NUR251 Assignment: Comprehensive Nursing Care Plan for David Smith
VerifiedAdded on 2022/09/16
|14
|3395
|22
Homework Assignment
AI Summary
This assignment presents a comprehensive nursing care plan for David Smith, a patient experiencing acute kidney injury (AKI). Task 1 details initial assessments including physical and vital signs, pain assessment using the PQRST algorithm, and fluid balance assessment. Task 2 outlines a detailed nursing care plan addressing acute pain, risk of fluid imbalance, risk of infection, anxiety, and impaired skin integrity, including goals, nursing interventions, rationale, and evaluations for each problem. Task 3 provides recommendations for discharge planning, emphasizing patient education on fluid balance, pain management, and the importance of reporting symptoms. Task 4 discusses the clinical reasoning cycle used in providing interventions, starting with initial assessments and culminating in the implementation of the care plan.
Nursing Assignment
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 1:
In the first instance, physical and vital signs assessment will be performed for David.
Physical assessment will be performed in the form objective findings through
observation, palpation, percussion and auscultation. Physical assessment and vital
signs assessment will be beneficial for identifying signs and symptoms of current
medical condition of David. Moreover, it will also be beneficial in integrating David’s
medical history and pathophysiology (Gabayan et al., 2017; Mok, Wang, and Liaw,
2015). Observed vital signs in case of David are outside normal range. If
assessment of vital signs of David would not have been done; it would be difficult to
gather information about normalisation of these vital signs. Consequently, it would be
difficult to plan specific intervention with respect to abnormal value of vital signs
(Mok, Wang, and Liaw, 2015). Data obtained from the physical and vital signs
assessment will be maintained in the observation chart, progress notes and
medication chart.
In the second instance, assessment of acute pain related to acute kidney injury (AKI)
will be performed in David. Acute pain in David will be assessed through
implementing PQRST algorithm. Accurate pain assessment in David in essential
because acute urinary bladder pain is the prominent symptom of AKI. Moreover,
most of the elder patients are hesitant to verbalise the pain. Hence, it is highly
possible that such pain might remain untreated. It is essential to assess pain and
provide relevant intervention because untreated persistent pain can lead to multiple
physical and psychological manifestations (Coluzzi, 2018). Information related to
pain assessment will be maintained in the records such observation chart, progress
notes and medication chart.
In the third instance, fluid balance assessment will be performed in David.
Assessment of fluid balance will be performed through monitoring fluid volume,
complications, cardiac rhythm and neurological manifestation (Chuang, 2016). Fluid
balance assessment is essential in case of David because he is associated with
kidney disease. Kidney diseases are mainly responsible for disturbed fluid balance. If
fluid balance assessment not performed in David, there is possibility of accumulation
of salt and water which lead to organ damage and exaggeration of the AKI (Chuang,
2016; Prowle, Kirwan, and Bellomo, 2014). Data and values obtained through fluid
balance will be maintained in the fluid balance chart, daily weight chart, stool chart,
fluid prescription chart and medication chart.
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
In the first instance, physical and vital signs assessment will be performed for David.
Physical assessment will be performed in the form objective findings through
observation, palpation, percussion and auscultation. Physical assessment and vital
signs assessment will be beneficial for identifying signs and symptoms of current
medical condition of David. Moreover, it will also be beneficial in integrating David’s
medical history and pathophysiology (Gabayan et al., 2017; Mok, Wang, and Liaw,
2015). Observed vital signs in case of David are outside normal range. If
assessment of vital signs of David would not have been done; it would be difficult to
gather information about normalisation of these vital signs. Consequently, it would be
difficult to plan specific intervention with respect to abnormal value of vital signs
(Mok, Wang, and Liaw, 2015). Data obtained from the physical and vital signs
assessment will be maintained in the observation chart, progress notes and
medication chart.
In the second instance, assessment of acute pain related to acute kidney injury (AKI)
will be performed in David. Acute pain in David will be assessed through
implementing PQRST algorithm. Accurate pain assessment in David in essential
because acute urinary bladder pain is the prominent symptom of AKI. Moreover,
most of the elder patients are hesitant to verbalise the pain. Hence, it is highly
possible that such pain might remain untreated. It is essential to assess pain and
provide relevant intervention because untreated persistent pain can lead to multiple
physical and psychological manifestations (Coluzzi, 2018). Information related to
pain assessment will be maintained in the records such observation chart, progress
notes and medication chart.
In the third instance, fluid balance assessment will be performed in David.
Assessment of fluid balance will be performed through monitoring fluid volume,
complications, cardiac rhythm and neurological manifestation (Chuang, 2016). Fluid
balance assessment is essential in case of David because he is associated with
kidney disease. Kidney diseases are mainly responsible for disturbed fluid balance. If
fluid balance assessment not performed in David, there is possibility of accumulation
of salt and water which lead to organ damage and exaggeration of the AKI (Chuang,
2016; Prowle, Kirwan, and Bellomo, 2014). Data and values obtained through fluid
balance will be maintained in the fluid balance chart, daily weight chart, stool chart,
fluid prescription chart and medication chart.
