Clinical Reasoning Report: Asthma Patient - Nursing Care Plan
VerifiedAdded on 2022/09/05
|13
|2750
|15
Report
AI Summary
This report provides a clinical reasoning analysis of a 25-year-old asthma patient who presented to the emergency room experiencing an asthma attack. The report details the patient's subjective and objective data, including his history of asthma, work environment as a carpenter, and current symptoms such as a tight chest, wheezing, and cyanosis. The analysis relates the patient's condition to his work environment and lack of preventative medication, inferring potential causes and predicting the severity of the attack if left untreated. The report identifies the primary problem as ineffective breathing and establishes goals to address this, outlining actions such as monitoring respiratory rate, oxygen saturation, and arterial blood gases. The justification for oxygen therapy is provided, along with strengths and weaknesses of the nursing interventions, and a reflection on the case using the clinical reasoning cycle to improve future patient care. The report highlights the importance of continuous patient assessment and feedback for optimal outcomes.

Clinical Reasoning 1
Clinical Reasoning for Asthma Patient
Name of Student
Name of Professor
Date
\
Clinical Reasoning for Asthma Patient
Name of Student
Name of Professor
Date
\
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning 2
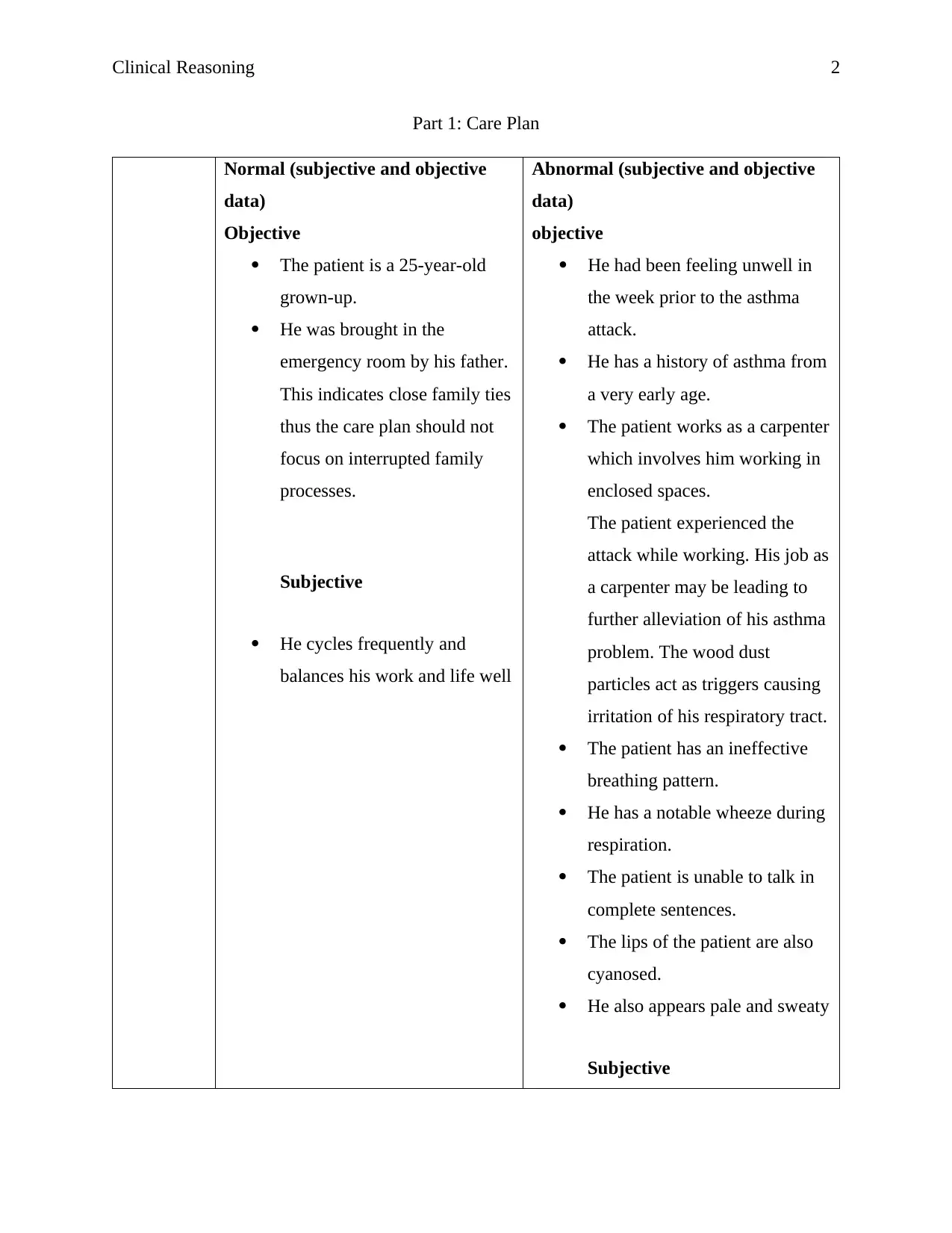
Part 1: Care Plan
Normal (subjective and objective
data)
Objective
The patient is a 25-year-old
grown-up.
He was brought in the
emergency room by his father.
This indicates close family ties
thus the care plan should not
focus on interrupted family
processes.
Subjective
He cycles frequently and
balances his work and life well
Abnormal (subjective and objective
data)
objective
He had been feeling unwell in
the week prior to the asthma
attack.
He has a history of asthma from
a very early age.
The patient works as a carpenter
which involves him working in
enclosed spaces.
The patient experienced the
attack while working. His job as
a carpenter may be leading to
further alleviation of his asthma
problem. The wood dust
particles act as triggers causing
irritation of his respiratory tract.
The patient has an ineffective
breathing pattern.
He has a notable wheeze during
respiration.
The patient is unable to talk in
complete sentences.
The lips of the patient are also
cyanosed.
He also appears pale and sweaty
Subjective
Part 1: Care Plan
Normal (subjective and objective
data)
Objective
The patient is a 25-year-old
grown-up.
He was brought in the
emergency room by his father.
This indicates close family ties
thus the care plan should not
focus on interrupted family
processes.
Subjective
He cycles frequently and
balances his work and life well
Abnormal (subjective and objective
data)
objective
He had been feeling unwell in
the week prior to the asthma
attack.
He has a history of asthma from
a very early age.
The patient works as a carpenter
which involves him working in
enclosed spaces.
