Nursing Case Study and Transition to Practice: Ashanti's Remote Clinic
VerifiedAdded on 2022/08/17
|10
|2502
|25
Case Study
AI Summary
This case study focuses on Ashanti, a 3-year-old indigenous girl presenting with dehydration at a remote clinic. The assignment addresses her condition, likely caused by diarrhea, and the absence of urine output despite fluid intake. It begins with an assessment of Ashanti's symptoms, vital signs, and the application of the 'Between the Flags' system. The analysis highlights the need for rapid response interventions based on her critical vital signs. The ISBAR handover report is then presented, detailing Ashanti's situation, background, assessment findings, and recommendations for immediate transfer to a Clinical Emergency Response System (CERS). The study proceeds to outline the immediate management plan, including the administration of oral rehydration solution (ORS) and frequent fluid intake. A multidisciplinary team is proposed to manage the case, involving a pediatrician, dietician, gastroenterologist, registered nurse, nephrologist, and general practitioner. The case study emphasizes the importance of educating Ashanti's parents on proper ORS preparation, dietary adjustments, and post-discharge care to prevent future episodes. Finally, the assignment concludes with a discussion on discharge criteria, ensuring the resolution of symptoms and parental understanding of the care plan. The analysis incorporates relevant literature, clinical guidelines and references to support the recommendations.

Running head: NURSING CASE STUDY AND TRANSITION TO PRACTICE
NURSING CASE STUDY AND TRANSITION TO PRACTICE
Name of the Student:
Name of the University:
Author note:
NURSING CASE STUDY AND TRANSITION TO PRACTICE
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING CASE STUDY AND TRANSITION TO PRACTICE
Question 1
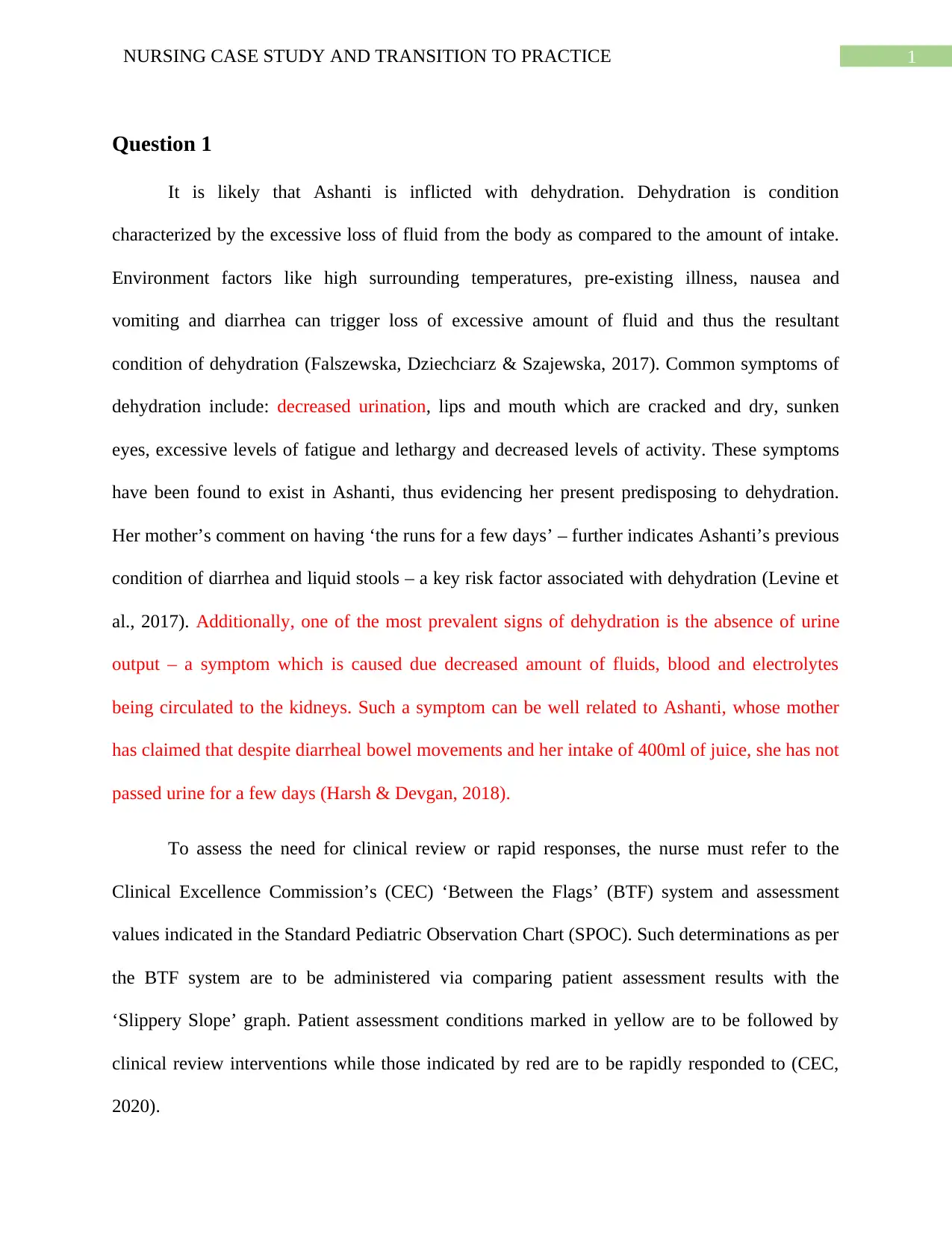
It is likely that Ashanti is inflicted with dehydration. Dehydration is condition
characterized by the excessive loss of fluid from the body as compared to the amount of intake.
