Comprehensive Case Study: Bipolar Disorder Patient Care and Planning
VerifiedAdded on 2020/03/04
|13
|2934
|186
Case Study
AI Summary
This case study presents a comprehensive analysis of a 42-year-old male patient experiencing a manic episode of bipolar disorder, leading to his admission to a mental health facility. It details a mental status examination, clinical formulation, and a nursing care plan addressing ineffective coping, risk of aggression, and violence. The study explores therapeutic relationships, cultural safety considerations, and recovery-oriented nursing interventions. It includes a clinical handover, and discusses the patient's psychosocial needs, potential barriers to well-being, and key mental health issues. The assignment emphasizes person-centered, holistic, and culturally appropriate care to enhance psychosocial outcomes, incorporating concepts of cultural safety and recovery-oriented approaches to patient care, as well as the importance of therapeutic communication and engagement to reduce the risk of self-inflicted injuries.
Part – 1 (Holistic Assessment and Planning)
Introduction
In the presented case study, the 42 years old male patient experienced bipolar disorder
manifested with the manic episode. The reason for patient’s admission in the medical facility
attributes to his psychological outbursts and aberrant behavior that eventually resulted in his
transfer to the mental health setting by the local police. Patient’s clinical history revealed the
elevated intensity of his psychosocial deterioration warranting the administration of person-
centered, holistic and culturally appropriate nursing care interventions for the systematic
enhancement of his psychosocial outcomes. The systematic analysis of this case study includes
the description of the mental status examination, clinical formulation table, nursing plan, clinical
handover, pattern of therapeutic relationship with the treated patient, cultural safety convention
and recovery-oriented nursing care interventions. The case analysis considered the conventions
of cultural safety that requires implementation for the enhancement of the mental health of the
admitted patient. The barriers to the establishment of mental well-being as well as the key-
mental issues of the patient are discussed in length in accordance with the standards of mental
health practice.
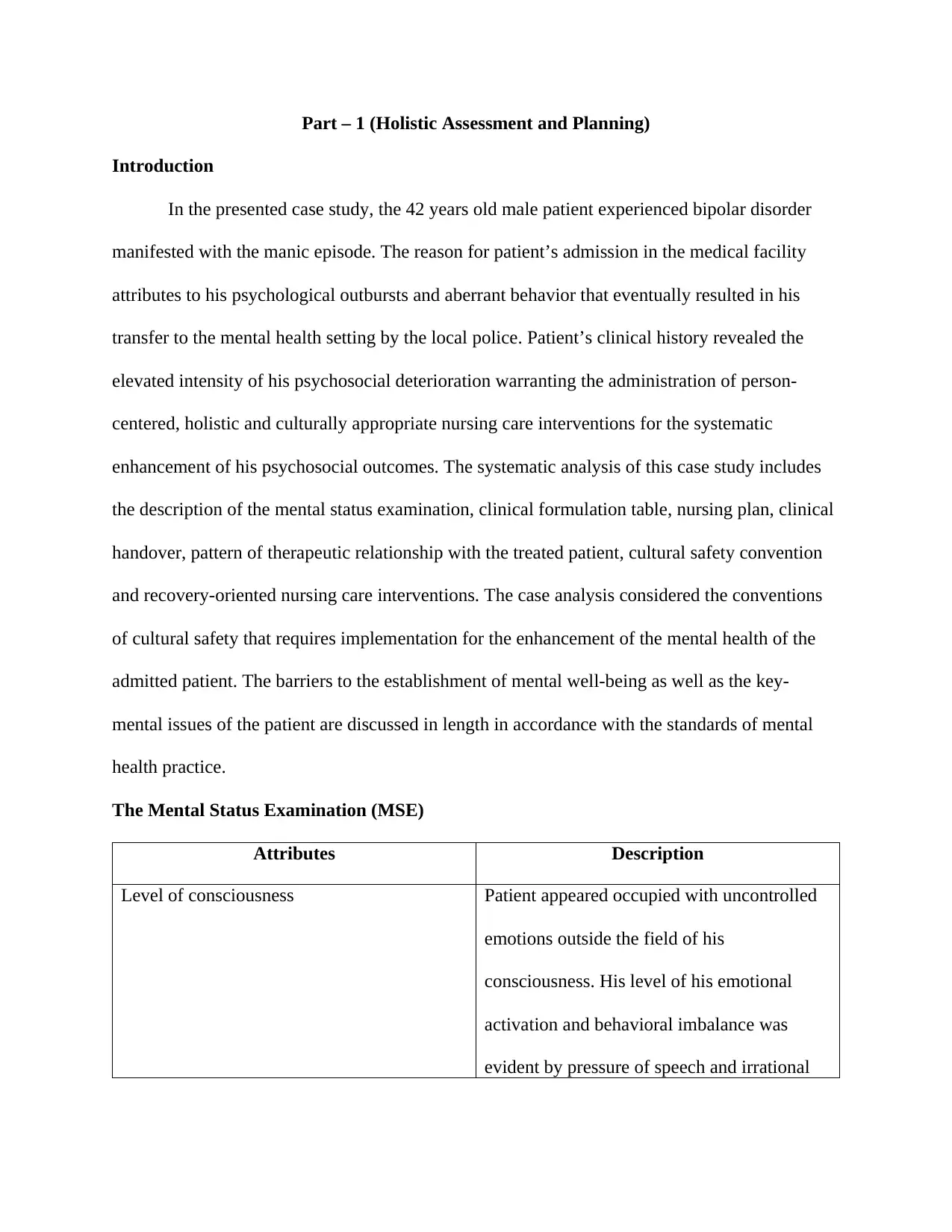
The Mental Status Examination (MSE)
Attributes Description
Level of consciousness Patient appeared occupied with uncontrolled
emotions outside the field of his
consciousness. His level of his emotional
activation and behavioral imbalance was
evident by pressure of speech and irrational
Introduction
In the presented case study, the 42 years old male patient experienced bipolar disorder
manifested with the manic episode. The reason for patient’s admission in the medical facility
attributes to his psychological outbursts and aberrant behavior that eventually resulted in his
transfer to the mental health setting by the local police. Patient’s clinical history revealed the
elevated intensity of his psychosocial deterioration warranting the administration of person-
centered, holistic and culturally appropriate nursing care interventions for the systematic
enhancement of his psychosocial outcomes. The systematic analysis of this case study includes
the description of the mental status examination, clinical formulation table, nursing plan, clinical
handover, pattern of therapeutic relationship with the treated patient, cultural safety convention
and recovery-oriented nursing care interventions. The case analysis considered the conventions
of cultural safety that requires implementation for the enhancement of the mental health of the
admitted patient. The barriers to the establishment of mental well-being as well as the key-
mental issues of the patient are discussed in length in accordance with the standards of mental
health practice.
