Strategies for Preventing Obesity in Children and Youths: A Report
VerifiedAdded on 2022/10/01
|11
|2929
|145
Report
AI Summary
This report addresses the critical issue of childhood obesity, presenting an integrated obesity prevention strategy suitable for community implementation. The report emphasizes the alarming rise in childhood obesity globally and in Australia, highlighting the need for effective interventions. It proposes a multi-strategic approach involving various stakeholders like the government, schools, community members, and the private sector, with a focus on policy changes, education, and environmental modifications to promote healthy eating and physical activity. The intervention, spanning two years, will include planning, community engagement, implementation, management, evaluation, and recommendations phases. The budget is estimated at $192,500, covering project team compensation, travel, advertising, educational materials, and community seminars. The report underscores the importance of stakeholder collaboration and provides recommendations for successful implementation.

OBESITY PREVENTION IN CHILDREN AND YOUTHS IN A COMMUNITY SETTING
Name of Student
Institution Affiliation
Name of Student
Institution Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
OBESITY PREVENTION IN CHILDREN AND YOUTHS IN A COMMUNITY SETTING
Introduction
Childhood obesity is one of the most severe health issues in the contemporary world.
According to experts, the increase in the prevalence of obesity among children and youths may
be attributed to various factors. Some of these causes include unhealthy eating habits, lack of
physical activity, genetic factors or a combination of these factors. However, in rare cases,
obesity may be caused by a hormonal problem. Childhood obesity is a global health issue,
increasingly becoming prevalent in both developed and developing countries. Additionally,
available evidence suggests that the prevalence of childhood obesity in developed countries
increased by a magnitude of two to three times between the 1980s and 1990s (Flynn, McNeil,
Maloff, Mutasingwa, Wu, Ford & Tough, 2006). According to the World Health Organization,
Childhood obesity is most prevalent in the urban centres of middle-income countries. Similarly,
the prevalence of childhood obesity has increased at an alarming rate in the recent past. Based on
2016 statistics, about 41 million children were overweight. Nearly half of the global populations
of obese children live in Africa and Asia (World Health Organization, 2019). The focus of this
paper will be on the prevention of obesity among children and Youths.
In Australia, it estimated that one in every four children is either overweight or obese.
Additionally, the severity of Obesity is intensified by the fact that once a person becomes obese,
it is quite hard to liberate them from the condition. Data from the Australian Bureau of Statistics
shows that 24.9% of children aged 5 to 17 years were obese or overweight (Australian Bureau of
Statistics, 2019). The medical costs attributed to the cases of obesity and overweight in Australia
was estimated at $43 Million in 2015 (Black, Hughes & Jones, 2018).
Obesity prevention interventions
Introduction
Childhood obesity is one of the most severe health issues in the contemporary world.
According to experts, the increase in the prevalence of obesity among children and youths may
be attributed to various factors. Some of these causes include unhealthy eating habits, lack of
physical activity, genetic factors or a combination of these factors. However, in rare cases,
obesity may be caused by a hormonal problem. Childhood obesity is a global health issue,
increasingly becoming prevalent in both developed and developing countries. Additionally,
available evidence suggests that the prevalence of childhood obesity in developed countries
increased by a magnitude of two to three times between the 1980s and 1990s (Flynn, McNeil,
Maloff, Mutasingwa, Wu, Ford & Tough, 2006). According to the World Health Organization,
Childhood obesity is most prevalent in the urban centres of middle-income countries. Similarly,
the prevalence of childhood obesity has increased at an alarming rate in the recent past. Based on
2016 statistics, about 41 million children were overweight. Nearly half of the global populations
of obese children live in Africa and Asia (World Health Organization, 2019). The focus of this
paper will be on the prevention of obesity among children and Youths.
In Australia, it estimated that one in every four children is either overweight or obese.
Additionally, the severity of Obesity is intensified by the fact that once a person becomes obese,
it is quite hard to liberate them from the condition. Data from the Australian Bureau of Statistics
shows that 24.9% of children aged 5 to 17 years were obese or overweight (Australian Bureau of
Statistics, 2019). The medical costs attributed to the cases of obesity and overweight in Australia
was estimated at $43 Million in 2015 (Black, Hughes & Jones, 2018).