The patient experienced the
attack while working. His job as
a carpenter may be leading to
further alleviation of his asthma
problem. The wood dust
particles act as triggers causing
irritation of his respiratory tract.
The patient has an ineffective
breathing pattern.
He has a notable wheeze during
respiration.
The patient is unable to talk in
complete sentences.
The lips of the patient are also
cyanosed.
He also appears pale and sweaty
Subjective
Clinical Reasoning 3
He has a tight chest.
The patient also states that he
has a persistent cough.
The patient also reported much
more regular use of his puffer
than normal and has also ceased
using his preventer.
He is unable to schedule a
meeting with his GP because of
his busy schedule.
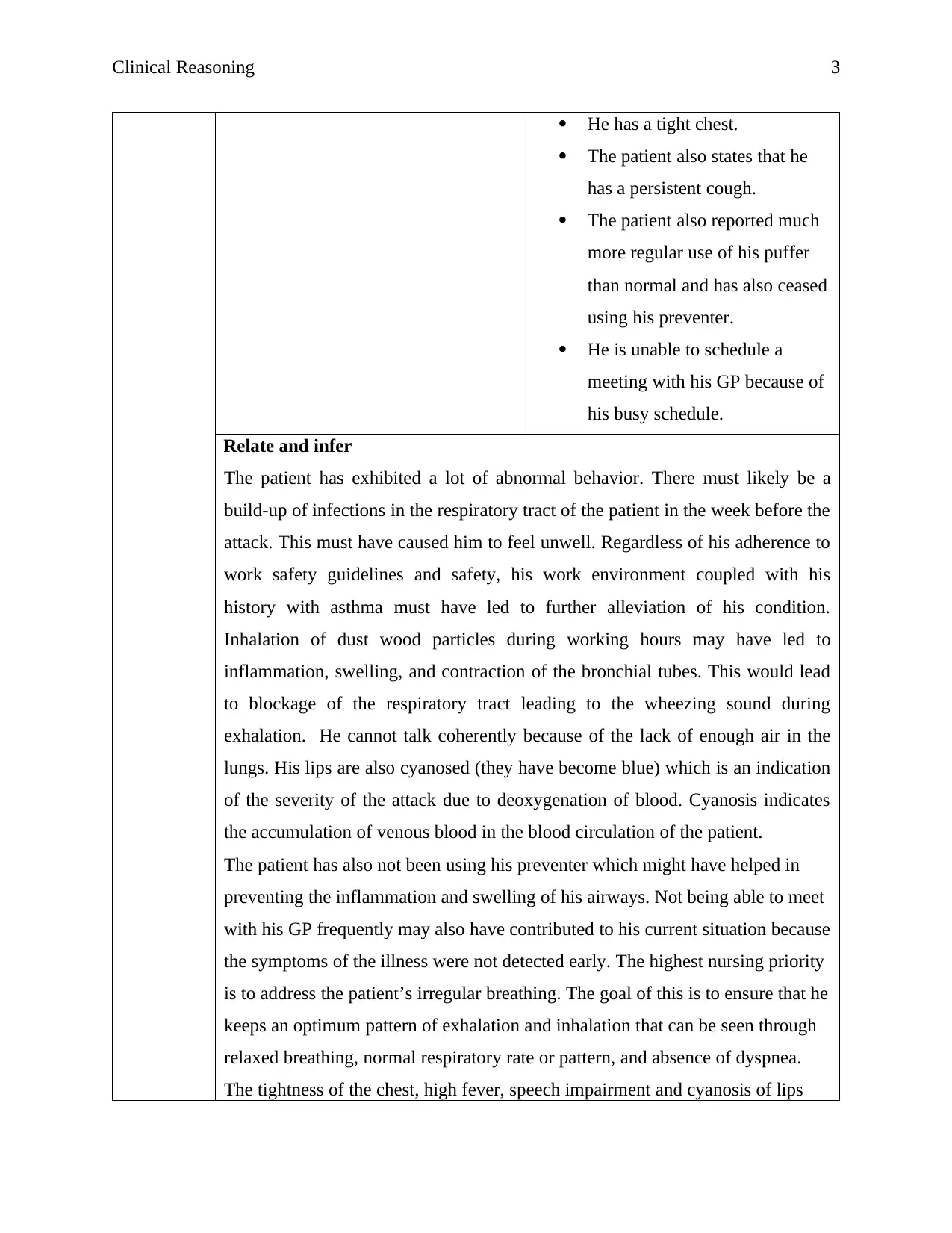
Relate and infer
The patient has exhibited a lot of abnormal behavior. There must likely be a
build-up of infections in the respiratory tract of the patient in the week before the
attack. This must have caused him to feel unwell. Regardless of his adherence to
work safety guidelines and safety, his work environment coupled with his
history with asthma must have led to further alleviation of his condition.
Inhalation of dust wood particles during working hours may have led to
inflammation, swelling, and contraction of the bronchial tubes. This would lead
to blockage of the respiratory tract leading to the wheezing sound during
exhalation. He cannot talk coherently because of the lack of enough air in the
lungs. His lips are also cyanosed (they have become blue) which is an indication
of the severity of the attack due to deoxygenation of blood. Cyanosis indicates
the accumulation of venous blood in the blood circulation of the patient.
The patient has also not been using his preventer which might have helped in
preventing the inflammation and swelling of his airways. Not being able to meet
with his GP frequently may also have contributed to his current situation because
the symptoms of the illness were not detected early. The highest nursing priority
is to address the patient’s irregular breathing. The goal of this is to ensure that he
keeps an optimum pattern of exhalation and inhalation that can be seen through
relaxed breathing, normal respiratory rate or pattern, and absence of dyspnea.
The tightness of the chest, high fever, speech impairment and cyanosis of lips
He has a tight chest.
The patient also states that he
has a persistent cough.
The patient also reported much
more regular use of his puffer
than normal and has also ceased
using his preventer.
He is unable to schedule a
meeting with his GP because of
his busy schedule.
Relate and infer
The patient has exhibited a lot of abnormal behavior. There must likely be a
build-up of infections in the respiratory tract of the patient in the week before the
attack. This must have caused him to feel unwell. Regardless of his adherence to
work safety guidelines and safety, his work environment coupled with his
history with asthma must have led to further alleviation of his condition.
