Nursing Assignment: Diabetes Care, Management and Interventions
VerifiedAdded on 2022/11/25
|20
|4728
|401
Homework Assignment
AI Summary
This assignment comprehensively addresses various aspects of diabetes care. It begins by examining common pathological indicators and emergency nursing interventions for conditions like hypoglycemia, hyperglycemia, ketoacidosis, and Hyperosmolar Hyperglycemic Syndrome (HHS). The assignment then delves into potential problems and preventive nursing interventions for health issues such as retinopathy, infections, and psychosocial issues. It also explores microvascular and macrovascular diseases associated with diabetes. Furthermore, the assignment discusses the role of family/carer understanding in diabetes management, environmental and social factors contributing to diabetes within the general Australian population, and specific factors affecting Aboriginal and/or Torres Strait Islander people. The assignment also addresses issues in diabetic care delivery in Australia and includes a detailed case study of a 52-year-old Aboriginal woman with type 2 diabetes, including a daily care plan, blood test interpretation, a management plan, and evidence-based practice considerations.
0
Diabetes
Diabetes
JULY 13, 2019
Student Details:
Diabetes
Diabetes
JULY 13, 2019
Student Details:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
Diabetes
Contents
Diabetes......................................................................................................................................2
1a. Common pathological indicators and emergency nursing interventions..........................2
1b. The potential problems for each of the following conditions and 2 nursing interventions
for prevention.........................................................................................................................5
2. Role of family/carer understanding about diabetes in the planning and implementation of
devised plan for diabetic person.............................................................................................7
3. Two environmental and social factors within the general population of Australia that
contributes to diabetes............................................................................................................7
4. Three factors experienced by Aboriginal and/or Torres Strait Islander people that may
contribute to their higher rates of diabetes.............................................................................8
5. Three issues relating to diabetic care delivery or services in Australia.........................8
6. Case Study..........................................................................................................................8
6a. Daily care plan from the information in the case study................................................9
6b. Evaluation and interpretation Kerry’s blood tests within this case study...................13
6c. Management plan........................................................................................................13
6d. Evidence-based practice relating to chosen Kerry’s outcomes as noted in the
management plan in Q6c..................................................................................................15
References................................................................................................................................16
Diabetes
Contents
Diabetes......................................................................................................................................2
1a. Common pathological indicators and emergency nursing interventions..........................2
1b. The potential problems for each of the following conditions and 2 nursing interventions
for prevention.........................................................................................................................5
2. Role of family/carer understanding about diabetes in the planning and implementation of
devised plan for diabetic person.............................................................................................7
3. Two environmental and social factors within the general population of Australia that
contributes to diabetes............................................................................................................7
4. Three factors experienced by Aboriginal and/or Torres Strait Islander people that may
contribute to their higher rates of diabetes.............................................................................8
5. Three issues relating to diabetic care delivery or services in Australia.........................8
6. Case Study..........................................................................................................................8
6a. Daily care plan from the information in the case study................................................9
6b. Evaluation and interpretation Kerry’s blood tests within this case study...................13
6c. Management plan........................................................................................................13
6d. Evidence-based practice relating to chosen Kerry’s outcomes as noted in the
management plan in Q6c..................................................................................................15
References................................................................................................................................16
2
Diabetes
Diabetes
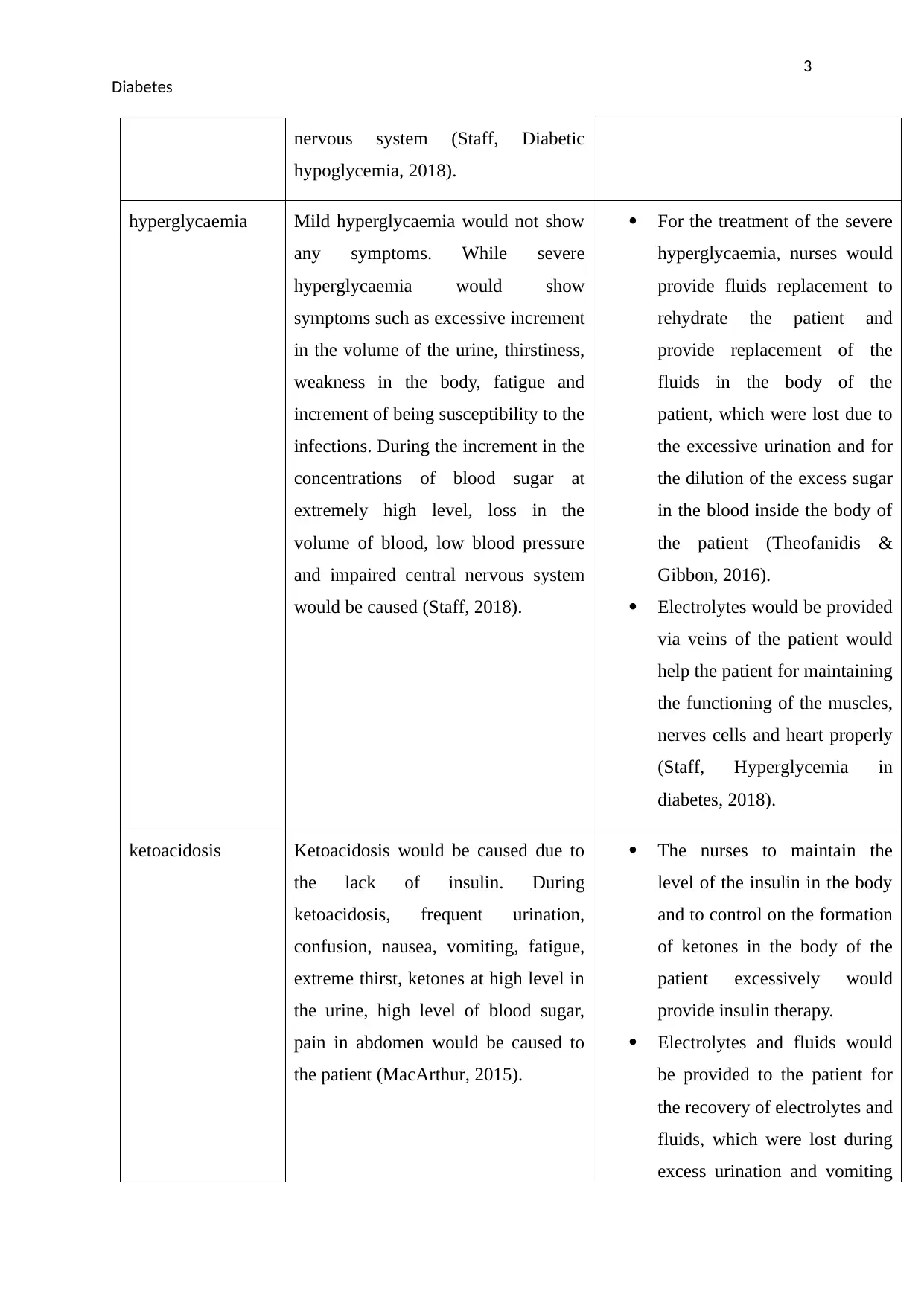
1a. Common pathological indicators and emergency nursing interventions
Condition Most common pathological indicator
of the condition
Discuss 2 emergency nursing
interventions for each condition you
may assist with under the guidance of
an RN.
