Nursing Case Study: Post-Operative Complications for THR Patients
VerifiedAdded on 2023/06/07
|13
|3737
|96
Report
AI Summary
This report presents a comprehensive nursing case study focusing on a 76-year-old patient, Mrs. Jean Bailey, who underwent a left total hip replacement (THR). It begins by identifying and explaining various risk factors associated with post-operative complications, such as bleeding, infections, blood clots, and joint stiffness. The report then discusses a potential post-operative complication for the patient, namely sepsis/septic shock, and its impact on various Activities of Daily Living (ADLs) including breathing, elimination, diet, and psychological needs. The aetiology of each complication is thoroughly discussed, supported by relevant literature. Furthermore, the report develops a detailed care plan addressing four potential complications, including appropriate nursing assessments, interventions, and rationales. The role of a physiotherapist in preventing complications and promoting recovery is analyzed, and the necessary education required for the patient before discharge is highlighted to support quick recovery. The report utilizes the Roper-Logan-Tierney model of nursing to structure the assessment of the patient's needs and the development of the care plan. The care plan includes detailed nursing interventions, assessments, and rationales to manage and prevent complications such as breathing problems, potential for deep vein thrombosis, bleeding, and psychological distress.

Running head: NURSING CASE STUDY 1
NURSING CASE STUDY
Student’s Name
Institutional Affiliation
Course
Date
NURSING CASE STUDY
Student’s Name
Institutional Affiliation
Course
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY 2
Introduction
Osteoarthritis is a very serious health condition that can lead to total hip replacement
surgery. Postoperatively, total hip replacement is associated with complications which
usually develops following various risk factors. This paper will identify and explain the risk
factors for postoperative complications for the client. The paper will identify and discuss one
possible post-operative complication for the client based on various Activities of Daily
Living (ADL’s) such as elimination, breathing, hygiene, diet and fluids, comfort and rest,
mobility, psychological and skin integrity and their aetiology. The paper will develop a care
plan addressing four potential complications with three appropriate nursing assessments,
nursing interventions and their rationale. Lastly, the paper will analyze the role of a
physiotherapist in the postoperative prevention of complications and prevention of
complications and highlight the appropriate education required for the client before discharge
to enhance and support quick recovery.
Risk factors for postoperative complications
Postoperatively, there is a wide of risk factors that can lead to complications
following total hip replacement in a patient. Some of these risk factors include; bleeding,
blood clots, infections, fractures, loosening, inflammation and swelling, hip stiffness,
hypersensitivity to the bone cement applied and damage to the surrounding tissues and
structures of the joint (Belmont et al, 2014, pp 597-604).
Postoperative hemorrhage is associated with the formation of blood clots. This is very
dangerous since a portion of the blood clot may break off and move to other body organs
such as the heart, lungs and sometimes to the brain. At the legs, the formation of clots leads
to the development of Deep Vein Thrombosis (DVT). Clot formation occurs due to
thickening of blood making it stick together. Formation of clots is important to prevent
excessive hemorrhage but it is very dangerous especially when it forms inside the blood
Introduction
Osteoarthritis is a very serious health condition that can lead to total hip replacement
surgery. Postoperatively, total hip replacement is associated with complications which
usually develops following various risk factors. This paper will identify and explain the risk
factors for postoperative complications for the client. The paper will identify and discuss one
possible post-operative complication for the client based on various Activities of Daily
Living (ADL’s) such as elimination, breathing, hygiene, diet and fluids, comfort and rest,
mobility, psychological and skin integrity and their aetiology. The paper will develop a care
plan addressing four potential complications with three appropriate nursing assessments,
nursing interventions and their rationale. Lastly, the paper will analyze the role of a
physiotherapist in the postoperative prevention of complications and prevention of
complications and highlight the appropriate education required for the client before discharge
to enhance and support quick recovery.
Risk factors for postoperative complications
Postoperatively, there is a wide of risk factors that can lead to complications
following total hip replacement in a patient. Some of these risk factors include; bleeding,
blood clots, infections, fractures, loosening, inflammation and swelling, hip stiffness,
hypersensitivity to the bone cement applied and damage to the surrounding tissues and
structures of the joint (Belmont et al, 2014, pp 597-604).
Postoperative hemorrhage is associated with the formation of blood clots. This is very
dangerous since a portion of the blood clot may break off and move to other body organs
such as the heart, lungs and sometimes to the brain. At the legs, the formation of clots leads
to the development of Deep Vein Thrombosis (DVT). Clot formation occurs due to
thickening of blood making it stick together. Formation of clots is important to prevent
excessive hemorrhage but it is very dangerous especially when it forms inside the blood
NURSING CASE STUDY 3
vessels. In the lungs, the presence of a blood clot can lead to pulmonary embolism which is
life-threatening because it causes obstruction and blockage of blood flow. After hip
replacement, prolonged stay in bed necessitates formation of blood clots because the flow of
blood in the deep veins is slowed down (Belmont et al, 2014, pp 597-604).
Another risk factor for postoperative complication in total hip replacement is
infections. Infections usually occur at the incision site and extends to the deeper tissues and
structures of the new hip (prosthesis). Infections may develop intraoperatively,
postoperatively or even after patient discharge. Mostly, postoperative infections are caused
by bacteria which might be present in gastrointestinal tract or the skin. Spread of the bacteria
into the bloodstream stimulates a rapid immune system response in an effort to kill them
(Courtney, Rozell, Melnic, & Lee, 2015, pp 1-4).
The immune response involves inflammatory process which involves production of
cytokines and mediators. Failure of the immune system to fight the bacterial pathogens may
lead to a serious complication such as sepsis which leads to multi-system dysfunctions. The
bacteria get into the body in various ways such as skin cuts or breaks and surgical wounds.
Some of the key indicators of infected joint replacement are; increased stiffness and pain,
swelling, redness and warmth around the joint, fatigue, wound drainage, fever, night sweats
and chills (Belmont et al, 2014, pp 597-604).
During surgery, fractures might occur on the healthy part of patient’s hip joint. These
fractures are usually small and may not be noticed by the physicians/surgeons hence leading
to a high risk of development of post-operative infections if they remain unmanaged or
untreated. Loosening of the hip joint as a result of failure to solidly fix the bone may lead to
pain at pain and other injuries hence predisposing the patient to hemorrhage and infections.
Other risk factors for post-operative complications is inflammation and swelling which
indicates healing response of the body to the surgery. Increased and rapid leg swelling and
vessels. In the lungs, the presence of a blood clot can lead to pulmonary embolism which is
life-threatening because it causes obstruction and blockage of blood flow. After hip
replacement, prolonged stay in bed necessitates formation of blood clots because the flow of
blood in the deep veins is slowed down (Belmont et al, 2014, pp 597-604).
