Nursing Rehabilitation Report: Rehabilitation Goals and Discharge Plan
VerifiedAdded on 2022/09/14
|11
|2591
|13
Report
AI Summary
This report presents a detailed analysis of a nursing rehabilitation case study involving a 29-year-old woman who sustained a spinal cord injury resulting in paraplegia. The report focuses on the crucial role of nurses in rehabilitation, emphasizing the establishment of care goals across physical, psychological, and psychosocial domains. It outlines the importance of preventing complications, such as neurogenic bladder and bowel dysfunction, and promoting patient mobility and emotional well-being. The report further details a comprehensive discharge plan, including specific nursing interventions aimed at improving physical mobility, managing diet and nutrition, addressing knowledge deficits, managing urinary elimination, alleviating pain, and addressing sensory perception alterations. Each intervention is accompanied by a rationale, highlighting the evidence-based approach to patient care. The report underscores the significance of a multidisciplinary approach and the nurse's role as a central support system for the patient throughout the rehabilitation process, contributing to the patient's recovery and successful reintegration into the community.

Running Head: NURSING REHABILITATION
NURSING REHABILITATION
Name of the student
Name of the University
Author Note
NURSING REHABILITATION
Name of the student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
NURSING REHABILITATION
Nurses play an essential role in providing rehabilitation care to newly injured patients
who have undergone trauma from an accident as they are not fully aware of the consequences
and challenges that emerge in the recovery management of the condition. Rehabilitation
nurses can significantly educate patients to support them during the recovery and help them
achieve self-care activities. This paper will focus on a given case scenario by critically
assessing the role of the nurse in achieving key rehabilitation goals and laying down a
discharge plan with specific interventions for the patient.
The patient is a 29 years old woman who has survived a fatal accident with severe
injury to the spinal cord. She has suffered a severe burst fracture and a compression in the
spinal cord at T9. This has caused paraplegia below T9, restricted her upper body movements
and limited her strength and functions. She has now been put into rehabilitation care for
achieving the best possible outcomes in her recovery.
The purpose of post-trauma rehabilitation is to provide an educational problem-
solving process intended to reduce the extent of disability and handicap (participation) caused
as a result of severe accident or injury. Rehabilitation services are an indispensable element
of both the acute and post-discharge care of the injured. They help to lessen any further
functional incapacities in the future and increases the rate of restoration for the injured person
to get back to a lively lifestyle in the community. For ensuring that life-threatening
complications do not arise due to the immobilization, a carefully planned treatment and
intervention are of utmost importance during the rehabilitation period immediately after an
injury. The rehabilitation phase is challenging for many patients, and they require a
permanent support system to rely on. Hence it is vital to set realistic care goals as part of the
priority health management, established collectively by the multidisciplinary team. The nurse
involved in this process particularly plays an integral part in acting as a comprehensive
support system for the patient and help speed up the recovery process. The care goals which
NURSING REHABILITATION
Nurses play an essential role in providing rehabilitation care to newly injured patients
who have undergone trauma from an accident as they are not fully aware of the consequences
and challenges that emerge in the recovery management of the condition. Rehabilitation
nurses can significantly educate patients to support them during the recovery and help them
achieve self-care activities. This paper will focus on a given case scenario by critically
assessing the role of the nurse in achieving key rehabilitation goals and laying down a
discharge plan with specific interventions for the patient.
The patient is a 29 years old woman who has survived a fatal accident with severe
injury to the spinal cord. She has suffered a severe burst fracture and a compression in the
spinal cord at T9. This has caused paraplegia below T9, restricted her upper body movements
and limited her strength and functions. She has now been put into rehabilitation care for
achieving the best possible outcomes in her recovery.
The purpose of post-trauma rehabilitation is to provide an educational problem-
solving process intended to reduce the extent of disability and handicap (participation) caused
as a result of severe accident or injury. Rehabilitation services are an indispensable element
of both the acute and post-discharge care of the injured. They help to lessen any further
functional incapacities in the future and increases the rate of restoration for the injured person
to get back to a lively lifestyle in the community. For ensuring that life-threatening
complications do not arise due to the immobilization, a carefully planned treatment and
intervention are of utmost importance during the rehabilitation period immediately after an
injury. The rehabilitation phase is challenging for many patients, and they require a
permanent support system to rely on. Hence it is vital to set realistic care goals as part of the
priority health management, established collectively by the multidisciplinary team. The nurse
involved in this process particularly plays an integral part in acting as a comprehensive
support system for the patient and help speed up the recovery process. The care goals which
2
NURSING REHABILITATION
are to be identified by the nurse encompasses different areas such as physical and functional
health, psychological and emotional health, and the psychosocial wellbeing of the individual.
Along with medical treatment, specialized nursing care is essential for the patient to
realize the implications of their disability, and act towards it with a positive outlook.
Motivation is a crucial factor which accelerates the restoration of the patient’s previous
abilities. The focus of the nursing rehabilitation, in this case, will be primarily on the
following areas-
Prevention of any complications and risks that may arise in the inpatient
settings- a spinal cord injury disrupts the bladder and bowel control of the
body by interrupting the interaction between nerves in the spinal cord and the
brain, which leads to incontinence (Sezer, Akkuş, & Uğurlu, 2015). This may
cause bladder or bowel dysfunction called as “neurogenic bladder” or
“neurogenic bowel”. Such complications may cause urinary tract infections,
for which the nurse should always remain alert to arrest any deterioration (Nas
et al., 2015; Schurch, Tawadros & Carda, 2015). The danger of further trauma
persists in the patient due to her weakness in the spinal column, due to which
if she is left unsupervised that may increase the possibilities of getting exposed
to the risk of falls and tissue injury. To prevent this, the nurse must ensure
proper alignment of the spine to be maintained thoroughly. Immobilization
devices, elevated traction and bedrest arrangement, and the use of an air
mattress must be ensured to avoid any further risk of developing spinal cord
trauma (Hagen, 2015).