hypoglycaemia Range of blood glucose lowering
would be from 60-70 mg/ml to less
than 40 mg/ml form mild
hypoglycaemia to severe
hypoglycaemia. Mild hypoglycaemia
would lead to the symptoms named
hunger, tremor, rapid pulse, anxiety
and fatigue and known to be
sympathoadrenal symptoms due to the
activation of these symptoms from the
sympathetic nervous system and
adrenal medulla. During the sleep,
diabetic hypoglycaemia can takes
place. During night many symptoms
takes place named as damp cloths and
bedclothes because of perspiration,
irritation during waking and
nightmares. Severe hypoglycaemia
would lead to the symptoms such as
blurred vision, unconsciousness and
impaired thinking, seizures, coma and
confusion and these symptoms known
as neurological symptoms due to the
occurrence of signs from the brain and
The nurses would follow 15-15
rule during nursing
intervention.
Carbohydrate would be
provided with the amount of 15
gram and then after 15
minutes, this would provide
increment about 75 mg/dL in
the plasma glucose within 15
minutes (Barbara, 2017).
In the severe hypoglycaemia,
nurses would provide
injections of glucagon for
providing increment for
glucose due to the inability of
the patients to swallow.
Because glucagon leads to the
stimulation for the release of
the glucose by the liver.
(Bilhimer, Treu, & Acquisto,
2017).
Diabetes
Diabetes
1a. Common pathological indicators and emergency nursing interventions
Condition Most common pathological indicator
of the condition
Discuss 2 emergency nursing
interventions for each condition you
may assist with under the guidance of
an RN.
hypoglycaemia Range of blood glucose lowering
would be from 60-70 mg/ml to less
than 40 mg/ml form mild
hypoglycaemia to severe
hypoglycaemia. Mild hypoglycaemia
would lead to the symptoms named
hunger, tremor, rapid pulse, anxiety
and fatigue and known to be
sympathoadrenal symptoms due to the
activation of these symptoms from the
sympathetic nervous system and
adrenal medulla. During the sleep,
diabetic hypoglycaemia can takes
place. During night many symptoms
takes place named as damp cloths and
bedclothes because of perspiration,
irritation during waking and
nightmares. Severe hypoglycaemia
would lead to the symptoms such as
blurred vision, unconsciousness and
impaired thinking, seizures, coma and
confusion and these symptoms known
as neurological symptoms due to the
occurrence of signs from the brain and
The nurses would follow 15-15
rule during nursing
intervention.
Carbohydrate would be
provided with the amount of 15
gram and then after 15
minutes, this would provide
increment about 75 mg/dL in
the plasma glucose within 15
minutes (Barbara, 2017).
In the severe hypoglycaemia,
nurses would provide
injections of glucagon for
providing increment for
glucose due to the inability of
the patients to swallow.
Because glucagon leads to the
stimulation for the release of
the glucose by the liver.
(Bilhimer, Treu, & Acquisto,
2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
Diabetes
nervous system (Staff, Diabetic
hypoglycemia, 2018).
hyperglycaemia Mild hyperglycaemia would not show
any symptoms. While severe
hyperglycaemia would show
symptoms such as excessive increment
in the volume of the urine, thirstiness,
weakness in the body, fatigue and
increment of being susceptibility to the
infections. During the increment in the
concentrations of blood sugar at
extremely high level, loss in the
volume of blood, low blood pressure
and impaired central nervous system
would be caused (Staff, 2018).
For the treatment of the severe
hyperglycaemia, nurses would
provide fluids replacement to
rehydrate the patient and
provide replacement of the
fluids in the body of the
patient, which were lost due to
the excessive urination and for
the dilution of the excess sugar
in the blood inside the body of
the patient (Theofanidis &
Gibbon, 2016).
Electrolytes would be provided
via veins of the patient would
help the patient for maintaining
the functioning of the muscles,
nerves cells and heart properly
(Staff, Hyperglycemia in
diabetes, 2018).
ketoacidosis Ketoacidosis would be caused due to
the lack of insulin. During
ketoacidosis, frequent urination,
confusion, nausea, vomiting, fatigue,
extreme thirst, ketones at high level in
the urine, high level of blood sugar,
pain in abdomen would be caused to
the patient (MacArthur, 2015).
The nurses to maintain the
level of the insulin in the body
and to control on the formation
of ketones in the body of the
patient excessively would
provide insulin therapy.
Electrolytes and fluids would
be provided to the patient for
the recovery of electrolytes and
fluids, which were lost during
excess urination and vomiting
Diabetes
nervous system (Staff, Diabetic
hypoglycemia, 2018).
hyperglycaemia Mild hyperglycaemia would not show
any symptoms. While severe
hyperglycaemia would show
symptoms such as excessive increment
in the volume of the urine, thirstiness,
weakness in the body, fatigue and
increment of being susceptibility to the
infections. During the increment in the
concentrations of blood sugar at
extremely high level, loss in the
volume of blood, low blood pressure
and impaired central nervous system
would be caused (Staff, 2018).
For the treatment of the severe
hyperglycaemia, nurses would
provide fluids replacement to
rehydrate the patient and
provide replacement of the
fluids in the body of the
patient, which were lost due to
the excessive urination and for
the dilution of the excess sugar
in the blood inside the body of
the patient (Theofanidis &
Gibbon, 2016).
Electrolytes would be provided
via veins of the patient would
help the patient for maintaining
the functioning of the muscles,
nerves cells and heart properly
(Staff, Hyperglycemia in
diabetes, 2018).
ketoacidosis Ketoacidosis would be caused due to
the lack of insulin. During
ketoacidosis, frequent urination,
confusion, nausea, vomiting, fatigue,
extreme thirst, ketones at high level in
the urine, high level of blood sugar,
pain in abdomen would be caused to
the patient (MacArthur, 2015).
The nurses to maintain the
level of the insulin in the body
and to control on the formation
of ketones in the body of the
patient excessively would
provide insulin therapy.
Electrolytes and fluids would
be provided to the patient for
the recovery of electrolytes and
fluids, which were lost during
excess urination and vomiting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
Diabetes
(Larson-Williams, et al., 2016).
