HLTENN015 - Case Study: Nursing in Primary Health Care Setting
VerifiedAdded on 2023/04/21
|11
|3776
|297
Case Study
AI Summary
This assignment presents two nursing case studies, one focusing on Mr. Jones, who is diagnosed with an arterial leg ulcer, and the other on Mr. Smith, who suffers from COPD and social isolation. For Mr. Jones, the nursing diagnosis involves assessing and managing the leg ulcer through compression therapy, pharmacological interventions for pain, and patient education on self-management, with regular evaluations of healing progress and mobility. The care plan includes a pre-visit checklist and identification of community resources. For Mr. Smith, the nursing diagnosis addresses his COPD, smoking habits, and social isolation by promoting social interaction, smoking cessation, lung assessment, and improved nutrition, also involving community resources and regular evaluations of his lifestyle changes and lung functionality. Both case studies emphasize comprehensive care, patient education, and the importance of community support in managing chronic conditions. Desklib provides solved assignments and past papers for students.
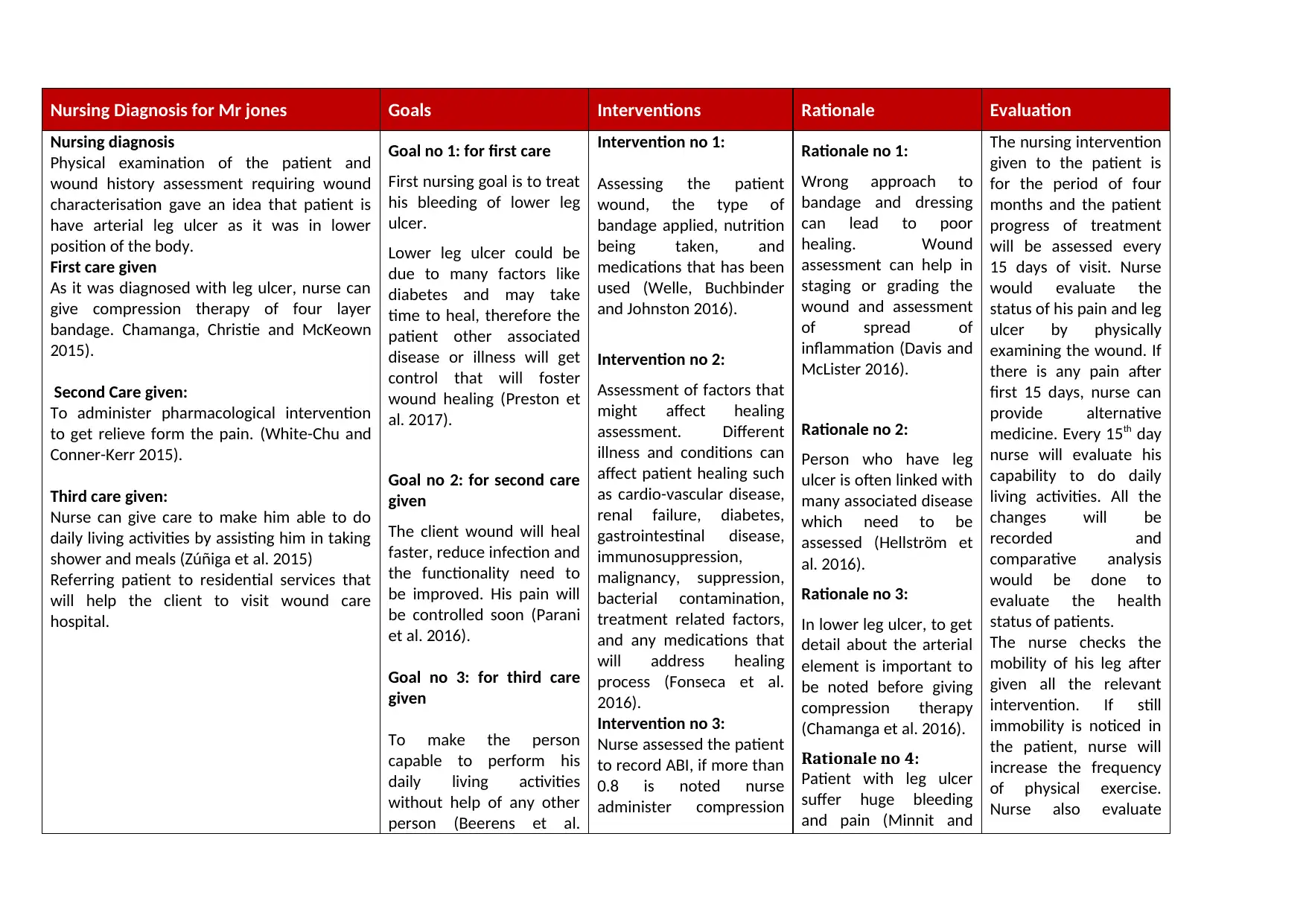
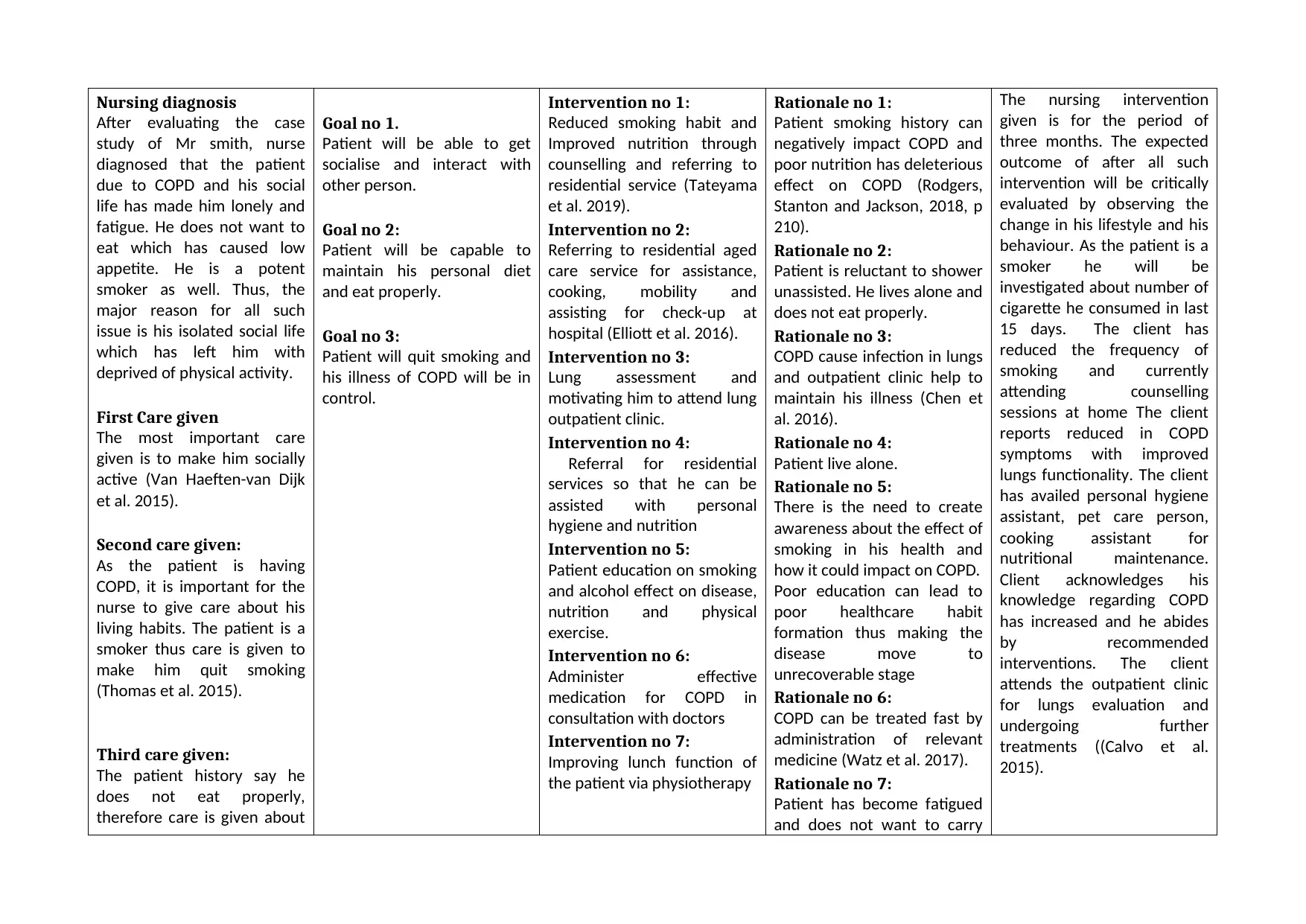
Nursing Diagnosis for Mr jones Goals Interventions Rationale Evaluation
Nursing diagnosis
Physical examination of the patient and
wound history assessment requiring wound
characterisation gave an idea that patient is
have arterial leg ulcer as it was in lower
position of the body.
First care given
As it was diagnosed with leg ulcer, nurse can
give compression therapy of four layer
bandage. Chamanga, Christie and McKeown
2015).
Second Care given:
To administer pharmacological intervention
to get relieve form the pain. (White-Chu and
Conner-Kerr 2015).
Third care given:
Nurse can give care to make him able to do
daily living activities by assisting him in taking
shower and meals (Zúñiga et al. 2015)
Referring patient to residential services that
will help the client to visit wound care
hospital.
Goal no 1: for first care
First nursing goal is to treat
his bleeding of lower leg
ulcer.
Lower leg ulcer could be
due to many factors like
diabetes and may take
time to heal, therefore the
patient other associated
disease or illness will get
control that will foster
wound healing (Preston et
al. 2017).
Goal no 2: for second care
given
The client wound will heal
faster, reduce infection and
the functionality need to
be improved. His pain will
be controlled soon (Parani
et al. 2016).
Goal no 3: for third care
given
To make the person
capable to perform his
daily living activities
without help of any other
person (Beerens et al.
Intervention no 1:
Assessing the patient
wound, the type of
bandage applied, nutrition
being taken, and
medications that has been
used (Welle, Buchbinder
and Johnston 2016).
Intervention no 2:
Assessment of factors that
might affect healing
assessment. Different
illness and conditions can
affect patient healing such
as cardio-vascular disease,
renal failure, diabetes,
gastrointestinal disease,
immunosuppression,
malignancy, suppression,