Improving the mobility of the patient - the nurse can effectively help the
patient in gaining control over her activities of daily life as much as possible,
and achieve independence. Due to the paraplegia, there is significant
NURSING REHABILITATION
are to be identified by the nurse encompasses different areas such as physical and functional
health, psychological and emotional health, and the psychosocial wellbeing of the individual.
Along with medical treatment, specialized nursing care is essential for the patient to
realize the implications of their disability, and act towards it with a positive outlook.
Motivation is a crucial factor which accelerates the restoration of the patient’s previous
abilities. The focus of the nursing rehabilitation, in this case, will be primarily on the
following areas-
Prevention of any complications and risks that may arise in the inpatient
settings- a spinal cord injury disrupts the bladder and bowel control of the
body by interrupting the interaction between nerves in the spinal cord and the
brain, which leads to incontinence (Sezer, Akkuş, & Uğurlu, 2015). This may
cause bladder or bowel dysfunction called as “neurogenic bladder” or
“neurogenic bowel”. Such complications may cause urinary tract infections,
for which the nurse should always remain alert to arrest any deterioration (Nas
et al., 2015; Schurch, Tawadros & Carda, 2015). The danger of further trauma
persists in the patient due to her weakness in the spinal column, due to which
if she is left unsupervised that may increase the possibilities of getting exposed
to the risk of falls and tissue injury. To prevent this, the nurse must ensure
proper alignment of the spine to be maintained thoroughly. Immobilization
devices, elevated traction and bedrest arrangement, and the use of an air
mattress must be ensured to avoid any further risk of developing spinal cord
trauma (Hagen, 2015).
Improving the mobility of the patient - the nurse can effectively help the
patient in gaining control over her activities of daily life as much as possible,
and achieve independence. Due to the paraplegia, there is significant
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
NURSING REHABILITATION
neuromuscular impairment, due to which the patient is unable to perform any
purposeful physical movement, which highly affects her quality of life and
ability to take care of herself. By delegation of work to an occupational
physiotherapist, her immobility can be reduced to a considerable extent. The
nurse can also help her perform some low-intensity exercises and
physiotherapy that will help her gain self-confidence and increase her
autonomy over her body by demonstrating techniques and behaviours that
enable resumption of her daily activities, and help ease her movement in the
wheelchair without any obstruction (Harvey, 2016; Gorgey, 2014).
Provide support to avoid any complications related to her emotional
wellbeing- the patient has a history of anxiety and depression for which she
was previously on medication. The recovery process can aggravate her
symptoms of depression or anxiety and cause low self-esteem and negative
perceptions of her self worth as a result of the present situation (Chen, Wu &
Lin, 2015). The nurse can substantially contribute towards alleviating the
patient’s perceived fears, by motivation and incorporating changes in her
lifestyle that provides her relief. Through compassionate behaviour and
effective communication to address the concerns that the patient might have,
the nurse can successfully develop a holistic environment for the patient
(Chaudhary & Mattu, 2018).
Once the nursing care goals are identified and achieved during the rehabilitation, it is
important to prepare for the next step, that is, discharge care planning (Weheida, Shabaan &
Fehr, 2018). It involves planning the interventions post-rehabilitation for patients with spinal
cord injuries which often includes strengthening their respiratory function, averting any
injury to the spinal cord, encourage flexibility in movement and independence, avoid or
NURSING REHABILITATION
neuromuscular impairment, due to which the patient is unable to perform any
purposeful physical movement, which highly affects her quality of life and
ability to take care of herself. By delegation of work to an occupational
physiotherapist, her immobility can be reduced to a considerable extent. The
nurse can also help her perform some low-intensity exercises and
physiotherapy that will help her gain self-confidence and increase her
autonomy over her body by demonstrating techniques and behaviours that
enable resumption of her daily activities, and help ease her movement in the
wheelchair without any obstruction (Harvey, 2016; Gorgey, 2014).
Provide support to avoid any complications related to her emotional
wellbeing- the patient has a history of anxiety and depression for which she
was previously on medication. The recovery process can aggravate her
symptoms of depression or anxiety and cause low self-esteem and negative
perceptions of her self worth as a result of the present situation (Chen, Wu &
Lin, 2015). The nurse can substantially contribute towards alleviating the
patient’s perceived fears, by motivation and incorporating changes in her
lifestyle that provides her relief. Through compassionate behaviour and
effective communication to address the concerns that the patient might have,
the nurse can successfully develop a holistic environment for the patient
(Chaudhary & Mattu, 2018).
