Nursing Care Plan for LINA: Clinical Reasoning Cycle and Interventions
VerifiedAdded on 2022/10/04
|6
|797
|21
Practical Assignment
AI Summary
This assignment presents a detailed nursing care plan for a LINA case study, focusing on the application of the Clinical Reasoning Cycle. The plan outlines four SMART goals aimed at improving mobilization, providing pain relief, promoting sleep, and enhancing functional independence. It describes specific nursing interventions to manage self-care deficits, emphasizing ADL and IADL assessments. The evaluation process includes regular assessments using the FIM scale and consideration of environmental risk factors. The reflection section highlights the sources of self-care deficits and the importance of a holistic, both biomedical and humanistic, approach to nursing care. The assignment includes relevant references and picture links to support the content.
Nursing Care Plan
LINA CASE STUDY
LINA CASE STUDY
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning Cycle step 5
Based on the patient situation and the nursing diagnosis – the following SMART Goals are established :-
• GOAL 1 – Improving mobilization – by controlling pain and by promoting ADLs and IADLs. Goal to be achieved in 1 week .
Regular ADL assessments will be done.
• GOAL 2 - Pain relief – is an important goal in the management of Lina’s case. Administering the pain relief medications
timely along proper positing and immobilization- mobilisation nursing strategy is important to manage the low back pain and
compression fracture L2. Goal to achieved in 3- 4 weeks. Numerical pain assessment scales will be used (Sandqvist et al.,
2018)
• GOAL 3 – Promoting sleep – is a vital goal which is impacted by fracture and pain. Goal to be achieved in 1 week. Stress and
anxiety assessment scales will be used and shall be correlated Epworth Sleepiness scale.
• GOAL 4 : Improved Functional Independence - As Lina has self care, mobility, physiological band cognitive deficits
pertaining to ADLs and IADLs ( as identified in the stage 2 of clinical reasoning cycle) – ADL training, counselling and
cognitive assistance has to be an important aspect of nursing case plan. Goal to be achieved in 5 weeks. The Functional
Independence Measurement (FIM) tool will be used for evaluation.
• Picture link –
https://tlcsr.com/assisted-living-facility-alf
/activities-of-daily-living-adls/
Based on the patient situation and the nursing diagnosis – the following SMART Goals are established :-
• GOAL 1 – Improving mobilization – by controlling pain and by promoting ADLs and IADLs. Goal to be achieved in 1 week .
Regular ADL assessments will be done.
• GOAL 2 - Pain relief – is an important goal in the management of Lina’s case. Administering the pain relief medications
timely along proper positing and immobilization- mobilisation nursing strategy is important to manage the low back pain and
compression fracture L2. Goal to achieved in 3- 4 weeks. Numerical pain assessment scales will be used (Sandqvist et al.,
2018)
• GOAL 3 – Promoting sleep – is a vital goal which is impacted by fracture and pain. Goal to be achieved in 1 week. Stress and
anxiety assessment scales will be used and shall be correlated Epworth Sleepiness scale.
• GOAL 4 : Improved Functional Independence - As Lina has self care, mobility, physiological band cognitive deficits
pertaining to ADLs and IADLs ( as identified in the stage 2 of clinical reasoning cycle) – ADL training, counselling and
cognitive assistance has to be an important aspect of nursing case plan. Goal to be achieved in 5 weeks. The Functional
Independence Measurement (FIM) tool will be used for evaluation.