Environment factors like high surrounding temperatures, pre-existing illness, nausea and
vomiting and diarrhea can trigger loss of excessive amount of fluid and thus the resultant
condition of dehydration (Falszewska, Dziechciarz & Szajewska, 2017). Common symptoms of
dehydration include: decreased urination, lips and mouth which are cracked and dry, sunken
eyes, excessive levels of fatigue and lethargy and decreased levels of activity. These symptoms
have been found to exist in Ashanti, thus evidencing her present predisposing to dehydration.
Her mother’s comment on having ‘the runs for a few days’ – further indicates Ashanti’s previous
condition of diarrhea and liquid stools – a key risk factor associated with dehydration (Levine et
al., 2017). Additionally, one of the most prevalent signs of dehydration is the absence of urine
output – a symptom which is caused due decreased amount of fluids, blood and electrolytes
being circulated to the kidneys. Such a symptom can be well related to Ashanti, whose mother
has claimed that despite diarrheal bowel movements and her intake of 400ml of juice, she has not
passed urine for a few days (Harsh & Devgan, 2018).
To assess the need for clinical review or rapid responses, the nurse must refer to the
Clinical Excellence Commission’s (CEC) ‘Between the Flags’ (BTF) system and assessment
values indicated in the Standard Pediatric Observation Chart (SPOC). Such determinations as per
the BTF system are to be administered via comparing patient assessment results with the
‘Slippery Slope’ graph. Patient assessment conditions marked in yellow are to be followed by
clinical review interventions while those indicated by red are to be rapidly responded to (CEC,
2020).
Question 1
It is likely that Ashanti is inflicted with dehydration. Dehydration is condition
characterized by the excessive loss of fluid from the body as compared to the amount of intake.
Environment factors like high surrounding temperatures, pre-existing illness, nausea and
vomiting and diarrhea can trigger loss of excessive amount of fluid and thus the resultant
condition of dehydration (Falszewska, Dziechciarz & Szajewska, 2017). Common symptoms of
dehydration include: decreased urination, lips and mouth which are cracked and dry, sunken
eyes, excessive levels of fatigue and lethargy and decreased levels of activity. These symptoms
have been found to exist in Ashanti, thus evidencing her present predisposing to dehydration.