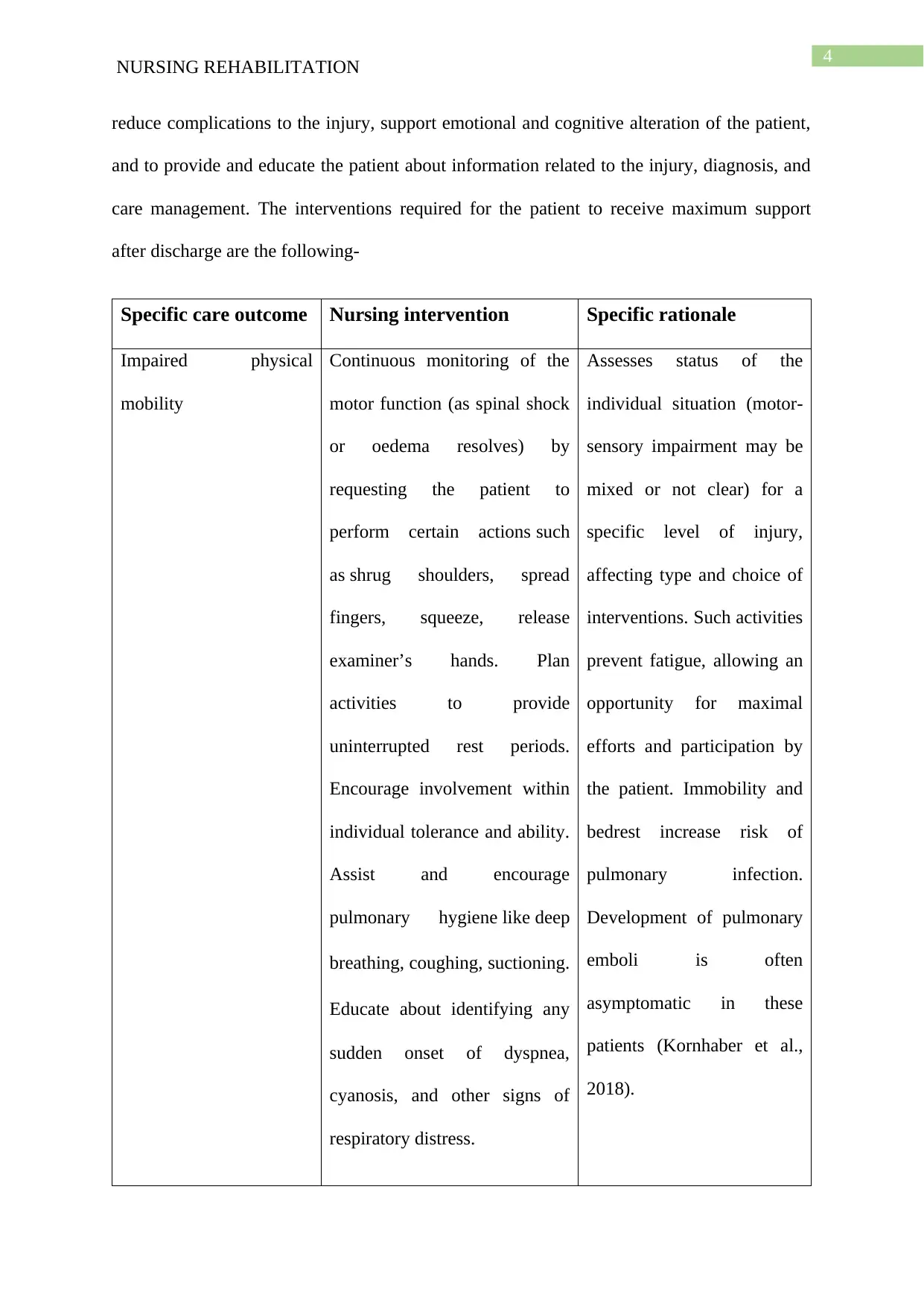
Once the nursing care goals are identified and achieved during the rehabilitation, it is
important to prepare for the next step, that is, discharge care planning (Weheida, Shabaan &
Fehr, 2018). It involves planning the interventions post-rehabilitation for patients with spinal
cord injuries which often includes strengthening their respiratory function, averting any
injury to the spinal cord, encourage flexibility in movement and independence, avoid or
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
NURSING REHABILITATION
reduce complications to the injury, support emotional and cognitive alteration of the patient,
and to provide and educate the patient about information related to the injury, diagnosis, and
care management. The interventions required for the patient to receive maximum support
after discharge are the following-
Specific care outcome Nursing intervention Specific rationale
Impaired physical
mobility
Continuous monitoring of the
motor function (as spinal shock
or oedema resolves) by
requesting the patient to
perform certain actions such
as shrug shoulders, spread
fingers, squeeze, release
examiner’s hands. Plan
activities to provide
uninterrupted rest periods.
Encourage involvement within
individual tolerance and ability.
Assist and encourage
pulmonary hygiene like deep
breathing, coughing, suctioning.
Educate about identifying any
sudden onset of dyspnea,
cyanosis, and other signs of
respiratory distress.
Assesses status of the
individual situation (motor-
sensory impairment may be
mixed or not clear) for a
specific level of injury,
affecting type and choice of
interventions. Such activities
prevent fatigue, allowing an
opportunity for maximal
efforts and participation by
the patient. Immobility and
bedrest increase risk of
pulmonary infection.
Development of pulmonary
emboli is often
asymptomatic in these
patients (Kornhaber et al.,
2018).
NURSING REHABILITATION
reduce complications to the injury, support emotional and cognitive alteration of the patient,
and to provide and educate the patient about information related to the injury, diagnosis, and
care management. The interventions required for the patient to receive maximum support
after discharge are the following-
Specific care outcome Nursing intervention Specific rationale
Impaired physical
mobility
Continuous monitoring of the
motor function (as spinal shock
or oedema resolves) by
requesting the patient to
perform certain actions such
as shrug shoulders, spread
fingers, squeeze, release
examiner’s hands. Plan
activities to provide
uninterrupted rest periods.
Encourage involvement within
individual tolerance and ability.
Assist and encourage
pulmonary hygiene like deep
breathing, coughing, suctioning.