bacterial contamination,
treatment related factors,
and any medications that
will address healing
process (Fonseca et al.
2016).
Intervention no 3:
Nurse assessed the patient
to record ABI, if more than
0.8 is noted nurse
administer compression
Rationale no 1:
Wrong approach to
bandage and dressing
can lead to poor
healing. Wound
assessment can help in
staging or grading the
wound and assessment
of spread of
inflammation (Davis and
McLister 2016).
Rationale no 2:
Person who have leg
ulcer is often linked with
many associated disease
which need to be
assessed (Hellström et
al. 2016).
Rationale no 3:
In lower leg ulcer, to get
detail about the arterial
element is important to
be noted before giving
compression therapy
(Chamanga et al. 2016).
Rationale no 4:
Patient with leg ulcer
suffer huge bleeding
and pain (Minnit and
The nursing intervention
given to the patient is
for the period of four
months and the patient
progress of treatment
will be assessed every
15 days of visit. Nurse
would evaluate the
status of his pain and leg
ulcer by physically
examining the wound. If
there is any pain after
first 15 days, nurse can
provide alternative
medicine. Every 15th day
nurse will evaluate his
capability to do daily
living activities. All the
changes will be
recorded and
comparative analysis
would be done to
evaluate the health
status of patients.
The nurse checks the
mobility of his leg after
given all the relevant
intervention. If still
immobility is noticed in
the patient, nurse will
increase the frequency
of physical exercise.
Nurse also evaluate
Nursing diagnosis
Physical examination of the patient and
wound history assessment requiring wound
characterisation gave an idea that patient is
have arterial leg ulcer as it was in lower
position of the body.
First care given
As it was diagnosed with leg ulcer, nurse can
give compression therapy of four layer
bandage. Chamanga, Christie and McKeown
2015).
Second Care given:
To administer pharmacological intervention
to get relieve form the pain. (White-Chu and
Conner-Kerr 2015).
Third care given:
Nurse can give care to make him able to do
daily living activities by assisting him in taking
shower and meals (Zúñiga et al. 2015)
Referring patient to residential services that
will help the client to visit wound care
hospital.
Goal no 1: for first care
First nursing goal is to treat
his bleeding of lower leg
ulcer.
Lower leg ulcer could be
due to many factors like
diabetes and may take
time to heal, therefore the
patient other associated
disease or illness will get
control that will foster
wound healing (Preston et
al. 2017).
Goal no 2: for second care
given
The client wound will heal
faster, reduce infection and
the functionality need to
be improved. His pain will
be controlled soon (Parani
et al. 2016).
Goal no 3: for third care
given
To make the person
capable to perform his
daily living activities
without help of any other
person (Beerens et al.
Intervention no 1:
Assessing the patient
wound, the type of
bandage applied, nutrition
being taken, and
medications that has been
used (Welle, Buchbinder
and Johnston 2016).