Another risk factor for postoperative complication in total hip replacement is
infections. Infections usually occur at the incision site and extends to the deeper tissues and
structures of the new hip (prosthesis). Infections may develop intraoperatively,
postoperatively or even after patient discharge. Mostly, postoperative infections are caused
by bacteria which might be present in gastrointestinal tract or the skin. Spread of the bacteria
into the bloodstream stimulates a rapid immune system response in an effort to kill them
(Courtney, Rozell, Melnic, & Lee, 2015, pp 1-4).
The immune response involves inflammatory process which involves production of
cytokines and mediators. Failure of the immune system to fight the bacterial pathogens may
lead to a serious complication such as sepsis which leads to multi-system dysfunctions. The
bacteria get into the body in various ways such as skin cuts or breaks and surgical wounds.
Some of the key indicators of infected joint replacement are; increased stiffness and pain,
swelling, redness and warmth around the joint, fatigue, wound drainage, fever, night sweats
and chills (Belmont et al, 2014, pp 597-604).
During surgery, fractures might occur on the healthy part of patient’s hip joint. These
fractures are usually small and may not be noticed by the physicians/surgeons hence leading
to a high risk of development of post-operative infections if they remain unmanaged or
untreated. Loosening of the hip joint as a result of failure to solidly fix the bone may lead to
pain at pain and other injuries hence predisposing the patient to hemorrhage and infections.
Other risk factors for post-operative complications is inflammation and swelling which
indicates healing response of the body to the surgery. Increased and rapid leg swelling and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING CASE STUDY 4
calf tenderness are indications of blood clots in blood vessels and can lead to serious post-
operative complications (Courtney et al, 2015, pp 1-4).
Hip stiffness is associated with the development of scar tissues around the newly
replaced hip hence hindering flexibility leading to joint stiffness. Joint stiffness results in
decreased blood supply to the surrounding tissues of the new hip. Postoperatively, there
might be allergic reactions to the bone cement applied to ensure adherence of the hip
prostheses to the already existing hip bone. The hypersensitivity reactions may lead to
inflammation, swelling, fever and redness of the surrounding tissues resulting to infections
and complications such as sepsis and septic shock (Pugely, Martin, Gao, Schweizer, &
Callaghan, 2015, pp 47-55)
Additionally, damage to the tissues and structures around the joint during surgery may
lead to complications. Some of the soft tissues damaged may be ligaments, muscles and
tendons. The damage may sometimes extend to the surrounding nerves, veins and arteries
resulting to weakness and reduced sensitivity of the leg (Pugely et al, 2015, pp 47-50).
Potential postoperative complication
The potential post-operative complication for this patient could be sepsis/septic shock.
This complication impacts various Activities of Daily Living (ADLs) in the patient. These
ADLs include diet and fluids, breathing, elimination, comfort and rest, hygiene, skin
integrity, mobility and psychological needs. Sepsis is a very serious and life-threatening
medical condition which involves response of the body to its own organs and tissues
following infection injuries (Singer et al, 2016, pp 801-810).
Sepsis involves production and release of cytokines by the body’s immune system
during inflammatory responses following bacterial or viral invasion. The inflammatory
response in sepsis/septic shock results in increased permeability of capillaries, massive
vasodilation and reduced systemic vascular resistance hence leading to hypotension.
calf tenderness are indications of blood clots in blood vessels and can lead to serious post-
operative complications (Courtney et al, 2015, pp 1-4).
Hip stiffness is associated with the development of scar tissues around the newly
replaced hip hence hindering flexibility leading to joint stiffness. Joint stiffness results in
decreased blood supply to the surrounding tissues of the new hip. Postoperatively, there
might be allergic reactions to the bone cement applied to ensure adherence of the hip
prostheses to the already existing hip bone. The hypersensitivity reactions may lead to
inflammation, swelling, fever and redness of the surrounding tissues resulting to infections
and complications such as sepsis and septic shock (Pugely, Martin, Gao, Schweizer, &
Callaghan, 2015, pp 47-55)
Additionally, damage to the tissues and structures around the joint during surgery may
lead to complications. Some of the soft tissues damaged may be ligaments, muscles and
tendons. The damage may sometimes extend to the surrounding nerves, veins and arteries
resulting to weakness and reduced sensitivity of the leg (Pugely et al, 2015, pp 47-50).
Potential postoperative complication
The potential post-operative complication for this patient could be sepsis/septic shock.
This complication impacts various Activities of Daily Living (ADLs) in the patient. These
ADLs include diet and fluids, breathing, elimination, comfort and rest, hygiene, skin
integrity, mobility and psychological needs. Sepsis is a very serious and life-threatening
medical condition which involves response of the body to its own organs and tissues
following infection injuries (Singer et al, 2016, pp 801-810).
Sepsis involves production and release of cytokines by the body’s immune system
during inflammatory responses following bacterial or viral invasion. The inflammatory
response in sepsis/septic shock results in increased permeability of capillaries, massive
vasodilation and reduced systemic vascular resistance hence leading to hypotension.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY 5
Consequently, hypotension results to reduced perfusion of body tissues leading to tissue
hypoxia which causes septic shock. During the inflammatory process in sepsis in response to
infections, formation of microthrombi obstructs arterial vessels hence decreasing the blood
flow to body tissues (Cawcutt, & Peters, 2014, pp 1572-1578)
Decreased tissue perfusion and hypoxia (tissue ischemia) leads to multi-organ
dysfunction and failure. Some of the organs affected include; heart, brain, lung, kidneys and
liver. Decreased tissue perfusion leads to decreased supply of blood to the kidneys hence
causing oliguria due to kidney dysfunctions. Decreased gastrointestinal supply of oxygen and
blood leads to hypomotility which then leads to constipation, swallowing difficulties
(dysphagia) and reduced appetite resulting to impaired elimination patterns of the patient.
This also leads to difficulties in breathing, dyspnea and tachypnea as a compensatory
mechanism for reduced oxygen supply to the alveolar (De Backer, Orbegozo Cortes,
Donadello, & Vincent, 2014, pp 73-79).
It can be triggered by bacteria, fungi or viruses. Post-operative sepsis in hip
replacement is associated with various factors such as spread of bacteria from the skin or the
gastrointestinal tract to the surgical site and other body parts. The bacterial multiplies at the
site causing severe which consequently triggers body’s immune response leading to sepsis
(De Backer et al, 2014, pp 73-79).
Postoperatively, the body produces some fluids in response to the surgical operation.
