Detailed Nursing Care Plan: Acute on Chronic Renal Failure Patient
VerifiedAdded on 2022/10/15
|22
|5457
|466
Report
AI Summary
This assignment is a comprehensive nursing care plan for a 72-year-old male patient admitted with acute kidney injury secondary to pyelonephritis, superimposed on chronic kidney disease. The report details the patient's medical history, current condition, and prescribed medical orders. The student nurse is tasked with conducting priority nursing assessments (vital signs, pain, and nutritional status), developing a care plan addressing physical, functional, and psychosocial aspects of care, providing patient education for discharge, and creating a progress note entry. The care plan includes five nursing problems with related factors, goals, interventions, rationales, and evaluation criteria. Patient education focuses on discharge preparation. The assignment emphasizes adherence to professional documentation standards, including the use of appropriate language and referencing. The student nurse is expected to use evidence-based practice to develop and implement this care plan, demonstrating a thorough understanding of renal failure management and patient-centered care.
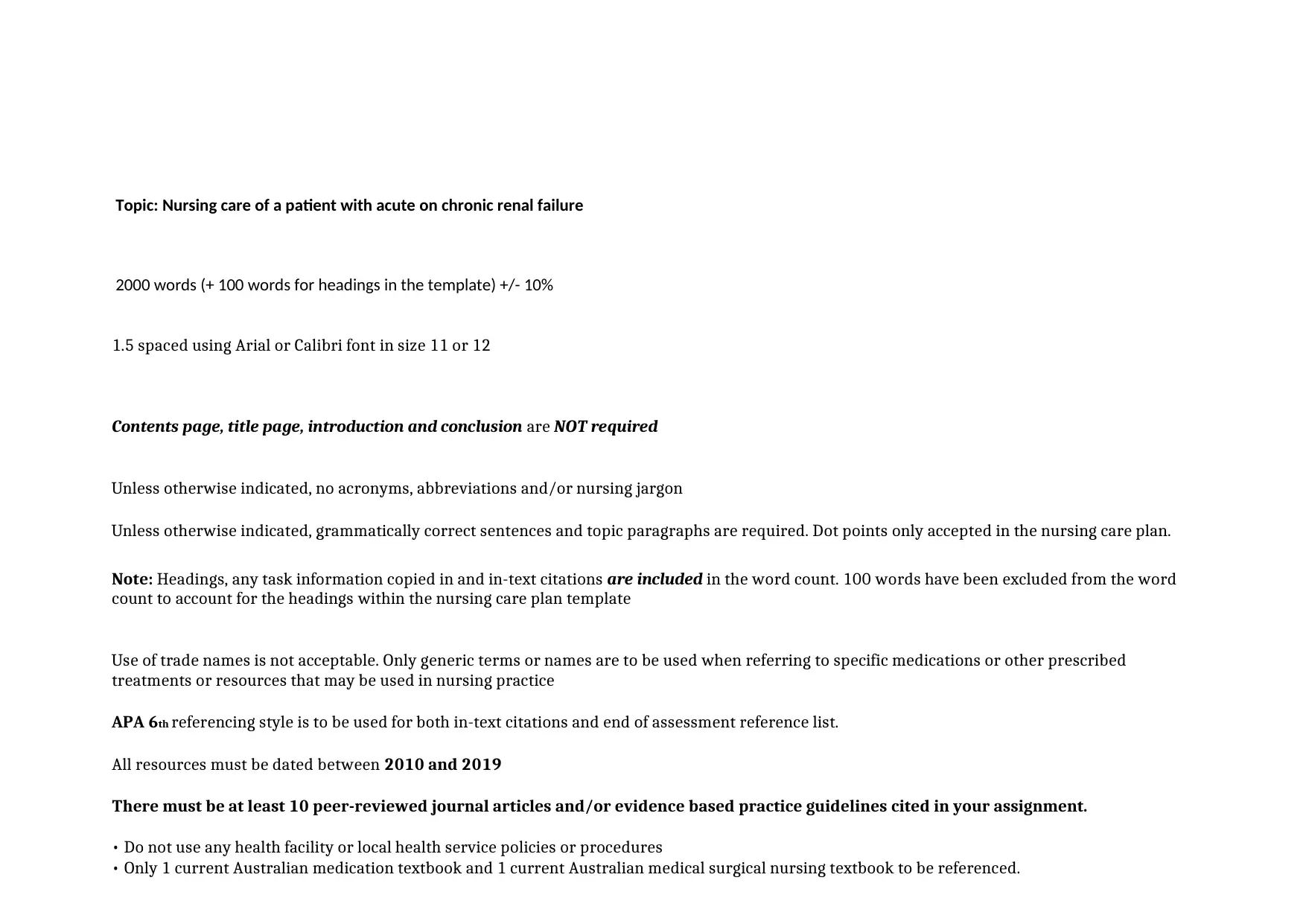
Topic: Nursing care of a patient with acute on chronic renal failure
2000 words (+ 100 words for headings in the template) +/- 10%
1.5 spaced using Arial or Calibri font in size 11 or 12
Contents page, title page, introduction and conclusion are NOT required
Unless otherwise indicated, no acronyms, abbreviations and/or nursing jargon
Unless otherwise indicated, grammatically correct sentences and topic paragraphs are required. Dot points only accepted in the nursing care plan.
Note: Headings, any task information copied in and in-text citations are included in the word count. 100 words have been excluded from the word
count to account for the headings within the nursing care plan template
Use of trade names is not acceptable. Only generic terms or names are to be used when referring to specific medications or other prescribed
treatments or resources that may be used in nursing practice
APA 6th referencing style is to be used for both in-text citations and end of assessment reference list.
All resources must be dated between 2010 and 2019
There must be at least 10 peer-reviewed journal articles and/or evidence based practice guidelines cited in your assignment.
• Do not use any health facility or local health service policies or procedures
• Only 1 current Australian medication textbook and 1 current Australian medical surgical nursing textbook to be referenced.
2000 words (+ 100 words for headings in the template) +/- 10%
1.5 spaced using Arial or Calibri font in size 11 or 12
Contents page, title page, introduction and conclusion are NOT required
Unless otherwise indicated, no acronyms, abbreviations and/or nursing jargon
Unless otherwise indicated, grammatically correct sentences and topic paragraphs are required. Dot points only accepted in the nursing care plan.
Note: Headings, any task information copied in and in-text citations are included in the word count. 100 words have been excluded from the word
count to account for the headings within the nursing care plan template
Use of trade names is not acceptable. Only generic terms or names are to be used when referring to specific medications or other prescribed
treatments or resources that may be used in nursing practice
APA 6th referencing style is to be used for both in-text citations and end of assessment reference list.
All resources must be dated between 2010 and 2019
There must be at least 10 peer-reviewed journal articles and/or evidence based practice guidelines cited in your assignment.
