University Nursing Research: Evidence-Based PICO Framework Analysis
VerifiedAdded on 2023/03/23
|11
|1946
|45
Report
AI Summary
This report presents an evidence-based nursing research study, conducted using the PICO (Population, Intervention, Comparison, Outcome) framework, to investigate the impact of allowing family members to be present during resuscitation procedures in acute care settings. The research question focuses on whether family presence enhances patient care. The study employed a secondary research approach, analyzing articles from CINAHL and MEDLINE databases, using relevant keywords and boolean operators. The report discusses findings from several studies, including randomized controlled trials and qualitative studies, which explore the experiences of family members, physicians, and nurses. Key themes include the emotional impact on families, the benefits of providing moral support, and the development of transparent policies. The report concludes that while family presence can increase understanding and alleviate anxiety, it may also create distractions, emphasizing the need for clear guidelines and educational interventions. The report also provides references for the included articles.

Running head: NURSING
Evidence Based Nursing Research using PICO
Name of the Student
Name of the University
Author Note
Evidence Based Nursing Research using PICO
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
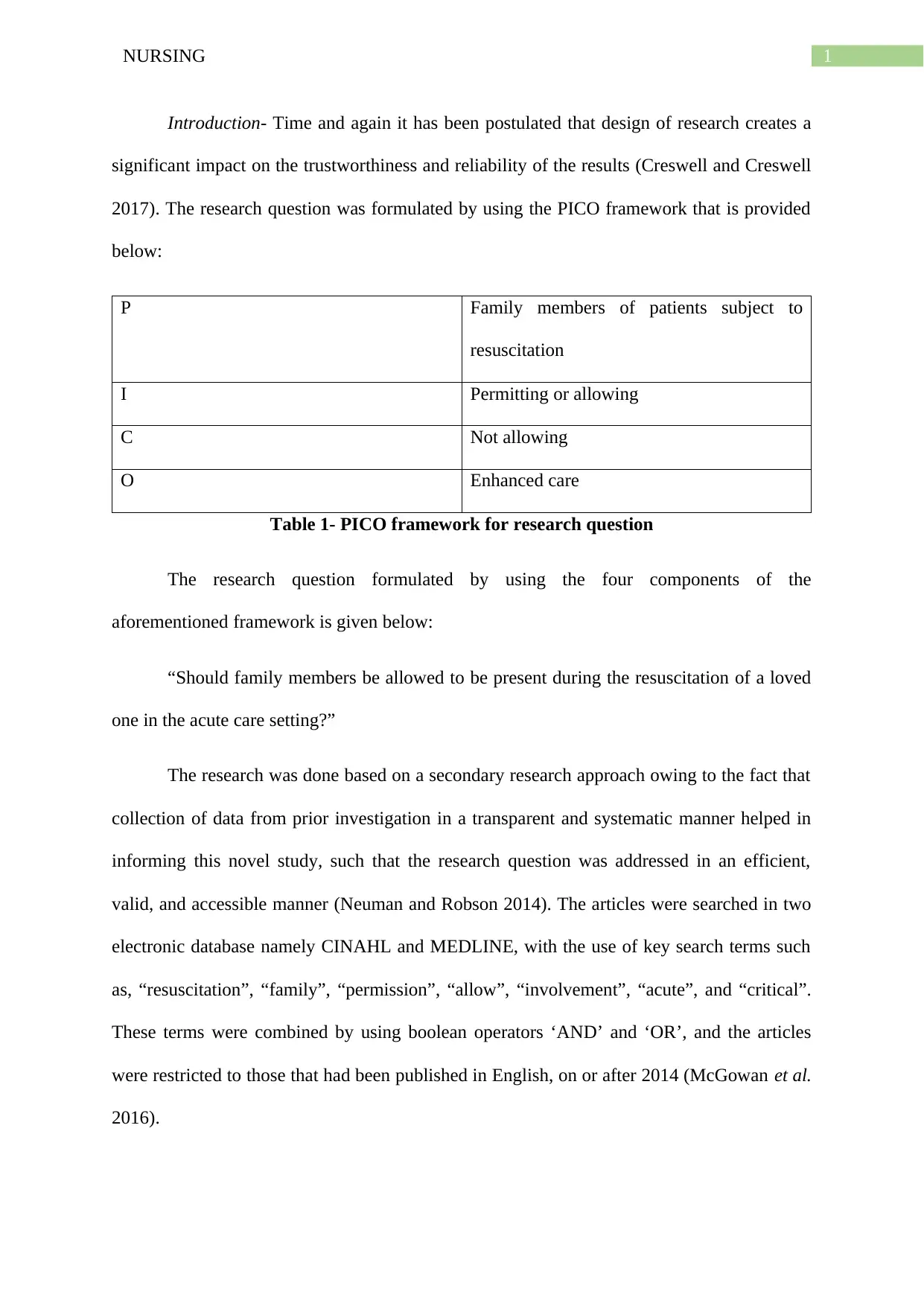
Introduction- Time and again it has been postulated that design of research creates a
significant impact on the trustworthiness and reliability of the results (Creswell and Creswell
2017). The research question was formulated by using the PICO framework that is provided
below:
P Family members of patients subject to
resuscitation
I Permitting or allowing
C Not allowing
O Enhanced care
Table 1- PICO framework for research question
The research question formulated by using the four components of the
aforementioned framework is given below:
“Should family members be allowed to be present during the resuscitation of a loved
one in the acute care setting?”
