Occupational Therapy Report: Michael's Intervention for Daily Living
VerifiedAdded on 2020/05/08
|15
|3366
|126
Report
AI Summary
This report presents an occupational therapy intervention plan for Michael, focusing on enhancing his motivation and skills in activities of daily living (ADL) and personal care, guided by the Model of Human Occupation (MOHO). The plan involves collaboration with a nutritionist to evaluate eating patterns and improve lunch preparation skills, along with assessments using the Canadian Occupational Performance Measure (COPM) to identify functional deficits and establish therapeutic goals. Short-term goals include internet research and family discussions, while long-term goals focus on improving postural control, strength, and motor skills through exercises and environmental adaptations. The intervention includes various sessions at home with positive reinforcement and family involvement. The Modified Barthel Index (MBI) is used to measure progress in ADL, covering areas such as ambulation, lunch preparation, and laundry management. The report emphasizes the importance of a patient-centered approach with clear goals and outcomes.
Answer 1
Michael is the subject of evidence-based occupational interventions advocated by Model of Human Occupation (MOHO) and
requiring administration with the objective of enhancing his motivation to facilitate the pattern of activities of daily living and
personal care. MOHO based approaches are prevalently utilized by occupational therapists in mental health practice in the context of
elevating the psychosocial outcomes in mentally challenged individuals (Lee, et al., 2012). The occupational therapist will attempt to
enhance the pattern of patient’s attributes including his performance, habituation and volition in the context of improving his skills
related to the configuration of a daily lunch for school. The therapist would require systematically collaborating with a qualified
nutritionist with the objective of evaluating the nutrition behavior and eating pattern of Michael in the community environment.
Accordingly, the occupational therapist and nutritionist will require actively engaging with the patient as well as his family members
in the process of lunch making and affectionately greet him at each step of lunch preparation for improving the level of his confidence
and motivation in undertaking the desirable task on a routine basis (Jastran, Bisogni, Sobal, Blake, & Devinee, 2009). The systematic
alteration in patient’s eating choices might prove to be a significant clue to the occupational therapist in relation to the induction of his
self-enhancement pattern regarding lunch preparation.
Answer 2
The occupational therapist will evaluate various performance indicators for Michael after obtaining consent from his family
members. This will require the systematic configuration of professional boundaries with the objective of engaging the patient for
identifying the functional deficits requiring systematic mitigation through occupational intervention. Utilization of COPM (Canadian
Michael is the subject of evidence-based occupational interventions advocated by Model of Human Occupation (MOHO) and
requiring administration with the objective of enhancing his motivation to facilitate the pattern of activities of daily living and
personal care. MOHO based approaches are prevalently utilized by occupational therapists in mental health practice in the context of
elevating the psychosocial outcomes in mentally challenged individuals (Lee, et al., 2012). The occupational therapist will attempt to
enhance the pattern of patient’s attributes including his performance, habituation and volition in the context of improving his skills
related to the configuration of a daily lunch for school. The therapist would require systematically collaborating with a qualified
nutritionist with the objective of evaluating the nutrition behavior and eating pattern of Michael in the community environment.
Accordingly, the occupational therapist and nutritionist will require actively engaging with the patient as well as his family members
in the process of lunch making and affectionately greet him at each step of lunch preparation for improving the level of his confidence
and motivation in undertaking the desirable task on a routine basis (Jastran, Bisogni, Sobal, Blake, & Devinee, 2009). The systematic
alteration in patient’s eating choices might prove to be a significant clue to the occupational therapist in relation to the induction of his
self-enhancement pattern regarding lunch preparation.