The fluids collect in body parts like pelvic or abdominal cavities where important body
organs such as urinary bladder, stomach, kidneys, gut, chest and womb are located. In these
organs, the produced fluids provide a favorable environment for bacterial replication and
spread leading to development of sepsis. Inability of the patient to sufficiently move and take
sufficient breath may cause development of pneumonia hence impairing the breathing aspect
Consequently, hypotension results to reduced perfusion of body tissues leading to tissue
hypoxia which causes septic shock. During the inflammatory process in sepsis in response to
infections, formation of microthrombi obstructs arterial vessels hence decreasing the blood
flow to body tissues (Cawcutt, & Peters, 2014, pp 1572-1578)
Decreased tissue perfusion and hypoxia (tissue ischemia) leads to multi-organ
dysfunction and failure. Some of the organs affected include; heart, brain, lung, kidneys and
liver. Decreased tissue perfusion leads to decreased supply of blood to the kidneys hence
causing oliguria due to kidney dysfunctions. Decreased gastrointestinal supply of oxygen and
blood leads to hypomotility which then leads to constipation, swallowing difficulties
(dysphagia) and reduced appetite resulting to impaired elimination patterns of the patient.
This also leads to difficulties in breathing, dyspnea and tachypnea as a compensatory
mechanism for reduced oxygen supply to the alveolar (De Backer, Orbegozo Cortes,
Donadello, & Vincent, 2014, pp 73-79).
It can be triggered by bacteria, fungi or viruses. Post-operative sepsis in hip
replacement is associated with various factors such as spread of bacteria from the skin or the
gastrointestinal tract to the surgical site and other body parts. The bacterial multiplies at the
site causing severe which consequently triggers body’s immune response leading to sepsis
(De Backer et al, 2014, pp 73-79).
Postoperatively, the body produces some fluids in response to the surgical operation.
The fluids collect in body parts like pelvic or abdominal cavities where important body
organs such as urinary bladder, stomach, kidneys, gut, chest and womb are located. In these
organs, the produced fluids provide a favorable environment for bacterial replication and
spread leading to development of sepsis. Inability of the patient to sufficiently move and take
sufficient breath may cause development of pneumonia hence impairing the breathing aspect
NURSING CASE STUDY 6
of patient’s ADLs. Following the prolonged history of the patient’s condition (osteoarthritis),
her nutritional state has been tampered with (De Backer et al, 2014, pp 73-79).
Postoperatively, the patient might have reduced appetite due to sepsis leading to
impaired dietary and fluid intake and output. Impaired nutritional state results to poor and
delayed wound healing hence making it more vulnerable to bacterial infections. In major
operations such as hip replacement involves use of special drips, drainage tubes and
monitoring lines place into her body. Despite that they are inserted in a clean and sterile
environment, they break the skin and prolonged use increases the risk of development of
infections since they have broken the protective bacteria of the patient (Seymour, &
Rosengart, 2015, pp 708-717).
Hypoperfusion of brain in septic shock leads to alteration in patient’s mental status
resulting in depression, confusion and anxiety. This impairs the psychological functioning of
the patient. Septic shock presents with weakness and fatigue leading to reduced patient
mobility since she requires bed rest and relaxation. Prolonged bed-stay has a greater risk of
development of pressure sores following tissue ischemia. As a result of impaired mobility,
the patient’s hygiene is impaired because she is strong enough to maintain her own hygiene
(oral care, cleaning, washing). At this stage, she might need total nursing care and assistance
in performance of her daily Activities of Living (ADLs) (Hotchkiss et al, 2016, pp 16045).
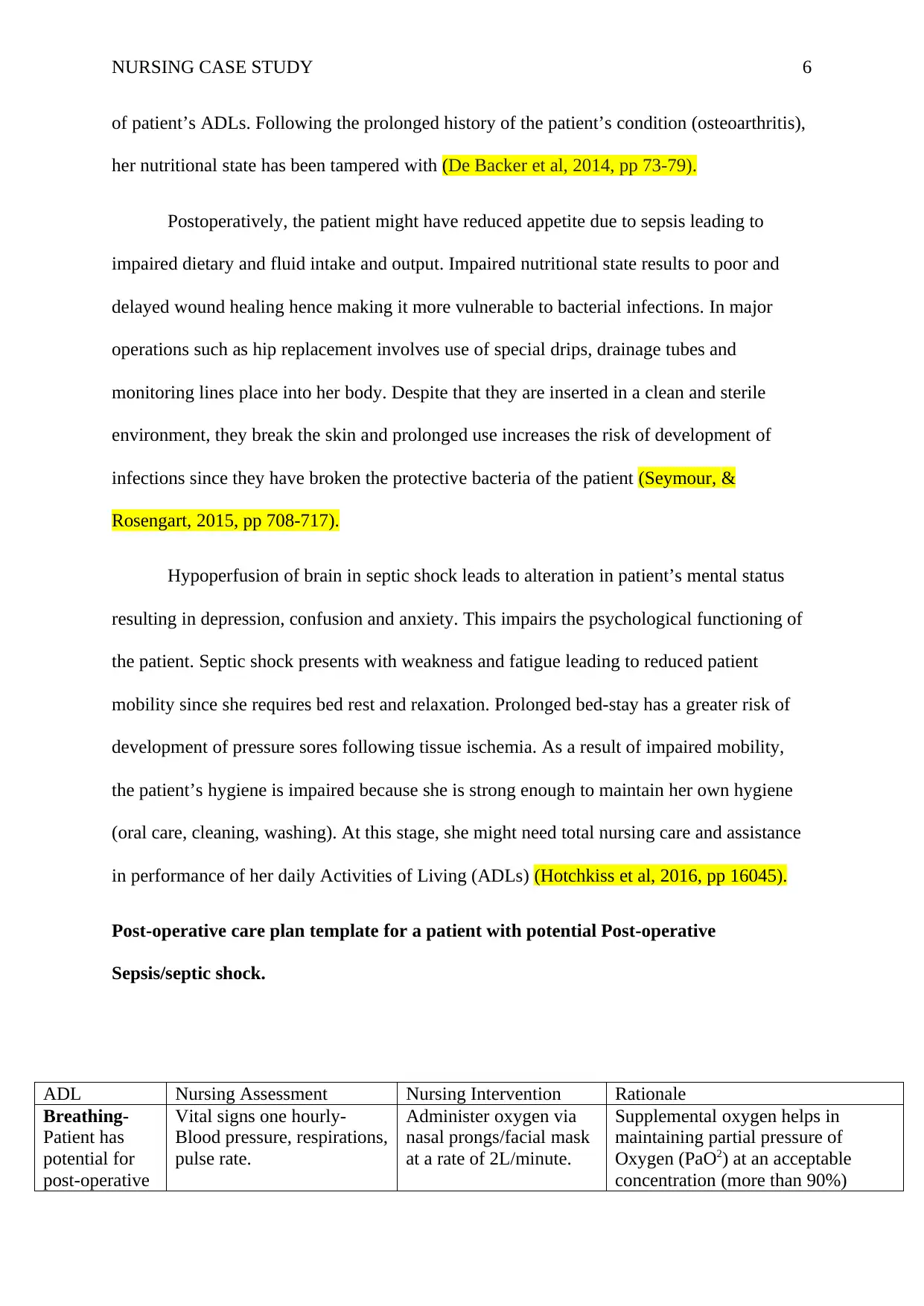
Post-operative care plan template for a patient with potential Post-operative
Sepsis/septic shock.