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1

3
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
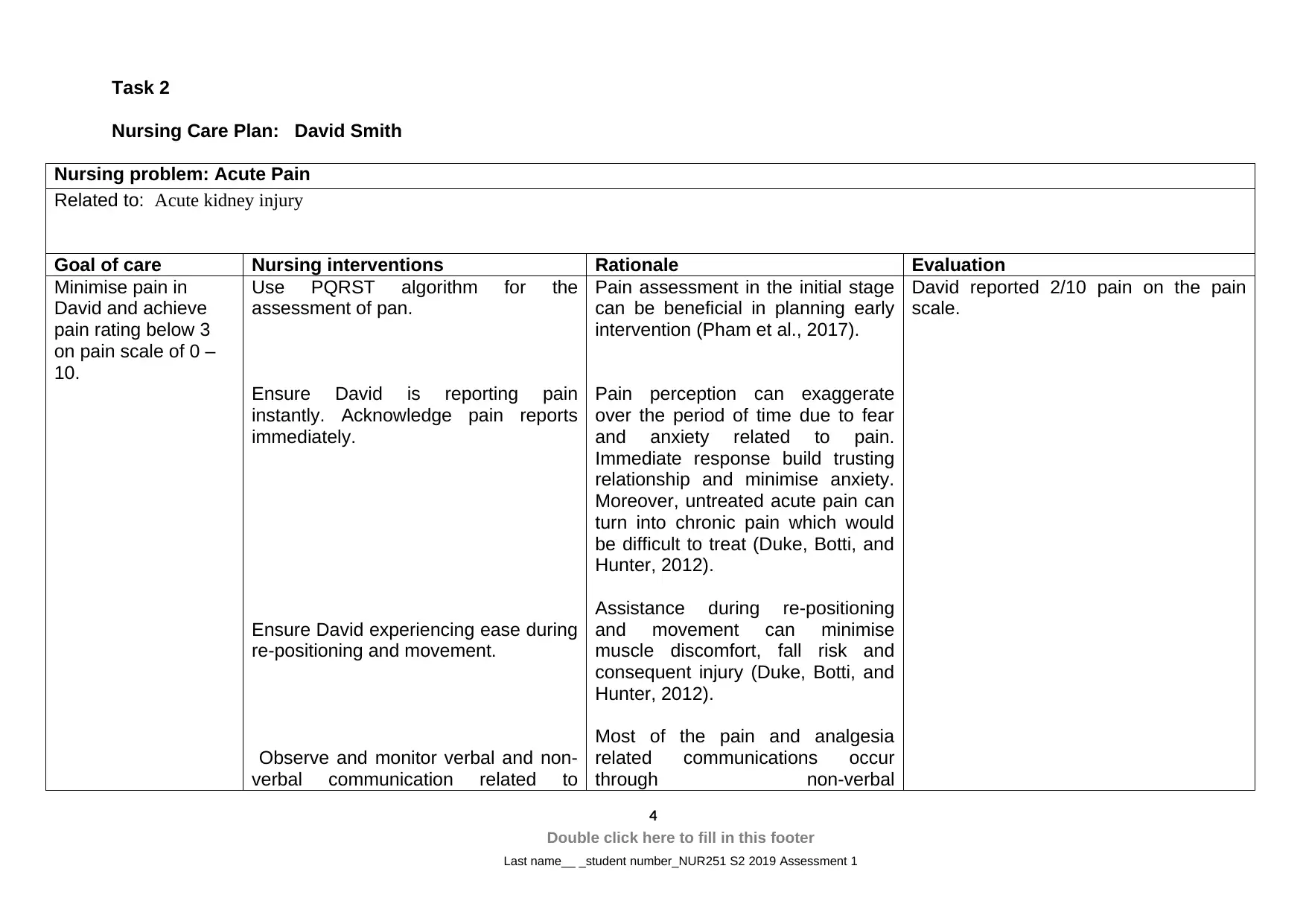
Task 2
Nursing Care Plan: David Smith
Nursing problem: Acute Pain
Related to: Acute kidney injury
Goal of care Nursing interventions Rationale Evaluation
Minimise pain in
David and achieve
pain rating below 3
on pain scale of 0 –
10.
Use PQRST algorithm for the
assessment of pan.
Ensure David is reporting pain
instantly. Acknowledge pain reports
immediately.
Ensure David experiencing ease during
re-positioning and movement.
Observe and monitor verbal and non-
verbal communication related to
Pain assessment in the initial stage
can be beneficial in planning early
intervention (Pham et al., 2017).
Pain perception can exaggerate
over the period of time due to fear
and anxiety related to pain.
Immediate response build trusting
relationship and minimise anxiety.
Moreover, untreated acute pain can
turn into chronic pain which would
be difficult to treat (Duke, Botti, and
Hunter, 2012).
Assistance during re-positioning
and movement can minimise
muscle discomfort, fall risk and
consequent injury (Duke, Botti, and
Hunter, 2012).
Most of the pain and analgesia
related communications occur
through non-verbal
David reported 2/10 pain on the pain
scale.
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Nursing Care Plan: David Smith
Nursing problem: Acute Pain
Related to: Acute kidney injury
Goal of care Nursing interventions Rationale Evaluation
Minimise pain in
David and achieve
pain rating below 3
on pain scale of 0 –
10.
Use PQRST algorithm for the
assessment of pan.
Ensure David is reporting pain
instantly. Acknowledge pain reports
immediately.
Ensure David experiencing ease during
re-positioning and movement.
Observe and monitor verbal and non-
verbal communication related to
Pain assessment in the initial stage
can be beneficial in planning early
intervention (Pham et al., 2017).
Pain perception can exaggerate
over the period of time due to fear
and anxiety related to pain.
Immediate response build trusting
relationship and minimise anxiety.
Moreover, untreated acute pain can
turn into chronic pain which would
be difficult to treat (Duke, Botti, and
Hunter, 2012).
Assistance during re-positioning
and movement can minimise
muscle discomfort, fall risk and
consequent injury (Duke, Botti, and
Hunter, 2012).
Most of the pain and analgesia
related communications occur
through non-verbal
David reported 2/10 pain on the pain
scale.
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
analgesia requirement, guarding and
moaning.
Advice David to consume pain
medication on regular basis. Administer
pain medication to David based on the
observed of pain rating on the pain
scale. Moreover, assess and monitor
therapeutic benefit and side effect of
analgesia.
communications. Hence, analgesia
can be given immediately (Pham et
al., 2017).
Regular observation and monitoring
of analgesia consumption can
improve therapeutic usefulness.
Moreover, it is can improve belief of
patient on medication (Pham et al.,
2017).
David reported pain relief after
consumption of pain medication and no
adverse effects analgesic medicines.
