Nursing Priorities: Status Asthmaticus - Simon's Case Study Analysis
VerifiedAdded on 2023/01/19
|23
|3456
|77
Essay
AI Summary
This essay provides a comprehensive analysis of nursing priorities in the case of a 14-year-old patient, Simon, experiencing status asthmaticus. It begins with an introduction to the condition, its pathophysiology, and the role of the nurse in patient care. The essay identifies and discusses two critical priority problems: ineffective breathing pattern and ineffective airway clearance. For each problem, it outlines specific assessment data, the underlying pathophysiology, and two major interventions, including both independent and collaborative approaches. The independent interventions include oxygen administration and controlled breathing exercises/patient positioning and education, while the collaborative interventions involve the administration of medications like Albuterol and Hydrocortisone, detailing their actions, dosages, precautions, and the nurse's responsibilities. The essay emphasizes the importance of a holistic approach, integrating both pharmacological and non-pharmacological interventions to improve patient outcomes and prevent complications associated with severe asthma exacerbations.

NURSING PRIORITIES-STATUS ASTHMATICUS
Student’s Name
Institutional Affiliation
Course
Date
Instructor
Student’s Name
Institutional Affiliation
Course
Date
Instructor
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The persistence and progress of the inflammatory process in the airway results in further limit of airflow. The factors which contribute to
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
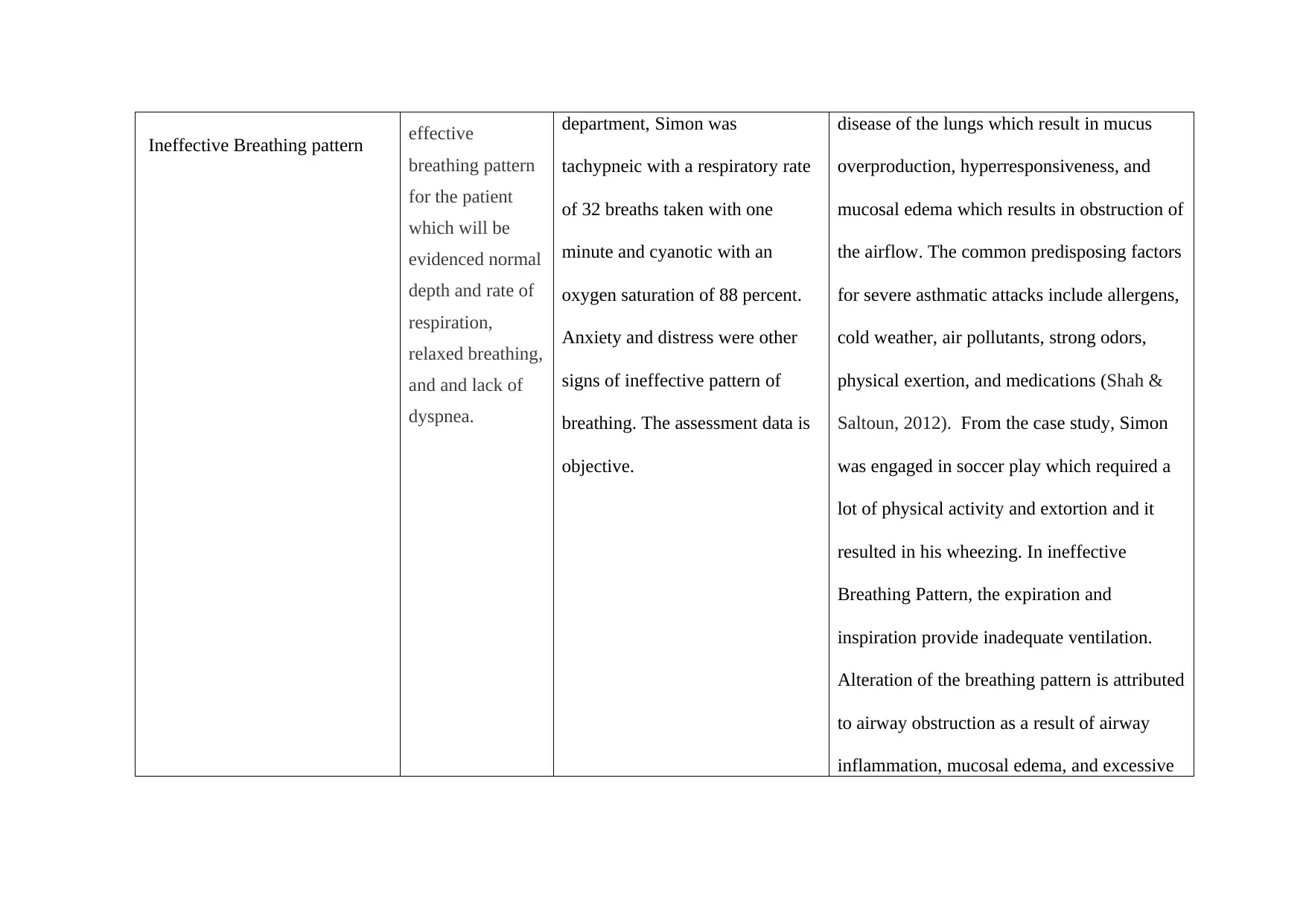
Ineffective Breathing pattern effective
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
production of secretions which results in
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
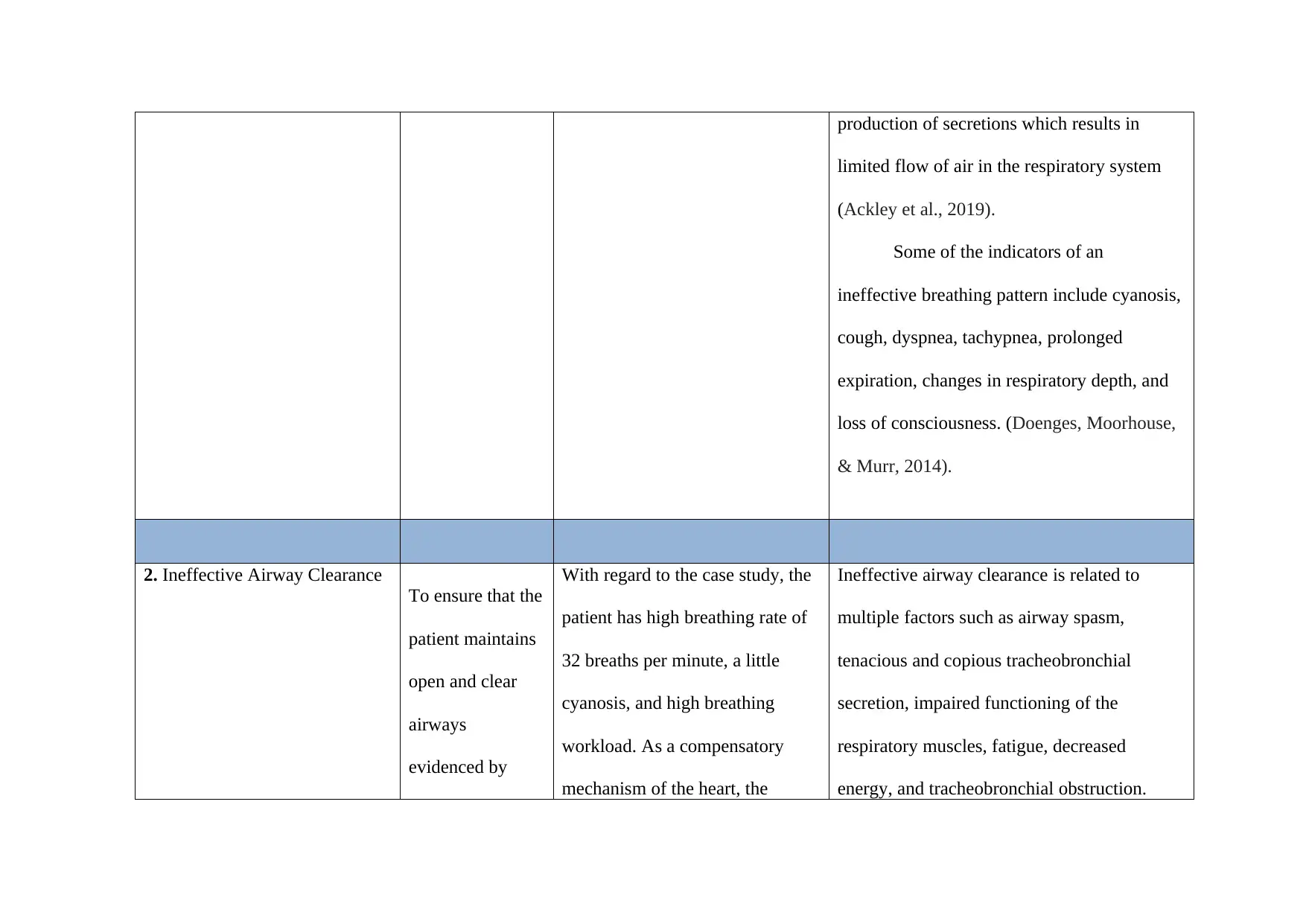
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
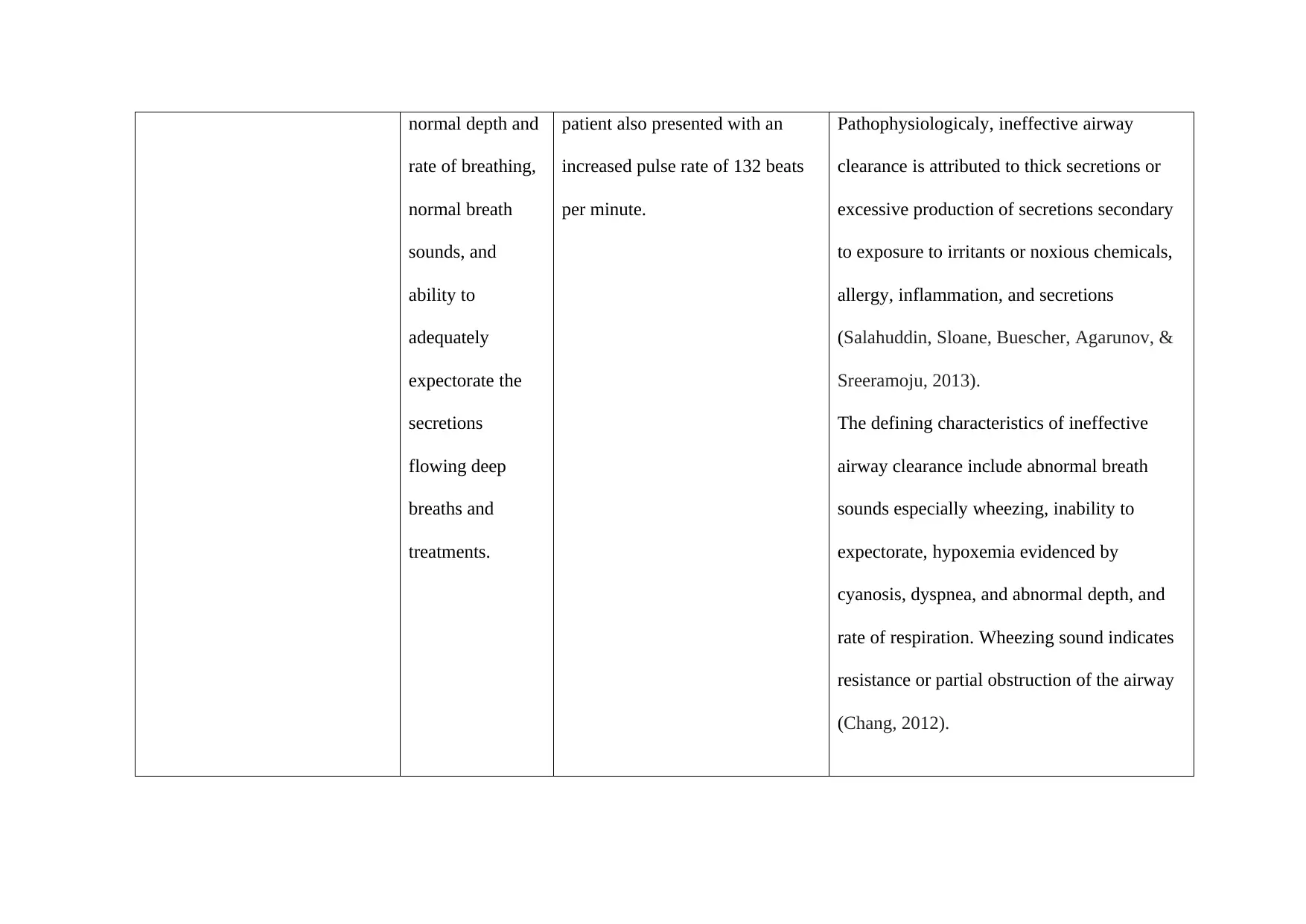
normal depth and
