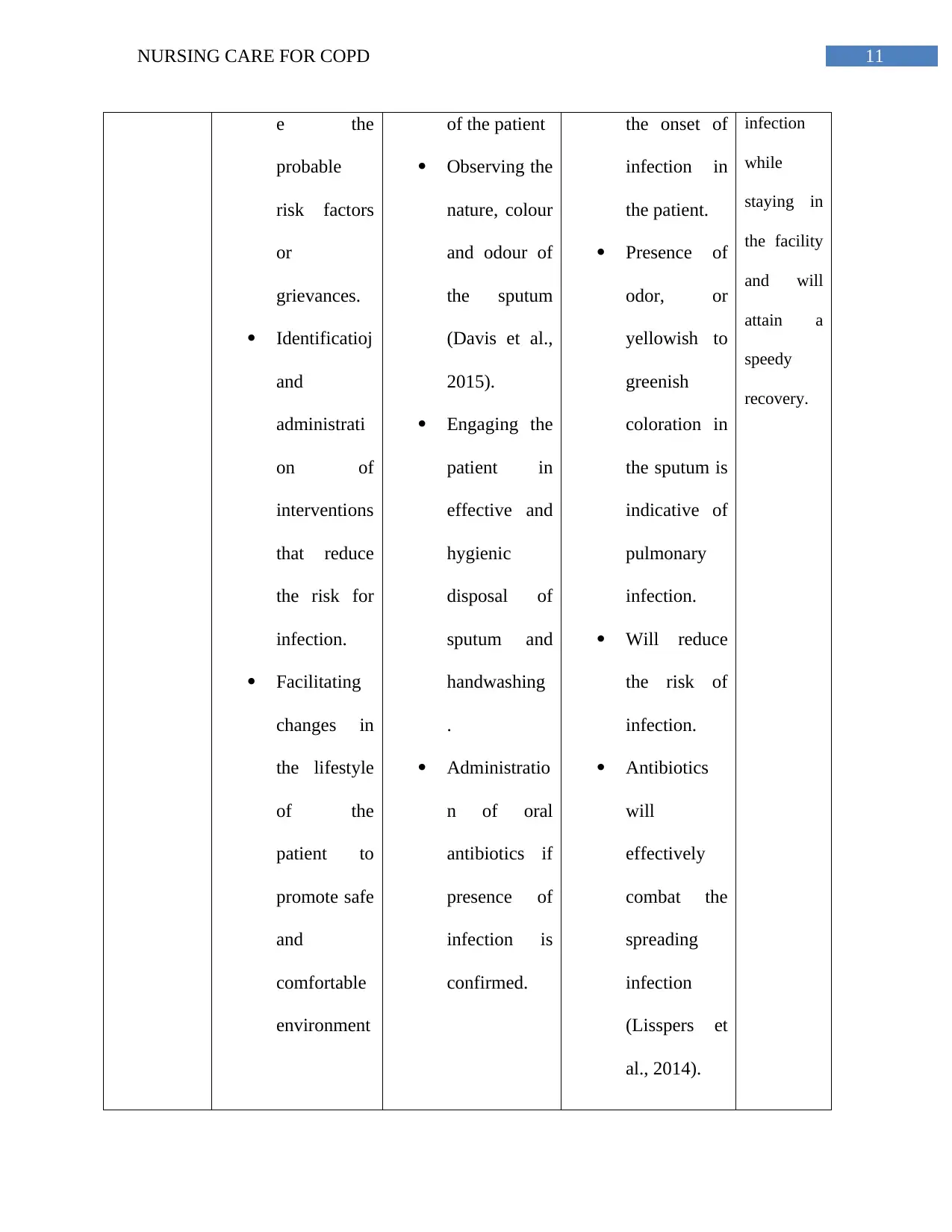
11NURSING CARE FOR COPD
e the
probable
risk factors
or
grievances.
Identificatioj
and
administrati
on of
interventions
that reduce
the risk for
infection.
Facilitating
changes in
the lifestyle
of the
patient to
promote safe
and
comfortable
environment
of the patient
Observing the
nature, colour
and odour of
the sputum
(Davis et al.,
2015).
Engaging the
patient in
effective and
hygienic
disposal of
sputum and
handwashing
.
Administratio
n of oral
antibiotics if
presence of
infection is
confirmed.
the onset of
infection in
the patient.
Presence of
odor, or
yellowish to
greenish
coloration in
the sputum is
indicative of
pulmonary
infection.
Will reduce
the risk of
infection.
Antibiotics
will
effectively
combat the
spreading
infection
(Lisspers et
al., 2014).
infection
while
staying in
the facility
and will
attain a
speedy
recovery.
e the
probable
risk factors
or
grievances.
Identificatioj
and
administrati
on of
interventions
that reduce
the risk for
infection.
Facilitating
changes in
the lifestyle
of the
patient to
promote safe
and
comfortable
environment
of the patient
Observing the
nature, colour
and odour of
the sputum
(Davis et al.,
2015).
Engaging the
patient in
effective and
hygienic
disposal of
sputum and
handwashing
.
Administratio
n of oral
antibiotics if
presence of
infection is
confirmed.
the onset of
infection in
the patient.
Presence of
odor, or
yellowish to
greenish
coloration in
the sputum is
indicative of
pulmonary
infection.
Will reduce
the risk of
infection.
Antibiotics
will
effectively
combat the
spreading
infection
(Lisspers et
al., 2014).
infection
while
staying in
the facility
and will
attain a
speedy
recovery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