The research was done based on a secondary research approach owing to the fact that
collection of data from prior investigation in a transparent and systematic manner helped in
informing this novel study, such that the research question was addressed in an efficient,
valid, and accessible manner (Neuman and Robson 2014). The articles were searched in two
electronic database namely CINAHL and MEDLINE, with the use of key search terms such
as, “resuscitation”, “family”, “permission”, “allow”, “involvement”, “acute”, and “critical”.
These terms were combined by using boolean operators ‘AND’ and ‘OR’, and the articles
were restricted to those that had been published in English, on or after 2014 (McGowan et al.
2016).
Introduction- Time and again it has been postulated that design of research creates a
significant impact on the trustworthiness and reliability of the results (Creswell and Creswell
2017). The research question was formulated by using the PICO framework that is provided
below:
P Family members of patients subject to
resuscitation
I Permitting or allowing
C Not allowing
O Enhanced care
Table 1- PICO framework for research question
The research question formulated by using the four components of the
aforementioned framework is given below:
“Should family members be allowed to be present during the resuscitation of a loved
one in the acute care setting?”
The research was done based on a secondary research approach owing to the fact that
collection of data from prior investigation in a transparent and systematic manner helped in
informing this novel study, such that the research question was addressed in an efficient,
valid, and accessible manner (Neuman and Robson 2014). The articles were searched in two
electronic database namely CINAHL and MEDLINE, with the use of key search terms such
as, “resuscitation”, “family”, “permission”, “allow”, “involvement”, “acute”, and “critical”.
These terms were combined by using boolean operators ‘AND’ and ‘OR’, and the articles
were restricted to those that had been published in English, on or after 2014 (McGowan et al.
2016).
2NURSING
The rationale behind selection of the papers can be accredited to the fact that the
randomised controlled trials were of high quality evidence since the procedures used at the
time of investigation minimised the possibility of confounding variables manipulating the
results. Furthermore, qualitative study was also used to gain a sound awareness of the
perceptions and opinions of nursing professionals and family members, on the probable
benefits of family inclusion during resuscitation procedure (Clarke et al. 2014).
Discussion- The RCT by De Stefano et al. (2016) was conducted with the primary
objective of understanding the experiences of members of the family regarding the
implementation of CPR on their loved persons. On subjecting the participants to telephone
interviews, three months following cardiac arrest of the patients, the researchers could
recognise four different themes namely, (i) selecting to be dynamically engaged in
resuscitation process, (ii) communiqué between the family member as well as emergency
care team, (iii) awareness of the realism of patient demise, encouraging reception of the loss,
and (iv) knowledge and responses of the kin who were a witness to the CPR process,
recounting their mental state. It was found that most often the family members displayed a
willingness to be present at the time of resuscitation of their kin, while anticipating the
emotional upheaval that they would be subjected to. The findings also suggested that support
is much needed by a patient who is being subjected to resuscitation. Hence, allowing family
members during the process helps the former to provide moral support, establish association
with the patient, maintain communication, and touch the patient. Although it was found that
permitting the relatives was beneficial in increasing awareness among them, some family
members were overwhelmed about the traumatic nature of the actions, and could often not
bear to witness the insertion of catheters, infusions, or sensors in the patients.
The study conducted by Twibell et al. (2017) also explored the factors that were
responsible for influencing decision making skills of physicians and nurses, in relation to
The rationale behind selection of the papers can be accredited to the fact that the
randomised controlled trials were of high quality evidence since the procedures used at the
time of investigation minimised the possibility of confounding variables manipulating the
results. Furthermore, qualitative study was also used to gain a sound awareness of the
perceptions and opinions of nursing professionals and family members, on the probable
benefits of family inclusion during resuscitation procedure (Clarke et al. 2014).
