Nursing Care Plan: Detailed Analysis of Mr. McFarlane's Case Study
VerifiedAdded on 2023/01/06
|18
|4502
|53
Homework Assignment
AI Summary
This homework assignment presents a comprehensive nursing care plan for Mr. McFarlane, a patient with multiple health issues including Type II Diabetes, COPD, Osteoarthritis, Peripheral Vascular Disease (PVD), and obesity. The assignment begins with a nursing admission form, followed by a detailed care plan outlining nursing diagnoses, interventions, and expected outcomes, considering the scope of practice for an Enrolled Nurse. The assignment addresses patient independence through privacy, dignity, informed consent, and pain management. It includes BMI calculation, strategies for skin integrity, and nutritional considerations. Additionally, the assignment covers respiratory interventions for COPD, including oxygen therapy, positioning, and breathing exercises. It highlights the importance of multi-disciplinary team collaboration and provides detailed responses to each question, demonstrating a thorough understanding of patient care and best practices in nursing.
Nursing Care Plan
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Table of Contents
Question 1...................................................................................................................................3
Question 2...................................................................................................................................6
Question 3...................................................................................................................................8
Question 4.................................................................................................................................10
Question 5.................................................................................................................................11
Question 6.................................................................................................................................13
Question 7.................................................................................................................................14
Question 8.................................................................................................................................15
Clinical report documentation................................................................................................17
REFERENCES..............................................................................................................................18
Question 1...................................................................................................................................3
Question 2...................................................................................................................................6
Question 3...................................................................................................................................8
Question 4.................................................................................................................................10
Question 5.................................................................................................................................11
Question 6.................................................................................................................................13
Question 7.................................................................................................................................14
Question 8.................................................................................................................................15
Clinical report documentation................................................................................................17
REFERENCES..............................................................................................................................18
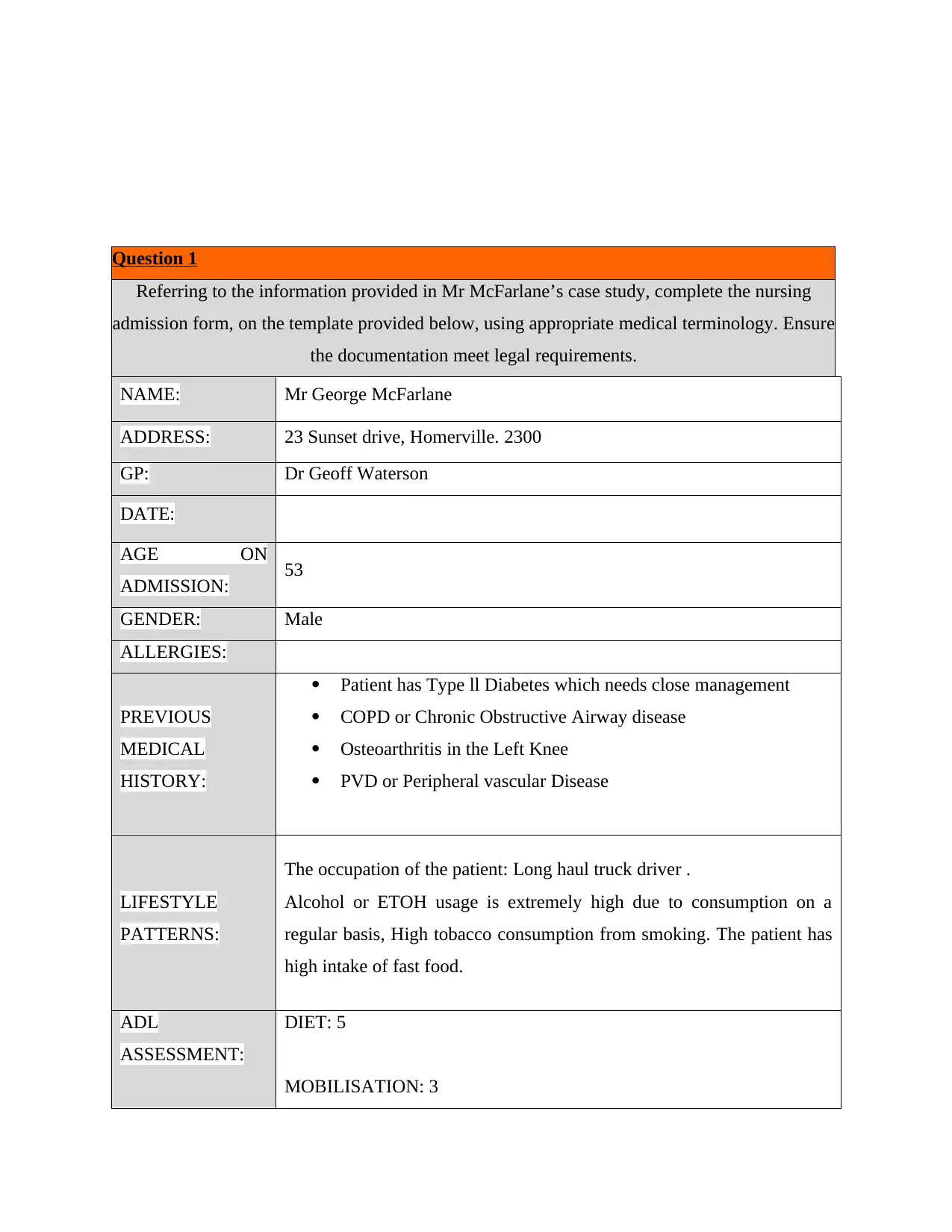
Question 1
Referring to the information provided in Mr McFarlane’s case study, complete the nursing
admission form, on the template provided below, using appropriate medical terminology. Ensure
the documentation meet legal requirements.
NAME: Mr George McFarlane
ADDRESS: 23 Sunset drive, Homerville. 2300
GP: Dr Geoff Waterson
DATE:
AGE ON
ADMISSION: 53
GENDER: Male
ALLERGIES:
PREVIOUS
MEDICAL
HISTORY:
Patient has Type ll Diabetes which needs close management
COPD or Chronic Obstructive Airway disease
Osteoarthritis in the Left Knee
PVD or Peripheral vascular Disease
LIFESTYLE
PATTERNS:
The occupation of the patient: Long haul truck driver .
Alcohol or ETOH usage is extremely high due to consumption on a
regular basis, High tobacco consumption from smoking. The patient has
high intake of fast food.
ADL
ASSESSMENT:
DIET: 5
MOBILISATION: 3
Referring to the information provided in Mr McFarlane’s case study, complete the nursing
admission form, on the template provided below, using appropriate medical terminology. Ensure
the documentation meet legal requirements.