Intervention no 2:
Assessment of factors that
might affect healing
assessment. Different
illness and conditions can
affect patient healing such
as cardio-vascular disease,
renal failure, diabetes,
gastrointestinal disease,
immunosuppression,
malignancy, suppression,
bacterial contamination,
treatment related factors,
and any medications that
will address healing
process (Fonseca et al.
2016).
Intervention no 3:
Nurse assessed the patient
to record ABI, if more than
0.8 is noted nurse
administer compression
Rationale no 1:
Wrong approach to
bandage and dressing
can lead to poor
healing. Wound
assessment can help in
staging or grading the
wound and assessment
of spread of
inflammation (Davis and
McLister 2016).
Rationale no 2:
Person who have leg
ulcer is often linked with
many associated disease
which need to be
assessed (Hellström et
al. 2016).
Rationale no 3:
In lower leg ulcer, to get
detail about the arterial
element is important to
be noted before giving
compression therapy
(Chamanga et al. 2016).
Rationale no 4:
Patient with leg ulcer
suffer huge bleeding
and pain (Minnit and
The nursing intervention
given to the patient is
for the period of four
months and the patient
progress of treatment
will be assessed every
15 days of visit. Nurse
would evaluate the
status of his pain and leg
ulcer by physically
examining the wound. If
there is any pain after
first 15 days, nurse can
provide alternative
medicine. Every 15th day
nurse will evaluate his
capability to do daily
living activities. All the
changes will be
recorded and
comparative analysis
would be done to
evaluate the health
status of patients.
The nurse checks the
mobility of his leg after
given all the relevant
intervention. If still
immobility is noticed in
the patient, nurse will
increase the frequency
of physical exercise.
Nurse also evaluate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing Diagnosis for Mr jones Goals Interventions Rationale Evaluation
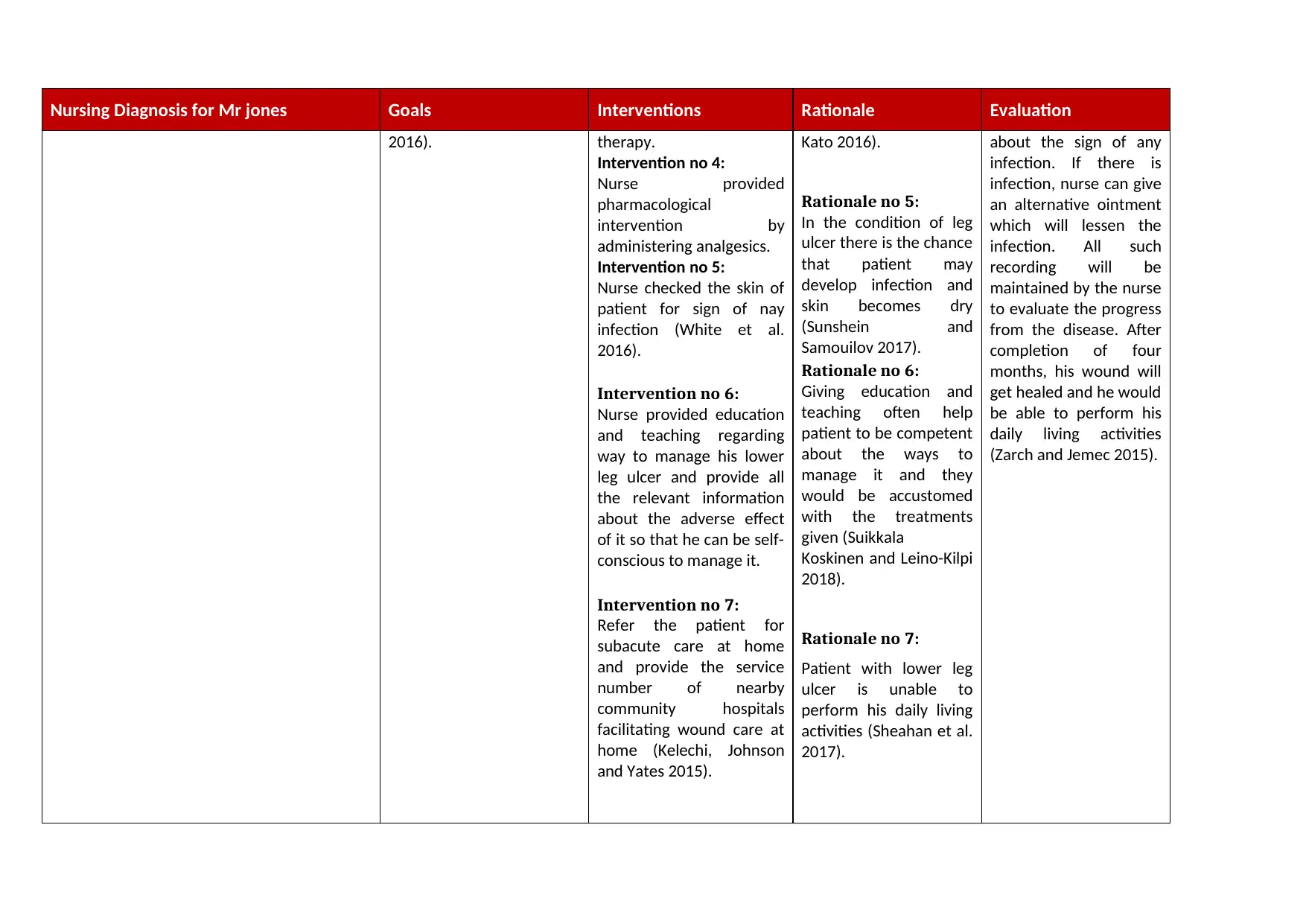
2016). therapy.
Intervention no 4:
Nurse provided
pharmacological
intervention by
administering analgesics.
Intervention no 5:
Nurse checked the skin of
patient for sign of nay
infection (White et al.
2016).
Intervention no 6:
Nurse provided education
and teaching regarding
way to manage his lower
leg ulcer and provide all
the relevant information
about the adverse effect
of it so that he can be self-
conscious to manage it.
Intervention no 7:
Refer the patient for
subacute care at home
and provide the service
number of nearby
community hospitals
facilitating wound care at
home (Kelechi, Johnson
and Yates 2015).
Kato 2016).
Rationale no 5:
In the condition of leg
ulcer there is the chance
that patient may
develop infection and
skin becomes dry
(Sunshein and
Samouilov 2017).
Rationale no 6:
Giving education and
teaching often help
patient to be competent
about the ways to
manage it and they
would be accustomed
with the treatments
given (Suikkala
Koskinen and Leino-Kilpi
2018).
