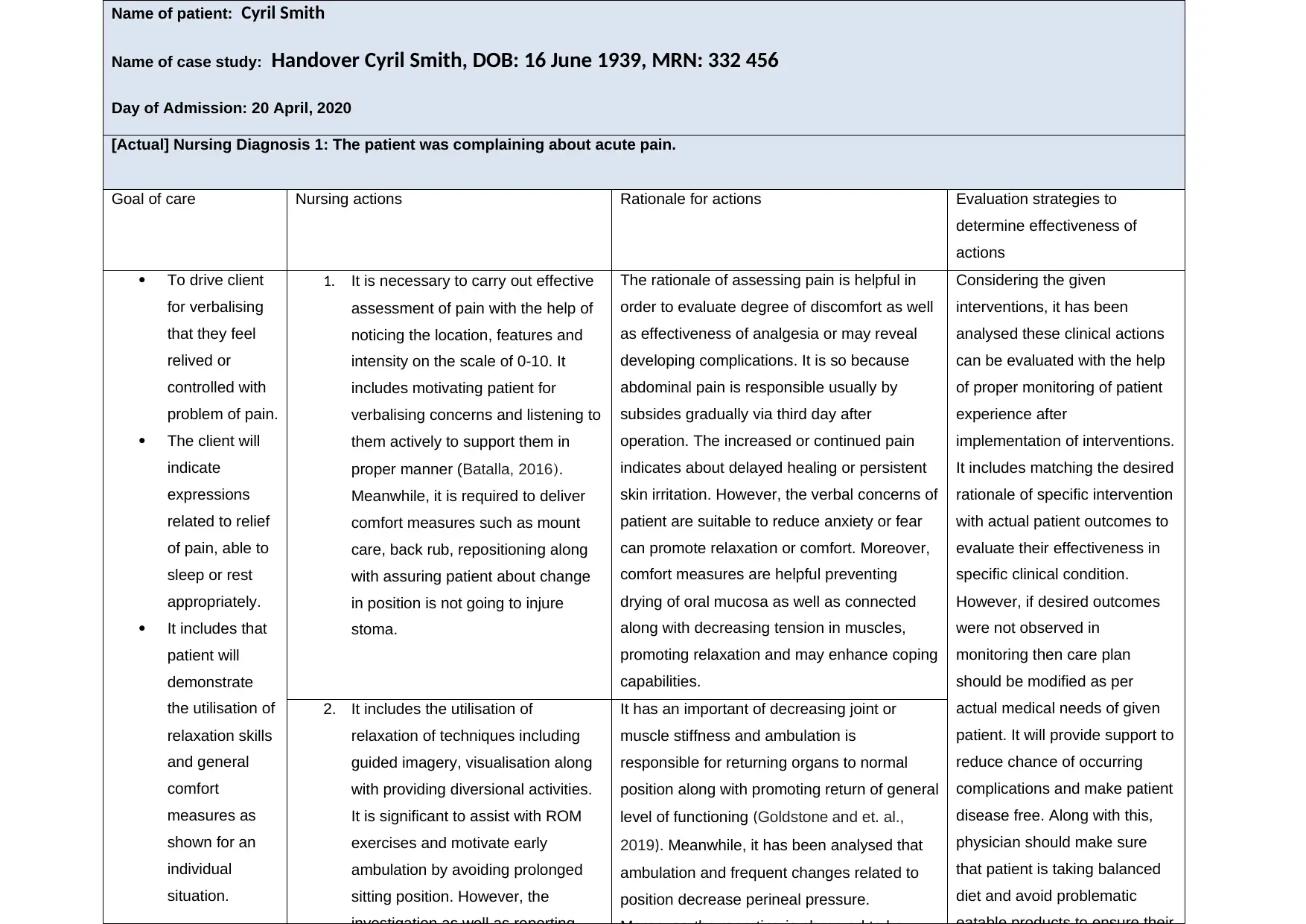
Detailed Nursing Care Plan for Cyril Smith: Post-Operative Recovery
VerifiedAdded on 2023/01/11
|3
|864
|95
Case Study
AI Summary
This case study presents a detailed nursing care plan for Cyril Smith, focusing on post-operative care. It identifies a nursing diagnosis of acute pain and outlines a goal of care, along with three nursing actions for pain assessment and management, including verbalizing concerns and implementing comfort measures. Each action is supported by a rationale explaining its effectiveness, such as promoting relaxation and preventing complications. Evaluation strategies, such as monitoring the patient's pain level and overall condition, are included to assess the effectiveness of interventions. References to relevant literature support the nursing actions and rationales. The care plan emphasizes a patient-centered approach, considering both physical and emotional needs to facilitate optimal recovery. It is a comprehensive analysis of the patient’s condition and the interventions required to ensure a positive health outcome.
1 out of 3








![[object Object]](/_next/static/media/star-bottom.7253800d.svg)