Case Study: Nursing Management of Cushing's Syndrome in Ms. Smith
VerifiedAdded on 2021/04/17
|11
|2732
|33
Case Study
AI Summary
This case study focuses on Ms. Maureen Smith, a 24-year-old female diagnosed with Cushing's syndrome. The assignment addresses the causes, pathophysiology, and risk factors associated with the disease, including the iatrogenic form due to rheumatoid arthritis medication. It explores the common signs and symptoms, such as fatigue, weight gain, moon face, diabetes, and hypertension, detailing their underlying mechanisms. The study also examines pharmacological interventions, including cortisol-lowering drugs like Ketoconazole and steroid inhibitors like Mifepristone, discussing their mechanisms of action and potential side effects. Furthermore, the assignment outlines priority nursing care strategies for the first 24 hours post-admission, emphasizing pain management, fluid volume regulation, injury prevention, infection control, and mental function improvement. The nursing care plan includes detailed rationales for each intervention, supported by relevant references.

Running head: NURSING
Nursing
Name of the Student
Name of the University
Author note
Nursing
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
CASE STUDY 2- MS MAUREEN SMITH
Answer to question- 1
Cushing syndrome is caused by the excess level of the hormone called Cortisol,
responsible for regulating blood pressure and cardiovascular function. Excess release of the
adrenocorticotropic hormone or ACTH by the pituitary gland due to tumor, is the other cause of
the disease. The ACTH hormone stimulates the adrenal glands to release more Cortisol. It is the
cause of the Cushing syndrome in 70% of the cases. Perforation in the descending colon leads to
the gastrointestinal discomfort. It is also the cause of gastric ulcer, due to the stimulation of vagal
nuclei. It is attributed to the increased intracranial pressure. It results in increased gastric
secretion via hydrogen potassium ATPase pathway. In case of the patient Ms Maureen Smith, the
Cushing syndrome may be due to the “iatrogenic” form as she is under medication for rheumatoid
arthritis (RA). This form is the side effect of the steroid hormone called glucocorticoids used in
treatment of RA and many other illnesses. Other causes of the disease are malnutrition (Lacroix et
al., 2015).
In Australia, the incidence of the disease is 1-2 cases per million populations. It is found ion
60% of the cases of hypercortisolism. The prevalence of the disease is 40 per million ( Steffensen
ET AL., 2010).
The risk factors associated with the Cushing syndrome are the type 2 diabetes, obesity,
poor regulation of blood glucose level, corticosteroid medications, and adrenal glands containing
benign nodular enlargements. Age and gender are the other risk factors. Cushing syndrome is
most common in females than males. It is commonly diagnosed in the age group of 25 to 40. Ms
Maureen Smith is a 24 year old female and is suffering from type 2 diabetes. Her BMI is 28kg/m2
CASE STUDY 2- MS MAUREEN SMITH
Answer to question- 1
Cushing syndrome is caused by the excess level of the hormone called Cortisol,
responsible for regulating blood pressure and cardiovascular function. Excess release of the
adrenocorticotropic hormone or ACTH by the pituitary gland due to tumor, is the other cause of
the disease. The ACTH hormone stimulates the adrenal glands to release more Cortisol. It is the
cause of the Cushing syndrome in 70% of the cases. Perforation in the descending colon leads to
the gastrointestinal discomfort. It is also the cause of gastric ulcer, due to the stimulation of vagal
nuclei. It is attributed to the increased intracranial pressure. It results in increased gastric
secretion via hydrogen potassium ATPase pathway. In case of the patient Ms Maureen Smith, the
Cushing syndrome may be due to the “iatrogenic” form as she is under medication for rheumatoid
arthritis (RA). This form is the side effect of the steroid hormone called glucocorticoids used in
treatment of RA and many other illnesses. Other causes of the disease are malnutrition (Lacroix et
al., 2015).
In Australia, the incidence of the disease is 1-2 cases per million populations. It is found ion
60% of the cases of hypercortisolism. The prevalence of the disease is 40 per million ( Steffensen
ET AL., 2010).
The risk factors associated with the Cushing syndrome are the type 2 diabetes, obesity,
poor regulation of blood glucose level, corticosteroid medications, and adrenal glands containing
benign nodular enlargements. Age and gender are the other risk factors. Cushing syndrome is
most common in females than males. It is commonly diagnosed in the age group of 25 to 40. Ms
Maureen Smith is a 24 year old female and is suffering from type 2 diabetes. Her BMI is 28kg/m2
2NURSING
indicating overweight and high BGL (14.0mmol/L). Ms. Smith works in Pizza restaurant and may
have been on high calorie and fat diet, which may have caused her vulnerable to the disease ( Raff &
Carroll, 2015).
The patient may experience social isolation due to the symptoms such as gastrointestinal
bleeding, muscle weakness and fatigue. It impacts the activities of daily living and occupation due to
lack of energy. The disease also alters the personality owing to the personality changes (moon face),
metabolic changes and impaired adjustment. It also alters the mood and may lead to depression and
anxiety as side effects and endocrine disorder. The overall quality of life is poor when the disease is
untreated. The illness may also affect the family members emotionally and financially. Lack of
awareness of medical jargons and diseases management strategies may add to stress (Siegel et al.,
2016).