Rationale no 7:
Patient with lower leg
ulcer is unable to
perform his daily living
activities (Sheahan et al.
2017).
about the sign of any
infection. If there is
infection, nurse can give
an alternative ointment
which will lessen the
infection. All such
recording will be
maintained by the nurse
to evaluate the progress
from the disease. After
completion of four
months, his wound will
get healed and he would
be able to perform his
daily living activities
(Zarch and Jemec 2015).
2016). therapy.
Intervention no 4:
Nurse provided
pharmacological
intervention by
administering analgesics.
Intervention no 5:
Nurse checked the skin of
patient for sign of nay
infection (White et al.
2016).
Intervention no 6:
Nurse provided education
and teaching regarding
way to manage his lower
leg ulcer and provide all
the relevant information
about the adverse effect
of it so that he can be self-
conscious to manage it.
Intervention no 7:
Refer the patient for
subacute care at home
and provide the service
number of nearby
community hospitals
facilitating wound care at
home (Kelechi, Johnson
and Yates 2015).
Kato 2016).
Rationale no 5:
In the condition of leg
ulcer there is the chance
that patient may
develop infection and
skin becomes dry
(Sunshein and
Samouilov 2017).
Rationale no 6:
Giving education and
teaching often help
patient to be competent
about the ways to
manage it and they
would be accustomed
with the treatments
given (Suikkala
Koskinen and Leino-Kilpi
2018).
Rationale no 7:
Patient with lower leg
ulcer is unable to
perform his daily living
activities (Sheahan et al.
2017).
about the sign of any
infection. If there is
infection, nurse can give
an alternative ointment
which will lessen the
infection. All such
recording will be
maintained by the nurse
to evaluate the progress
from the disease. After
completion of four
months, his wound will
get healed and he would
be able to perform his
daily living activities
(Zarch and Jemec 2015).
Nursing Diagnosis for Mr jones Goals Interventions Rationale Evaluation
Pre-visit checklist of Mr Jones:
1. Is the patient able to walk?
2. Is there any medical history related to leg trauma or deep vein thrombosis?
3. Is he having problem with mobility?
4. Any sign of skin allergy?
5. Does patient had dermatitis in future?
6. Anyone in the family ever had venous or arterial leg ulcer?
7. Is patient allergic to any kind of medicine?
8. Does patient need assistance in shower?
9. What are the medication he is currently taking?
10. Is he having pain? If yes where?
Identified community and other resource:
1. Professional driver to take him to hospital from his home.
2. Physiotherapist to make his leg ulcer treatment fast.
3. Domestic helper to assist him in his daily living activities (Garvey et al. 2015).
Identification of ways to access the community and other resource:
1. By contacting the concern person who can give assistance
2. By searching online through mean of advertisement
Assessment of nursing intervention given to Mr Jones:
Nurse would keep regular monitoring on healing process of leg ulcer by physical examination of wound. The wound is checked every week and nurse
checked the status of pain by giving slight pressure. There is the 90% chance that intervention given will treat his leg ulcer and he would be able do his daily living
activities
Documentation done on arrival nurse in case of Mr Jones:
The documents must involve client consent form, assessments carried out, intervention and follow up. The referral service and patient education facilitated.
1. Nurse introduced herself and asked about good name of patient
Pre-visit checklist of Mr Jones:
1. Is the patient able to walk?
2. Is there any medical history related to leg trauma or deep vein thrombosis?
3. Is he having problem with mobility?
4. Any sign of skin allergy?
5. Does patient had dermatitis in future?
6. Anyone in the family ever had venous or arterial leg ulcer?
7. Is patient allergic to any kind of medicine?
8. Does patient need assistance in shower?
9. What are the medication he is currently taking?
10. Is he having pain? If yes where?
Identified community and other resource:
1. Professional driver to take him to hospital from his home.
2. Physiotherapist to make his leg ulcer treatment fast.
3. Domestic helper to assist him in his daily living activities (Garvey et al. 2015).
Identification of ways to access the community and other resource:
1. By contacting the concern person who can give assistance
2. By searching online through mean of advertisement
Assessment of nursing intervention given to Mr Jones:
Nurse would keep regular monitoring on healing process of leg ulcer by physical examination of wound. The wound is checked every week and nurse
checked the status of pain by giving slight pressure. There is the 90% chance that intervention given will treat his leg ulcer and he would be able do his daily living
activities
Documentation done on arrival nurse in case of Mr Jones:
The documents must involve client consent form, assessments carried out, intervention and follow up. The referral service and patient education facilitated.
1. Nurse introduced herself and asked about good name of patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2. Nurse documented his current status of leg ulcer
3. Nurse documented about patient’s medical history
4. Nurse noted sign of allergy or infection in the skin
5. Nurse noted the vital signs
6. Nurse documented about current status of pain
7. Nurse asked about the current medicine he is taking
8. Nurse noted any allergy to current medicine he is having.
Specific documentation the need to be done after home visit to Mr Jones:
Nurse visit to Mr Jones gave many data about his status of leg ulcer. Nurse would document those changes that has happen in course of treatment. Nurse
document the status of his leg ulcer and all the assessment made for evaluating pain. Nurse notes all the changed medicine that is being given to Mr Jones.