Educate about identifying any
sudden onset of dyspnea,
cyanosis, and other signs of
respiratory distress.
Assesses status of the
individual situation (motor-
sensory impairment may be
mixed or not clear) for a
specific level of injury,
affecting type and choice of
interventions. Such activities
prevent fatigue, allowing an
opportunity for maximal
efforts and participation by
the patient. Immobility and
bedrest increase risk of
pulmonary infection.
Development of pulmonary
emboli is often
asymptomatic in these
patients (Kornhaber et al.,
2018).
5
NURSING REHABILITATION
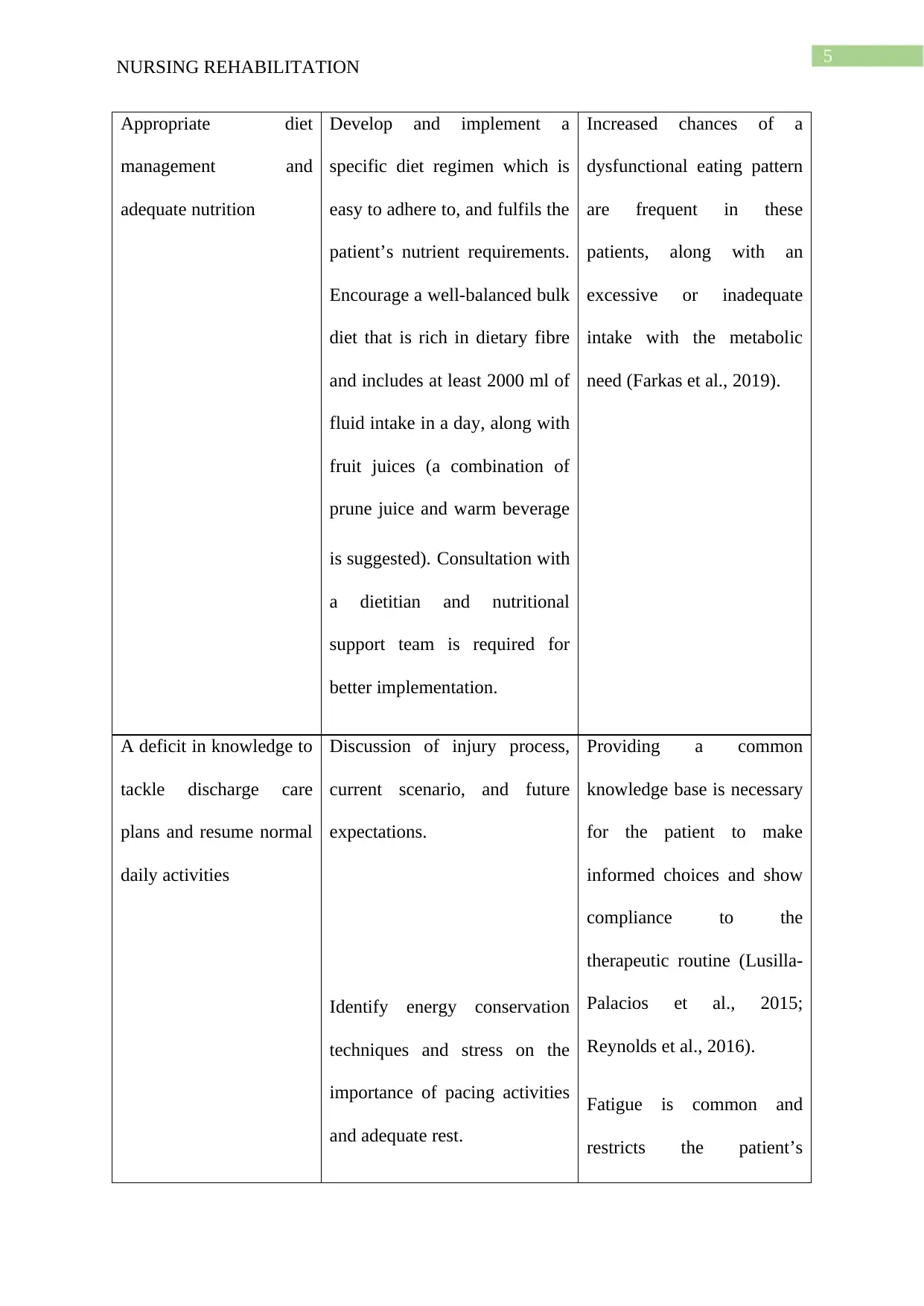
Appropriate diet
management and
adequate nutrition
Develop and implement a
specific diet regimen which is
easy to adhere to, and fulfils the
patient’s nutrient requirements.
Encourage a well-balanced bulk
diet that is rich in dietary fibre
and includes at least 2000 ml of
fluid intake in a day, along with
fruit juices (a combination of
prune juice and warm beverage
is suggested). Consultation with
a dietitian and nutritional
support team is required for
better implementation.
Increased chances of a
dysfunctional eating pattern
are frequent in these
patients, along with an
excessive or inadequate
intake with the metabolic
need (Farkas et al., 2019).
A deficit in knowledge to
tackle discharge care
plans and resume normal
daily activities
Discussion of injury process,
current scenario, and future
expectations.
Identify energy conservation
techniques and stress on the
importance of pacing activities
and adequate rest.
Providing a common
knowledge base is necessary
for the patient to make
informed choices and show
compliance to the
therapeutic routine (Lusilla-
Palacios et al., 2015;
Reynolds et al., 2016).