Answer 2
The occupational therapist will evaluate various performance indicators for Michael after obtaining consent from his family
members. This will require the systematic configuration of professional boundaries with the objective of engaging the patient for
identifying the functional deficits requiring systematic mitigation through occupational intervention. Utilization of COPM (Canadian
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Occupational Performance Measure) diagnostic modality will assist in evaluating the patient perspective for taking informed clinical
decisions in the context of acquiring desirable mental health outcomes (Colquhoun, Letts, Law, MacDermid, & Missiuna, 2012). The
COPM assessment tool will assist in identifying the individual perception of the patient in relation to the constraints faced by him in
day-to-day life. This tool will facilitate the administration of personalized healthcare interventions with the objective of mitigating the
constraints and challenges experienced by Michael in real life situations. The occupational intervention would require conducting
semi-structured interview with the objective of evaluating the apprehensions, perspectives, thought process and fears of the patient in
relation to the effective undertaking of tasks attributing to the lunch preparation, laundry management and traveling through bus to a
pre-defined destination. Indeed, after the systematic evaluation of Michael’s perceptions regarding the functional activities the
occupational therapist will systematically establish therapeutic goals and their accomplishment timeline with the objective of
facilitating their step-by-step accomplishment for the acquisition of the desirable functional outcomes. These therapeutic goals require
a thorough discussion with the patient and his family members before their eventual establishment. The occupational therapist will
require accessing patient’s immediate environment for identifying the significant cues could facilitate his functional enhancement in
accordance with the established therapeutic goals. For example, the occupational therapist will require accessing patient’s kitchen and
evaluate the space and types of equipment available for helping Michael in the process of lunch-preparation. This will assist in the
systematic configuration of various motivational interventions warranting administration for improving patient’s cooking capacity
required to facilitate his self-sufficiency in relation to the process of lunch making on a routine basis. Similarly, the occupational
therapist would require assessing patient’s laundry management skills with the objective of exploring the scope of improvement in
decisions in the context of acquiring desirable mental health outcomes (Colquhoun, Letts, Law, MacDermid, & Missiuna, 2012). The
COPM assessment tool will assist in identifying the individual perception of the patient in relation to the constraints faced by him in
day-to-day life. This tool will facilitate the administration of personalized healthcare interventions with the objective of mitigating the
constraints and challenges experienced by Michael in real life situations. The occupational intervention would require conducting
semi-structured interview with the objective of evaluating the apprehensions, perspectives, thought process and fears of the patient in
relation to the effective undertaking of tasks attributing to the lunch preparation, laundry management and traveling through bus to a
pre-defined destination. Indeed, after the systematic evaluation of Michael’s perceptions regarding the functional activities the
occupational therapist will systematically establish therapeutic goals and their accomplishment timeline with the objective of
facilitating their step-by-step accomplishment for the acquisition of the desirable functional outcomes. These therapeutic goals require
a thorough discussion with the patient and his family members before their eventual establishment. The occupational therapist will
require accessing patient’s immediate environment for identifying the significant cues could facilitate his functional enhancement in
accordance with the established therapeutic goals. For example, the occupational therapist will require accessing patient’s kitchen and
evaluate the space and types of equipment available for helping Michael in the process of lunch-preparation. This will assist in the
systematic configuration of various motivational interventions warranting administration for improving patient’s cooking capacity
required to facilitate his self-sufficiency in relation to the process of lunch making on a routine basis. Similarly, the occupational
therapist would require assessing patient’s laundry management skills with the objective of exploring the scope of improvement in
undertaking laundry associated tasks. The occupational therapist will systematically evaluate patient’s confidence level in relation to
the process of independent commutation through bus and other transport vehicles. This will assist in the identification of sustained
psychosomatic deficits that hinder the motivation of the patient in terms of commuting through the bus to the local shops. The patient
feedback obtained through the COPM Intervention will substantially assist the occupational therapist as well as patient’s family
members in terms of establishing evidence-based therapeutic goals for the substantial enhancement of patient’s psychosocial potential
warranted for undertaking the desirable activities of daily living and personal care (Yang, Lin, Lee, & Chang, 2017). The COPM
intervention will also evaluate the level of patient’s responsiveness as well as willingness in terms of undertaking and accomplishing
desirable occupational goals (Rehab Measures: Canadian Occupational Performance Measure, 2013). The COPM measure will also
record the subjective experiences of Michael in relation to the prospective personal care goals, including any associated performance
failures that he might have had experienced in the past while attempting to prepare his school lunch, managing the laundry and
traveling to local shops through bus after School. These measurements will substantially assist the occupational therapist in terms of
configuring real time strategies for the acquisition of Michale’s occupational outcomes. Data obtained from the semi-structured
interview will require systematic recording the clinical database for its statistical analysis.