3. Nurse documented about patient’s medical history
4. Nurse noted sign of allergy or infection in the skin
5. Nurse noted the vital signs
6. Nurse documented about current status of pain
7. Nurse asked about the current medicine he is taking
8. Nurse noted any allergy to current medicine he is having.
Specific documentation the need to be done after home visit to Mr Jones:
Nurse visit to Mr Jones gave many data about his status of leg ulcer. Nurse would document those changes that has happen in course of treatment. Nurse
document the status of his leg ulcer and all the assessment made for evaluating pain. Nurse notes all the changed medicine that is being given to Mr Jones.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
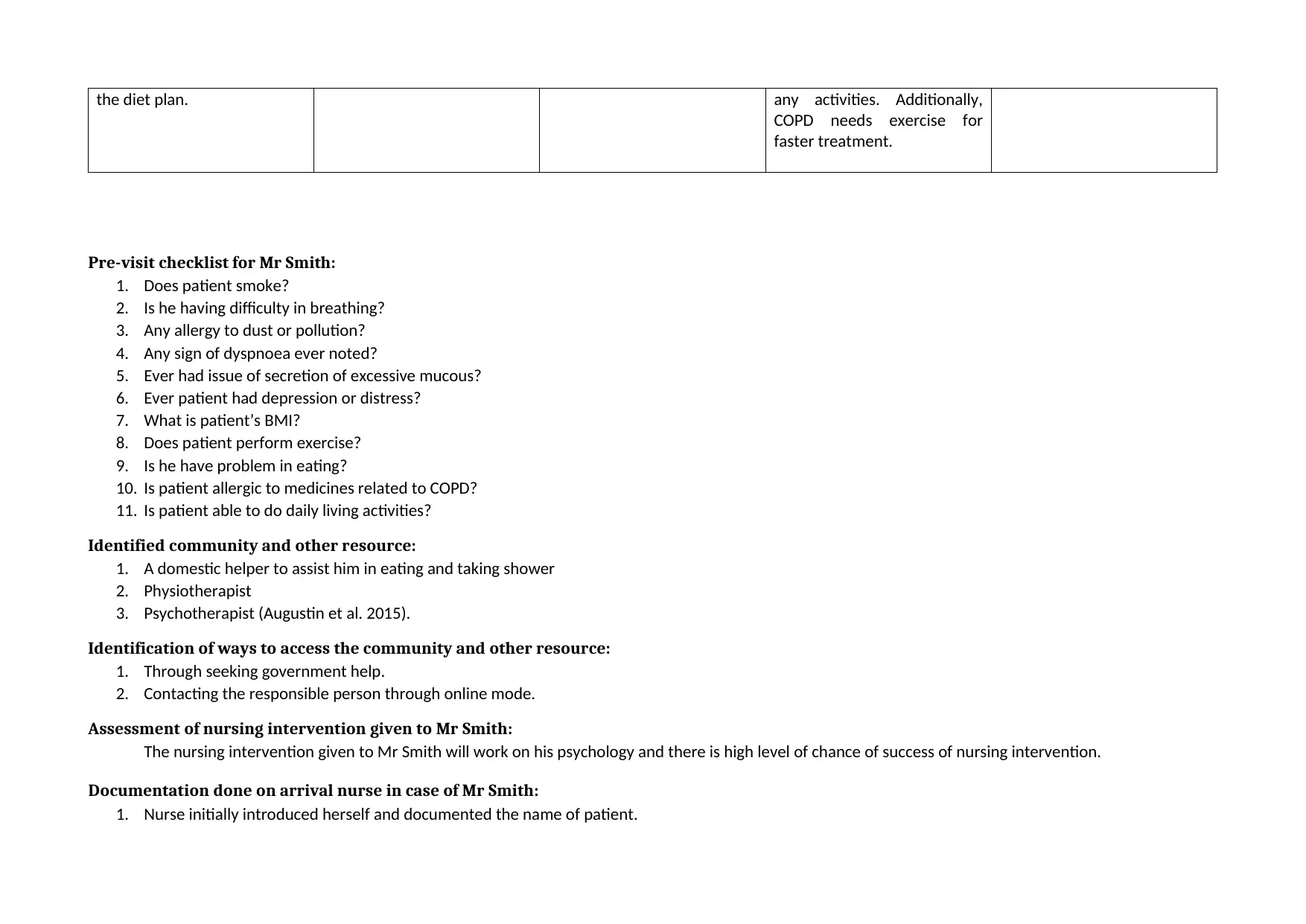
Nursing Diagnosis for Mr
smith Goals Interventions Rationale Evaluation
smith Goals Interventions Rationale Evaluation
Nursing diagnosis
After evaluating the case
study of Mr smith, nurse
diagnosed that the patient
due to COPD and his social
life has made him lonely and
fatigue. He does not want to
eat which has caused low
appetite. He is a potent
smoker as well. Thus, the
major reason for all such
issue is his isolated social life
which has left him with
deprived of physical activity.
First Care given
The most important care
given is to make him socially
active (Van Haeften-van Dijk
et al. 2015).
Second care given:
As the patient is having
COPD, it is important for the
nurse to give care about his
living habits. The patient is a
smoker thus care is given to
make him quit smoking
(Thomas et al. 2015).
Third care given:
The patient history say he
does not eat properly,
therefore care is given about
Goal no 1.
Patient will be able to get
socialise and interact with
other person.
Goal no 2:
Patient will be capable to
maintain his personal diet
and eat properly.
Goal no 3:
Patient will quit smoking and
his illness of COPD will be in
control.
Intervention no 1:
Reduced smoking habit and
Improved nutrition through
counselling and referring to
residential service (Tateyama
et al. 2019).
Intervention no 2:
Referring to residential aged
care service for assistance,
cooking, mobility and
assisting for check-up at
hospital (Elliott et al. 2016).
Intervention no 3:
Lung assessment and
motivating him to attend lung
outpatient clinic.
Intervention no 4:
Referral for residential
services so that he can be
assisted with personal
hygiene and nutrition
Intervention no 5:
Patient education on smoking
and alcohol effect on disease,
nutrition and physical
exercise.
Intervention no 6:
Administer effective
medication for COPD in
consultation with doctors
Intervention no 7:
Improving lunch function of
the patient via physiotherapy
Rationale no 1:
Patient smoking history can
negatively impact COPD and
poor nutrition has deleterious
effect on COPD (Rodgers,
Stanton and Jackson, 2018, p
210).
Rationale no 2:
Patient is reluctant to shower
unassisted. He lives alone and
does not eat properly.
Rationale no 3:
COPD cause infection in lungs
and outpatient clinic help to
maintain his illness (Chen et
al. 2016).
Rationale no 4:
Patient live alone.
Rationale no 5:
There is the need to create
awareness about the effect of
smoking in his health and
how it could impact on COPD.
Poor education can lead to
poor healthcare habit
formation thus making the
disease move to
unrecoverable stage
Rationale no 6:
COPD can be treated fast by
administration of relevant
medicine (Watz et al. 2017).
Rationale no 7:
Patient has become fatigued
and does not want to carry
The nursing intervention
given is for the period of
three months. The expected
outcome of after all such
intervention will be critically
evaluated by observing the
change in his lifestyle and his
behaviour. As the patient is a
smoker he will be
investigated about number of
cigarette he consumed in last
15 days. The client has
reduced the frequency of
smoking and currently
attending counselling
sessions at home The client
reports reduced in COPD
symptoms with improved
lungs functionality. The client
has availed personal hygiene
assistant, pet care person,
cooking assistant for
nutritional maintenance.
Client acknowledges his
knowledge regarding COPD
has increased and he abides
by recommended
interventions. The client
attends the outpatient clinic
for lungs evaluation and
undergoing further
treatments ((Calvo et al.
2015).