Fatigue is common and
restricts the patient’s
NURSING REHABILITATION
Appropriate diet
management and
adequate nutrition
Develop and implement a
specific diet regimen which is
easy to adhere to, and fulfils the
patient’s nutrient requirements.
Encourage a well-balanced bulk
diet that is rich in dietary fibre
and includes at least 2000 ml of
fluid intake in a day, along with
fruit juices (a combination of
prune juice and warm beverage
is suggested). Consultation with
a dietitian and nutritional
support team is required for
better implementation.
Increased chances of a
dysfunctional eating pattern
are frequent in these
patients, along with an
excessive or inadequate
intake with the metabolic
need (Farkas et al., 2019).
A deficit in knowledge to
tackle discharge care
plans and resume normal
daily activities
Discussion of injury process,
current scenario, and future
expectations.
Identify energy conservation
techniques and stress on the
importance of pacing activities
and adequate rest.
Providing a common
knowledge base is necessary
for the patient to make
informed choices and show
compliance to the
therapeutic routine (Lusilla-
Palacios et al., 2015;
Reynolds et al., 2016).
Fatigue is common and
restricts the patient’s
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
NURSING REHABILITATION
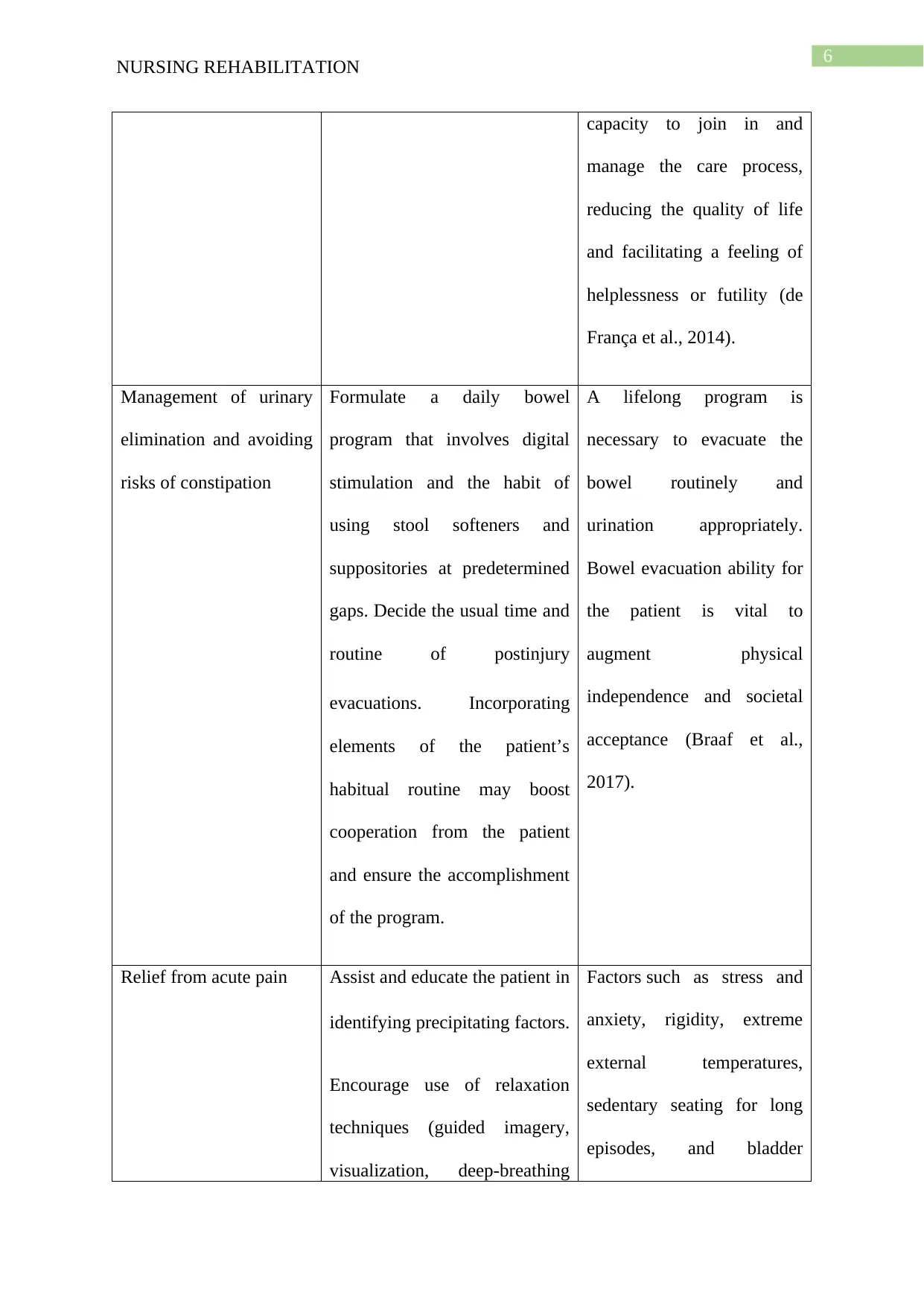
capacity to join in and
manage the care process,
reducing the quality of life
and facilitating a feeling of
helplessness or futility (de
França et al., 2014).
Management of urinary
elimination and avoiding
risks of constipation
Formulate a daily bowel
program that involves digital
stimulation and the habit of
using stool softeners and
suppositories at predetermined
gaps. Decide the usual time and
routine of postinjury
evacuations. Incorporating
elements of the patient’s
habitual routine may boost
cooperation from the patient
and ensure the accomplishment
of the program.
A lifelong program is
necessary to evacuate the
bowel routinely and
urination appropriately.