NAME: Mr George McFarlane
ADDRESS: 23 Sunset drive, Homerville. 2300
GP: Dr Geoff Waterson
DATE:
AGE ON
ADMISSION: 53
GENDER: Male
ALLERGIES:
PREVIOUS
MEDICAL
HISTORY:
Patient has Type ll Diabetes which needs close management
COPD or Chronic Obstructive Airway disease
Osteoarthritis in the Left Knee
PVD or Peripheral vascular Disease
LIFESTYLE
PATTERNS:
The occupation of the patient: Long haul truck driver .
Alcohol or ETOH usage is extremely high due to consumption on a
regular basis, High tobacco consumption from smoking. The patient has
high intake of fast food.
ADL
ASSESSMENT:
DIET: 5
MOBILISATION: 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
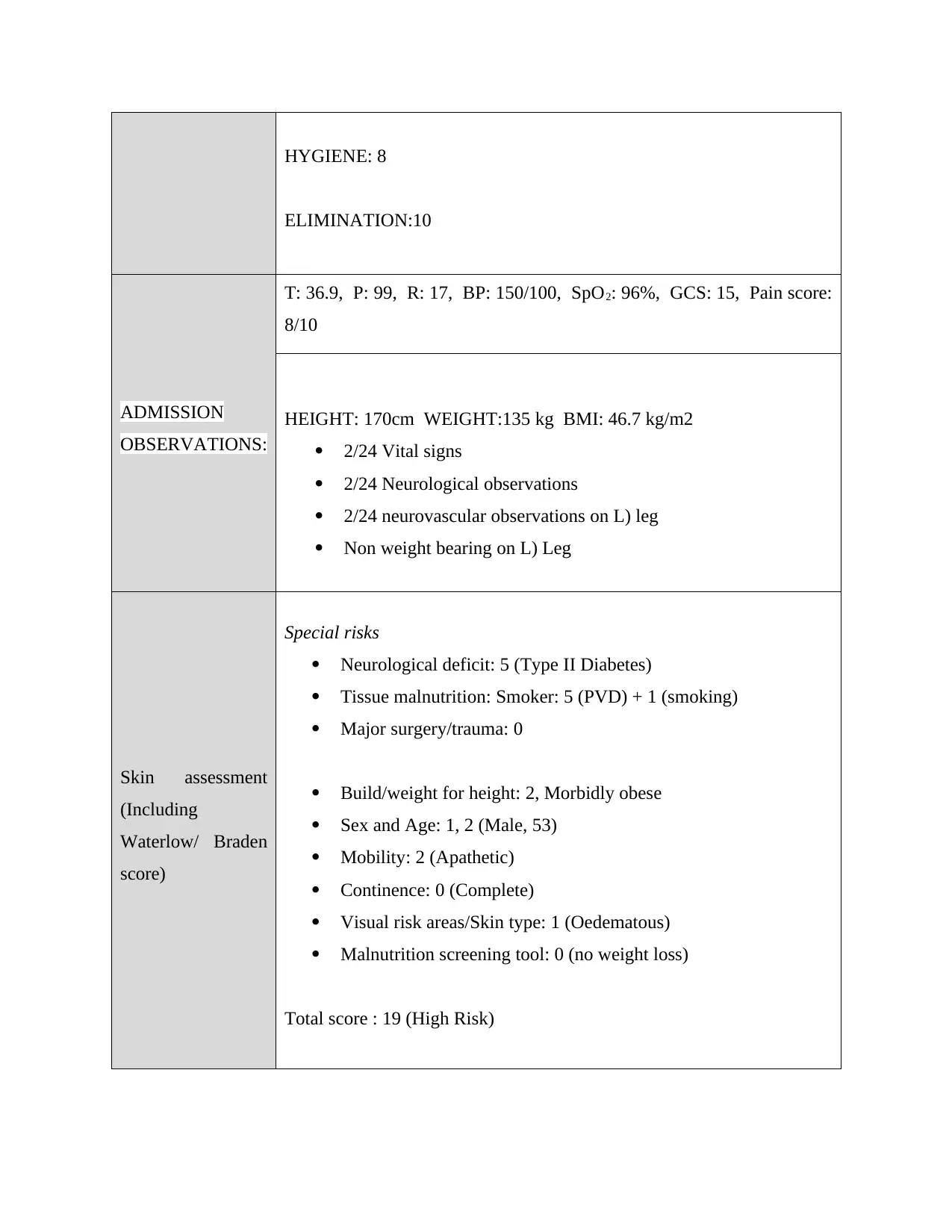
HYGIENE: 8
ELIMINATION:10
ADMISSION
OBSERVATIONS:
T: 36.9, P: 99, R: 17, BP: 150/100, SpO2: 96%, GCS: 15, Pain score:
8/10
HEIGHT: 170cm WEIGHT:135 kg BMI: 46.7 kg/m2
2/24 Vital signs
2/24 Neurological observations
2/24 neurovascular observations on L) leg
Non weight bearing on L) Leg
Skin assessment
(Including
Waterlow/ Braden
score)
Special risks
Neurological deficit: 5 (Type II Diabetes)
Tissue malnutrition: Smoker: 5 (PVD) + 1 (smoking)
Major surgery/trauma: 0
Build/weight for height: 2, Morbidly obese
Sex and Age: 1, 2 (Male, 53)
Mobility: 2 (Apathetic)
Continence: 0 (Complete)
Visual risk areas/Skin type: 1 (Oedematous)
Malnutrition screening tool: 0 (no weight loss)
Total score : 19 (High Risk)
ELIMINATION:10
ADMISSION
OBSERVATIONS:
T: 36.9, P: 99, R: 17, BP: 150/100, SpO2: 96%, GCS: 15, Pain score:
8/10
HEIGHT: 170cm WEIGHT:135 kg BMI: 46.7 kg/m2
2/24 Vital signs
2/24 Neurological observations
2/24 neurovascular observations on L) leg
Non weight bearing on L) Leg
Skin assessment
(Including
Waterlow/ Braden
score)
Special risks
Neurological deficit: 5 (Type II Diabetes)
Tissue malnutrition: Smoker: 5 (PVD) + 1 (smoking)
Major surgery/trauma: 0
Build/weight for height: 2, Morbidly obese