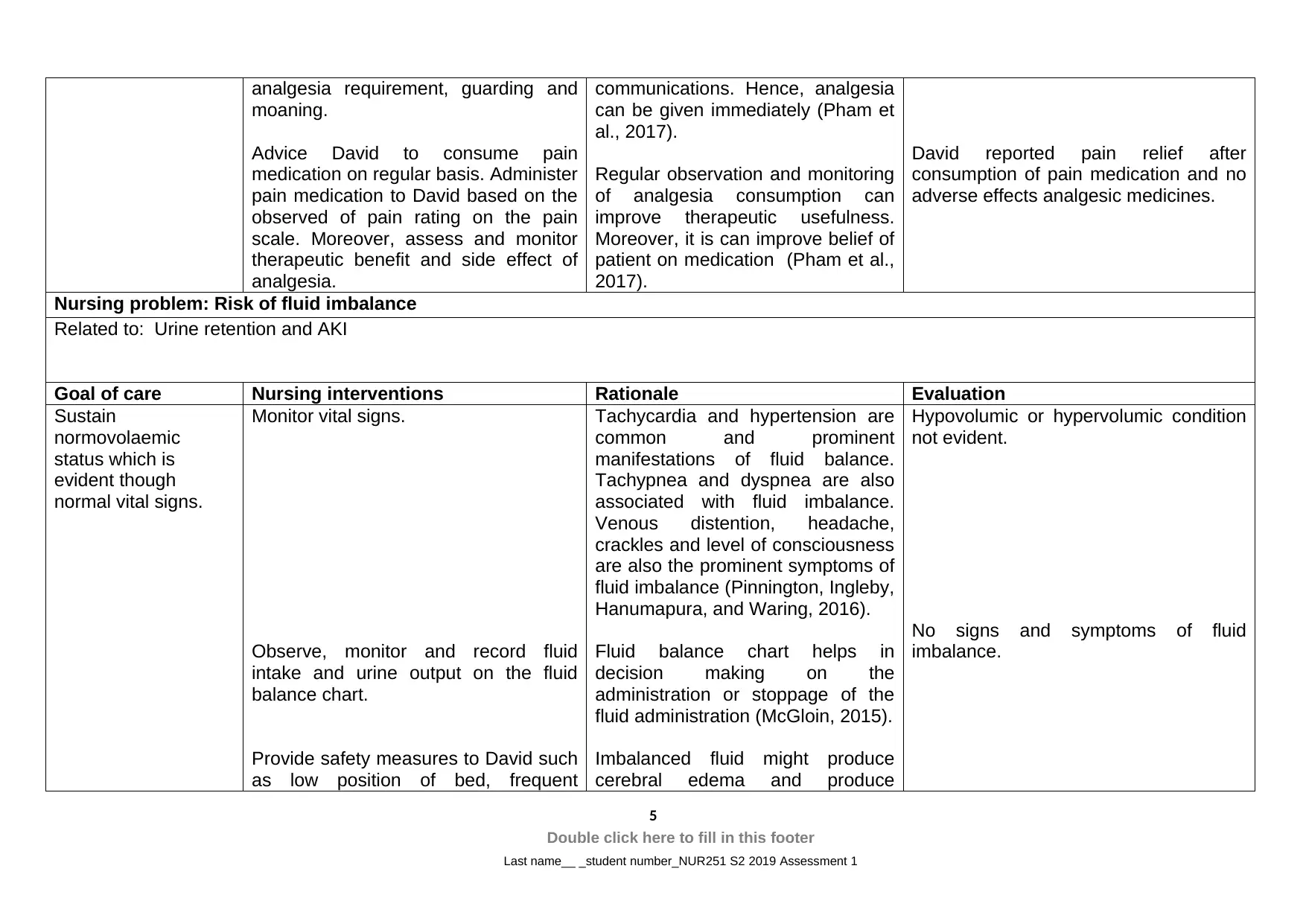
Nursing problem: Risk of fluid imbalance
Related to: Urine retention and AKI
Goal of care Nursing interventions Rationale Evaluation
Sustain
normovolaemic
status which is
evident though
normal vital signs.
Monitor vital signs.
Observe, monitor and record fluid
intake and urine output on the fluid
balance chart.
Provide safety measures to David such
as low position of bed, frequent
Tachycardia and hypertension are
common and prominent
manifestations of fluid balance.
Tachypnea and dyspnea are also
associated with fluid imbalance.
Venous distention, headache,
crackles and level of consciousness
are also the prominent symptoms of
fluid imbalance (Pinnington, Ingleby,
Hanumapura, and Waring, 2016).
Fluid balance chart helps in
decision making on the
administration or stoppage of the
fluid administration (McGloin, 2015).
Imbalanced fluid might produce
cerebral edema and produce
Hypovolumic or hypervolumic condition
not evident.
No signs and symptoms of fluid
imbalance.
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
moaning.
Advice David to consume pain
medication on regular basis. Administer
pain medication to David based on the
observed of pain rating on the pain
scale. Moreover, assess and monitor
therapeutic benefit and side effect of
analgesia.
communications. Hence, analgesia
can be given immediately (Pham et
al., 2017).
Regular observation and monitoring
of analgesia consumption can
improve therapeutic usefulness.
Moreover, it is can improve belief of
patient on medication (Pham et al.,
2017).
David reported pain relief after
consumption of pain medication and no
adverse effects analgesic medicines.
Nursing problem: Risk of fluid imbalance
Related to: Urine retention and AKI
Goal of care Nursing interventions Rationale Evaluation
Sustain
normovolaemic
status which is
evident though
normal vital signs.
Monitor vital signs.
Observe, monitor and record fluid
intake and urine output on the fluid
balance chart.
Provide safety measures to David such
as low position of bed, frequent
Tachycardia and hypertension are
common and prominent
manifestations of fluid balance.
Tachypnea and dyspnea are also
associated with fluid imbalance.
Venous distention, headache,
crackles and level of consciousness
are also the prominent symptoms of
fluid imbalance (Pinnington, Ingleby,
Hanumapura, and Waring, 2016).
Fluid balance chart helps in
decision making on the
administration or stoppage of the
fluid administration (McGloin, 2015).
Imbalanced fluid might produce
cerebral edema and produce
Hypovolumic or hypervolumic condition
not evident.
No signs and symptoms of fluid
imbalance.