After evaluating the case
study of Mr smith, nurse
diagnosed that the patient
due to COPD and his social
life has made him lonely and
fatigue. He does not want to
eat which has caused low
appetite. He is a potent
smoker as well. Thus, the
major reason for all such
issue is his isolated social life
which has left him with
deprived of physical activity.
First Care given
The most important care
given is to make him socially
active (Van Haeften-van Dijk
et al. 2015).
Second care given:
As the patient is having
COPD, it is important for the
nurse to give care about his
living habits. The patient is a
smoker thus care is given to
make him quit smoking
(Thomas et al. 2015).
Third care given:
The patient history say he
does not eat properly,
therefore care is given about
Goal no 1.
Patient will be able to get
socialise and interact with
other person.
Goal no 2:
Patient will be capable to
maintain his personal diet
and eat properly.
Goal no 3:
Patient will quit smoking and
his illness of COPD will be in
control.
Intervention no 1:
Reduced smoking habit and
Improved nutrition through
counselling and referring to
residential service (Tateyama
et al. 2019).
Intervention no 2:
Referring to residential aged
care service for assistance,
cooking, mobility and
assisting for check-up at
hospital (Elliott et al. 2016).
Intervention no 3:
Lung assessment and
motivating him to attend lung
outpatient clinic.
Intervention no 4:
Referral for residential
services so that he can be
assisted with personal
hygiene and nutrition
Intervention no 5:
Patient education on smoking
and alcohol effect on disease,
nutrition and physical
exercise.
Intervention no 6:
Administer effective
medication for COPD in
consultation with doctors
Intervention no 7:
Improving lunch function of
the patient via physiotherapy
Rationale no 1:
Patient smoking history can
negatively impact COPD and
poor nutrition has deleterious
effect on COPD (Rodgers,
Stanton and Jackson, 2018, p
210).
Rationale no 2:
Patient is reluctant to shower
unassisted. He lives alone and
does not eat properly.
Rationale no 3:
COPD cause infection in lungs
and outpatient clinic help to
maintain his illness (Chen et
al. 2016).
Rationale no 4:
Patient live alone.
Rationale no 5:
There is the need to create
awareness about the effect of
smoking in his health and
how it could impact on COPD.
Poor education can lead to
poor healthcare habit
formation thus making the
disease move to
unrecoverable stage
Rationale no 6:
COPD can be treated fast by
administration of relevant
medicine (Watz et al. 2017).
Rationale no 7:
Patient has become fatigued
and does not want to carry
The nursing intervention
given is for the period of
three months. The expected
outcome of after all such
intervention will be critically
evaluated by observing the
change in his lifestyle and his
behaviour. As the patient is a
smoker he will be
investigated about number of
cigarette he consumed in last
15 days. The client has
reduced the frequency of
smoking and currently
attending counselling
sessions at home The client
reports reduced in COPD
symptoms with improved
lungs functionality. The client
has availed personal hygiene
assistant, pet care person,
cooking assistant for
nutritional maintenance.
Client acknowledges his
knowledge regarding COPD
has increased and he abides
by recommended
interventions. The client
attends the outpatient clinic
for lungs evaluation and
undergoing further
treatments ((Calvo et al.
2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
the diet plan. any activities. Additionally,
COPD needs exercise for
faster treatment.
Pre-visit checklist for Mr Smith:
1. Does patient smoke?
2. Is he having difficulty in breathing?
3. Any allergy to dust or pollution?
4. Any sign of dyspnoea ever noted?
5. Ever had issue of secretion of excessive mucous?
6. Ever patient had depression or distress?
7. What is patient’s BMI?
8. Does patient perform exercise?
9. Is he have problem in eating?
10. Is patient allergic to medicines related to COPD?
11. Is patient able to do daily living activities?
Identified community and other resource:
1. A domestic helper to assist him in eating and taking shower
2. Physiotherapist
3. Psychotherapist (Augustin et al. 2015).
Identification of ways to access the community and other resource:
1. Through seeking government help.
2. Contacting the responsible person through online mode.
Assessment of nursing intervention given to Mr Smith:
The nursing intervention given to Mr Smith will work on his psychology and there is high level of chance of success of nursing intervention.
Documentation done on arrival nurse in case of Mr Smith:
1. Nurse initially introduced herself and documented the name of patient.
COPD needs exercise for
faster treatment.
Pre-visit checklist for Mr Smith:
1. Does patient smoke?
2. Is he having difficulty in breathing?
3. Any allergy to dust or pollution?
4. Any sign of dyspnoea ever noted?
5. Ever had issue of secretion of excessive mucous?
6. Ever patient had depression or distress?
7. What is patient’s BMI?
8. Does patient perform exercise?
9. Is he have problem in eating?
10. Is patient allergic to medicines related to COPD?
11. Is patient able to do daily living activities?
Identified community and other resource:
1. A domestic helper to assist him in eating and taking shower
2. Physiotherapist
3. Psychotherapist (Augustin et al. 2015).
Identification of ways to access the community and other resource:
1. Through seeking government help.
2. Contacting the responsible person through online mode.
Assessment of nursing intervention given to Mr Smith:
The nursing intervention given to Mr Smith will work on his psychology and there is high level of chance of success of nursing intervention.
Documentation done on arrival nurse in case of Mr Smith:
1. Nurse initially introduced herself and documented the name of patient.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2. Nurse asked about his present problem
3. Nurse documented patients medical history
4. Nurse recorded his vital sign by examining his blood pressure, pulse rate, heart rate and temperature
5. Nurse documented about his current status of breathing
6. Nurse noted his current medication
7. Nurse noted his daily activities
Specific documentation the need to be done after home visit to Mr Smith
Nurse after visiting from home, will document each changes note on the behaviour of the patient. Nurse will gather those vital signs which has showed
some changes from the previous recording. The medicine given to the patient will be documented with time and size of dose. Nurse will note progress in
treatment of COPD and compare from previous files.
Outcome of the evaluation of Mr Jones and Mr Smith
After evaluating the outcome of the Mr Jones and Mr Smith, all the information will be summarised and communicated to the concern host organisation
who havw arranged home visit care. Further, information will be communicated to health care professional to give all the important information about the
patients. This is done because if there will be need to make some changes in course of treatment, the care provider can easily assess them.
3. Nurse documented patients medical history
4. Nurse recorded his vital sign by examining his blood pressure, pulse rate, heart rate and temperature
5. Nurse documented about his current status of breathing
6. Nurse noted his current medication
7. Nurse noted his daily activities
Specific documentation the need to be done after home visit to Mr Smith
Nurse after visiting from home, will document each changes note on the behaviour of the patient. Nurse will gather those vital signs which has showed
some changes from the previous recording. The medicine given to the patient will be documented with time and size of dose. Nurse will note progress in
treatment of COPD and compare from previous files.