The Mental Status Examination (MSE)
Attributes Description
Level of consciousness Patient appeared occupied with uncontrolled
emotions outside the field of his
consciousness. His level of his emotional
activation and behavioral imbalance was
evident by pressure of speech and irrational
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
thoughts (Lee, Kim, & Lee, 2016).
Appearance and general behavior Patient presented in shorts and a bright multi-
colored shirt. He appeared overwhelmed and
influenced with positive emotions.
Speech and motor activity Patient exhibited the pattern of abrupt
conversation and severe mood variability that
evidently indicated his motor hyperactivity
pattern (Krane-Gartiser, et al., 2016).
Affect and mood Patient appeared in a dysregulated mood as
well as euthymic state, reflected by his
functional disturbances (Kumar, Sinha, &
Mondal, 2016).
Thought and perception Patient exhibited the pattern of disturbed
thought process reflected by the unscrambling
of negative sentences that evidentially
indicated the existence of his negative
cognition (Miklowitz, Alatiq, Geddes,
Goodwin, & Williams, 2010).
Attitude and insight Patient’s stereotypical attitude was exhibited
the pattern of his aggressive, illogical and
dangerous behavior. Patient’s manic state was
indicative of his unmet personal needs (Hajda,
et al., 2016). Patient exhibited impaired
insight substantiated with the state of
Appearance and general behavior Patient presented in shorts and a bright multi-
colored shirt. He appeared overwhelmed and
influenced with positive emotions.