• Picture link –
https://tlcsr.com/assisted-living-facility-alf
/activities-of-daily-living-adls/
Clinical Reasoning Cycle step 6
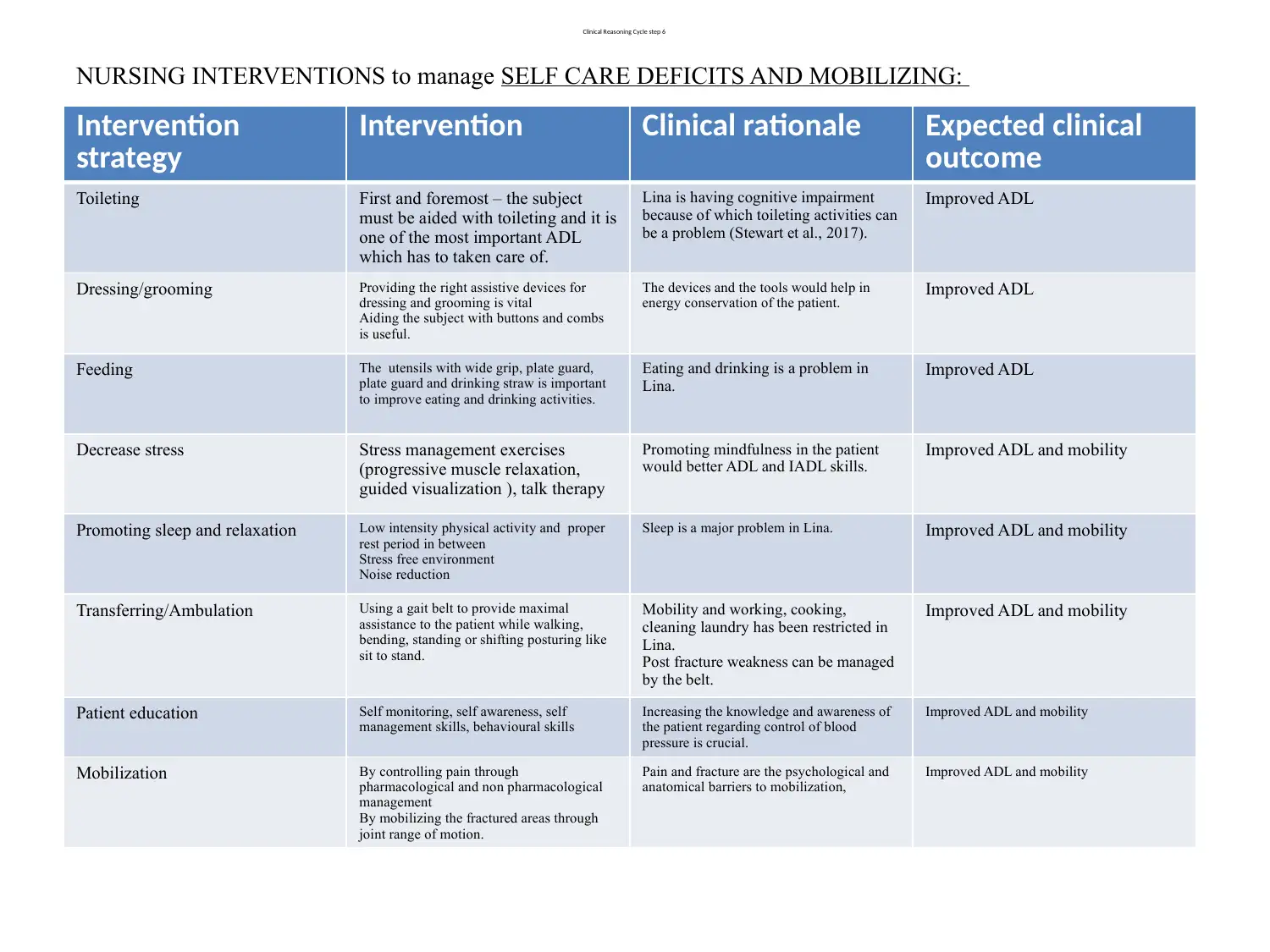
NURSING INTERVENTIONS to manage SELF CARE DEFICITS AND MOBILIZING:
Intervention
strategy
Intervention Clinical rationale Expected clinical
outcome
Toileting First and foremost – the subject
must be aided with toileting and it is
one of the most important ADL
which has to taken care of.
Lina is having cognitive impairment
because of which toileting activities can
be a problem (Stewart et al., 2017).
Improved ADL
Dressing/grooming Providing the right assistive devices for
dressing and grooming is vital
Aiding the subject with buttons and combs
is useful.
The devices and the tools would help in
energy conservation of the patient. Improved ADL
Feeding The utensils with wide grip, plate guard,
plate guard and drinking straw is important
to improve eating and drinking activities.
Eating and drinking is a problem in
Lina.
Improved ADL
Decrease stress Stress management exercises
(progressive muscle relaxation,
guided visualization ), talk therapy
Promoting mindfulness in the patient
would better ADL and IADL skills.