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
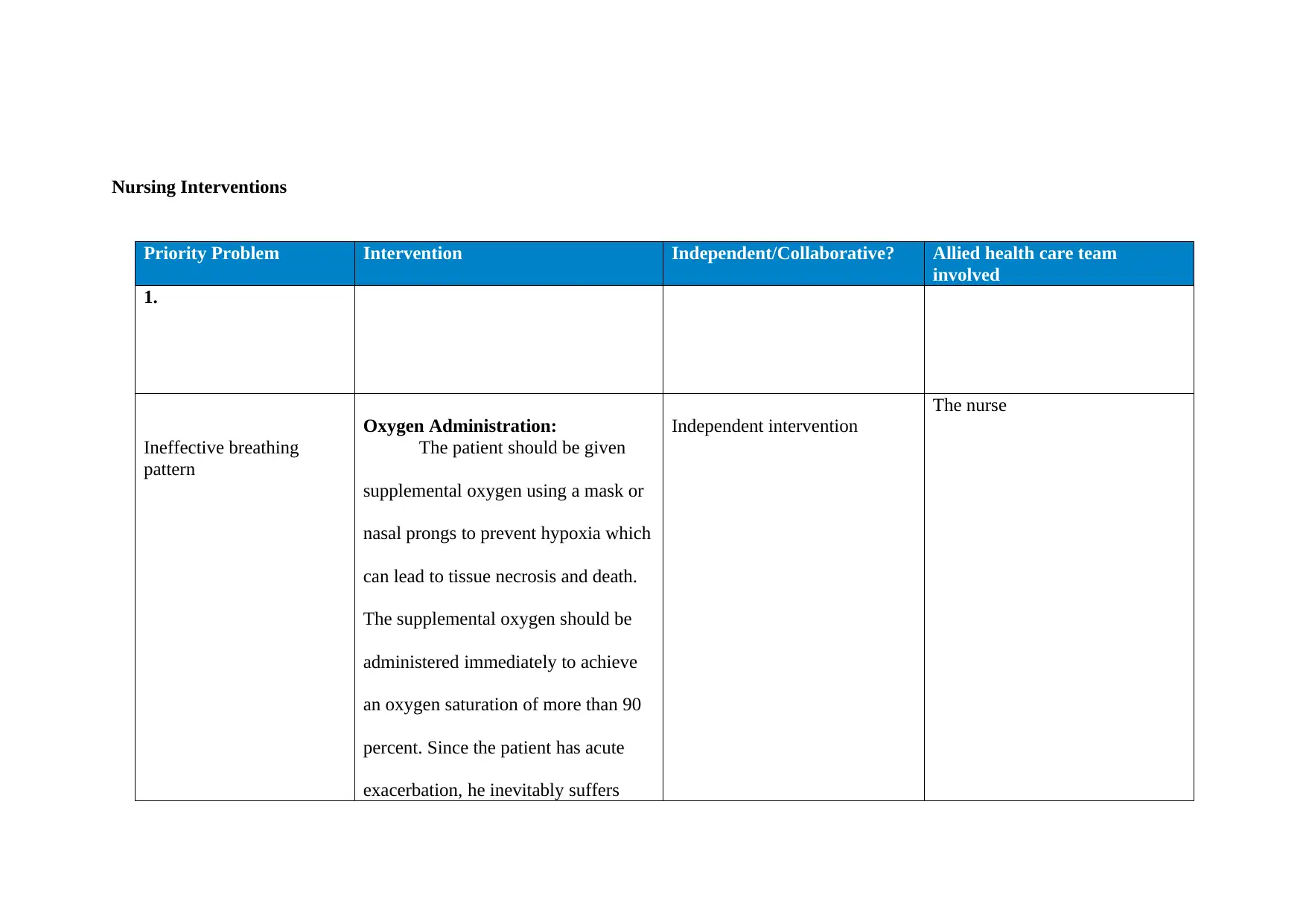
Nursing Interventions
Priority Problem Intervention Independent/Collaborative? Allied health care team
involved
1.
Ineffective breathing
pattern
Oxygen Administration:
The patient should be given
supplemental oxygen using a mask or
nasal prongs to prevent hypoxia which
can lead to tissue necrosis and death.
The supplemental oxygen should be
administered immediately to achieve
an oxygen saturation of more than 90
percent. Since the patient has acute
exacerbation, he inevitably suffers
Independent intervention
The nurse
Priority Problem Intervention Independent/Collaborative? Allied health care team
involved
1.