Answer 3
Short-term goal for Michael will include accessing internet for reading the methods for lunch preparation and laundry
management. The patient will require understanding each step of both processes through the internet and then discussing the content
with his family members. This will eventually prepare his mind towards undertaking these activities of daily living and personal care
the process of independent commutation through bus and other transport vehicles. This will assist in the identification of sustained
psychosomatic deficits that hinder the motivation of the patient in terms of commuting through the bus to the local shops. The patient
feedback obtained through the COPM Intervention will substantially assist the occupational therapist as well as patient’s family
members in terms of establishing evidence-based therapeutic goals for the substantial enhancement of patient’s psychosocial potential
warranted for undertaking the desirable activities of daily living and personal care (Yang, Lin, Lee, & Chang, 2017). The COPM
intervention will also evaluate the level of patient’s responsiveness as well as willingness in terms of undertaking and accomplishing
desirable occupational goals (Rehab Measures: Canadian Occupational Performance Measure, 2013). The COPM measure will also
record the subjective experiences of Michael in relation to the prospective personal care goals, including any associated performance
failures that he might have had experienced in the past while attempting to prepare his school lunch, managing the laundry and
traveling to local shops through bus after School. These measurements will substantially assist the occupational therapist in terms of
configuring real time strategies for the acquisition of Michale’s occupational outcomes. Data obtained from the semi-structured
interview will require systematic recording the clinical database for its statistical analysis.
Answer 3
Short-term goal for Michael will include accessing internet for reading the methods for lunch preparation and laundry
management. The patient will require understanding each step of both processes through the internet and then discussing the content
with his family members. This will eventually prepare his mind towards undertaking these activities of daily living and personal care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
while effectively mitigating the negative apprehensions. Michael will require visiting the bus stand on a daily basis and view the
process of visitors boarding from buses. This will increase his confidence and motivation in terms of taking systematic steps for
accomplishing the long-term occupational therapy goals.
The long-term OT goal will include the sustained enhancement of patient’s postural control, strength and physical endurance to
facilitate the coordinated functioning of upper extremities. The patient will learn to maintain appropriate posture consistently for a
duration of 30 minutes without experiencing the pattern of ataxia or gait related abnormality. Improved postural control will
eventually improve the pattern of patient’s fine motor skills required for undertaking the activities of daily living (Wang, Howe,
Hinojosa, & Weinberg, 2011). The enhancement of patient’s motor skills will also improve his pattern of his attention and focus while
performing the desirable activities (Wulf, Shea, & Lewthwaite, 2010). This administration of this self-controlled intervention under
the assistance of occupational therapist and family members will facilitate the timely accomplishment of patient’s ADL-goals. Patient
will also require undertaking dumbbell exercise with the objective of improving his extremity function required for activities like
lunch preparation, laundry management and traveling through bus. Indeed, patient’s extremity improvement will substantially restore
the pattern of his functional independence in the community environment (Wang, Greendale, Kazadi, & Salem, 2012).
process of visitors boarding from buses. This will increase his confidence and motivation in terms of taking systematic steps for
accomplishing the long-term occupational therapy goals.