Obesity prevention interventions
The persistent increase in the cases of obesity among youths and children demonstrate
that there is a need for effective interventions among the affected populations. Traditionally,
many strategies focused on the promotion of healthy food choices and regular activities
individuals have been used to deal with cases of obesity. The continuous increase in cases of
obesity among children and youths may, therefore, be as a result of the failure of the adopted
intervention, failure on the part of an individual or both. However, available evidence suggests
that the majority of the obese population have been actively trying to control their weight. This
strategy seeks to manage obesity by promoting physical activity and facilitating physical activity
trough a collaborative approach. It aims to understand the environmental factors in which people
engage in physical activity and make food choices to actively deal with Obesity among children
and Youths. This approach is based on the fact that understanding the root cause of the problem
would make it easier to solve it. It is widely accepted that the use of effective strategies may aid
in the management of obesity, on the same note a multi-strategic approach involving all
community levels including individuals and the wider population is required to effectively
address the obesity epidemic (Flynn, McNeil, Maloff, Mutasingwa, Wu, Ford & Tough, 2006).
The suitability of the intervention is also based on the fact that it focuses on individuals,
community and environmental causes of obesity among children and youths and tries to address
them as a whole. For example, by focusing on environmental limitations of healthy lifestyles, the
intervention seeks to create awareness about other factors that contribute to the prevalence of
obesity. Through its focus on agriculture, taxation and urban planning, the strategy aims to
address the root causes of obesity among children.
The integrated obesity preventions strategy is, therefore, best suited to deal with issues of
obesity. The adoption of an integrated approach is necessitated mainly by the failure of single
that there is a need for effective interventions among the affected populations. Traditionally,
many strategies focused on the promotion of healthy food choices and regular activities
individuals have been used to deal with cases of obesity. The continuous increase in cases of
obesity among children and youths may, therefore, be as a result of the failure of the adopted
intervention, failure on the part of an individual or both. However, available evidence suggests
that the majority of the obese population have been actively trying to control their weight. This
strategy seeks to manage obesity by promoting physical activity and facilitating physical activity
trough a collaborative approach. It aims to understand the environmental factors in which people
engage in physical activity and make food choices to actively deal with Obesity among children
and Youths. This approach is based on the fact that understanding the root cause of the problem
would make it easier to solve it. It is widely accepted that the use of effective strategies may aid
in the management of obesity, on the same note a multi-strategic approach involving all
community levels including individuals and the wider population is required to effectively
address the obesity epidemic (Flynn, McNeil, Maloff, Mutasingwa, Wu, Ford & Tough, 2006).
The suitability of the intervention is also based on the fact that it focuses on individuals,
community and environmental causes of obesity among children and youths and tries to address
them as a whole. For example, by focusing on environmental limitations of healthy lifestyles, the
intervention seeks to create awareness about other factors that contribute to the prevalence of
obesity. Through its focus on agriculture, taxation and urban planning, the strategy aims to
address the root causes of obesity among children.
The integrated obesity preventions strategy is, therefore, best suited to deal with issues of
obesity. The adoption of an integrated approach is necessitated mainly by the failure of single
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
interventions to curb the prevalence of obesity among children and youths. The use of an
integrated strategy to deal with obesity would necessitate the incorporation of multiple
stakeholders and a wide range of interventions (World Health Organization, 2019 b).
Additionally, this strategy would require sustained interventions at various levels including
school and community levels to facilitate behavioural change and at. Additionally, the approach
would also focus on sector changes in urban planning, transportation, education, food
manufacturing and agriculture. The adoption of all these interventions as a single obesity
prevention strategy would be quite useful as opposed to the use of each on its own (World Health
Organization, 2019). An integrated obesity prevention strategy targets nongovernmental
organisations, private organisations, the government and communities. Additionally, they also
need to be integrated with issues such as undernutrition and food security especially in middle
and low-income countries (World Health Organization, 2019 b). However, for an integrated
strategy to become effective, all stakeholders need to be involved across the development,
implementation and evaluation (Flynn et al., 2006).
In an integrated obesity prevention strategy, the government would play a leading role in
the provision of leadership and funding required for successful implementation. Additionally, the
government would be responsible for creating environments that support physical activity and
healthy diets through policy changes in the areas of agriculture, transport, urban planning, fiscal
policy, food labelling and marketing. The approach involves policy changes targeted at making it
mandatory for children and adults to undertake the rigorous activity of at least one hour every
day. This strategy would also require integration of behaviour modification education at the
school and community levels. An integrated approach would, therefore, lead to the effective
management of obesity by involving key stakeholders and streamlining various efforts into a
integrated strategy to deal with obesity would necessitate the incorporation of multiple
stakeholders and a wide range of interventions (World Health Organization, 2019 b).