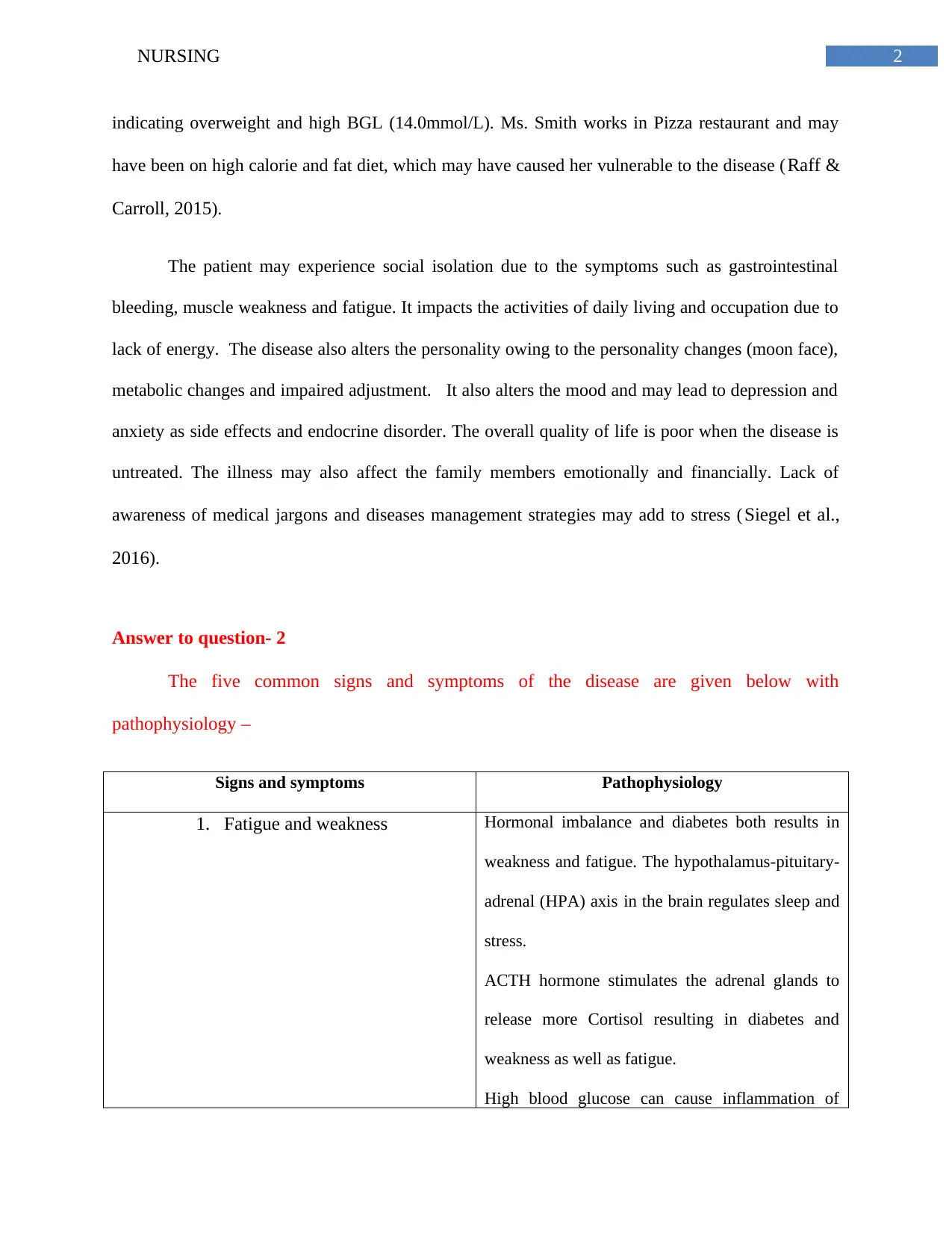
Answer to question- 2
The five common signs and symptoms of the disease are given below with
pathophysiology –
Signs and symptoms Pathophysiology
1. Fatigue and weakness Hormonal imbalance and diabetes both results in
weakness and fatigue. The hypothalamus-pituitary-
adrenal (HPA) axis in the brain regulates sleep and
stress.
ACTH hormone stimulates the adrenal glands to
release more Cortisol resulting in diabetes and
weakness as well as fatigue.
High blood glucose can cause inflammation of
indicating overweight and high BGL (14.0mmol/L). Ms. Smith works in Pizza restaurant and may
have been on high calorie and fat diet, which may have caused her vulnerable to the disease ( Raff &
Carroll, 2015).
The patient may experience social isolation due to the symptoms such as gastrointestinal
bleeding, muscle weakness and fatigue. It impacts the activities of daily living and occupation due to
lack of energy. The disease also alters the personality owing to the personality changes (moon face),
metabolic changes and impaired adjustment. It also alters the mood and may lead to depression and
anxiety as side effects and endocrine disorder. The overall quality of life is poor when the disease is
untreated. The illness may also affect the family members emotionally and financially. Lack of
awareness of medical jargons and diseases management strategies may add to stress (Siegel et al.,
2016).
Answer to question- 2
The five common signs and symptoms of the disease are given below with
pathophysiology –
Signs and symptoms Pathophysiology
1. Fatigue and weakness Hormonal imbalance and diabetes both results in
weakness and fatigue. The hypothalamus-pituitary-
adrenal (HPA) axis in the brain regulates sleep and
stress.
ACTH hormone stimulates the adrenal glands to
release more Cortisol resulting in diabetes and
weakness as well as fatigue.
High blood glucose can cause inflammation of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
blood vessels and increase monocytes
concentration in brain, causing fatigue.
It is also the side effects of medication for chronic
illness such as rheumatoid arthritis (Lacroix et al.,
2015)
2. Weight gain Increased Cortisol increases weight by fat
accumulation in various body parts, by stimulating
the fat metabolism during stress.
It increases blood sugar and insulin resistance
leading to high appetitite.
Excess glucose is converted to fat resulting in
weight (Bizarro et al., 2015). Medicines like
prednisone for rheumatoid arthritis also causes
weight gain as side effect.
3. Moon face and hump- Round shape of the face due to specific pattern of
fat distribution such as on sides of face.
Fat deposition such as on shoulders may appear as
hump.
It is attributed to increase fat metabolism
stimulated by cortisol and obesity (Nieman, 2015).
Prednisone also causes increase in fat distribution
and swelling in face and neck.