• Do not use any health facility or local health service policies or procedures
• Only 1 current Australian medication textbook and 1 current Australian medical surgical nursing textbook to be referenced.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
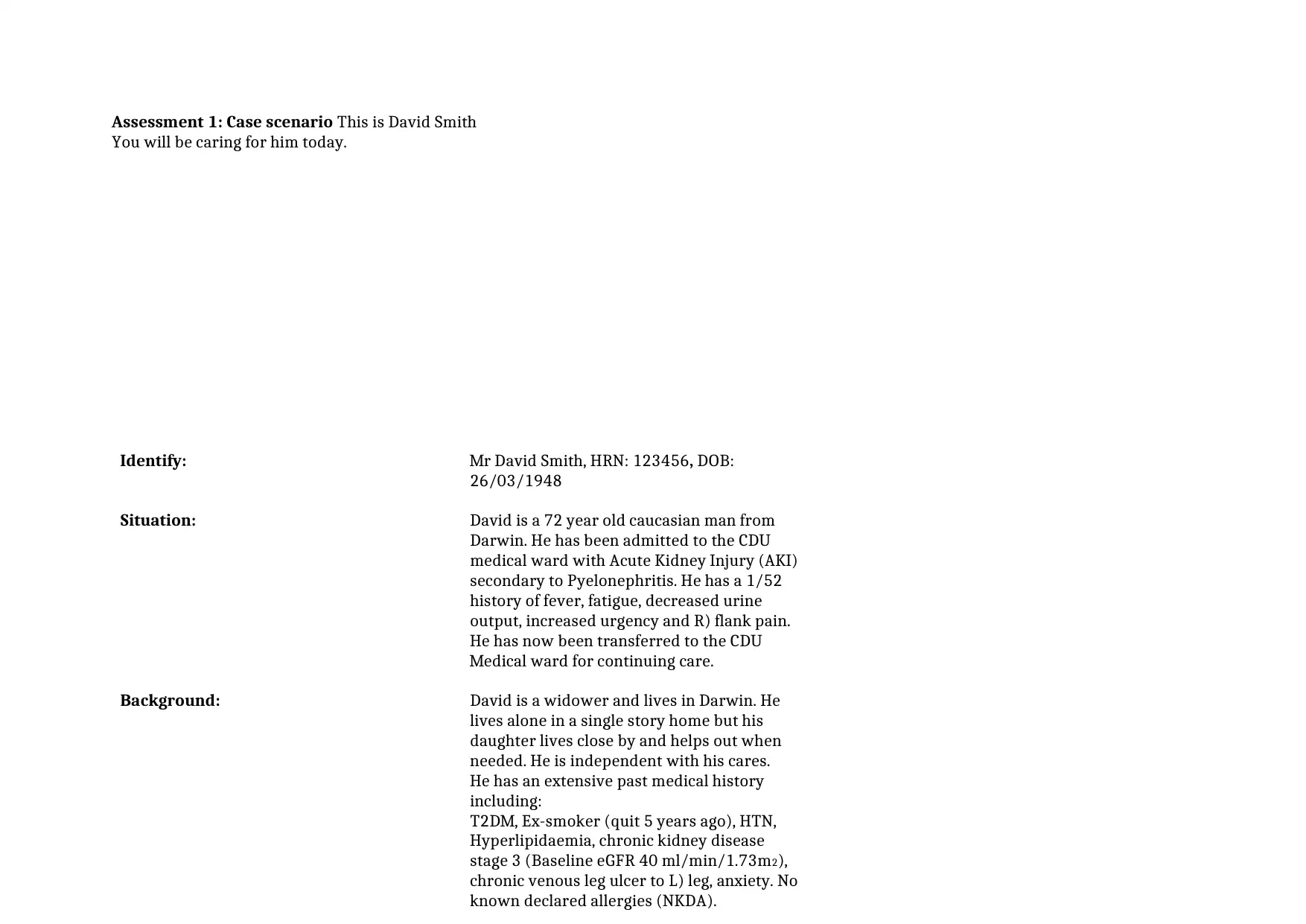
Assessment 1: Case scenario This is David Smith
You will be caring for him today.
Identify: Mr David Smith, HRN: 123456, DOB:
26/03/1948
Situation: David is a 72 year old caucasian man from
Darwin. He has been admitted to the CDU
medical ward with Acute Kidney Injury (AKI)
secondary to Pyelonephritis. He has a 1/52
history of fever, fatigue, decreased urine
output, increased urgency and R) flank pain.
He has now been transferred to the CDU
Medical ward for continuing care.
Background: David is a widower and lives in Darwin. He
lives alone in a single story home but his
daughter lives close by and helps out when
needed. He is independent with his cares.
He has an extensive past medical history
including:
T2DM, Ex-smoker (quit 5 years ago), HTN,
Hyperlipidaemia, chronic kidney disease
stage 3 (Baseline eGFR 40 ml/min/1.73m2),
chronic venous leg ulcer to L) leg, anxiety. No
known declared allergies (NKDA).
You will be caring for him today.
Identify: Mr David Smith, HRN: 123456, DOB:
26/03/1948
Situation: David is a 72 year old caucasian man from
Darwin. He has been admitted to the CDU
medical ward with Acute Kidney Injury (AKI)
secondary to Pyelonephritis. He has a 1/52
history of fever, fatigue, decreased urine
output, increased urgency and R) flank pain.
He has now been transferred to the CDU
Medical ward for continuing care.
Background: David is a widower and lives in Darwin. He
lives alone in a single story home but his
daughter lives close by and helps out when
needed. He is independent with his cares.
He has an extensive past medical history
including:
T2DM, Ex-smoker (quit 5 years ago), HTN,
Hyperlipidaemia, chronic kidney disease
stage 3 (Baseline eGFR 40 ml/min/1.73m2),
chronic venous leg ulcer to L) leg, anxiety. No
known declared allergies (NKDA).
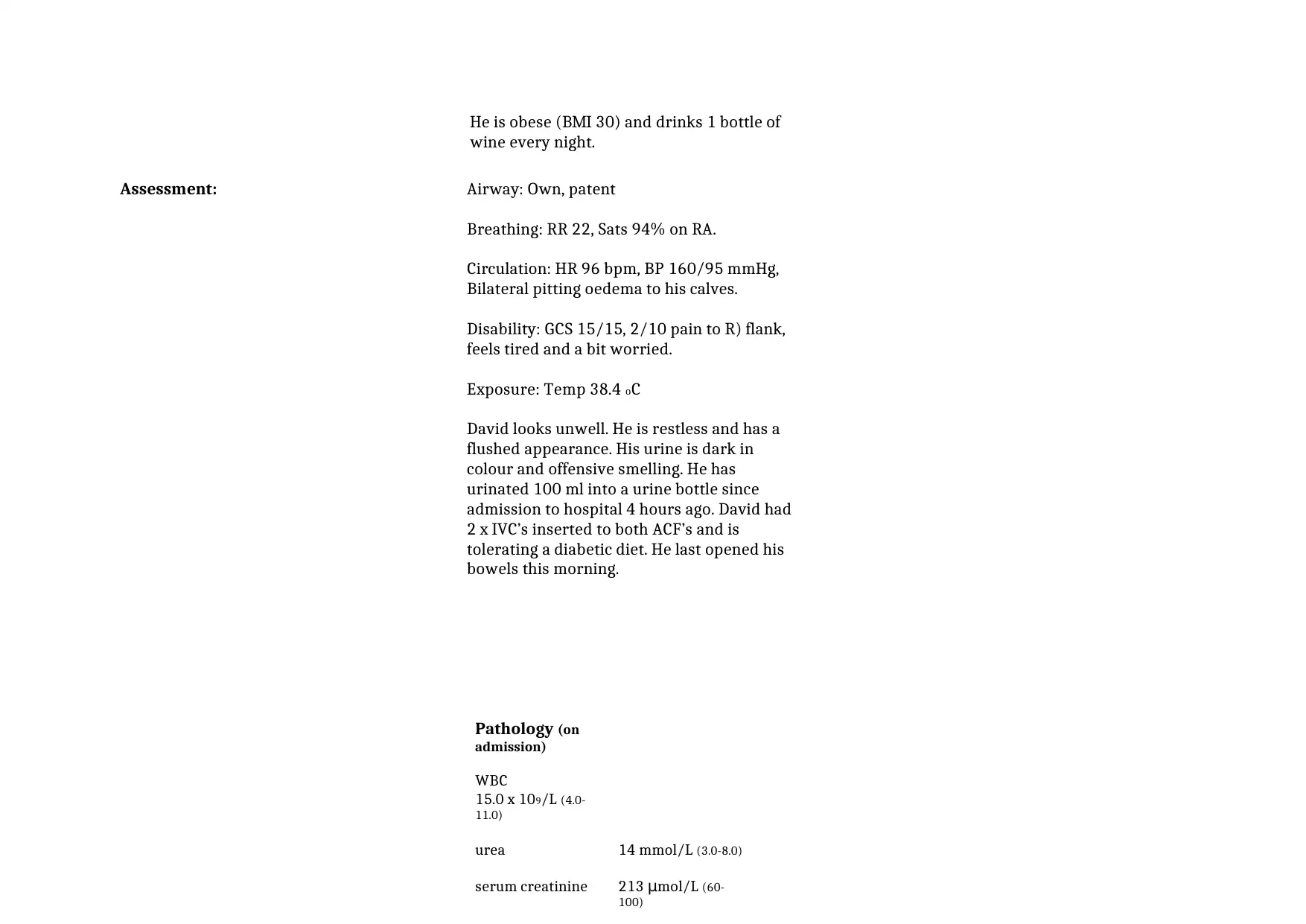
He is obese (BMI 30) and drinks 1 bottle of
wine every night.