Inhalation of dust wood particles during working hours may have led to
inflammation, swelling, and contraction of the bronchial tubes. This would lead
to blockage of the respiratory tract leading to the wheezing sound during
exhalation. He cannot talk coherently because of the lack of enough air in the
lungs. His lips are also cyanosed (they have become blue) which is an indication
of the severity of the attack due to deoxygenation of blood. Cyanosis indicates
the accumulation of venous blood in the blood circulation of the patient.
The patient has also not been using his preventer which might have helped in
preventing the inflammation and swelling of his airways. Not being able to meet
with his GP frequently may also have contributed to his current situation because
the symptoms of the illness were not detected early. The highest nursing priority
is to address the patient’s irregular breathing. The goal of this is to ensure that he
keeps an optimum pattern of exhalation and inhalation that can be seen through
relaxed breathing, normal respiratory rate or pattern, and absence of dyspnea.
The tightness of the chest, high fever, speech impairment and cyanosis of lips
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical Reasoning 4
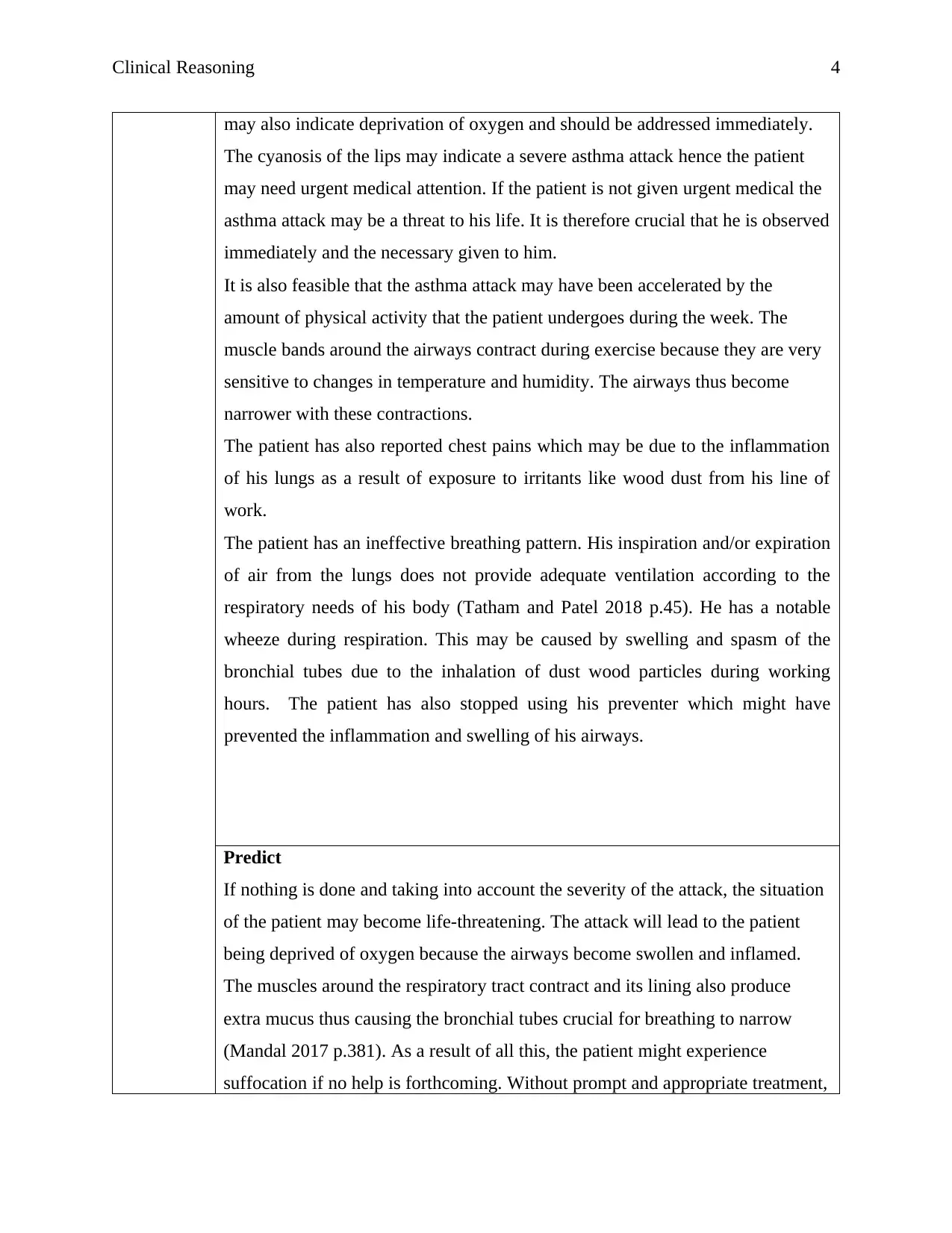
may also indicate deprivation of oxygen and should be addressed immediately.
The cyanosis of the lips may indicate a severe asthma attack hence the patient
may need urgent medical attention. If the patient is not given urgent medical the
asthma attack may be a threat to his life. It is therefore crucial that he is observed
immediately and the necessary given to him.
It is also feasible that the asthma attack may have been accelerated by the
amount of physical activity that the patient undergoes during the week. The
muscle bands around the airways contract during exercise because they are very
sensitive to changes in temperature and humidity. The airways thus become
narrower with these contractions.
The patient has also reported chest pains which may be due to the inflammation
of his lungs as a result of exposure to irritants like wood dust from his line of
work.
The patient has an ineffective breathing pattern. His inspiration and/or expiration
of air from the lungs does not provide adequate ventilation according to the
respiratory needs of his body (Tatham and Patel 2018 p.45). He has a notable
wheeze during respiration. This may be caused by swelling and spasm of the
bronchial tubes due to the inhalation of dust wood particles during working
hours. The patient has also stopped using his preventer which might have
prevented the inflammation and swelling of his airways.
Predict
If nothing is done and taking into account the severity of the attack, the situation
of the patient may become life-threatening. The attack will lead to the patient
being deprived of oxygen because the airways become swollen and inflamed.
The muscles around the respiratory tract contract and its lining also produce
extra mucus thus causing the bronchial tubes crucial for breathing to narrow
(Mandal 2017 p.381). As a result of all this, the patient might experience
suffocation if no help is forthcoming. Without prompt and appropriate treatment,
may also indicate deprivation of oxygen and should be addressed immediately.