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
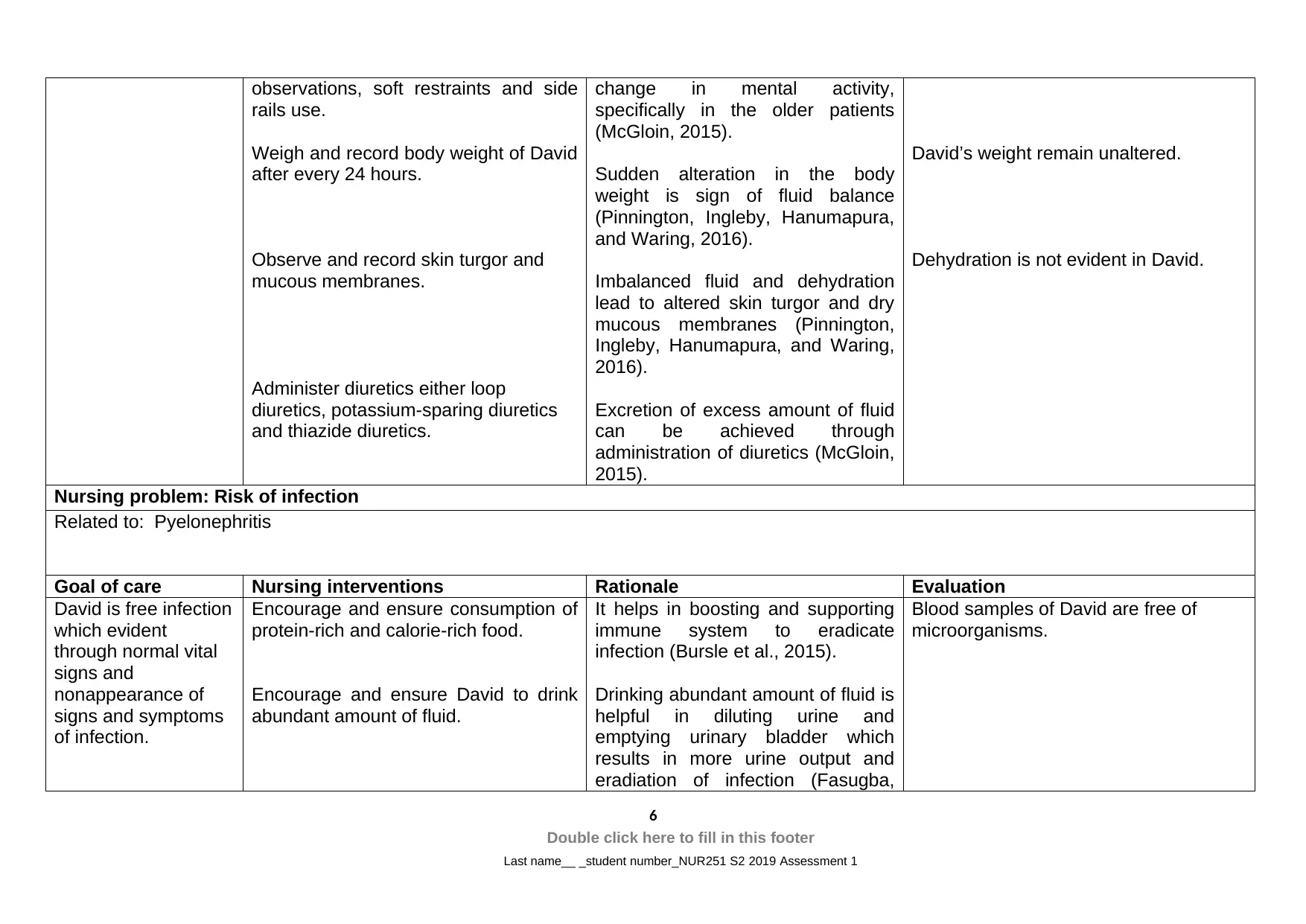
observations, soft restraints and side
rails use.
Weigh and record body weight of David
after every 24 hours.
Observe and record skin turgor and
mucous membranes.
Administer diuretics either loop
diuretics, potassium-sparing diuretics
and thiazide diuretics.
change in mental activity,
specifically in the older patients
(McGloin, 2015).
Sudden alteration in the body
weight is sign of fluid balance
(Pinnington, Ingleby, Hanumapura,
and Waring, 2016).
Imbalanced fluid and dehydration
lead to altered skin turgor and dry
mucous membranes (Pinnington,
Ingleby, Hanumapura, and Waring,
2016).
Excretion of excess amount of fluid
can be achieved through
administration of diuretics (McGloin,
2015).
David’s weight remain unaltered.
Dehydration is not evident in David.
Nursing problem: Risk of infection
Related to: Pyelonephritis
Goal of care Nursing interventions Rationale Evaluation
David is free infection
which evident
through normal vital
signs and
nonappearance of
signs and symptoms
of infection.
Encourage and ensure consumption of
protein-rich and calorie-rich food.
Encourage and ensure David to drink
abundant amount of fluid.
It helps in boosting and supporting
immune system to eradicate
infection (Bursle et al., 2015).
Drinking abundant amount of fluid is
helpful in diluting urine and
emptying urinary bladder which
results in more urine output and
eradiation of infection (Fasugba,
Blood samples of David are free of
microorganisms.
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
rails use.
Weigh and record body weight of David
after every 24 hours.
Observe and record skin turgor and
mucous membranes.
Administer diuretics either loop
diuretics, potassium-sparing diuretics
and thiazide diuretics.
change in mental activity,
specifically in the older patients
(McGloin, 2015).
Sudden alteration in the body
weight is sign of fluid balance
(Pinnington, Ingleby, Hanumapura,
and Waring, 2016).
Imbalanced fluid and dehydration
lead to altered skin turgor and dry
mucous membranes (Pinnington,
Ingleby, Hanumapura, and Waring,
2016).
Excretion of excess amount of fluid
can be achieved through
administration of diuretics (McGloin,
2015).
David’s weight remain unaltered.
Dehydration is not evident in David.
Nursing problem: Risk of infection
Related to: Pyelonephritis
Goal of care Nursing interventions Rationale Evaluation
David is free infection
which evident
through normal vital
signs and
nonappearance of
signs and symptoms
of infection.
Encourage and ensure consumption of
protein-rich and calorie-rich food.
Encourage and ensure David to drink
abundant amount of fluid.
It helps in boosting and supporting
immune system to eradicate
infection (Bursle et al., 2015).
Drinking abundant amount of fluid is
helpful in diluting urine and
emptying urinary bladder which
results in more urine output and
eradiation of infection (Fasugba,
Blood samples of David are free of
microorganisms.