Her mother’s comment on having ‘the runs for a few days’ – further indicates Ashanti’s previous
condition of diarrhea and liquid stools – a key risk factor associated with dehydration (Levine et
al., 2017). Additionally, one of the most prevalent signs of dehydration is the absence of urine
output – a symptom which is caused due decreased amount of fluids, blood and electrolytes
being circulated to the kidneys. Such a symptom can be well related to Ashanti, whose mother
has claimed that despite diarrheal bowel movements and her intake of 400ml of juice, she has not
passed urine for a few days (Harsh & Devgan, 2018).
To assess the need for clinical review or rapid responses, the nurse must refer to the
Clinical Excellence Commission’s (CEC) ‘Between the Flags’ (BTF) system and assessment
values indicated in the Standard Pediatric Observation Chart (SPOC). Such determinations as per
the BTF system are to be administered via comparing patient assessment results with the
‘Slippery Slope’ graph. Patient assessment conditions marked in yellow are to be followed by
clinical review interventions while those indicated by red are to be rapidly responded to (CEC,
2020).
2NURSING CASE STUDY AND TRANSITION TO PRACTICE
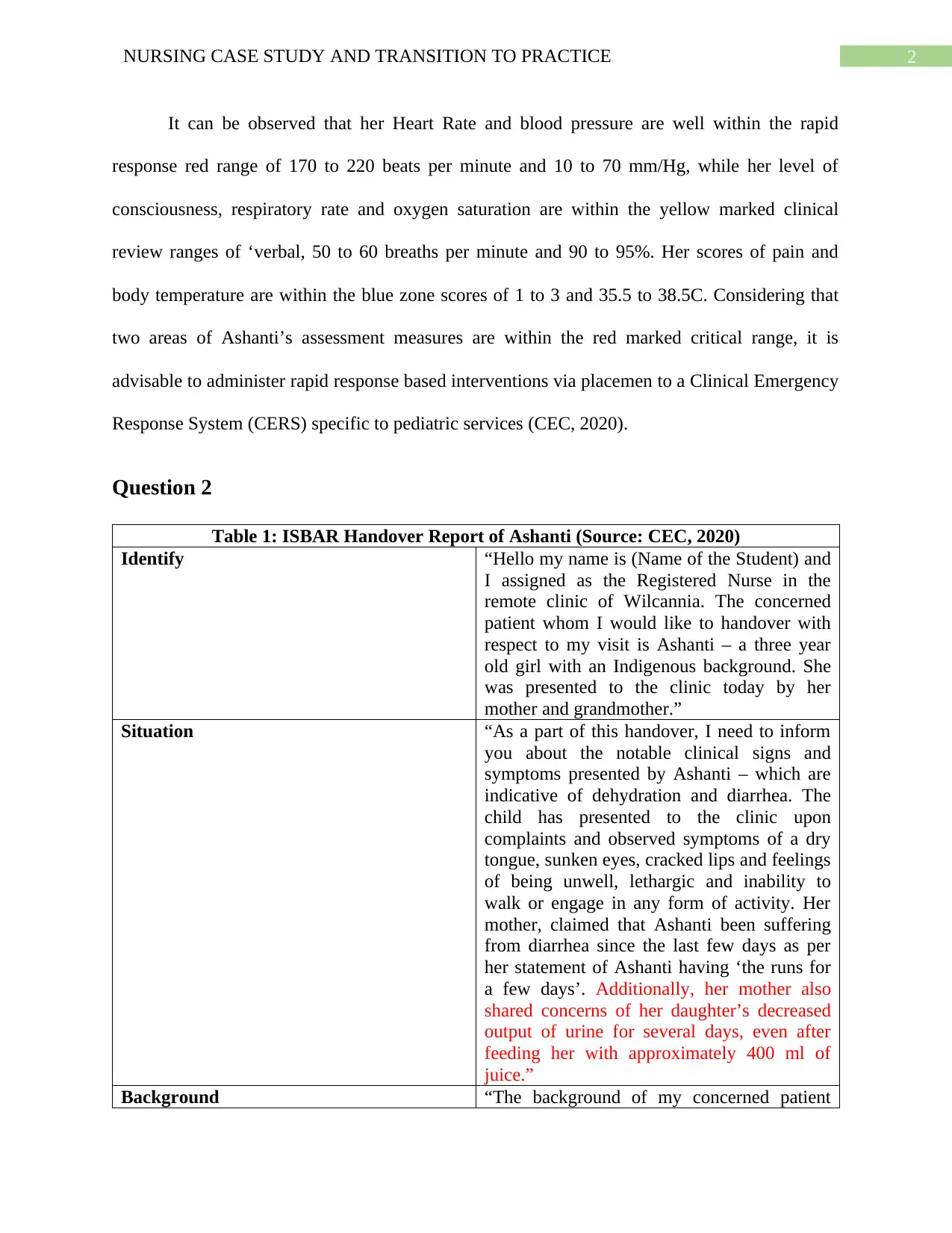
It can be observed that her Heart Rate and blood pressure are well within the rapid
response red range of 170 to 220 beats per minute and 10 to 70 mm/Hg, while her level of
consciousness, respiratory rate and oxygen saturation are within the yellow marked clinical
review ranges of ‘verbal, 50 to 60 breaths per minute and 90 to 95%. Her scores of pain and
body temperature are within the blue zone scores of 1 to 3 and 35.5 to 38.5C. Considering that
two areas of Ashanti’s assessment measures are within the red marked critical range, it is
advisable to administer rapid response based interventions via placemen to a Clinical Emergency
Response System (CERS) specific to pediatric services (CEC, 2020).
Question 2
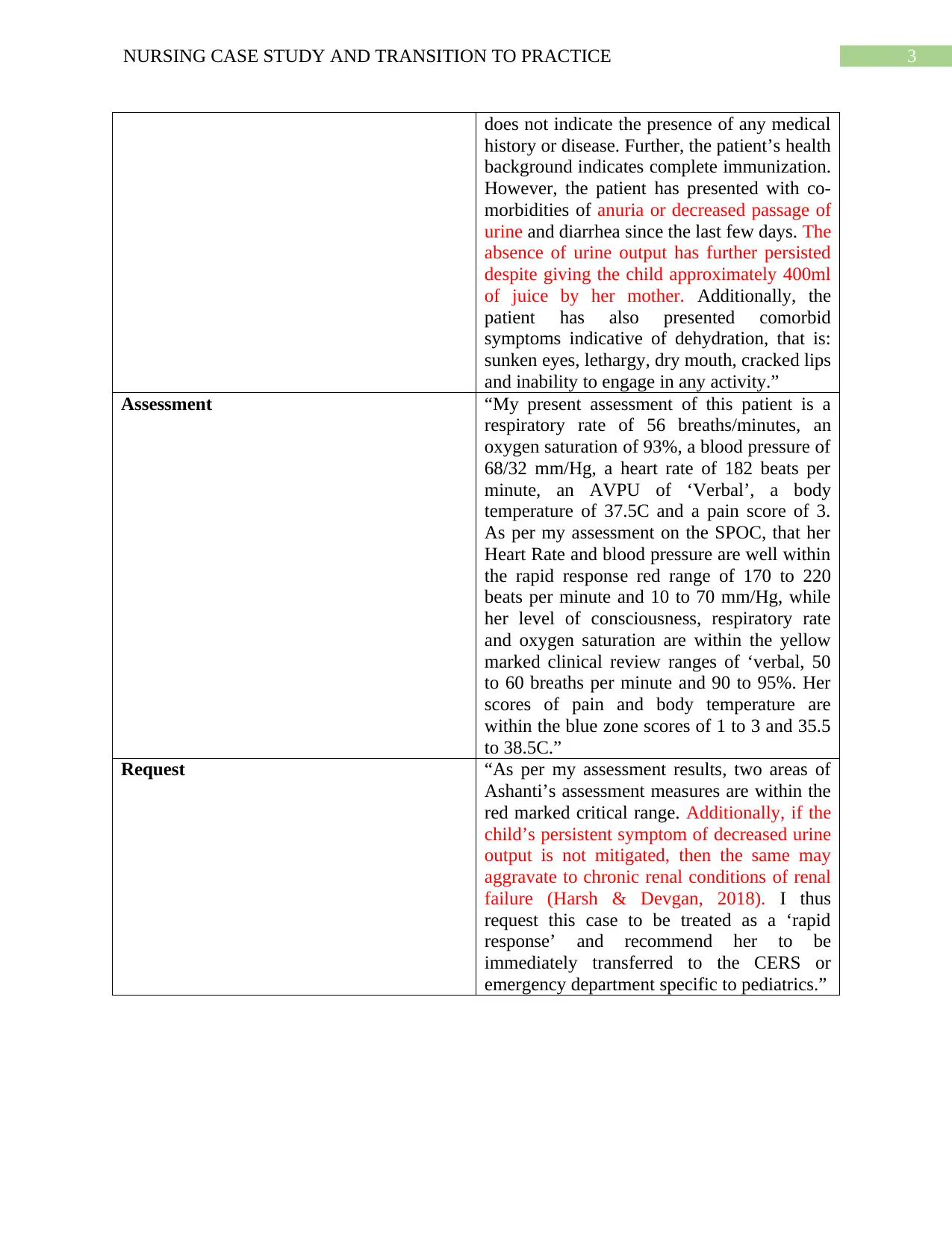
Table 1: ISBAR Handover Report of Ashanti (Source: CEC, 2020)
Identify “Hello my name is (Name of the Student) and
I assigned as the Registered Nurse in the
remote clinic of Wilcannia. The concerned
patient whom I would like to handover with
respect to my visit is Ashanti – a three year
old girl with an Indigenous background. She
was presented to the clinic today by her
mother and grandmother.”