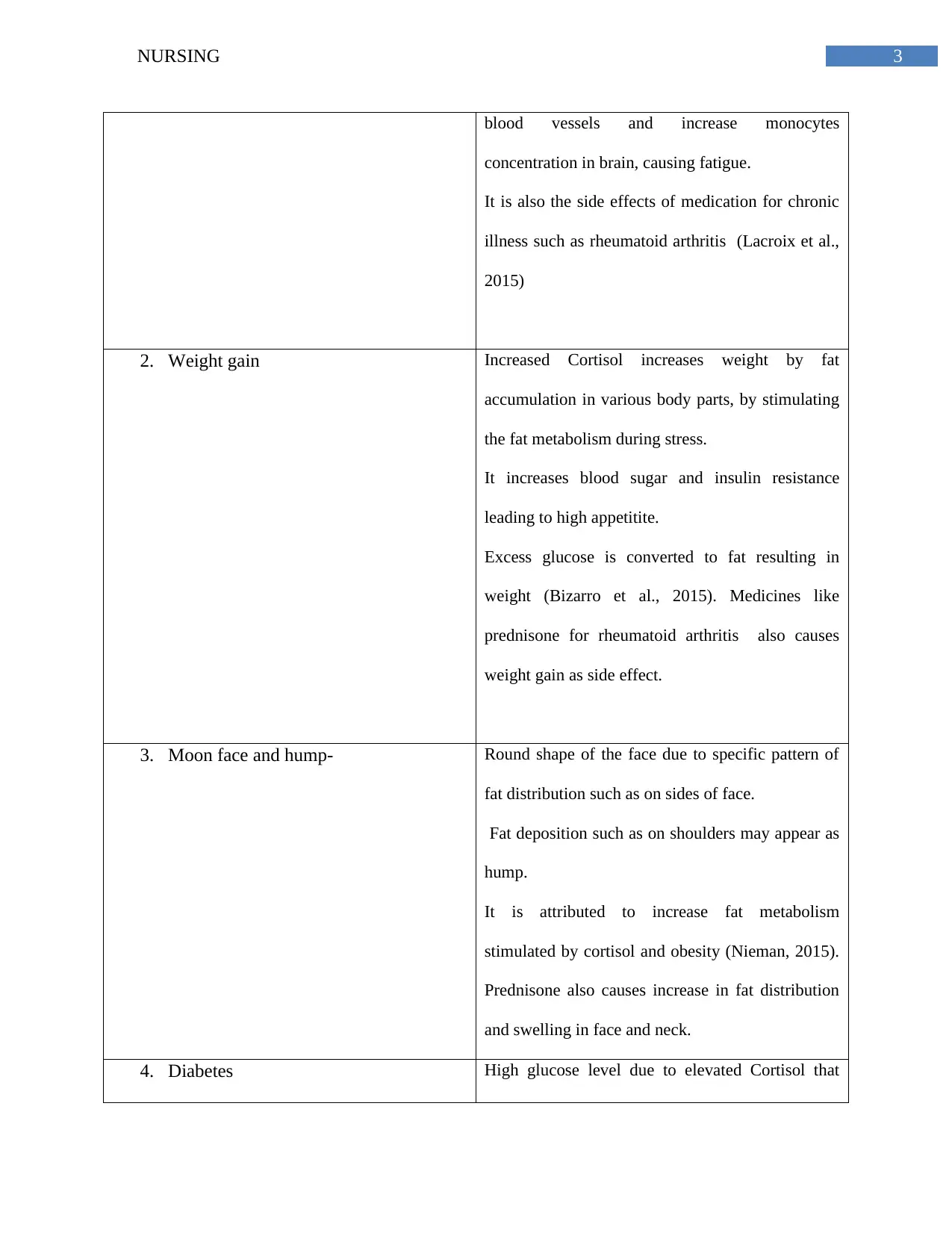
4. Diabetes High glucose level due to elevated Cortisol that
blood vessels and increase monocytes
concentration in brain, causing fatigue.
It is also the side effects of medication for chronic
illness such as rheumatoid arthritis (Lacroix et al.,
2015)
2. Weight gain Increased Cortisol increases weight by fat
accumulation in various body parts, by stimulating
the fat metabolism during stress.
It increases blood sugar and insulin resistance
leading to high appetitite.
Excess glucose is converted to fat resulting in
weight (Bizarro et al., 2015). Medicines like
prednisone for rheumatoid arthritis also causes
weight gain as side effect.
3. Moon face and hump- Round shape of the face due to specific pattern of
fat distribution such as on sides of face.
Fat deposition such as on shoulders may appear as
hump.
It is attributed to increase fat metabolism
stimulated by cortisol and obesity (Nieman, 2015).
Prednisone also causes increase in fat distribution
and swelling in face and neck.
4. Diabetes High glucose level due to elevated Cortisol that
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
impairs the glucose metabolism.
Excess glucocorticoid stimulates gluconeogenesis
in the liver,inhibist insulin sensitivity, and increases
glucose production.
Consequently the insulin sensitivity is impaired and
manifested as diabetes (Karaman et al., 2017)
5. High blood pressure Increased Cortisol leads to mineralocorticoid
activity in high concentration.
It worsens the hypertension as excess
glucocorticoids results in high plasma volume,
peripheral vascular resistance and cardiac output.
Glucocorticoids also exert hypertensive effects on
cardiovascular regulation.
This happens through central nervous system via
mineralocorticoid receptors and glucocorticoid
receptors. Glucocorticoids increases cardiac output.
It also elevates renovascular resistance and
peripheral resistance and ultimately results in
hypertension (Pivonello et al., 2016).
impairs the glucose metabolism.
Excess glucocorticoid stimulates gluconeogenesis
in the liver,inhibist insulin sensitivity, and increases
glucose production.
Consequently the insulin sensitivity is impaired and
manifested as diabetes (Karaman et al., 2017)
5. High blood pressure Increased Cortisol leads to mineralocorticoid
activity in high concentration.
It worsens the hypertension as excess
glucocorticoids results in high plasma volume,
peripheral vascular resistance and cardiac output.
Glucocorticoids also exert hypertensive effects on
cardiovascular regulation.
This happens through central nervous system via
mineralocorticoid receptors and glucocorticoid
receptors. Glucocorticoids increases cardiac output.
It also elevates renovascular resistance and
peripheral resistance and ultimately results in
hypertension (Pivonello et al., 2016).
