Neonatal Case Study: Hyperbilirubinemia, Assessment, and Interventions
VerifiedAdded on 2022/10/04
|8
|1729
|15
Case Study
AI Summary
This case study focuses on a 2-day-old female newborn, Maria, presenting with symptoms of hyperbilirubinemia. The assessment reveals a N-PASS pain score of 5, indicating pain, and a yellow tint indicative of jaundice. The mother reports the baby is sleepy, has poor feeding, and is frustrated during breastfeeding. The assessment, using the SBAR format, highlights the need for delayed discharge and further investigation. Maria falls into the low-intermediate risk zone of hyperbilirubinemia based on the Bhutani Nomogram. The diagnosis is advancing pathological unconjugated hyperbilirubinemia, with an expected treatment plan of phototherapy. The case study outlines the treatment plan, potential complications such as bilirubin-induced neurologic dysfunction (BIND) and kernicterus, and family-centered interventions, including education about jaundice, home management, and the importance of follow-up. Bowlby's attachment theory is also applied, highlighting the importance of secure attachments. The nursing interventions include monitoring bilirubin levels, providing phototherapy, and educating the parents about the condition, its management, and potential complications. The expected outcomes are to control the jaundice, resolve it within the first week of life, and prevent CNS involvement. Further laboratory tests will be warranted if hyperbilirubinemia persists. References are provided in APA format, including peer-reviewed articles and textbook references, as per the assignment brief requirements.
Mini case study #2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1. When nurse assessed the baby, her pain score based on N-PASS tool was 5 and a score
which is more than +3 indicates pain in N-PASS tool (Hillman, Tabrizi, Gauda, Carson,
& Aucott, 2015). Nurse also noticed a yellow tint to her face that spreads to her bilateral
nipple line which was unnatural as opposed to normal baby’s skin. When nurse enquired
the mother about the baby she complained that the baby is always sleepy, does not want
to breastfeed and when she latched after multiple attempts, baby used to get frustrated
and begin to cry.
2. Report of pertinent findings
S Maria is a full term baby who was planned to be discharged but there are
certain signs of complications.
B The delivery was normal without complications and the first two days post-
delivery also seemed normal for both baby and mother.
A During discharge planning, the assessment done by the off-going nurse but
second assessment done on mother’s distress
R Discharge of baby should be delayed and further investigations based on new
findings must be done in order to find out the underlying cause of newly
developed symptoms.
3. As per Bhutani Nomogram, Maria falls into low intermediate risk zone of
hyperbilirubinemia (O'Reilly, Walsh, Allen, & Corcoran, 2015).
which is more than +3 indicates pain in N-PASS tool (Hillman, Tabrizi, Gauda, Carson,
& Aucott, 2015). Nurse also noticed a yellow tint to her face that spreads to her bilateral
nipple line which was unnatural as opposed to normal baby’s skin. When nurse enquired
the mother about the baby she complained that the baby is always sleepy, does not want
to breastfeed and when she latched after multiple attempts, baby used to get frustrated
and begin to cry.
2. Report of pertinent findings
S Maria is a full term baby who was planned to be discharged but there are
certain signs of complications.
B The delivery was normal without complications and the first two days post-
delivery also seemed normal for both baby and mother.
A During discharge planning, the assessment done by the off-going nurse but
second assessment done on mother’s distress
R Discharge of baby should be delayed and further investigations based on new
findings must be done in order to find out the underlying cause of newly
developed symptoms.
3. As per Bhutani Nomogram, Maria falls into low intermediate risk zone of
hyperbilirubinemia (O'Reilly, Walsh, Allen, & Corcoran, 2015).