The long-term OT goal will include the sustained enhancement of patient’s postural control, strength and physical endurance to
facilitate the coordinated functioning of upper extremities. The patient will learn to maintain appropriate posture consistently for a
duration of 30 minutes without experiencing the pattern of ataxia or gait related abnormality. Improved postural control will
eventually improve the pattern of patient’s fine motor skills required for undertaking the activities of daily living (Wang, Howe,
Hinojosa, & Weinberg, 2011). The enhancement of patient’s motor skills will also improve his pattern of his attention and focus while
performing the desirable activities (Wulf, Shea, & Lewthwaite, 2010). This administration of this self-controlled intervention under
the assistance of occupational therapist and family members will facilitate the timely accomplishment of patient’s ADL-goals. Patient
will also require undertaking dumbbell exercise with the objective of improving his extremity function required for activities like
lunch preparation, laundry management and traveling through bus. Indeed, patient’s extremity improvement will substantially restore
the pattern of his functional independence in the community environment (Wang, Greendale, Kazadi, & Salem, 2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
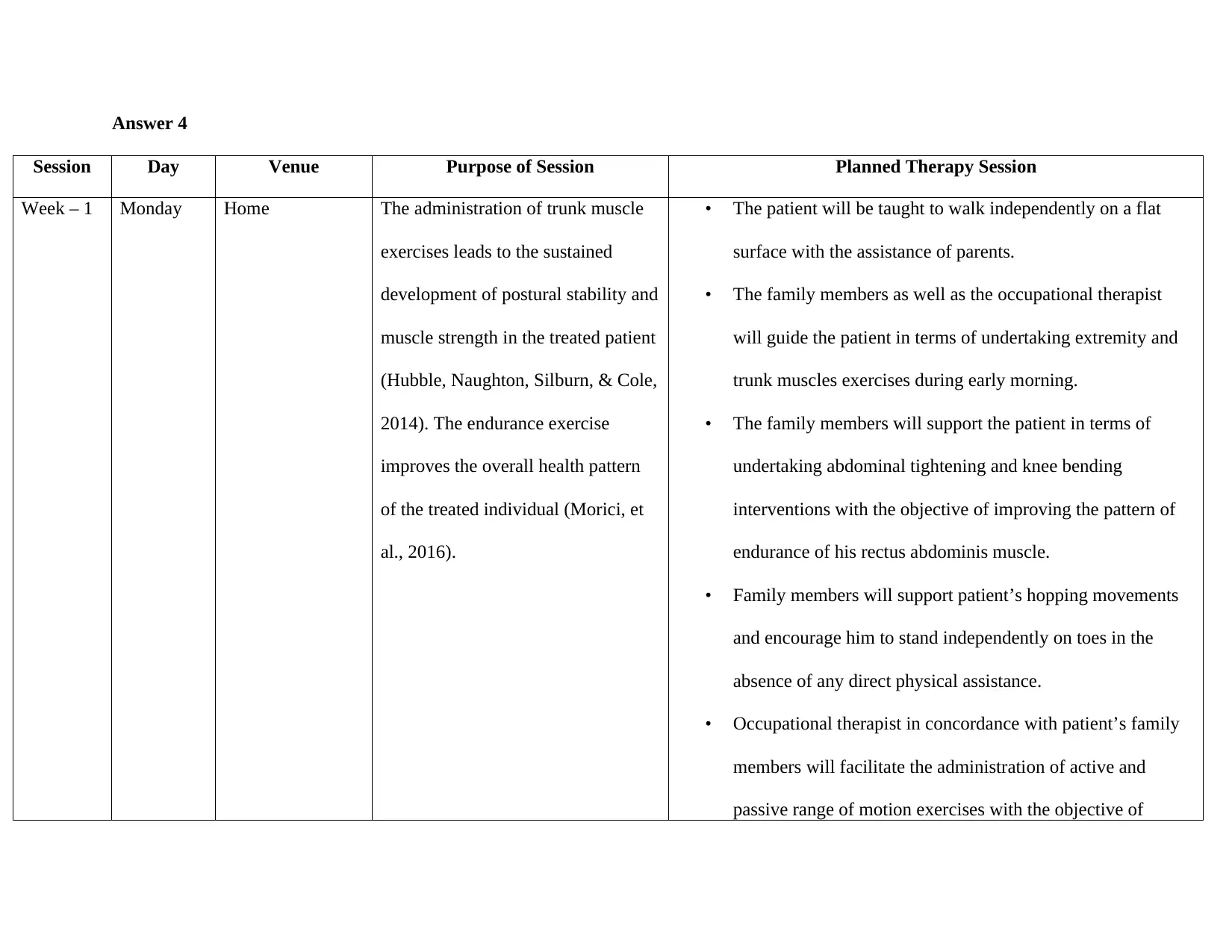
Answer 4
Session Day Venue Purpose of Session Planned Therapy Session
Week – 1 Monday Home The administration of trunk muscle
exercises leads to the sustained
development of postural stability and
muscle strength in the treated patient
(Hubble, Naughton, Silburn, & Cole,
2014). The endurance exercise
improves the overall health pattern
of the treated individual (Morici, et
al., 2016).
• The patient will be taught to walk independently on a flat
surface with the assistance of parents.