5NURSING
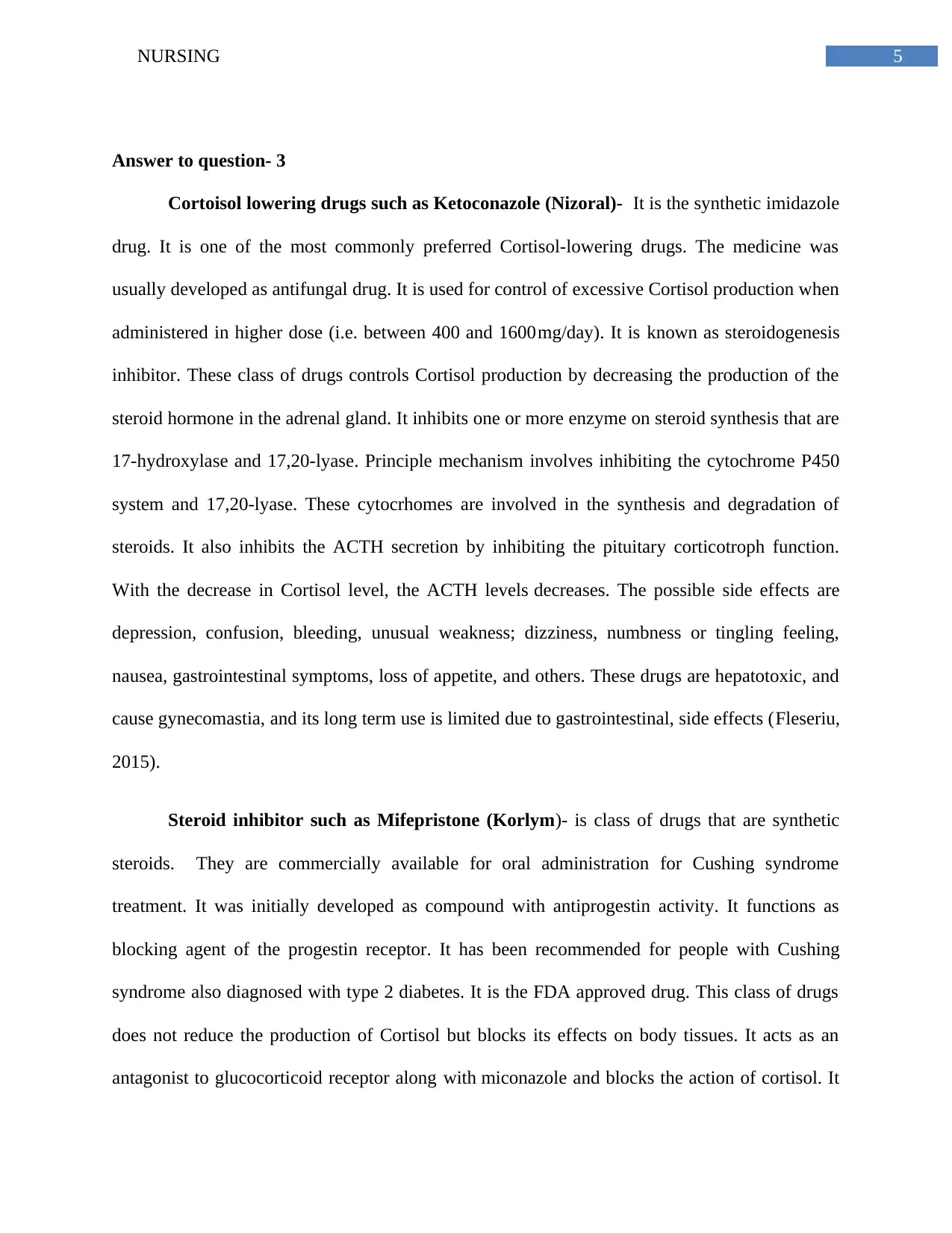
Answer to question- 3
Cortoisol lowering drugs such as Ketoconazole (Nizoral)- It is the synthetic imidazole
drug. It is one of the most commonly preferred Cortisol-lowering drugs. The medicine was
usually developed as antifungal drug. It is used for control of excessive Cortisol production when
administered in higher dose (i.e. between 400 and 1600 mg/day). It is known as steroidogenesis
inhibitor. These class of drugs controls Cortisol production by decreasing the production of the
steroid hormone in the adrenal gland. It inhibits one or more enzyme on steroid synthesis that are
17-hydroxylase and 17,20-lyase. Principle mechanism involves inhibiting the cytochrome P450
system and 17,20-lyase. These cytocrhomes are involved in the synthesis and degradation of
steroids. It also inhibits the ACTH secretion by inhibiting the pituitary corticotroph function.
With the decrease in Cortisol level, the ACTH levels decreases. The possible side effects are
depression, confusion, bleeding, unusual weakness; dizziness, numbness or tingling feeling,
nausea, gastrointestinal symptoms, loss of appetite, and others. These drugs are hepatotoxic, and
cause gynecomastia, and its long term use is limited due to gastrointestinal, side effects (Fleseriu,
2015).
Steroid inhibitor such as Mifepristone (Korlym)- is class of drugs that are synthetic
steroids. They are commercially available for oral administration for Cushing syndrome
treatment. It was initially developed as compound with antiprogestin activity. It functions as
blocking agent of the progestin receptor. It has been recommended for people with Cushing
syndrome also diagnosed with type 2 diabetes. It is the FDA approved drug. This class of drugs
does not reduce the production of Cortisol but blocks its effects on body tissues. It acts as an
antagonist to glucocorticoid receptor along with miconazole and blocks the action of cortisol. It
Answer to question- 3
Cortoisol lowering drugs such as Ketoconazole (Nizoral)- It is the synthetic imidazole
drug. It is one of the most commonly preferred Cortisol-lowering drugs. The medicine was
usually developed as antifungal drug. It is used for control of excessive Cortisol production when
administered in higher dose (i.e. between 400 and 1600 mg/day). It is known as steroidogenesis
inhibitor. These class of drugs controls Cortisol production by decreasing the production of the
steroid hormone in the adrenal gland. It inhibits one or more enzyme on steroid synthesis that are
17-hydroxylase and 17,20-lyase. Principle mechanism involves inhibiting the cytochrome P450
system and 17,20-lyase. These cytocrhomes are involved in the synthesis and degradation of
steroids. It also inhibits the ACTH secretion by inhibiting the pituitary corticotroph function.
With the decrease in Cortisol level, the ACTH levels decreases. The possible side effects are
depression, confusion, bleeding, unusual weakness; dizziness, numbness or tingling feeling,
nausea, gastrointestinal symptoms, loss of appetite, and others. These drugs are hepatotoxic, and
cause gynecomastia, and its long term use is limited due to gastrointestinal, side effects (Fleseriu,
2015).