Assessment: Airway: Own, patent
Breathing: RR 22, Sats 94% on RA.
Circulation: HR 96 bpm, BP 160/95 mmHg,
Bilateral pitting oedema to his calves.
Disability: GCS 15/15, 2/10 pain to R) flank,
feels tired and a bit worried.
Exposure: Temp 38.4 oC
David looks unwell. He is restless and has a
flushed appearance. His urine is dark in
colour and offensive smelling. He has
urinated 100 ml into a urine bottle since
admission to hospital 4 hours ago. David had
2 x IVC’s inserted to both ACF’s and is
tolerating a diabetic diet. He last opened his
bowels this morning.
Pathology (on
admission)
WBC
15.0 x 109/L (4.0-
11.0)
urea 14 mmol/L (3.0-8.0)
serum creatinine 213 μmol/L (60-
100)
wine every night.
Assessment: Airway: Own, patent
Breathing: RR 22, Sats 94% on RA.
Circulation: HR 96 bpm, BP 160/95 mmHg,
Bilateral pitting oedema to his calves.
Disability: GCS 15/15, 2/10 pain to R) flank,
feels tired and a bit worried.
Exposure: Temp 38.4 oC
David looks unwell. He is restless and has a
flushed appearance. His urine is dark in
colour and offensive smelling. He has
urinated 100 ml into a urine bottle since
admission to hospital 4 hours ago. David had
2 x IVC’s inserted to both ACF’s and is
tolerating a diabetic diet. He last opened his
bowels this morning.
Pathology (on
admission)
WBC
15.0 x 109/L (4.0-
11.0)
urea 14 mmol/L (3.0-8.0)
serum creatinine 213 μmol/L (60-
100)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
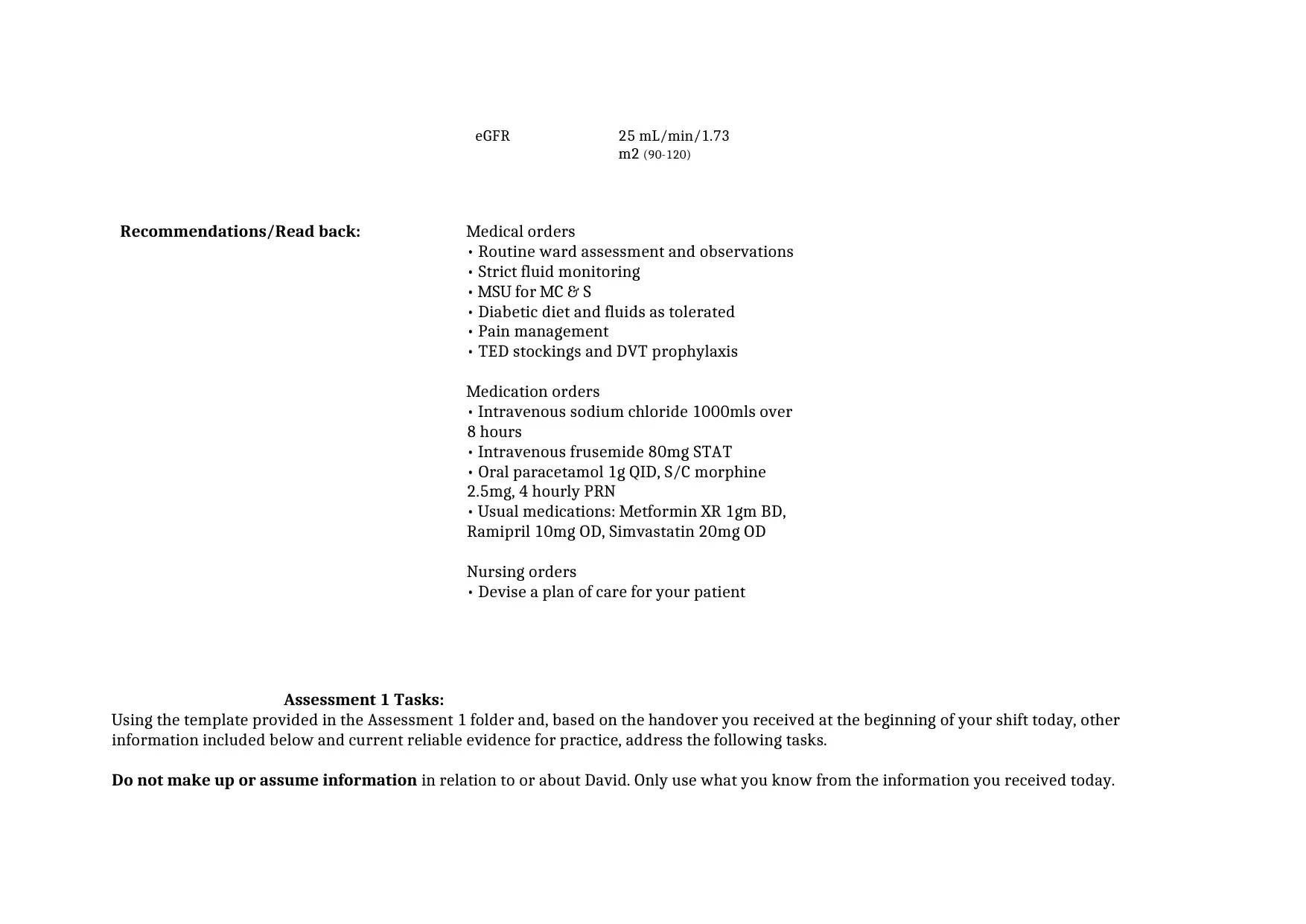
eGFR 25 mL/min/1.73
m2 (90-120)
Recommendations/Read back: Medical orders
• Routine ward assessment and observations
• Strict fluid monitoring
• MSU for MC & S
• Diabetic diet and fluids as tolerated
• Pain management
• TED stockings and DVT prophylaxis
Medication orders
• Intravenous sodium chloride 1000mls over
8 hours
• Intravenous frusemide 80mg STAT
• Oral paracetamol 1g QID, S/C morphine
2.5mg, 4 hourly PRN
• Usual medications: Metformin XR 1gm BD,
Ramipril 10mg OD, Simvastatin 20mg OD
Nursing orders
• Devise a plan of care for your patient
Assessment 1 Tasks:
Using the template provided in the Assessment 1 folder and, based on the handover you received at the beginning of your shift today, other
information included below and current reliable evidence for practice, address the following tasks.