Improved ADL and mobility
Promoting sleep and relaxation Low intensity physical activity and proper
rest period in between
Stress free environment
Noise reduction
Sleep is a major problem in Lina. Improved ADL and mobility
Transferring/Ambulation Using a gait belt to provide maximal
assistance to the patient while walking,
bending, standing or shifting posturing like
sit to stand.
Mobility and working, cooking,
cleaning laundry has been restricted in
Lina.
Post fracture weakness can be managed
by the belt.
Improved ADL and mobility
Patient education Self monitoring, self awareness, self
management skills, behavioural skills
Increasing the knowledge and awareness of
the patient regarding control of blood
pressure is crucial.
Improved ADL and mobility
Mobilization By controlling pain through
pharmacological and non pharmacological
management
By mobilizing the fractured areas through
joint range of motion.
Pain and fracture are the psychological and
anatomical barriers to mobilization,
Improved ADL and mobility
NURSING INTERVENTIONS to manage SELF CARE DEFICITS AND MOBILIZING:
Intervention
strategy
Intervention Clinical rationale Expected clinical
outcome
Toileting First and foremost – the subject
must be aided with toileting and it is
one of the most important ADL
which has to taken care of.
Lina is having cognitive impairment
because of which toileting activities can
be a problem (Stewart et al., 2017).
Improved ADL
Dressing/grooming Providing the right assistive devices for
dressing and grooming is vital
Aiding the subject with buttons and combs
is useful.
The devices and the tools would help in
energy conservation of the patient. Improved ADL
Feeding The utensils with wide grip, plate guard,
plate guard and drinking straw is important
to improve eating and drinking activities.
Eating and drinking is a problem in
Lina.
Improved ADL
Decrease stress Stress management exercises
(progressive muscle relaxation,
guided visualization ), talk therapy
Promoting mindfulness in the patient
would better ADL and IADL skills.
Improved ADL and mobility
Promoting sleep and relaxation Low intensity physical activity and proper
rest period in between
Stress free environment
Noise reduction
Sleep is a major problem in Lina. Improved ADL and mobility
Transferring/Ambulation Using a gait belt to provide maximal
assistance to the patient while walking,
bending, standing or shifting posturing like
sit to stand.
Mobility and working, cooking,
cleaning laundry has been restricted in
Lina.
Post fracture weakness can be managed
by the belt.
Improved ADL and mobility
Patient education Self monitoring, self awareness, self
management skills, behavioural skills
Increasing the knowledge and awareness of
the patient regarding control of blood
pressure is crucial.
Improved ADL and mobility
Mobilization By controlling pain through
pharmacological and non pharmacological
management
By mobilizing the fractured areas through
joint range of motion.
Pain and fracture are the psychological and
anatomical barriers to mobilization,
Improved ADL and mobility
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Clinical Reasoning Cycle Step 7
Nursing Evaluation:
• The nursing evaluation will include regular ADL and IADL assessments (Benetos et al.,
2015). A FIM scale will be used to evaluate the subject’s functional independence.
• The environmental risk factors should be assessed, managed and prevented by the nurse to
reduce the incidences of falls and any restriction impended to the ADL improvement
(Vedanthan et al., 2015).
• The major ADL lacking areas of the patient is communication, eating, drinking, sleeping,
mobilizing, working – hence after the ADL assistance is provided in this areas, the ADL
assessment pertaining to the same has to be performed.
• The cardinal IADL lacking areas are cooking, cleaning, laundry, transportation – ADL and
mobility assessments are to be taken.
Picture link - http://www.priva.care/2017/05/activities-daily-living-adls/
Nursing Evaluation:
• The nursing evaluation will include regular ADL and IADL assessments (Benetos et al.,
2015). A FIM scale will be used to evaluate the subject’s functional independence.
• The environmental risk factors should be assessed, managed and prevented by the nurse to
reduce the incidences of falls and any restriction impended to the ADL improvement
(Vedanthan et al., 2015).
• The major ADL lacking areas of the patient is communication, eating, drinking, sleeping,
mobilizing, working – hence after the ADL assistance is provided in this areas, the ADL
assessment pertaining to the same has to be performed.
