Nursing Case Study: Clinical Reasoning and Patient Prioritization
VerifiedAdded on 2021/05/31
|11
|3144
|25
Case Study
AI Summary
This nursing case study analyzes the care of a 24-year-old patient, Mr. Harry Flanagan, who was injured in a road accident. The study employs the DRABC assessment tool to identify nursing priorities. The assessment reveals the need for pain management, blood pressure control, and stress management. Patient-centered goals are established for each priority, followed by detailed nursing interventions with rationales and evaluation criteria. The case study highlights the importance of clinical reasoning in prioritizing patient care, providing specific strategies for pain relief, blood pressure management, and stress reduction to improve patient outcomes. The interventions include medication, environmental modifications, and patient education, with outcomes measured through pain scales, blood pressure monitoring, and assessing the patient's coping mechanisms.

Running head:NURSING
Nursing
Name of student:
Name of university:
Author note:
Nursing
Name of student:
Name of university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
Nursing professionals are to address complex health problems of patients by application
of suitable skills and adequate knowledge. Appropriate clinical reasoning skills are required for
recognizing the most important patient needs and delivering interventions accordingly. Clinical
reasoning is the valuable tool with which nurses can process the patient information and set up
nursing priorities for the patient. The next step is to outline interventions that can help in
achieving better patient outcomes. The present paper is a nursing case study analysis report that
utilizes the clinical reasoning process to prioritize patient care. The aim is to critically analyze
the patient assessment findings. This takes into consideration the patient’s situation and the
medical diagnosis. The data is collected and processed in terms of relevance to nursing care
using DRABC (Danger, Response, Airway, Breathing and Circulation). Thereafter, three nursing
priorities are identified for this person, one of which is a psychosocial need. One patient centered
goal is then established for the nursing diagnosis. For each of the diagnosis, particular nursing
interventions are identified including rationale and evaluation criteria.
The patient in the present case scenario is Mr. Harry Flanagan, a 24 year old individual,
who suffered injury due to a road accident. The ambulance had to extract him since he was in
pain and was not able to move his left leg. The patient had no significant medical history and is
normally fit. Harry moved to Canberra from Alice Springs three years ago to play rugby, and has
recently engaged to his partner with whom he has an 18 month old daughter. Upon arriving on
the emergency department his vital signs were BP: 153/ 74 mm hg; HR: 112 beats/ minute; RR:
22 breaths / minute; Temp: 35.9 degree C and SpO2: 96% on room air. Harry complained of
severe pain on the right side of his chest and there was bruising in the area. An ECG was done
that indicated normal sinus rhythm. The paramedics had placed a splint on the patient’s left leg.
He reported to have a pain score of 8/10 at the site in the left leg. He was given morphine on
Nursing professionals are to address complex health problems of patients by application
of suitable skills and adequate knowledge. Appropriate clinical reasoning skills are required for
recognizing the most important patient needs and delivering interventions accordingly. Clinical
reasoning is the valuable tool with which nurses can process the patient information and set up
nursing priorities for the patient. The next step is to outline interventions that can help in
achieving better patient outcomes. The present paper is a nursing case study analysis report that
utilizes the clinical reasoning process to prioritize patient care. The aim is to critically analyze
the patient assessment findings. This takes into consideration the patient’s situation and the
medical diagnosis. The data is collected and processed in terms of relevance to nursing care
using DRABC (Danger, Response, Airway, Breathing and Circulation). Thereafter, three nursing
priorities are identified for this person, one of which is a psychosocial need. One patient centered
goal is then established for the nursing diagnosis. For each of the diagnosis, particular nursing
interventions are identified including rationale and evaluation criteria.
The patient in the present case scenario is Mr. Harry Flanagan, a 24 year old individual,
who suffered injury due to a road accident. The ambulance had to extract him since he was in
pain and was not able to move his left leg. The patient had no significant medical history and is
normally fit. Harry moved to Canberra from Alice Springs three years ago to play rugby, and has
recently engaged to his partner with whom he has an 18 month old daughter. Upon arriving on
the emergency department his vital signs were BP: 153/ 74 mm hg; HR: 112 beats/ minute; RR:
22 breaths / minute; Temp: 35.9 degree C and SpO2: 96% on room air. Harry complained of
severe pain on the right side of his chest and there was bruising in the area. An ECG was done
that indicated normal sinus rhythm. The paramedics had placed a splint on the patient’s left leg.
He reported to have a pain score of 8/10 at the site in the left leg. He was given morphine on
2NURSING
arrival to the ED that was effective in reducing the pain to 5/10. He suffered a large laceration to
the left thigh that had been bleeding profusely and needed to pressure bandage to cover it up. The
patient was administered normal saline IV infusion. CT scan and X-ray were performed to assess
further injuries. The chest X-ray revealed that there was no rib fracture and lung fields had good
air entry. There was no bone displacement or evidence fracture in the pelvis. X-ray of the limb
revealed simple and closed fracture of the left femur with swelling around the left thigh. There
were no other signs of injuries. It was determined that he needed surgery for stabilizing his
conditions.
the second day, Harry underwent an open reduction and internal fixation (ORIF) of his
left femur. Upon discharge to the ward he was given standard post-operative care, including
fluids, observations, analgesia and enoxaparin. The patient’s progress had been uneventful till
the fourth day. He however had difficulty complying with the physiotherapists’ direction to do
deep breathing and coughing exercises. This was due to bruising and pain in the chest. Further,
harry could not comply with the instructions for leg exercises. His vital signs are BP: 133/73;
HR: 92 beats/ minute; Respiratory rate: 18 breaths/ minute; Temp: 35.6 OC; SpO2: 97% on room
air. Harry reports swelling in his right calf and pain.