Do not make up or assume information in relation to or about David. Only use what you know from the information you received today.
m2 (90-120)
Recommendations/Read back: Medical orders
• Routine ward assessment and observations
• Strict fluid monitoring
• MSU for MC & S
• Diabetic diet and fluids as tolerated
• Pain management
• TED stockings and DVT prophylaxis
Medication orders
• Intravenous sodium chloride 1000mls over
8 hours
• Intravenous frusemide 80mg STAT
• Oral paracetamol 1g QID, S/C morphine
2.5mg, 4 hourly PRN
• Usual medications: Metformin XR 1gm BD,
Ramipril 10mg OD, Simvastatin 20mg OD
Nursing orders
• Devise a plan of care for your patient
Assessment 1 Tasks:
Using the template provided in the Assessment 1 folder and, based on the handover you received at the beginning of your shift today, other
information included below and current reliable evidence for practice, address the following tasks.
Do not make up or assume information in relation to or about David. Only use what you know from the information you received today.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 1: Assessment
Based on the case scenario and in grammatically correct sentences identify:
• Three (3) priority nursing assessments you would conduct at the commencement of your shift
AND
For each assessment you have identified explain:
• Why it is necessary for David’s condition and nursing care?
• What consequences can occur if this assessment is not completed accurately?
• What chart or document could you use to assist with/record your assessments?
(Approximately 350 words)
Task 2:
Based solely on the handover you have received and using the template provided, complete a nursing care plan for David. Your plan must address
the physical, functional and psychosocial aspects of care.
Five (5) nursing problems have been provided for you. For each nursing problem on your care plan you need to identify;
• What it is related to?
• Goal of care
• Interventions
• Rationales for interventions
• Evaluation
Notes for Task 2 only
• Dot points may be used in the care plan template
• Appropriate professional language must be used – legally recognised abbreviations may be used in this task (care plan) but a KEY with full
terminology must be provided after
the assignment references – key will be excluded from word count tally
• Rationales must be appropriately referenced
(Approximately 1000 words)
Task 3: Patient education
Discharge planning
An important aspect of nursing practice is to effectively and succinctly communicate relevant information related to ongoing disease management or
prevention of reinfection or deterioration on discharge.
Based on the case scenario and in grammatically correct sentences identify:
• Three (3) priority nursing assessments you would conduct at the commencement of your shift
AND
For each assessment you have identified explain:
• Why it is necessary for David’s condition and nursing care?
• What consequences can occur if this assessment is not completed accurately?
• What chart or document could you use to assist with/record your assessments?
(Approximately 350 words)
Task 2:
Based solely on the handover you have received and using the template provided, complete a nursing care plan for David. Your plan must address
the physical, functional and psychosocial aspects of care.
Five (5) nursing problems have been provided for you. For each nursing problem on your care plan you need to identify;
• What it is related to?
• Goal of care
• Interventions
• Rationales for interventions
• Evaluation
Notes for Task 2 only
• Dot points may be used in the care plan template
• Appropriate professional language must be used – legally recognised abbreviations may be used in this task (care plan) but a KEY with full
terminology must be provided after
the assignment references – key will be excluded from word count tally
• Rationales must be appropriately referenced
(Approximately 1000 words)
Task 3: Patient education
Discharge planning
An important aspect of nursing practice is to effectively and succinctly communicate relevant information related to ongoing disease management or
prevention of reinfection or deterioration on discharge.
Patient education and discharge planning starts on admission and you need to provide David with education during your shift in
preparation for discharge home.
• Explain two (2) important points/topics you will need to include in David’s preparation for discharge to aid healing and prevent further illness.
For each education point identified provide:
• One (1) strategy to assist David to implement the education into his daily routine.
(Approximately 350 words)
Task 4: Documentation
An important legal requirement of nursing practice is to effectively and succinctly document relevant information, actions and outcomes related to
patient care and provide an accurate reflection of the health status of the patient, their responses to care and the patient’s perspective.
• Make an entry into David’s patient progress notes documenting the successful implementation of your nursing care plan.
You can choose any progress note format but your documentation must:
Demonstrate person-centred care
Adhere to the legal and professional standards for documentation
Appropriate professional language must be used – legally recognised abbreviations may be used in this task but a KEY with full terminology must
be provided after the assignment references - key will be excluded from word count tally
(Approximately 300 words)
Your assignment must include a reference list after the completion of the tasks and a key if you have used abbreviations in task 2 or 4.
Task 1
preparation for discharge home.
• Explain two (2) important points/topics you will need to include in David’s preparation for discharge to aid healing and prevent further illness.
For each education point identified provide:
• One (1) strategy to assist David to implement the education into his daily routine.
(Approximately 350 words)
Task 4: Documentation
An important legal requirement of nursing practice is to effectively and succinctly document relevant information, actions and outcomes related to
patient care and provide an accurate reflection of the health status of the patient, their responses to care and the patient’s perspective.
• Make an entry into David’s patient progress notes documenting the successful implementation of your nursing care plan.
You can choose any progress note format but your documentation must:
Demonstrate person-centred care
Adhere to the legal and professional standards for documentation
Appropriate professional language must be used – legally recognised abbreviations may be used in this task but a KEY with full terminology must
be provided after the assignment references - key will be excluded from word count tally
(Approximately 300 words)
Your assignment must include a reference list after the completion of the tasks and a key if you have used abbreviations in task 2 or 4.
Task 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Introduction:
The case scenario deals with a patient, M. David Smith who is a 72 year old Caucasian male who hails from Darwin. The patient at
present has been admitted to the CDU medical ward with a presenting complaint of Acute Kidney Injury which is secondary to Pyelonephritis.
The patient has a medical history of 1/52 fever, fatigue, decreased urine output, increased urgency and flank pain. In addition to this, the patient
is a widower who lives independently and is able to effectively manage his activities of daily living. Mr. Smith has a daughter who stays nearby
and occasionally helps him with his every day activities if required. The provided medical history of the patient further suggests that he is
diagnosed with Type II Diaabetes, HTN, Hyperlipidaemia, Chronic Kidney disease stage 3 (Baseline Egfr 40ml/min/1.73m2), chronic venous leg
ulcer in the left leg, obesity and anxiety. The provided information also reveals that Mr. Smith is an ex-smoker who quit smoking 5 years ago
and consumes a bottle of wine every night. This case study intends to delve deeper into the patient’s case scenario and make use of the evidence
based treatment strategies to prioritise care and create an effective care plan.
Task 1 Assessment:
On critically analysing the case scenario, it can be mentioned that the three nursing assessments that would be conducted by me at the
commencement of my shift would include, conducting a vital sign assessment, pain assessment and nutritional assessment. The rationale for
conducting a vital assessment would include assessing the vital signs of the patient so as to develop an overview about the state of physiological
condition of the patient. Research studies report that hypertension is one of the foremost co-morbid factors of Type II Diabetes mellitus (De Boer
et al. 2017). Hence, it is vital that while caring for a patient with Diabetes, a nursing professional must assess the level of blood pressure
periodically and document the observations. In addition to this, other vital signs that would be assessed include assessing the body temperature,
airway, heart rate, respiratory rate and the oxygen saturation rate. The documented observation data would suggest the current physiological
condition of the patient and based on the documented observation, appropriate intervention would be applied. The second set of assessment that
would be conducted would include the pain assessment. Upon presentment the patient had mentioned about experiencing pain in the right flank
region. Therefore, conducting a pain assessment would help to assess the level and type of pain sustained by the patient after the commencement
of the medication. The rationale for conducting the assessment can therefore be explained as the analysing the quality of pain currently
experienced by the patient and applying appropriate interventions to optimise the impact of pain (Cameron et al., 2015). The third assessment
that would be conducted includes the nutritional assessment and the rationale for the same can be explained as assessing the nutritional intake
and the nutritional needs of the patient. Research studies suggest that nutritional assessment is the systematic procedure of interpreting and
collecting health related information to understand the cause and nature of nutritional related health disorders (Landoni et al., 2016; James et al.,
2015). In this context it should be noted that the patient is tolerating a Diabetic diet, therefore conducting the nutritional assessment would help
to understand that whether or not the patient is consuming an optimal diet which has been devised as per his physical health condition. In
addition to this, the assessment would also help to estimate the impact of the Diabetic medications that the patient is currently consuming which
would help to analyse the blood glucose level. As suggested by the evidence base, Diabetic medication works by lowering the blood glucose
level but in order to maintain normal physiological functions, a minimal amount of blood glucose level is required (James et al., 2015). If a
patient does not consume an adequate amount of nutrition, then the blood glucose level might fall below the normal range and lead to adverse
complications.