• The cardinal IADL lacking areas are cooking, cleaning, laundry, transportation – ADL and
mobility assessments are to be taken.
Picture link - http://www.priva.care/2017/05/activities-daily-living-adls/
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Clinical Reasoning Cycle Step 8
Nursing Reflection
During management of Lina, I learned that self care deficits has different
sources ( that is different sets of origin). The self care deficits generally occurs due to
cognitive impairment and acute confusional states in addition to physical and
physiological restrictions which in this case was lumbar fracture and the resultant pain.
I learned that the nursing approach to the improvement of self care deficit should be
holistic and it should be intervened with both biomedical and humanistic processes.
Picture link - https://www.kindlycare.com/activities-of-daily-living/
Nursing Reflection
During management of Lina, I learned that self care deficits has different
sources ( that is different sets of origin). The self care deficits generally occurs due to
cognitive impairment and acute confusional states in addition to physical and
physiological restrictions which in this case was lumbar fracture and the resultant pain.
I learned that the nursing approach to the improvement of self care deficit should be
holistic and it should be intervened with both biomedical and humanistic processes.
Picture link - https://www.kindlycare.com/activities-of-daily-living/
References
Benetos, A., Labat, C., Rossignol, P., Fay, R., Rolland, Y., Valbusa, F., ... & Gautier, S. (2015).
Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older
nursing home residents: the PARTAGE study. JAMA internal medicine, 175(6), 989-995.
Sandqvist, G., Wollmer, P., Scheja, A., Wildt, M., & Hesselstrand, R. (2018). Raynaud’s phenomenon
and its impact on activities in daily life during one year of follow-up in early systemic sclerosis.
Scandinavian journal of rheumatology, 47(3), 206-209
Stewart, C. D., Saint-Hilaire, M., Thomas, C. A., & Tickle-Degnen, L. (2017). The Association of
Energy Depletion Problems With Retention of Daily Life Activities in People With Parkinson’s Disease.
American Journal of Occupational Therapy, 71(4_Supplement_1), 7111500039p1-7111500039p1.
Vedanthan, R., Blank, E., Tuikong, N., Kamano, J., Misoi, L., Tulienge, D., ... & Were, M. C. (2015).
Usability and feasibility of a tablet-based Decision-Support and Integrated Record-keeping (DESIRE)
tool in the nurse management of hypertension in rural western Kenya. International journal of medical
informatics, 84(3), 207-219.
.
Picture link - https://tlcsr.com/assisted-living-facility-alf/activities-of-daily-living-adls/
Picture link - https://www.kindlycare.com/activities-of-daily-living/
Picture link - http://www.priva.care/2017/05/activities-daily-living-adls
Benetos, A., Labat, C., Rossignol, P., Fay, R., Rolland, Y., Valbusa, F., ... & Gautier, S. (2015).
Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older
nursing home residents: the PARTAGE study. JAMA internal medicine, 175(6), 989-995.
Sandqvist, G., Wollmer, P., Scheja, A., Wildt, M., & Hesselstrand, R. (2018). Raynaud’s phenomenon
and its impact on activities in daily life during one year of follow-up in early systemic sclerosis.
Scandinavian journal of rheumatology, 47(3), 206-209
Stewart, C. D., Saint-Hilaire, M., Thomas, C. A., & Tickle-Degnen, L. (2017). The Association of
Energy Depletion Problems With Retention of Daily Life Activities in People With Parkinson’s Disease.
American Journal of Occupational Therapy, 71(4_Supplement_1), 7111500039p1-7111500039p1.
Vedanthan, R., Blank, E., Tuikong, N., Kamano, J., Misoi, L., Tulienge, D., ... & Were, M. C. (2015).
Usability and feasibility of a tablet-based Decision-Support and Integrated Record-keeping (DESIRE)
tool in the nurse management of hypertension in rural western Kenya. International journal of medical
informatics, 84(3), 207-219.
.
Picture link - https://tlcsr.com/assisted-living-facility-alf/activities-of-daily-living-adls/
Picture link - https://www.kindlycare.com/activities-of-daily-living/
Picture link - http://www.priva.care/2017/05/activities-daily-living-adls
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