Steroid inhibitor such as Mifepristone (Korlym)- is class of drugs that are synthetic
steroids. They are commercially available for oral administration for Cushing syndrome
treatment. It was initially developed as compound with antiprogestin activity. It functions as
blocking agent of the progestin receptor. It has been recommended for people with Cushing
syndrome also diagnosed with type 2 diabetes. It is the FDA approved drug. This class of drugs
does not reduce the production of Cortisol but blocks its effects on body tissues. It acts as an
antagonist to glucocorticoid receptor along with miconazole and blocks the action of cortisol. It
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
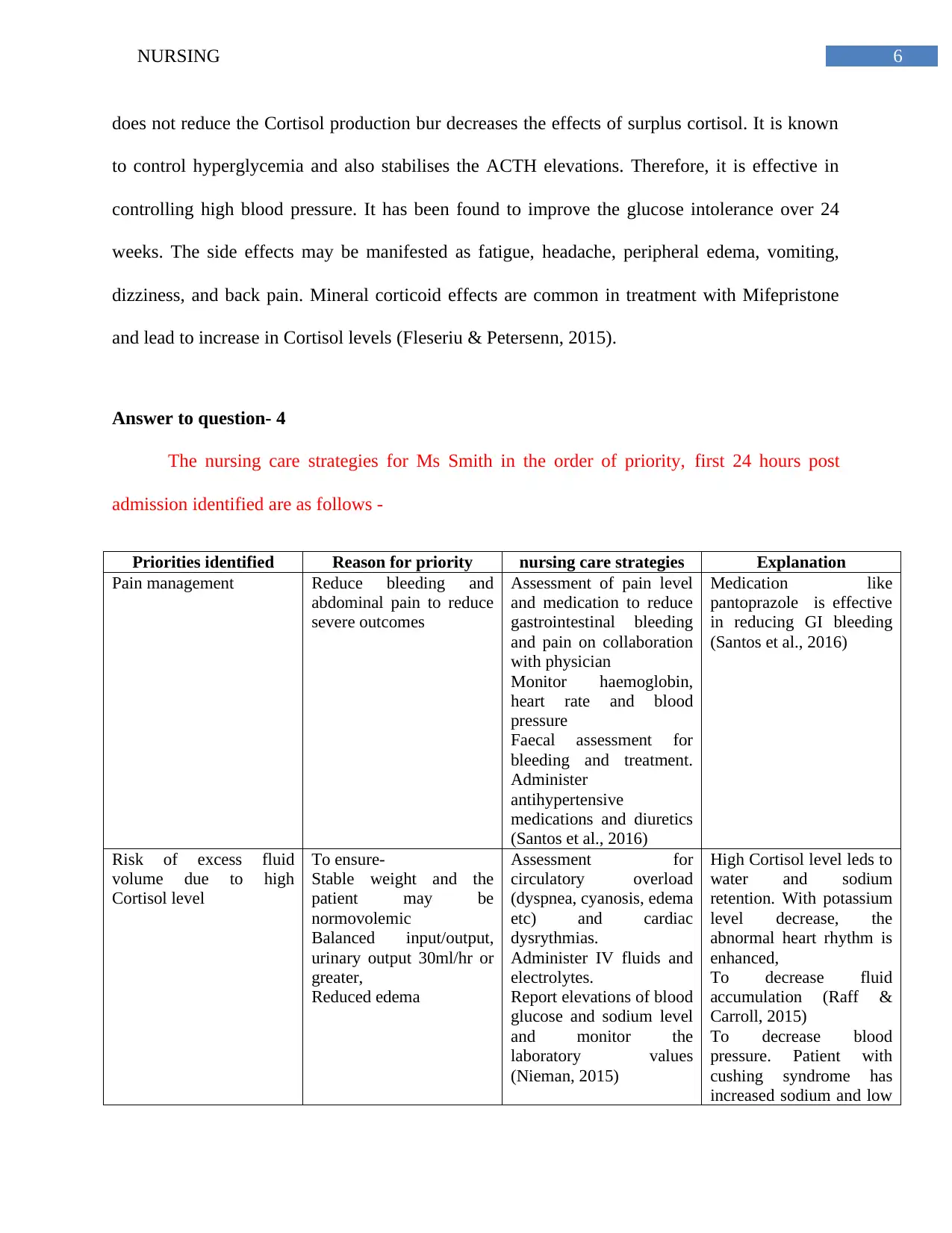
6NURSING
does not reduce the Cortisol production bur decreases the effects of surplus cortisol. It is known
to control hyperglycemia and also stabilises the ACTH elevations. Therefore, it is effective in
controlling high blood pressure. It has been found to improve the glucose intolerance over 24
weeks. The side effects may be manifested as fatigue, headache, peripheral edema, vomiting,
dizziness, and back pain. Mineral corticoid effects are common in treatment with Mifepristone
and lead to increase in Cortisol levels (Fleseriu & Petersenn, 2015).
Answer to question- 4
The nursing care strategies for Ms Smith in the order of priority, first 24 hours post
admission identified are as follows -
Priorities identified Reason for priority nursing care strategies Explanation
Pain management Reduce bleeding and
abdominal pain to reduce
severe outcomes
Assessment of pain level
and medication to reduce
gastrointestinal bleeding
and pain on collaboration
with physician
Monitor haemoglobin,
heart rate and blood
pressure
Faecal assessment for
bleeding and treatment.
Administer
antihypertensive
medications and diuretics
(Santos et al., 2016)
Medication like
pantoprazole is effective
in reducing GI bleeding
(Santos et al., 2016)
Risk of excess fluid
volume due to high
Cortisol level
To ensure-
Stable weight and the
patient may be
normovolemic
Balanced input/output,
urinary output 30ml/hr or
greater,
Reduced edema
Assessment for
circulatory overload
(dyspnea, cyanosis, edema
etc) and cardiac
dysrythmias.
Administer IV fluids and
electrolytes.
Report elevations of blood
glucose and sodium level
and monitor the
laboratory values
(Nieman, 2015)
High Cortisol level leds to
water and sodium
retention. With potassium
level decrease, the
abnormal heart rhythm is
enhanced,
To decrease fluid
accumulation (Raff &
Carroll, 2015)
To decrease blood
pressure. Patient with
cushing syndrome has
increased sodium and low
does not reduce the Cortisol production bur decreases the effects of surplus cortisol. It is known
to control hyperglycemia and also stabilises the ACTH elevations. Therefore, it is effective in
controlling high blood pressure. It has been found to improve the glucose intolerance over 24
weeks. The side effects may be manifested as fatigue, headache, peripheral edema, vomiting,
dizziness, and back pain. Mineral corticoid effects are common in treatment with Mifepristone
and lead to increase in Cortisol levels (Fleseriu & Petersenn, 2015).
Answer to question- 4
The nursing care strategies for Ms Smith in the order of priority, first 24 hours post
admission identified are as follows -
Priorities identified Reason for priority nursing care strategies Explanation
Pain management Reduce bleeding and
abdominal pain to reduce
severe outcomes
Assessment of pain level
and medication to reduce
gastrointestinal bleeding
and pain on collaboration
with physician
Monitor haemoglobin,
heart rate and blood
pressure
Faecal assessment for
bleeding and treatment.
Administer
antihypertensive
medications and diuretics
(Santos et al., 2016)
Medication like
pantoprazole is effective
in reducing GI bleeding
(Santos et al., 2016)
Risk of excess fluid
volume due to high
Cortisol level
To ensure-
Stable weight and the
patient may be
normovolemic
Balanced input/output,
urinary output 30ml/hr or
greater,
Reduced edema
Assessment for
circulatory overload
(dyspnea, cyanosis, edema
etc) and cardiac
dysrythmias.
Administer IV fluids and
electrolytes.