The cyanosis of the lips may indicate a severe asthma attack hence the patient
may need urgent medical attention. If the patient is not given urgent medical the
asthma attack may be a threat to his life. It is therefore crucial that he is observed
immediately and the necessary given to him.
It is also feasible that the asthma attack may have been accelerated by the
amount of physical activity that the patient undergoes during the week. The
muscle bands around the airways contract during exercise because they are very
sensitive to changes in temperature and humidity. The airways thus become
narrower with these contractions.
The patient has also reported chest pains which may be due to the inflammation
of his lungs as a result of exposure to irritants like wood dust from his line of
work.
The patient has an ineffective breathing pattern. His inspiration and/or expiration
of air from the lungs does not provide adequate ventilation according to the
respiratory needs of his body (Tatham and Patel 2018 p.45). He has a notable
wheeze during respiration. This may be caused by swelling and spasm of the
bronchial tubes due to the inhalation of dust wood particles during working
hours. The patient has also stopped using his preventer which might have
prevented the inflammation and swelling of his airways.
Predict
If nothing is done and taking into account the severity of the attack, the situation
of the patient may become life-threatening. The attack will lead to the patient
being deprived of oxygen because the airways become swollen and inflamed.
The muscles around the respiratory tract contract and its lining also produce
extra mucus thus causing the bronchial tubes crucial for breathing to narrow
(Mandal 2017 p.381). As a result of all this, the patient might experience
suffocation if no help is forthcoming. Without prompt and appropriate treatment,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning 5
the asthma attack may result in respiratory arrest due to ventilatory failure and
death. Thus, the attack will prove to be fatal if the patient is not afforded
immediate medical care.
Because the patient has been feeling unwell for a week, it can be deduced that
there has been a slow onset of the disease. There is the development of
hypercapnic respiratory failure and mixed acidosis which may lead to the patient
succumbing to asphyxia if he is not afforded urgent medical care.
Identify
the
problem/s
The expiration and inspiration of the patient especially the wheezing
sound made during exhalation patient’s expiration and inspiration
especially the wheezing sound made during exhalation.
Ineffective airway clearance.
Establish
Goal and
Take
Action
Problem Goal Related
actions
Rationale Evaluate
outcomes
The
highest
nursing
priority is
to address
the
irregular
breathing
of the
patient.
The main goal
is to ensure that
the patient’s
expiration is
brought back to
optimal
breathing
pattern which
is evidenced by
relaxed
breathing and
absence of
wheezing
during
Evaluate
the rate,
depth, and
pattern of
respiration
of the
patient.
This can be
done using
a
spirometer
(Koltowski
et al.,
2019). This
Impending
respiratory
distress can be
inferred from
changes in the
rate and pattern
of respiration
The respiratory
rate and rhythm
of the patient
should be stable
and regular.
(Levett-Jones
2018 p.7).
the asthma attack may result in respiratory arrest due to ventilatory failure and
death. Thus, the attack will prove to be fatal if the patient is not afforded
immediate medical care.
Because the patient has been feeling unwell for a week, it can be deduced that
there has been a slow onset of the disease. There is the development of
hypercapnic respiratory failure and mixed acidosis which may lead to the patient
succumbing to asphyxia if he is not afforded urgent medical care.
Identify
the
problem/s
The expiration and inspiration of the patient especially the wheezing
sound made during exhalation patient’s expiration and inspiration
especially the wheezing sound made during exhalation.
Ineffective airway clearance.
Establish
Goal and
Take
Action
Problem Goal Related
actions
Rationale Evaluate
outcomes
The
highest
nursing
priority is
to address
the
irregular
breathing
of the
patient.
The main goal
is to ensure that
the patient’s
expiration is
brought back to
optimal
breathing
pattern which
is evidenced by
relaxed
breathing and
absence of
wheezing
during
Evaluate
the rate,
depth, and
pattern of
respiration
of the
patient.
This can be
done using
a
spirometer
(Koltowski
et al.,
2019). This
Impending
respiratory
distress can be
inferred from
changes in the
rate and pattern
of respiration
The respiratory
rate and rhythm
of the patient
should be stable
and regular.
(Levett-Jones
2018 p.7).
Clinical Reasoning 6
expiration. measures
the volume
of air
inhaled and
exhaled
during
breathing
and then
analyzing
the
changing
volumes
over time.
Evaluate
the sounds
made when
breathing
and other
adventitious
sounds such
as wheezes
and stridor
(Rubner et
al., 2017)
This may
be done
using
spirometry.
The
improvement
or decline of
the situation
might be
inferred from
this. It might
also indicate
the onset and/or
development of
further related
complications
like pneumonia
(Levy et al.
2016 p.1872).
The respiratory
tract should be
cleared to ensure
the clear
breathing of the
patient.
Achievement of
a return to
normal
inhalation and
exhalation
shows
improvement in
the condition of
the patient.
expiration. measures
the volume
of air
inhaled and
exhaled
during
breathing
and then
analyzing
the
changing
volumes
over time.
Evaluate
the sounds
made when
breathing
and other
adventitious
sounds such
as wheezes
and stridor
(Rubner et
al., 2017)
This may
be done
using
spirometry.
The
improvement
or decline of
the situation
might be
inferred from
this. It might
also indicate
the onset and/or
development of
further related
complications
like pneumonia
(Levy et al.
2016 p.1872).
The respiratory
tract should be
cleared to ensure
the clear
breathing of the
patient.
Achievement of
a return to
normal
inhalation and
exhalation
shows
improvement in
the condition of
the patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical Reasoning 7
This is a
test that is
used to
measure the
amount of
air that can
be exhaled
or inhaled
by a patient.
Wheezing
happens as a
result of the
contraction of
the bronchial
tubes.
Diminishing
wheezing and
indistinct
breath sounds
may also
suggest
impending
respiratory
failure.
If the values
found by the
spirometry test
are lower than
normal, it can
be inferred that
the patient has
impaired
respiratory
function.