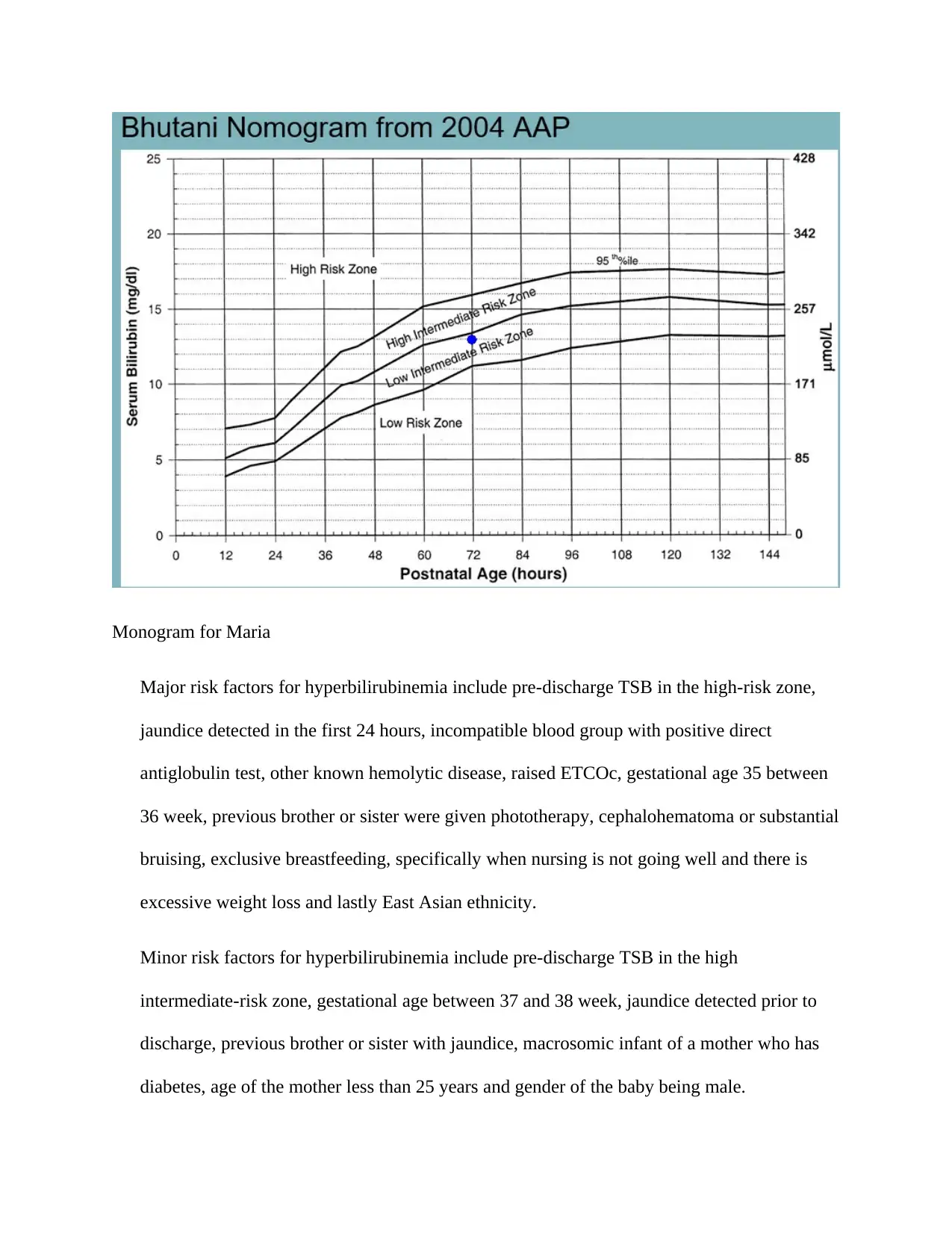
Monogram for Maria
Major risk factors for hyperbilirubinemia include pre-discharge TSB in the high-risk zone,
jaundice detected in the first 24 hours, incompatible blood group with positive direct
antiglobulin test, other known hemolytic disease, raised ETCOc, gestational age 35 between
36 week, previous brother or sister were given phototherapy, cephalohematoma or substantial
bruising, exclusive breastfeeding, specifically when nursing is not going well and there is
excessive weight loss and lastly East Asian ethnicity.
Minor risk factors for hyperbilirubinemia include pre-discharge TSB in the high
intermediate-risk zone, gestational age between 37 and 38 week, jaundice detected prior to
discharge, previous brother or sister with jaundice, macrosomic infant of a mother who has
diabetes, age of the mother less than 25 years and gender of the baby being male.
Major risk factors for hyperbilirubinemia include pre-discharge TSB in the high-risk zone,
jaundice detected in the first 24 hours, incompatible blood group with positive direct
antiglobulin test, other known hemolytic disease, raised ETCOc, gestational age 35 between
36 week, previous brother or sister were given phototherapy, cephalohematoma or substantial
bruising, exclusive breastfeeding, specifically when nursing is not going well and there is
excessive weight loss and lastly East Asian ethnicity.
Minor risk factors for hyperbilirubinemia include pre-discharge TSB in the high
intermediate-risk zone, gestational age between 37 and 38 week, jaundice detected prior to
discharge, previous brother or sister with jaundice, macrosomic infant of a mother who has
diabetes, age of the mother less than 25 years and gender of the baby being male.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4. It is suspected that Maria most likely has pathological unconjugated hyperbilirubinemia.