Discussion- The RCT by De Stefano et al. (2016) was conducted with the primary
objective of understanding the experiences of members of the family regarding the
implementation of CPR on their loved persons. On subjecting the participants to telephone
interviews, three months following cardiac arrest of the patients, the researchers could
recognise four different themes namely, (i) selecting to be dynamically engaged in
resuscitation process, (ii) communiqué between the family member as well as emergency
care team, (iii) awareness of the realism of patient demise, encouraging reception of the loss,
and (iv) knowledge and responses of the kin who were a witness to the CPR process,
recounting their mental state. It was found that most often the family members displayed a
willingness to be present at the time of resuscitation of their kin, while anticipating the
emotional upheaval that they would be subjected to. The findings also suggested that support
is much needed by a patient who is being subjected to resuscitation. Hence, allowing family
members during the process helps the former to provide moral support, establish association
with the patient, maintain communication, and touch the patient. Although it was found that
permitting the relatives was beneficial in increasing awareness among them, some family
members were overwhelmed about the traumatic nature of the actions, and could often not
bear to witness the insertion of catheters, infusions, or sensors in the patients.
The study conducted by Twibell et al. (2017) also explored the factors that were
responsible for influencing decision making skills of physicians and nurses, in relation to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
allowing relatives during resuscitation of patients. The researchers recognised the fact that
several hospitals lack presence of a definite policy for guiding family presence at the time of
resuscitation, which often gives rise to negotiation. On subjecting the participants to open-
ended questions, it was found that the physicians and nursing professionals assessed three
comparable factors and four contradictory factors, at the time of making necessary decisions
of whether they should invite the attendance of family for the duration of resuscitation. Both
of them often disapproved the idea of involving relatives owing to the possibility of families
for disrupting the process of resuscitation. In addition, not involving family was also
accredited to the traumatic type of resuscitation. Additionally, it was found that physicians
often considered that lack of knowledge among family members on resuscitation to be a
major barrier to their involvement. The possible family benefit on allowing the relatives was
also acknowledged as a crucial factor by the participants. Furthermore, health condition of
the family members was of significant interest since nurses reported not encouraging family
presence if the relative was frail or stress on observing resuscitation had the potential of
creating detrimental health impacts.
With the aim of developing a sound understanding of the apparent benefits, obstacles
and facilitators to applying family presence all through resuscitation, Porter, Cooper and
Sellick (2014) conducted a literature review. Their findings elaborated on the fact that the
professed benefits of permitting family presence included, assisting them with the grieving
procedure, taking all possible efforts for revival of the patients, facilitating patient
recuperation, and increasing the family understanding by guiding them to recognise the
medical efforts undertaken. However, the findings also helped in identification of several
barriers that typically made the healthcare practitioners decide against family presence during
resuscitation. It was reported that presence of relatives during the procedure often increased
their stress and resulted in nervousness and apprehensions, thereby making the relatives
allowing relatives during resuscitation of patients. The researchers recognised the fact that
several hospitals lack presence of a definite policy for guiding family presence at the time of
resuscitation, which often gives rise to negotiation. On subjecting the participants to open-
ended questions, it was found that the physicians and nursing professionals assessed three
comparable factors and four contradictory factors, at the time of making necessary decisions
of whether they should invite the attendance of family for the duration of resuscitation. Both
of them often disapproved the idea of involving relatives owing to the possibility of families
for disrupting the process of resuscitation. In addition, not involving family was also
accredited to the traumatic type of resuscitation. Additionally, it was found that physicians
often considered that lack of knowledge among family members on resuscitation to be a
major barrier to their involvement. The possible family benefit on allowing the relatives was
also acknowledged as a crucial factor by the participants. Furthermore, health condition of
the family members was of significant interest since nurses reported not encouraging family
presence if the relative was frail or stress on observing resuscitation had the potential of
creating detrimental health impacts.