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
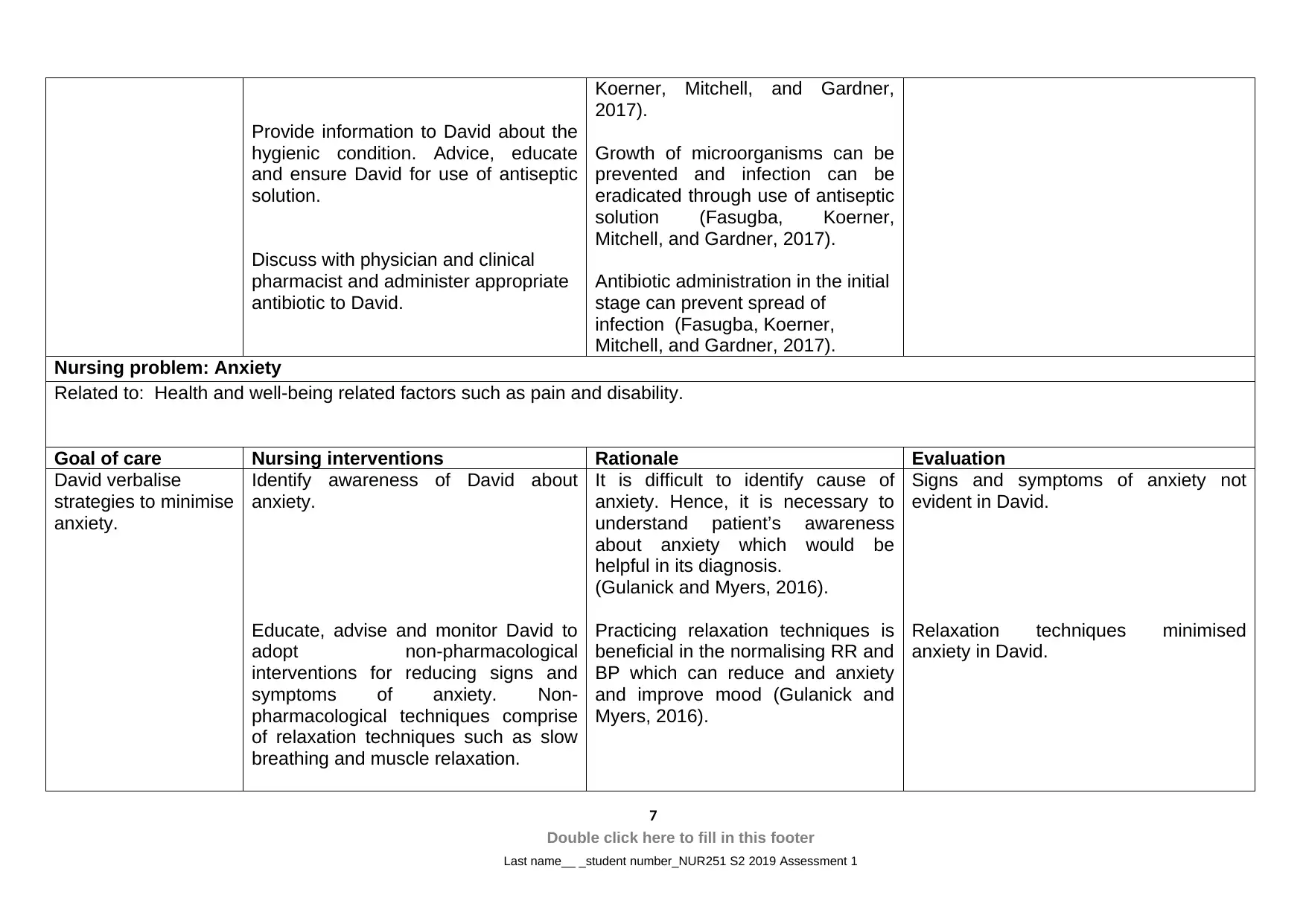
Provide information to David about the
hygienic condition. Advice, educate
and ensure David for use of antiseptic
solution.
Discuss with physician and clinical
pharmacist and administer appropriate
antibiotic to David.
Koerner, Mitchell, and Gardner,
2017).
Growth of microorganisms can be
prevented and infection can be
eradicated through use of antiseptic
solution (Fasugba, Koerner,
Mitchell, and Gardner, 2017).
Antibiotic administration in the initial
stage can prevent spread of
infection (Fasugba, Koerner,
Mitchell, and Gardner, 2017).
Nursing problem: Anxiety
Related to: Health and well-being related factors such as pain and disability.
Goal of care Nursing interventions Rationale Evaluation
David verbalise
strategies to minimise
anxiety.
Identify awareness of David about
anxiety.
Educate, advise and monitor David to
adopt non-pharmacological
interventions for reducing signs and
symptoms of anxiety. Non-
pharmacological techniques comprise
of relaxation techniques such as slow
breathing and muscle relaxation.
It is difficult to identify cause of
anxiety. Hence, it is necessary to
understand patient’s awareness
about anxiety which would be
helpful in its diagnosis.
(Gulanick and Myers, 2016).
Practicing relaxation techniques is
beneficial in the normalising RR and
BP which can reduce and anxiety
and improve mood (Gulanick and
Myers, 2016).
Signs and symptoms of anxiety not
evident in David.
Relaxation techniques minimised
anxiety in David.
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
hygienic condition. Advice, educate
and ensure David for use of antiseptic
solution.
Discuss with physician and clinical
pharmacist and administer appropriate
antibiotic to David.
Koerner, Mitchell, and Gardner,
2017).
Growth of microorganisms can be
prevented and infection can be
eradicated through use of antiseptic
solution (Fasugba, Koerner,
Mitchell, and Gardner, 2017).
Antibiotic administration in the initial
stage can prevent spread of
infection (Fasugba, Koerner,
Mitchell, and Gardner, 2017).
Nursing problem: Anxiety
Related to: Health and well-being related factors such as pain and disability.
Goal of care Nursing interventions Rationale Evaluation
David verbalise
strategies to minimise
anxiety.
Identify awareness of David about
anxiety.
Educate, advise and monitor David to
adopt non-pharmacological
interventions for reducing signs and
symptoms of anxiety. Non-
pharmacological techniques comprise
of relaxation techniques such as slow
breathing and muscle relaxation.
It is difficult to identify cause of
anxiety. Hence, it is necessary to
understand patient’s awareness
about anxiety which would be
helpful in its diagnosis.
(Gulanick and Myers, 2016).
Practicing relaxation techniques is
beneficial in the normalising RR and
BP which can reduce and anxiety
and improve mood (Gulanick and
Myers, 2016).
Signs and symptoms of anxiety not
evident in David.
Relaxation techniques minimised
anxiety in David.