Report elevations of blood
glucose and sodium level
and monitor the
laboratory values
(Nieman, 2015)
High Cortisol level leds to
water and sodium
retention. With potassium
level decrease, the
abnormal heart rhythm is
enhanced,
To decrease fluid
accumulation (Raff &
Carroll, 2015)
To decrease blood
pressure. Patient with
cushing syndrome has
increased sodium and low
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
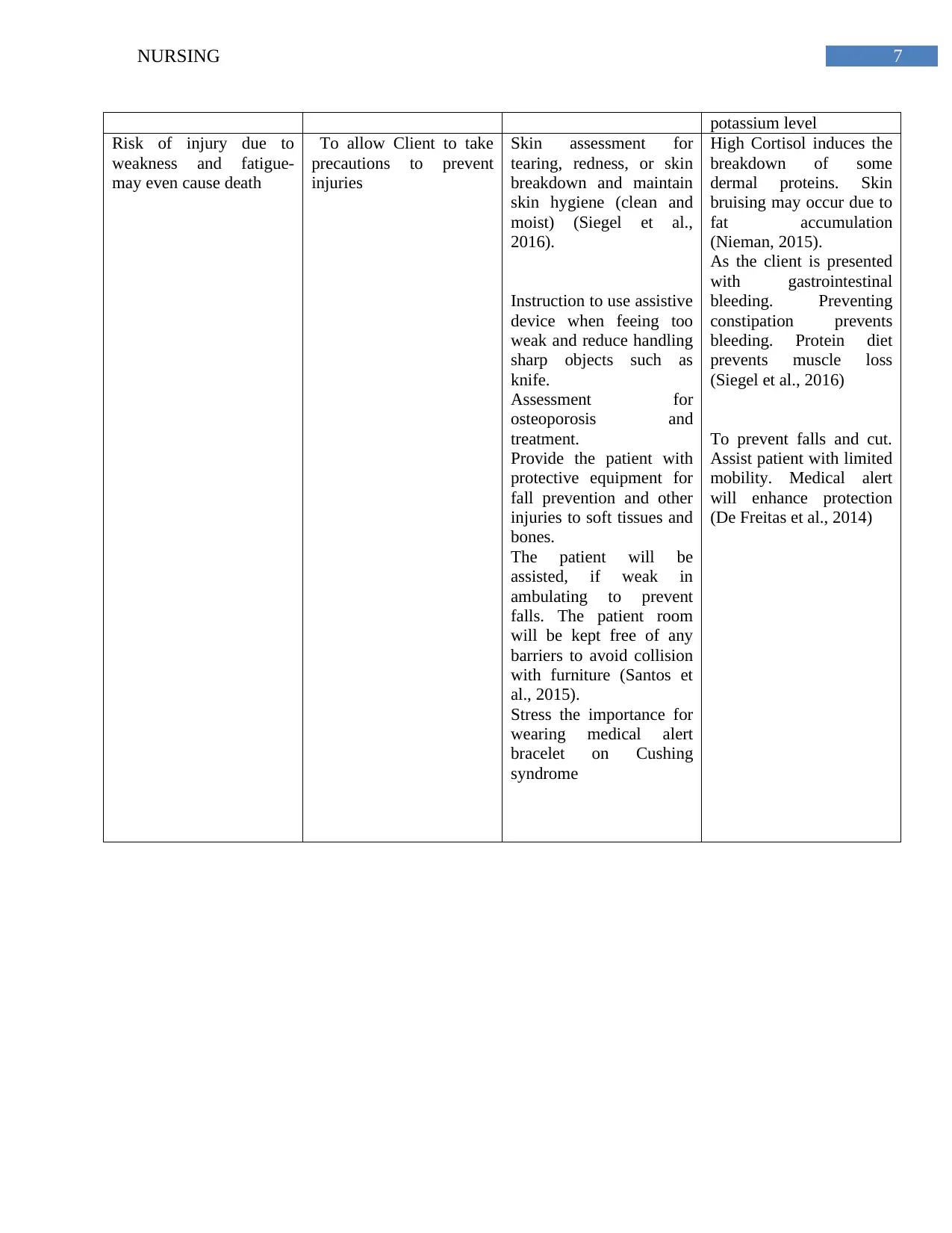
7NURSING
potassium level
Risk of injury due to
weakness and fatigue-
may even cause death
To allow Client to take
precautions to prevent
injuries
Skin assessment for
tearing, redness, or skin
breakdown and maintain
skin hygiene (clean and
moist) (Siegel et al.,
2016).
Instruction to use assistive
device when feeing too
weak and reduce handling
sharp objects such as
knife.
Assessment for
osteoporosis and
treatment.
Provide the patient with
protective equipment for
fall prevention and other
injuries to soft tissues and
bones.
The patient will be
assisted, if weak in
ambulating to prevent
falls. The patient room
will be kept free of any
barriers to avoid collision
with furniture (Santos et
al., 2015).
Stress the importance for
wearing medical alert
bracelet on Cushing
syndrome
High Cortisol induces the
breakdown of some
dermal proteins. Skin
bruising may occur due to
fat accumulation
(Nieman, 2015).
As the client is presented
with gastrointestinal
bleeding. Preventing
constipation prevents
bleeding. Protein diet
prevents muscle loss
(Siegel et al., 2016)
To prevent falls and cut.
Assist patient with limited
mobility. Medical alert
will enhance protection
(De Freitas et al., 2014)
potassium level
Risk of injury due to
weakness and fatigue-
may even cause death
To allow Client to take
precautions to prevent
injuries
Skin assessment for
tearing, redness, or skin
breakdown and maintain
skin hygiene (clean and
moist) (Siegel et al.,
2016).
Instruction to use assistive
device when feeing too
weak and reduce handling
sharp objects such as
knife.
Assessment for
osteoporosis and
treatment.
Provide the patient with
protective equipment for
fall prevention and other
injuries to soft tissues and
bones.
The patient will be
assisted, if weak in
ambulating to prevent
falls. The patient room
will be kept free of any
barriers to avoid collision
with furniture (Santos et
al., 2015).
Stress the importance for
wearing medical alert
bracelet on Cushing
syndrome
High Cortisol induces the
breakdown of some
dermal proteins. Skin
bruising may occur due to
fat accumulation
(Nieman, 2015).
As the client is presented
with gastrointestinal
bleeding. Preventing
constipation prevents
bleeding. Protein diet
prevents muscle loss
(Siegel et al., 2016)
To prevent falls and cut.
