Implantable Cardioverter Defibrillator: Comprehensive Nursing Care
VerifiedAdded on 2023/05/27
|4
|1184
|408
Presentation
AI Summary
This presentation provides an overview of nursing care for patients with implantable cardioverter defibrillators (ICDs). It covers essential aspects such as patient assessment (including vital signs, physical assessment, and wound site assessment), wound care (emphasizing infection control and sterile dressing techniques), chest drain management, pain management (utilizing pain assessment scales and cautious analgesia administration), patient education on lifestyle changes and precautionary measures, and discharge planning. The presentation highlights the importance of addressing potential discomfort issues and ensuring patients understand when to seek medical help, with references to relevant research and clinical guidelines.
NURSING CARE FOR
IMPLANTABLE CARDIOVERTER
DEFIBRILLATOR.
NAME OF THE STUDENT:
NAME OF THE UNIVERSITY:
AUTHOR NOTE:
IMPLANTABLE CARDIOVERTER
DEFIBRILLATOR.
NAME OF THE STUDENT:
NAME OF THE UNIVERSITY:
AUTHOR NOTE:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BACKGROUND INFORMATION
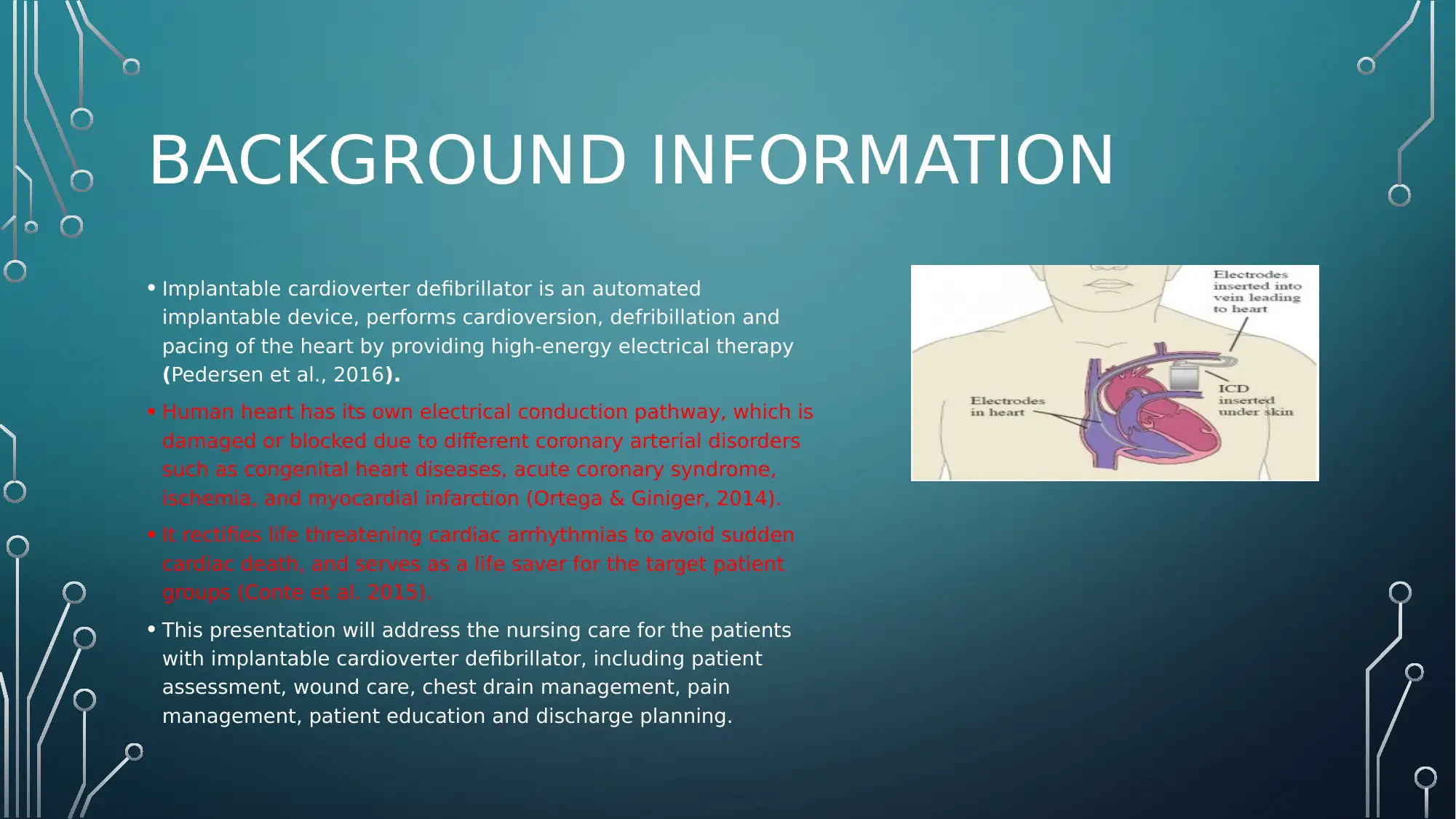
• Implantable cardioverter defibrillator is an automated
implantable device, performs cardioversion, defribillation and
pacing of the heart by providing high-energy electrical therapy
(Pedersen et al., 2016).
• Human heart has its own electrical conduction pathway, which is
damaged or blocked due to different coronary arterial disorders
such as congenital heart diseases, acute coronary syndrome,
ischemia, and myocardial infarction (Ortega & Giniger, 2014).
• It rectifies life threatening cardiac arrhythmias to avoid sudden
cardiac death, and serves as a life saver for the target patient
groups (Conte et al. 2015).
• This presentation will address the nursing care for the patients
with implantable cardioverter defibrillator, including patient
assessment, wound care, chest drain management, pain
management, patient education and discharge planning.
• Implantable cardioverter defibrillator is an automated
implantable device, performs cardioversion, defribillation and
pacing of the heart by providing high-energy electrical therapy
(Pedersen et al., 2016).
• Human heart has its own electrical conduction pathway, which is