Speech and motor activity Patient exhibited the pattern of abrupt
conversation and severe mood variability that
evidently indicated his motor hyperactivity
pattern (Krane-Gartiser, et al., 2016).
Affect and mood Patient appeared in a dysregulated mood as
well as euthymic state, reflected by his
functional disturbances (Kumar, Sinha, &
Mondal, 2016).
Thought and perception Patient exhibited the pattern of disturbed
thought process reflected by the unscrambling
of negative sentences that evidentially
indicated the existence of his negative
cognition (Miklowitz, Alatiq, Geddes,
Goodwin, & Williams, 2010).
Attitude and insight Patient’s stereotypical attitude was exhibited
the pattern of his aggressive, illogical and
dangerous behavior. Patient’s manic state was
indicative of his unmet personal needs (Hajda,
et al., 2016). Patient exhibited impaired
insight substantiated with the state of
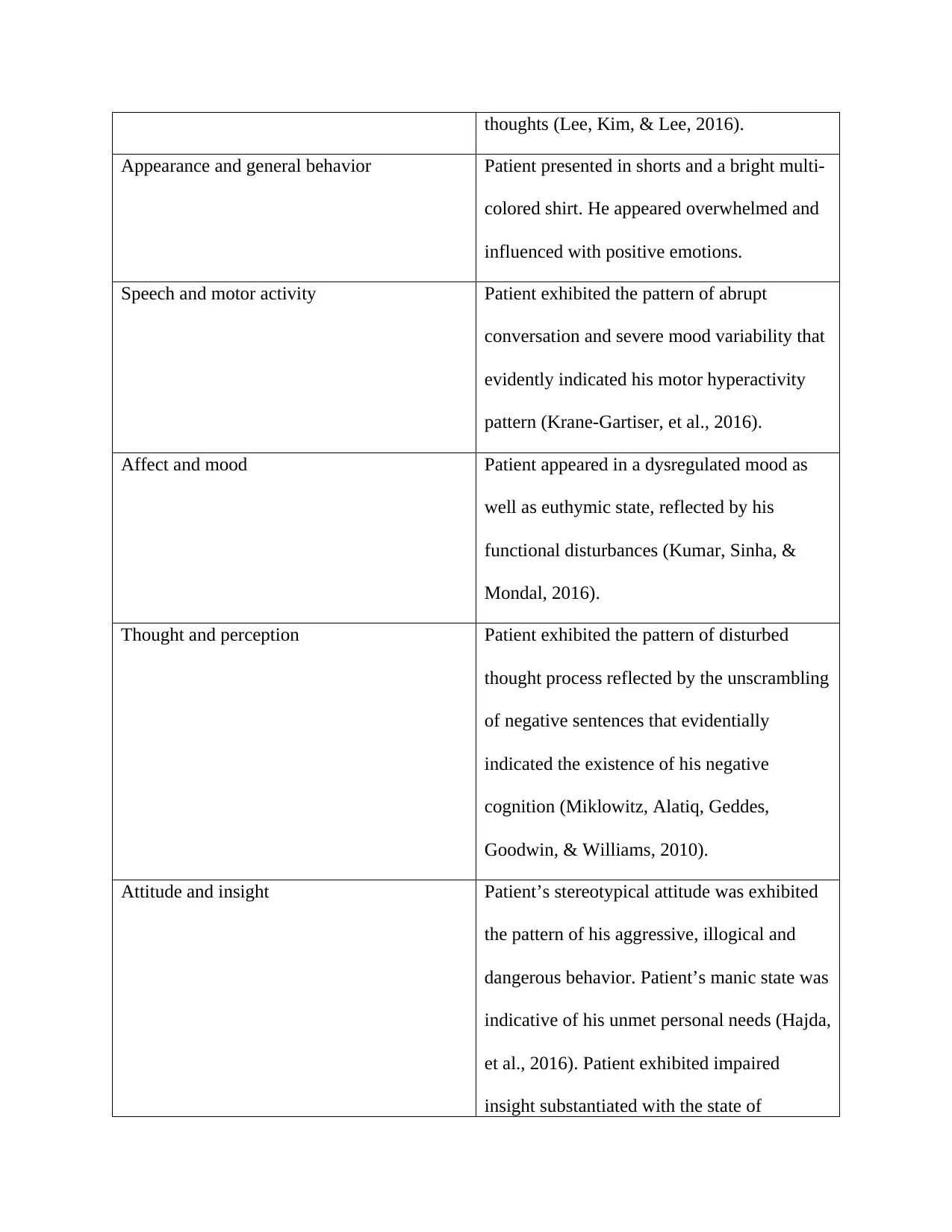
hypersexuality, humor, euphoria and
grandiosity (Cassidy, 2010).
Attention The patient appeared influenced by the
pattern of sustained attention interrupted by
euthymic periods, thereby indicating his
cognitive vulnerability (Ancín, et al., 2010).
Language Patient reportedly made personal and
offensive comments to the medical staff and
appeared violent and loud in speech.
Memory Patient reportedly exhibit the pattern of
memory loss during MSE
Constructional ability and praxis Normal
Abstract reasoning Normal
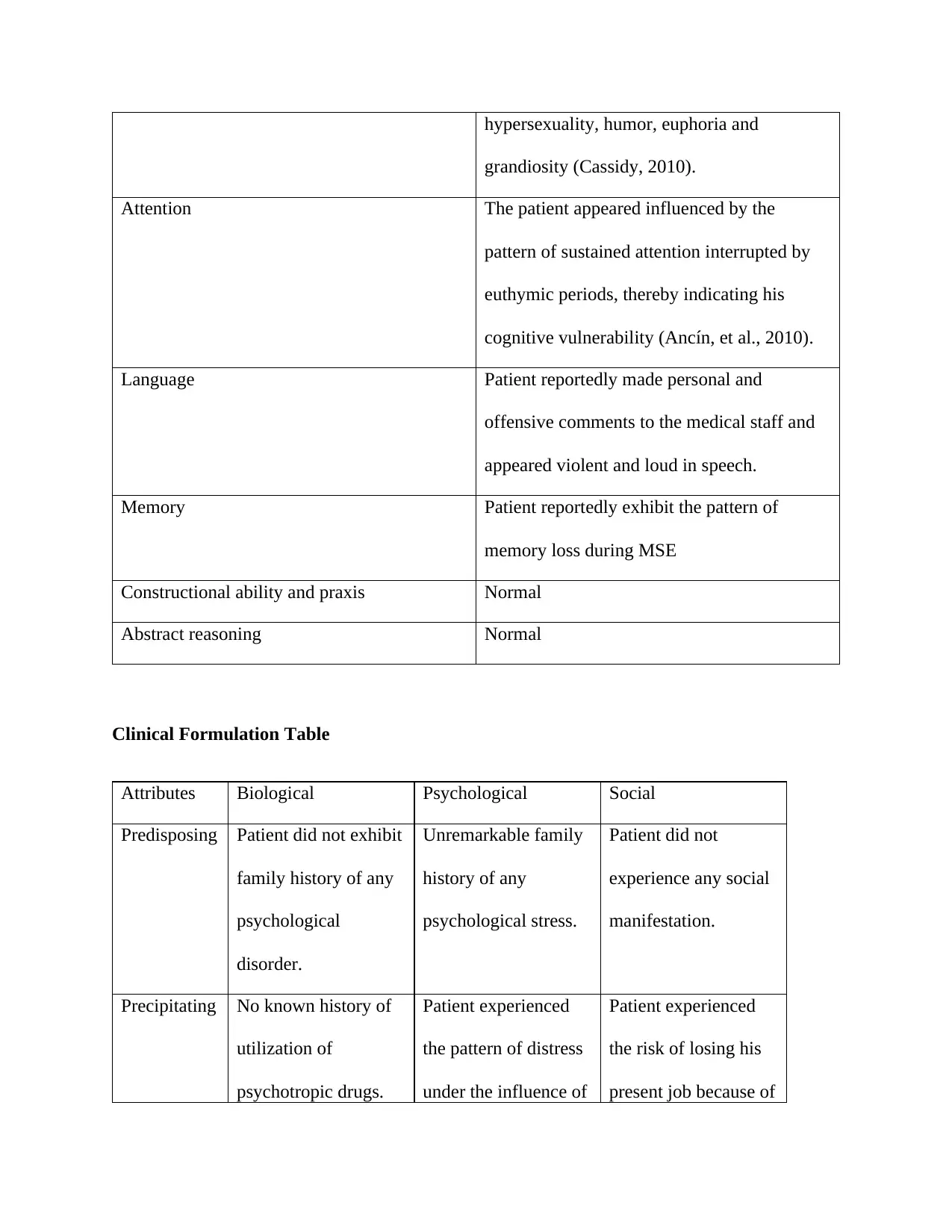
Clinical Formulation Table
Attributes Biological Psychological Social
Predisposing Patient did not exhibit
family history of any
psychological
disorder.