With the aim of developing a sound understanding of the apparent benefits, obstacles
and facilitators to applying family presence all through resuscitation, Porter, Cooper and
Sellick (2014) conducted a literature review. Their findings elaborated on the fact that the
professed benefits of permitting family presence included, assisting them with the grieving
procedure, taking all possible efforts for revival of the patients, facilitating patient
recuperation, and increasing the family understanding by guiding them to recognise the
medical efforts undertaken. However, the findings also helped in identification of several
barriers that typically made the healthcare practitioners decide against family presence during
resuscitation. It was reported that presence of relatives during the procedure often increased
their stress and resulted in nervousness and apprehensions, thereby making the relatives
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
distract the practitioners. In addition, the circumstances also involve anxiety of litigation due
to family interference, thus often making the practitioners question the purpose of permitting
the relatives. This was in accordance to the findings presented in a meta-analysis conducted
by Oczkowski et al. (2015) where it was suggested that providing family members the
occasion to participate in resuscitation of their loved ones did not create much of an impact
on the outcomes of resuscitation, and was also found to greatly enhance the psychological
wellbeing of the relatives. Offering them the chance to be a witness to the clinical procedure
generally reduced symptoms of depression and anxiety among the relatives. Furthermore, the
researchers also illustrated that offering the opportunity also helps in recognition of high-risk
relatives who are prone to suicidal ideations, thus preventing any adverse event.
Jabre et al. (2014) also conducted an assessment with the aim of assessing the
psychological impacts among kin who were present in the course of CPR of their relatives, in
comparison to those without the permission. On conducting a randomised trial, the
researchers found that the prevalence of PTSD symptoms were more frequent among
relatives who were in control group, in comparison to those who had been a witness to
resuscitation [adjusted odds ratio, 1.8; 95 % confidence interval (CI) 1.1–3.0; P = 0.02].
Furthermore, the proportion of relatives without any signs of depression and complicated
grief was meaningfully less in those who were present during the process, compared to the
control group (31 vs. 23 %; P = 0.02). Hence, providing permission was associated with
psychological benefits.
Conclusion- Thus, it can be concluded that permitting family members to be a witness
to resuscitation procedure that is conducted upon one of their loved ones increases
understanding of the former on the clinical procedure, helps in alleviating their anxiety and
depression, and also provides them the opportunity to witness that all possible efforts are
being taken by the practitioners to revive their relatives. However, they might often hinder
distract the practitioners. In addition, the circumstances also involve anxiety of litigation due
to family interference, thus often making the practitioners question the purpose of permitting
the relatives. This was in accordance to the findings presented in a meta-analysis conducted
by Oczkowski et al. (2015) where it was suggested that providing family members the
occasion to participate in resuscitation of their loved ones did not create much of an impact
on the outcomes of resuscitation, and was also found to greatly enhance the psychological
wellbeing of the relatives. Offering them the chance to be a witness to the clinical procedure
generally reduced symptoms of depression and anxiety among the relatives. Furthermore, the
researchers also illustrated that offering the opportunity also helps in recognition of high-risk
relatives who are prone to suicidal ideations, thus preventing any adverse event.
Jabre et al. (2014) also conducted an assessment with the aim of assessing the
psychological impacts among kin who were present in the course of CPR of their relatives, in
comparison to those without the permission. On conducting a randomised trial, the
researchers found that the prevalence of PTSD symptoms were more frequent among
relatives who were in control group, in comparison to those who had been a witness to
resuscitation [adjusted odds ratio, 1.8; 95 % confidence interval (CI) 1.1–3.0; P = 0.02].
Furthermore, the proportion of relatives without any signs of depression and complicated
grief was meaningfully less in those who were present during the process, compared to the
control group (31 vs. 23 %; P = 0.02). Hence, providing permission was associated with
psychological benefits.
Conclusion- Thus, it can be concluded that permitting family members to be a witness
to resuscitation procedure that is conducted upon one of their loved ones increases
understanding of the former on the clinical procedure, helps in alleviating their anxiety and
depression, and also provides them the opportunity to witness that all possible efforts are
being taken by the practitioners to revive their relatives. However, they might often hinder
5NURSING
the clinical process and distract the practitioners, thereby threatening the health and safety of
the patient. Thus, transparent policies must be developed across all healthcare organisations,
based on which family presence can be permitted. In addition, there is a need to implement
intensive educational intervention and accompany the family members must be accompanied
by experienced chaperones, to help them realise the importance of the resuscitation process.
the clinical process and distract the practitioners, thereby threatening the health and safety of
the patient. Thus, transparent policies must be developed across all healthcare organisations,
based on which family presence can be permitted. In addition, there is a need to implement
intensive educational intervention and accompany the family members must be accompanied
by experienced chaperones, to help them realise the importance of the resuscitation process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING
References
Clarke, B., Gillies, D., Illari, P., Russo, F. and Williamson, J., 2014. Mechanisms and the
evidence hierarchy. Topoi, 33(2), pp.339-360.
Creswell, J.W. and Creswell, J.D., 2017. Research design: Qualitative, quantitative, and
mixed methods approaches. Sage publications.