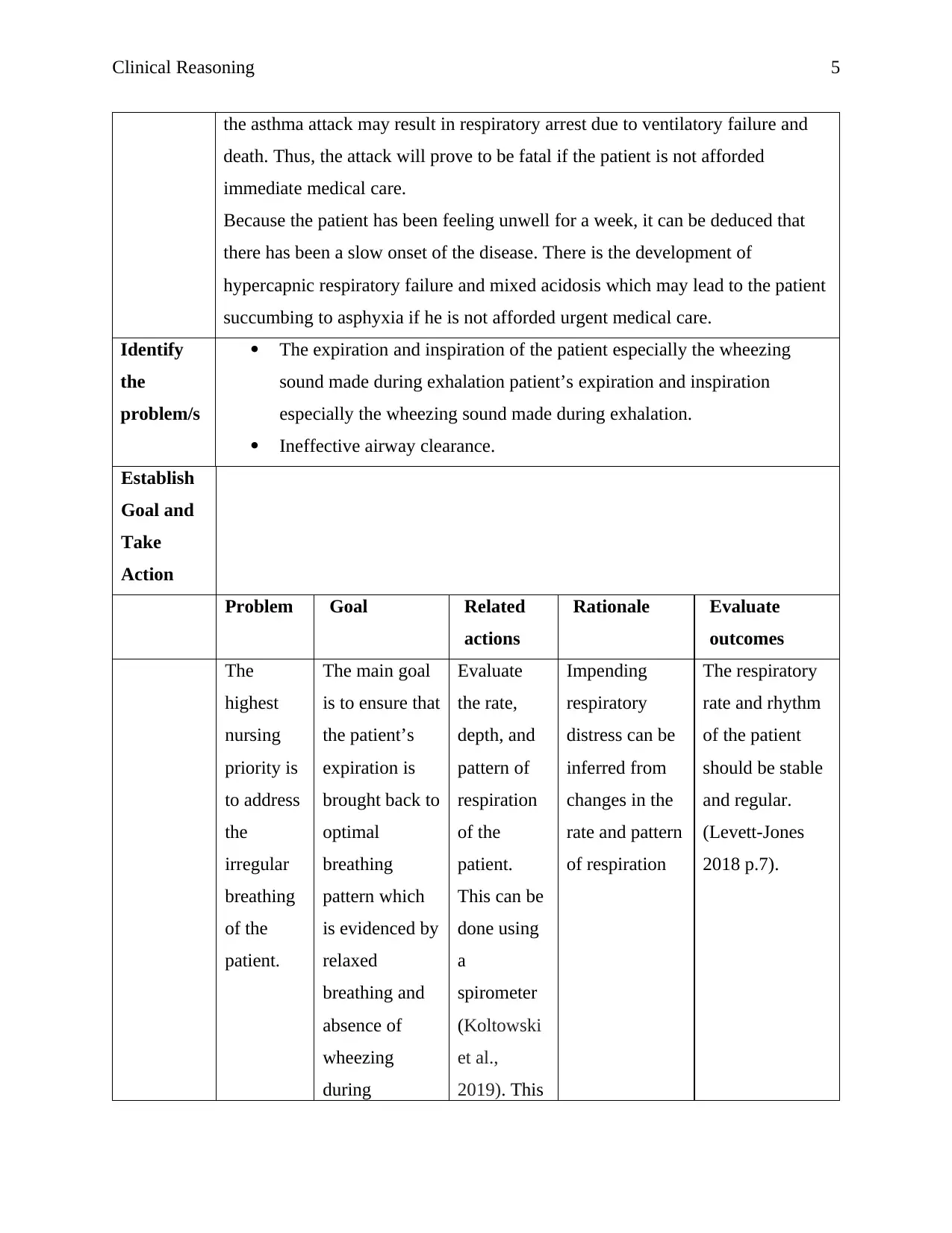
Monitor
oxygen
saturation
(Sundbom
et al.,
Oxygen
saturation
refers to the
fraction of
oxygen
Performing
oxygen therapy
on the patient
should improve
his oxygen
This is a
test that is
used to
measure the
amount of
air that can
be exhaled
or inhaled
by a patient.
Wheezing
happens as a
result of the
contraction of
the bronchial
tubes.
Diminishing
wheezing and
indistinct
breath sounds
may also
suggest
impending
respiratory
failure.
If the values
found by the
spirometry test
are lower than
normal, it can
be inferred that
the patient has
impaired
respiratory
function.
Monitor
oxygen
saturation
(Sundbom
et al.,
Oxygen
saturation
refers to the
fraction of
oxygen
Performing
oxygen therapy
on the patient
should improve
his oxygen
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning 8
2018). This
is done
using a
pulse
oximeter. It
is a non-
invasive
test that
measures
the oxygen
saturation
in the
patient’s
blood.
saturated
hemoglobin
relative to the
total
hemoglobin in
the blood.
Normal oxygen
saturation
levels are
considered to
be about 95%-
100%. The
pulse oximeter
test is useful in
monitoring the
oxygen level of
the patient and
also helps to
evaluate
whether the
condition of the
patient is
improving or
worsening.
Very low
oxygen levels
are an
indication that
the patient
needs urgent
medical help.
saturation. The
cyanosis of the
lips should
subside with
increase
oxidation of the
patient’s blood.
It would also
help the patient
to improve his
coherence which
might likely be
caused by lack
of enough air.
The patient
should therefore
be able to talk
more clearly.
His chest pains
should also
subside with
additional
oxidation.
2018). This
is done
using a
pulse
oximeter. It
is a non-
invasive
test that
measures
the oxygen
saturation
in the
patient’s
blood.
saturated
hemoglobin
relative to the
total
hemoglobin in
the blood.
Normal oxygen
saturation
levels are
considered to
be about 95%-
100%. The
pulse oximeter
test is useful in
monitoring the
oxygen level of
the patient and
also helps to
evaluate
whether the
condition of the
patient is
improving or
worsening.
Very low
oxygen levels
are an
indication that
the patient
needs urgent
medical help.
saturation. The
cyanosis of the
lips should
subside with
increase
oxidation of the
patient’s blood.
It would also
help the patient
to improve his
coherence which
might likely be
caused by lack
of enough air.
The patient
should therefore
be able to talk
more clearly.
His chest pains
should also
subside with
additional
oxidation.
Clinical Reasoning 9
Monitor
arterial
blood gases
(ABG)
This is done
using a
minimally
invasive blood
test where
blood is drawn
from an artery
of the patient.
The test may be
used to
measure the
oxygen level,
pH of blood,
the level of
carbon dioxide,
and bicarbonate
level.
Patients might
develop
respiratory
alkalosis during
a mild to
moderate
asthma attack.
Hypoxemia
leads to
increased
respiratory rate
and depth, and
carbon dioxide
is blown off
The arterial
blood gases
value obtained
are used to
evaluate the
severity of the
asthma attack.