Unremarkable family
history of any
psychological stress.
Patient did not
experience any social
manifestation.
Precipitating No known history of
utilization of
psychotropic drugs.
Patient experienced
the pattern of distress
under the influence of
Patient experienced
the risk of losing his
present job because of
grandiosity (Cassidy, 2010).
Attention The patient appeared influenced by the
pattern of sustained attention interrupted by
euthymic periods, thereby indicating his
cognitive vulnerability (Ancín, et al., 2010).
Language Patient reportedly made personal and
offensive comments to the medical staff and
appeared violent and loud in speech.
Memory Patient reportedly exhibit the pattern of
memory loss during MSE
Constructional ability and praxis Normal
Abstract reasoning Normal
Clinical Formulation Table
Attributes Biological Psychological Social
Predisposing Patient did not exhibit
family history of any
psychological
disorder.
Unremarkable family
history of any
psychological stress.
Patient did not
experience any social
manifestation.
Precipitating No known history of
utilization of
psychotropic drugs.
Patient experienced
the pattern of distress
under the influence of
Patient experienced
the risk of losing his
present job because of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

However, the state of
patient’s sleeplessness
increased his
psychological stress
and disrupted the
sleep physiology. This
psychosomatic
disturbance appeared
to precipitate his
bipolar disorder.
psychosocial
circumstances. His
desire of gaining
sexual gains and false
claims apparently
exhibited the state of
his uncontrolled
emotions that proved
to be the precipitating
factors of his bipolar
manifestations.
recession and major
restructuring in his
company
Perpetuating No apparent
perpetuating factor
noticed during the
clinical investigation.
Inconsistent insight
and aberrant behavior.
The state of patient’s
euphoria and illusion
substantially
perpetuates his bipolar
manifestations.
Emotional and
physical distances
from the spouse. The
absence of a strong
family support system
appeared to be the
perpetuating factor of
patient’s bipolar
complications.
Protective No apparent
protective factor
recorded during the
Patient appears
educated with a well-
to-do social and
Stable pattern of the
social circle and
relationship with
patient’s sleeplessness
increased his
psychological stress
and disrupted the
sleep physiology. This
psychosomatic
disturbance appeared
to precipitate his
bipolar disorder.
psychosocial
circumstances. His
desire of gaining
sexual gains and false
claims apparently
exhibited the state of
his uncontrolled
emotions that proved
to be the precipitating
factors of his bipolar
manifestations.
recession and major
restructuring in his
company
Perpetuating No apparent
perpetuating factor
noticed during the
clinical investigation.
Inconsistent insight
and aberrant behavior.
The state of patient’s
euphoria and illusion
substantially
perpetuates his bipolar
manifestations.
Emotional and
physical distances
from the spouse. The
absence of a strong
family support system
appeared to be the
perpetuating factor of
patient’s bipolar
complications.
Protective No apparent
protective factor
recorded during the
Patient appears
educated with a well-
to-do social and
Stable pattern of the
social circle and
relationship with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
clinical investigation. professional
background.
spouse.