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
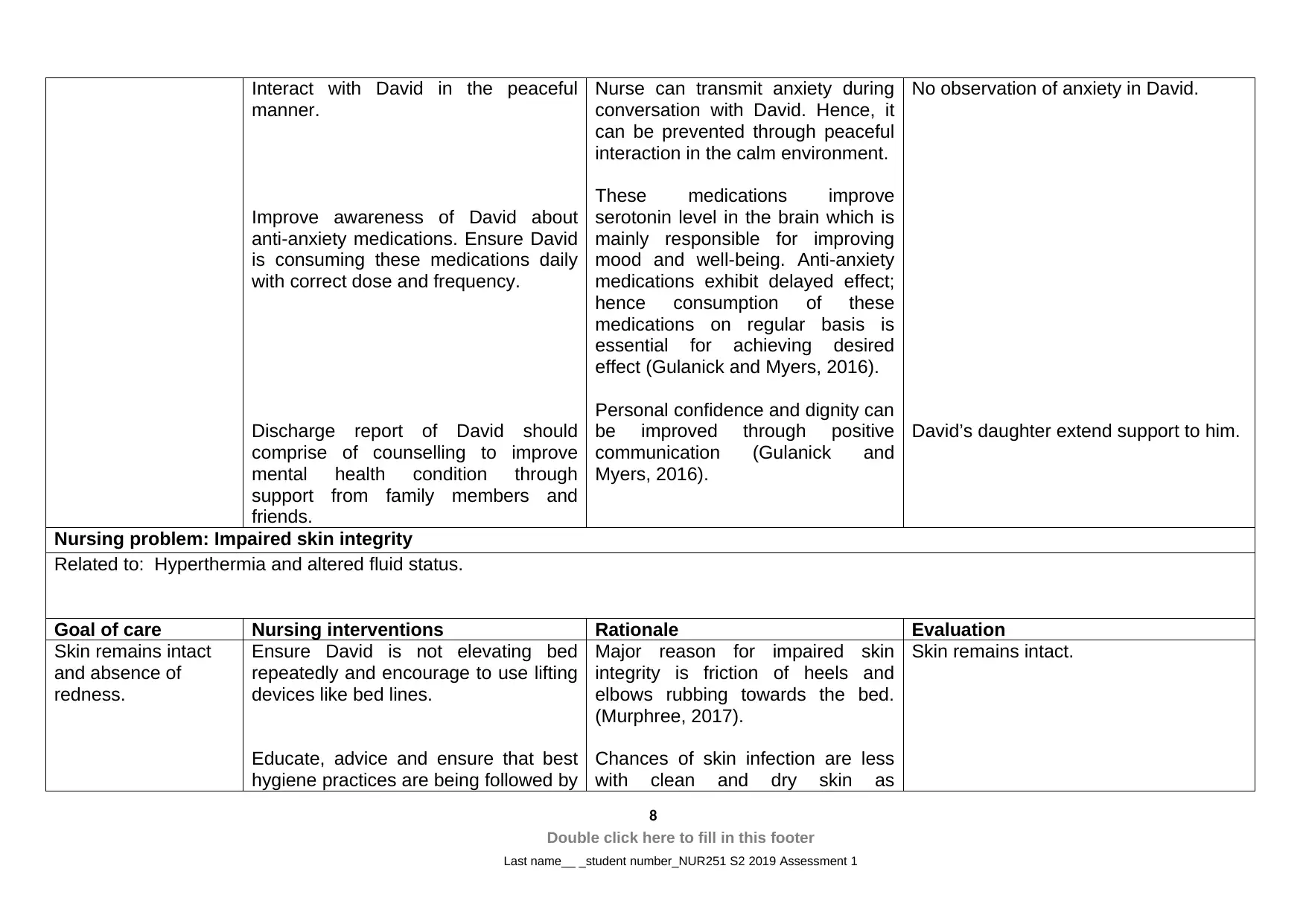
Interact with David in the peaceful
manner.
Improve awareness of David about
anti-anxiety medications. Ensure David
is consuming these medications daily
with correct dose and frequency.
Discharge report of David should
comprise of counselling to improve
mental health condition through
support from family members and
friends.
Nurse can transmit anxiety during
conversation with David. Hence, it
can be prevented through peaceful
interaction in the calm environment.
These medications improve
serotonin level in the brain which is
mainly responsible for improving
mood and well-being. Anti-anxiety
medications exhibit delayed effect;
hence consumption of these
medications on regular basis is
essential for achieving desired
effect (Gulanick and Myers, 2016).
Personal confidence and dignity can
be improved through positive
communication (Gulanick and
Myers, 2016).
No observation of anxiety in David.
David’s daughter extend support to him.
Nursing problem: Impaired skin integrity
Related to: Hyperthermia and altered fluid status.
Goal of care Nursing interventions Rationale Evaluation
Skin remains intact
and absence of
redness.
Ensure David is not elevating bed
repeatedly and encourage to use lifting
devices like bed lines.
Educate, advice and ensure that best
hygiene practices are being followed by
Major reason for impaired skin
integrity is friction of heels and
elbows rubbing towards the bed.
(Murphree, 2017).
Chances of skin infection are less
with clean and dry skin as
Skin remains intact.
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
manner.
Improve awareness of David about
anti-anxiety medications. Ensure David
is consuming these medications daily
with correct dose and frequency.
Discharge report of David should
comprise of counselling to improve
mental health condition through
support from family members and
friends.
Nurse can transmit anxiety during
conversation with David. Hence, it
can be prevented through peaceful
interaction in the calm environment.
These medications improve
serotonin level in the brain which is
mainly responsible for improving
mood and well-being. Anti-anxiety
medications exhibit delayed effect;
hence consumption of these
medications on regular basis is
essential for achieving desired
effect (Gulanick and Myers, 2016).
Personal confidence and dignity can
be improved through positive
communication (Gulanick and
Myers, 2016).
No observation of anxiety in David.
David’s daughter extend support to him.
Nursing problem: Impaired skin integrity
Related to: Hyperthermia and altered fluid status.
Goal of care Nursing interventions Rationale Evaluation
Skin remains intact
and absence of
redness.
Ensure David is not elevating bed
repeatedly and encourage to use lifting
devices like bed lines.
Educate, advice and ensure that best
hygiene practices are being followed by
Major reason for impaired skin
integrity is friction of heels and
elbows rubbing towards the bed.