damaged or blocked due to different coronary arterial disorders
such as congenital heart diseases, acute coronary syndrome,
ischemia, and myocardial infarction (Ortega & Giniger, 2014).
• It rectifies life threatening cardiac arrhythmias to avoid sudden
cardiac death, and serves as a life saver for the target patient
groups (Conte et al. 2015).
• This presentation will address the nursing care for the patients
with implantable cardioverter defibrillator, including patient
assessment, wound care, chest drain management, pain
management, patient education and discharge planning.
NURSING CARE
• Patient assessment is to be carried out involving vital signs assessment, physical assessment and wound site assessment.
• Vital assessment helps in assessing the physiological and metabolic processes of the patient and recognize any anomaly
before it can manifest into a complication (Storm‐Versloot et al., 2014).
• Assessing the wound for any signs of redness, pain and swelling in the insertion site. Nurse would need to follow the infection
control protocol diligently. Nurse will have to apply sterile dressing and keep changing the dressing once every day until the
wound heals completely.
• As mentioned by Leung and Danik (2016), a single dose of cefazolin within an hour prior to implantation significantly reduced
the risk of infection as well.
• Inui and Bandyk (2015) have recommended that limiting the duration for temporary pacing can also reduce the rate of
infection after the initial few days after the implant.
• chest drain management will involve regular cleaning or emptying of the drain to avoid infection or blockage.
• The nurse might use pain assessment scales such as PQRST or 1-10 numerical pain scoring technique. The nurse will have to
provide analgesia very cautiously concerning the fragile condition of the patient.
• After critical implantation surgery, the patent might feel extremely groggy and not be able to go through the PQRST, in such
cases the use of VAS or visual analogue scale can be useful (Wylde et al., 2015).
• Patient education on lifestyle changes and precautionary measures after the discharge such as dietary modifications, medication
management and activity restriction is to be given. Patients must also be educated to report issues with functionality of the device
and any discomfort.