ADL Nursing Assessment Nursing Intervention Rationale
Breathing-
Patient has
potential for
post-operative
Vital signs one hourly-
Blood pressure, respirations,
pulse rate.
Administer oxygen via
nasal prongs/facial mask
at a rate of 2L/minute.
Supplemental oxygen helps in
maintaining partial pressure of
Oxygen (PaO2) at an acceptable
concentration (more than 90%)
of patient’s ADLs. Following the prolonged history of the patient’s condition (osteoarthritis),
her nutritional state has been tampered with (De Backer et al, 2014, pp 73-79).
Postoperatively, the patient might have reduced appetite due to sepsis leading to
impaired dietary and fluid intake and output. Impaired nutritional state results to poor and
delayed wound healing hence making it more vulnerable to bacterial infections. In major
operations such as hip replacement involves use of special drips, drainage tubes and
monitoring lines place into her body. Despite that they are inserted in a clean and sterile
environment, they break the skin and prolonged use increases the risk of development of
infections since they have broken the protective bacteria of the patient (Seymour, &
Rosengart, 2015, pp 708-717).
Hypoperfusion of brain in septic shock leads to alteration in patient’s mental status
resulting in depression, confusion and anxiety. This impairs the psychological functioning of
the patient. Septic shock presents with weakness and fatigue leading to reduced patient
mobility since she requires bed rest and relaxation. Prolonged bed-stay has a greater risk of
development of pressure sores following tissue ischemia. As a result of impaired mobility,
the patient’s hygiene is impaired because she is strong enough to maintain her own hygiene
(oral care, cleaning, washing). At this stage, she might need total nursing care and assistance
in performance of her daily Activities of Living (ADLs) (Hotchkiss et al, 2016, pp 16045).
Post-operative care plan template for a patient with potential Post-operative
Sepsis/septic shock.
ADL Nursing Assessment Nursing Intervention Rationale
Breathing-
Patient has
potential for
post-operative
Vital signs one hourly-
Blood pressure, respirations,
pulse rate.
Administer oxygen via
nasal prongs/facial mask
at a rate of 2L/minute.
Supplemental oxygen helps in
maintaining partial pressure of
Oxygen (PaO2) at an acceptable
concentration (more than 90%)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
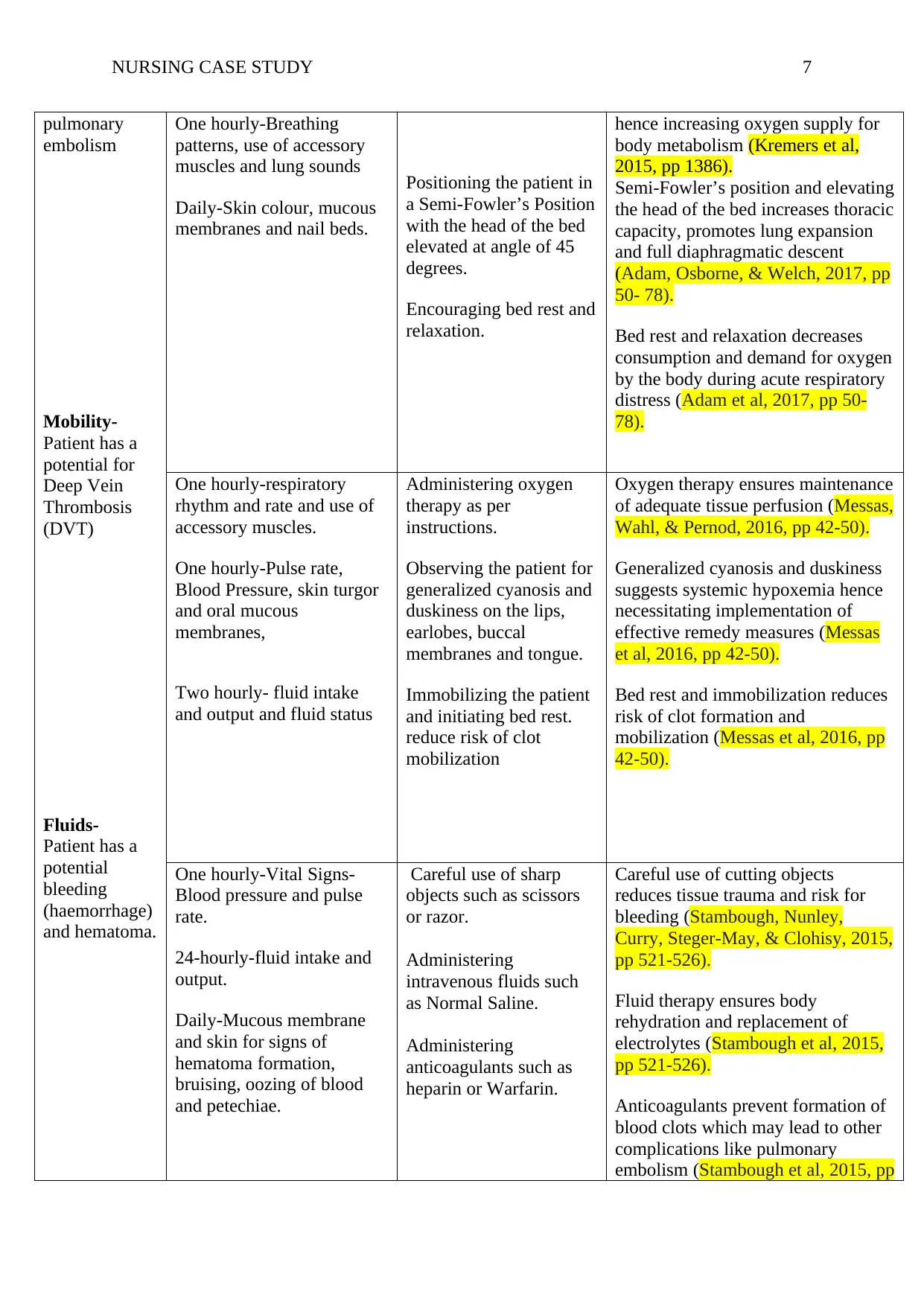
NURSING CASE STUDY 7
pulmonary
embolism
Mobility-
Patient has a
potential for
Deep Vein
Thrombosis
(DVT)
Fluids-
Patient has a
potential
bleeding
(haemorrhage)
and hematoma.