Based on the patient information collected it would be appropriate to carry out an
assessment with the help of the DRAC (Danger, Response, Airway, Breathing and Circulation)
assessment tool. The tool helps in assessing the situation and identifying the nursing priorities for
care (Blais, 2015). The patient has suffered large laceration to his left thigh and had been
bleeding profusely when he had been attended. The patient had to undergo open reduction and
internal fixation (ORIF) for minimizing further complications from the injury. An open reduction
internal fixation is the surgical process undertaken for fixing a severe bone fracture. Open
arrival to the ED that was effective in reducing the pain to 5/10. He suffered a large laceration to
the left thigh that had been bleeding profusely and needed to pressure bandage to cover it up. The
patient was administered normal saline IV infusion. CT scan and X-ray were performed to assess
further injuries. The chest X-ray revealed that there was no rib fracture and lung fields had good
air entry. There was no bone displacement or evidence fracture in the pelvis. X-ray of the limb
revealed simple and closed fracture of the left femur with swelling around the left thigh. There
were no other signs of injuries. It was determined that he needed surgery for stabilizing his
conditions.
the second day, Harry underwent an open reduction and internal fixation (ORIF) of his
left femur. Upon discharge to the ward he was given standard post-operative care, including
fluids, observations, analgesia and enoxaparin. The patient’s progress had been uneventful till
the fourth day. He however had difficulty complying with the physiotherapists’ direction to do
deep breathing and coughing exercises. This was due to bruising and pain in the chest. Further,
harry could not comply with the instructions for leg exercises. His vital signs are BP: 133/73;
HR: 92 beats/ minute; Respiratory rate: 18 breaths/ minute; Temp: 35.6 OC; SpO2: 97% on room
air. Harry reports swelling in his right calf and pain.
Based on the patient information collected it would be appropriate to carry out an
assessment with the help of the DRAC (Danger, Response, Airway, Breathing and Circulation)
assessment tool. The tool helps in assessing the situation and identifying the nursing priorities for
care (Blais, 2015). The patient has suffered large laceration to his left thigh and had been
bleeding profusely when he had been attended. The patient had to undergo open reduction and
internal fixation (ORIF) for minimizing further complications from the injury. An open reduction
internal fixation is the surgical process undertaken for fixing a severe bone fracture. Open
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
reduction refers to the realignment of the fractured bone into the normal position. Internal
fixation refers to the use of plates, screws and steel rods for keeping the bone fracture in a stable
condition for healing and preventing any chances of infection (Assal et al., 2015). While the
patient was normally responsive after the surgery, he reported pain and swelling in the right calf
that was found to be red. Pain is common after surgery in some patients who are at increased risk
of swelling. Swelling is a part of the healing process and surgeries such as open reduction and
internal fixation is involved with manifestations such as swelling and pain. The magnitude of it
depends on the extent of the tissue damage that is suffered at the site. The development of pain
following surgery is due to changes in the central nervous system and peripheral nervous system
(Majuta et al., 2015).
Though Harry’s progress had been uneventful after the surgery, he had difficulty in
complying with the instructions on deep breathing and coughing exercises, and leg exercises. As
opined by Tripathi and Sharma (2017) deep breathing and coughing exercises help in increased
mobility after a patient has undergone surgery. The exercises help in the breathing pattern and
augment clearing of lungs, thereby reducing the risks of infection. In the present case Harry was
unable to carry out the exercises due to pain and bruising. The difficulty in carrying out
breathing exercises denotes airway obstructions. Airway obstruction leads to paradoxical chest
movements and the use of accessory muscles of respiration. At the time of assessment of
breathing it is crucial to diagnose any abnormalities in the respiratory rate ad oxygen
concentrations. The patient’s respiratory rate was 18 breaths/ min while his oxygen saturation
was 97% on room air. The normal respiratory rate for adults is 12-20 breaths per minute while
the normal oxygen saturation level is 94-99% (Jain, 2017). In all surgical emergencies, it is
crucial to assess risks of cardiac complications. This is to be done by assessing pulse rate of the
reduction refers to the realignment of the fractured bone into the normal position. Internal
fixation refers to the use of plates, screws and steel rods for keeping the bone fracture in a stable
condition for healing and preventing any chances of infection (Assal et al., 2015). While the
patient was normally responsive after the surgery, he reported pain and swelling in the right calf
that was found to be red. Pain is common after surgery in some patients who are at increased risk
of swelling. Swelling is a part of the healing process and surgeries such as open reduction and
internal fixation is involved with manifestations such as swelling and pain. The magnitude of it
depends on the extent of the tissue damage that is suffered at the site. The development of pain
following surgery is due to changes in the central nervous system and peripheral nervous system
(Majuta et al., 2015).
Though Harry’s progress had been uneventful after the surgery, he had difficulty in
complying with the instructions on deep breathing and coughing exercises, and leg exercises. As
opined by Tripathi and Sharma (2017) deep breathing and coughing exercises help in increased
mobility after a patient has undergone surgery. The exercises help in the breathing pattern and
augment clearing of lungs, thereby reducing the risks of infection. In the present case Harry was
unable to carry out the exercises due to pain and bruising. The difficulty in carrying out
breathing exercises denotes airway obstructions. Airway obstruction leads to paradoxical chest
movements and the use of accessory muscles of respiration. At the time of assessment of
breathing it is crucial to diagnose any abnormalities in the respiratory rate ad oxygen
concentrations. The patient’s respiratory rate was 18 breaths/ min while his oxygen saturation
was 97% on room air. The normal respiratory rate for adults is 12-20 breaths per minute while
the normal oxygen saturation level is 94-99% (Jain, 2017). In all surgical emergencies, it is
crucial to assess risks of cardiac complications. This is to be done by assessing pulse rate of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
patient and blood pressure. In the present case, Harry’s heart rate was 92 beats/minute while his
blood pressure was 133/73 mmHg which was previously BP153/ 74. A normal resting heart rate
for adult is between 60 to 100 beats per minute (Portnoy & Farrington, 2015). The systolic
reading of 133 is in the prehypertension range as outlined by the American Heart Association’s
guidelines for blood pressure. The diastolic reading of 73 is in the normal range. The patient is
thus subjected to prehypertension.