• The lack of this information and strategies are not properly disseminated to the patient and their family members or carers will
directly impact the safety and wellbeing of the patient post the discharge and will stall the recovery process (A Lane, V Barker &
YH Lip, 2015).
• Hence, the nurse will also need to be address and discuss the possible discomfort issues that the patient may encounter
and how to address it effectively in the education and discharge planning so that patients understand to seek medical help
in any emergencies (Ting & Lee, 2015).
• Patient assessment is to be carried out involving vital signs assessment, physical assessment and wound site assessment.
• Vital assessment helps in assessing the physiological and metabolic processes of the patient and recognize any anomaly
before it can manifest into a complication (Storm‐Versloot et al., 2014).
• Assessing the wound for any signs of redness, pain and swelling in the insertion site. Nurse would need to follow the infection
control protocol diligently. Nurse will have to apply sterile dressing and keep changing the dressing once every day until the
wound heals completely.
• As mentioned by Leung and Danik (2016), a single dose of cefazolin within an hour prior to implantation significantly reduced
the risk of infection as well.
• Inui and Bandyk (2015) have recommended that limiting the duration for temporary pacing can also reduce the rate of
infection after the initial few days after the implant.
• chest drain management will involve regular cleaning or emptying of the drain to avoid infection or blockage.
• The nurse might use pain assessment scales such as PQRST or 1-10 numerical pain scoring technique. The nurse will have to
provide analgesia very cautiously concerning the fragile condition of the patient.
• After critical implantation surgery, the patent might feel extremely groggy and not be able to go through the PQRST, in such
cases the use of VAS or visual analogue scale can be useful (Wylde et al., 2015).
• Patient education on lifestyle changes and precautionary measures after the discharge such as dietary modifications, medication
management and activity restriction is to be given. Patients must also be educated to report issues with functionality of the device
and any discomfort.
• The lack of this information and strategies are not properly disseminated to the patient and their family members or carers will
directly impact the safety and wellbeing of the patient post the discharge and will stall the recovery process (A Lane, V Barker &
YH Lip, 2015).
• Hence, the nurse will also need to be address and discuss the possible discomfort issues that the patient may encounter
and how to address it effectively in the education and discharge planning so that patients understand to seek medical help
in any emergencies (Ting & Lee, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES:
• A Lane, D., V Barker, R., & YH Lip, G. (2015). Best practice for atrial fibrillation patient education. Current pharmaceutical design, 21(5), 533-543.
• Chou, R., Gordon, D. B., de Leon-Casasola, O. A., Rosenberg, J. M., Bickler, S., Brennan, T., ... & Griffith, S. (2016). Management of Postoperative Pain: a clinical practice guideline from the American
pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' committee on regional anesthesia, executive committee, and
administrative council. The Journal of Pain, 17(2), 131-157.
• Conte, G., Sieira, J., Ciconte, G., De Asmundis, C., Chierchia, G. B., Baltogiannis, G., ... & Wauters, K. (2015). Implantable cardioverter-defibrillator therapy in Brugada syndrome: a 20-year single-
center experience. Journal of the American College of Cardiology, 65(9), 879-888.
• Inui, T., & Bandyk, D. F. (2015, September). Vascular surgical site infection: risk factors and preventive measures. In Seminars in vascular surgery (Vol. 28, No. 3-4, pp. 201-207). WB Saunders.
• Leung, S., & Danik, S. (2016). Prevention, diagnosis, and treatment of cardiac implantable electronic device infections. Current cardiology reports, 18(6), 58.
• Moffatt, C., Murray, S., Keeley, V., & Aubeeluck, A. (2017). Non‐adherence to treatment of chronic wounds: patient versus professional perspectives. International wound journal, 14(6), 1305-1312.
• Ortega, D. F., & Giniger, A. G. (2014). U.S. Patent No. 8,812,106. Washington, DC: U.S. Patent and Trademark Office.