Situation “As a part of this handover, I need to inform
you about the notable clinical signs and
symptoms presented by Ashanti – which are
indicative of dehydration and diarrhea. The
child has presented to the clinic upon
complaints and observed symptoms of a dry
tongue, sunken eyes, cracked lips and feelings
of being unwell, lethargic and inability to
walk or engage in any form of activity. Her
mother, claimed that Ashanti been suffering
from diarrhea since the last few days as per
her statement of Ashanti having ‘the runs for
a few days’. Additionally, her mother also
shared concerns of her daughter’s decreased
output of urine for several days, even after
feeding her with approximately 400 ml of
juice.”
Background “The background of my concerned patient
It can be observed that her Heart Rate and blood pressure are well within the rapid
response red range of 170 to 220 beats per minute and 10 to 70 mm/Hg, while her level of
consciousness, respiratory rate and oxygen saturation are within the yellow marked clinical
review ranges of ‘verbal, 50 to 60 breaths per minute and 90 to 95%. Her scores of pain and
body temperature are within the blue zone scores of 1 to 3 and 35.5 to 38.5C. Considering that
two areas of Ashanti’s assessment measures are within the red marked critical range, it is
advisable to administer rapid response based interventions via placemen to a Clinical Emergency
Response System (CERS) specific to pediatric services (CEC, 2020).
Question 2
Table 1: ISBAR Handover Report of Ashanti (Source: CEC, 2020)
Identify “Hello my name is (Name of the Student) and
I assigned as the Registered Nurse in the
remote clinic of Wilcannia. The concerned
patient whom I would like to handover with
respect to my visit is Ashanti – a three year
old girl with an Indigenous background. She
was presented to the clinic today by her
mother and grandmother.”
Situation “As a part of this handover, I need to inform
you about the notable clinical signs and
symptoms presented by Ashanti – which are
indicative of dehydration and diarrhea. The
child has presented to the clinic upon
complaints and observed symptoms of a dry
tongue, sunken eyes, cracked lips and feelings
of being unwell, lethargic and inability to
walk or engage in any form of activity. Her
mother, claimed that Ashanti been suffering
from diarrhea since the last few days as per
her statement of Ashanti having ‘the runs for
a few days’. Additionally, her mother also
shared concerns of her daughter’s decreased
output of urine for several days, even after
feeding her with approximately 400 ml of
juice.”
Background “The background of my concerned patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING CASE STUDY AND TRANSITION TO PRACTICE
does not indicate the presence of any medical
history or disease. Further, the patient’s health
background indicates complete immunization.
However, the patient has presented with co-
morbidities of anuria or decreased passage of
urine and diarrhea since the last few days. The
absence of urine output has further persisted
despite giving the child approximately 400ml
of juice by her mother. Additionally, the
patient has also presented comorbid
symptoms indicative of dehydration, that is:
sunken eyes, lethargy, dry mouth, cracked lips
and inability to engage in any activity.”
Assessment “My present assessment of this patient is a
respiratory rate of 56 breaths/minutes, an
oxygen saturation of 93%, a blood pressure of
68/32 mm/Hg, a heart rate of 182 beats per
minute, an AVPU of ‘Verbal’, a body
temperature of 37.5C and a pain score of 3.
As per my assessment on the SPOC, that her
Heart Rate and blood pressure are well within
the rapid response red range of 170 to 220
beats per minute and 10 to 70 mm/Hg, while
her level of consciousness, respiratory rate
and oxygen saturation are within the yellow
marked clinical review ranges of ‘verbal, 50
to 60 breaths per minute and 90 to 95%. Her
scores of pain and body temperature are
within the blue zone scores of 1 to 3 and 35.5
to 38.5C.”
Request “As per my assessment results, two areas of
Ashanti’s assessment measures are within the
red marked critical range. Additionally, if the
child’s persistent symptom of decreased urine
output is not mitigated, then the same may
aggravate to chronic renal conditions of renal
failure (Harsh & Devgan, 2018). I thus
request this case to be treated as a ‘rapid
response’ and recommend her to be
immediately transferred to the CERS or
emergency department specific to pediatrics.”
does not indicate the presence of any medical
history or disease. Further, the patient’s health
background indicates complete immunization.