Sex and Age: 1, 2 (Male, 53)
Mobility: 2 (Apathetic)
Continence: 0 (Complete)
Visual risk areas/Skin type: 1 (Oedematous)
Malnutrition screening tool: 0 (no weight loss)
Total score : 19 (High Risk)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
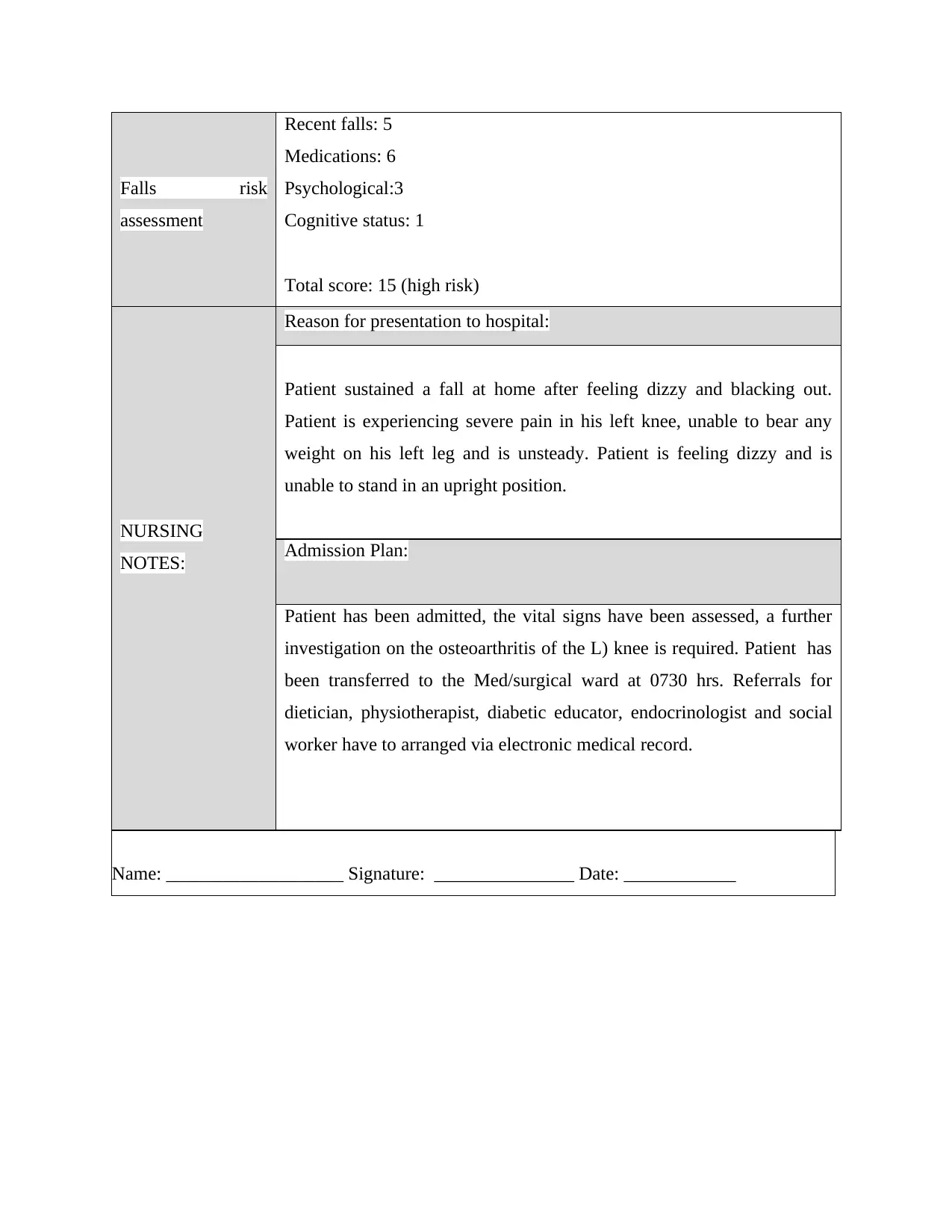
Falls risk
assessment
Recent falls: 5
Medications: 6
Psychological:3
Cognitive status: 1
Total score: 15 (high risk)
NURSING
NOTES:
Reason for presentation to hospital:
Patient sustained a fall at home after feeling dizzy and blacking out.
Patient is experiencing severe pain in his left knee, unable to bear any
weight on his left leg and is unsteady. Patient is feeling dizzy and is
unable to stand in an upright position.
Admission Plan:
Patient has been admitted, the vital signs have been assessed, a further
investigation on the osteoarthritis of the L) knee is required. Patient has
been transferred to the Med/surgical ward at 0730 hrs. Referrals for
dietician, physiotherapist, diabetic educator, endocrinologist and social
worker have to arranged via electronic medical record.
Name: ___________________ Signature: _______________ Date: ____________
assessment
Recent falls: 5
Medications: 6
Psychological:3
Cognitive status: 1
Total score: 15 (high risk)
NURSING
NOTES:
Reason for presentation to hospital:
Patient sustained a fall at home after feeling dizzy and blacking out.
Patient is experiencing severe pain in his left knee, unable to bear any
weight on his left leg and is unsteady. Patient is feeling dizzy and is
unable to stand in an upright position.
Admission Plan:
Patient has been admitted, the vital signs have been assessed, a further
investigation on the osteoarthritis of the L) knee is required. Patient has
been transferred to the Med/surgical ward at 0730 hrs. Referrals for
dietician, physiotherapist, diabetic educator, endocrinologist and social
worker have to arranged via electronic medical record.