• The family members as well as the occupational therapist
will guide the patient in terms of undertaking extremity and
trunk muscles exercises during early morning.
• The family members will support the patient in terms of
undertaking abdominal tightening and knee bending
interventions with the objective of improving the pattern of
endurance of his rectus abdominis muscle.
• Family members will support patient’s hopping movements
and encourage him to stand independently on toes in the
absence of any direct physical assistance.
• Occupational therapist in concordance with patient’s family
members will facilitate the administration of active and
passive range of motion exercises with the objective of
Session Day Venue Purpose of Session Planned Therapy Session
Week – 1 Monday Home The administration of trunk muscle
exercises leads to the sustained
development of postural stability and
muscle strength in the treated patient
(Hubble, Naughton, Silburn, & Cole,
2014). The endurance exercise
improves the overall health pattern
of the treated individual (Morici, et
al., 2016).
• The patient will be taught to walk independently on a flat
surface with the assistance of parents.
• The family members as well as the occupational therapist
will guide the patient in terms of undertaking extremity and
trunk muscles exercises during early morning.
• The family members will support the patient in terms of
undertaking abdominal tightening and knee bending
interventions with the objective of improving the pattern of
endurance of his rectus abdominis muscle.
• Family members will support patient’s hopping movements
and encourage him to stand independently on toes in the
absence of any direct physical assistance.
• Occupational therapist in concordance with patient’s family
members will facilitate the administration of active and
passive range of motion exercises with the objective of
improving the muscle flexibility.
• Patient’s family members will configure a safe and protective
environment for the patient while motivating him for
physical exercise in the context of reducing the scope of
prospective trauma and associated adverse manifestations.