The above mentioned three assessments are vital for David as it would help to analyse the current physiological state of David and direct
the nursing care professional to implement appropriate measures so as to monitor the physical health condition of the patient and implement
appropriate care interventions to accelerate the process of recovery.
The case scenario deals with a patient, M. David Smith who is a 72 year old Caucasian male who hails from Darwin. The patient at
present has been admitted to the CDU medical ward with a presenting complaint of Acute Kidney Injury which is secondary to Pyelonephritis.
The patient has a medical history of 1/52 fever, fatigue, decreased urine output, increased urgency and flank pain. In addition to this, the patient
is a widower who lives independently and is able to effectively manage his activities of daily living. Mr. Smith has a daughter who stays nearby
and occasionally helps him with his every day activities if required. The provided medical history of the patient further suggests that he is
diagnosed with Type II Diaabetes, HTN, Hyperlipidaemia, Chronic Kidney disease stage 3 (Baseline Egfr 40ml/min/1.73m2), chronic venous leg
ulcer in the left leg, obesity and anxiety. The provided information also reveals that Mr. Smith is an ex-smoker who quit smoking 5 years ago
and consumes a bottle of wine every night. This case study intends to delve deeper into the patient’s case scenario and make use of the evidence
based treatment strategies to prioritise care and create an effective care plan.
Task 1 Assessment:
On critically analysing the case scenario, it can be mentioned that the three nursing assessments that would be conducted by me at the
commencement of my shift would include, conducting a vital sign assessment, pain assessment and nutritional assessment. The rationale for
conducting a vital assessment would include assessing the vital signs of the patient so as to develop an overview about the state of physiological
condition of the patient. Research studies report that hypertension is one of the foremost co-morbid factors of Type II Diabetes mellitus (De Boer
et al. 2017). Hence, it is vital that while caring for a patient with Diabetes, a nursing professional must assess the level of blood pressure
periodically and document the observations. In addition to this, other vital signs that would be assessed include assessing the body temperature,
airway, heart rate, respiratory rate and the oxygen saturation rate. The documented observation data would suggest the current physiological
condition of the patient and based on the documented observation, appropriate intervention would be applied. The second set of assessment that
would be conducted would include the pain assessment. Upon presentment the patient had mentioned about experiencing pain in the right flank
region. Therefore, conducting a pain assessment would help to assess the level and type of pain sustained by the patient after the commencement
of the medication. The rationale for conducting the assessment can therefore be explained as the analysing the quality of pain currently
experienced by the patient and applying appropriate interventions to optimise the impact of pain (Cameron et al., 2015). The third assessment
that would be conducted includes the nutritional assessment and the rationale for the same can be explained as assessing the nutritional intake
and the nutritional needs of the patient. Research studies suggest that nutritional assessment is the systematic procedure of interpreting and
collecting health related information to understand the cause and nature of nutritional related health disorders (Landoni et al., 2016; James et al.,
2015). In this context it should be noted that the patient is tolerating a Diabetic diet, therefore conducting the nutritional assessment would help
to understand that whether or not the patient is consuming an optimal diet which has been devised as per his physical health condition. In
addition to this, the assessment would also help to estimate the impact of the Diabetic medications that the patient is currently consuming which
would help to analyse the blood glucose level. As suggested by the evidence base, Diabetic medication works by lowering the blood glucose
level but in order to maintain normal physiological functions, a minimal amount of blood glucose level is required (James et al., 2015). If a
patient does not consume an adequate amount of nutrition, then the blood glucose level might fall below the normal range and lead to adverse
complications.
The above mentioned three assessments are vital for David as it would help to analyse the current physiological state of David and direct
the nursing care professional to implement appropriate measures so as to monitor the physical health condition of the patient and implement
appropriate care interventions to accelerate the process of recovery.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
If the above listed assessments are not carried out then the process of monitoring the physiological body process of the patient would
become exceedingly difficult. In addition to this, evaluation of the impact of the administered medication would also be extremely complex
which serves as a key indication of the effectiveness of the devised treatment measures.
For the purpose of documentation the progress notes and the medication chart would be filled up by me and in order to assist the next RN
after the completion of my shift, I would effectively communicate and present a brief about the current physiological state of the patient. In
addition to this, I would also hand over the progress notes, medication chart and the ISBAR handover which would detail the observed data and
assist the RN with the continued treatment process.
Task 2
become exceedingly difficult. In addition to this, evaluation of the impact of the administered medication would also be extremely complex
which serves as a key indication of the effectiveness of the devised treatment measures.
For the purpose of documentation the progress notes and the medication chart would be filled up by me and in order to assist the next RN
after the completion of my shift, I would effectively communicate and present a brief about the current physiological state of the patient. In
addition to this, I would also hand over the progress notes, medication chart and the ISBAR handover which would detail the observed data and
assist the RN with the continued treatment process.
Task 2
Nursing Care Plan: David Smith
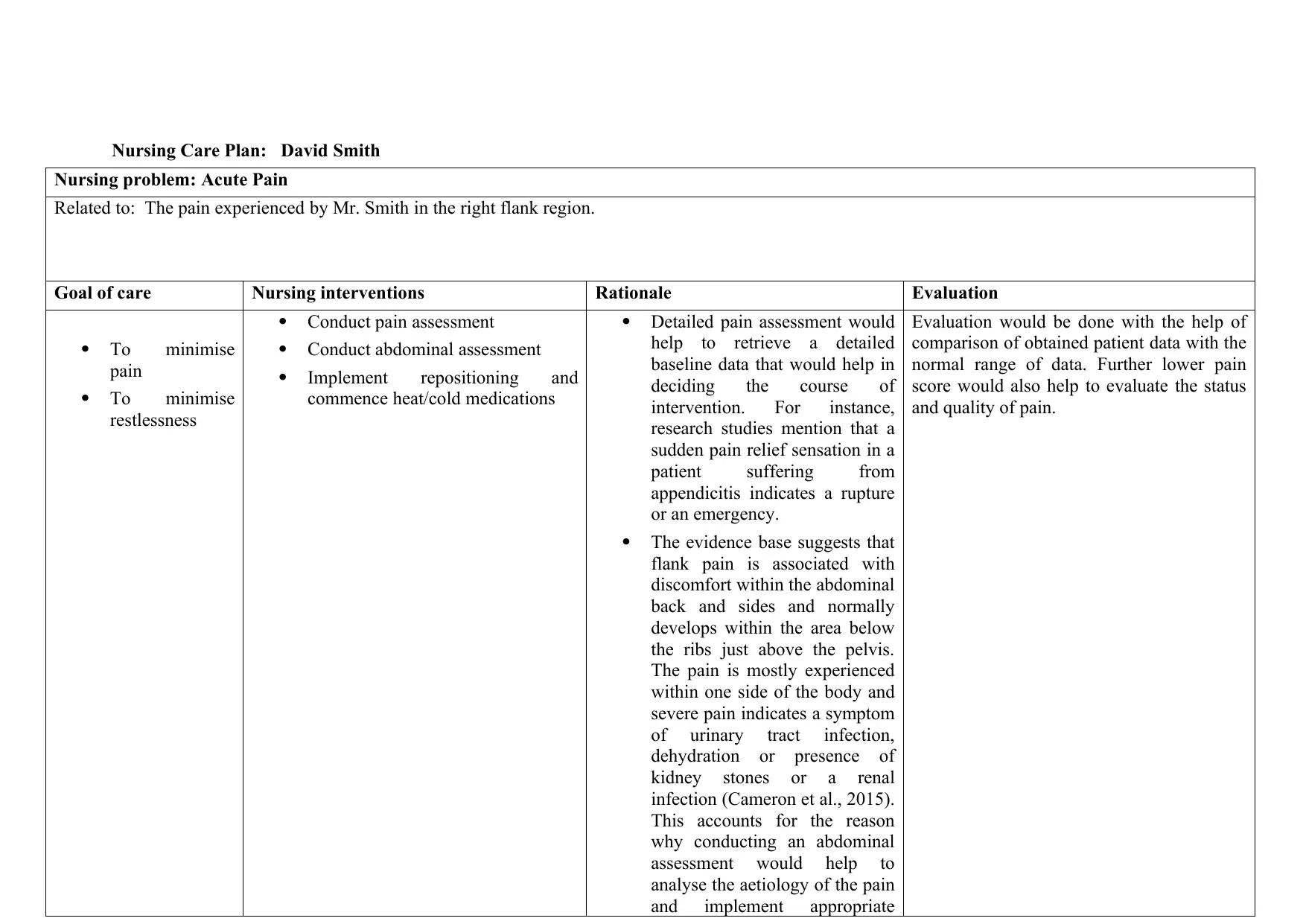
Nursing problem: Acute Pain
Related to: The pain experienced by Mr. Smith in the right flank region.