Outcome of the evaluation of Mr Jones and Mr Smith
After evaluating the outcome of the Mr Jones and Mr Smith, all the information will be summarised and communicated to the concern host organisation
who havw arranged home visit care. Further, information will be communicated to health care professional to give all the important information about the
patients. This is done because if there will be need to make some changes in course of treatment, the care provider can easily assess them.
Reference
Augustin, M., Brocatti, L.K., Rustenbach, S.J., Schäfer, I. and Herberger, K., 2014. Cost of illness of leg ulcers in the community.‐ ‐ International wound journal, 11(3),
pp.283-292.
Beerens, H.C., de Boer, B., Zwakhalen, S.M., Tan, F.E., Ruwaard, D., Hamers, J.P. and Verbeek, H., 2016. The association between aspects of daily life and quality of
life of people with dementia living in long-term care facilities: a momentary assessment study. International psychogeriatrics, 28(8), pp.1323-1331.
Calvo, G.S., Gómez-Suárez, C., Soriano, J.B., Zamora, E., Gónzalez-Gamarra, A., González-Béjar, M., Jordán, A., Tadeo, E., Sebastián, A., Fernández, G. and
Ancochea, J., 2014. A home telehealth program for patients with severe COPD: the PROMETE study. Respiratory medicine, 108(3), pp.453-462.
Chamanga, E., Christie, J. and McKeown, E., 2015. Community nurses' experiences of treating patients with leg ulcers. Journal of community nursing, 28(6), pp.27-
34.
Chamanga, E.T., 2016. Managing leg ulcers in primary care. Nurs Practice, pp.68-71.
Chen, K.H., Liu, C.Y., Shyu, Y.I.L. and Yeh, S.L., 2016. Living with chronic obstructive pulmonary disease: The process of self-managing chronic obstructive
pulmonary disease. Journal of Nursing Research, 24(3), pp.262-271.
Davis, J. and McLister, A., 2016. History and Evolution of Bandages, Dressings, and Plasters. Smart Bandage Technologies: Design and Application, p.63.
Fonseca, C., Lopes, M., Ramos, A., Santos, V., Esquinas, A. and Parreira, P., 2016. Nursing interventions in prevention and healing of leg ulcers: Systematic review of
the literature. Worldwide Wound Healing: Innovation in Natural and Conventional Methods, p.93.
Garvey, C., Spruit, M.A., Hill, K., Pitta, F. and Shioya, T., 2013. International COPD Coalition Column: pulmonary rehabilitation-reaching out to our international
community. Journal of thoracic disease, 5(3), p.343.
Hellström, A., Nilsson, C., Nilsson, A. and Fagerström, C., 2016. Leg ulcers in older people: a national study addressing variation in diagnosis, pain and sleep
disturbance. BMC geriatrics, 16(1), p.25.
Kelechi, T.J., Johnson, J.J. and Yates, S., 2015. Chronic venous disease and venous leg ulcers: an evidence-based update. Journal of Vascular Nursing, 33(2), pp.36-
46.
Minniti, C.P. and Kato, G.J., 2016. Critical reviews: how we treat sickle cell patients with leg ulcers. American journal of hematology, 91(1), pp.22-30.
Augustin, M., Brocatti, L.K., Rustenbach, S.J., Schäfer, I. and Herberger, K., 2014. Cost of illness of leg ulcers in the community.‐ ‐ International wound journal, 11(3),
pp.283-292.
Beerens, H.C., de Boer, B., Zwakhalen, S.M., Tan, F.E., Ruwaard, D., Hamers, J.P. and Verbeek, H., 2016. The association between aspects of daily life and quality of
life of people with dementia living in long-term care facilities: a momentary assessment study. International psychogeriatrics, 28(8), pp.1323-1331.
Calvo, G.S., Gómez-Suárez, C., Soriano, J.B., Zamora, E., Gónzalez-Gamarra, A., González-Béjar, M., Jordán, A., Tadeo, E., Sebastián, A., Fernández, G. and
Ancochea, J., 2014. A home telehealth program for patients with severe COPD: the PROMETE study. Respiratory medicine, 108(3), pp.453-462.
Chamanga, E., Christie, J. and McKeown, E., 2015. Community nurses' experiences of treating patients with leg ulcers. Journal of community nursing, 28(6), pp.27-
34.
Chamanga, E.T., 2016. Managing leg ulcers in primary care. Nurs Practice, pp.68-71.
Chen, K.H., Liu, C.Y., Shyu, Y.I.L. and Yeh, S.L., 2016. Living with chronic obstructive pulmonary disease: The process of self-managing chronic obstructive
pulmonary disease. Journal of Nursing Research, 24(3), pp.262-271.
Davis, J. and McLister, A., 2016. History and Evolution of Bandages, Dressings, and Plasters. Smart Bandage Technologies: Design and Application, p.63.
Fonseca, C., Lopes, M., Ramos, A., Santos, V., Esquinas, A. and Parreira, P., 2016. Nursing interventions in prevention and healing of leg ulcers: Systematic review of
the literature. Worldwide Wound Healing: Innovation in Natural and Conventional Methods, p.93.
Garvey, C., Spruit, M.A., Hill, K., Pitta, F. and Shioya, T., 2013. International COPD Coalition Column: pulmonary rehabilitation-reaching out to our international
community. Journal of thoracic disease, 5(3), p.343.
Hellström, A., Nilsson, C., Nilsson, A. and Fagerström, C., 2016. Leg ulcers in older people: a national study addressing variation in diagnosis, pain and sleep
disturbance. BMC geriatrics, 16(1), p.25.
Kelechi, T.J., Johnson, J.J. and Yates, S., 2015. Chronic venous disease and venous leg ulcers: an evidence-based update. Journal of Vascular Nursing, 33(2), pp.36-
46.
Minniti, C.P. and Kato, G.J., 2016. Critical reviews: how we treat sickle cell patients with leg ulcers. American journal of hematology, 91(1), pp.22-30.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Parani, M., Lokhande, G., Singh, A. and Gaharwar, A.K., 2016. Engineered nanomaterials for infection control and healing acute and chronic wounds. ACS applied
materials & interfaces, 8(16), pp.10049-10069.
Preston, A., Rao, A., Strauss, R., Stamm, R. and Zalman, D., 2017. Deep tissue pressure injury: a clinical review. AJN The American Journal of Nursing, 117(5), pp.50-
57.