Assist patient with limited
mobility. Medical alert
will enhance protection
(De Freitas et al., 2014)
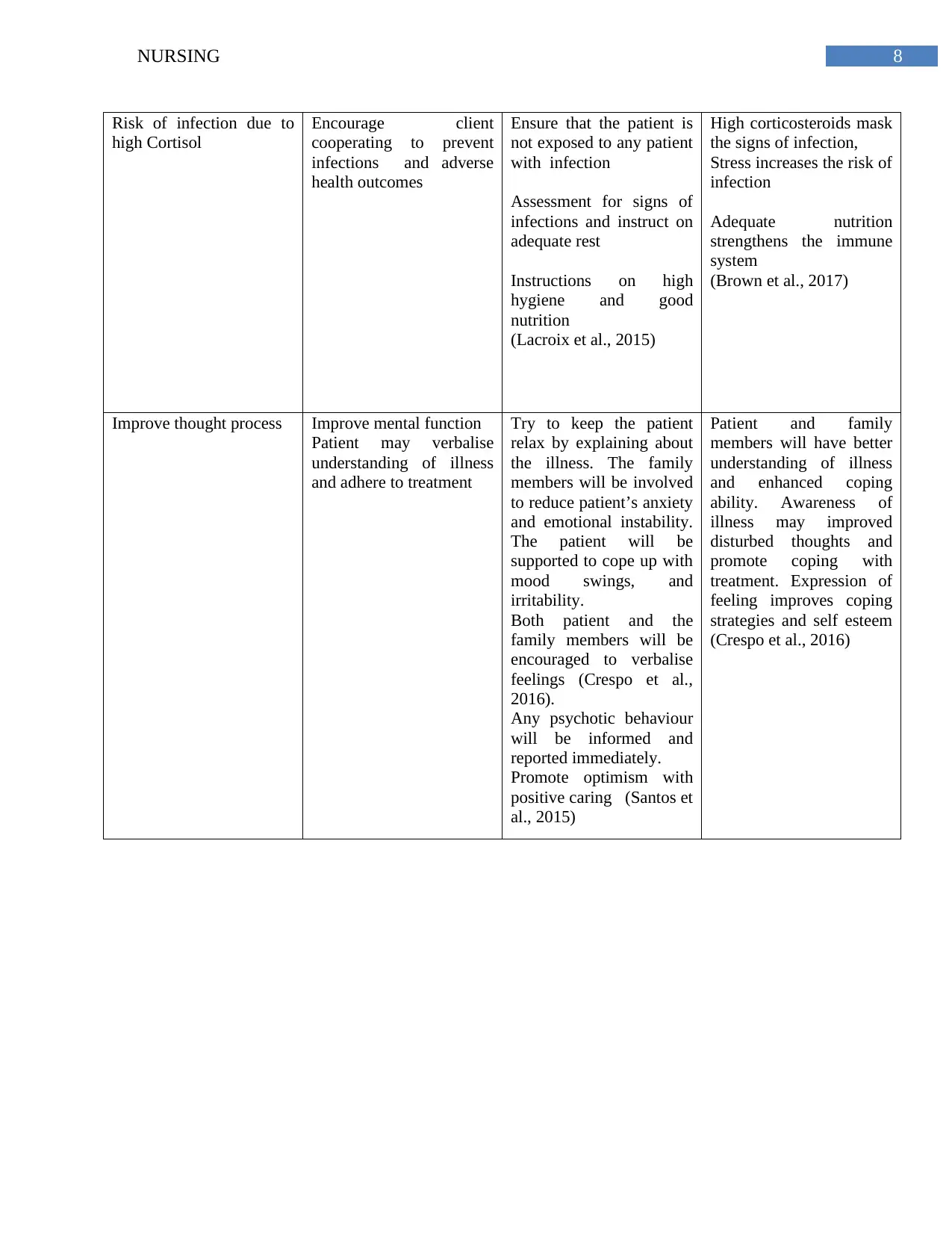
8NURSING
Risk of infection due to
high Cortisol
Encourage client
cooperating to prevent
infections and adverse
health outcomes
Ensure that the patient is
not exposed to any patient
with infection
Assessment for signs of
infections and instruct on
adequate rest
Instructions on high
hygiene and good
nutrition
(Lacroix et al., 2015)
High corticosteroids mask
the signs of infection,
Stress increases the risk of
infection
Adequate nutrition
strengthens the immune
system
(Brown et al., 2017)
Improve thought process Improve mental function
Patient may verbalise
understanding of illness
and adhere to treatment
Try to keep the patient
relax by explaining about
the illness. The family
members will be involved
to reduce patient’s anxiety
and emotional instability.
The patient will be
supported to cope up with
mood swings, and
irritability.
Both patient and the
family members will be
encouraged to verbalise
feelings (Crespo et al.,
2016).
Any psychotic behaviour
will be informed and
reported immediately.
Promote optimism with
positive caring (Santos et
al., 2015)
Patient and family
members will have better
understanding of illness
and enhanced coping
ability. Awareness of
illness may improved
disturbed thoughts and
promote coping with
treatment. Expression of
feeling improves coping
strategies and self esteem
(Crespo et al., 2016)
Risk of infection due to
high Cortisol
Encourage client
cooperating to prevent
infections and adverse
health outcomes
Ensure that the patient is
not exposed to any patient
with infection
Assessment for signs of
infections and instruct on
adequate rest
Instructions on high
hygiene and good
nutrition
(Lacroix et al., 2015)
High corticosteroids mask
the signs of infection,
Stress increases the risk of
infection
Adequate nutrition
strengthens the immune
system
(Brown et al., 2017)
Improve thought process Improve mental function
Patient may verbalise
understanding of illness
and adhere to treatment
Try to keep the patient
relax by explaining about
the illness. The family
members will be involved
to reduce patient’s anxiety
and emotional instability.
The patient will be
supported to cope up with
mood swings, and
irritability.
Both patient and the
family members will be
encouraged to verbalise
feelings (Crespo et al.,
2016).
Any psychotic behaviour
will be informed and
reported immediately.
Promote optimism with
positive caring (Santos et
al., 2015)
Patient and family
members will have better
understanding of illness
and enhanced coping
ability. Awareness of
illness may improved
disturbed thoughts and
promote coping with
treatment. Expression of
feeling improves coping
strategies and self esteem
(Crespo et al., 2016)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
References
Bizarro, V. R., Araujo, L. M. M., Santos, J. C. S., Lima, A. G., Resende, P. C., de Jesus, A. L.
C., ... & Arbex, A. K. (2015, December). Diabetes and weight gain after bariatric surgery,
due to Cushing's syndrome. In Diabetology & metabolic syndrome, 7(1), 97.