Ineffective breathing
pattern
Oxygen Administration:
The patient should be given
supplemental oxygen using a mask or
nasal prongs to prevent hypoxia which
can lead to tissue necrosis and death.
The supplemental oxygen should be
administered immediately to achieve
an oxygen saturation of more than 90
percent. Since the patient has acute
exacerbation, he inevitably suffers
Independent intervention
The nurse
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
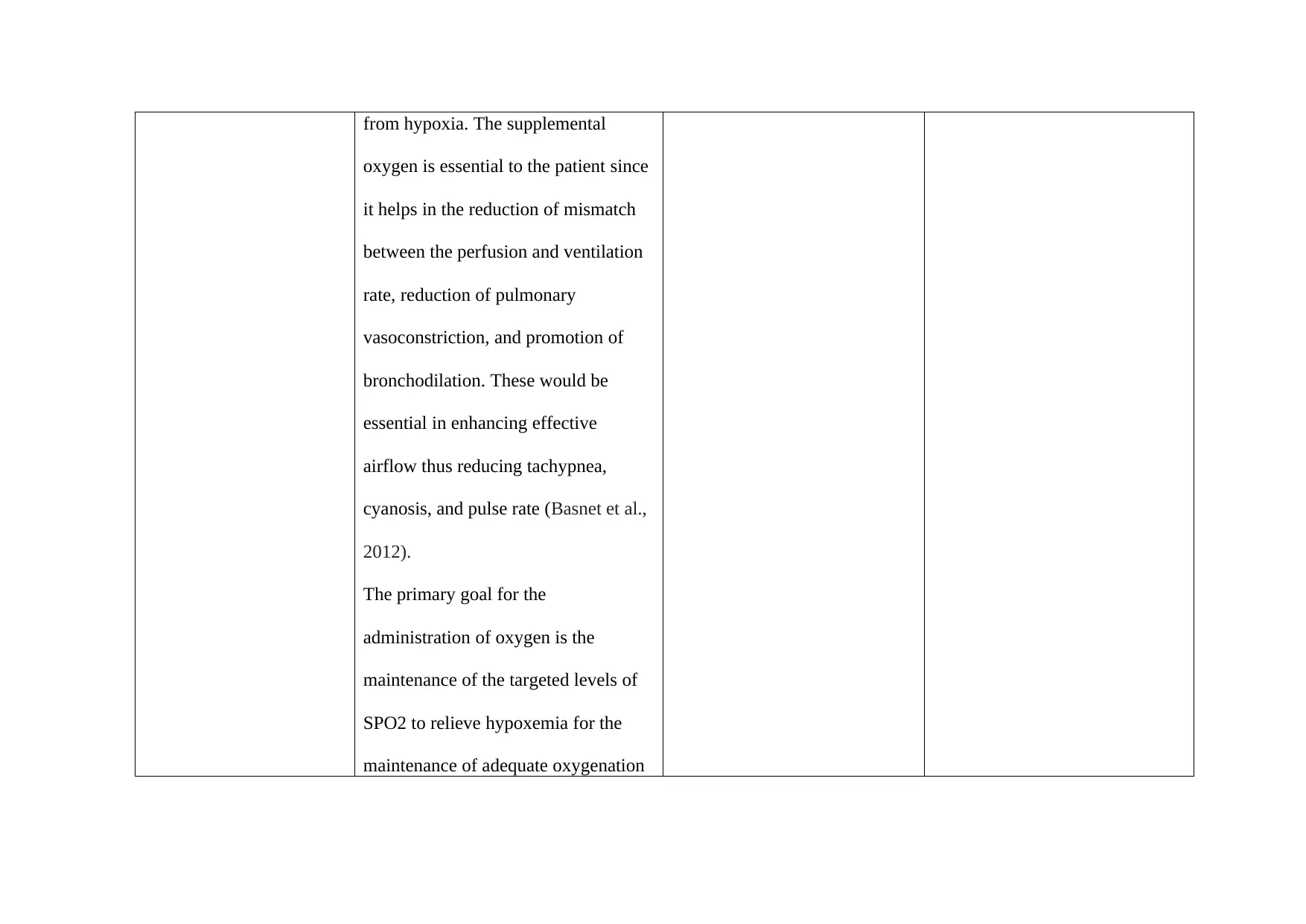
from hypoxia. The supplemental
oxygen is essential to the patient since
it helps in the reduction of mismatch
between the perfusion and ventilation
rate, reduction of pulmonary
vasoconstriction, and promotion of
bronchodilation. These would be
essential in enhancing effective
airflow thus reducing tachypnea,
cyanosis, and pulse rate (Basnet et al.,
2012).