Name: ___________________ Signature: _______________ Date: ____________
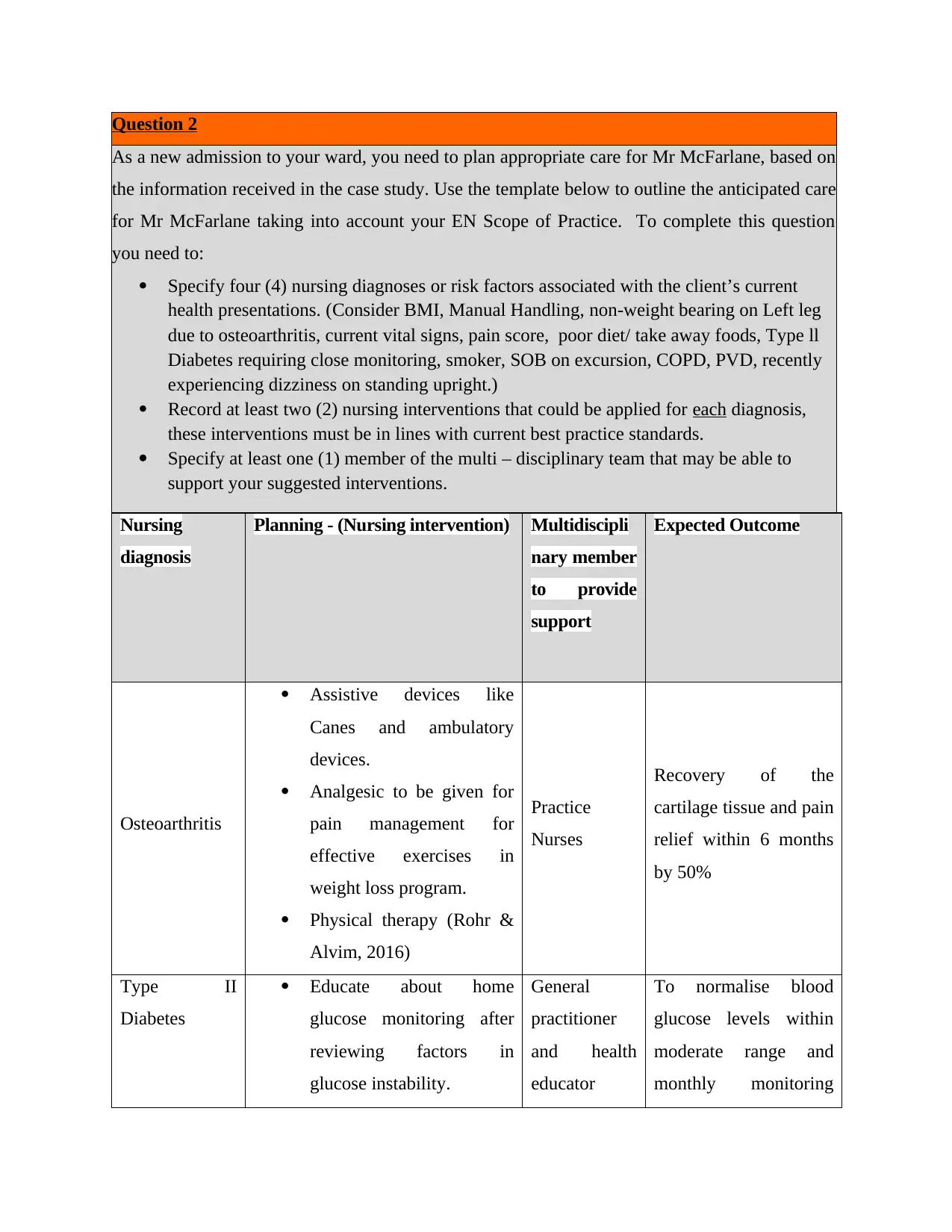
Question 2
As a new admission to your ward, you need to plan appropriate care for Mr McFarlane, based on
the information received in the case study. Use the template below to outline the anticipated care
for Mr McFarlane taking into account your EN Scope of Practice. To complete this question
you need to:
Specify four (4) nursing diagnoses or risk factors associated with the client’s current
health presentations. (Consider BMI, Manual Handling, non-weight bearing on Left leg
due to osteoarthritis, current vital signs, pain score, poor diet/ take away foods, Type ll
Diabetes requiring close monitoring, smoker, SOB on excursion, COPD, PVD, recently
experiencing dizziness on standing upright.)
Record at least two (2) nursing interventions that could be applied for each diagnosis,
these interventions must be in lines with current best practice standards.
Specify at least one (1) member of the multi – disciplinary team that may be able to
support your suggested interventions.
Nursing
diagnosis
Planning - (Nursing intervention) Multidiscipli
nary member
to provide
support
Expected Outcome
Osteoarthritis
Assistive devices like
Canes and ambulatory
devices.
Analgesic to be given for
pain management for
effective exercises in
weight loss program.
Physical therapy (Rohr &
Alvim, 2016)
Practice
Nurses
Recovery of the
cartilage tissue and pain
relief within 6 months
by 50%
Type II
Diabetes
Educate about home
glucose monitoring after
reviewing factors in
glucose instability.
General
practitioner
and health
educator
To normalise blood
glucose levels within
moderate range and
monthly monitoring
As a new admission to your ward, you need to plan appropriate care for Mr McFarlane, based on
the information received in the case study. Use the template below to outline the anticipated care
for Mr McFarlane taking into account your EN Scope of Practice. To complete this question
you need to:
Specify four (4) nursing diagnoses or risk factors associated with the client’s current
health presentations. (Consider BMI, Manual Handling, non-weight bearing on Left leg
due to osteoarthritis, current vital signs, pain score, poor diet/ take away foods, Type ll
Diabetes requiring close monitoring, smoker, SOB on excursion, COPD, PVD, recently
experiencing dizziness on standing upright.)
Record at least two (2) nursing interventions that could be applied for each diagnosis,
these interventions must be in lines with current best practice standards.
Specify at least one (1) member of the multi – disciplinary team that may be able to
support your suggested interventions.
Nursing
diagnosis
Planning - (Nursing intervention) Multidiscipli
nary member
to provide
support
Expected Outcome
Osteoarthritis
Assistive devices like
Canes and ambulatory
devices.
Analgesic to be given for
pain management for
effective exercises in
weight loss program.
Physical therapy (Rohr &
Alvim, 2016)
Practice
Nurses
Recovery of the
cartilage tissue and pain
relief within 6 months
by 50%
Type II
Diabetes
Educate about home
glucose monitoring after
reviewing factors in
glucose instability.
General
practitioner
and health
educator
To normalise blood
glucose levels within
moderate range and
monthly monitoring
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Checking viability of
insulin and reviewing type
of insulin used.
(AM & San Martín
Rodríguez, 2020).