It is suspected as the mother indicated that Maria is lethargic and has been exhibiting
poor feeding. The peak total serum bilirubin is less than 15 mg/dL in the case of a full-
term, breastfed infant and for Maria it is 13 mg/dL. All these report findings and
observations indicate that Maria has pathological unconjugated hyperbilirubinemia.
5. The expected treatment plan for Maria will include phototherapy. Phototherapy is the key
treatment option in newborn who are diagnosed with unconjugated hyperbilirubinemia
(ULLAH, RAHMAN, & HEDAYATI, 2016). In phototherapy, Maria will be exposed to
blue light which has wavelength between 420 and 480 nm. It will convert unconjugated
bilirubin in skin which is hydrophobic in nature to a form which is water-soluble. Then
the water soluble form will get excreted in urine and/or bile. Phototherapy will be
performed until total bilirubin levels is less than 15 mg/dL. Adequate fluid will be
supplemented to Maria for prevention of dehydration. Furthermore, her eyes will be
protected against UV light. In case Maria does not respond to phototherapy adequately or
there is a rapid increase in TSB level, that is more than 6 mg/dL within 6 hours, exchange
transfusion will be done.
If Maria is left untreated, she may develop severe hyperbilirubinemia and will be at risk
of developing bilirubin-induced neurologic dysfunction (BIND) if the bilirubin crosses
the blood-brain barrier. The condition neurotoxicity which is manifested as acute
bilirubin encephalopathy (ABE) distinguished by reversible lethargy, hypotonia, and
reduced suck (Karadag, et al., 2013). And if ABE advances, kernicterus may occur which
It is suspected as the mother indicated that Maria is lethargic and has been exhibiting
poor feeding. The peak total serum bilirubin is less than 15 mg/dL in the case of a full-
term, breastfed infant and for Maria it is 13 mg/dL. All these report findings and
observations indicate that Maria has pathological unconjugated hyperbilirubinemia.
5. The expected treatment plan for Maria will include phototherapy. Phototherapy is the key
treatment option in newborn who are diagnosed with unconjugated hyperbilirubinemia
(ULLAH, RAHMAN, & HEDAYATI, 2016). In phototherapy, Maria will be exposed to
blue light which has wavelength between 420 and 480 nm. It will convert unconjugated
bilirubin in skin which is hydrophobic in nature to a form which is water-soluble. Then
the water soluble form will get excreted in urine and/or bile. Phototherapy will be
performed until total bilirubin levels is less than 15 mg/dL. Adequate fluid will be
supplemented to Maria for prevention of dehydration. Furthermore, her eyes will be
protected against UV light. In case Maria does not respond to phototherapy adequately or
there is a rapid increase in TSB level, that is more than 6 mg/dL within 6 hours, exchange
transfusion will be done.
If Maria is left untreated, she may develop severe hyperbilirubinemia and will be at risk
of developing bilirubin-induced neurologic dysfunction (BIND) if the bilirubin crosses
the blood-brain barrier. The condition neurotoxicity which is manifested as acute
bilirubin encephalopathy (ABE) distinguished by reversible lethargy, hypotonia, and
reduced suck (Karadag, et al., 2013). And if ABE advances, kernicterus may occur which
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
is a permanent condition. Kernicterus exhibits as cerebral palsy, seizures, arching,
posturing, and sensorineural hearing loss.
6. Plan for implementation based on family centered interventions and education
Nurse will make Maria’s parents aware about the types of jaundice, the type
which has affected Maria, pathophysiological factors and complications of
hyperbilirubinemia. It will improve their understanding of Maria’s condition,
correct any false impression and prevent the feelings of guilt and fear particularly
her in her mother.
Nurse will also have a discussion regarding possible long-term impacts
of hyperbilirubinemia and why is it essential to continue the assessment and
intervention.
Nurse will explain the home management of mild or moderate physiological
jaundice which will consist of more number of feedings, diffused sunlight
exposure, and follow-up serum testing program. Gaining parents’ understanding
is vital as it nurtures their cooperation post-discharge. In addition, the knowledge
given by nurse will help Maria’s parents to perform home management in a safe
and suitable manner and to appreciate the significance of every aspect of
management intervention.
Nurse will also give a demonstration of means of examining Maria for increasing
bilirubin levels by techniques of skin blanching with digital pressure to identify
the skin colour, weight supervision, or behavioral modification, especially if
infant is to be discharged early. It will help the parents in detecting the signs and
symptoms of elevated bilirubin levels.
posturing, and sensorineural hearing loss.