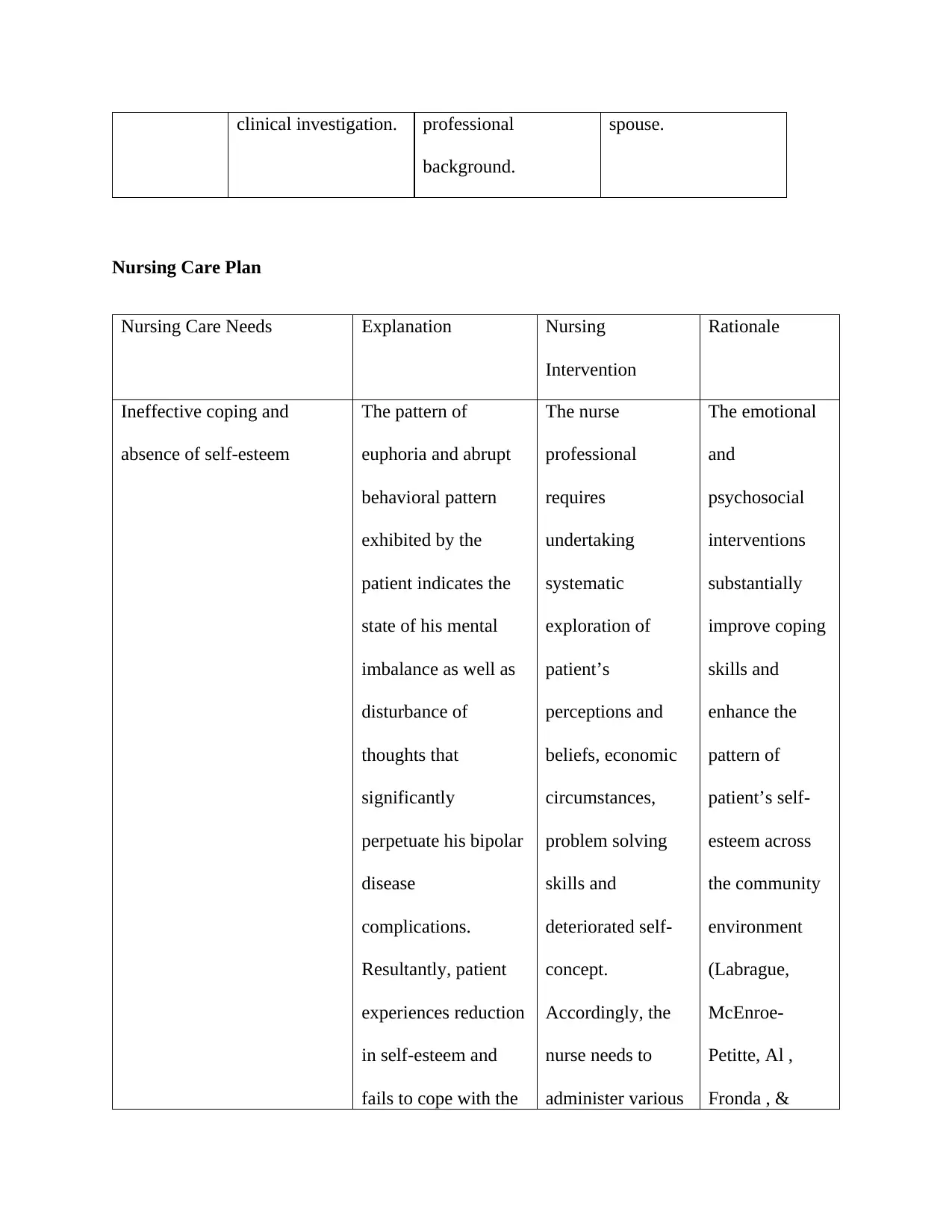
Nursing Care Plan
Nursing Care Needs Explanation Nursing
Intervention
Rationale
Ineffective coping and
absence of self-esteem
The pattern of
euphoria and abrupt
behavioral pattern
exhibited by the
patient indicates the
state of his mental
imbalance as well as
disturbance of
thoughts that
significantly
perpetuate his bipolar
disease
complications.
Resultantly, patient
experiences reduction
in self-esteem and
fails to cope with the
The nurse
professional
requires
undertaking
systematic
exploration of
patient’s
perceptions and
beliefs, economic
circumstances,
problem solving
skills and
deteriorated self-
concept.
Accordingly, the
nurse needs to
administer various
The emotional
and
psychosocial
interventions
substantially
improve coping
skills and
enhance the
pattern of
patient’s self-
esteem across
the community
environment
(Labrague,
McEnroe-
Petitte, Al ,
Fronda , &
background.
spouse.
Nursing Care Plan
Nursing Care Needs Explanation Nursing
Intervention
Rationale
Ineffective coping and
absence of self-esteem
The pattern of
euphoria and abrupt
behavioral pattern
exhibited by the
patient indicates the
state of his mental
imbalance as well as
disturbance of
thoughts that
significantly
perpetuate his bipolar
disease
complications.
Resultantly, patient
experiences reduction
in self-esteem and
fails to cope with the
The nurse
professional
requires
undertaking
systematic
exploration of
patient’s
perceptions and
beliefs, economic
circumstances,
problem solving
skills and
deteriorated self-
concept.
Accordingly, the
nurse needs to
administer various
The emotional
and
psychosocial
interventions
substantially
improve coping
skills and
enhance the
pattern of
patient’s self-
esteem across
the community
environment
(Labrague,
McEnroe-
Petitte, Al ,
Fronda , &

emotional
inconsistencies.
Resultantly, these
psychosocial deficits
require systematic
mitigation on highest
priority.
physical and
mental
interventions for
encouraging
patient’s
participation in
various social
activities like
exercise, outing
and excursion.
Obeidat, 2017).
Self-directed risk of
aggression, violence and
resultant injury
Patient’s manic state
substantiates the
pattern of his
irritation, mood
deterioration, anger
and frustration.
Resultantly, the
patient remains
occupied with the
offensive tendency of
attacking himself or
other people in his
immediate
The nurse
professional
requires
administering
cognitive
behavioral therapy
(CBT) for
controlling the
state of patient’s
self-directed
violence.
CBT proves to
be a highly
influential
technique
requiring
administration
for controlling
the pattern of
patient’s self-
directed
aggression and
the resultant
risk of trauma
inconsistencies.
Resultantly, these
psychosocial deficits
require systematic
mitigation on highest
priority.
physical and
mental
interventions for
encouraging
patient’s
participation in
various social
activities like
exercise, outing
and excursion.
Obeidat, 2017).
Self-directed risk of
aggression, violence and
resultant injury
Patient’s manic state
substantiates the
pattern of his
irritation, mood
deterioration, anger
and frustration.
Resultantly, the
patient remains
occupied with the
offensive tendency of
attacking himself or
other people in his
immediate
The nurse
professional
requires
administering
cognitive
behavioral therapy
(CBT) for
controlling the
state of patient’s
self-directed
violence.