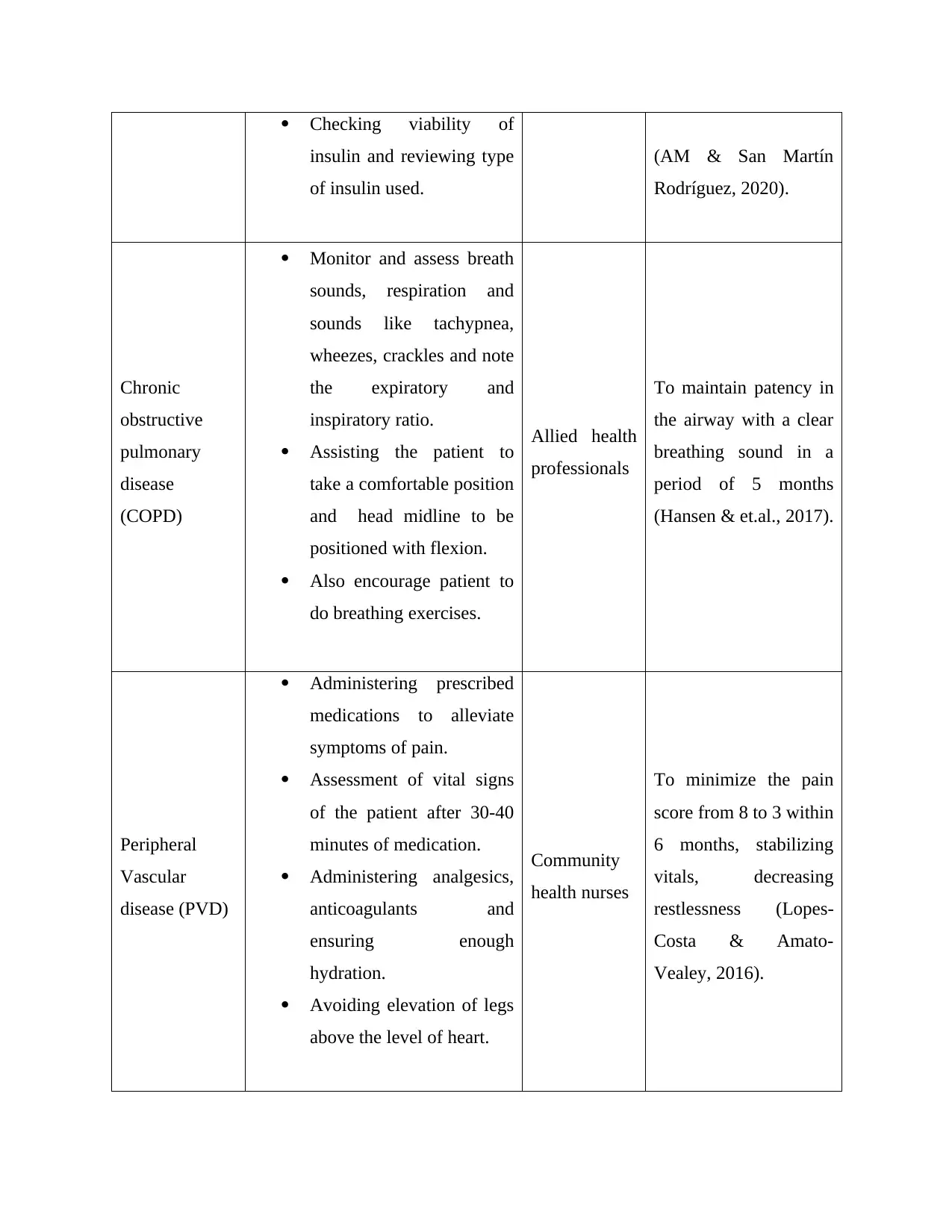
Chronic
obstructive
pulmonary
disease
(COPD)
Monitor and assess breath
sounds, respiration and
sounds like tachypnea,
wheezes, crackles and note
the expiratory and
inspiratory ratio.
Assisting the patient to
take a comfortable position
and head midline to be
positioned with flexion.
Also encourage patient to
do breathing exercises.
Allied health
professionals
To maintain patency in
the airway with a clear
breathing sound in a
period of 5 months
(Hansen & et.al., 2017).
Peripheral
Vascular
disease (PVD)
Administering prescribed
medications to alleviate
symptoms of pain.
Assessment of vital signs
of the patient after 30-40
minutes of medication.
Administering analgesics,
anticoagulants and
ensuring enough
hydration.
Avoiding elevation of legs
above the level of heart.
Community
health nurses
To minimize the pain
score from 8 to 3 within
6 months, stabilizing
vitals, decreasing
restlessness (Lopes-
Costa & Amato-
Vealey, 2016).
insulin and reviewing type
of insulin used.
(AM & San Martín
Rodríguez, 2020).
Chronic
obstructive
pulmonary
disease
(COPD)
Monitor and assess breath
sounds, respiration and
sounds like tachypnea,
wheezes, crackles and note
the expiratory and
inspiratory ratio.
Assisting the patient to
take a comfortable position
and head midline to be
positioned with flexion.
Also encourage patient to
do breathing exercises.
Allied health
professionals
To maintain patency in
the airway with a clear
breathing sound in a
period of 5 months
(Hansen & et.al., 2017).
Peripheral
Vascular
disease (PVD)
Administering prescribed
medications to alleviate
symptoms of pain.
Assessment of vital signs
of the patient after 30-40
minutes of medication.
Administering analgesics,
anticoagulants and
ensuring enough
hydration.
Avoiding elevation of legs
above the level of heart.
Community
health nurses
To minimize the pain
score from 8 to 3 within
6 months, stabilizing
vitals, decreasing
restlessness (Lopes-
Costa & Amato-
Vealey, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
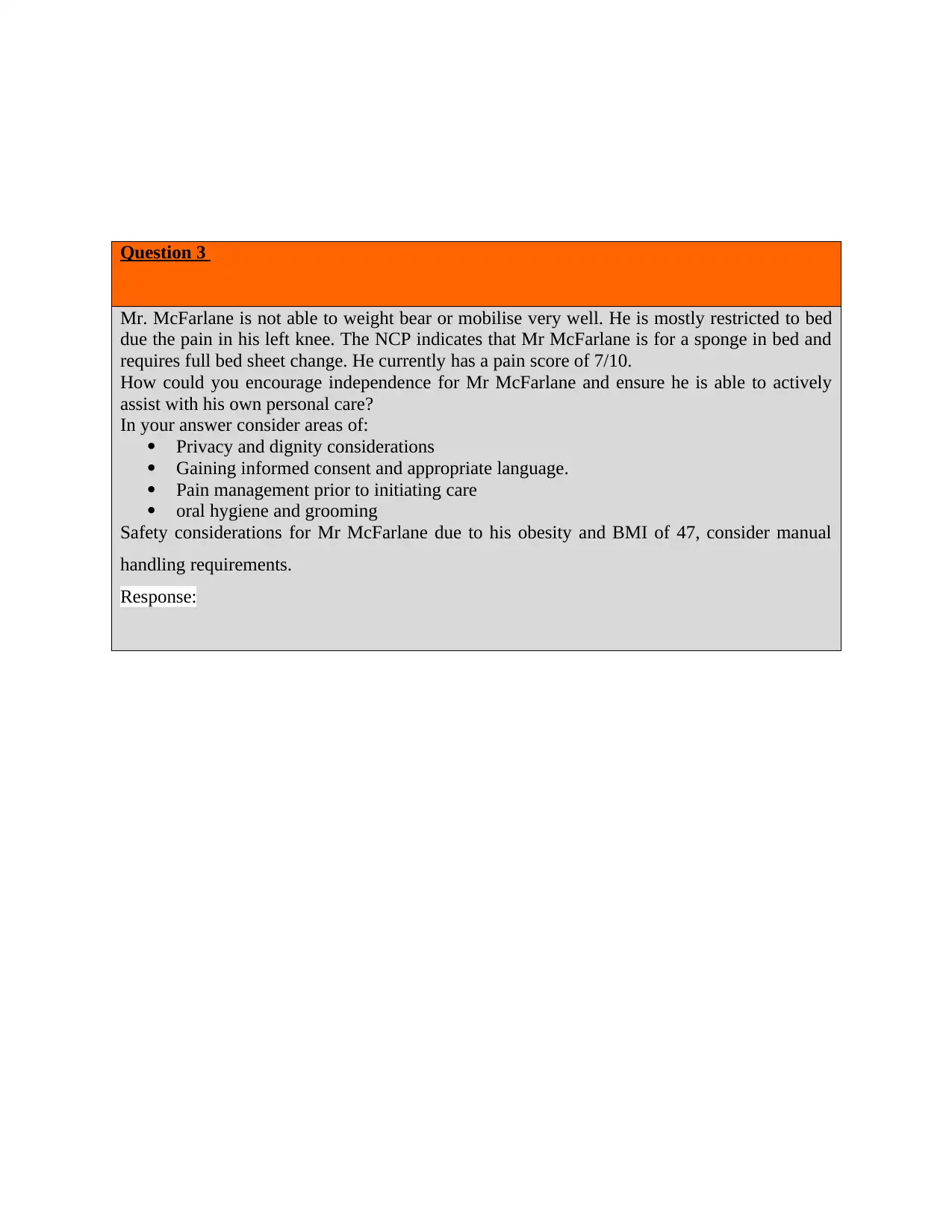
Question 3
Mr. McFarlane is not able to weight bear or mobilise very well. He is mostly restricted to bed
due the pain in his left knee. The NCP indicates that Mr McFarlane is for a sponge in bed and
requires full bed sheet change. He currently has a pain score of 7/10.
How could you encourage independence for Mr McFarlane and ensure he is able to actively
assist with his own personal care?
In your answer consider areas of:
Privacy and dignity considerations
Gaining informed consent and appropriate language.
Pain management prior to initiating care
oral hygiene and grooming
Safety considerations for Mr McFarlane due to his obesity and BMI of 47, consider manual
handling requirements.
Response:
Mr. McFarlane is not able to weight bear or mobilise very well. He is mostly restricted to bed
due the pain in his left knee. The NCP indicates that Mr McFarlane is for a sponge in bed and