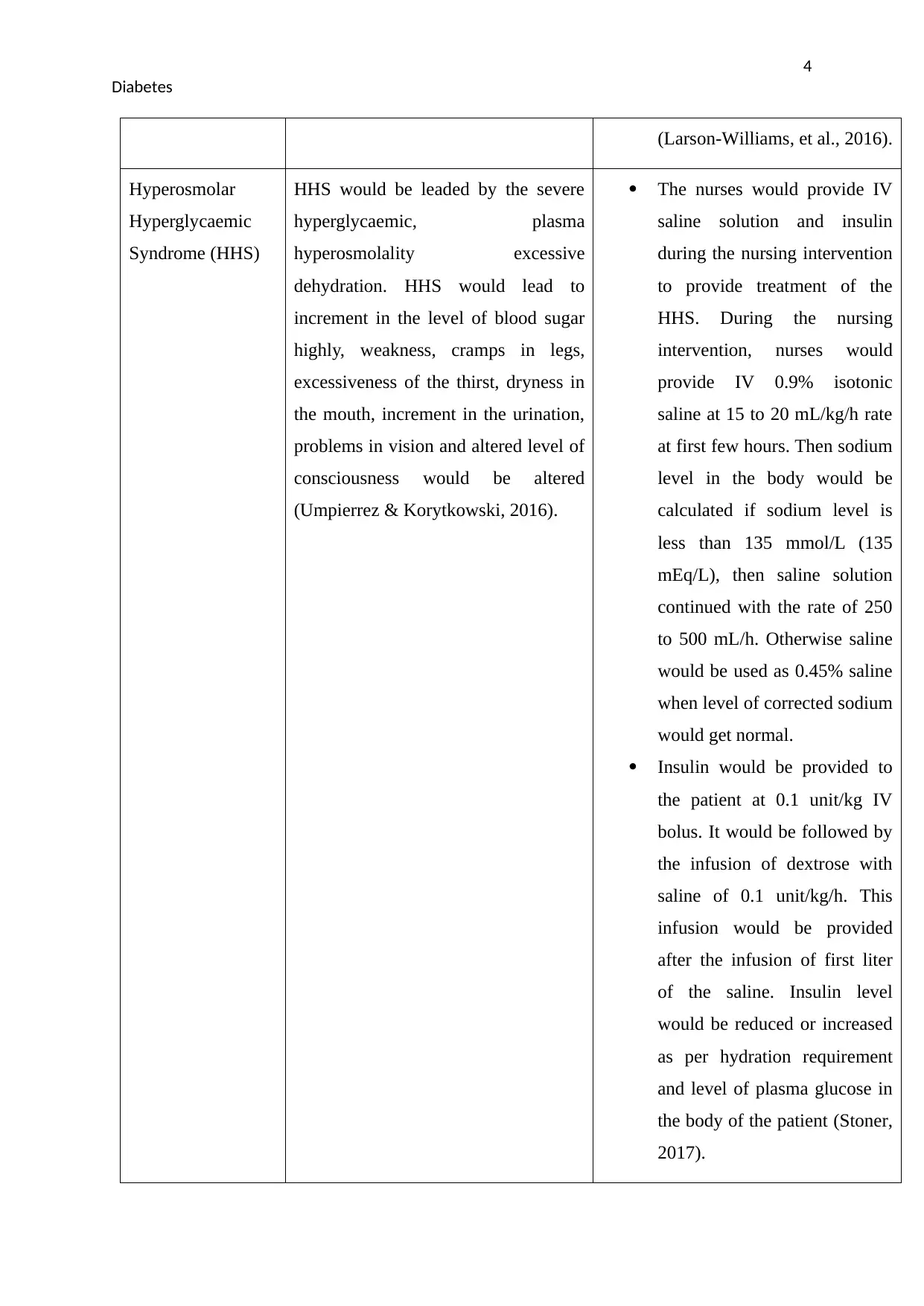
Hyperosmolar
Hyperglycaemic
Syndrome (HHS)
HHS would be leaded by the severe
hyperglycaemic, plasma
hyperosmolality excessive
dehydration. HHS would lead to
increment in the level of blood sugar
highly, weakness, cramps in legs,
excessiveness of the thirst, dryness in
the mouth, increment in the urination,
problems in vision and altered level of
consciousness would be altered
(Umpierrez & Korytkowski, 2016).
The nurses would provide IV
saline solution and insulin
during the nursing intervention
to provide treatment of the
HHS. During the nursing
intervention, nurses would
provide IV 0.9% isotonic
saline at 15 to 20 mL/kg/h rate
at first few hours. Then sodium
level in the body would be
calculated if sodium level is
less than 135 mmol/L (135
mEq/L), then saline solution
continued with the rate of 250
to 500 mL/h. Otherwise saline
would be used as 0.45% saline
when level of corrected sodium
would get normal.
Insulin would be provided to
the patient at 0.1 unit/kg IV
bolus. It would be followed by
the infusion of dextrose with
saline of 0.1 unit/kg/h. This
infusion would be provided
after the infusion of first liter
of the saline. Insulin level
would be reduced or increased
as per hydration requirement
and level of plasma glucose in
the body of the patient (Stoner,
2017).
Diabetes
(Larson-Williams, et al., 2016).
Hyperosmolar
Hyperglycaemic
Syndrome (HHS)
HHS would be leaded by the severe
hyperglycaemic, plasma
hyperosmolality excessive
dehydration. HHS would lead to
increment in the level of blood sugar
highly, weakness, cramps in legs,
excessiveness of the thirst, dryness in
the mouth, increment in the urination,
problems in vision and altered level of
consciousness would be altered
(Umpierrez & Korytkowski, 2016).
The nurses would provide IV
saline solution and insulin
during the nursing intervention
to provide treatment of the
HHS. During the nursing
intervention, nurses would
provide IV 0.9% isotonic
saline at 15 to 20 mL/kg/h rate
at first few hours. Then sodium
level in the body would be
calculated if sodium level is
less than 135 mmol/L (135
mEq/L), then saline solution
continued with the rate of 250
to 500 mL/h. Otherwise saline
would be used as 0.45% saline
when level of corrected sodium
would get normal.
Insulin would be provided to
the patient at 0.1 unit/kg IV
bolus. It would be followed by
the infusion of dextrose with
saline of 0.1 unit/kg/h. This
infusion would be provided
after the infusion of first liter
of the saline. Insulin level
would be reduced or increased
as per hydration requirement
and level of plasma glucose in
the body of the patient (Stoner,
2017).