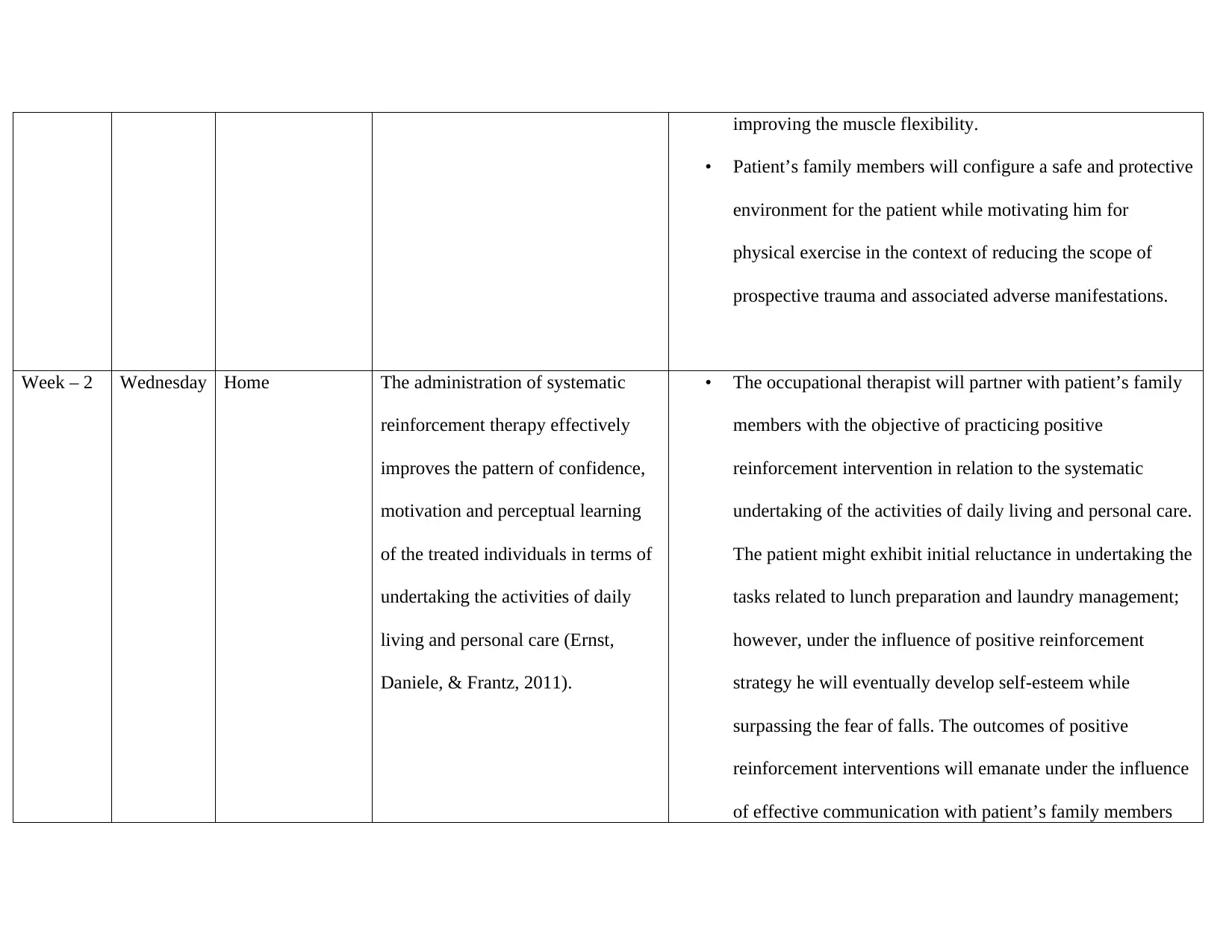
Week – 2 Wednesday Home The administration of systematic
reinforcement therapy effectively
improves the pattern of confidence,
motivation and perceptual learning
of the treated individuals in terms of
undertaking the activities of daily
living and personal care (Ernst,
Daniele, & Frantz, 2011).
• The occupational therapist will partner with patient’s family
members with the objective of practicing positive
reinforcement intervention in relation to the systematic
undertaking of the activities of daily living and personal care.
The patient might exhibit initial reluctance in undertaking the
tasks related to lunch preparation and laundry management;
however, under the influence of positive reinforcement
strategy he will eventually develop self-esteem while
surpassing the fear of falls. The outcomes of positive
reinforcement interventions will emanate under the influence
of effective communication with patient’s family members
• Patient’s family members will configure a safe and protective
environment for the patient while motivating him for
physical exercise in the context of reducing the scope of
prospective trauma and associated adverse manifestations.
Week – 2 Wednesday Home The administration of systematic
reinforcement therapy effectively
improves the pattern of confidence,
motivation and perceptual learning
of the treated individuals in terms of
undertaking the activities of daily
living and personal care (Ernst,
Daniele, & Frantz, 2011).
• The occupational therapist will partner with patient’s family
members with the objective of practicing positive
reinforcement intervention in relation to the systematic
undertaking of the activities of daily living and personal care.
The patient might exhibit initial reluctance in undertaking the
tasks related to lunch preparation and laundry management;
however, under the influence of positive reinforcement
strategy he will eventually develop self-esteem while
surpassing the fear of falls. The outcomes of positive
reinforcement interventions will emanate under the influence
of effective communication with patient’s family members
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(Greenberg, 2010).