requires full bed sheet change. He currently has a pain score of 7/10.
How could you encourage independence for Mr McFarlane and ensure he is able to actively
assist with his own personal care?
In your answer consider areas of:
Privacy and dignity considerations
Gaining informed consent and appropriate language.
Pain management prior to initiating care
oral hygiene and grooming
Safety considerations for Mr McFarlane due to his obesity and BMI of 47, consider manual
handling requirements.
Response:

Self -management and self-care support consists of a comprehensive way to assist the patient
and not only supply patients with information. A committed patient-centred care has to be
devised for Mr.McFarlane to enable him to manage health on a regular basis and take active
role in his healthcare. A compassionate and complete care has to be made in which whole team
has to be plan, carry out and follow up on patient visits. Planning the patient visits has to focus
upon care management and prevention instead of acute or critical care. Mr.McFarlane has to be
involved in the goal setting and his perspectives, needs and requirements have to be assessed.
According to his understanding levels and education, provision of customised skill and training
have to be used while taking care of the culture, values, beliefs and demands. The self care
program should be based on privacy and dignity considerations such as not breaching the
personal space of Mr.McFarlane and entering in the room while curtains or door is closed for
maintaining privacy. The removal of clothing should be done with a consent and appropriate
hospital gown have to be given. Religious values, gender based concerns and individual views
have to be respected and sensitivity should be there. Importance of personal hygiene should be
taught with regular oral and grooming practices. Pain management has to be administered
before initiating care. Informed consent has to be obtained and appropriate language has to be
used while informing the patients regarding decisions in self care. Referrals to community
resources have to be made considering his existing health condition for programs such as
healthy lifestyle, following a moderate exercise plan, programs to quit smoking and minimize
alcohol consumption. The follow up of patients has to be done periodically through phone, text
messages, email and overall inducing a high motivation level to encourage self-care (Duprez &
et.al., 2017).
and not only supply patients with information. A committed patient-centred care has to be
devised for Mr.McFarlane to enable him to manage health on a regular basis and take active
role in his healthcare. A compassionate and complete care has to be made in which whole team
has to be plan, carry out and follow up on patient visits. Planning the patient visits has to focus
upon care management and prevention instead of acute or critical care. Mr.McFarlane has to be
involved in the goal setting and his perspectives, needs and requirements have to be assessed.