The primary goal for the
administration of oxygen is the
maintenance of the targeted levels of
SPO2 to relieve hypoxemia for the
maintenance of adequate oxygenation
oxygen is essential to the patient since
it helps in the reduction of mismatch
between the perfusion and ventilation
rate, reduction of pulmonary
vasoconstriction, and promotion of
bronchodilation. These would be
essential in enhancing effective
airflow thus reducing tachypnea,
cyanosis, and pulse rate (Basnet et al.,
2012).
The primary goal for the
administration of oxygen is the
maintenance of the targeted levels of
SPO2 to relieve hypoxemia for the
maintenance of adequate oxygenation
of vital body organs and tissues. The
intervention would also help in the
reduction of patient’s work of
breathing and maintain economical
and efficient use of oxygen. (Peters et
a., 2012).
In the administration of oxygen, the
nurse plays a fundamental role in the
assessment, administration,
monitoring, and evaluating the
patient’s progress while informing the
GP. The nurse should examine the
patient’s airway and optimize his
position, for example, head tilt and
chin lift. The nurse should take
patient’s vital signs while on oxygen
intervention would also help in the
reduction of patient’s work of
breathing and maintain economical
and efficient use of oxygen. (Peters et
a., 2012).
In the administration of oxygen, the
nurse plays a fundamental role in the
assessment, administration,
monitoring, and evaluating the
patient’s progress while informing the
GP. The nurse should examine the
patient’s airway and optimize his
position, for example, head tilt and
chin lift. The nurse should take
patient’s vital signs while on oxygen
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
to check for the progress by reduction
of the respiration rate and respiratory
rates which are common in severe
asthmatic attacks (Lewis et al., 2015).
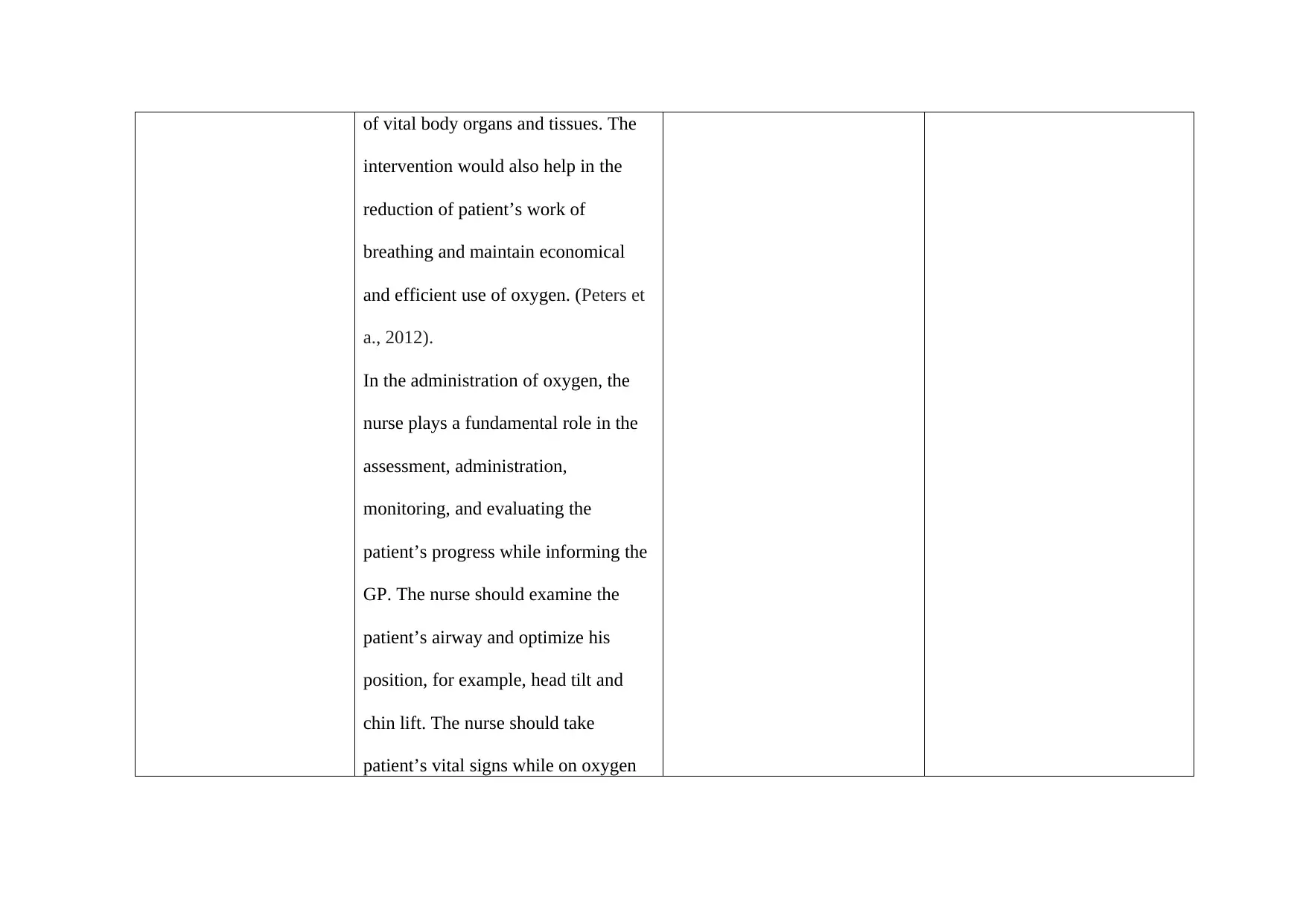
Controlled Breathing Exercises
The breathing exercise would
be essential to the patient to aid in the
reduction of shortness of breath,
anxiety, distress, and encourage
adequate supply of oxygen in the
respiratory system to reduce the risk of
reoccurrence of the severe asthmatic
attack. The nurse should guide the
patient in taking short and shallow
breaths into his chest to reduce anxiety
and zap his energy. The nurse should
of the respiration rate and respiratory
rates which are common in severe
asthmatic attacks (Lewis et al., 2015).
Controlled Breathing Exercises
The breathing exercise would
be essential to the patient to aid in the
reduction of shortness of breath,
anxiety, distress, and encourage