One hourly-Breathing
patterns, use of accessory
muscles and lung sounds
Daily-Skin colour, mucous
membranes and nail beds.
Positioning the patient in
a Semi-Fowler’s Position
with the head of the bed
elevated at angle of 45
degrees.
Encouraging bed rest and
relaxation.
hence increasing oxygen supply for
body metabolism (Kremers et al,
2015, pp 1386).
Semi-Fowler’s position and elevating
the head of the bed increases thoracic
capacity, promotes lung expansion
and full diaphragmatic descent
(Adam, Osborne, & Welch, 2017, pp
50- 78).
Bed rest and relaxation decreases
consumption and demand for oxygen
by the body during acute respiratory
distress (Adam et al, 2017, pp 50-
78).
One hourly-respiratory
rhythm and rate and use of
accessory muscles.
One hourly-Pulse rate,
Blood Pressure, skin turgor
and oral mucous
membranes,
Two hourly- fluid intake
and output and fluid status
Administering oxygen
therapy as per
instructions.
Observing the patient for
generalized cyanosis and
duskiness on the lips,
earlobes, buccal
membranes and tongue.
Immobilizing the patient
and initiating bed rest.
reduce risk of clot
mobilization
Oxygen therapy ensures maintenance
of adequate tissue perfusion (Messas,
Wahl, & Pernod, 2016, pp 42-50).
Generalized cyanosis and duskiness
suggests systemic hypoxemia hence
necessitating implementation of
effective remedy measures (Messas
et al, 2016, pp 42-50).
Bed rest and immobilization reduces
risk of clot formation and
mobilization (Messas et al, 2016, pp
42-50).
One hourly-Vital Signs-
Blood pressure and pulse
rate.
24-hourly-fluid intake and
output.
Daily-Mucous membrane
and skin for signs of
hematoma formation,
bruising, oozing of blood
and petechiae.
Careful use of sharp
objects such as scissors
or razor.
Administering
intravenous fluids such
as Normal Saline.
Administering
anticoagulants such as
heparin or Warfarin.
Careful use of cutting objects
reduces tissue trauma and risk for
bleeding (Stambough, Nunley,
Curry, Steger-May, & Clohisy, 2015,
pp 521-526).
Fluid therapy ensures body
rehydration and replacement of
electrolytes (Stambough et al, 2015,
pp 521-526).
Anticoagulants prevent formation of
blood clots which may lead to other
complications like pulmonary
embolism (Stambough et al, 2015, pp
pulmonary
embolism
Mobility-
Patient has a
potential for
Deep Vein
Thrombosis
(DVT)
Fluids-
Patient has a
potential
bleeding
(haemorrhage)
and hematoma.
One hourly-Breathing
patterns, use of accessory
muscles and lung sounds
Daily-Skin colour, mucous
membranes and nail beds.
Positioning the patient in
a Semi-Fowler’s Position
with the head of the bed
elevated at angle of 45
degrees.
Encouraging bed rest and
relaxation.
hence increasing oxygen supply for
body metabolism (Kremers et al,
2015, pp 1386).
Semi-Fowler’s position and elevating
the head of the bed increases thoracic
capacity, promotes lung expansion
and full diaphragmatic descent
(Adam, Osborne, & Welch, 2017, pp
50- 78).
Bed rest and relaxation decreases
consumption and demand for oxygen
by the body during acute respiratory
distress (Adam et al, 2017, pp 50-
78).
One hourly-respiratory
rhythm and rate and use of
accessory muscles.
One hourly-Pulse rate,
Blood Pressure, skin turgor
and oral mucous
membranes,
Two hourly- fluid intake
and output and fluid status
Administering oxygen
therapy as per
instructions.
Observing the patient for
generalized cyanosis and
duskiness on the lips,
earlobes, buccal
membranes and tongue.
Immobilizing the patient
and initiating bed rest.
reduce risk of clot
mobilization
Oxygen therapy ensures maintenance
of adequate tissue perfusion (Messas,
Wahl, & Pernod, 2016, pp 42-50).
Generalized cyanosis and duskiness
suggests systemic hypoxemia hence
necessitating implementation of
effective remedy measures (Messas
et al, 2016, pp 42-50).
Bed rest and immobilization reduces
risk of clot formation and
mobilization (Messas et al, 2016, pp
42-50).
One hourly-Vital Signs-
Blood pressure and pulse
rate.
24-hourly-fluid intake and
output.
Daily-Mucous membrane
and skin for signs of
hematoma formation,
bruising, oozing of blood
and petechiae.
Careful use of sharp
objects such as scissors
or razor.
Administering
intravenous fluids such
as Normal Saline.
Administering
anticoagulants such as
heparin or Warfarin.
Careful use of cutting objects
reduces tissue trauma and risk for
bleeding (Stambough, Nunley,
Curry, Steger-May, & Clohisy, 2015,
pp 521-526).
Fluid therapy ensures body
rehydration and replacement of
electrolytes (Stambough et al, 2015,
pp 521-526).