Brown, D., Edwards, H., Seaton, L., & Buckley, T. (2017). Lewis's Medical-Surgical Nursing:
Assessment and Management of Clinical Problems. Elsevier Health Sciences.
Crespo Martín, I., Youdale, S. W., Valassi, E., & Resmini, E. (2016). Neuropsychological
evaluation of patients with acromegaly and Cushing's syndrome: Long-term effects.
De Freitas Luzia, M., de Goes Victor, M. A., & de Fátima Lucena, A. (2014). Nursing Diagnosis
Risk for falls: prevalence and clinical profile of hospitalized patients. Revista Latino-
Americana de Enfermagem, 22(2), 262.
Fleseriu, M. (2015). Medical treatment of Cushing disease: new targets, new
hope. Endocrinology and Metabolism Clinics, 44(1), 51-70.
Fleseriu, M., & Petersenn, S. (2015). Medical therapy for Cushing’s disease: adrenal
steroidogenesis inhibitors and glucocorticoid receptor blockers. Pituitary, 18(2), 245-252.
Karaman, O., Zuhur, S. S., Cil, E., Ozderya, A., Ozturk, F. Y., Ilhan, M., & Altuntas, Y. (2017).
Cushing’s syndrome in obese patients with type 2 diabetes: A single center screening
study. International Journal of Diabetes in Developing Countries, 37(1), 63-68.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
References
Bizarro, V. R., Araujo, L. M. M., Santos, J. C. S., Lima, A. G., Resende, P. C., de Jesus, A. L.
C., ... & Arbex, A. K. (2015, December). Diabetes and weight gain after bariatric surgery,
due to Cushing's syndrome. In Diabetology & metabolic syndrome, 7(1), 97.
Brown, D., Edwards, H., Seaton, L., & Buckley, T. (2017). Lewis's Medical-Surgical Nursing:
Assessment and Management of Clinical Problems. Elsevier Health Sciences.
Crespo Martín, I., Youdale, S. W., Valassi, E., & Resmini, E. (2016). Neuropsychological
evaluation of patients with acromegaly and Cushing's syndrome: Long-term effects.
De Freitas Luzia, M., de Goes Victor, M. A., & de Fátima Lucena, A. (2014). Nursing Diagnosis
Risk for falls: prevalence and clinical profile of hospitalized patients. Revista Latino-
Americana de Enfermagem, 22(2), 262.
Fleseriu, M. (2015). Medical treatment of Cushing disease: new targets, new
hope. Endocrinology and Metabolism Clinics, 44(1), 51-70.
Fleseriu, M., & Petersenn, S. (2015). Medical therapy for Cushing’s disease: adrenal
steroidogenesis inhibitors and glucocorticoid receptor blockers. Pituitary, 18(2), 245-252.
Karaman, O., Zuhur, S. S., Cil, E., Ozderya, A., Ozturk, F. Y., Ilhan, M., & Altuntas, Y. (2017).
Cushing’s syndrome in obese patients with type 2 diabetes: A single center screening
study. International Journal of Diabetes in Developing Countries, 37(1), 63-68.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
Martínez-Momblán, M. A., Gómez, C., Santos, A., Porta, N., Esteve, J., Ubeda, I., ... & Resmini,
E. (2016). A specific nursing educational program in patients with Cushing’s
syndrome. Endocrine, 53(1), 199-209.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European journal of endocrinology, 173(4), 33-38.
Pivonello, R., Isidori, A. M., De Martino, M. C., Newell-Price, J., Biller, B. M., & Colao, A.
(2016). Complications of Cushing's syndrome: state of the art. The Lancet Diabetes &
Endocrinology, 4(7), 611-629.
Raff, H., & Carroll, T. (2015). Cushing's syndrome: from physiological principles to diagnosis
and clinical care. The Journal of physiology, 593(3), 493-506.
Santos, A., Crespo, I., Aulinas, A., Resmini, E., Valassi, E., & Webb, S. M. (2015). Quality of
life in Cushing’s syndrome. Pituitary, 18(2), 195-200.
Santos, A., Resmini, E., Pascual, J. C., Crespo, I., & Webb, S. M. (2017). Psychiatric symptoms
in patients with Cushing’s syndrome: prevalence, diagnosis and
management. Drugs, 77(8), 829-842.
Siegel, S., Milian, M., Kleist, B., Psaras, T., Tsiogka, M., Führer, D., ... & Menzel, C. (2016).
Coping strategies have a strong impact on quality of life, depression, and embitterment in
patients with Cushing’s disease. Pituitary, 19(6), 590-600.
Steffensen, C., Bak, A. M., Rubeck, K. Z., & Jørgensen, J. O. L. (2010). Epidemiology of
Cushing’s syndrome. Neuroendocrinology, 92(1), 1-5.
Martínez-Momblán, M. A., Gómez, C., Santos, A., Porta, N., Esteve, J., Ubeda, I., ... & Resmini,
E. (2016). A specific nursing educational program in patients with Cushing’s
syndrome. Endocrine, 53(1), 199-209.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European journal of endocrinology, 173(4), 33-38.
Pivonello, R., Isidori, A. M., De Martino, M. C., Newell-Price, J., Biller, B. M., & Colao, A.
(2016). Complications of Cushing's syndrome: state of the art. The Lancet Diabetes &
Endocrinology, 4(7), 611-629.
Raff, H., & Carroll, T. (2015). Cushing's syndrome: from physiological principles to diagnosis
and clinical care. The Journal of physiology, 593(3), 493-506.
Santos, A., Crespo, I., Aulinas, A., Resmini, E., Valassi, E., & Webb, S. M. (2015). Quality of
life in Cushing’s syndrome. Pituitary, 18(2), 195-200.
Santos, A., Resmini, E., Pascual, J. C., Crespo, I., & Webb, S. M. (2017). Psychiatric symptoms
in patients with Cushing’s syndrome: prevalence, diagnosis and
management. Drugs, 77(8), 829-842.
Siegel, S., Milian, M., Kleist, B., Psaras, T., Tsiogka, M., Führer, D., ... & Menzel, C. (2016).
Coping strategies have a strong impact on quality of life, depression, and embitterment in
patients with Cushing’s disease. Pituitary, 19(6), 590-600.
Steffensen, C., Bak, A. M., Rubeck, K. Z., & Jørgensen, J. O. L. (2010). Epidemiology of
Cushing’s syndrome. Neuroendocrinology, 92(1), 1-5.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