Sheahan, H., Canning, K., Refausse, N., Kinnear, E.M., Jorgensen, G., Walsh, J.R. and Lazzarini, P.A., 2017. Differences in the daily activity of patients with diabetic
foot ulcers compared to controls in their free living environments.‐ International wound journal, 14(6), pp.1175-1182.
Suikkala, A., Koskinen, S. and Leino-Kilpi, H., 2018. Patients’ involvement in nursing students’ clinical education: A scoping review. International journal of nursing
studies, 84, pp.40-51.
Sunshein, K.F. and Samouilov, A., 2017. Evaluation of peripheral neuropathy in the diabetic foot. Primary Care Reports, 23(3).
Tateyama, Y., Musumari, P.M., Techasrivichien, T., Suguimoto, S.P., Zulu, R., Dube, C., Feldman, M.D., Ono-Kihara, M. and Kihara, M., 2019. Dietary habits, body
image, and health service access related to cardiovascular diseases in rural Zambia: A qualitative study. PloS one, 14(2), p.e0212739.
Elliott, R.A., Lee, C.Y., Beanland, C., Vakil, K. and Goeman, D., 2016. Medicines management, medication errors and adverse medication events in older people
referred to a community nursing service: a retrospective observational study. Drugs-real world outcomes, 3(1), pp.13-24.
Thomas, D., Abramson, M.J., Bonevski, B., Taylor, S., Poole, S.G., Weeks, G.R., Dooley, M.J. and George, J., 2015. Quitting experiences and preferences for a future
quit attempt: a study among inpatient smokers. BMJ open, 5(4), p.e006959
Van Haeften-van Dijk, A.M., Meiland, F.J.M., Van Mierlo, L.D. and Dröes, R.M., 2015. Transforming nursing home-based day care for people with dementia into
socially integrated community day care: process analysis of the transition of six day care centres. International journal of nursing studies, 52(8), pp.1310-1322.
Watz, H., Mailänder, C., May, C., Baier, M. and Kirsten, A.M., 2017. Fast onset of action of glycopyrronium compared with tiotropium in patients with moderate to
severe COPD—a randomised, multicentre, crossover trial. Pulmonary pharmacology & therapeutics, 42, pp.13-20.
Weller, C.D., Buchbinder, R. and Johnston, R.V., 2016. Interventions for helping people adhere to compression treatments for venous leg ulceration. Cochrane
database of systematic reviews, (3).
White, R.I.C.H.A.R.D., Witts, S., Hopkins, A. and Ewart, J., 2016. The differences in approach and clinical outcomes of venous leg ulcers managed in primary and
secondary care. Wounds UK12, 2, pp.10-9.
materials & interfaces, 8(16), pp.10049-10069.
Preston, A., Rao, A., Strauss, R., Stamm, R. and Zalman, D., 2017. Deep tissue pressure injury: a clinical review. AJN The American Journal of Nursing, 117(5), pp.50-
57.
Sheahan, H., Canning, K., Refausse, N., Kinnear, E.M., Jorgensen, G., Walsh, J.R. and Lazzarini, P.A., 2017. Differences in the daily activity of patients with diabetic
foot ulcers compared to controls in their free living environments.‐ International wound journal, 14(6), pp.1175-1182.
Suikkala, A., Koskinen, S. and Leino-Kilpi, H., 2018. Patients’ involvement in nursing students’ clinical education: A scoping review. International journal of nursing
studies, 84, pp.40-51.
Sunshein, K.F. and Samouilov, A., 2017. Evaluation of peripheral neuropathy in the diabetic foot. Primary Care Reports, 23(3).
Tateyama, Y., Musumari, P.M., Techasrivichien, T., Suguimoto, S.P., Zulu, R., Dube, C., Feldman, M.D., Ono-Kihara, M. and Kihara, M., 2019. Dietary habits, body
image, and health service access related to cardiovascular diseases in rural Zambia: A qualitative study. PloS one, 14(2), p.e0212739.
Elliott, R.A., Lee, C.Y., Beanland, C., Vakil, K. and Goeman, D., 2016. Medicines management, medication errors and adverse medication events in older people
referred to a community nursing service: a retrospective observational study. Drugs-real world outcomes, 3(1), pp.13-24.
Thomas, D., Abramson, M.J., Bonevski, B., Taylor, S., Poole, S.G., Weeks, G.R., Dooley, M.J. and George, J., 2015. Quitting experiences and preferences for a future
quit attempt: a study among inpatient smokers. BMJ open, 5(4), p.e006959
Van Haeften-van Dijk, A.M., Meiland, F.J.M., Van Mierlo, L.D. and Dröes, R.M., 2015. Transforming nursing home-based day care for people with dementia into
socially integrated community day care: process analysis of the transition of six day care centres. International journal of nursing studies, 52(8), pp.1310-1322.
Watz, H., Mailänder, C., May, C., Baier, M. and Kirsten, A.M., 2017. Fast onset of action of glycopyrronium compared with tiotropium in patients with moderate to
severe COPD—a randomised, multicentre, crossover trial. Pulmonary pharmacology & therapeutics, 42, pp.13-20.
Weller, C.D., Buchbinder, R. and Johnston, R.V., 2016. Interventions for helping people adhere to compression treatments for venous leg ulceration. Cochrane
database of systematic reviews, (3).
White, R.I.C.H.A.R.D., Witts, S., Hopkins, A. and Ewart, J., 2016. The differences in approach and clinical outcomes of venous leg ulcers managed in primary and
secondary care. Wounds UK12, 2, pp.10-9.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
White-Chu, E.F. and Conner-Kerr, T.A., 2015. Overview of guidelines for the prevention and treatment of venous leg ulcers: a US perspective. Journal of
multidisciplinary healthcare, 7, p.111.
Zarchi, K. and Jemec, G.B., 2015. Delivery of compression therapy for venous leg ulcers. JAMA dermatology, 150(7), pp.730-736.
Zúñiga, F., Ausserhofer, D., Hamers, J.P., Engberg, S., Simon, M. and Schwendimann, R., 2015. The relationship of staffing and work environment with implicit
rationing of nursing care in Swiss nursing homes–a cross-sectional study. International journal of nursing studies, 52(9), pp.1463-1474.
multidisciplinary healthcare, 7, p.111.
Zarchi, K. and Jemec, G.B., 2015. Delivery of compression therapy for venous leg ulcers. JAMA dermatology, 150(7), pp.730-736.
Zúñiga, F., Ausserhofer, D., Hamers, J.P., Engberg, S., Simon, M. and Schwendimann, R., 2015. The relationship of staffing and work environment with implicit
rationing of nursing care in Swiss nursing homes–a cross-sectional study. International journal of nursing studies, 52(9), pp.1463-1474.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