5
Diabetes
1b. The potential problems for each of the following conditions and 2 nursing interventions
for prevention
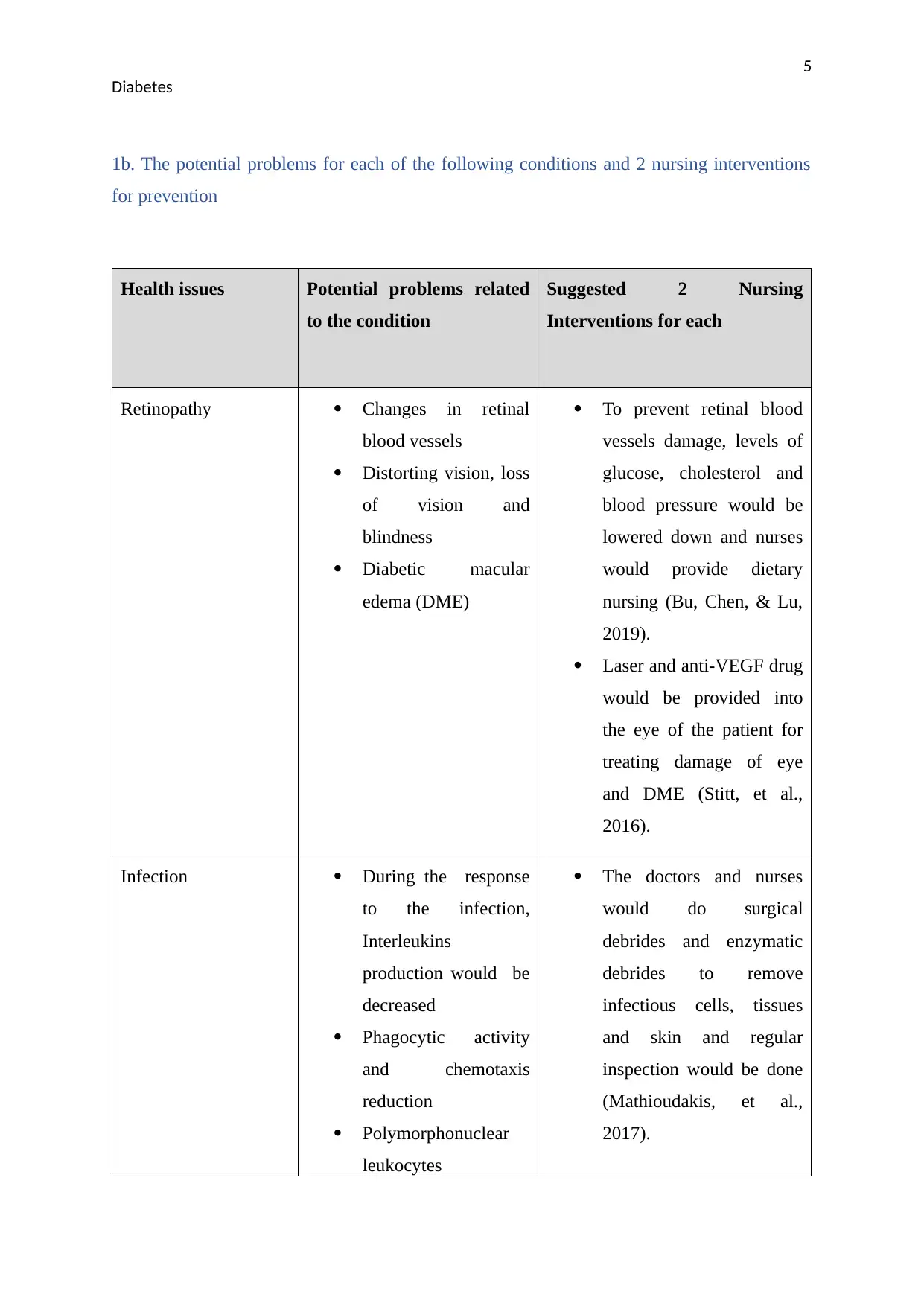
Health issues Potential problems related
to the condition
Suggested 2 Nursing
Interventions for each
Retinopathy Changes in retinal
blood vessels
Distorting vision, loss
of vision and
blindness
Diabetic macular
edema (DME)
To prevent retinal blood
vessels damage, levels of
glucose, cholesterol and
blood pressure would be
lowered down and nurses
would provide dietary
nursing (Bu, Chen, & Lu,
2019).
Laser and anti-VEGF drug
would be provided into
the eye of the patient for
treating damage of eye
and DME (Stitt, et al.,
2016).
Infection During the response
to the infection,
Interleukins
production would be
decreased
Phagocytic activity
and chemotaxis
reduction
Polymorphonuclear
leukocytes
The doctors and nurses
would do surgical
debrides and enzymatic
debrides to remove
infectious cells, tissues
and skin and regular
inspection would be done
(Mathioudakis, et al.,
2017).
Diabetes
1b. The potential problems for each of the following conditions and 2 nursing interventions
for prevention
Health issues Potential problems related
to the condition
Suggested 2 Nursing
Interventions for each
Retinopathy Changes in retinal
blood vessels
Distorting vision, loss
of vision and
blindness
Diabetic macular
edema (DME)
To prevent retinal blood
vessels damage, levels of
glucose, cholesterol and
blood pressure would be
lowered down and nurses
would provide dietary
nursing (Bu, Chen, & Lu,
2019).
Laser and anti-VEGF drug
would be provided into
the eye of the patient for
treating damage of eye
and DME (Stitt, et al.,
2016).
Infection During the response
to the infection,
Interleukins
production would be
decreased
Phagocytic activity
and chemotaxis
reduction
Polymorphonuclear
leukocytes
The doctors and nurses
would do surgical
debrides and enzymatic
debrides to remove
infectious cells, tissues
and skin and regular
inspection would be done
(Mathioudakis, et al.,
2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
Diabetes
immobilization
Glycosuria
Dysmotility in the
gastrointestinal and
urinary tract
(Casqueiro,
Casqueiro, & Alves,
2012`).
Education would be
provided to the patient and
their family to prevent
infectious situation
(Schaper, Netten,
Apelqvist, Lipsky, &
Bakkerr, 2016).