Anticoagulants prevent formation of
blood clots which may lead to other
complications like pulmonary
embolism (Stambough et al, 2015, pp
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
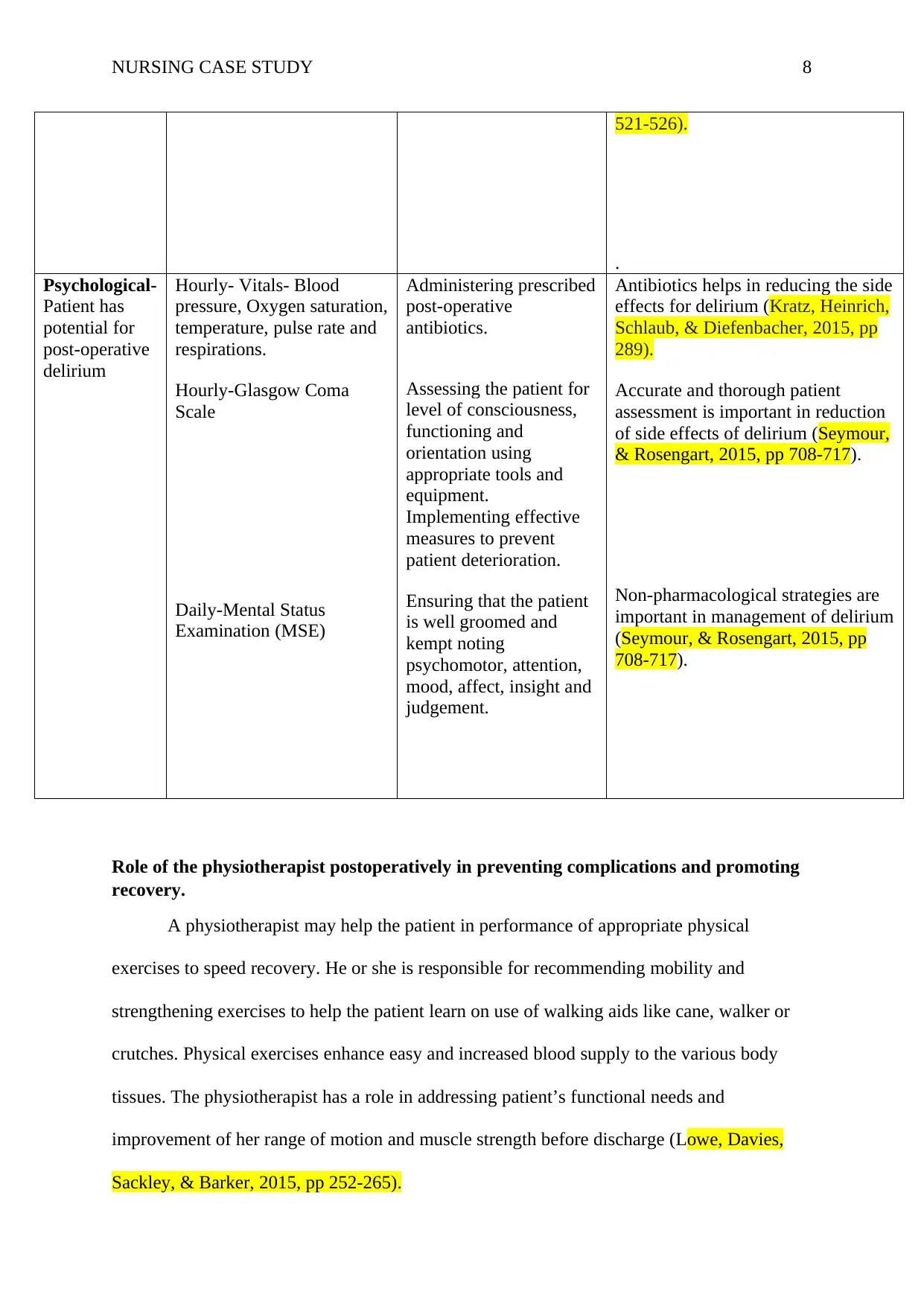
NURSING CASE STUDY 8
521-526).
.
Psychological-
Patient has
potential for
post-operative
delirium
Hourly- Vitals- Blood
pressure, Oxygen saturation,
temperature, pulse rate and
respirations.
Hourly-Glasgow Coma
Scale
Daily-Mental Status
Examination (MSE)
Administering prescribed
post-operative
antibiotics.
Assessing the patient for
level of consciousness,
functioning and
orientation using
appropriate tools and
equipment.
Implementing effective
measures to prevent
patient deterioration.
Ensuring that the patient
is well groomed and
kempt noting
psychomotor, attention,
mood, affect, insight and
judgement.
Antibiotics helps in reducing the side
effects for delirium (Kratz, Heinrich,
Schlaub, & Diefenbacher, 2015, pp
289).
Accurate and thorough patient
assessment is important in reduction
of side effects of delirium (Seymour,
& Rosengart, 2015, pp 708-717).
Non-pharmacological strategies are
important in management of delirium
(Seymour, & Rosengart, 2015, pp
708-717).
Role of the physiotherapist postoperatively in preventing complications and promoting
recovery.
A physiotherapist may help the patient in performance of appropriate physical
exercises to speed recovery. He or she is responsible for recommending mobility and
strengthening exercises to help the patient learn on use of walking aids like cane, walker or
crutches. Physical exercises enhance easy and increased blood supply to the various body
tissues. The physiotherapist has a role in addressing patient’s functional needs and
improvement of her range of motion and muscle strength before discharge (Lowe, Davies,
Sackley, & Barker, 2015, pp 252-265).
521-526).
.
Psychological-
Patient has
potential for
post-operative
delirium
Hourly- Vitals- Blood
pressure, Oxygen saturation,
temperature, pulse rate and
respirations.
Hourly-Glasgow Coma
Scale
Daily-Mental Status
Examination (MSE)
Administering prescribed
post-operative
antibiotics.
Assessing the patient for
level of consciousness,
functioning and
orientation using
appropriate tools and
equipment.
Implementing effective
measures to prevent
patient deterioration.
Ensuring that the patient
is well groomed and
kempt noting
psychomotor, attention,
mood, affect, insight and
judgement.
Antibiotics helps in reducing the side
effects for delirium (Kratz, Heinrich,
Schlaub, & Diefenbacher, 2015, pp
289).
Accurate and thorough patient
assessment is important in reduction
of side effects of delirium (Seymour,
& Rosengart, 2015, pp 708-717).
Non-pharmacological strategies are
important in management of delirium
(Seymour, & Rosengart, 2015, pp
708-717).
Role of the physiotherapist postoperatively in preventing complications and promoting
recovery.
A physiotherapist may help the patient in performance of appropriate physical
exercises to speed recovery. He or she is responsible for recommending mobility and
strengthening exercises to help the patient learn on use of walking aids like cane, walker or
crutches. Physical exercises enhance easy and increased blood supply to the various body
tissues. The physiotherapist has a role in addressing patient’s functional needs and
improvement of her range of motion and muscle strength before discharge (Lowe, Davies,
Sackley, & Barker, 2015, pp 252-265).