Additionally, this strategy would require sustained interventions at various levels including
school and community levels to facilitate behavioural change and at. Additionally, the approach
would also focus on sector changes in urban planning, transportation, education, food
manufacturing and agriculture. The adoption of all these interventions as a single obesity
prevention strategy would be quite useful as opposed to the use of each on its own (World Health
Organization, 2019). An integrated obesity prevention strategy targets nongovernmental
organisations, private organisations, the government and communities. Additionally, they also
need to be integrated with issues such as undernutrition and food security especially in middle
and low-income countries (World Health Organization, 2019 b). However, for an integrated
strategy to become effective, all stakeholders need to be involved across the development,
implementation and evaluation (Flynn et al., 2006).
In an integrated obesity prevention strategy, the government would play a leading role in
the provision of leadership and funding required for successful implementation. Additionally, the
government would be responsible for creating environments that support physical activity and
healthy diets through policy changes in the areas of agriculture, transport, urban planning, fiscal
policy, food labelling and marketing. The approach involves policy changes targeted at making it
mandatory for children and adults to undertake the rigorous activity of at least one hour every
day. This strategy would also require integration of behaviour modification education at the
school and community levels. An integrated approach would, therefore, lead to the effective
management of obesity by involving key stakeholders and streamlining various efforts into a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
single more effective strategy (World Health Organization, 2019 b).This intervention. Duration
of two years would be sufficient for the implementation of the intervention.
The strategy would be divided into different phases such as planning, community
engagement, implementation, management, evaluation and recommendations. Each of these
phases will involve specific activities focused on enhancing the success of the intervention
Planning stage
Under the planning stage, activities such as mapping out the steps that will be required to
meet the objectives of the strategy and the identification of all the tasks to be carried out will be
done. Similarly, the functions and resources needed for the project will also be identified as well
as the strategy that will be used in producing them.
Community engagement
Community involvement stage would entail seeking the input of the community members
in the effective management of childhood obesity. Here the community will have an opportunity
to make suggestions on what needs to be done and explain what needs to be prioritized based on
their personal experience.
Implementation
The implementation would involve activities such as carrying out the tasks specified in
the planning stage to objectives of the intervention. It would also include the making of
necessary adjustments necessitated by a change in some factors of the project Lombard et
al.,2014).
Management stage
The management stage would involve activities such as ensuring that each step of the
implementation process is carried out as anticipated.
of two years would be sufficient for the implementation of the intervention.
The strategy would be divided into different phases such as planning, community
engagement, implementation, management, evaluation and recommendations. Each of these
phases will involve specific activities focused on enhancing the success of the intervention
Planning stage
Under the planning stage, activities such as mapping out the steps that will be required to
meet the objectives of the strategy and the identification of all the tasks to be carried out will be
done. Similarly, the functions and resources needed for the project will also be identified as well
as the strategy that will be used in producing them.
Community engagement
Community involvement stage would entail seeking the input of the community members
in the effective management of childhood obesity. Here the community will have an opportunity
to make suggestions on what needs to be done and explain what needs to be prioritized based on
their personal experience.
Implementation
The implementation would involve activities such as carrying out the tasks specified in
the planning stage to objectives of the intervention. It would also include the making of
necessary adjustments necessitated by a change in some factors of the project Lombard et
al.,2014).
Management stage
The management stage would involve activities such as ensuring that each step of the
implementation process is carried out as anticipated.
Evaluation
The evaluation phase would be characterised by activities such as comparing the outcome
with what was envisioned in the project plan to identify any deviations or conformity.
Recommendation
The recommendation phase
The final phase of the strategy would involve activities such as making suggestions on
what ought to have been improved in the implementation or what needs to be improved in the
next project. The success of each of these phases would significantly contribute to the success of
the strategy Lombard et al., 2015).
Various stakeholders would be needed to implement the obesity prevention strategy
successfully. The stakeholders include the Government, private organizations, the family and
community members, healthcare providers and schools. Each of these stakeholders would play
an essential role in the successful implementation of the intervention.