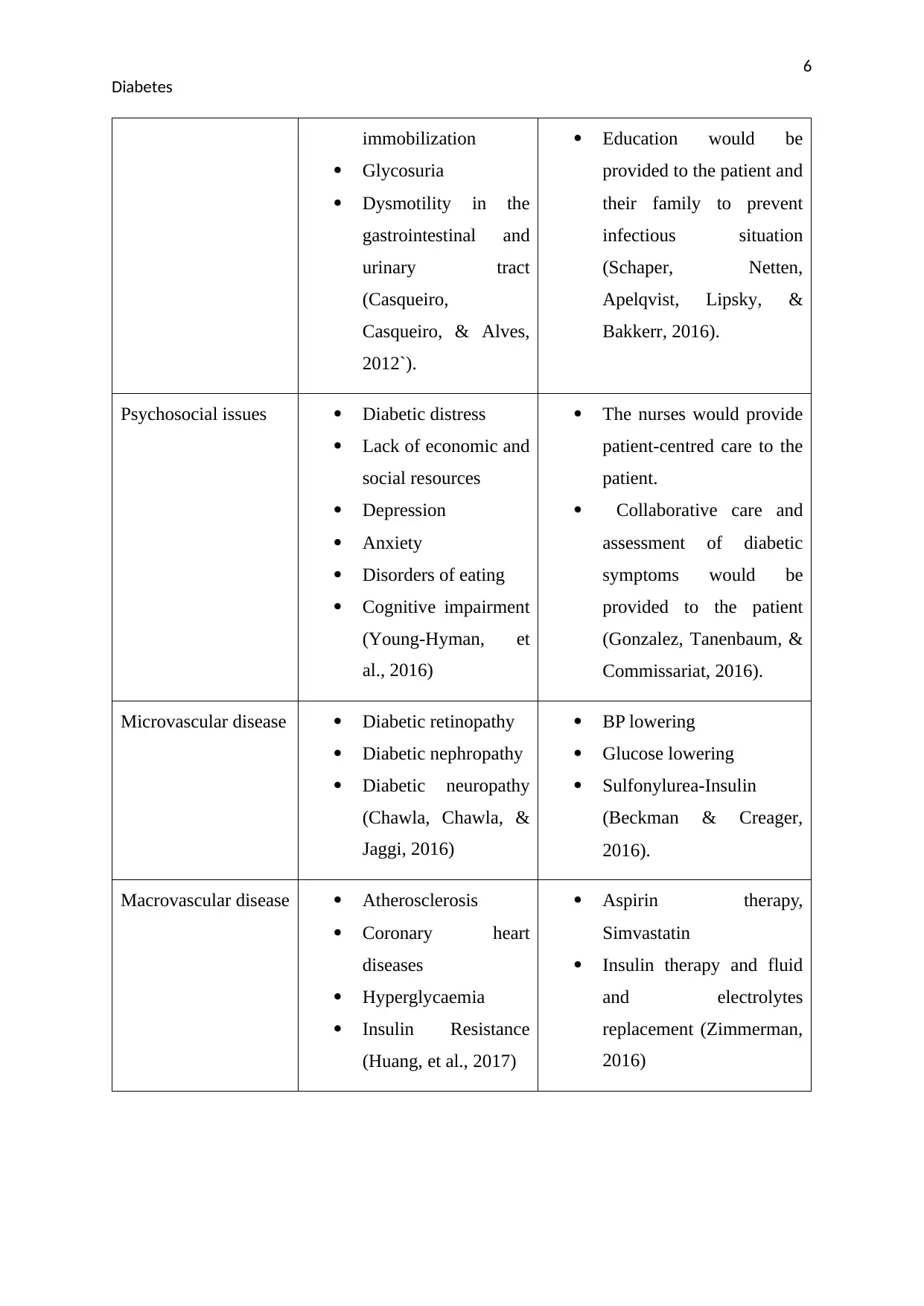
Psychosocial issues Diabetic distress
Lack of economic and
social resources
Depression
Anxiety
Disorders of eating
Cognitive impairment
(Young-Hyman, et
al., 2016)
The nurses would provide
patient-centred care to the
patient.
Collaborative care and
assessment of diabetic
symptoms would be
provided to the patient
(Gonzalez, Tanenbaum, &
Commissariat, 2016).
Microvascular disease Diabetic retinopathy
Diabetic nephropathy
Diabetic neuropathy
(Chawla, Chawla, &
Jaggi, 2016)
BP lowering
Glucose lowering
Sulfonylurea-Insulin
(Beckman & Creager,
2016).
Macrovascular disease Atherosclerosis
Coronary heart
diseases
Hyperglycaemia
Insulin Resistance
(Huang, et al., 2017)
Aspirin therapy,
Simvastatin
Insulin therapy and fluid
and electrolytes
replacement (Zimmerman,
2016)
Diabetes
immobilization
Glycosuria
Dysmotility in the
gastrointestinal and
urinary tract
(Casqueiro,
Casqueiro, & Alves,
2012`).
Education would be
provided to the patient and
their family to prevent
infectious situation
(Schaper, Netten,
Apelqvist, Lipsky, &
Bakkerr, 2016).
Psychosocial issues Diabetic distress
Lack of economic and
social resources
Depression
Anxiety
Disorders of eating
Cognitive impairment
(Young-Hyman, et
al., 2016)
The nurses would provide
patient-centred care to the
patient.
Collaborative care and
assessment of diabetic
symptoms would be
provided to the patient
(Gonzalez, Tanenbaum, &
Commissariat, 2016).
Microvascular disease Diabetic retinopathy
Diabetic nephropathy
Diabetic neuropathy
(Chawla, Chawla, &
Jaggi, 2016)
BP lowering
Glucose lowering
Sulfonylurea-Insulin
(Beckman & Creager,
2016).
Macrovascular disease Atherosclerosis
Coronary heart
diseases
Hyperglycaemia
Insulin Resistance
(Huang, et al., 2017)
Aspirin therapy,
Simvastatin
Insulin therapy and fluid
and electrolytes
replacement (Zimmerman,
2016)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
Diabetes
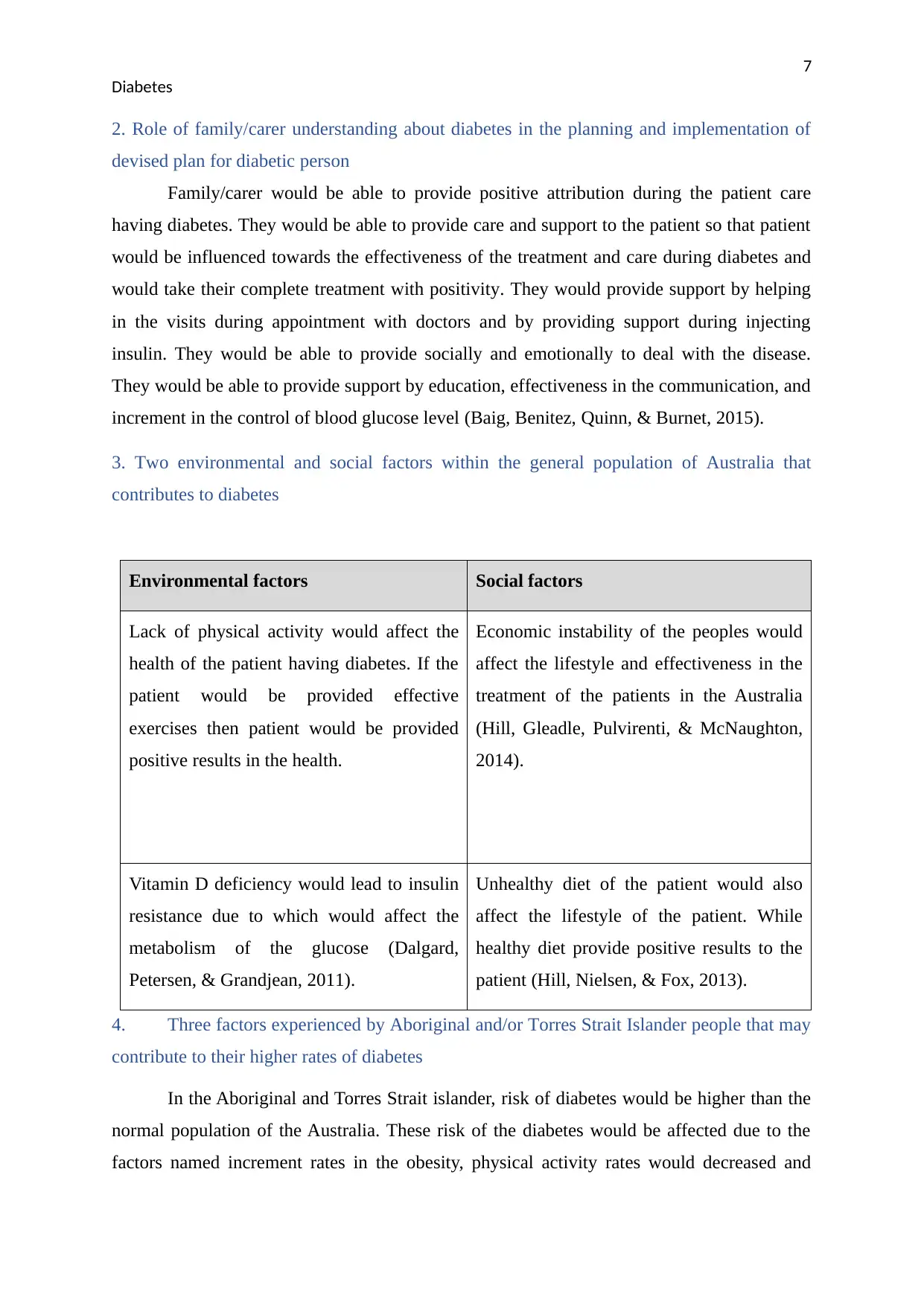
2. Role of family/carer understanding about diabetes in the planning and implementation of
devised plan for diabetic person
Family/carer would be able to provide positive attribution during the patient care
having diabetes. They would be able to provide care and support to the patient so that patient
would be influenced towards the effectiveness of the treatment and care during diabetes and
would take their complete treatment with positivity. They would provide support by helping
in the visits during appointment with doctors and by providing support during injecting
insulin. They would be able to provide socially and emotionally to deal with the disease.