However, the patient has presented with co-
morbidities of anuria or decreased passage of
urine and diarrhea since the last few days. The
absence of urine output has further persisted
despite giving the child approximately 400ml
of juice by her mother. Additionally, the
patient has also presented comorbid
symptoms indicative of dehydration, that is:
sunken eyes, lethargy, dry mouth, cracked lips
and inability to engage in any activity.”
Assessment “My present assessment of this patient is a
respiratory rate of 56 breaths/minutes, an
oxygen saturation of 93%, a blood pressure of
68/32 mm/Hg, a heart rate of 182 beats per
minute, an AVPU of ‘Verbal’, a body
temperature of 37.5C and a pain score of 3.
As per my assessment on the SPOC, that her
Heart Rate and blood pressure are well within
the rapid response red range of 170 to 220
beats per minute and 10 to 70 mm/Hg, while
her level of consciousness, respiratory rate
and oxygen saturation are within the yellow
marked clinical review ranges of ‘verbal, 50
to 60 breaths per minute and 90 to 95%. Her
scores of pain and body temperature are
within the blue zone scores of 1 to 3 and 35.5
to 38.5C.”
Request “As per my assessment results, two areas of
Ashanti’s assessment measures are within the
red marked critical range. Additionally, if the
child’s persistent symptom of decreased urine
output is not mitigated, then the same may
aggravate to chronic renal conditions of renal
failure (Harsh & Devgan, 2018). I thus
request this case to be treated as a ‘rapid
response’ and recommend her to be
immediately transferred to the CERS or
emergency department specific to pediatrics.”
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING CASE STUDY AND TRANSITION TO PRACTICE
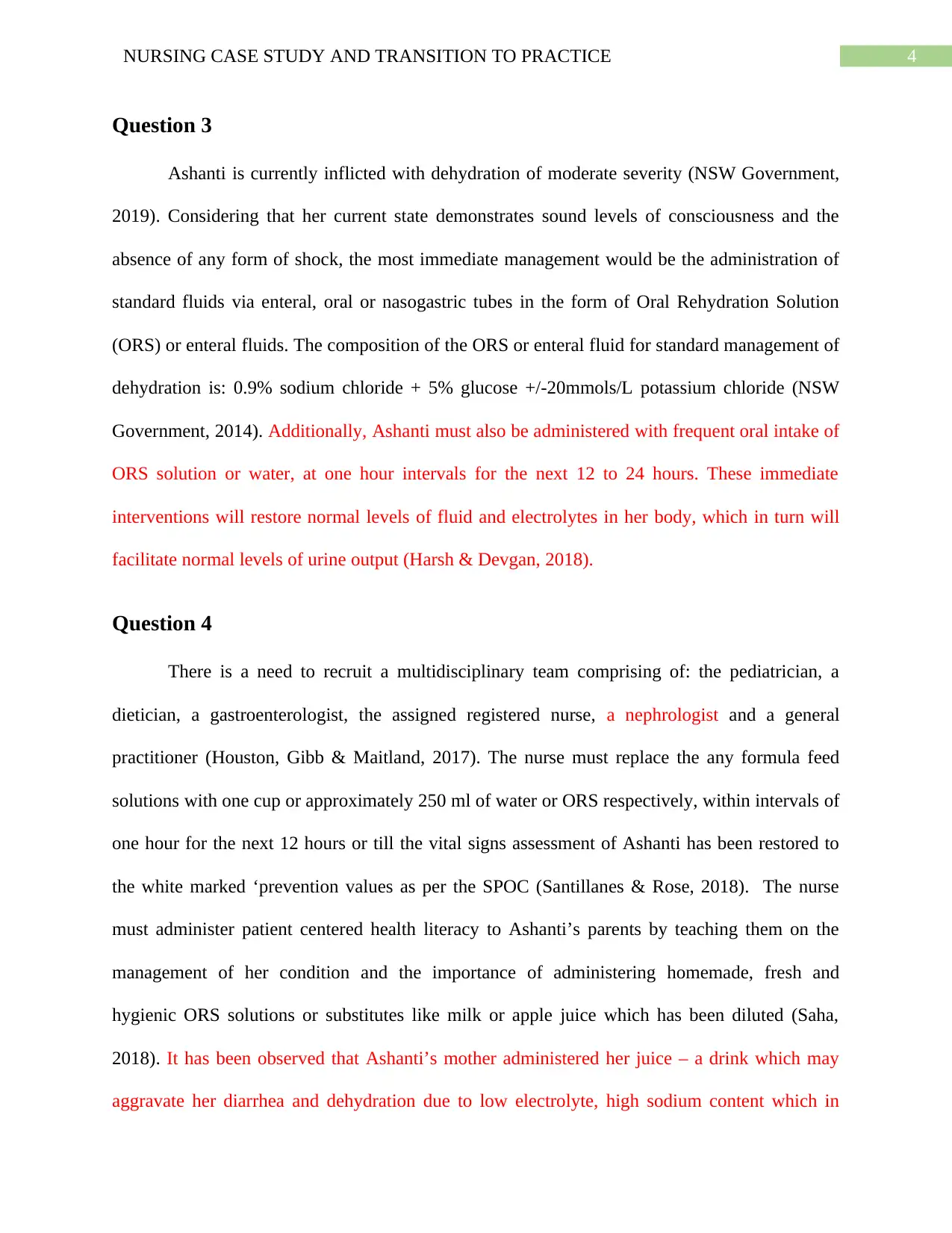
Question 3
Ashanti is currently inflicted with dehydration of moderate severity (NSW Government,
2019). Considering that her current state demonstrates sound levels of consciousness and the
absence of any form of shock, the most immediate management would be the administration of
standard fluids via enteral, oral or nasogastric tubes in the form of Oral Rehydration Solution
(ORS) or enteral fluids. The composition of the ORS or enteral fluid for standard management of
dehydration is: 0.9% sodium chloride + 5% glucose +/-20mmols/L potassium chloride (NSW
Government, 2014). Additionally, Ashanti must also be administered with frequent oral intake of
ORS solution or water, at one hour intervals for the next 12 to 24 hours. These immediate
interventions will restore normal levels of fluid and electrolytes in her body, which in turn will
facilitate normal levels of urine output (Harsh & Devgan, 2018).