The government would be a key player for several reasons. Policy changes targeted at the
production manufacture, packaging, marketing and labelling of food is only possible through the
intervention of the government. Notably, the role of the government in enhancing food security
would improve the availability of healthy food choices for the target population (World Health
Organization, 2019 b). Similarly, the use of government subsidies, regulation of quotas, import
tariffs and taxes would enhance the availability and affordability of healthy foods. Besides,
taxation policies are an essential requirement in the reduction of socioeconomic inequalities
attributed to health inequalities. Notably, the implementation of urban planning and transport
policies such as the availing of recreational spaces, provision of walking and cycling spaces as
well as the prioritization of public transport is a role of the government (Novak & Brownell,
The evaluation phase would be characterised by activities such as comparing the outcome
with what was envisioned in the project plan to identify any deviations or conformity.
Recommendation
The recommendation phase
The final phase of the strategy would involve activities such as making suggestions on
what ought to have been improved in the implementation or what needs to be improved in the
next project. The success of each of these phases would significantly contribute to the success of
the strategy Lombard et al., 2015).
Various stakeholders would be needed to implement the obesity prevention strategy
successfully. The stakeholders include the Government, private organizations, the family and
community members, healthcare providers and schools. Each of these stakeholders would play
an essential role in the successful implementation of the intervention.
The government would be a key player for several reasons. Policy changes targeted at the
production manufacture, packaging, marketing and labelling of food is only possible through the
intervention of the government. Notably, the role of the government in enhancing food security
would improve the availability of healthy food choices for the target population (World Health
Organization, 2019 b). Similarly, the use of government subsidies, regulation of quotas, import
tariffs and taxes would enhance the availability and affordability of healthy foods. Besides,
taxation policies are an essential requirement in the reduction of socioeconomic inequalities
attributed to health inequalities. Notably, the implementation of urban planning and transport
policies such as the availing of recreational spaces, provision of walking and cycling spaces as
well as the prioritization of public transport is a role of the government (Novak & Brownell,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2012). Besides, the government would also be a significant player in the development of
education materials especially those focused on school children to ensure that the included
content meets various educational guidelines.
Secondly, schools are also a key player in the successful implementation of the
intervention. The role of the school would be majorly in the provision of the necessary education
to enable children and youths to lead healthier lives through healthy food selections. Also,
schools play a substantial role in obesity prevention by observing nutritional guidelines such as
offering meals with sufficient nutrients and calories. Similarly, their role in the provision of
opportunities for physical activities is a crucial aspect of the intervention (Harrison & Peggs,
2012).
Thirdly, the role of the community is also a substantial requirement in the success of the
intervention. Generally, children and youth’s behavior patterns are a reflection of the
communities in which they have grown. In the community setting, Parents play a significant role
in shaping the behavior of their children. On this note, parents who highly value activity and
healthier eating habits are likely to have children portraying the same traits (Ward et al., 2011).
Consequently, children who have grown in communities that highly value physical activity and
healthy eating habits are more likely to make healthy food choices and take part in physical
activities. The focus of members of the community in encouraging healthy lifestyles among
children and youths is, therefore, a significant determinant of the success of the intervention.
Also, the private sector is a significant player in the intervention. The role of the private
sector in childhood and youth obesity prevention lies in the creation and promotion of
information, opportunities and products targeted at encouraging regular physical activity and
healthy eating. The private sector in collaboration with the public sector would also be required
education materials especially those focused on school children to ensure that the included
content meets various educational guidelines.
Secondly, schools are also a key player in the successful implementation of the
intervention. The role of the school would be majorly in the provision of the necessary education
to enable children and youths to lead healthier lives through healthy food selections. Also,
schools play a substantial role in obesity prevention by observing nutritional guidelines such as
offering meals with sufficient nutrients and calories. Similarly, their role in the provision of
opportunities for physical activities is a crucial aspect of the intervention (Harrison & Peggs,
2012).
Thirdly, the role of the community is also a substantial requirement in the success of the
intervention. Generally, children and youth’s behavior patterns are a reflection of the
communities in which they have grown. In the community setting, Parents play a significant role
in shaping the behavior of their children. On this note, parents who highly value activity and
healthier eating habits are likely to have children portraying the same traits (Ward et al., 2011).
Consequently, children who have grown in communities that highly value physical activity and
healthy eating habits are more likely to make healthy food choices and take part in physical
activities. The focus of members of the community in encouraging healthy lifestyles among
children and youths is, therefore, a significant determinant of the success of the intervention.