• Pedersen, S. S., Knudsen, C., Dilling, K., Sandgaard, N. C., & Johansen, J. B. (2016). Living with an implantable cardioverter defibrillator: patients' preferences and needs for information provision
and care options. Ep Europace, 19(6), 983-990.
• Rch.org.au (2018). Clinical Guidelines (Nursing) : Chest Drain Management. [Online]. Retrieved from https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
[Accessed on 11th Dec]
• Storm‐Versloot, M. N., Verweij, L., Lucas, C., Ludikhuize, J., Goslings, J. C., Legemate, D. A., & Vermeulen, H. (2014). Clinical relevance of routinely measured vital signs in hospitalized patients: a
systematic review. Journal of Nursing Scholarship, 46(1), 39-49.
• Ting, F. F., & Lee, G. A. (2015). Nurses' knowledge of caring for patients with ICDs. British Journal of Cardiac Nursing, 10(6), 296-302.
• Wylde, V., MacKichan, F., Bruce, J., & Gooberman‐Hill, R. (2015). Assessment of chronic post‐surgical pain after knee replacement: Development of a core outcome set. European Journal of
Pain, 19(5), 611-620.
• A Lane, D., V Barker, R., & YH Lip, G. (2015). Best practice for atrial fibrillation patient education. Current pharmaceutical design, 21(5), 533-543.
• Chou, R., Gordon, D. B., de Leon-Casasola, O. A., Rosenberg, J. M., Bickler, S., Brennan, T., ... & Griffith, S. (2016). Management of Postoperative Pain: a clinical practice guideline from the American
pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' committee on regional anesthesia, executive committee, and
administrative council. The Journal of Pain, 17(2), 131-157.
• Conte, G., Sieira, J., Ciconte, G., De Asmundis, C., Chierchia, G. B., Baltogiannis, G., ... & Wauters, K. (2015). Implantable cardioverter-defibrillator therapy in Brugada syndrome: a 20-year single-
center experience. Journal of the American College of Cardiology, 65(9), 879-888.
• Inui, T., & Bandyk, D. F. (2015, September). Vascular surgical site infection: risk factors and preventive measures. In Seminars in vascular surgery (Vol. 28, No. 3-4, pp. 201-207). WB Saunders.
• Leung, S., & Danik, S. (2016). Prevention, diagnosis, and treatment of cardiac implantable electronic device infections. Current cardiology reports, 18(6), 58.
• Moffatt, C., Murray, S., Keeley, V., & Aubeeluck, A. (2017). Non‐adherence to treatment of chronic wounds: patient versus professional perspectives. International wound journal, 14(6), 1305-1312.
• Ortega, D. F., & Giniger, A. G. (2014). U.S. Patent No. 8,812,106. Washington, DC: U.S. Patent and Trademark Office.
• Pedersen, S. S., Knudsen, C., Dilling, K., Sandgaard, N. C., & Johansen, J. B. (2016). Living with an implantable cardioverter defibrillator: patients' preferences and needs for information provision
and care options. Ep Europace, 19(6), 983-990.
• Rch.org.au (2018). Clinical Guidelines (Nursing) : Chest Drain Management. [Online]. Retrieved from https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
[Accessed on 11th Dec]
• Storm‐Versloot, M. N., Verweij, L., Lucas, C., Ludikhuize, J., Goslings, J. C., Legemate, D. A., & Vermeulen, H. (2014). Clinical relevance of routinely measured vital signs in hospitalized patients: a
systematic review. Journal of Nursing Scholarship, 46(1), 39-49.
• Ting, F. F., & Lee, G. A. (2015). Nurses' knowledge of caring for patients with ICDs. British Journal of Cardiac Nursing, 10(6), 296-302.
• Wylde, V., MacKichan, F., Bruce, J., & Gooberman‐Hill, R. (2015). Assessment of chronic post‐surgical pain after knee replacement: Development of a core outcome set. European Journal of
Pain, 19(5), 611-620.
1 out of 4
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