Bowel evacuation ability for
the patient is vital to
augment physical
independence and societal
acceptance (Braaf et al.,
2017).
Relief from acute pain Assist and educate the patient in
identifying precipitating factors.
Encourage use of relaxation
techniques (guided imagery,
visualization, deep-breathing
Factors such as stress and
anxiety, rigidity, extreme
external temperatures,
sedentary seating for long
episodes, and bladder
NURSING REHABILITATION
capacity to join in and
manage the care process,
reducing the quality of life
and facilitating a feeling of
helplessness or futility (de
França et al., 2014).
Management of urinary
elimination and avoiding
risks of constipation
Formulate a daily bowel
program that involves digital
stimulation and the habit of
using stool softeners and
suppositories at predetermined
gaps. Decide the usual time and
routine of postinjury
evacuations. Incorporating
elements of the patient’s
habitual routine may boost
cooperation from the patient
and ensure the accomplishment
of the program.
A lifelong program is
necessary to evacuate the
bowel routinely and
urination appropriately.
Bowel evacuation ability for
the patient is vital to
augment physical
independence and societal
acceptance (Braaf et al.,
2017).
Relief from acute pain Assist and educate the patient in
identifying precipitating factors.
Encourage use of relaxation
techniques (guided imagery,
visualization, deep-breathing
Factors such as stress and
anxiety, rigidity, extreme
external temperatures,
sedentary seating for long
episodes, and bladder
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
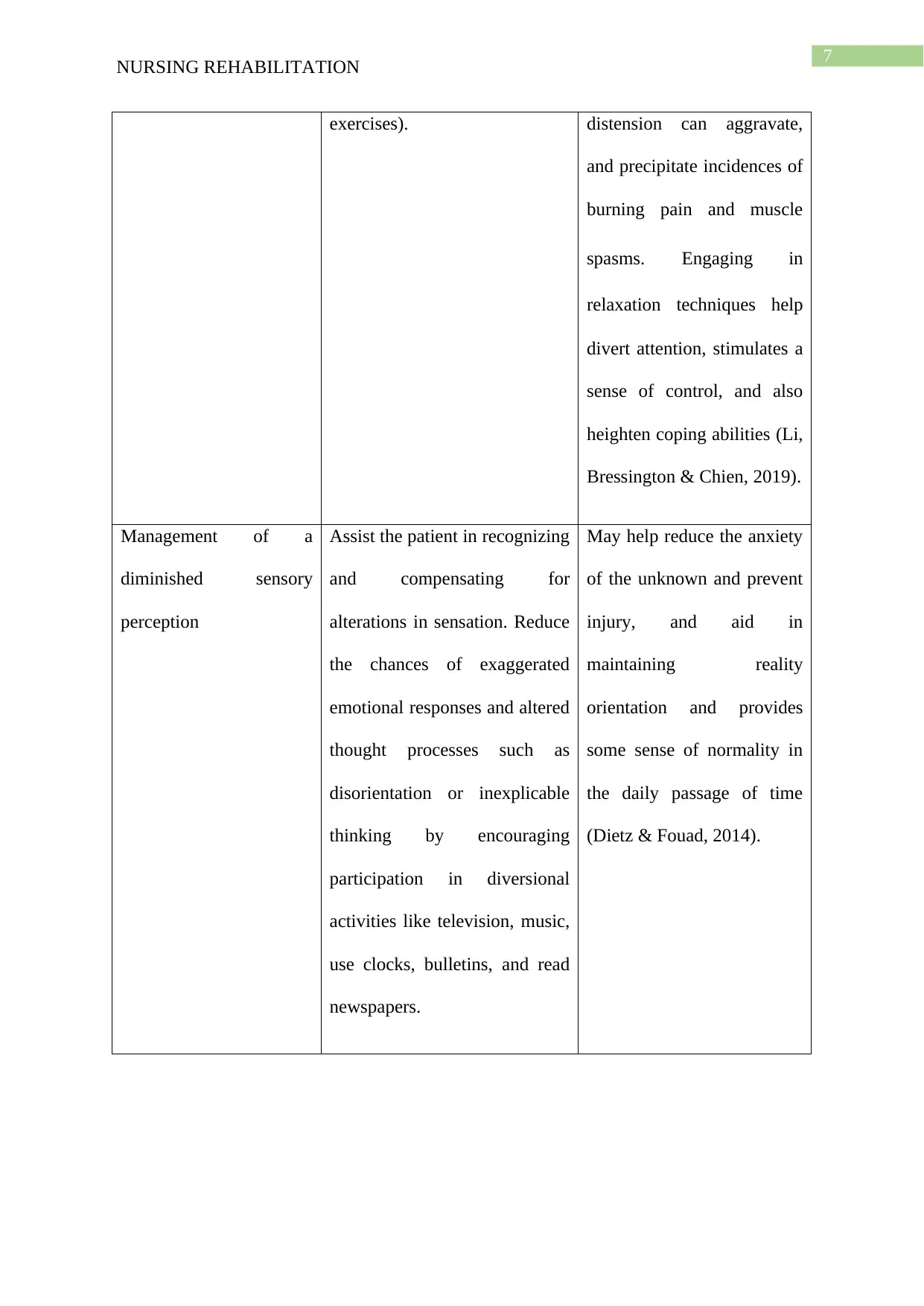
NURSING REHABILITATION
exercises). distension can aggravate,
and precipitate incidences of
burning pain and muscle
spasms. Engaging in
relaxation techniques help
divert attention, stimulates a
sense of control, and also
heighten coping abilities (Li,
Bressington & Chien, 2019).