(Murphree, 2017).
Chances of skin infection are less
with clean and dry skin as
Skin remains intact.
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
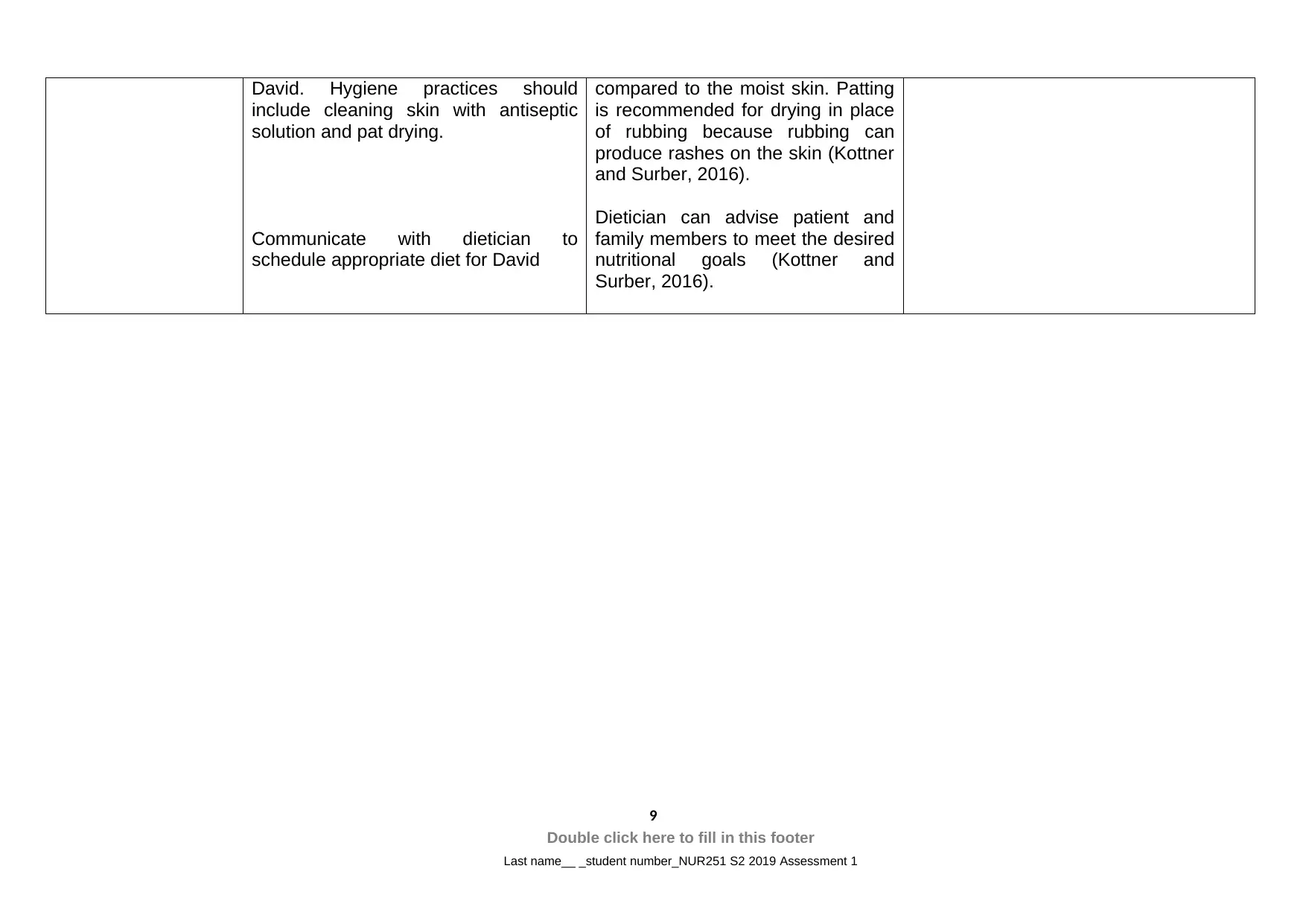
David. Hygiene practices should
include cleaning skin with antiseptic
solution and pat drying.
Communicate with dietician to
schedule appropriate diet for David
compared to the moist skin. Patting
is recommended for drying in place
of rubbing because rubbing can
produce rashes on the skin (Kottner
and Surber, 2016).
Dietician can advise patient and
family members to meet the desired
nutritional goals (Kottner and
Surber, 2016).
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
include cleaning skin with antiseptic
solution and pat drying.
Communicate with dietician to
schedule appropriate diet for David
compared to the moist skin. Patting
is recommended for drying in place
of rubbing because rubbing can
produce rashes on the skin (Kottner
and Surber, 2016).
Dietician can advise patient and
family members to meet the desired
nutritional goals (Kottner and
Surber, 2016).
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Task 3
Recommendations like observation of fluid balance and acute pain should be
incorporated in discharge planning of David. These two recommendations are
essential in David’s case because routine monitoring of these aspects can improve
his condition.
David should be educated about the signs and symptoms of the fluid imbalance.
Advice David to inform nurse about the sings and symptoms of imbalanced fluid such
as fatigue, lethargy, muscle weakness, muscle cramping and confusion. David
should be encouraged to consume abundant amount of water or fluid (2000 to 3000
ml per day). In case, these is no improvement in symptoms of fluid imbalance after
consumption of adequate fluid; David should be instructed to inform the nurse.
Hence, nurse, dietician and physician can change the course of action to IV fluid or
other intervention (Xue, Li, Liu, and Sun, 2016; Lemone et al., 2017). David should
be advised to keep record of daily body weight because abrupt body weight change
is the significant indication of the fluid imbalance.
Nurse should increase awareness of David about the pain related to AKI. His painful
condition is mainly due to the AKI and he is not associated with any other pain
related disease. Urinary distension and raised pressure in the urinary tract are mainly
responsible for his pain. He should not be worried about his lower back pain, if any,
because chances of urinary bladder pain radiating to the lower back are high
(Bellomo, Vaara, and Kellum, 2017). Hence, he should be focused on reducing pain
related to urinary tract. Education should be provided to David to identify various
parameters of pain such as time, quality, intensity and location of pain and inform
these parameters to nurse. Hence, nurse can plan necessary intervention based on
the duration and intensity of pain. It is advisable to educate David about the use of
various accessories such as warm baths or heating pads which can be helpful in
minimising pain intensity. Nurse should advise him and ensure that he is consuming
adequate amount of fluid on daily basis. He should be informed that consumption of
adequate amount of fluid would dilute urine and minimise bladder irritation. Hence,
pain can be managed effectively (Meersch, Volmering, and Zarbock, 2017; Bryant,
Knights, Darroch, and Rowland, 2018).