Goal of care Nursing interventions Rationale Evaluation
To minimise
pain
To minimise
restlessness
Conduct pain assessment
Conduct abdominal assessment
Implement repositioning and
commence heat/cold medications
Detailed pain assessment would
help to retrieve a detailed
baseline data that would help in
deciding the course of
intervention. For instance,
research studies mention that a
sudden pain relief sensation in a
patient suffering from
appendicitis indicates a rupture
or an emergency.
The evidence base suggests that
flank pain is associated with
discomfort within the abdominal
back and sides and normally
develops within the area below
the ribs just above the pelvis.
The pain is mostly experienced
within one side of the body and
severe pain indicates a symptom
of urinary tract infection,
dehydration or presence of
kidney stones or a renal
infection (Cameron et al., 2015).
This accounts for the reason
why conducting an abdominal
assessment would help to
analyse the aetiology of the pain
and implement appropriate
Evaluation would be done with the help of
comparison of obtained patient data with the
normal range of data. Further lower pain
score would also help to evaluate the status
and quality of pain.
Nursing problem: Acute Pain
Related to: The pain experienced by Mr. Smith in the right flank region.
Goal of care Nursing interventions Rationale Evaluation
To minimise
pain
To minimise
restlessness
Conduct pain assessment
Conduct abdominal assessment
Implement repositioning and
commence heat/cold medications
Detailed pain assessment would
help to retrieve a detailed
baseline data that would help in
deciding the course of
intervention. For instance,
research studies mention that a
sudden pain relief sensation in a
patient suffering from
appendicitis indicates a rupture
or an emergency.
The evidence base suggests that
flank pain is associated with
discomfort within the abdominal
back and sides and normally
develops within the area below
the ribs just above the pelvis.
The pain is mostly experienced
within one side of the body and
severe pain indicates a symptom
of urinary tract infection,
dehydration or presence of
kidney stones or a renal
infection (Cameron et al., 2015).
This accounts for the reason
why conducting an abdominal
assessment would help to
analyse the aetiology of the pain
and implement appropriate
Evaluation would be done with the help of
comparison of obtained patient data with the
normal range of data. Further lower pain
score would also help to evaluate the status
and quality of pain.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
measures to foster improved
outcome.
The evidence base also suggests
that flank pain is associated with
discomfort experienced while
relaxing or sleeping.
Repositioning the patient and
inducing hot/cold treatment can
help in envisioning relief (James
et al., 2015).
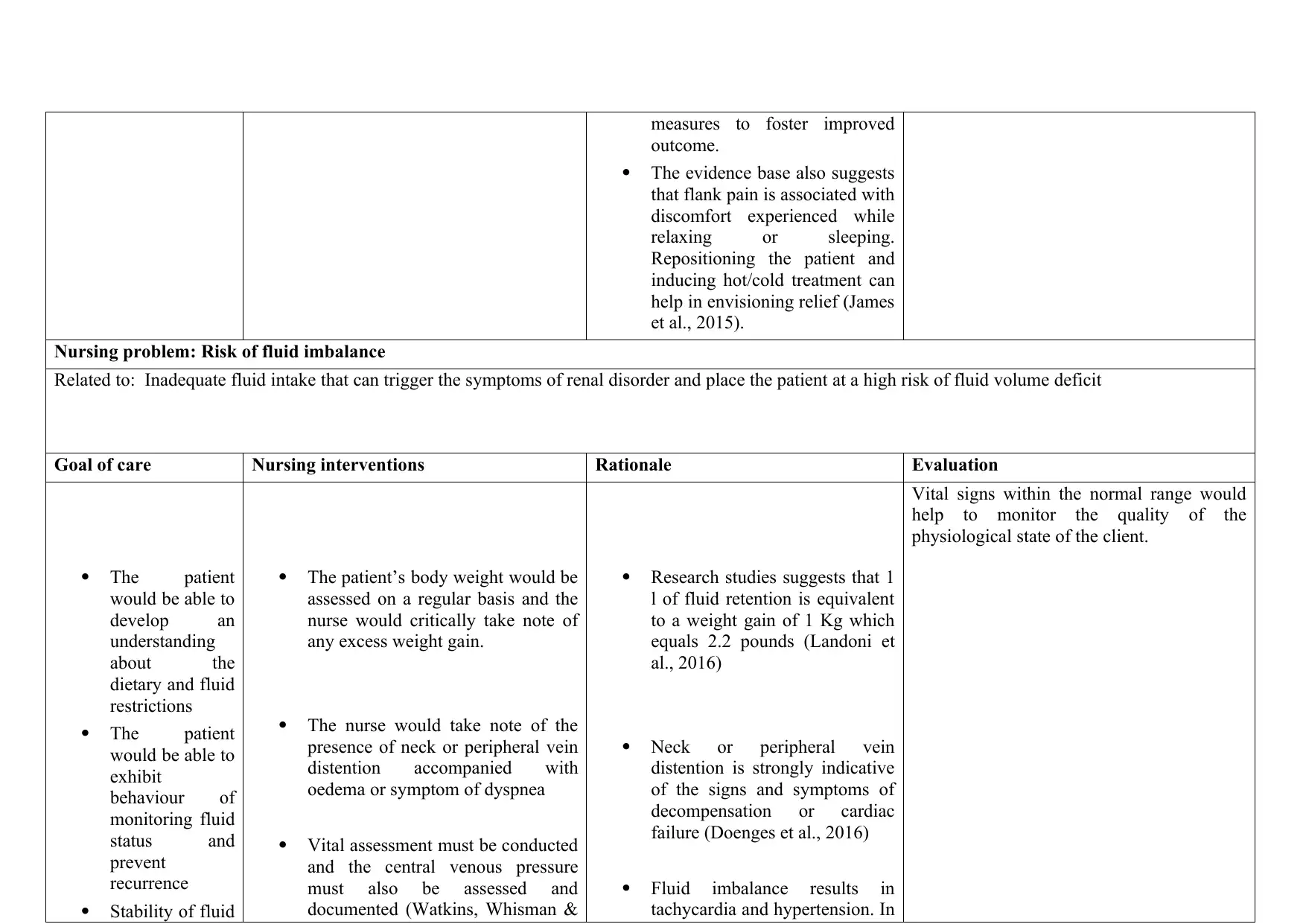
Nursing problem: Risk of fluid imbalance
Related to: Inadequate fluid intake that can trigger the symptoms of renal disorder and place the patient at a high risk of fluid volume deficit
Goal of care Nursing interventions Rationale Evaluation
The patient
would be able to
develop an
understanding
about the
dietary and fluid
restrictions
The patient
would be able to
exhibit
behaviour of
monitoring fluid
status and
prevent
recurrence
Stability of fluid
The patient’s body weight would be
assessed on a regular basis and the
nurse would critically take note of
any excess weight gain.