Based on the DRABC assessment carried out on the patient, the three nursing priorities
that have been identified for the patient are pain management, blood pressure management, and
stress management. For pain management, the patient-centered goal would be to enable the
patient describe satisfactory pain control at a level less than 4 on a scale of 1-10. In relation to
blood pressure management, the goal would be to maintain the patient’s blood pressure within
the acceptable range. In relation to stress management, the goal would be to enable the patient
gain mobility and resume normal life (Butcher et al., 2018).
Nurses are responsible for addressing the concerns of the patient in relation to pain
suffered. The first intervention would be foreseeing the need for pain relief. Early intervention
reduces the total amount of analgesic required. Report of pain is to be acknowledged
immediately for preventing further aggravation. Demonstration of the concern for the comfort
and welfare of the patient helps in development of a comforting and trusting relationship
(DeVore et al., 2017). Additional stressors that might lead to further discomfort are to be
removed from the environment. The rationale is that patients often experience pain exaggeration
if there are intrapersonal, environmental or intrapsychic factors present causing stress. Providing
rest periods is important for promotion of sleep, relief and relaxation. This is because pain is
aggravated due to exhaustion (Andersson et al., 2017). The patient might be given non-opioid
patient and blood pressure. In the present case, Harry’s heart rate was 92 beats/minute while his
blood pressure was 133/73 mmHg which was previously BP153/ 74. A normal resting heart rate
for adult is between 60 to 100 beats per minute (Portnoy & Farrington, 2015). The systolic
reading of 133 is in the prehypertension range as outlined by the American Heart Association’s
guidelines for blood pressure. The diastolic reading of 73 is in the normal range. The patient is
thus subjected to prehypertension.
Based on the DRABC assessment carried out on the patient, the three nursing priorities
that have been identified for the patient are pain management, blood pressure management, and
stress management. For pain management, the patient-centered goal would be to enable the
patient describe satisfactory pain control at a level less than 4 on a scale of 1-10. In relation to
blood pressure management, the goal would be to maintain the patient’s blood pressure within
the acceptable range. In relation to stress management, the goal would be to enable the patient
gain mobility and resume normal life (Butcher et al., 2018).
Nurses are responsible for addressing the concerns of the patient in relation to pain
suffered. The first intervention would be foreseeing the need for pain relief. Early intervention
reduces the total amount of analgesic required. Report of pain is to be acknowledged
immediately for preventing further aggravation. Demonstration of the concern for the comfort
and welfare of the patient helps in development of a comforting and trusting relationship
(DeVore et al., 2017). Additional stressors that might lead to further discomfort are to be
removed from the environment. The rationale is that patients often experience pain exaggeration
if there are intrapersonal, environmental or intrapsychic factors present causing stress. Providing
rest periods is important for promotion of sleep, relief and relaxation. This is because pain is
aggravated due to exhaustion (Andersson et al., 2017). The patient might be given non-opioid
5NURSING
pharmacological drug for effectively managing pain through blockage of prostaglandin
synthesis. The effectiveness of the interventions would be evaluated by assessing the patient’s
level of pain and the individual’s improvement in coping (Lehne& Rosenthal, 2014).
For addressing pre-hypertension stage, it is crucial to note presence and quality of
peripheral and central pulses. Pulses in the legs might be diminished, reflecting the impact of
venous congestion and vasoconstriction systemic vascular resistance (Hering et al., 2016). The
patient’s capillary refill time, and skin color, moisture and temperature are to be recorded. Such
assessment reflects decreased cardiac output. The patient is to be provided with restful, calm
surrounding for minimizing environmental activity. This helps in promotion of relaxation. It is
also crucial to schedule periods of uninterrupted rests and provide assistance for self-care
activities. The rationale is that such measures reduce the physical stress and lessens the tension
that otherwise leads to blood pressure (Butcher et al., 2018). Monitoring response to medication
is crucial for controlling blood pressure. Response to drug delivery is dependent on a number of
factors. Medications such as thiazide or beta-blockers can be administered as an anti-
hypertensive drug (Lehne& Rosenthal, 2014). The outcome of the intervention would be
evaluated by monitoring the blood pressure of the patient on a regular basis.
Stress management for the patient would be crucial to promote better mobility and
enhance his quality of life. The first intervention would be to assist the patient to identify
feelings of depression and stress. The strategy would be to establish a therapeutic relationship for
two-way communication. The patient is to be assisted to develop self-awareness of pain (Black,
2016). The patient is to be further assisted to identify methods of coping. It is important to
review feelings and thoughts related to surgery and pain. This would guide in coping and help
the patient lead a normal life. Since the patient is a rugby player and lives alone, it is crucial that
pharmacological drug for effectively managing pain through blockage of prostaglandin
synthesis. The effectiveness of the interventions would be evaluated by assessing the patient’s
level of pain and the individual’s improvement in coping (Lehne& Rosenthal, 2014).