Also, the private sector is a significant player in the intervention. The role of the private
sector in childhood and youth obesity prevention lies in the creation and promotion of
information, opportunities and products targeted at encouraging regular physical activity and
healthy eating. The private sector in collaboration with the public sector would also be required
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
to take part in efforts to modify the environments limiting health behaviours such as physical
activity and healthy eating habits (Huang & Yaroch, 2009). The private sector would also be a
significant source of funding for the implementation of the intervention.
Healthcare providers are largely more knowledgeable on the interventions and strategies
needed to deal with health issues. For this reason, they would be a significant player in the
development of obesity prevention education materials targeted at communities, individuals and
schools. Because of their knowledge on health issues, they would ensure that the educational
materials align with the requirements of the strategy and meet the needs of the target population.
The delivery of educational materials to individuals and communities would also be done by
healthcare providers in collaboration with private organizations and members of the community
(Wolfenden et al., 2016)
Because of the collaborative nature of the intervention, the leadership of the project
would comprise selected persons from all stakeholder groups. This would also apply to the
management of the budget and finances for the project. The use of multidimensional teams to
carry out these activities would enhance efficiency; promote accountability and success of the
intervention.
.
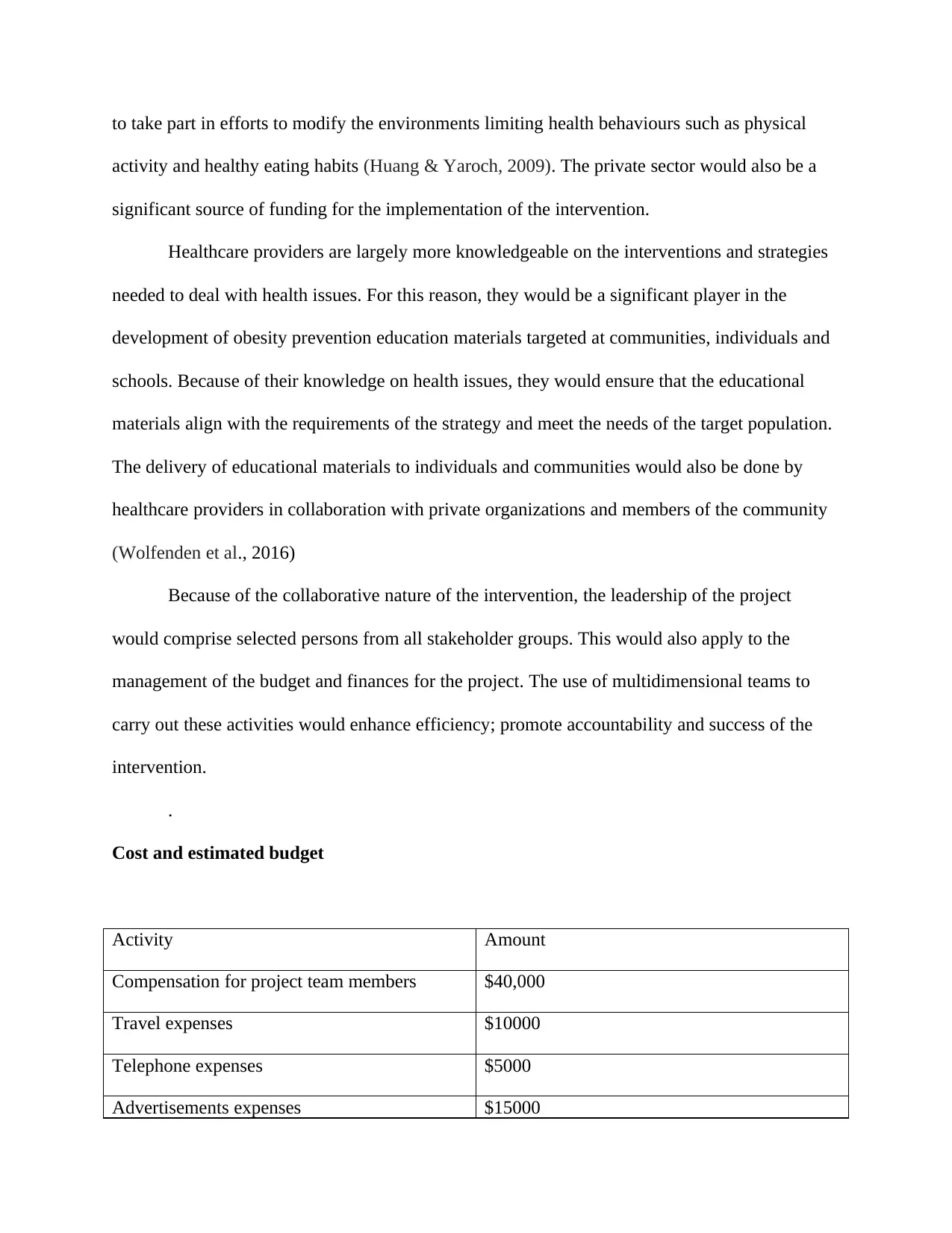
Cost and estimated budget
Activity Amount
Compensation for project team members $40,000
Travel expenses $10000
Telephone expenses $5000
Advertisements expenses $15000
activity and healthy eating habits (Huang & Yaroch, 2009). The private sector would also be a
significant source of funding for the implementation of the intervention.