The nurse would take note of the
presence of neck or peripheral vein
distention accompanied with
oedema or symptom of dyspnea
Vital assessment must be conducted
and the central venous pressure
must also be assessed and
documented (Watkins, Whisman &
Research studies suggests that 1
l of fluid retention is equivalent
to a weight gain of 1 Kg which
equals 2.2 pounds (Landoni et
al., 2016)
Neck or peripheral vein
distention is strongly indicative
of the signs and symptoms of
decompensation or cardiac
failure (Doenges et al., 2016)
Fluid imbalance results in
tachycardia and hypertension. In
Vital signs within the normal range would
help to monitor the quality of the
physiological state of the client.
outcome.
The evidence base also suggests
that flank pain is associated with
discomfort experienced while
relaxing or sleeping.
Repositioning the patient and
inducing hot/cold treatment can
help in envisioning relief (James
et al., 2015).
Nursing problem: Risk of fluid imbalance
Related to: Inadequate fluid intake that can trigger the symptoms of renal disorder and place the patient at a high risk of fluid volume deficit
Goal of care Nursing interventions Rationale Evaluation
The patient
would be able to
develop an
understanding
about the
dietary and fluid
restrictions
The patient
would be able to
exhibit
behaviour of
monitoring fluid
status and
prevent
recurrence
Stability of fluid
The patient’s body weight would be
assessed on a regular basis and the
nurse would critically take note of
any excess weight gain.
The nurse would take note of the
presence of neck or peripheral vein
distention accompanied with
oedema or symptom of dyspnea
Vital assessment must be conducted
and the central venous pressure
must also be assessed and
documented (Watkins, Whisman &
Research studies suggests that 1
l of fluid retention is equivalent
to a weight gain of 1 Kg which
equals 2.2 pounds (Landoni et
al., 2016)
Neck or peripheral vein
distention is strongly indicative
of the signs and symptoms of
decompensation or cardiac
failure (Doenges et al., 2016)
Fluid imbalance results in
tachycardia and hypertension. In
Vital signs within the normal range would
help to monitor the quality of the
physiological state of the client.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
volume would
be detected by
means of stable
vital sign
assessment
Booker, 2016) certain cases, Tachypnea might
be present with or without
Dyspnea. Increase in central
venous pressure accompanied
with adventitious breath sounds
is generally indicative of
Dyspnea. In addition to this,
hypertension may also occur
which might trigger serious
conditions such as cardiac
failure (Doenges et al., 2016).
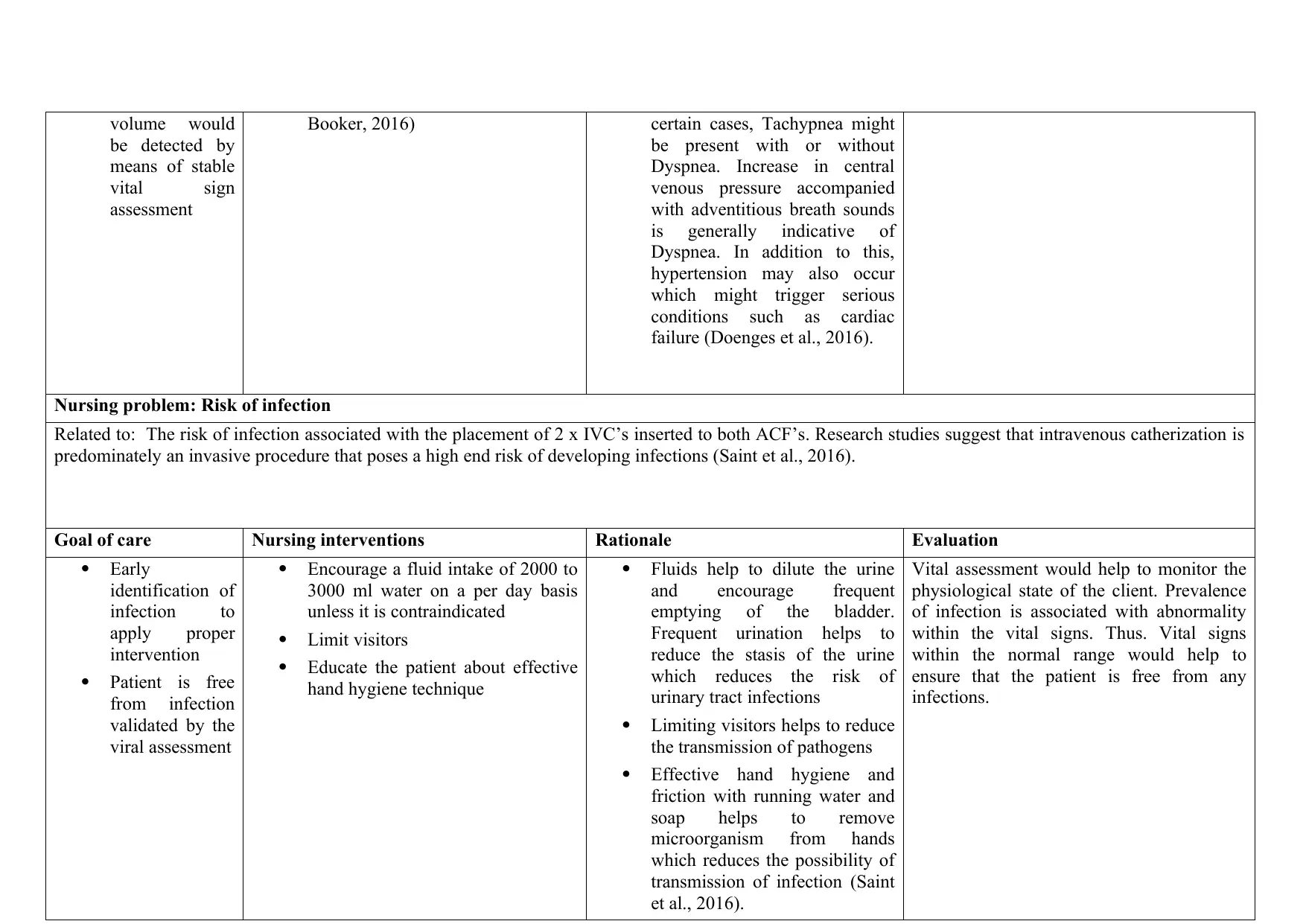
Nursing problem: Risk of infection
Related to: The risk of infection associated with the placement of 2 x IVC’s inserted to both ACF’s. Research studies suggest that intravenous catherization is
predominately an invasive procedure that poses a high end risk of developing infections (Saint et al., 2016).
Goal of care Nursing interventions Rationale Evaluation
Early
identification of
infection to
apply proper
intervention
Patient is free
from infection
validated by the
viral assessment
Encourage a fluid intake of 2000 to
3000 ml water on a per day basis
unless it is contraindicated
Limit visitors
Educate the patient about effective
hand hygiene technique
Fluids help to dilute the urine
and encourage frequent
emptying of the bladder.
Frequent urination helps to
reduce the stasis of the urine
which reduces the risk of
urinary tract infections
Limiting visitors helps to reduce
the transmission of pathogens
Effective hand hygiene and
friction with running water and
soap helps to remove
microorganism from hands
which reduces the possibility of
transmission of infection (Saint
et al., 2016).