For addressing pre-hypertension stage, it is crucial to note presence and quality of
peripheral and central pulses. Pulses in the legs might be diminished, reflecting the impact of
venous congestion and vasoconstriction systemic vascular resistance (Hering et al., 2016). The
patient’s capillary refill time, and skin color, moisture and temperature are to be recorded. Such
assessment reflects decreased cardiac output. The patient is to be provided with restful, calm
surrounding for minimizing environmental activity. This helps in promotion of relaxation. It is
also crucial to schedule periods of uninterrupted rests and provide assistance for self-care
activities. The rationale is that such measures reduce the physical stress and lessens the tension
that otherwise leads to blood pressure (Butcher et al., 2018). Monitoring response to medication
is crucial for controlling blood pressure. Response to drug delivery is dependent on a number of
factors. Medications such as thiazide or beta-blockers can be administered as an anti-
hypertensive drug (Lehne& Rosenthal, 2014). The outcome of the intervention would be
evaluated by monitoring the blood pressure of the patient on a regular basis.
Stress management for the patient would be crucial to promote better mobility and
enhance his quality of life. The first intervention would be to assist the patient to identify
feelings of depression and stress. The strategy would be to establish a therapeutic relationship for
two-way communication. The patient is to be assisted to develop self-awareness of pain (Black,
2016). The patient is to be further assisted to identify methods of coping. It is important to
review feelings and thoughts related to surgery and pain. This would guide in coping and help
the patient lead a normal life. Since the patient is a rugby player and lives alone, it is crucial that