According to his understanding levels and education, provision of customised skill and training
have to be used while taking care of the culture, values, beliefs and demands. The self care
program should be based on privacy and dignity considerations such as not breaching the
personal space of Mr.McFarlane and entering in the room while curtains or door is closed for
maintaining privacy. The removal of clothing should be done with a consent and appropriate
hospital gown have to be given. Religious values, gender based concerns and individual views
have to be respected and sensitivity should be there. Importance of personal hygiene should be
taught with regular oral and grooming practices. Pain management has to be administered
before initiating care. Informed consent has to be obtained and appropriate language has to be
used while informing the patients regarding decisions in self care. Referrals to community
resources have to be made considering his existing health condition for programs such as
healthy lifestyle, following a moderate exercise plan, programs to quit smoking and minimize
alcohol consumption. The follow up of patients has to be done periodically through phone, text
messages, email and overall inducing a high motivation level to encourage self-care (Duprez &
et.al., 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
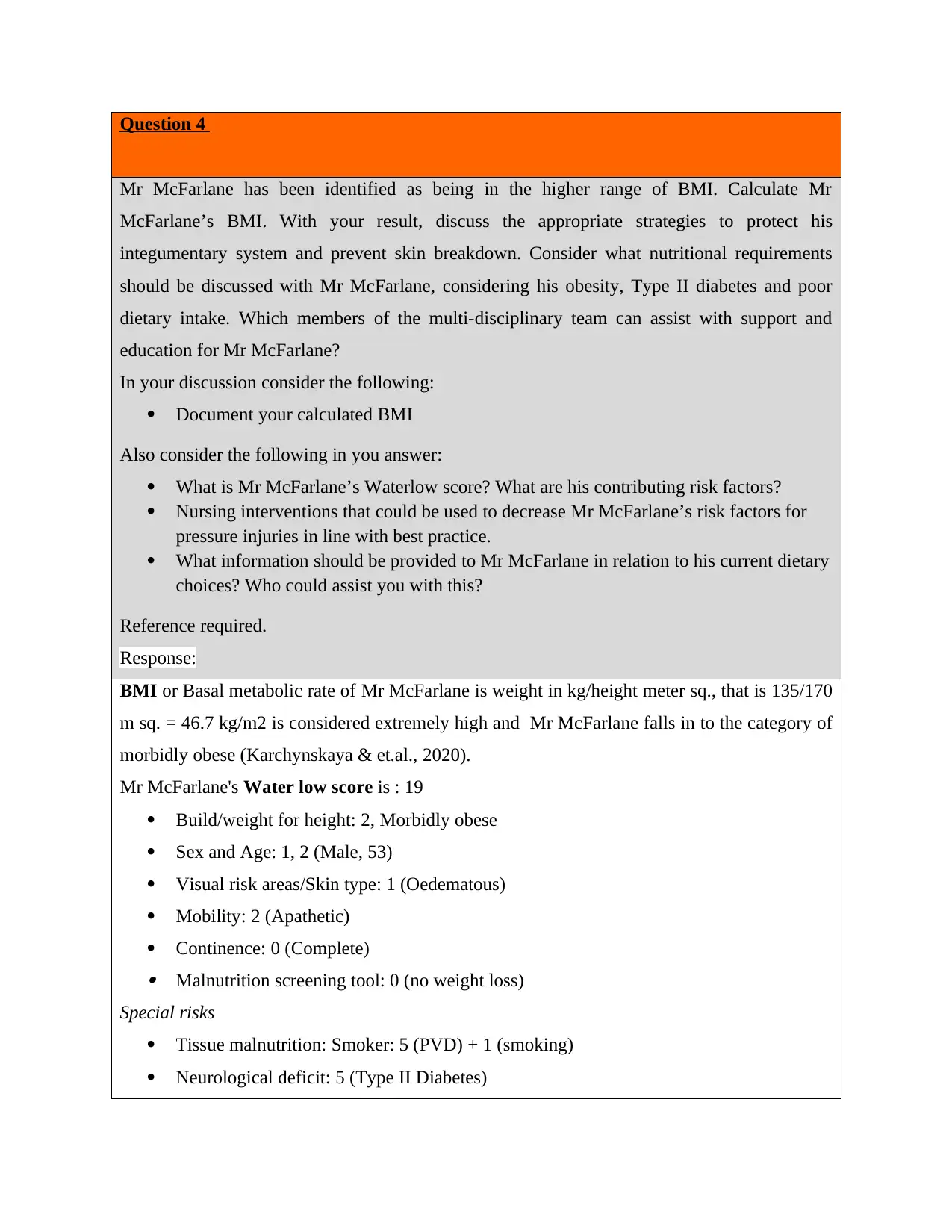
Question 4
Mr McFarlane has been identified as being in the higher range of BMI. Calculate Mr
McFarlane’s BMI. With your result, discuss the appropriate strategies to protect his
integumentary system and prevent skin breakdown. Consider what nutritional requirements
should be discussed with Mr McFarlane, considering his obesity, Type II diabetes and poor
dietary intake. Which members of the multi-disciplinary team can assist with support and
education for Mr McFarlane?
In your discussion consider the following:
Document your calculated BMI
Also consider the following in you answer:
What is Mr McFarlane’s Waterlow score? What are his contributing risk factors?
Nursing interventions that could be used to decrease Mr McFarlane’s risk factors for
pressure injuries in line with best practice.
What information should be provided to Mr McFarlane in relation to his current dietary
choices? Who could assist you with this?
Reference required.
Response:
BMI or Basal metabolic rate of Mr McFarlane is weight in kg/height meter sq., that is 135/170
m sq. = 46.7 kg/m2 is considered extremely high and Mr McFarlane falls in to the category of
morbidly obese (Karchynskaya & et.al., 2020).
Mr McFarlane's Water low score is : 19
Build/weight for height: 2, Morbidly obese
Sex and Age: 1, 2 (Male, 53)
Visual risk areas/Skin type: 1 (Oedematous)
Mobility: 2 (Apathetic)
Continence: 0 (Complete) Malnutrition screening tool: 0 (no weight loss)
Special risks
Tissue malnutrition: Smoker: 5 (PVD) + 1 (smoking)
Neurological deficit: 5 (Type II Diabetes)
Mr McFarlane has been identified as being in the higher range of BMI. Calculate Mr
McFarlane’s BMI. With your result, discuss the appropriate strategies to protect his
integumentary system and prevent skin breakdown. Consider what nutritional requirements
should be discussed with Mr McFarlane, considering his obesity, Type II diabetes and poor
dietary intake. Which members of the multi-disciplinary team can assist with support and
education for Mr McFarlane?
In your discussion consider the following:
Document your calculated BMI
Also consider the following in you answer:
What is Mr McFarlane’s Waterlow score? What are his contributing risk factors?
Nursing interventions that could be used to decrease Mr McFarlane’s risk factors for
pressure injuries in line with best practice.
What information should be provided to Mr McFarlane in relation to his current dietary
choices? Who could assist you with this?
Reference required.
Response:
BMI or Basal metabolic rate of Mr McFarlane is weight in kg/height meter sq., that is 135/170
m sq. = 46.7 kg/m2 is considered extremely high and Mr McFarlane falls in to the category of
morbidly obese (Karchynskaya & et.al., 2020).
Mr McFarlane's Water low score is : 19
Build/weight for height: 2, Morbidly obese
Sex and Age: 1, 2 (Male, 53)
Visual risk areas/Skin type: 1 (Oedematous)
Mobility: 2 (Apathetic)
Continence: 0 (Complete) Malnutrition screening tool: 0 (no weight loss)
Special risks
Tissue malnutrition: Smoker: 5 (PVD) + 1 (smoking)
Neurological deficit: 5 (Type II Diabetes)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Major surgery/trauma: 0
The major contributing risk factors include : PVD, Obesity, mobility issues, Smoking, Type II
diabetes (Wang & et.al., 2019).
The strategies that can be used for protecting the integumentary system of the patient and
prevent the skin breakdown are limiting the bath time, avoiding too hot showers or showers for
a very long time and avoiding strong soaps they remove the natural oils from the body.