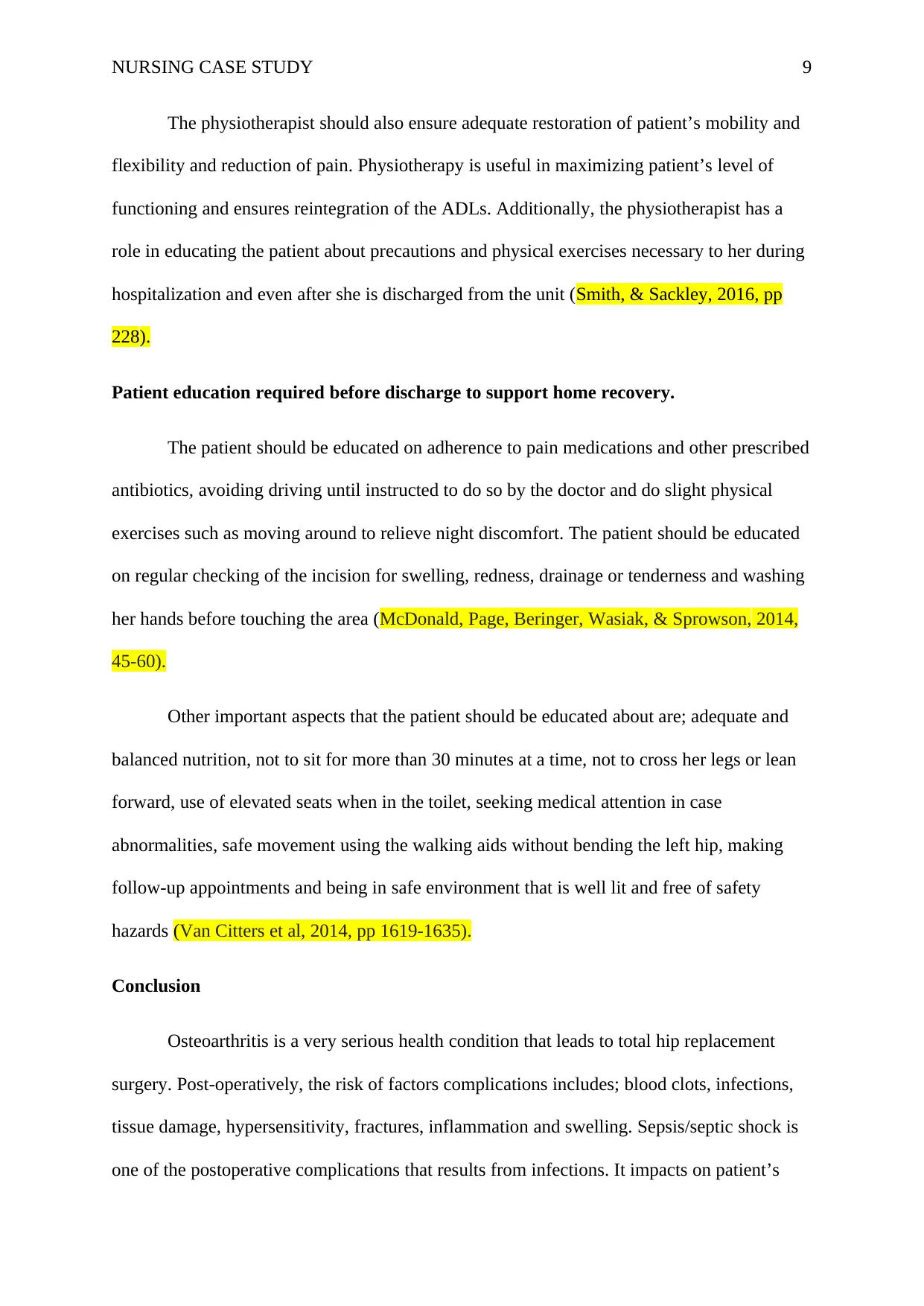
NURSING CASE STUDY 9
The physiotherapist should also ensure adequate restoration of patient’s mobility and
flexibility and reduction of pain. Physiotherapy is useful in maximizing patient’s level of
functioning and ensures reintegration of the ADLs. Additionally, the physiotherapist has a
role in educating the patient about precautions and physical exercises necessary to her during
hospitalization and even after she is discharged from the unit (Smith, & Sackley, 2016, pp
228).
Patient education required before discharge to support home recovery.
The patient should be educated on adherence to pain medications and other prescribed
antibiotics, avoiding driving until instructed to do so by the doctor and do slight physical
exercises such as moving around to relieve night discomfort. The patient should be educated
on regular checking of the incision for swelling, redness, drainage or tenderness and washing
her hands before touching the area (McDonald, Page, Beringer, Wasiak, & Sprowson, 2014,
45-60).
Other important aspects that the patient should be educated about are; adequate and
balanced nutrition, not to sit for more than 30 minutes at a time, not to cross her legs or lean
forward, use of elevated seats when in the toilet, seeking medical attention in case
abnormalities, safe movement using the walking aids without bending the left hip, making
follow-up appointments and being in safe environment that is well lit and free of safety
hazards (Van Citters et al, 2014, pp 1619-1635).
Conclusion
Osteoarthritis is a very serious health condition that leads to total hip replacement
surgery. Post-operatively, the risk of factors complications includes; blood clots, infections,
tissue damage, hypersensitivity, fractures, inflammation and swelling. Sepsis/septic shock is
one of the postoperative complications that results from infections. It impacts on patient’s
The physiotherapist should also ensure adequate restoration of patient’s mobility and
flexibility and reduction of pain. Physiotherapy is useful in maximizing patient’s level of
functioning and ensures reintegration of the ADLs. Additionally, the physiotherapist has a
role in educating the patient about precautions and physical exercises necessary to her during
hospitalization and even after she is discharged from the unit (Smith, & Sackley, 2016, pp
228).
Patient education required before discharge to support home recovery.
The patient should be educated on adherence to pain medications and other prescribed
antibiotics, avoiding driving until instructed to do so by the doctor and do slight physical
exercises such as moving around to relieve night discomfort. The patient should be educated
on regular checking of the incision for swelling, redness, drainage or tenderness and washing
her hands before touching the area (McDonald, Page, Beringer, Wasiak, & Sprowson, 2014,
45-60).
Other important aspects that the patient should be educated about are; adequate and
balanced nutrition, not to sit for more than 30 minutes at a time, not to cross her legs or lean
forward, use of elevated seats when in the toilet, seeking medical attention in case
abnormalities, safe movement using the walking aids without bending the left hip, making
follow-up appointments and being in safe environment that is well lit and free of safety
hazards (Van Citters et al, 2014, pp 1619-1635).
Conclusion
Osteoarthritis is a very serious health condition that leads to total hip replacement
surgery. Post-operatively, the risk of factors complications includes; blood clots, infections,
tissue damage, hypersensitivity, fractures, inflammation and swelling. Sepsis/septic shock is
one of the postoperative complications that results from infections. It impacts on patient’s
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING CASE STUDY 10
ADLs such as breathing, hygiene, diet and fluids, mobility, skin integrity, psychological
needs, comfort and rest and elimination. Following hip replacement surgery, a
physiotherapist plays an important role in prevention of complications and promotion of
patient recovery. Before discharge, it is important to enlighten and educate the patient on
effective management of the new prosthesis to ensure home recovery and prevent any
potential complications that may arise due to poor home management techniques.
References
ADLs such as breathing, hygiene, diet and fluids, mobility, skin integrity, psychological
needs, comfort and rest and elimination. Following hip replacement surgery, a
physiotherapist plays an important role in prevention of complications and promotion of
patient recovery. Before discharge, it is important to enlighten and educate the patient on
effective management of the new prosthesis to ensure home recovery and prevent any
potential complications that may arise due to poor home management techniques.
References
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING CASE STUDY 11
Adam, S., Osborne, S., & Welch, J. (Eds.). (2017). Critical care nursing: science and
practice. Oxford University Press., pp.50-78
Belmont, P. J., E’Stephan, J. G., Romano, D., Bader, J. O., Nelson, K. J., & Schoenfeld, A. J.