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING
he demonstrates suitable coping mechanism (Moorhead et al., 2014). The patient is to be further
encouraged to be independent in movement and positive reinforcement would be crucial for such
behaviors. Positive reinforcement is essential for enhancing self-esteem. Enhanced self-esteem is
crucial for leading a better quality of life. The evaluation of the interventions would be done by
assessing the patient’s level of coping (Khan et al., 2016).
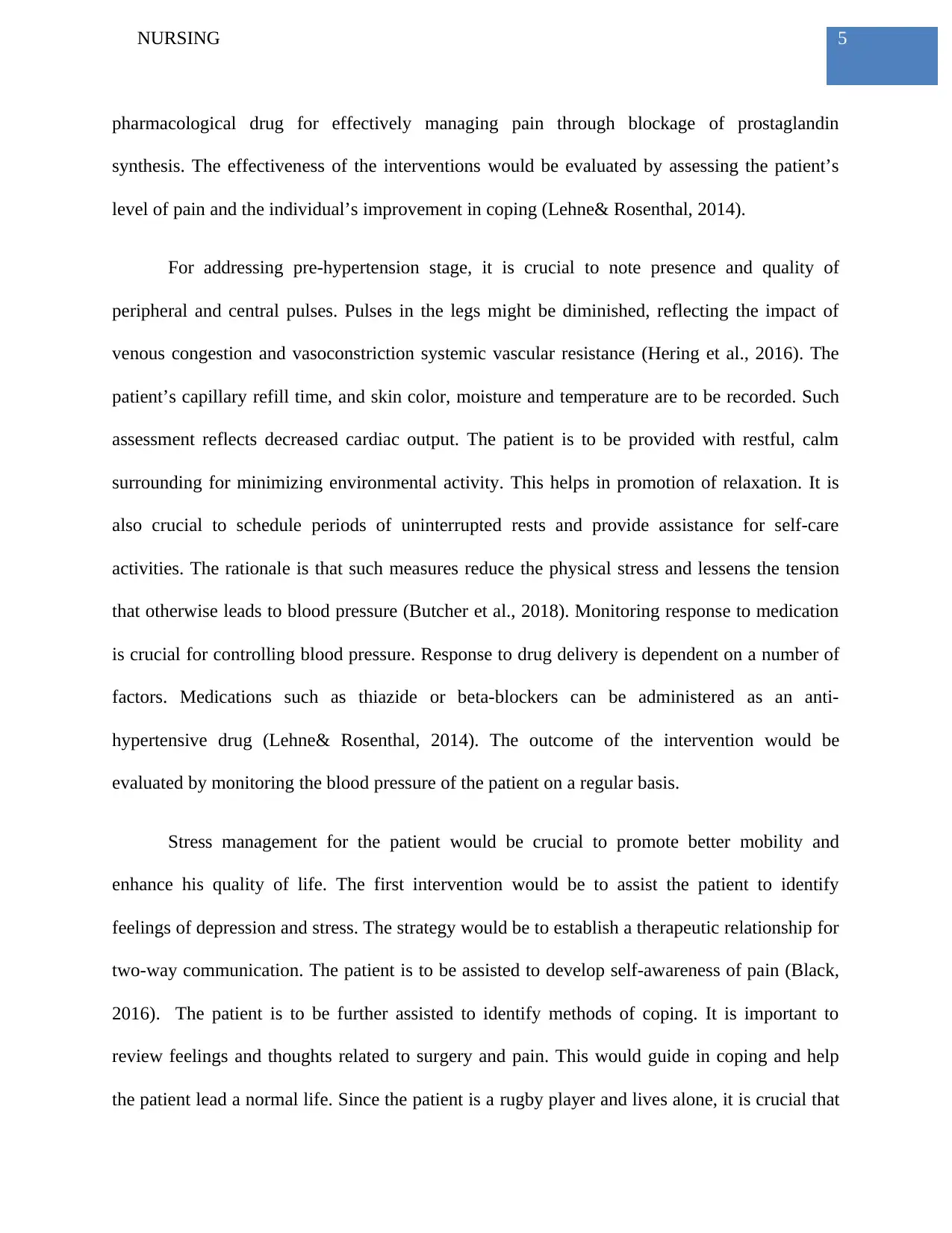
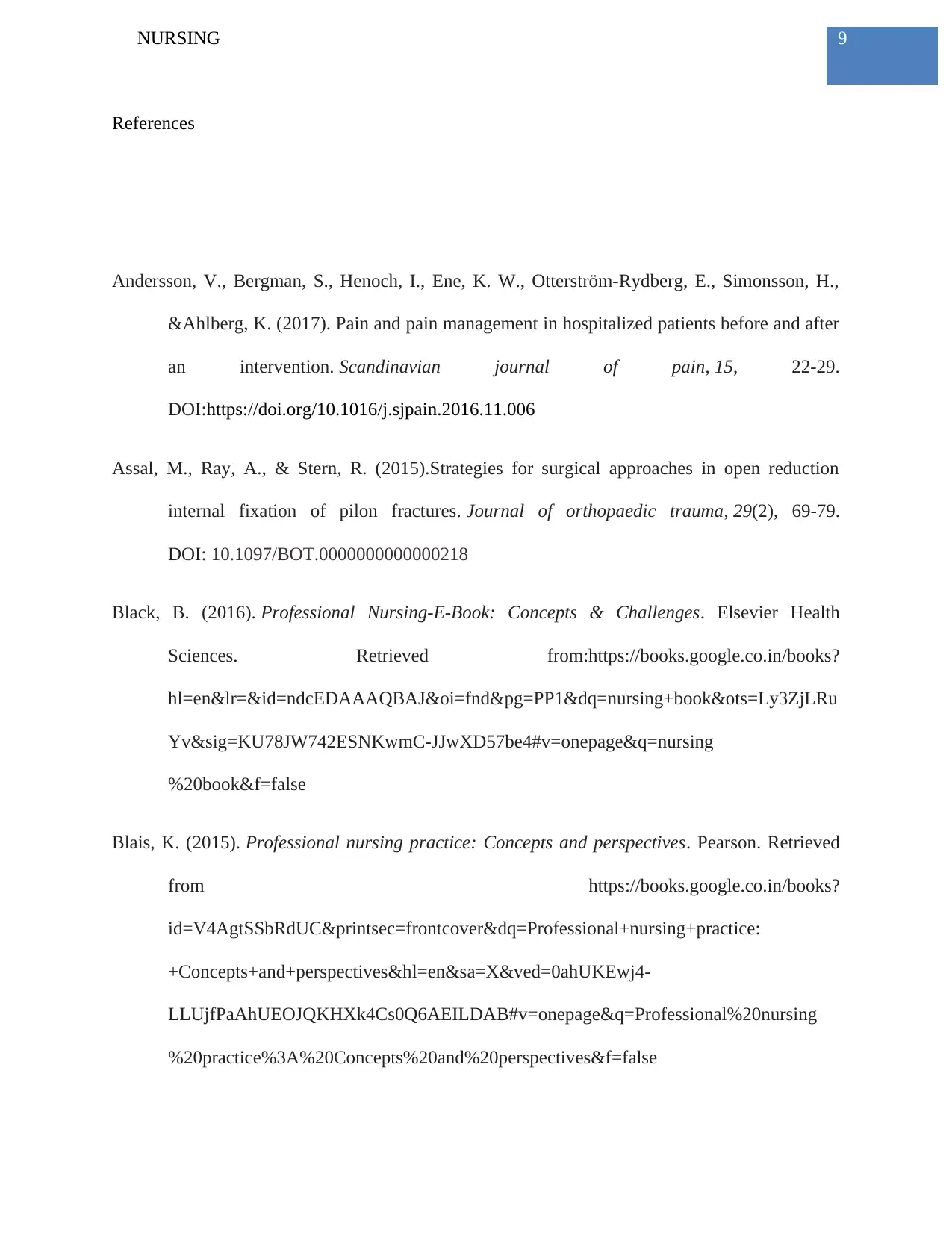
Below is a detailed structure of the nursing care plan explained under a tabular format.
Serial
number
Nursing priorities Goals of care Interventions Measuring the
outcomes
1 Pain management Patient-
centred goals
to improve
the quality of
life
Pain relief
1. Immediate reporting of
pain in order to prevent
further aggravation
(DeVore et al., 2017)
2. Providing rest periods in
order to reduce exhaustion
and thereby promoting
sleep, relief and relaxation
(Andersson et al., 2017)
3. Administration of non-
opioid pharmacological
drug for effective pain
management (Lehne &
Rosenthal, 2014)
Effectiveness of
interventions would
be evaluated via
assessing patient’s
level of pain along
with individual’s
improvement in
coping
he demonstrates suitable coping mechanism (Moorhead et al., 2014). The patient is to be further
encouraged to be independent in movement and positive reinforcement would be crucial for such
behaviors. Positive reinforcement is essential for enhancing self-esteem. Enhanced self-esteem is
crucial for leading a better quality of life. The evaluation of the interventions would be done by
assessing the patient’s level of coping (Khan et al., 2016).
Below is a detailed structure of the nursing care plan explained under a tabular format.