Question 4
There is a need to recruit a multidisciplinary team comprising of: the pediatrician, a
dietician, a gastroenterologist, the assigned registered nurse, a nephrologist and a general
practitioner (Houston, Gibb & Maitland, 2017). The nurse must replace the any formula feed
solutions with one cup or approximately 250 ml of water or ORS respectively, within intervals of
one hour for the next 12 hours or till the vital signs assessment of Ashanti has been restored to
the white marked ‘prevention values as per the SPOC (Santillanes & Rose, 2018). The nurse
must administer patient centered health literacy to Ashanti’s parents by teaching them on the
management of her condition and the importance of administering homemade, fresh and
hygienic ORS solutions or substitutes like milk or apple juice which has been diluted (Saha,
2018). It has been observed that Ashanti’s mother administered her juice – a drink which may
aggravate her diarrhea and dehydration due to low electrolyte, high sodium content which in
Question 3
Ashanti is currently inflicted with dehydration of moderate severity (NSW Government,
2019). Considering that her current state demonstrates sound levels of consciousness and the
absence of any form of shock, the most immediate management would be the administration of
standard fluids via enteral, oral or nasogastric tubes in the form of Oral Rehydration Solution
(ORS) or enteral fluids. The composition of the ORS or enteral fluid for standard management of
dehydration is: 0.9% sodium chloride + 5% glucose +/-20mmols/L potassium chloride (NSW
Government, 2014). Additionally, Ashanti must also be administered with frequent oral intake of
ORS solution or water, at one hour intervals for the next 12 to 24 hours. These immediate
interventions will restore normal levels of fluid and electrolytes in her body, which in turn will
facilitate normal levels of urine output (Harsh & Devgan, 2018).
Question 4
There is a need to recruit a multidisciplinary team comprising of: the pediatrician, a
dietician, a gastroenterologist, the assigned registered nurse, a nephrologist and a general
practitioner (Houston, Gibb & Maitland, 2017). The nurse must replace the any formula feed
solutions with one cup or approximately 250 ml of water or ORS respectively, within intervals of
one hour for the next 12 hours or till the vital signs assessment of Ashanti has been restored to
the white marked ‘prevention values as per the SPOC (Santillanes & Rose, 2018). The nurse
must administer patient centered health literacy to Ashanti’s parents by teaching them on the
management of her condition and the importance of administering homemade, fresh and
hygienic ORS solutions or substitutes like milk or apple juice which has been diluted (Saha,
2018). It has been observed that Ashanti’s mother administered her juice – a drink which may
aggravate her diarrhea and dehydration due to low electrolyte, high sodium content which in
5NURSING CASE STUDY AND TRANSITION TO PRACTICE
turn, facilitates the hygroscopic property of sugar to retain urine as demonstrated in the case
study (Harsh & Devgan, 2018). Thus, the registered nurse as well as the general practitioner may
collaborate to educate Ashanti’s parents on the importance of avoiding any soft drinks or sports
drinks and the need to replace the same with diluted juices or standardized, homemade ORS
solutions to mitigate her diarrhea and dehydration (Paramasivam, Earan, Arunagirinadhan &
Kantamneni, 2017). There is also a need to educate Ashanti’s parents post discharge on the
avoidance of excessive outdoor activity by Ashanti during hot climatic conditions as well as the
importance of drinking fluids and water frequently pre and post activity (Kauna, Sobi, Pameh,
Vince & Duke, 2019).
There is a need for the gastroenterologist to assess the prevalence of any bacterial
infections or gastroenteritis in Ashanti. The gastroenterologist may collaborate with the dietician
and pediatrician to administer a semi solid or soft diet to Ashanti comprising of rice, bananas,
toast and applesauce to relieve her diarrheal symptoms when normal eating patterns will be
introduced (Ali, 2019). Additionally, Ashanti’s diet may be supplemented with zinc or probiotic
rich foods like yoghurt for prevention of diarrheal symptoms (Afroz, 2018).