(2014). Risk factors for complications and in-hospital mortality following hip
fractures: a study using the National Trauma Data Bank. Archives of orthopaedic and
trauma surgery, 134(5), 597-604.
Cawcutt, K. A., & Peters, S. G. (2014, November). Severe sepsis and septic shock: clinical
overview and update on management. In Mayo Clinic Proceedings (Vol. 89, No. 11,
pp. 1572-1578). Elsevier.
Courtney, P. M., Rozell, J. C., Melnic, C. M., & Lee, G. C. (2015). Who should not undergo
short stay hip and knee arthroplasty? Risk factors associated with major medical
complications following primary total joint arthroplasty. The Journal of
arthroplasty, 30(9), 1-4.
De Backer, D., Orbegozo Cortes, D., Donadello, K., & Vincent, J. L. (2014).
Pathophysiology of microcirculatory dysfunction and the pathogenesis of septic
shock. Virulence, 5(1), 73-79.
Hotchkiss, R. S., Moldawer, L. L., Opal, S. M., Reinhart, K., Turnbull, I. R., & Vincent, J. L.
(2016). Sepsis and septic shock. Nature reviews Disease primers, 2, 16045.
Kratz, T., Heinrich, M., Schlaub, E., & Diefenbacher, A. (2015). Preventing postoperative
delirium: a prospective intervention with psychogeriatric liaison on surgical wards in
a general hospital. Deutsches Ärzteblatt International, 112(17), 289.
Adam, S., Osborne, S., & Welch, J. (Eds.). (2017). Critical care nursing: science and
practice. Oxford University Press., pp.50-78
Belmont, P. J., E’Stephan, J. G., Romano, D., Bader, J. O., Nelson, K. J., & Schoenfeld, A. J.
(2014). Risk factors for complications and in-hospital mortality following hip
fractures: a study using the National Trauma Data Bank. Archives of orthopaedic and
trauma surgery, 134(5), 597-604.
Cawcutt, K. A., & Peters, S. G. (2014, November). Severe sepsis and septic shock: clinical
overview and update on management. In Mayo Clinic Proceedings (Vol. 89, No. 11,
pp. 1572-1578). Elsevier.
Courtney, P. M., Rozell, J. C., Melnic, C. M., & Lee, G. C. (2015). Who should not undergo
short stay hip and knee arthroplasty? Risk factors associated with major medical
complications following primary total joint arthroplasty. The Journal of
arthroplasty, 30(9), 1-4.
De Backer, D., Orbegozo Cortes, D., Donadello, K., & Vincent, J. L. (2014).
Pathophysiology of microcirculatory dysfunction and the pathogenesis of septic
shock. Virulence, 5(1), 73-79.
Hotchkiss, R. S., Moldawer, L. L., Opal, S. M., Reinhart, K., Turnbull, I. R., & Vincent, J. L.
(2016). Sepsis and septic shock. Nature reviews Disease primers, 2, 16045.
Kratz, T., Heinrich, M., Schlaub, E., & Diefenbacher, A. (2015). Preventing postoperative
delirium: a prospective intervention with psychogeriatric liaison on surgical wards in
a general hospital. Deutsches Ärzteblatt International, 112(17), 289.
NURSING CASE STUDY 12
Lowe, C. J. M., Davies, L., Sackley, C. M., & Barker, K. L. (2015). Effectiveness of land-
based physiotherapy exercise following hospital discharge following hip arthroplasty
for osteoarthritis: an updated systematic review. Physiotherapy, 101(3), 252-265.
McDonald, S., Page, M. J., Beringer, K., Wasiak, J., & Sprowson, A. (2014). Preoperative
education for hip or knee replacement. Cochrane Database of Systematic Reviews,
(5), 45-60
Messas, E., Wahl, D., & Pernod, G. (2016). Management of deep-vein thrombosis: a 2015
update. Journal des maladies vasculaires, 41(1), 42-50.
Pugely, A. J., Martin, C. T., Gao, Y., Schweizer, M. L., & Callaghan, J. J. (2015). The
incidence of and risk factors for 30-day surgical site infections following primary and
revision total joint arthroplasty. The Journal of arthroplasty, 30(9), 47-50.
Seymour, C. W., & Rosengart, M. R. (2015). Septic shock: advances in diagnosis and
treatment. jama, 314(7), 708-717.
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., ...
& Hotchkiss, R. S. (2016). The third international consensus definitions for sepsis and
septic shock (Sepsis-3). Jama, 315(8), 801-810.
Smith, T. O., & Sackley, C. M. (2016). UK survey of occupational therapist’s and
physiotherapist’s experiences and attitudes towards hip replacement precautions and
equipment. BMC musculoskeletal disorders, 17(1), 228
Stambough, J. B., Nunley, R. M., Curry, M. C., Steger-May, K., & Clohisy, J. C. (2015).
Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of
stay without increasing readmissions. The Journal of arthroplasty, 30(4), 521-526.
Lowe, C. J. M., Davies, L., Sackley, C. M., & Barker, K. L. (2015). Effectiveness of land-
based physiotherapy exercise following hospital discharge following hip arthroplasty
for osteoarthritis: an updated systematic review. Physiotherapy, 101(3), 252-265.
McDonald, S., Page, M. J., Beringer, K., Wasiak, J., & Sprowson, A. (2014). Preoperative
education for hip or knee replacement. Cochrane Database of Systematic Reviews,
(5), 45-60
Messas, E., Wahl, D., & Pernod, G. (2016). Management of deep-vein thrombosis: a 2015
update. Journal des maladies vasculaires, 41(1), 42-50.
Pugely, A. J., Martin, C. T., Gao, Y., Schweizer, M. L., & Callaghan, J. J. (2015). The
incidence of and risk factors for 30-day surgical site infections following primary and
revision total joint arthroplasty. The Journal of arthroplasty, 30(9), 47-50.
Seymour, C. W., & Rosengart, M. R. (2015). Septic shock: advances in diagnosis and
treatment. jama, 314(7), 708-717.
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., ...
& Hotchkiss, R. S. (2016). The third international consensus definitions for sepsis and
septic shock (Sepsis-3). Jama, 315(8), 801-810.
Smith, T. O., & Sackley, C. M. (2016). UK survey of occupational therapist’s and
physiotherapist’s experiences and attitudes towards hip replacement precautions and
equipment. BMC musculoskeletal disorders, 17(1), 228
Stambough, J. B., Nunley, R. M., Curry, M. C., Steger-May, K., & Clohisy, J. C. (2015).
Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of
stay without increasing readmissions. The Journal of arthroplasty, 30(4), 521-526.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