Serial
number
Nursing priorities Goals of care Interventions Measuring the
outcomes
1 Pain management Patient-
centred goals
to improve
the quality of
life
Pain relief
1. Immediate reporting of
pain in order to prevent
further aggravation
(DeVore et al., 2017)
2. Providing rest periods in
order to reduce exhaustion
and thereby promoting
sleep, relief and relaxation
(Andersson et al., 2017)
3. Administration of non-
opioid pharmacological
drug for effective pain
management (Lehne &
Rosenthal, 2014)
Effectiveness of
interventions would
be evaluated via
assessing patient’s
level of pain along
with individual’s
improvement in
coping
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
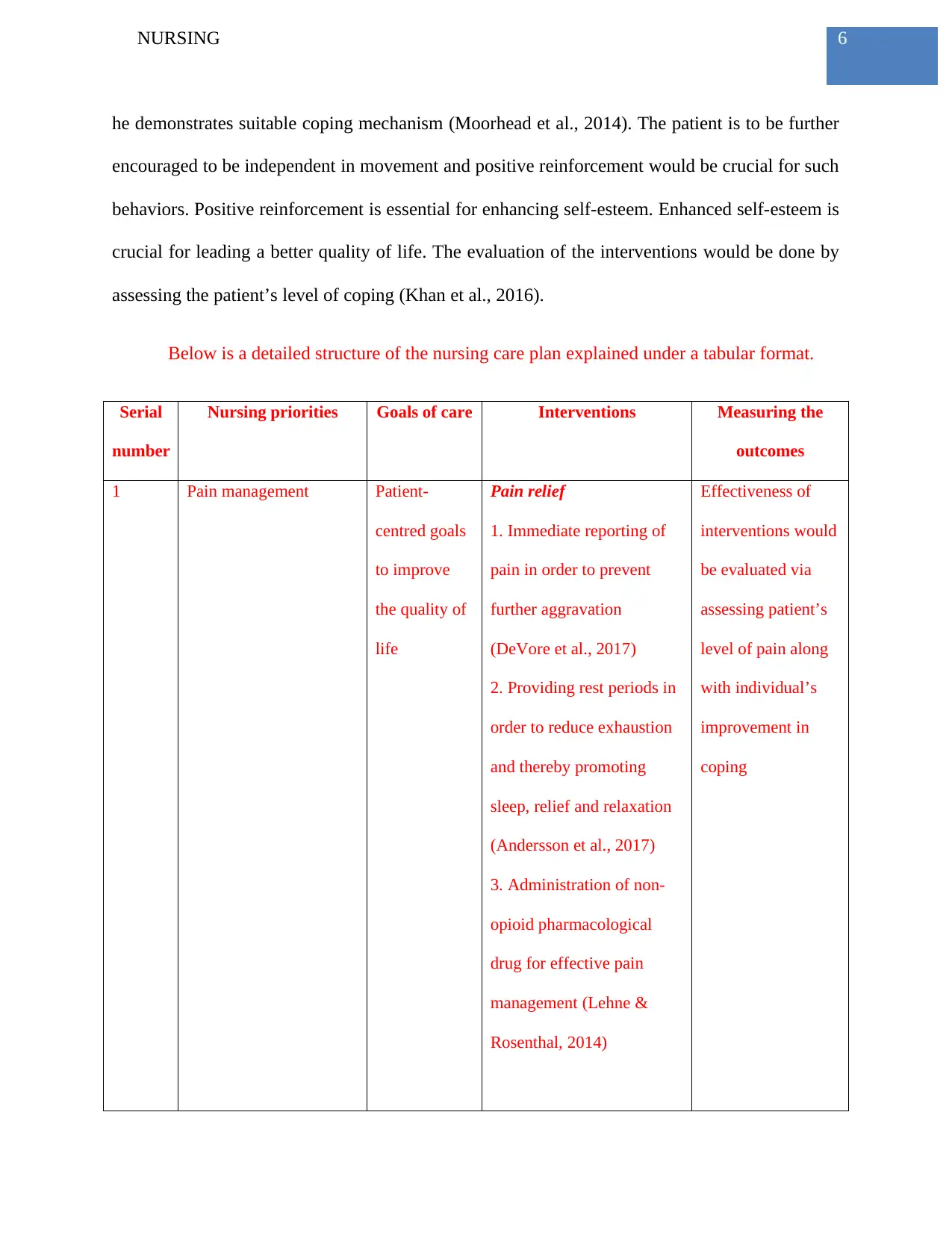
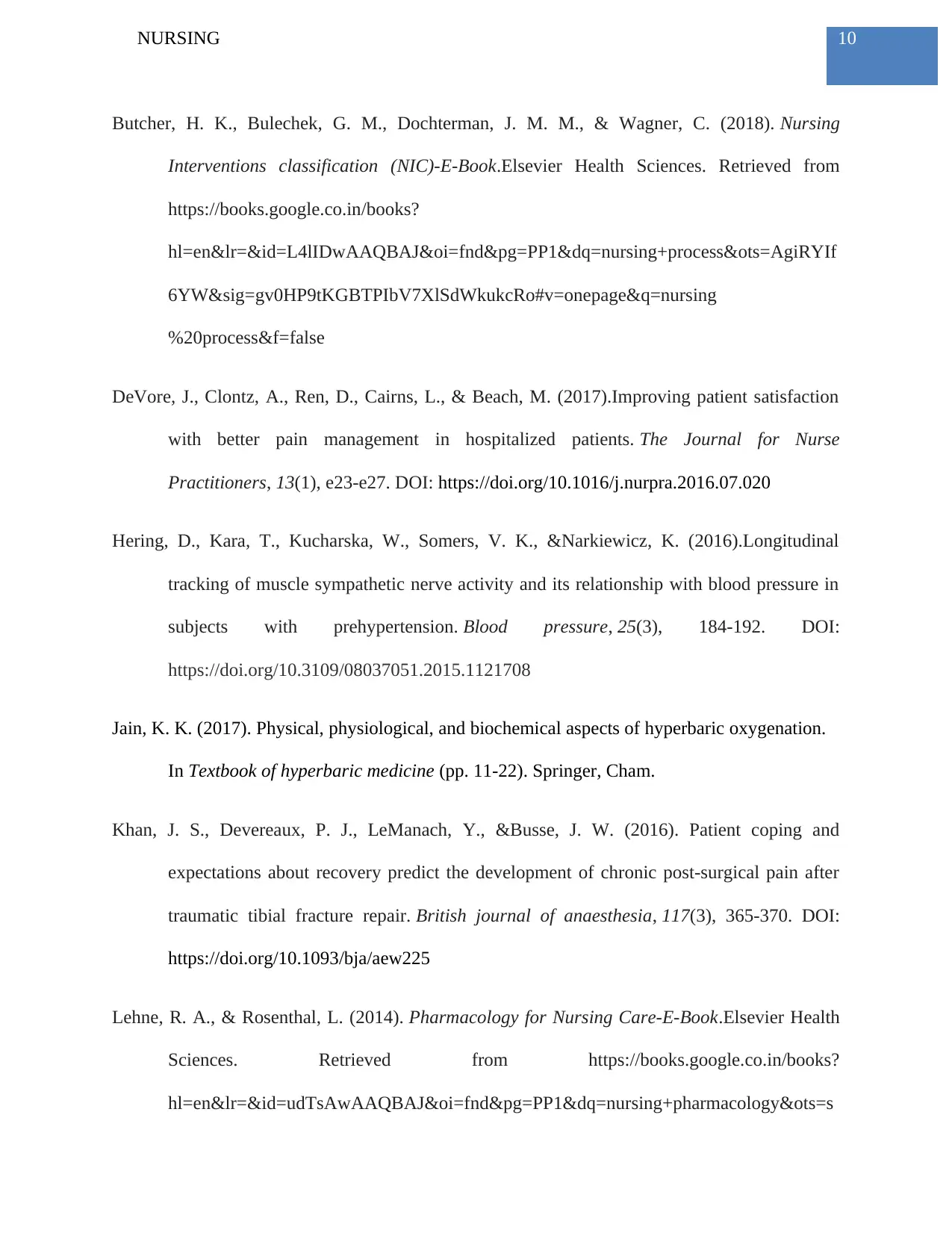
2 Blood pressure
management
Maintaining
patient’s
blood
pressure
within
acceptable
range
Effective detection of the
pre-hypertension stage
1. Noting down patient’s
capillary refill time, colour
of the skin, body
temperature and skin
moisture (Hering et al.,
2016)
Medication management
of blood pressure
1. Use of beta blockers as
anti-hypertensive drug
(Lehne & Rosenthal, 2014)
The outcome will
be measure via
monitoring blood
pressure level of the
patients on a
periodic manner
3 Stress management Enable
patient’s
mobility to
resume
normal life
Identification of feelings of
depression
1. Therapeutic relationship
for two-ways
communication.
2. Assistance of patients to
develop self-awareness of
pain (Black, 2016)
Patient encouragement
Patient will be encourage to
lead an independent life
along with positive
reinforcement of
Evaluation of
interventions will
be done ia assessing
patient’s level of
coping
2 Blood pressure
management
Maintaining
patient’s
blood
pressure
within
acceptable
range
Effective detection of the
pre-hypertension stage
1. Noting down patient’s
capillary refill time, colour
of the skin, body
temperature and skin
moisture (Hering et al.,
2016)
Medication management
of blood pressure
1. Use of beta blockers as
anti-hypertensive drug
(Lehne & Rosenthal, 2014)
The outcome will
be measure via
monitoring blood