The arterial
blood gases of
the patient
should improve
to more
optimum levels.
Monitor
arterial
blood gases
(ABG)
This is done
using a
minimally
invasive blood
test where
blood is drawn
from an artery
of the patient.
The test may be
used to
measure the
oxygen level,
pH of blood,
the level of
carbon dioxide,
and bicarbonate
level.
Patients might
develop
respiratory
alkalosis during
a mild to
moderate
asthma attack.
Hypoxemia
leads to
increased
respiratory rate
and depth, and
carbon dioxide
is blown off
The arterial
blood gases
value obtained
are used to
evaluate the
severity of the
asthma attack.
The arterial
blood gases of
the patient
should improve
to more
optimum levels.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical Reasoning 10
(Wiestra et al.
2018).
Respiratory
acidosis usually
indicates that
respiratory
failure is
imminent and
that mechanical
ventilation is
necessary.
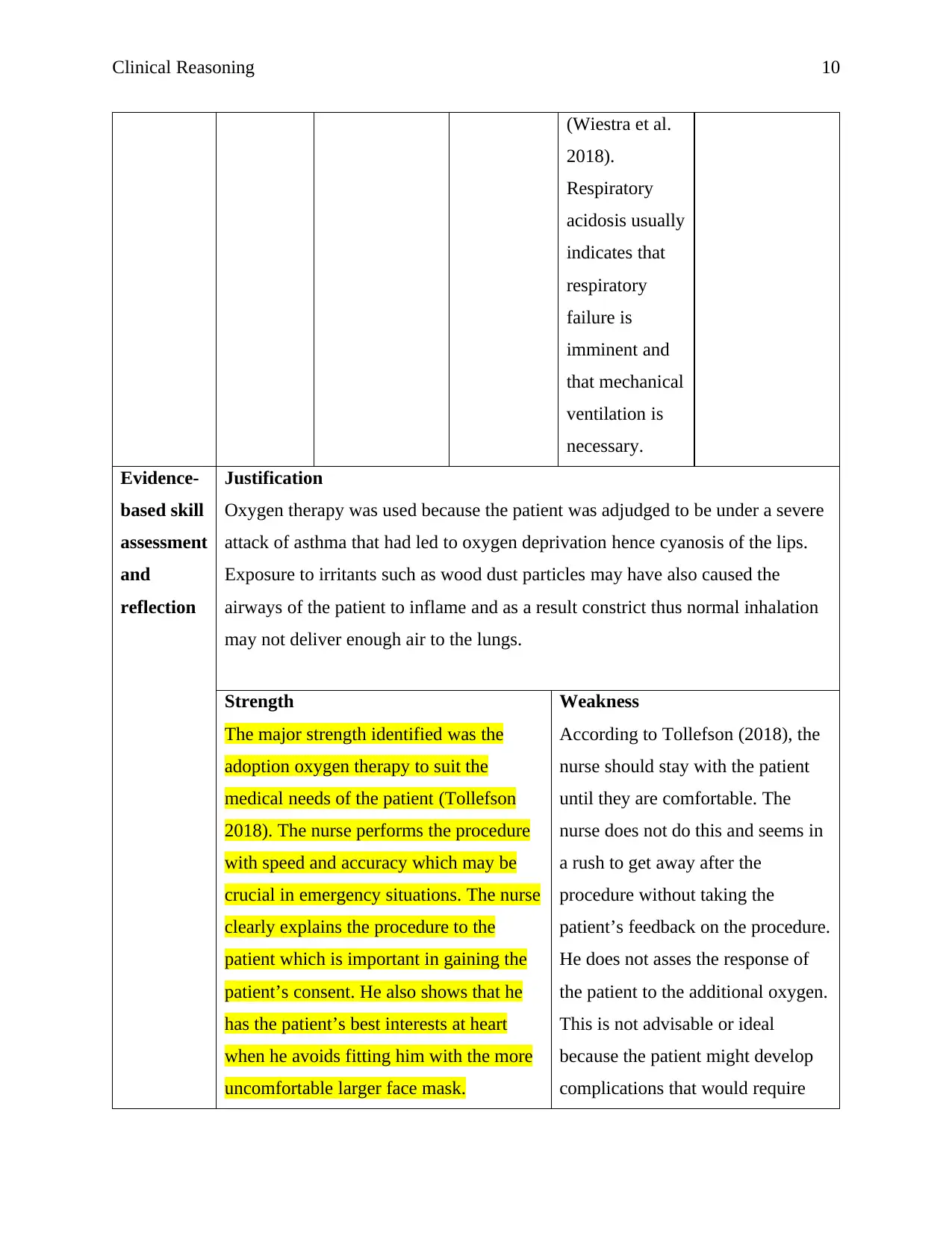
Evidence-
based skill
assessment
and
reflection
Justification
Oxygen therapy was used because the patient was adjudged to be under a severe
attack of asthma that had led to oxygen deprivation hence cyanosis of the lips.
Exposure to irritants such as wood dust particles may have also caused the
airways of the patient to inflame and as a result constrict thus normal inhalation
may not deliver enough air to the lungs.
Strength
The major strength identified was the
adoption oxygen therapy to suit the
medical needs of the patient (Tollefson
2018). The nurse performs the procedure
with speed and accuracy which may be
crucial in emergency situations. The nurse
clearly explains the procedure to the
patient which is important in gaining the
patient’s consent. He also shows that he
has the patient’s best interests at heart
when he avoids fitting him with the more
uncomfortable larger face mask.
Weakness
According to Tollefson (2018), the
nurse should stay with the patient
until they are comfortable. The
nurse does not do this and seems in
a rush to get away after the
procedure without taking the
patient’s feedback on the procedure.
He does not asses the response of
the patient to the additional oxygen.
This is not advisable or ideal
because the patient might develop
complications that would require
(Wiestra et al.
2018).
Respiratory
acidosis usually
indicates that
respiratory
failure is
imminent and
that mechanical
ventilation is
necessary.
Evidence-
based skill
assessment
and
reflection
Justification
Oxygen therapy was used because the patient was adjudged to be under a severe
attack of asthma that had led to oxygen deprivation hence cyanosis of the lips.
Exposure to irritants such as wood dust particles may have also caused the
airways of the patient to inflame and as a result constrict thus normal inhalation
may not deliver enough air to the lungs.