CBT proves to
be a highly
influential
technique
requiring
administration
for controlling
the pattern of
patient’s self-
directed
aggression and
the resultant
risk of trauma
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
surroundings.
Therefore, this
psychological
condition requires
mitigation on highest
priority.
(Chen , et al.,
2014).
Clinical Handover
Luis is a 42 years old male who is a known case of bipolar disorder and admitted to the
mental health facility because of his manic episode. The patient experiences the state of mental
inconsistency substantiated by the pattern of his behavioural and emotional imbalances and
pressured speech pattern. The serious and abrupt mood variations of the patient are indicative of
his negative emotional pattern and facilitate the pattern of his aggressive and violent behaviour.
The patient appears euthymic and focuses too much on his self-perceived notions. His
deleterious thoughts evidentially elevate the risk of self-inflicted injuries. The patient lacks
effective coping skills warranted for dealing with his psychosocial circumstances and exhibits
diminished pattern of self-esteem. He does not exhibit any family history of psychological
disorder and remains socially connected with his friends and peers. The marital relationship of
the patient with his wife remains at risk because of his false apprehensions and abnormal
behavior. Patient needs to comply effectively on the prescribed medications and requires regular
nursing care for controlling his psychological symptoms.
Part – 2 (Therapeutic Engagement and Clinical Interpretation)
The Therapeutic Relationship
Therefore, this
psychological
condition requires
mitigation on highest
priority.
(Chen , et al.,
2014).
Clinical Handover
Luis is a 42 years old male who is a known case of bipolar disorder and admitted to the
mental health facility because of his manic episode. The patient experiences the state of mental
inconsistency substantiated by the pattern of his behavioural and emotional imbalances and
pressured speech pattern. The serious and abrupt mood variations of the patient are indicative of
his negative emotional pattern and facilitate the pattern of his aggressive and violent behaviour.
The patient appears euthymic and focuses too much on his self-perceived notions. His
deleterious thoughts evidentially elevate the risk of self-inflicted injuries. The patient lacks
effective coping skills warranted for dealing with his psychosocial circumstances and exhibits
diminished pattern of self-esteem. He does not exhibit any family history of psychological
disorder and remains socially connected with his friends and peers. The marital relationship of
the patient with his wife remains at risk because of his false apprehensions and abnormal
behavior. Patient needs to comply effectively on the prescribed medications and requires regular
nursing care for controlling his psychological symptoms.
Part – 2 (Therapeutic Engagement and Clinical Interpretation)
The Therapeutic Relationship
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The nurse professional requires establishing the pattern of a therapeutic alliance with the
treated patient in the context of improving the level of his trust, confidence and satisfaction on
the recommended psychotherapeutic interventions (Sylvia, et al., 2013). In the presented clinical
scenario, the nurse professional needs to identify the individual perceptions, culture, concerns,
beliefs, difficulties, treatment challenges and environmental constraints faced by the patient
while configuring a protective environment. Accordingly, nurse professionals need to dominate
the thought process of the patient with the utilization of motivational interventions in the context
of overcoming his psychosocial deficits and associated mental manifestations (Manetta, Gentile,
& Gillig, 2011). Registered nurse understanding the pattern of patient’s resistant behavior and
psychosocial conflicts through the utilization of a therapeutic relationship. The nurse
professional must administer a therapeutic dialogue with the treated patient in the context of
evaluating the causative factors of his behavioral disruptions and enhancing his compliance to
the recommended therapeutic interventions. The nurse professional requires understanding the
pattern of patient’s violent behavior and his individualized psychosocial requirements through
the systematic utilization of therapeutic communication. The assessment of patient’s dangerous
indicators, safety risks, social support system, opinions and strengths are highly required by the
nurse professional in the context of administering holistic healthcare interventions for reducing
the risk of self-inflicted injuries (Usta & Taleb, 2014). The nurse professional requires utilizing
therapeutic communication for the effective administration of cognitive behavioral intervention
to the treated patient (Ardito & Rabellino, 2011). The cognitive intervention with the
configuration of the therapeutic relationship assists the nurse professional in reducing the
orientation of the treated patient towards practicing violent approaches that substantially
decrease the risk of experiencing self-inflicted injuries.
treated patient in the context of improving the level of his trust, confidence and satisfaction on
the recommended psychotherapeutic interventions (Sylvia, et al., 2013). In the presented clinical
scenario, the nurse professional needs to identify the individual perceptions, culture, concerns,
beliefs, difficulties, treatment challenges and environmental constraints faced by the patient
while configuring a protective environment. Accordingly, nurse professionals need to dominate
the thought process of the patient with the utilization of motivational interventions in the context
of overcoming his psychosocial deficits and associated mental manifestations (Manetta, Gentile,
& Gillig, 2011). Registered nurse understanding the pattern of patient’s resistant behavior and
psychosocial conflicts through the utilization of a therapeutic relationship. The nurse
professional must administer a therapeutic dialogue with the treated patient in the context of
evaluating the causative factors of his behavioral disruptions and enhancing his compliance to
the recommended therapeutic interventions. The nurse professional requires understanding the
pattern of patient’s violent behavior and his individualized psychosocial requirements through
the systematic utilization of therapeutic communication. The assessment of patient’s dangerous
indicators, safety risks, social support system, opinions and strengths are highly required by the
nurse professional in the context of administering holistic healthcare interventions for reducing
the risk of self-inflicted injuries (Usta & Taleb, 2014). The nurse professional requires utilizing
therapeutic communication for the effective administration of cognitive behavioral intervention
to the treated patient (Ardito & Rabellino, 2011). The cognitive intervention with the
configuration of the therapeutic relationship assists the nurse professional in reducing the
orientation of the treated patient towards practicing violent approaches that substantially
decrease the risk of experiencing self-inflicted injuries.