pressure level of the
patients on a
periodic manner
3 Stress management Enable
patient’s
mobility to
resume
normal life
Identification of feelings of
depression
1. Therapeutic relationship
for two-ways
communication.
2. Assistance of patients to
develop self-awareness of
pain (Black, 2016)
Patient encouragement
Patient will be encourage to
lead an independent life
along with positive
reinforcement of
Evaluation of
interventions will
be done ia assessing
patient’s level of
coping
8NURSING
behaviours
(Moorhead et al., 2014)
In conclusion, the present case study analysis offered an opportunity to apply clinical
reasoning cycle in nursing practice. The processing of collected information was helpful in
understanding the key issues faced by the patient. On the basis of such as an assessment with the
DRABC framework nursing priorities of care could be identified. These are related to pain
management, high blood pressure management and stress management. Suitable nursing
interventions would enable faster recovery of the patient.
behaviours
(Moorhead et al., 2014)
In conclusion, the present case study analysis offered an opportunity to apply clinical
reasoning cycle in nursing practice. The processing of collected information was helpful in
understanding the key issues faced by the patient. On the basis of such as an assessment with the
DRABC framework nursing priorities of care could be identified. These are related to pain
management, high blood pressure management and stress management. Suitable nursing
interventions would enable faster recovery of the patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
References
Andersson, V., Bergman, S., Henoch, I., Ene, K. W., Otterström-Rydberg, E., Simonsson, H.,
&Ahlberg, K. (2017). Pain and pain management in hospitalized patients before and after
an intervention. Scandinavian journal of pain, 15, 22-29.
DOI:https://doi.org/10.1016/j.sjpain.2016.11.006
Assal, M., Ray, A., & Stern, R. (2015).Strategies for surgical approaches in open reduction
internal fixation of pilon fractures. Journal of orthopaedic trauma, 29(2), 69-79.