Management of a
diminished sensory
perception
Assist the patient in recognizing
and compensating for
alterations in sensation. Reduce
the chances of exaggerated
emotional responses and altered
thought processes such as
disorientation or inexplicable
thinking by encouraging
participation in diversional
activities like television, music,
use clocks, bulletins, and read
newspapers.
May help reduce the anxiety
of the unknown and prevent
injury, and aid in
maintaining reality
orientation and provides
some sense of normality in
the daily passage of time
(Dietz & Fouad, 2014).
NURSING REHABILITATION
exercises). distension can aggravate,
and precipitate incidences of
burning pain and muscle
spasms. Engaging in
relaxation techniques help
divert attention, stimulates a
sense of control, and also
heighten coping abilities (Li,
Bressington & Chien, 2019).
Management of a
diminished sensory
perception
Assist the patient in recognizing
and compensating for
alterations in sensation. Reduce
the chances of exaggerated
emotional responses and altered
thought processes such as
disorientation or inexplicable
thinking by encouraging
participation in diversional
activities like television, music,
use clocks, bulletins, and read
newspapers.
May help reduce the anxiety
of the unknown and prevent
injury, and aid in
maintaining reality
orientation and provides
some sense of normality in
the daily passage of time
(Dietz & Fouad, 2014).
8
NURSING REHABILITATION
References
Braaf, S., Lennox, A., Nunn, A., & Gabbe, B. (2017). Social activity and relationship changes
experienced by people with bowel and bladder dysfunction following spinal cord
injury. Spinal cord, 55(7), 679-686. DOI: 10.1038/sc.2017.19
Chaudhary, G., & Mattu, S. (2018). Perceived Stress and Quality of Life in Spinal Cord
Injured Individuals. International Journal of Neurosurgery, 2(2), 27. DOI:
10.11648/j.ijn.20180202.12
Chen, H. Y., Wu, T. J., & Lin, C. C. (2015). Improving self‐perception and self‐efficacy in
patients with spinal cord injury: the efficacy of DVD‐based instructions. Journal of
clinical nursing, 24(11-12), 1666-1675. DOI: 10.1111/jocn.12768
de França, X., Sátiro, I., Cruz Enders, B., Silva Coura, A., Pereira Cruz, G. K., da Silva
Aragão, J., & Carvalho de Oliveira, D. R. (2014). Lifestyle and health conditions of
adults with spinal cord injury. Investigacion y educacion en enfermeria, 32(2), 244-
251. Retrieved from http://www.scielo.org.co/scielo.php?pid=S0120-
53072014000200007&script=sci_arttext&tlng=en
Dietz, V., & Fouad, K. (2014). Restoration of sensorimotor functions after spinal cord injury.
Brain, 137(3), 654-667. DOI: 10.1093/brain/awt262
Farkas, G. J., Pitot, M. A., Berg, A. S., & Gater, D. R. (2019). Nutritional status in chronic
spinal cord injury: a systematic review and meta-analysis. Spinal cord, 57(1), 3-17.
Retrieved from https://www.nature.com/articles/s41393-018-0218-4
Gorgey, A. S. (2014). Exercise awareness and barriers after spinal cord injury. World journal
of orthopedics, 5(3), 158. DOI: 10.5312/wjo.v5.i3.158
NURSING REHABILITATION
References
Braaf, S., Lennox, A., Nunn, A., & Gabbe, B. (2017). Social activity and relationship changes
experienced by people with bowel and bladder dysfunction following spinal cord
injury. Spinal cord, 55(7), 679-686. DOI: 10.1038/sc.2017.19
Chaudhary, G., & Mattu, S. (2018). Perceived Stress and Quality of Life in Spinal Cord
Injured Individuals. International Journal of Neurosurgery, 2(2), 27. DOI:
10.11648/j.ijn.20180202.12
Chen, H. Y., Wu, T. J., & Lin, C. C. (2015). Improving self‐perception and self‐efficacy in
patients with spinal cord injury: the efficacy of DVD‐based instructions. Journal of
clinical nursing, 24(11-12), 1666-1675. DOI: 10.1111/jocn.12768
de França, X., Sátiro, I., Cruz Enders, B., Silva Coura, A., Pereira Cruz, G. K., da Silva
Aragão, J., & Carvalho de Oliveira, D. R. (2014). Lifestyle and health conditions of
adults with spinal cord injury. Investigacion y educacion en enfermeria, 32(2), 244-
251. Retrieved from http://www.scielo.org.co/scielo.php?pid=S0120-
53072014000200007&script=sci_arttext&tlng=en
Dietz, V., & Fouad, K. (2014). Restoration of sensorimotor functions after spinal cord injury.
Brain, 137(3), 654-667. DOI: 10.1093/brain/awt262
Farkas, G. J., Pitot, M. A., Berg, A. S., & Gater, D. R. (2019). Nutritional status in chronic
spinal cord injury: a systematic review and meta-analysis. Spinal cord, 57(1), 3-17.
Retrieved from https://www.nature.com/articles/s41393-018-0218-4
Gorgey, A. S. (2014). Exercise awareness and barriers after spinal cord injury. World journal
of orthopedics, 5(3), 158. DOI: 10.5312/wjo.v5.i3.158
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
NURSING REHABILITATION
Hagen, E. M. (2015). Acute complications of spinal cord injuries. World journal of
orthopedics, 6(1), 17. DOI: 10.5312/wjo.v6.i1.17
Harvey, L. A. (2016). Physiotherapy rehabilitation for people with spinal cord injuries.