6. Plan for implementation based on family centered interventions and education
Nurse will make Maria’s parents aware about the types of jaundice, the type
which has affected Maria, pathophysiological factors and complications of
hyperbilirubinemia. It will improve their understanding of Maria’s condition,
correct any false impression and prevent the feelings of guilt and fear particularly
her in her mother.
Nurse will also have a discussion regarding possible long-term impacts
of hyperbilirubinemia and why is it essential to continue the assessment and
intervention.
Nurse will explain the home management of mild or moderate physiological
jaundice which will consist of more number of feedings, diffused sunlight
exposure, and follow-up serum testing program. Gaining parents’ understanding
is vital as it nurtures their cooperation post-discharge. In addition, the knowledge
given by nurse will help Maria’s parents to perform home management in a safe
and suitable manner and to appreciate the significance of every aspect of
management intervention.
Nurse will also give a demonstration of means of examining Maria for increasing
bilirubin levels by techniques of skin blanching with digital pressure to identify
the skin colour, weight supervision, or behavioral modification, especially if
infant is to be discharged early. It will help the parents in detecting the signs and
symptoms of elevated bilirubin levels.
While giving information to Maria’s parents about her daughter’s condition,
Nurse will encourage them to ask questions and gain clarity of Maria’s condition.
Nurse will give a 24-hr emergency telephone number and name of contact person
to Maria’s parents and emphasise on the significance of informing about
worsening of jaundice.
Nurse will also make an assessment of Maria’s family situation and support
systems.
Nurse will provide an easy to understand and comprehensive written explanation
of home phototherapy to Maria’s parents which will include explanation of
procedure, potential issues and safety precautions (Lynn & Linda, 2007).
7. Bowlby's attachment theory proposed that children are born with an inherent must form
attachments. These attachments will assist the child to survive by making sure that the
child will receive care and protection. In this theory, attachment is seen as a product of
evolutionary processes. Maria is born with an innate drive to form attachments with
caregivers. However, currently she is in pre-attachment stage which ranges between birth
and three months, infants do not show any particular attachment to a specific caregiver.
But in the next stage which is indiscriminate infant prefers her primary and secondary
caregivers. So if Maria’s hospitalization is extended then her primary and secondary
caregivers will become nurse and her other healthcare professional instead of what should
have been parents and other family member. In this phase, Maria will build a feeling of
trust that the caregiver will respond to her needs. It has been found that when children fail
to build secure attachments in early life can may show a negative effect on behavior in
Nurse will encourage them to ask questions and gain clarity of Maria’s condition.
Nurse will give a 24-hr emergency telephone number and name of contact person
to Maria’s parents and emphasise on the significance of informing about
worsening of jaundice.
Nurse will also make an assessment of Maria’s family situation and support
systems.
Nurse will provide an easy to understand and comprehensive written explanation
of home phototherapy to Maria’s parents which will include explanation of
procedure, potential issues and safety precautions (Lynn & Linda, 2007).
7. Bowlby's attachment theory proposed that children are born with an inherent must form
attachments. These attachments will assist the child to survive by making sure that the
child will receive care and protection. In this theory, attachment is seen as a product of
evolutionary processes. Maria is born with an innate drive to form attachments with
caregivers. However, currently she is in pre-attachment stage which ranges between birth
and three months, infants do not show any particular attachment to a specific caregiver.
But in the next stage which is indiscriminate infant prefers her primary and secondary
caregivers. So if Maria’s hospitalization is extended then her primary and secondary
caregivers will become nurse and her other healthcare professional instead of what should
have been parents and other family member. In this phase, Maria will build a feeling of
trust that the caregiver will respond to her needs. It has been found that when children fail
to build secure attachments in early life can may show a negative effect on behavior in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
later childhood or may be their whole life (Young, Simpson, Griskevicius, Huelsnitz, &
Fleck, 2019). Children who are diagnosed with certain psychological issues often exhibit
attachment issues.
8. Diagnosis- The diagnosis for Maria is advancing pathological unconjugated
hyperbilirubinemia.
Goal-The goal is to control the jaundice for progressing further and reversing the child
back to non-jaundice state.
Intervention- Intervention is assessment of Maria for signs of progression of
hyperbilirubinemia or behavioural changes. Nurse must be aware of the different stages
of CNS involvement which are neuro-depression, neuro hyperreflexia, lack of
manifestations and lastly cerebral palsy (Lauer & Spector, 2011).