Strength
The major strength identified was the
adoption oxygen therapy to suit the
medical needs of the patient (Tollefson
2018). The nurse performs the procedure
with speed and accuracy which may be
crucial in emergency situations. The nurse
clearly explains the procedure to the
patient which is important in gaining the
patient’s consent. He also shows that he
has the patient’s best interests at heart
when he avoids fitting him with the more
uncomfortable larger face mask.
Weakness
According to Tollefson (2018), the
nurse should stay with the patient
until they are comfortable. The
nurse does not do this and seems in
a rush to get away after the
procedure without taking the
patient’s feedback on the procedure.
He does not asses the response of
the patient to the additional oxygen.
This is not advisable or ideal
because the patient might develop
complications that would require
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning 11
the nurse to be around.
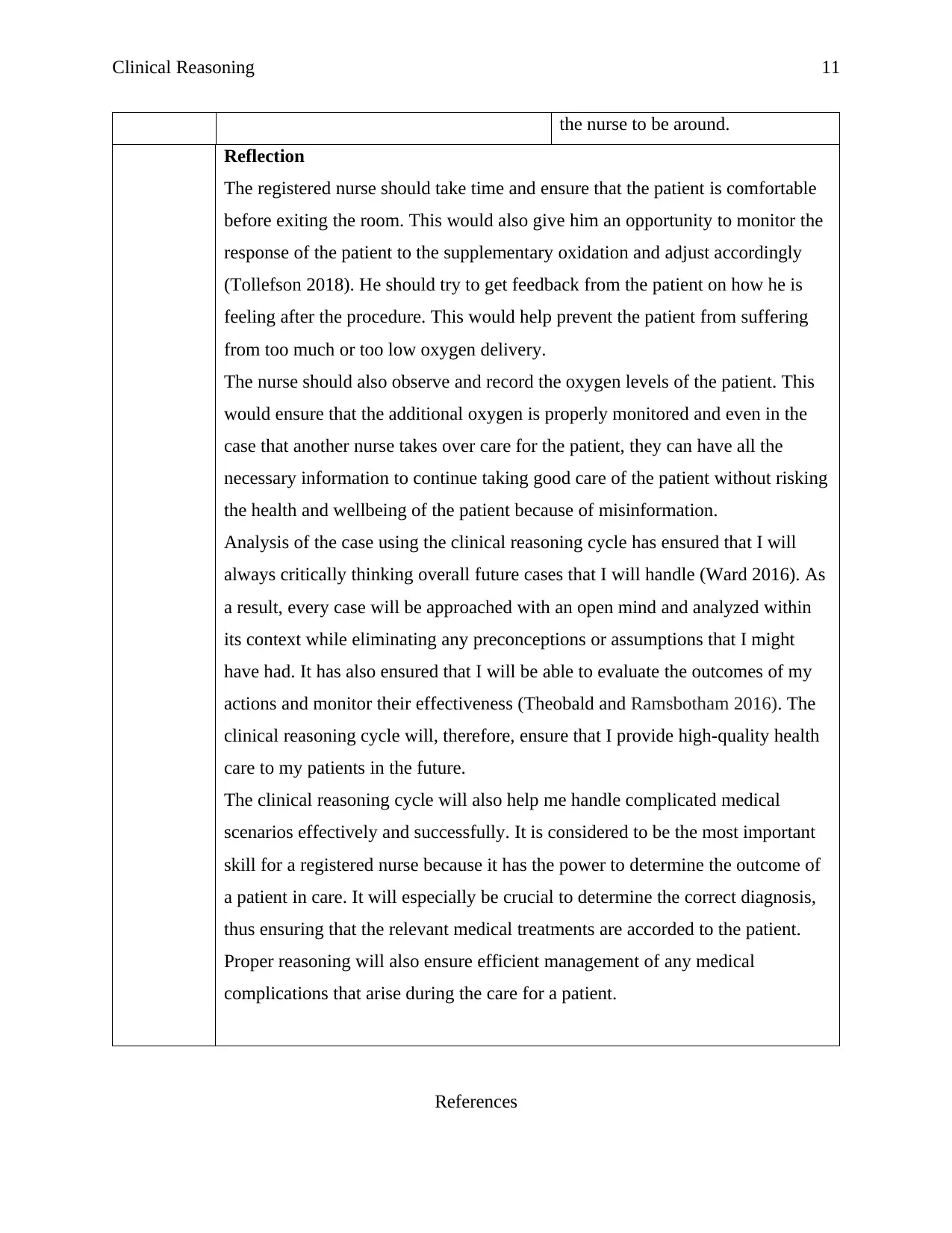
Reflection
The registered nurse should take time and ensure that the patient is comfortable
before exiting the room. This would also give him an opportunity to monitor the
response of the patient to the supplementary oxidation and adjust accordingly
(Tollefson 2018). He should try to get feedback from the patient on how he is
feeling after the procedure. This would help prevent the patient from suffering
from too much or too low oxygen delivery.
The nurse should also observe and record the oxygen levels of the patient. This
would ensure that the additional oxygen is properly monitored and even in the
case that another nurse takes over care for the patient, they can have all the
necessary information to continue taking good care of the patient without risking
the health and wellbeing of the patient because of misinformation.
Analysis of the case using the clinical reasoning cycle has ensured that I will
always critically thinking overall future cases that I will handle (Ward 2016). As
a result, every case will be approached with an open mind and analyzed within
its context while eliminating any preconceptions or assumptions that I might
have had. It has also ensured that I will be able to evaluate the outcomes of my
actions and monitor their effectiveness (Theobald and Ramsbotham 2016). The
clinical reasoning cycle will, therefore, ensure that I provide high-quality health
care to my patients in the future.
The clinical reasoning cycle will also help me handle complicated medical
scenarios effectively and successfully. It is considered to be the most important
skill for a registered nurse because it has the power to determine the outcome of
a patient in care. It will especially be crucial to determine the correct diagnosis,
thus ensuring that the relevant medical treatments are accorded to the patient.
Proper reasoning will also ensure efficient management of any medical
complications that arise during the care for a patient.
References
the nurse to be around.
Reflection
The registered nurse should take time and ensure that the patient is comfortable
before exiting the room. This would also give him an opportunity to monitor the
response of the patient to the supplementary oxidation and adjust accordingly
(Tollefson 2018). He should try to get feedback from the patient on how he is
feeling after the procedure. This would help prevent the patient from suffering
from too much or too low oxygen delivery.