Journal of physiotherapy, 62(1), 4-11. DOI: 10.1016/j.jphys.2015.11.004
Kornhaber, R., Mclean, L., Betihavas, V., & Cleary, M. (2018). Resilience and the
rehabilitation of adult spinal cord injury survivors: a qualitative systematic review.
Journal of advanced nursing, 74(1), 23-33. DOI: 10.1111/jan.13396
Li, Y., Bressington, D., & Chien, W. T. (2019). Pilot evaluation of a coping-oriented
supportive program for people with spinal cord injury during inpatient rehabilitation.
Disability and rehabilitation, 41(2), 182-190. DOI: 10.1080/09638288.2017.1386238
Lusilla-Palacios, P., Castellano-Tejedor, C., Lucrecia-Ramirez-Garceran, Navarro-Sanchís, J.
A., Rodríguez-Urrutia, A., Parramon-Puig, G., ... & Cuxart-Fina, A. (2015). Training
professionals’ communication and motivation skills to improve spinal cord injury
patients’ satisfaction and clinical outcomes: study protocol of the ESPELMA trial.
Journal of health psychology, 20(10), 1357-1368. DOI:
10.1177%2F1359105313512351
Nas, K., Yazmalar, L., Şah, V., Aydın, A., & Öneş, K. (2015). Rehabilitation of spinal cord
injuries. World journal of orthopedics, 6(1), 8. DOI: 10.5312/wjo.v6.i1.8.
Reynolds, S. S., Murray, L. L., McLennon, S. M., Ebright, P. R., & Bakas, T. (2016).
Implementation strategies to improve knowledge and adherence to spinal cord injury
guidelines. Rehabilitation Nursing. DOI: 10.1002/rnj.304
Schurch, B., Tawadros, C., & Carda, S. (2015). Dysfunction of lower urinary tract in patients
with spinal cord injury. In Handbook of clinical neurology (Vol. 130, pp. 247-267).
NURSING REHABILITATION
Hagen, E. M. (2015). Acute complications of spinal cord injuries. World journal of
orthopedics, 6(1), 17. DOI: 10.5312/wjo.v6.i1.17
Harvey, L. A. (2016). Physiotherapy rehabilitation for people with spinal cord injuries.
Journal of physiotherapy, 62(1), 4-11. DOI: 10.1016/j.jphys.2015.11.004
Kornhaber, R., Mclean, L., Betihavas, V., & Cleary, M. (2018). Resilience and the
rehabilitation of adult spinal cord injury survivors: a qualitative systematic review.
Journal of advanced nursing, 74(1), 23-33. DOI: 10.1111/jan.13396
Li, Y., Bressington, D., & Chien, W. T. (2019). Pilot evaluation of a coping-oriented
supportive program for people with spinal cord injury during inpatient rehabilitation.
Disability and rehabilitation, 41(2), 182-190. DOI: 10.1080/09638288.2017.1386238
Lusilla-Palacios, P., Castellano-Tejedor, C., Lucrecia-Ramirez-Garceran, Navarro-Sanchís, J.
A., Rodríguez-Urrutia, A., Parramon-Puig, G., ... & Cuxart-Fina, A. (2015). Training
professionals’ communication and motivation skills to improve spinal cord injury
patients’ satisfaction and clinical outcomes: study protocol of the ESPELMA trial.
Journal of health psychology, 20(10), 1357-1368. DOI:
10.1177%2F1359105313512351
Nas, K., Yazmalar, L., Şah, V., Aydın, A., & Öneş, K. (2015). Rehabilitation of spinal cord
injuries. World journal of orthopedics, 6(1), 8. DOI: 10.5312/wjo.v6.i1.8.
Reynolds, S. S., Murray, L. L., McLennon, S. M., Ebright, P. R., & Bakas, T. (2016).
Implementation strategies to improve knowledge and adherence to spinal cord injury
guidelines. Rehabilitation Nursing. DOI: 10.1002/rnj.304
Schurch, B., Tawadros, C., & Carda, S. (2015). Dysfunction of lower urinary tract in patients
with spinal cord injury. In Handbook of clinical neurology (Vol. 130, pp. 247-267).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
NURSING REHABILITATION
Elsevier. Retrieved from
http://scitechconnect.elsevier.com/wp-content/uploads/2016/03/1-s2.0-
B9780444632470000146-main.pdf
Sezer, N., Akkuş, S., & Uğurlu, F. G. (2015). Chronic complications of spinal cord injury.
World journal of orthopedics, 6(1), 24. DOI: 10.5312%2Fwjo.v6.i1.24.
Weheida, S. M., Shabaan, E. G. E., & Fehr, A. (2018). Effect of pre-discharge instructions on
patients’ activities and functional ability post spinal cord injury. Egyptian Nursing
Journal, 15(2), 135. DOI: 10.4103/ENJ.ENJ_44_17
NURSING REHABILITATION
Elsevier. Retrieved from
http://scitechconnect.elsevier.com/wp-content/uploads/2016/03/1-s2.0-
B9780444632470000146-main.pdf
Sezer, N., Akkuş, S., & Uğurlu, F. G. (2015). Chronic complications of spinal cord injury.
World journal of orthopedics, 6(1), 24. DOI: 10.5312%2Fwjo.v6.i1.24.
Weheida, S. M., Shabaan, E. G. E., & Fehr, A. (2018). Effect of pre-discharge instructions on
patients’ activities and functional ability post spinal cord injury. Egyptian Nursing
Journal, 15(2), 135. DOI: 10.4103/ENJ.ENJ_44_17
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