Expected outcome- The expected outcome is by ensuring that Maria indicates indirect
bilirubin levels less than 12 mg/dl, resolve jaundice by completion of the 1st week of her
life and CNS does not get involved.
Plan of implementation and evaluation- If hyperbilirubinemia persists for more than two
weeks in Maria then the nurse will evaluate further. Further laboratory tests would be
warranted such as a fractionated bilirubin level, thyroid profiles, assessment for
metabolic or hemolytic ailments, and an examination to check for intestinal obstruction.
References
Fleck, 2019). Children who are diagnosed with certain psychological issues often exhibit
attachment issues.
8. Diagnosis- The diagnosis for Maria is advancing pathological unconjugated
hyperbilirubinemia.
Goal-The goal is to control the jaundice for progressing further and reversing the child
back to non-jaundice state.
Intervention- Intervention is assessment of Maria for signs of progression of
hyperbilirubinemia or behavioural changes. Nurse must be aware of the different stages
of CNS involvement which are neuro-depression, neuro hyperreflexia, lack of
manifestations and lastly cerebral palsy (Lauer & Spector, 2011).
Expected outcome- The expected outcome is by ensuring that Maria indicates indirect
bilirubin levels less than 12 mg/dl, resolve jaundice by completion of the 1st week of her
life and CNS does not get involved.
Plan of implementation and evaluation- If hyperbilirubinemia persists for more than two
weeks in Maria then the nurse will evaluate further. Further laboratory tests would be
warranted such as a fractionated bilirubin level, thyroid profiles, assessment for
metabolic or hemolytic ailments, and an examination to check for intestinal obstruction.
References
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Hillman, B., Tabrizi, M., Gauda, E., Carson, K., & Aucott, S. (2015). The Neonatal Pain,
Agitation and Sedation Scale and the bedside nurse’s assessment of neonates. J
Perinatol., 35(2), 128-31. doi:10.1038/jp.2014.154
Karadag, Zenciroglu, Eminoglu, Dilli, Karagol, Kundak, . . . Okumus. (2013). Literature review
and outcome of classic galactosemia diagnosed in the neonatal period. Clin. Lab, 59(9-
10), 1139-46.
Lauer, B. J., & Spector, N. D. (2011). Hyperbilirubinemia in the Newborn. Pediatrics in Review,
32(8).
Lynn, C., & Linda. (2007). Mosby's Pediatric Nursing Reference (6 ed.). Mosby.
O'Reilly, Walsh, Allen, & Corcoran. (2015). The Bhutani Nomogram Reduces Incidence of
Severe Hyperbilirubinaemia in Term and Near Term Infants. Ir Med J., 108(6), 181-2.
ULLAH, S., RAHMAN, K., & HEDAYATI, M. (2016). Hyperbilirubinemia in Neonates: Types,
Causes, Clinical Examinations, Preventive Measures and Treatments: A Narrative
Review Article. Iran J Public Health, 45(5), 558–568.
Young, E. S., Simpson, J. A., Griskevicius, V., Huelsnitz, C. O., & Fleck, C. (2019). Childhood
attachment and adult personality: A life history perspective. Self and Identity, 22-38.
doi:10.1080/15298868.2017.1353540
Agitation and Sedation Scale and the bedside nurse’s assessment of neonates. J
Perinatol., 35(2), 128-31. doi:10.1038/jp.2014.154
Karadag, Zenciroglu, Eminoglu, Dilli, Karagol, Kundak, . . . Okumus. (2013). Literature review
and outcome of classic galactosemia diagnosed in the neonatal period. Clin. Lab, 59(9-
10), 1139-46.
Lauer, B. J., & Spector, N. D. (2011). Hyperbilirubinemia in the Newborn. Pediatrics in Review,
32(8).
Lynn, C., & Linda. (2007). Mosby's Pediatric Nursing Reference (6 ed.). Mosby.
O'Reilly, Walsh, Allen, & Corcoran. (2015). The Bhutani Nomogram Reduces Incidence of
Severe Hyperbilirubinaemia in Term and Near Term Infants. Ir Med J., 108(6), 181-2.
ULLAH, S., RAHMAN, K., & HEDAYATI, M. (2016). Hyperbilirubinemia in Neonates: Types,
Causes, Clinical Examinations, Preventive Measures and Treatments: A Narrative
Review Article. Iran J Public Health, 45(5), 558–568.
Young, E. S., Simpson, J. A., Griskevicius, V., Huelsnitz, C. O., & Fleck, C. (2019). Childhood
attachment and adult personality: A life history perspective. Self and Identity, 22-38.
doi:10.1080/15298868.2017.1353540
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