Vital assessment would help to monitor the
physiological state of the client. Prevalence
of infection is associated with abnormality
within the vital signs. Thus. Vital signs
within the normal range would help to
ensure that the patient is free from any
infections.
be detected by
means of stable
vital sign
assessment
Booker, 2016) certain cases, Tachypnea might
be present with or without
Dyspnea. Increase in central
venous pressure accompanied
with adventitious breath sounds
is generally indicative of
Dyspnea. In addition to this,
hypertension may also occur
which might trigger serious
conditions such as cardiac
failure (Doenges et al., 2016).
Nursing problem: Risk of infection
Related to: The risk of infection associated with the placement of 2 x IVC’s inserted to both ACF’s. Research studies suggest that intravenous catherization is
predominately an invasive procedure that poses a high end risk of developing infections (Saint et al., 2016).
Goal of care Nursing interventions Rationale Evaluation
Early
identification of
infection to
apply proper
intervention
Patient is free
from infection
validated by the
viral assessment
Encourage a fluid intake of 2000 to
3000 ml water on a per day basis
unless it is contraindicated
Limit visitors
Educate the patient about effective
hand hygiene technique
Fluids help to dilute the urine
and encourage frequent
emptying of the bladder.
Frequent urination helps to
reduce the stasis of the urine
which reduces the risk of
urinary tract infections
Limiting visitors helps to reduce
the transmission of pathogens
Effective hand hygiene and
friction with running water and
soap helps to remove
microorganism from hands
which reduces the possibility of
transmission of infection (Saint
et al., 2016).
Vital assessment would help to monitor the
physiological state of the client. Prevalence
of infection is associated with abnormality
within the vital signs. Thus. Vital signs
within the normal range would help to
ensure that the patient is free from any
infections.
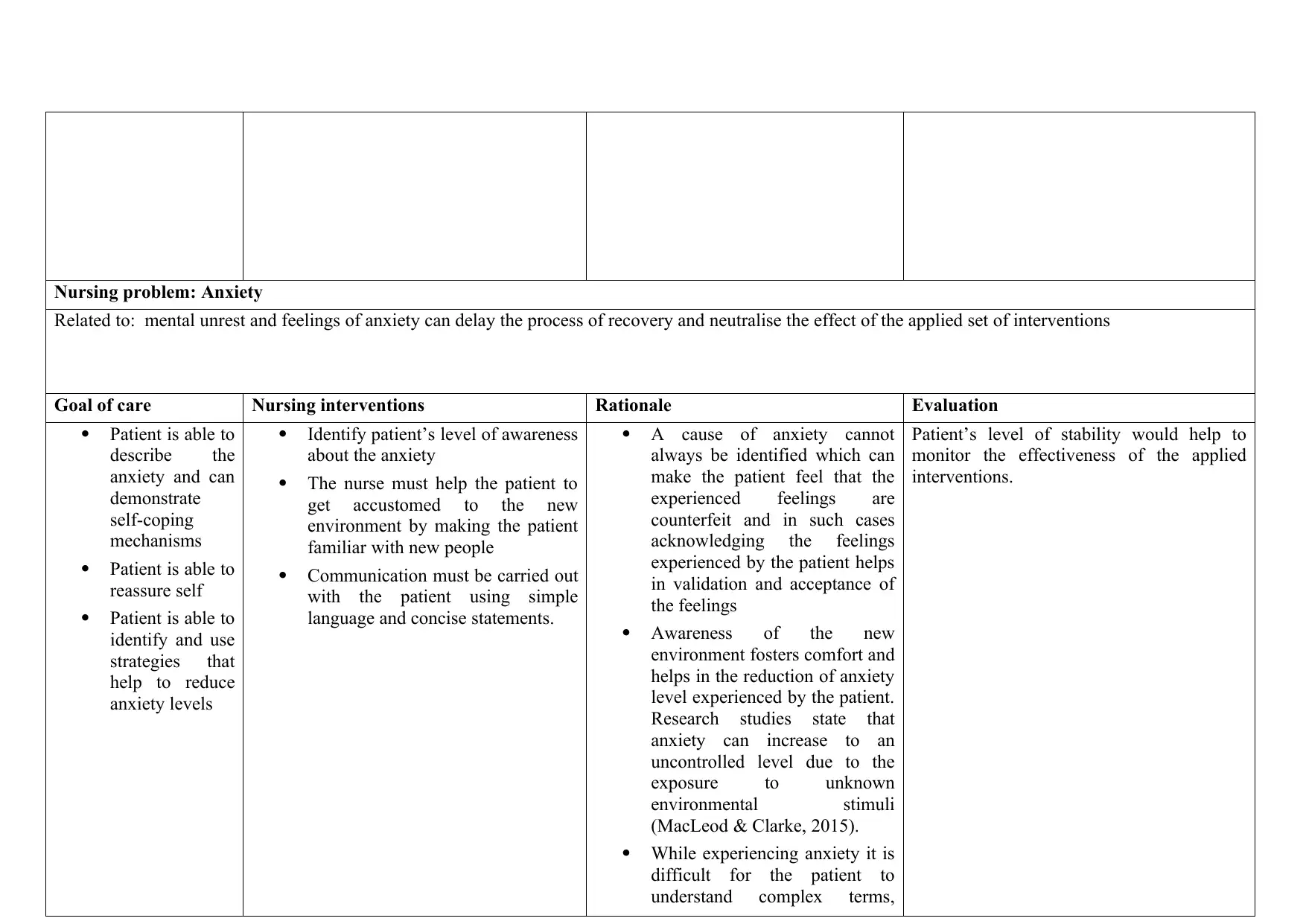
Nursing problem: Anxiety
Related to: mental unrest and feelings of anxiety can delay the process of recovery and neutralise the effect of the applied set of interventions
Goal of care Nursing interventions Rationale Evaluation
Patient is able to
describe the
anxiety and can
demonstrate
self-coping
mechanisms
Patient is able to
reassure self
Patient is able to
identify and use
strategies that
help to reduce
anxiety levels
Identify patient’s level of awareness
about the anxiety
The nurse must help the patient to
get accustomed to the new
environment by making the patient
familiar with new people
Communication must be carried out
with the patient using simple
language and concise statements.
A cause of anxiety cannot
always be identified which can
make the patient feel that the
experienced feelings are
counterfeit and in such cases
acknowledging the feelings
experienced by the patient helps
in validation and acceptance of
the feelings
Awareness of the new
environment fosters comfort and
helps in the reduction of anxiety
level experienced by the patient.
Research studies state that
anxiety can increase to an
uncontrolled level due to the
exposure to unknown
environmental stimuli
(MacLeod & Clarke, 2015).
While experiencing anxiety it is
difficult for the patient to
understand complex terms,
Patient’s level of stability would help to
monitor the effectiveness of the applied
interventions.
Related to: mental unrest and feelings of anxiety can delay the process of recovery and neutralise the effect of the applied set of interventions
Goal of care Nursing interventions Rationale Evaluation
Patient is able to
describe the
anxiety and can
demonstrate
self-coping
mechanisms
Patient is able to
reassure self
Patient is able to
identify and use
strategies that
help to reduce
anxiety levels
Identify patient’s level of awareness
about the anxiety
The nurse must help the patient to
get accustomed to the new
environment by making the patient
familiar with new people
Communication must be carried out
with the patient using simple
language and concise statements.
A cause of anxiety cannot
always be identified which can
make the patient feel that the
experienced feelings are
counterfeit and in such cases
acknowledging the feelings
experienced by the patient helps
in validation and acceptance of
the feelings
Awareness of the new
environment fosters comfort and
helps in the reduction of anxiety
level experienced by the patient.
Research studies state that
anxiety can increase to an
uncontrolled level due to the
exposure to unknown
environmental stimuli
(MacLeod & Clarke, 2015).
While experiencing anxiety it is
difficult for the patient to
understand complex terms,
Patient’s level of stability would help to
monitor the effectiveness of the applied
interventions.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