The nurse should also observe and record the oxygen levels of the patient. This
would ensure that the additional oxygen is properly monitored and even in the
case that another nurse takes over care for the patient, they can have all the
necessary information to continue taking good care of the patient without risking
the health and wellbeing of the patient because of misinformation.
Analysis of the case using the clinical reasoning cycle has ensured that I will
always critically thinking overall future cases that I will handle (Ward 2016). As
a result, every case will be approached with an open mind and analyzed within
its context while eliminating any preconceptions or assumptions that I might
have had. It has also ensured that I will be able to evaluate the outcomes of my
actions and monitor their effectiveness (Theobald and Ramsbotham 2016). The
clinical reasoning cycle will, therefore, ensure that I provide high-quality health
care to my patients in the future.
The clinical reasoning cycle will also help me handle complicated medical
scenarios effectively and successfully. It is considered to be the most important
skill for a registered nurse because it has the power to determine the outcome of
a patient in care. It will especially be crucial to determine the correct diagnosis,
thus ensuring that the relevant medical treatments are accorded to the patient.
Proper reasoning will also ensure efficient management of any medical
complications that arise during the care for a patient.
References
Clinical Reasoning 12
Koltowski, L., Hofman, A., Kupczyk, M., Kuna, P., &# 321; ukaszyk, M., Buczy&# 322; ko, K.,
D&# 261; browiecki, P., Bodzenta-&# 321; ukaszyk, A., Nasta&# 322; ek, P. and Soli&# 324;
ski, M., 2019. Self-Monitoring of Lung Function in Mild Asthma Patients Using Connected
Mobile Spirometry System-Feasibility Study. In B37. NOVEL APPROACHES TO ASTHMA
MANAGEMENT AND OUTCOMES (pp. A3036-A3036). American Thoracic Society.
Levett-Jones, T., Courtney-Pratt, H. and Govind, N., 2018. Implementation and Evaluation of the
Post-Practicum Oral Clinical Reasoning Exam. In Augmenting Health and Social Care Students’
Clinical Learning Experiences (pp. 5-13). Springer, Cham.
Levy, S.D., Alladina, J.W., Hibbert, K.A., Harris, R.S., Bajwa, E.K. and Hess, D.R., 2016. High-
flow oxygen therapy and other inhaled therapies in intensive care units. The Lancet, 387(10030),
pp.1867-1878.
Mandal, S., 2017. Acute asthma. Acute Medicine: A Practical Guide to the Management of
Medical Emergencies, pp.378-383.
Rubner, F.J., Jackson, D.J., Evans, M.D., Gangnon, R.E., Tisler, C.J., Pappas, T.E., Gern, J.E.
and Lemanske Jr, R.F., 2017. Early life rhinovirus wheezing, allergic sensitization, and asthma
risk at adolescence. Journal of Allergy and Clinical Immunology, 139(2), pp.501-507.
Sundbom, F., Janson, C., Malinovschi, A. and Lindberg, E., 2018. Effects of coexisting asthma
and obstructive sleep apnea on sleep architecture, oxygen saturation, and systemic inflammation
in women. Journal of Clinical Sleep Medicine, 14(02), pp.253-259.
Theobald, K.A. and Ramsbotham, J., 2019. Inquiry-based learning and clinical reasoning
scaffolds: An action research project to support undergraduate students' learning to ‘think like a
nurse’. Nurse education in practice.
Tatham, K. and Patel, K., 2018. Examination: Respiratory. In Complete OSCE Skills for Medical
and Surgical Finals (pp. 43-58). CRC Press.
Tollefson, J., 2018. Clinical Psychomotor Skills (3-Point): Assessment Tools for Nurses.
Cengage AU.
Ward, T.D., 2016. Think Like a Nurse: A Critical Thinking Initiative. ABNF Journal, 27(3).
Koltowski, L., Hofman, A., Kupczyk, M., Kuna, P., &# 321; ukaszyk, M., Buczy&# 322; ko, K.,
D&# 261; browiecki, P., Bodzenta-&# 321; ukaszyk, A., Nasta&# 322; ek, P. and Soli&# 324;
ski, M., 2019. Self-Monitoring of Lung Function in Mild Asthma Patients Using Connected
Mobile Spirometry System-Feasibility Study. In B37. NOVEL APPROACHES TO ASTHMA
MANAGEMENT AND OUTCOMES (pp. A3036-A3036). American Thoracic Society.
Levett-Jones, T., Courtney-Pratt, H. and Govind, N., 2018. Implementation and Evaluation of the
Post-Practicum Oral Clinical Reasoning Exam. In Augmenting Health and Social Care Students’
Clinical Learning Experiences (pp. 5-13). Springer, Cham.
Levy, S.D., Alladina, J.W., Hibbert, K.A., Harris, R.S., Bajwa, E.K. and Hess, D.R., 2016. High-
flow oxygen therapy and other inhaled therapies in intensive care units. The Lancet, 387(10030),
pp.1867-1878.
Mandal, S., 2017. Acute asthma. Acute Medicine: A Practical Guide to the Management of
Medical Emergencies, pp.378-383.
Rubner, F.J., Jackson, D.J., Evans, M.D., Gangnon, R.E., Tisler, C.J., Pappas, T.E., Gern, J.E.
and Lemanske Jr, R.F., 2017. Early life rhinovirus wheezing, allergic sensitization, and asthma
risk at adolescence. Journal of Allergy and Clinical Immunology, 139(2), pp.501-507.
Sundbom, F., Janson, C., Malinovschi, A. and Lindberg, E., 2018. Effects of coexisting asthma
and obstructive sleep apnea on sleep architecture, oxygen saturation, and systemic inflammation
in women. Journal of Clinical Sleep Medicine, 14(02), pp.253-259.
Theobald, K.A. and Ramsbotham, J., 2019. Inquiry-based learning and clinical reasoning
scaffolds: An action research project to support undergraduate students' learning to ‘think like a
nurse’. Nurse education in practice.
Tatham, K. and Patel, K., 2018. Examination: Respiratory. In Complete OSCE Skills for Medical
and Surgical Finals (pp. 43-58). CRC Press.
Tollefson, J., 2018. Clinical Psychomotor Skills (3-Point): Assessment Tools for Nurses.
Cengage AU.
Ward, T.D., 2016. Think Like a Nurse: A Critical Thinking Initiative. ABNF Journal, 27(3).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