Healthcare providers are largely more knowledgeable on the interventions and strategies
needed to deal with health issues. For this reason, they would be a significant player in the
development of obesity prevention education materials targeted at communities, individuals and
schools. Because of their knowledge on health issues, they would ensure that the educational
materials align with the requirements of the strategy and meet the needs of the target population.
The delivery of educational materials to individuals and communities would also be done by
healthcare providers in collaboration with private organizations and members of the community
(Wolfenden et al., 2016)
Because of the collaborative nature of the intervention, the leadership of the project
would comprise selected persons from all stakeholder groups. This would also apply to the
management of the budget and finances for the project. The use of multidimensional teams to
carry out these activities would enhance efficiency; promote accountability and success of the
intervention.
.
Cost and estimated budget
Activity Amount
Compensation for project team members $40,000
Travel expenses $10000
Telephone expenses $5000
Advertisements expenses $15000
Material purchasing and cost for printing
educational materials
$20,000
Community educational seminars $100,000
Miscellaneous $2500
Total Budget $192500
Recommendations
Generally, various strategies may be used to deal with the issue of childhood obesity. The
first strategy would be encouraging healthy eating habits at the family level. Focusing on healthy
eating from the family level would mould infants into individuals who can choose appropriate
diets. Secondly, acting as role models may also be an effective strategy to encourage healthy
habits in children and youths. Parents need to b actively involved in physical activity and healthy
living habits to have their children emulate them. Promoting physical activity would also
contribute to reduced cases of childhood obesity. Whether at home or in the home environment,
there is a need to ensure that children engage in at least one hour of physical activity every day.
References
educational materials
$20,000
Community educational seminars $100,000
Miscellaneous $2500
Total Budget $192500
Recommendations
Generally, various strategies may be used to deal with the issue of childhood obesity. The
first strategy would be encouraging healthy eating habits at the family level. Focusing on healthy
eating from the family level would mould infants into individuals who can choose appropriate
diets. Secondly, acting as role models may also be an effective strategy to encourage healthy
habits in children and youths. Parents need to b actively involved in physical activity and healthy
living habits to have their children emulate them. Promoting physical activity would also
contribute to reduced cases of childhood obesity. Whether at home or in the home environment,
there is a need to ensure that children engage in at least one hour of physical activity every day.
References
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Arora, A., Poudel, P., Manohar, N., Bhole, S., & Baur, L. A. (2019). The role of oral health care
professionals in preventing and managing obesity: A systematic review of current
practices and perceived barriers. Obesity research & clinical practice.
Australian Bureau of Statistics. (2019). 4364.0.55.001 - National Health Survey: First Results,
2017-18. Retrieved 21 October 2019, from
https://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001
Black, N., Hughes, R., & Jones, A. M. (2018). The health care costs of childhood obesity in
Australia: An instrumental variables approach. Economics & Human Biology, 31, 1-13.
Harrison, M. K., & Peggs, C. (2012). The role of schools in preventing childhood obesity. The
West Virginia Medical Journal, 98(6), 260-262.
Huang, T. T., & Yaroch, A. L. (2009). A public-private partnership model for obesity
prevention. Preventing chronic disease, 6(3).
Flynn, M. A. T., McNeil, D. A., Maloff, B., Mutasingwa, D., Wu, M., Ford, C., & Tough, S. C.