adequate supply of oxygen in the
respiratory system to reduce the risk of
reoccurrence of the severe asthmatic
attack. The nurse should guide the
patient in taking short and shallow
breaths into his chest to reduce anxiety
and zap his energy. The nurse should
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
instruct the patient to get comfortable
whereby he can lie in the bed or the
floor with a pillow under his knees and
head. The patient can also sit in a chair
with his shoulders, neck, and head
supported on the back of the chair. The
nurse should instruct the patient to
breath in via his nose and let his belly
fill with air and breath out. Since in
asthmatic attacks, the air is trapped in
the lungs, the breathing exercises can
help the patient get more air out thus
making the breathing easier (Lewis et
al., 2015).
The nurse can also guide the
patient to do the diaphragmatic
whereby he can lie in the bed or the
floor with a pillow under his knees and
head. The patient can also sit in a chair
with his shoulders, neck, and head
supported on the back of the chair. The
nurse should instruct the patient to
breath in via his nose and let his belly
fill with air and breath out. Since in
asthmatic attacks, the air is trapped in
the lungs, the breathing exercises can
help the patient get more air out thus
making the breathing easier (Lewis et
al., 2015).
The nurse can also guide the
patient to do the diaphragmatic
breathing technique which maximizes
the distribution of air in the lungs.
Another technique is the Buteyko
breathing which would help James to
consciously reduce the breathing
volume or breathing rate. He can do
this by sitting upright and relaxing his
belly muscles and the chest while
breathing. The patient should then
breath shallow and slowly via the nose
while his mouth is closed. He should
then breath out slowly until no air is
left in the lungs. Additionally, James
can be instructed to hold his breath for
a certain period based on his ability
and return to his gentle breathing
the distribution of air in the lungs.
Another technique is the Buteyko
breathing which would help James to
consciously reduce the breathing
volume or breathing rate. He can do
this by sitting upright and relaxing his
belly muscles and the chest while
breathing. The patient should then
breath shallow and slowly via the nose
while his mouth is closed. He should
then breath out slowly until no air is
left in the lungs. Additionally, James
can be instructed to hold his breath for
a certain period based on his ability
and return to his gentle breathing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