Grooming has to be done carefully for shaving purposes. Skin creams that are antibacterial and
moisturisers have to be applied. Investigation and management of incontinence also involves
not being harsh on skin or rub anything vigorously and also using pH appropriate skin cleanser
(Davila, 2019).
Nutritional requirements for controlling the obesity and type II diabetes include consultation
with a dietician or advisor, taking a balanced diet, avoiding allergic foods, junk food,
consuming more complex carbohydrates, complete proteins, omega 3 and omega 6 fatty acids
and other healthy fats, eating plenty of green vegetables and fruits with low sucrose.
Other requirements include remaining adequately hydrated, decreasing the consumption of
caffeine, limiting drinking and quitting smoking. The multidisciplinary team that can assist for
the support provision to Mr McFarlane are practice nurses, general practitioner, dietician, and
allied health professionals.
Question 5
Mr McFarlane has pre-existing COPD and on examination you observe that his O2 saturations
on room air are 91%. Consider your nursing interventions, within your EN scope of practice.
How could you assist Mr McFarlane with ease of respiratory functioning whilst lying in bed
and sitting out in the chair?
In your discussion consider the following:
What are the ‘normal’ ranges for this measurement, comment on Mr McFarlane’s ranges
compare to his SpO2 on admission, and state what actions you need to take.
How would you demonstrate/ explain the importance of deep breathing exercises and
coughing exercises to the client.
Which MDT member could assist with active exercises to aid Mr McFarlane’s breathing?
The major contributing risk factors include : PVD, Obesity, mobility issues, Smoking, Type II
diabetes (Wang & et.al., 2019).
The strategies that can be used for protecting the integumentary system of the patient and
prevent the skin breakdown are limiting the bath time, avoiding too hot showers or showers for
a very long time and avoiding strong soaps they remove the natural oils from the body.
Grooming has to be done carefully for shaving purposes. Skin creams that are antibacterial and
moisturisers have to be applied. Investigation and management of incontinence also involves
not being harsh on skin or rub anything vigorously and also using pH appropriate skin cleanser
(Davila, 2019).
Nutritional requirements for controlling the obesity and type II diabetes include consultation
with a dietician or advisor, taking a balanced diet, avoiding allergic foods, junk food,
consuming more complex carbohydrates, complete proteins, omega 3 and omega 6 fatty acids
and other healthy fats, eating plenty of green vegetables and fruits with low sucrose.
Other requirements include remaining adequately hydrated, decreasing the consumption of
caffeine, limiting drinking and quitting smoking. The multidisciplinary team that can assist for
the support provision to Mr McFarlane are practice nurses, general practitioner, dietician, and
allied health professionals.
Question 5
Mr McFarlane has pre-existing COPD and on examination you observe that his O2 saturations
on room air are 91%. Consider your nursing interventions, within your EN scope of practice.
How could you assist Mr McFarlane with ease of respiratory functioning whilst lying in bed
and sitting out in the chair?
In your discussion consider the following:
What are the ‘normal’ ranges for this measurement, comment on Mr McFarlane’s ranges
compare to his SpO2 on admission, and state what actions you need to take.
How would you demonstrate/ explain the importance of deep breathing exercises and
coughing exercises to the client.
Which MDT member could assist with active exercises to aid Mr McFarlane’s breathing?
Response:
Oxygen Saturation are a measurement of amount of haemoglobin that carries oxygen in the
blood relative to the amount nor carrying it. The standard value is above 60mm Hg and any
value below it requires supplemental oxygen. The standard oximeter value ranges from 95-
100%. Values under 90% are considered low for functioning properly. spO2 levels of Mr
McFarlane on admission were 96% and post observation the percentage decreased to 91%
while examining again.
Nursing intervention for COPD include:
Oxygen therapy has to be initiated if the oxygen levels drop less than 88% as for
patients suffering from COPD, spO2 level range is 88-92%. Supplemental oxygen has
to provided in severe cases and carefully managing the equipment, preference to
portable tank and seeing if the airflow is not obstructed (SAH, 2020).
Raising the head of the bed for promoting effective breathing , descenting of diaphragm
and maximizing inhalation. Positioning will enhance airway patency.
Deep breathing and coughing techniques have to taught to help Mr McFarlane for
clearing airway through controlled coughing, huffing technique, inspiratory muscle
training, pursed lip breathing and diaphragmatic breathing etc.
Bronchodilators and corticosteroids have to administered appropriately.
Management of daily activities with support devices, effective exercise programs,
walking aids.
Monitoring and managing potential complications by periodical evaluation of cognitive
changes such as memory impairment personality or behavioural changes.
Pulse oximetry values have to monitored to assess the need for oxygen and manage
administration of supplemental oxygen.
Prevention of further infections by focussing on immunization of Mr McFarlane
against pneumonia and influenza as he is prone to respiratory diseases.
The MDT member that can assist with the nursing interventions are allied health
professional and practice nurses.
Oxygen Saturation are a measurement of amount of haemoglobin that carries oxygen in the
blood relative to the amount nor carrying it. The standard value is above 60mm Hg and any
value below it requires supplemental oxygen. The standard oximeter value ranges from 95-
100%. Values under 90% are considered low for functioning properly. spO2 levels of Mr
McFarlane on admission were 96% and post observation the percentage decreased to 91%
while examining again.
Nursing intervention for COPD include:
Oxygen therapy has to be initiated if the oxygen levels drop less than 88% as for
patients suffering from COPD, spO2 level range is 88-92%. Supplemental oxygen has
to provided in severe cases and carefully managing the equipment, preference to
portable tank and seeing if the airflow is not obstructed (SAH, 2020).
Raising the head of the bed for promoting effective breathing , descenting of diaphragm
and maximizing inhalation. Positioning will enhance airway patency.
Deep breathing and coughing techniques have to taught to help Mr McFarlane for
clearing airway through controlled coughing, huffing technique, inspiratory muscle
training, pursed lip breathing and diaphragmatic breathing etc.
Bronchodilators and corticosteroids have to administered appropriately.
Management of daily activities with support devices, effective exercise programs,
walking aids.
Monitoring and managing potential complications by periodical evaluation of cognitive
changes such as memory impairment personality or behavioural changes.
Pulse oximetry values have to monitored to assess the need for oxygen and manage
administration of supplemental oxygen.
Prevention of further infections by focussing on immunization of Mr McFarlane
against pneumonia and influenza as he is prone to respiratory diseases.
The MDT member that can assist with the nursing interventions are allied health
professional and practice nurses.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