They would be able to provide support by education, effectiveness in the communication, and
increment in the control of blood glucose level (Baig, Benitez, Quinn, & Burnet, 2015).
3. Two environmental and social factors within the general population of Australia that
contributes to diabetes
Environmental factors Social factors
Lack of physical activity would affect the
health of the patient having diabetes. If the
patient would be provided effective
exercises then patient would be provided
positive results in the health.
Economic instability of the peoples would
affect the lifestyle and effectiveness in the
treatment of the patients in the Australia
(Hill, Gleadle, Pulvirenti, & McNaughton,
2014).
Vitamin D deficiency would lead to insulin
resistance due to which would affect the
metabolism of the glucose (Dalgard,
Petersen, & Grandjean, 2011).
Unhealthy diet of the patient would also
affect the lifestyle of the patient. While
healthy diet provide positive results to the
patient (Hill, Nielsen, & Fox, 2013).
4. Three factors experienced by Aboriginal and/or Torres Strait Islander people that may
contribute to their higher rates of diabetes
In the Aboriginal and Torres Strait islander, risk of diabetes would be higher than the
normal population of the Australia. These risk of the diabetes would be affected due to the
factors named increment rates in the obesity, physical activity rates would decreased and
Diabetes
2. Role of family/carer understanding about diabetes in the planning and implementation of
devised plan for diabetic person
Family/carer would be able to provide positive attribution during the patient care
having diabetes. They would be able to provide care and support to the patient so that patient
would be influenced towards the effectiveness of the treatment and care during diabetes and
would take their complete treatment with positivity. They would provide support by helping
in the visits during appointment with doctors and by providing support during injecting
insulin. They would be able to provide socially and emotionally to deal with the disease.
They would be able to provide support by education, effectiveness in the communication, and
increment in the control of blood glucose level (Baig, Benitez, Quinn, & Burnet, 2015).
3. Two environmental and social factors within the general population of Australia that
contributes to diabetes
Environmental factors Social factors
Lack of physical activity would affect the
health of the patient having diabetes. If the
patient would be provided effective
exercises then patient would be provided
positive results in the health.
Economic instability of the peoples would
affect the lifestyle and effectiveness in the
treatment of the patients in the Australia
(Hill, Gleadle, Pulvirenti, & McNaughton,
2014).
Vitamin D deficiency would lead to insulin
resistance due to which would affect the
metabolism of the glucose (Dalgard,
Petersen, & Grandjean, 2011).
Unhealthy diet of the patient would also
affect the lifestyle of the patient. While
healthy diet provide positive results to the
patient (Hill, Nielsen, & Fox, 2013).
4. Three factors experienced by Aboriginal and/or Torres Strait Islander people that may
contribute to their higher rates of diabetes
In the Aboriginal and Torres Strait islander, risk of diabetes would be higher than the
normal population of the Australia. These risk of the diabetes would be affected due to the
factors named increment rates in the obesity, physical activity rates would decreased and
8
Diabetes
changes in the diets of the aboriginal and Torres strait islander. Nowadays these islanders lead
their lifestyle towards the western lifestyle. Due to which they focus on the diet, which would
be low fibrous and having high sugar and fat in their diet. They also adopt alcohol, smoking
cigarette in their lifestyle, which lead to high risk of the diabetes in these peoples (Knibbs &
Sly, 2014).
5. Three issues relating to diabetic care delivery or services in Australia
Three issues named increment in the urbanization, inequity of health in the city and
rural area people and health funds issues lead to the ineffectiveness in the care delivery or
services during diabetes in the Australia. Due to the increment in the urbanization, people
would focus on the diet that would lead to the increment in the rate of being diseased with
obesity. Due to the lack of facilities in the rural areas and due to the financial issues with
them they would not be able to take effective diabetic care delivery (You & Henneberg,
2016).
6. Case Study
Kerry is a 52 y.o. woman of Aboriginal decent. She was diagnosed with type 2
diabetes at the age of 40. She is obese with a BMI of 32.5; she has a history of complications
which include a prior myocardial infarction a year ago with the introduction of a stent, mild
retinopathy and previous foot ulcers.
Kerry has had multiple admissions to a large public hospital for episodes of both hypo
and hyperglycaemia due to poor blood glucose control, her current admission to an acute
medical ward was due to hyperglycaemia. She arrived at emergency feeling nauseous, with a
severe headache and confused.
Pathology is as follows:
BGL reading recorded 27 mmol/litre
HbA1c of 13.1%.
Positive for Ketones in her urinalysis
Her current medication regime was Mixtard 30/70 twice daily.
Diabetes
changes in the diets of the aboriginal and Torres strait islander. Nowadays these islanders lead
their lifestyle towards the western lifestyle. Due to which they focus on the diet, which would
be low fibrous and having high sugar and fat in their diet. They also adopt alcohol, smoking
cigarette in their lifestyle, which lead to high risk of the diabetes in these peoples (Knibbs &
Sly, 2014).
5. Three issues relating to diabetic care delivery or services in Australia
Three issues named increment in the urbanization, inequity of health in the city and
rural area people and health funds issues lead to the ineffectiveness in the care delivery or
services during diabetes in the Australia. Due to the increment in the urbanization, people
would focus on the diet that would lead to the increment in the rate of being diseased with
obesity. Due to the lack of facilities in the rural areas and due to the financial issues with
them they would not be able to take effective diabetic care delivery (You & Henneberg,
2016).
6. Case Study
Kerry is a 52 y.o. woman of Aboriginal decent. She was diagnosed with type 2
diabetes at the age of 40. She is obese with a BMI of 32.5; she has a history of complications
which include a prior myocardial infarction a year ago with the introduction of a stent, mild
retinopathy and previous foot ulcers.