Cultural Safety
Culturally safe nursing interventions require utilization with the objective of preserving
the beliefs and practices of the treated patients while effectively including them in the process of
their medical decision-making (Vogel, 2015). In the presented case scenario, the patient might
prove to be overenthusiastic in terms of disclosing personal matters in front of public.
Dysfunctional beliefs of the patient might also prove to be the greatest barrier in administering
goal oriented nursing care interventions in the mental healthcare setting (Geddes & Miklowitz,
2013). The nurse professional in the presented case scenario would require developing the
pattern of cultural connectedness with the treated patient. This cultural connectedness is
evidentially warranted for the systematic administration of culturally competent biopsychosocial
interventions in the context of acquiring the desirable treatment outcomes. In the presented case
scenario, the nurse professional needs to consider the cultural background of the treated patient
for customizing the nursing interventions in accordance with his individualized requirements and
self-care needs. Accordingly, the nurse professional would enhance the activities of daily living
of the treated patient while effectively increasing his trust and confidence on the recommended
psychosocial and therapeutic remediation. This will substantially influence patient’s thought
process and assist in reducing the intensity of his bipolar manifestations.
Recovery-Oriented Nursing Care
The recovery-oriented nursing care model effectively considers entire aspects of patient’s
healthcare with the objective of developing the pattern of self-sufficiency and self-efficacy in the
treated patient (Cleary, Lees, Molloy, Escott, & Sayers, 2017). The nurse professional requires
exploring the social support systems of the treated patient (in the presented case scenario) with
the objective of enhancing the power of patient’s medical decision-making. The registered nurse
Culturally safe nursing interventions require utilization with the objective of preserving
the beliefs and practices of the treated patients while effectively including them in the process of
their medical decision-making (Vogel, 2015). In the presented case scenario, the patient might
prove to be overenthusiastic in terms of disclosing personal matters in front of public.
Dysfunctional beliefs of the patient might also prove to be the greatest barrier in administering
goal oriented nursing care interventions in the mental healthcare setting (Geddes & Miklowitz,
2013). The nurse professional in the presented case scenario would require developing the
pattern of cultural connectedness with the treated patient. This cultural connectedness is
evidentially warranted for the systematic administration of culturally competent biopsychosocial
interventions in the context of acquiring the desirable treatment outcomes. In the presented case
scenario, the nurse professional needs to consider the cultural background of the treated patient
for customizing the nursing interventions in accordance with his individualized requirements and
self-care needs. Accordingly, the nurse professional would enhance the activities of daily living
of the treated patient while effectively increasing his trust and confidence on the recommended
psychosocial and therapeutic remediation. This will substantially influence patient’s thought
process and assist in reducing the intensity of his bipolar manifestations.
Recovery-Oriented Nursing Care
The recovery-oriented nursing care model effectively considers entire aspects of patient’s
healthcare with the objective of developing the pattern of self-sufficiency and self-efficacy in the
treated patient (Cleary, Lees, Molloy, Escott, & Sayers, 2017). The nurse professional requires
exploring the social support systems of the treated patient (in the presented case scenario) with
the objective of enhancing the power of patient’s medical decision-making. The registered nurse
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
needs to increase the confidence of the treated patient and develop the elements of self-
confidence, accountability and reliability with the systematic utilization of value-driven
behavioral strategies (AGDOH, 2017). The nurse professional requires undertaking the
systematic evaluation of the pattern of patient’s psychological strengths and weaknesses as well
as social engagement and familial controversies. The assessment of these attributes is necessarily
required for enhancing the pattern of patient’s positive belief and adding value and meaning in
his life to the desirable extent (AGDOH, 2017). The utilization of person-centered, holistic and
culturally appropriate nursing care interventions is necessarily required for enhancing the pattern
of patient’s individual autonomy for improving the pattern of his self-perception and associated
psychosocial outcomes. The development of a positive healing culture for the treated patient is
highly warranted for improving his speech and communication pattern, rights and attitudes and
respect and dignity in the context of effectively controlling his behavioral outcomes. The
systematic partnering of the treated patient, his friends and family members in the process of
medical decision making is necessarily required for providing him the best treatment choices in
the mental healthcare setting (AGDOH, 2017). The eventual empowerment of the treated patient
would assist him in making calculated healthcare choices for the systematic acquisition of the
goal oriented mental health outcomes. Accordingly, the patient would be able to control and
mitigate the perpetuating and precipitating factors of his bipolar disorder (AGDOH, 2017). The
pattern of courteous interactions with the treated patient would assist in the systematic evaluation
of the recovery process and enhance his quality of life and associated wellness-outcomes. The
periodic discussion regarding the social matters, family relationships, economic constraints and
behavioral constraints with the treated patient will eventually create a sense of recovery in the
confidence, accountability and reliability with the systematic utilization of value-driven
behavioral strategies (AGDOH, 2017). The nurse professional requires undertaking the
systematic evaluation of the pattern of patient’s psychological strengths and weaknesses as well
as social engagement and familial controversies. The assessment of these attributes is necessarily
required for enhancing the pattern of patient’s positive belief and adding value and meaning in
his life to the desirable extent (AGDOH, 2017). The utilization of person-centered, holistic and
culturally appropriate nursing care interventions is necessarily required for enhancing the pattern
of patient’s individual autonomy for improving the pattern of his self-perception and associated
psychosocial outcomes. The development of a positive healing culture for the treated patient is
highly warranted for improving his speech and communication pattern, rights and attitudes and
respect and dignity in the context of effectively controlling his behavioral outcomes. The
systematic partnering of the treated patient, his friends and family members in the process of
medical decision making is necessarily required for providing him the best treatment choices in
the mental healthcare setting (AGDOH, 2017). The eventual empowerment of the treated patient
would assist him in making calculated healthcare choices for the systematic acquisition of the
goal oriented mental health outcomes. Accordingly, the patient would be able to control and
mitigate the perpetuating and precipitating factors of his bipolar disorder (AGDOH, 2017). The
pattern of courteous interactions with the treated patient would assist in the systematic evaluation
of the recovery process and enhance his quality of life and associated wellness-outcomes. The
periodic discussion regarding the social matters, family relationships, economic constraints and
behavioral constraints with the treated patient will eventually create a sense of recovery in the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

treated patient (AGDOH, 2017). Resultantly, the patient will attempt to develop purpose and
focus in life while systematically mitigating the bipolar symptomatology.