DOI: 10.1097/BOT.0000000000000218
Black, B. (2016). Professional Nursing-E-Book: Concepts & Challenges. Elsevier Health
Sciences. Retrieved from:https://books.google.co.in/books?
hl=en&lr=&id=ndcEDAAAQBAJ&oi=fnd&pg=PP1&dq=nursing+book&ots=Ly3ZjLRu
Yv&sig=KU78JW742ESNKwmC-JJwXD57be4#v=onepage&q=nursing
%20book&f=false
Blais, K. (2015). Professional nursing practice: Concepts and perspectives. Pearson. Retrieved
from https://books.google.co.in/books?
id=V4AgtSSbRdUC&printsec=frontcover&dq=Professional+nursing+practice:
+Concepts+and+perspectives&hl=en&sa=X&ved=0ahUKEwj4-
LLUjfPaAhUEOJQKHXk4Cs0Q6AEILDAB#v=onepage&q=Professional%20nursing
%20practice%3A%20Concepts%20and%20perspectives&f=false
References
Andersson, V., Bergman, S., Henoch, I., Ene, K. W., Otterström-Rydberg, E., Simonsson, H.,
&Ahlberg, K. (2017). Pain and pain management in hospitalized patients before and after
an intervention. Scandinavian journal of pain, 15, 22-29.
DOI:https://doi.org/10.1016/j.sjpain.2016.11.006
Assal, M., Ray, A., & Stern, R. (2015).Strategies for surgical approaches in open reduction
internal fixation of pilon fractures. Journal of orthopaedic trauma, 29(2), 69-79.
DOI: 10.1097/BOT.0000000000000218
Black, B. (2016). Professional Nursing-E-Book: Concepts & Challenges. Elsevier Health
Sciences. Retrieved from:https://books.google.co.in/books?
hl=en&lr=&id=ndcEDAAAQBAJ&oi=fnd&pg=PP1&dq=nursing+book&ots=Ly3ZjLRu
Yv&sig=KU78JW742ESNKwmC-JJwXD57be4#v=onepage&q=nursing
%20book&f=false
Blais, K. (2015). Professional nursing practice: Concepts and perspectives. Pearson. Retrieved
from https://books.google.co.in/books?
id=V4AgtSSbRdUC&printsec=frontcover&dq=Professional+nursing+practice:
+Concepts+and+perspectives&hl=en&sa=X&ved=0ahUKEwj4-
LLUjfPaAhUEOJQKHXk4Cs0Q6AEILDAB#v=onepage&q=Professional%20nursing
%20practice%3A%20Concepts%20and%20perspectives&f=false
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. (2018). Nursing
Interventions classification (NIC)-E-Book.Elsevier Health Sciences. Retrieved from
https://books.google.co.in/books?
hl=en&lr=&id=L4lIDwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+process&ots=AgiRYIf
6YW&sig=gv0HP9tKGBTPIbV7XlSdWkukcRo#v=onepage&q=nursing
%20process&f=false
DeVore, J., Clontz, A., Ren, D., Cairns, L., & Beach, M. (2017).Improving patient satisfaction
with better pain management in hospitalized patients. The Journal for Nurse
Practitioners, 13(1), e23-e27. DOI: https://doi.org/10.1016/j.nurpra.2016.07.020
Hering, D., Kara, T., Kucharska, W., Somers, V. K., &Narkiewicz, K. (2016).Longitudinal
tracking of muscle sympathetic nerve activity and its relationship with blood pressure in
subjects with prehypertension. Blood pressure, 25(3), 184-192. DOI:
https://doi.org/10.3109/08037051.2015.1121708
Jain, K. K. (2017). Physical, physiological, and biochemical aspects of hyperbaric oxygenation.
In Textbook of hyperbaric medicine (pp. 11-22). Springer, Cham.
Khan, J. S., Devereaux, P. J., LeManach, Y., &Busse, J. W. (2016). Patient coping and
expectations about recovery predict the development of chronic post-surgical pain after
traumatic tibial fracture repair. British journal of anaesthesia, 117(3), 365-370. DOI:
https://doi.org/10.1093/bja/aew225
Lehne, R. A., & Rosenthal, L. (2014). Pharmacology for Nursing Care-E-Book.Elsevier Health
Sciences. Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=udTsAwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+pharmacology&ots=s
Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. (2018). Nursing
Interventions classification (NIC)-E-Book.Elsevier Health Sciences. Retrieved from
https://books.google.co.in/books?
hl=en&lr=&id=L4lIDwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+process&ots=AgiRYIf
6YW&sig=gv0HP9tKGBTPIbV7XlSdWkukcRo#v=onepage&q=nursing
%20process&f=false
DeVore, J., Clontz, A., Ren, D., Cairns, L., & Beach, M. (2017).Improving patient satisfaction
with better pain management in hospitalized patients. The Journal for Nurse
Practitioners, 13(1), e23-e27. DOI: https://doi.org/10.1016/j.nurpra.2016.07.020
Hering, D., Kara, T., Kucharska, W., Somers, V. K., &Narkiewicz, K. (2016).Longitudinal
tracking of muscle sympathetic nerve activity and its relationship with blood pressure in
subjects with prehypertension. Blood pressure, 25(3), 184-192. DOI:
https://doi.org/10.3109/08037051.2015.1121708
Jain, K. K. (2017). Physical, physiological, and biochemical aspects of hyperbaric oxygenation.
In Textbook of hyperbaric medicine (pp. 11-22). Springer, Cham.
Khan, J. S., Devereaux, P. J., LeManach, Y., &Busse, J. W. (2016). Patient coping and
expectations about recovery predict the development of chronic post-surgical pain after
traumatic tibial fracture repair. British journal of anaesthesia, 117(3), 365-370. DOI:
https://doi.org/10.1093/bja/aew225
Lehne, R. A., & Rosenthal, L. (2014). Pharmacology for Nursing Care-E-Book.Elsevier Health
Sciences. Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=udTsAwAAQBAJ&oi=fnd&pg=PP1&dq=nursing+pharmacology&ots=s
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