Kerry has had multiple admissions to a large public hospital for episodes of both hypo
and hyperglycaemia due to poor blood glucose control, her current admission to an acute
medical ward was due to hyperglycaemia. She arrived at emergency feeling nauseous, with a
severe headache and confused.
Pathology is as follows:
BGL reading recorded 27 mmol/litre
HbA1c of 13.1%.
Positive for Ketones in her urinalysis
Her current medication regime was Mixtard 30/70 twice daily.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
Diabetes
She was given NovoRapid whilst in emergency and then transferred once she was
stable to ward for further review. Kerry has a IV cannula insitu, therefore she is on a fluid
balance chart.
Kerry is allowed to mobilise with supervision.
Kerry’s condition is further complicated by several social, financial and physical
factors. Her only child whom Kerry gave birth to at 17, died several years ago from a serious
metabolic condition related to diabetes at age 6.
She lives alone in a rented flat and has no immediate family close by so is usually
housebound. Kerry also has a mild learning disability and is stressed, she recently lost her
job in a call centre which she states occurred because of workplace bullying. Shortly after
losing her job she had a car accident which resulted in the loss of her car because she was not
insured.
Furthermore, over the past several weeks she has felt very depressed and said that
when she feels sad she no longer bothers with her medications or recording her BGL’s.
Whilst in hospital Kerry was started on NovoRapid 3 times per day prior to meals and
Lantus at night before bed.
Kerry has been under the care of the diabetic unit at the hospital for the past four
years however her attendance at appointments is very erratic. She is to be seen by the
hospital’s diabetes educator whist in hospital.
6a. Daily care plan from the information in the case study
Unit Record No: 2345678
Surname: Jones
Given Names: Kerry
D.O.B: 23/5/75 _ Sex: F
AFFIX PATIENT IDENTIFICATION LABEL HERE
Diabetes
She was given NovoRapid whilst in emergency and then transferred once she was
stable to ward for further review. Kerry has a IV cannula insitu, therefore she is on a fluid
balance chart.
Kerry is allowed to mobilise with supervision.
Kerry’s condition is further complicated by several social, financial and physical
factors. Her only child whom Kerry gave birth to at 17, died several years ago from a serious
metabolic condition related to diabetes at age 6.
She lives alone in a rented flat and has no immediate family close by so is usually
housebound. Kerry also has a mild learning disability and is stressed, she recently lost her
job in a call centre which she states occurred because of workplace bullying. Shortly after
losing her job she had a car accident which resulted in the loss of her car because she was not
insured.
Furthermore, over the past several weeks she has felt very depressed and said that
when she feels sad she no longer bothers with her medications or recording her BGL’s.
Whilst in hospital Kerry was started on NovoRapid 3 times per day prior to meals and
Lantus at night before bed.
Kerry has been under the care of the diabetic unit at the hospital for the past four
years however her attendance at appointments is very erratic. She is to be seen by the
hospital’s diabetes educator whist in hospital.
6a. Daily care plan from the information in the case study
Unit Record No: 2345678
Surname: Jones
Given Names: Kerry
D.O.B: 23/5/75 _ Sex: F
AFFIX PATIENT IDENTIFICATION LABEL HERE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Diabetes
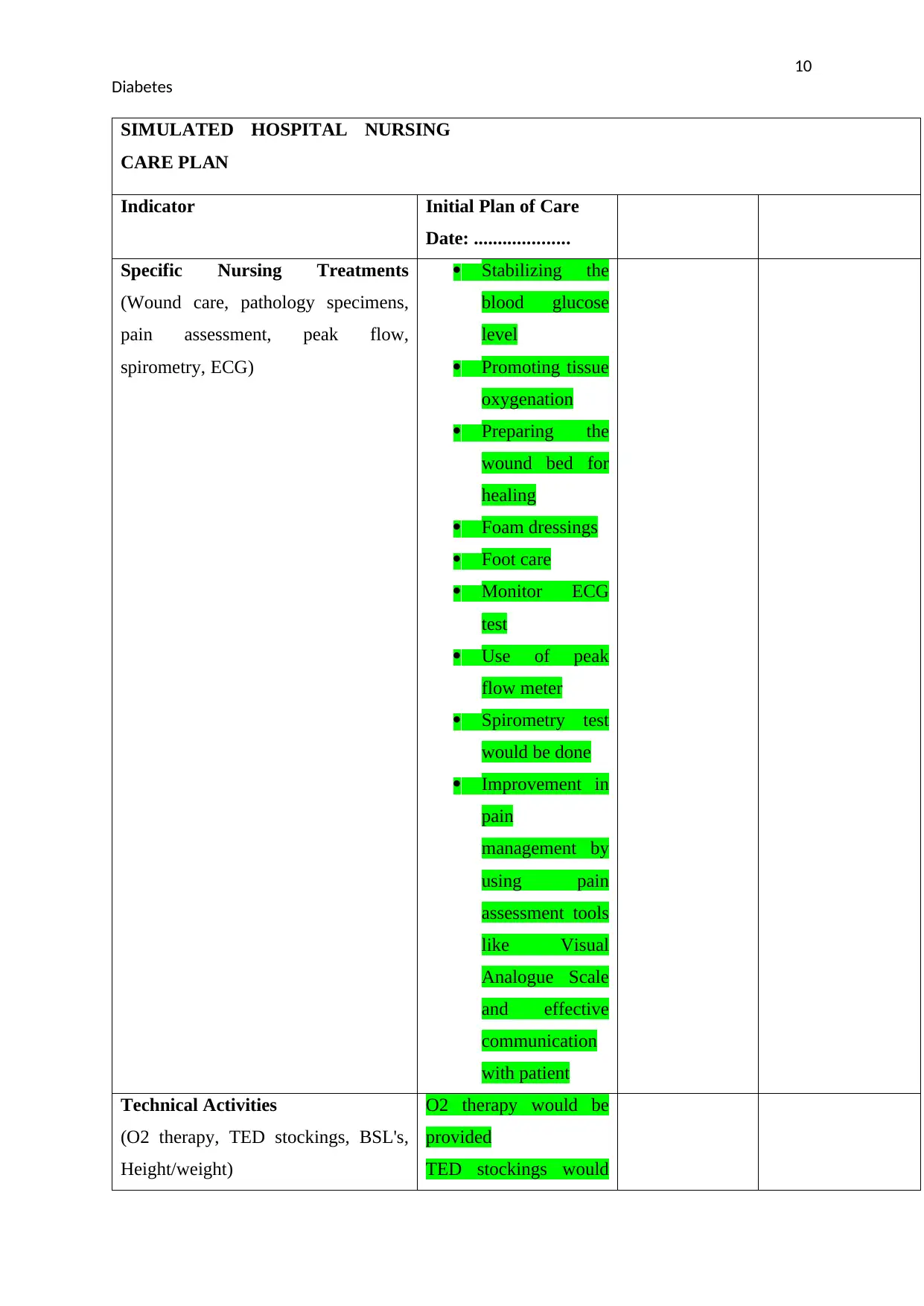
SIMULATED HOSPITAL NURSING
CARE PLAN
Indicator Initial Plan of Care
Date: ....................