(2006). Reducing obesity and related chronic disease risk in children and youth: a
synthesis of evidence with ‘best practice’recommendations. Obesity reviews, 7, 7-66.
Kar, S. S., Dube, R., & Kar, S. S. (2014). Childhood obesity-an insight into preventive
strategies. Avicenna journal of medicine, 4(4), 88.
Lombard, C. B., Harrison, C. L., Kozica, S. L., Zoungas, S., Keating, C., & Teede, H. J. (2014).
Effectiveness and implementation of an obesity prevention intervention: the HeLP-her
Rural cluster randomised controlled trial. BMC public health, 14(1), 608.
Novak, N. L., & Brownell, K. D. (2012). Role of policy and government in the obesity
epidemic. Circulation, 126(19), 2345-2352.
professionals in preventing and managing obesity: A systematic review of current
practices and perceived barriers. Obesity research & clinical practice.
Australian Bureau of Statistics. (2019). 4364.0.55.001 - National Health Survey: First Results,
2017-18. Retrieved 21 October 2019, from
https://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001
Black, N., Hughes, R., & Jones, A. M. (2018). The health care costs of childhood obesity in
Australia: An instrumental variables approach. Economics & Human Biology, 31, 1-13.
Harrison, M. K., & Peggs, C. (2012). The role of schools in preventing childhood obesity. The
West Virginia Medical Journal, 98(6), 260-262.
Huang, T. T., & Yaroch, A. L. (2009). A public-private partnership model for obesity
prevention. Preventing chronic disease, 6(3).
Flynn, M. A. T., McNeil, D. A., Maloff, B., Mutasingwa, D., Wu, M., Ford, C., & Tough, S. C.
(2006). Reducing obesity and related chronic disease risk in children and youth: a
synthesis of evidence with ‘best practice’recommendations. Obesity reviews, 7, 7-66.
Kar, S. S., Dube, R., & Kar, S. S. (2014). Childhood obesity-an insight into preventive
strategies. Avicenna journal of medicine, 4(4), 88.
Lombard, C. B., Harrison, C. L., Kozica, S. L., Zoungas, S., Keating, C., & Teede, H. J. (2014).
Effectiveness and implementation of an obesity prevention intervention: the HeLP-her
Rural cluster randomised controlled trial. BMC public health, 14(1), 608.
Novak, N. L., & Brownell, K. D. (2012). Role of policy and government in the obesity
epidemic. Circulation, 126(19), 2345-2352.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
World Health Organization. (2019). Childhood overweight and obesity. Retrieved 21 October
2019, from https://www.who.int/dietphysicalactivity/childhood/en/
World Health Organization. (2019). Population-based approaches to CHILDHOOD OBESITY
PREVENTION. Retrieved 21 October 2019, from
https://www.who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREV
ENTION_27nov_HR_PRINT_OK.pdf
Ward, D. S., Vaughn, A. E., Bangdiwala, S. I., Campbell, M., Jones, D. J., Panter, A. T., &
Stevens, J. (2011). Integrating a family-focused approach into child obesity prevention:
Rationale and design for the My Parenting SOS study randomized control trial. BMC
public health, 11(1), 431.
Wolfenden, L., Jones, J., Williams, C. M., Finch, M., Wyse, R. J., Kingsland, M., ... & Small, T.
(2016). Strategies to improve the implementation of healthy eating, physical activity and
obesity prevention policies, practices or programmes within childcare services. Cochrane
Database of Systematic Reviews, (10).
2019, from https://www.who.int/dietphysicalactivity/childhood/en/
World Health Organization. (2019). Population-based approaches to CHILDHOOD OBESITY
PREVENTION. Retrieved 21 October 2019, from
https://www.who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREV
ENTION_27nov_HR_PRINT_OK.pdf
Ward, D. S., Vaughn, A. E., Bangdiwala, S. I., Campbell, M., Jones, D. J., Panter, A. T., &
Stevens, J. (2011). Integrating a family-focused approach into child obesity prevention:
Rationale and design for the My Parenting SOS study randomized control trial. BMC
public health, 11(1), 431.
Wolfenden, L., Jones, J., Williams, C. M., Finch, M., Wyse, R. J., Kingsland, M., ... & Small, T.
(2016). Strategies to improve the implementation of healthy eating, physical activity and
obesity prevention policies, practices or programmes within childcare services. Cochrane
Database of Systematic Reviews, (10).
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