The above interventions are expected to be administered for the next 12 to 24 hours after
which the registered nurse must reassess Ashanti as per the screening values enlisted on the
SPOC. It is expected these interventions will restore Ashanti’s levels of electrolytes, fluids and
urine output to normal levels. In case of persistent symptoms of decreased urine output, the nurse
and nephrologist may conduct a urine analysis to assess the prevalence of any urinary tract or
microbial infection which may increase risks of renal disorders or decreased urinary output
(Paramasivam, Earan, Arunagirinadhan & Kantamneni, 2017). Ashanti will be discharged only
after demonstrating absence of any symptoms of gastroenteritis or diarrhea and after her
turn, facilitates the hygroscopic property of sugar to retain urine as demonstrated in the case
study (Harsh & Devgan, 2018). Thus, the registered nurse as well as the general practitioner may
collaborate to educate Ashanti’s parents on the importance of avoiding any soft drinks or sports
drinks and the need to replace the same with diluted juices or standardized, homemade ORS
solutions to mitigate her diarrhea and dehydration (Paramasivam, Earan, Arunagirinadhan &
Kantamneni, 2017). There is also a need to educate Ashanti’s parents post discharge on the
avoidance of excessive outdoor activity by Ashanti during hot climatic conditions as well as the
importance of drinking fluids and water frequently pre and post activity (Kauna, Sobi, Pameh,
Vince & Duke, 2019).
There is a need for the gastroenterologist to assess the prevalence of any bacterial
infections or gastroenteritis in Ashanti. The gastroenterologist may collaborate with the dietician
and pediatrician to administer a semi solid or soft diet to Ashanti comprising of rice, bananas,
toast and applesauce to relieve her diarrheal symptoms when normal eating patterns will be
introduced (Ali, 2019). Additionally, Ashanti’s diet may be supplemented with zinc or probiotic
rich foods like yoghurt for prevention of diarrheal symptoms (Afroz, 2018).
The above interventions are expected to be administered for the next 12 to 24 hours after
which the registered nurse must reassess Ashanti as per the screening values enlisted on the
SPOC. It is expected these interventions will restore Ashanti’s levels of electrolytes, fluids and
urine output to normal levels. In case of persistent symptoms of decreased urine output, the nurse
and nephrologist may conduct a urine analysis to assess the prevalence of any urinary tract or
microbial infection which may increase risks of renal disorders or decreased urinary output
(Paramasivam, Earan, Arunagirinadhan & Kantamneni, 2017). Ashanti will be discharged only
after demonstrating absence of any symptoms of gastroenteritis or diarrhea and after her
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING CASE STUDY AND TRANSITION TO PRACTICE
symptoms have progressed to the mild dehydration or complete rehydrated stage. Ashanti may
also be discharged after she has not reported any profuse gastrointestinal losses and has reported
normal passage of urine within the last 4 hours (NSW Government, 2019). Additionally,
Ashanti’s parents will be taught by the nurse on correct preparation and administration of ORS
as well as on the need to follow up within 48 hours in case of any deteriorations. It is only after
her parents have successfully learned and demonstrated these skills will Ashanti be discharged
(Ali, 2019).
symptoms have progressed to the mild dehydration or complete rehydrated stage. Ashanti may
also be discharged after she has not reported any profuse gastrointestinal losses and has reported
normal passage of urine within the last 4 hours (NSW Government, 2019). Additionally,
Ashanti’s parents will be taught by the nurse on correct preparation and administration of ORS
as well as on the need to follow up within 48 hours in case of any deteriorations. It is only after
her parents have successfully learned and demonstrated these skills will Ashanti be discharged
(Ali, 2019).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING CASE STUDY AND TRANSITION TO PRACTICE
References
Afroz, S. (2018). Use of improperly mixed oral rehydration salts (ORS) and hypernatraemia in
children–A burning issue. Paed Neph J. Bang, 3(2), 77-82. Retrieved from:
http://mail.pnsbbd.org/asset/borcheure/Banner_1547712988.pdf#page=23.
Ali, R. (2019). The Use of Probiotic with ORS and ORS Only in Children with Acute
Diarrhea. Journal of the College of Physicians and Surgeons Pakistan, 29(12), 1179-
1182. Retrieved from: https://jcpsp.pk/archive/2019/Dec2019/11.pdf.
CEC. (2020). Between The Flags - Clinical Excellence Commission. Retrieved 7 March 2020,
from http://cec.health.nsw.gov.au/keep-patients-safe/Deteriorating-patients/between-the-
flags.
CEC. (2020). Clinical Handover - Clinical Excellence Commission. Retrieved 7 March 2020,
from http://cec.health.nsw.gov.au/improve-quality/team-stripes/clinical-handover.
CEC. (2020). Paediatrics - Clinical Excellence Commission. Retrieved 7 March 2020, from
http://www.cec.health.nsw.gov.au/keep-patients-safe/Deteriorating-patients/between-the-
flags/Paediatrics.
Falszewska, A., Dziechciarz, P., & Szajewska, H. (2017). Diagnostic accuracy of clinical
dehydration scales in children. European journal of pediatrics, 176(8), 1021-1026. doi:
https://doi.org/10.1007/s00431-017-2942-8.
Harsh, P., & Devgan, A. (2018). A Neonate with Hypernatremic Dehydration. Journal of Case
Reports, 8(1), 80-82. doi: http://dx.doi.org/10.17659/01.2018.0021.
References
Afroz, S. (2018). Use of improperly mixed oral rehydration salts (ORS) and hypernatraemia in
children–A burning issue. Paed Neph J. Bang, 3(2), 77-82. Retrieved from:
http://mail.pnsbbd.org/asset/borcheure/Banner_1547712988.pdf#page=23.