Specific Nursing Treatments
(Wound care, pathology specimens,
pain assessment, peak flow,
spirometry, ECG)
Stabilizing the
blood glucose
level
Promoting tissue
oxygenation
Preparing the
wound bed for
healing
Foam dressings
Foot care
Monitor ECG
test
Use of peak
flow meter
Spirometry test
would be done
Improvement in
pain
management by
using pain
assessment tools
like Visual
Analogue Scale
and effective
communication
with patient
Technical Activities
(O2 therapy, TED stockings, BSL's,
Height/weight)
O2 therapy would be
provided
TED stockings would
Diabetes
SIMULATED HOSPITAL NURSING
CARE PLAN
Indicator Initial Plan of Care
Date: ....................
Specific Nursing Treatments
(Wound care, pathology specimens,
pain assessment, peak flow,
spirometry, ECG)
Stabilizing the
blood glucose
level
Promoting tissue
oxygenation
Preparing the
wound bed for
healing
Foam dressings
Foot care
Monitor ECG
test
Use of peak
flow meter
Spirometry test
would be done
Improvement in
pain
management by
using pain
assessment tools
like Visual
Analogue Scale
and effective
communication
with patient
Technical Activities
(O2 therapy, TED stockings, BSL's,
Height/weight)
O2 therapy would be
provided
TED stockings would
11
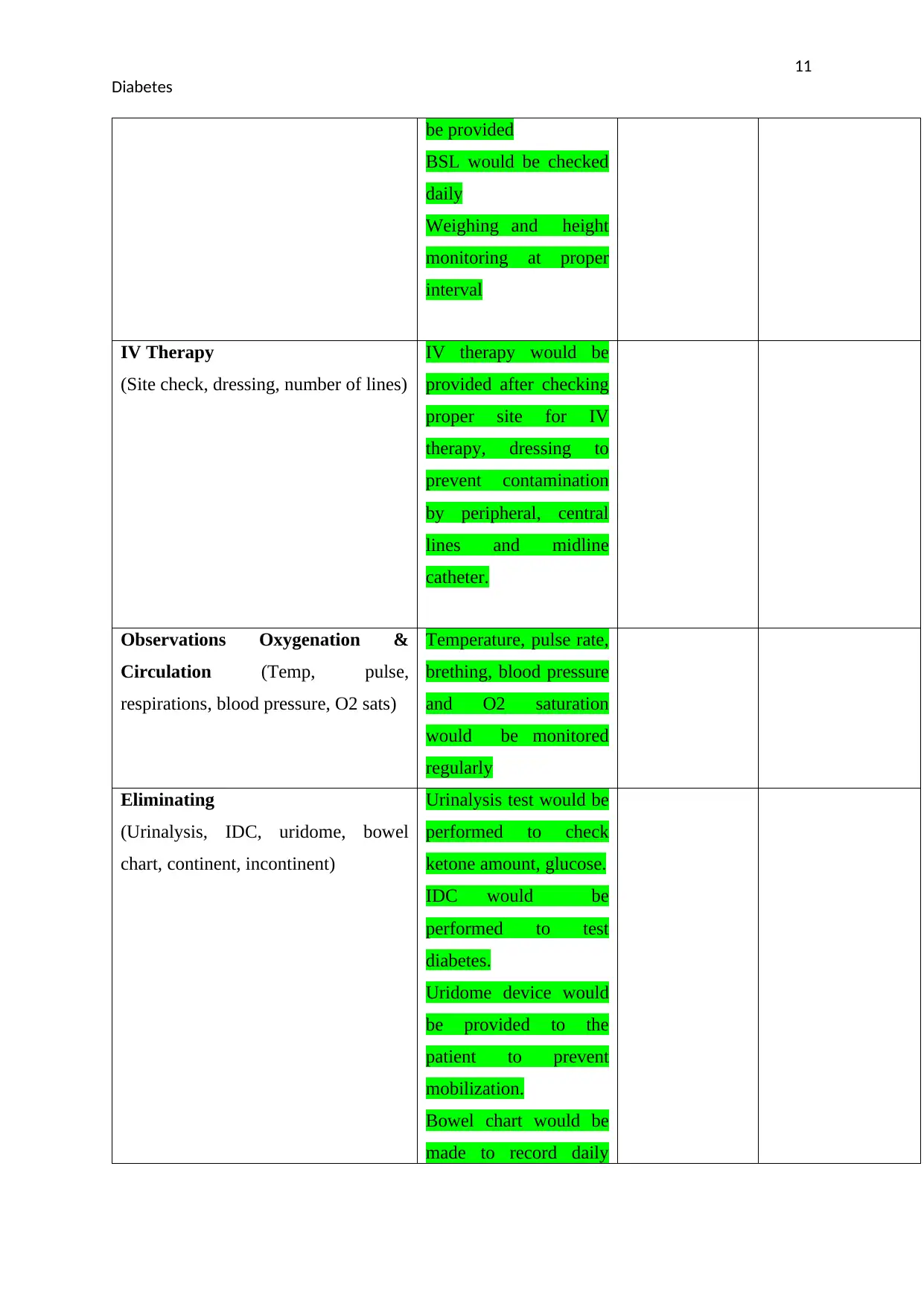
Diabetes
be provided
BSL would be checked
daily
Weighing and height
monitoring at proper
interval
IV Therapy
(Site check, dressing, number of lines)
IV therapy would be
provided after checking
proper site for IV
therapy, dressing to
prevent contamination
by peripheral, central
lines and midline
catheter.
Observations Oxygenation &
Circulation (Temp, pulse,
respirations, blood pressure, O2 sats)
Temperature, pulse rate,
brething, blood pressure
and O2 saturation
would be monitored
regularly
Eliminating
(Urinalysis, IDC, uridome, bowel
chart, continent, incontinent)
Urinalysis test would be
performed to check
ketone amount, glucose.
IDC would be
performed to test
diabetes.
Uridome device would
be provided to the
patient to prevent
mobilization.
Bowel chart would be
made to record daily
Diabetes
be provided
BSL would be checked
daily
Weighing and height
monitoring at proper
interval
IV Therapy
(Site check, dressing, number of lines)
IV therapy would be
provided after checking
proper site for IV
therapy, dressing to
prevent contamination
by peripheral, central
lines and midline
catheter.
Observations Oxygenation &
Circulation (Temp, pulse,
respirations, blood pressure, O2 sats)
Temperature, pulse rate,
brething, blood pressure
and O2 saturation
would be monitored
regularly
Eliminating
(Urinalysis, IDC, uridome, bowel
chart, continent, incontinent)
Urinalysis test would be
performed to check
ketone amount, glucose.
IDC would be
performed to test
diabetes.
Uridome device would
be provided to the
patient to prevent
mobilization.
Bowel chart would be
made to record daily
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