Bibliography
AGDOH. (2017). Principles of recovery oriented mental health practice. Retrieved from
http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-n-
servst10-toc~mental-pubs-n-servst10-pri
Ancín , I., Santos , J. L., Teijeira , C., Sánchez-Morla , E. M., Bescós, M. J., Argudo , I., . . .
Cabranes-Díaz , J. A. (2010). Sustained attention as a potential endophenotype for bipolar
focus in life while systematically mitigating the bipolar symptomatology.
Bibliography
AGDOH. (2017). Principles of recovery oriented mental health practice. Retrieved from
http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-n-
servst10-toc~mental-pubs-n-servst10-pri
Ancín , I., Santos , J. L., Teijeira , C., Sánchez-Morla , E. M., Bescós, M. J., Argudo , I., . . .
Cabranes-Díaz , J. A. (2010). Sustained attention as a potential endophenotype for bipolar
disorder. Acta Psychiatrica Scandinavica, 235-245. doi:10.1111/j.1600-
0447.2009.01532.x
Ardito, R. B., & Rabellino, D. (2011). Therapeutic Alliance and Outcome of Psychotherapy:
Historical Excursus, Measurements, and Prospects for Research. Frontiers in Psychology.
doi:10.3389/fpsyg.2011.00270
Cassidy, F. (2010). Insight in bipolar disorder: relationship to episode subtypes and symptom
dimensions. Neuropsychiatric Disease and Treatment, 627-631.
doi:10.2147/NDT.S12663
Chen , C., Li, C., Wang, H., Ou, J. J., Zhou, J. S., & Wang , S. P. (2014). Cognitive behavioral
therapy to reduce overt aggression behavior in Chinese young male violent offenders.
Aggressive Behavior, 40(4), 329-336. doi:10.1002/ab.21521
Cleary, M., Lees, D., Molloy, L., Escott, P., & Sayers, J. (2017). Recovery-oriented Care and
Leadership in Mental Health Nursing. Issues in Mental Health Nursing. Retrieved from
http://www.tandfonline.com/doi/abs/10.1080/01612840.2017.1314738?
journalCode=imhn20
Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. Lancet, 381(9878).
doi:10.1016/S0140-6736(13)60857-0
Hajda, M., Prasko, J., Latalova, K., Hruby, R., Ociskova, M., Holubova, M., . . . Mainerova, B.
(2016). Unmet needs of bipolar disorder patients. Neuropsychiatric Disease and
Treatment, 1561-1570. doi:10.2147/NDT.S105728
0447.2009.01532.x
Ardito, R. B., & Rabellino, D. (2011). Therapeutic Alliance and Outcome of Psychotherapy:
Historical Excursus, Measurements, and Prospects for Research. Frontiers in Psychology.
doi:10.3389/fpsyg.2011.00270
Cassidy, F. (2010). Insight in bipolar disorder: relationship to episode subtypes and symptom
dimensions. Neuropsychiatric Disease and Treatment, 627-631.
doi:10.2147/NDT.S12663
Chen , C., Li, C., Wang, H., Ou, J. J., Zhou, J. S., & Wang , S. P. (2014). Cognitive behavioral
therapy to reduce overt aggression behavior in Chinese young male violent offenders.
Aggressive Behavior, 40(4), 329-336. doi:10.1002/ab.21521
Cleary, M., Lees, D., Molloy, L., Escott, P., & Sayers, J. (2017). Recovery-oriented Care and
Leadership in Mental Health Nursing. Issues in Mental Health Nursing. Retrieved from
http://www.tandfonline.com/doi/abs/10.1080/01612840.2017.1314738?
journalCode=imhn20
Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. Lancet, 381(9878).
doi:10.1016/S0140-6736(13)60857-0
Hajda, M., Prasko, J., Latalova, K., Hruby, R., Ociskova, M., Holubova, M., . . . Mainerova, B.
(2016). Unmet needs of bipolar disorder patients. Neuropsychiatric Disease and
Treatment, 1561-1570. doi:10.2147/NDT.S105728
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