De Stefano, C., Normand, D., Jabre, P., Azoulay, E., Kentish-Barnes, N., Lapostolle, F.,
Baubet, T., Reuter, P.G., Javaud, N., Borron, S.W. and Vicaut, E., 2016. Family presence
during resuscitation: a qualitative analysis from a national multicenter randomized clinical
trial. PloS one, 11(6), p.e0156100.
Jabre, P., Tazarourte, K., Azoulay, E., Borron, S.W., Belpomme, V., Jacob, L., Bertrand, L.,
Lapostolle, F., Combes, X., Galinski, M. and Pinaud, V., 2014. Offering the opportunity for
family to be present during cardiopulmonary resuscitation: 1-year assessment. Intensive care
medicine, 40(7), pp.981-987.
McGowan, J., Sampson, M., Salzwedel, D.M., Cogo, E., Foerster, V. and Lefebvre, C., 2016.
PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of
clinical epidemiology, 75, pp.40-46.
Neuman, W.L. and Robson, K., 2014. Basics of social research. Toronto: Pearson Canada.
Oczkowski, S.J., Mazzetti, I., Cupido, C. and Fox-Robichaud, A.E., 2015. The offering of
family presence during resuscitation: a systematic review and meta-analysis. Journal of
intensive care, 3(1), p.41.
Porter, J.E., Cooper, S.J. and Sellick, K., 2014. Family presence during resuscitation (FPDR):
perceived benefits, barriers and enablers to implementation and practice. International
emergency nursing, 22(2), pp.69-74.
References
Clarke, B., Gillies, D., Illari, P., Russo, F. and Williamson, J., 2014. Mechanisms and the
evidence hierarchy. Topoi, 33(2), pp.339-360.
Creswell, J.W. and Creswell, J.D., 2017. Research design: Qualitative, quantitative, and
mixed methods approaches. Sage publications.
De Stefano, C., Normand, D., Jabre, P., Azoulay, E., Kentish-Barnes, N., Lapostolle, F.,
Baubet, T., Reuter, P.G., Javaud, N., Borron, S.W. and Vicaut, E., 2016. Family presence
during resuscitation: a qualitative analysis from a national multicenter randomized clinical
trial. PloS one, 11(6), p.e0156100.
Jabre, P., Tazarourte, K., Azoulay, E., Borron, S.W., Belpomme, V., Jacob, L., Bertrand, L.,
Lapostolle, F., Combes, X., Galinski, M. and Pinaud, V., 2014. Offering the opportunity for
family to be present during cardiopulmonary resuscitation: 1-year assessment. Intensive care
medicine, 40(7), pp.981-987.
McGowan, J., Sampson, M., Salzwedel, D.M., Cogo, E., Foerster, V. and Lefebvre, C., 2016.
PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of
clinical epidemiology, 75, pp.40-46.
Neuman, W.L. and Robson, K., 2014. Basics of social research. Toronto: Pearson Canada.
Oczkowski, S.J., Mazzetti, I., Cupido, C. and Fox-Robichaud, A.E., 2015. The offering of
family presence during resuscitation: a systematic review and meta-analysis. Journal of
intensive care, 3(1), p.41.
Porter, J.E., Cooper, S.J. and Sellick, K., 2014. Family presence during resuscitation (FPDR):
perceived benefits, barriers and enablers to implementation and practice. International
emergency nursing, 22(2), pp.69-74.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
Twibell, R., Siela, D., Riwitis, C., Neal, A. and Waters, N., 2018. A qualitative study of
factors in nurses' and physicians' decision‐making related to family presence during
resuscitation. Journal of clinical nursing, 27(1-2), pp.e320-e334.
Twibell, R., Siela, D., Riwitis, C., Neal, A. and Waters, N., 2018. A qualitative study of
factors in nurses' and physicians' decision‐making related to family presence during
resuscitation. Journal of clinical nursing, 27(1-2), pp.e320-e334.
8NURSING
Appendix
Article 1- (Jabre et al. 2014)
Article 2- (Porter, Cooper and Sellick 2014)
Appendix
Article 1- (Jabre et al. 2014)
Article 2- (Porter, Cooper and Sellick 2014)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
Article 3- (De Stefano et al. 2016)
Article 4- (Twibell et al. 2018)
Article 3- (De Stefano et al. 2016)
Article 4- (Twibell et al. 2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
Article 5- (Oczkowski et al. 2015)
Article 5- (Oczkowski et al. 2015)
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