Ali, R. (2019). The Use of Probiotic with ORS and ORS Only in Children with Acute
Diarrhea. Journal of the College of Physicians and Surgeons Pakistan, 29(12), 1179-
1182. Retrieved from: https://jcpsp.pk/archive/2019/Dec2019/11.pdf.
CEC. (2020). Between The Flags - Clinical Excellence Commission. Retrieved 7 March 2020,
from http://cec.health.nsw.gov.au/keep-patients-safe/Deteriorating-patients/between-the-
flags.
CEC. (2020). Clinical Handover - Clinical Excellence Commission. Retrieved 7 March 2020,
from http://cec.health.nsw.gov.au/improve-quality/team-stripes/clinical-handover.
CEC. (2020). Paediatrics - Clinical Excellence Commission. Retrieved 7 March 2020, from
http://www.cec.health.nsw.gov.au/keep-patients-safe/Deteriorating-patients/between-the-
flags/Paediatrics.
Falszewska, A., Dziechciarz, P., & Szajewska, H. (2017). Diagnostic accuracy of clinical
dehydration scales in children. European journal of pediatrics, 176(8), 1021-1026. doi:
https://doi.org/10.1007/s00431-017-2942-8.
Harsh, P., & Devgan, A. (2018). A Neonate with Hypernatremic Dehydration. Journal of Case
Reports, 8(1), 80-82. doi: http://dx.doi.org/10.17659/01.2018.0021.
8NURSING CASE STUDY AND TRANSITION TO PRACTICE
Houston, K. A., Gibb, J. G., & Maitland, K. (2017). Oral rehydration of malnourished children
with diarrhoea and dehydration: A systematic review. Wellcome open research, 2. doi:
https://dx.doi.org/10.12688%2Fwellcomeopenres.12357.3.
Kauna, R., Sobi, K., Pameh, W., Vince, J. D., & Duke, T. (2019). Oral Rehydration in Children
with Acute Diarrhoea and Moderate Dehydration—Effectiveness of an ORS Tolerance
Test. Journal of tropical pediatrics, 65(6), 583-591. doi:
https://doi.org/10.1093/tropej/fmz017.
Levine, A. C., Glavis‐Bloom, J., Modi, P., Nasrin, S., Atika, B., Rege, S., ... & Alam, N. H.
(2017). External Validation of the DHAKA Score for Diagnosing Severe Dehydration in
Children with Acute Diarrhea in Resource‐limited Settings. Academic Emergency
Medicine, 24(4), 501-501. doi: https://doi.org/10.1111/acem.13076.
NSW Government. (2014). Infants and Children: Management of Acute Gastroenteritis, Fourth
Edition. Retrieved 7 March 2020, from
https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2014_024.pdf.
Paramasivam, P., Earan, S. K., Arunagirinadhan, A., & Kantamneni, S. (2017). Life Threatening
Severe Hypernatraemic Dehydration in Neonates: A Report of Two Cases. Journal of
clinical and diagnostic research: JCDR, 11(7), SD10. doi:
https://dx.doi.org/10.7860%2FJCDR%2F2017%2F25312.10298.
Saha, A. (2018). Clinical Scales for Assessment of Dehydration in Children with
Diarrhea. Indian Pediatr, 55, 513-518. Retrieved from:
https://indianpediatrics.net/june2018/june-513-518.htm.
Houston, K. A., Gibb, J. G., & Maitland, K. (2017). Oral rehydration of malnourished children
with diarrhoea and dehydration: A systematic review. Wellcome open research, 2. doi:
https://dx.doi.org/10.12688%2Fwellcomeopenres.12357.3.
Kauna, R., Sobi, K., Pameh, W., Vince, J. D., & Duke, T. (2019). Oral Rehydration in Children
with Acute Diarrhoea and Moderate Dehydration—Effectiveness of an ORS Tolerance
Test. Journal of tropical pediatrics, 65(6), 583-591. doi:
https://doi.org/10.1093/tropej/fmz017.
Levine, A. C., Glavis‐Bloom, J., Modi, P., Nasrin, S., Atika, B., Rege, S., ... & Alam, N. H.
(2017). External Validation of the DHAKA Score for Diagnosing Severe Dehydration in
Children with Acute Diarrhea in Resource‐limited Settings. Academic Emergency
Medicine, 24(4), 501-501. doi: https://doi.org/10.1111/acem.13076.
NSW Government. (2014). Infants and Children: Management of Acute Gastroenteritis, Fourth
Edition. Retrieved 7 March 2020, from
https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2014_024.pdf.
Paramasivam, P., Earan, S. K., Arunagirinadhan, A., & Kantamneni, S. (2017). Life Threatening
Severe Hypernatraemic Dehydration in Neonates: A Report of Two Cases. Journal of
clinical and diagnostic research: JCDR, 11(7), SD10. doi:
https://dx.doi.org/10.7860%2FJCDR%2F2017%2F25312.10298.
Saha, A. (2018). Clinical Scales for Assessment of Dehydration in Children with
Diarrhea. Indian Pediatr, 55, 513-518. Retrieved from:
https://indianpediatrics.net/june2018/june-513-518.htm.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING CASE STUDY AND TRANSITION TO PRACTICE
Santillanes, G., & Rose, E. (2018). Evaluation and management of dehydration in
children. Emergency Medicine Clinics, 36(2), 259-273. doi:
https://doi.org/10.1016/j.emc.2017.12.004.
Santillanes, G., & Rose, E. (2018). Evaluation and management of dehydration in
children. Emergency Medicine Clinics, 36(2), 259-273. doi:
https://doi.org/10.1016/j.emc.2017.12.004.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