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Recommendations like observation of fluid balance and acute pain should be
incorporated in discharge planning of David. These two recommendations are
essential in David’s case because routine monitoring of these aspects can improve
his condition.
David should be educated about the signs and symptoms of the fluid imbalance.
Advice David to inform nurse about the sings and symptoms of imbalanced fluid such
as fatigue, lethargy, muscle weakness, muscle cramping and confusion. David
should be encouraged to consume abundant amount of water or fluid (2000 to 3000
ml per day). In case, these is no improvement in symptoms of fluid imbalance after
consumption of adequate fluid; David should be instructed to inform the nurse.
Hence, nurse, dietician and physician can change the course of action to IV fluid or
other intervention (Xue, Li, Liu, and Sun, 2016; Lemone et al., 2017). David should
be advised to keep record of daily body weight because abrupt body weight change
is the significant indication of the fluid imbalance.
Nurse should increase awareness of David about the pain related to AKI. His painful
condition is mainly due to the AKI and he is not associated with any other pain
related disease. Urinary distension and raised pressure in the urinary tract are mainly
responsible for his pain. He should not be worried about his lower back pain, if any,
because chances of urinary bladder pain radiating to the lower back are high
(Bellomo, Vaara, and Kellum, 2017). Hence, he should be focused on reducing pain
related to urinary tract. Education should be provided to David to identify various
parameters of pain such as time, quality, intensity and location of pain and inform
these parameters to nurse. Hence, nurse can plan necessary intervention based on
the duration and intensity of pain. It is advisable to educate David about the use of
various accessories such as warm baths or heating pads which can be helpful in
minimising pain intensity. Nurse should advise him and ensure that he is consuming
adequate amount of fluid on daily basis. He should be informed that consumption of
adequate amount of fluid would dilute urine and minimise bladder irritation. Hence,
pain can be managed effectively (Meersch, Volmering, and Zarbock, 2017; Bryant,
Knights, Darroch, and Rowland, 2018).
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 4
Clinical reasoning cycle was followed for providing intervention to David. Physical
and vital signs assessment were performed in the initial hours of admission. Physical
assessment indicated he feels tired, disability and pain. His vital signs assessment
indicated that his vital signs were beyond the normal range. His recorded values of
vital signs were BP (160/95 mmHg), RR (22) and HR (96 bpm). Since, his vital sings
are not within normal range; he is associated with psychological issues such as no
alertness to time and place, anxiety and worrisome behaviour. Hence, his
appearance is restless and unwell. It might be due his physical, physiological and
psychological health issues. His urine output is less, as his recorded urine output in
the last four hours is 100 ml. However, urine quality is abnormal because it is dark
coloured with offensive smell. It indicates he is associated with renal infection. He
opened his bowel in the morning. He is consuming diabetic food comfortably without
any complain. He displayed no hesitation in mobility for the completion of his ADL’s.
There is no evidence of dehydration and turgor on his skin which indicate his skin is
intact.
Based on the observations and assessment specific medications were administered
to him and effect of these medications were assessed. His pain intensity was
reduced to 2/10 after the administration of medications like paracetamol 1 g QID and
morphine 2.5 mg. However, his BP remain at the above normal level even after the
administration of Ramipril 10 mg OD. Moreover, his temperature also remains
elevated even after administration of paracetamol 1 g QID. Increased WBC count
(1.5 X 109/L) indicates infection. Hence, antibiotic is recommended to be ordered for
him. Education provided to him about pain management, fluid balance and infection
identification and management. Doctor recommended discharge and ordered revisit
after three weeks for F/U. Paperwork of D/C completed.
11
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Clinical reasoning cycle was followed for providing intervention to David. Physical
and vital signs assessment were performed in the initial hours of admission. Physical
assessment indicated he feels tired, disability and pain. His vital signs assessment
indicated that his vital signs were beyond the normal range. His recorded values of
vital signs were BP (160/95 mmHg), RR (22) and HR (96 bpm). Since, his vital sings
are not within normal range; he is associated with psychological issues such as no
alertness to time and place, anxiety and worrisome behaviour. Hence, his
appearance is restless and unwell. It might be due his physical, physiological and
psychological health issues. His urine output is less, as his recorded urine output in
the last four hours is 100 ml. However, urine quality is abnormal because it is dark
coloured with offensive smell. It indicates he is associated with renal infection. He
opened his bowel in the morning. He is consuming diabetic food comfortably without
any complain. He displayed no hesitation in mobility for the completion of his ADL’s.
There is no evidence of dehydration and turgor on his skin which indicate his skin is
intact.
Based on the observations and assessment specific medications were administered
to him and effect of these medications were assessed. His pain intensity was
reduced to 2/10 after the administration of medications like paracetamol 1 g QID and
morphine 2.5 mg. However, his BP remain at the above normal level even after the
administration of Ramipril 10 mg OD. Moreover, his temperature also remains
elevated even after administration of paracetamol 1 g QID. Increased WBC count
(1.5 X 109/L) indicates infection. Hence, antibiotic is recommended to be ordered for
him. Education provided to him about pain management, fluid balance and infection
identification and management. Doctor recommended discharge and ordered revisit
after three weeks for F/U. Paperwork of D/C completed.
11
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
Key (if required)
AKI – Acute kidney injury
BP – Blood pressure
RR – Respiratory rate
HR – Heart rate
D/C discharge
F/U follow-up
ADL’s activities of daily living
PQRST provocation/palliation, quality/quantity, region/radiation, severity
scale, timing
12
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
AKI – Acute kidney injury
BP – Blood pressure
RR – Respiratory rate
HR – Heart rate
D/C discharge
F/U follow-up
ADL’s activities of daily living
PQRST provocation/palliation, quality/quantity, region/radiation, severity
scale, timing
12
Double click here to fill in this footer
Last name__ _student number_NUR251 S2 2019 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