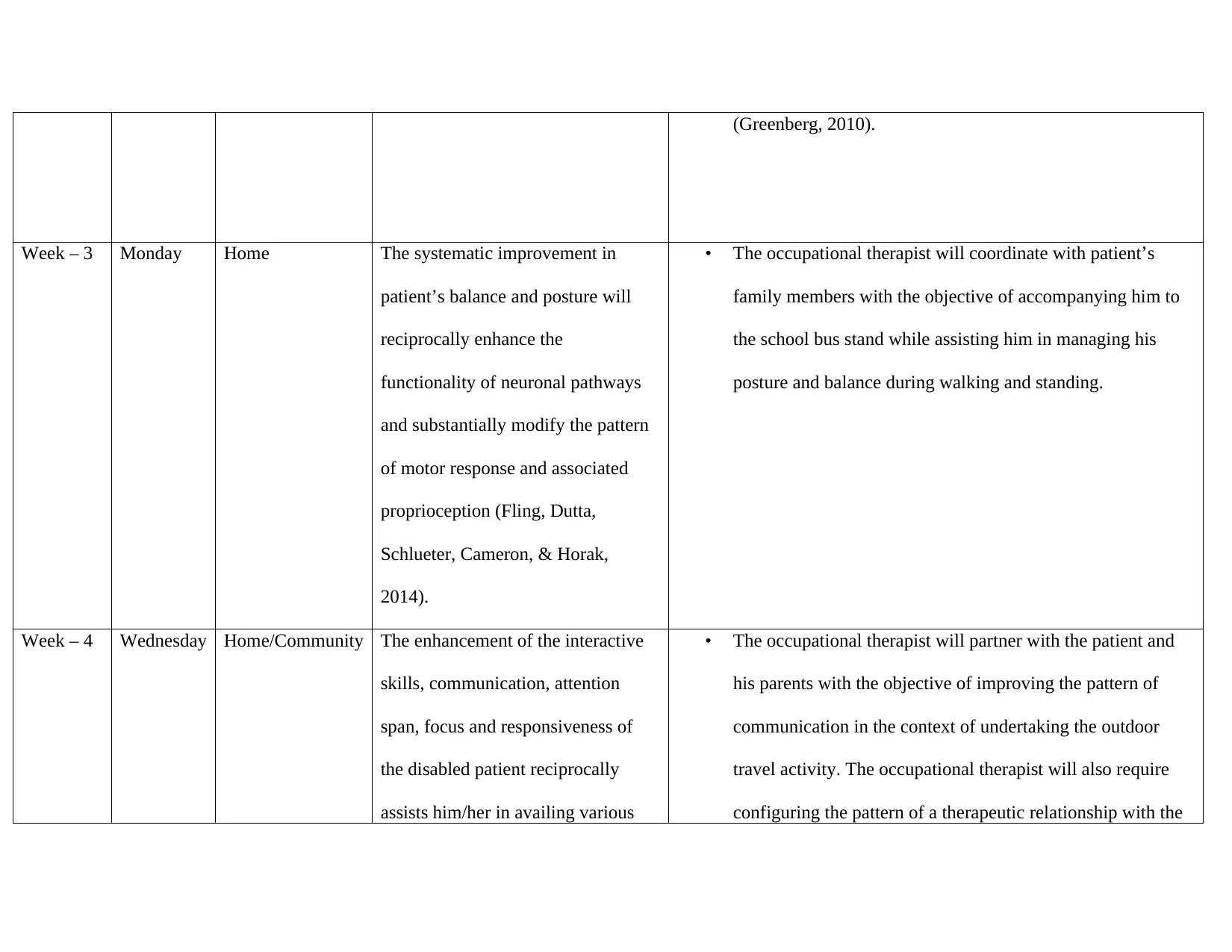
Week – 3 Monday Home The systematic improvement in
patient’s balance and posture will
reciprocally enhance the
functionality of neuronal pathways
and substantially modify the pattern
of motor response and associated
proprioception (Fling, Dutta,
Schlueter, Cameron, & Horak,
2014).
• The occupational therapist will coordinate with patient’s
family members with the objective of accompanying him to
the school bus stand while assisting him in managing his
posture and balance during walking and standing.
Week – 4 Wednesday Home/Community The enhancement of the interactive
skills, communication, attention
span, focus and responsiveness of
the disabled patient reciprocally
assists him/her in availing various
• The occupational therapist will partner with the patient and
his parents with the objective of improving the pattern of
communication in the context of undertaking the outdoor
travel activity. The occupational therapist will also require
configuring the pattern of a therapeutic relationship with the
Week – 3 Monday Home The systematic improvement in
patient’s balance and posture will
reciprocally enhance the
functionality of neuronal pathways
and substantially modify the pattern
of motor response and associated
proprioception (Fling, Dutta,
Schlueter, Cameron, & Horak,
2014).
• The occupational therapist will coordinate with patient’s
family members with the objective of accompanying him to
the school bus stand while assisting him in managing his
posture and balance during walking and standing.
Week – 4 Wednesday Home/Community The enhancement of the interactive
skills, communication, attention
span, focus and responsiveness of
the disabled patient reciprocally
assists him/her in availing various
• The occupational therapist will partner with the patient and
his parents with the objective of improving the pattern of
communication in the context of undertaking the outdoor
travel activity. The occupational therapist will also require
configuring the pattern of a therapeutic relationship with the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
public transport and shopping
services (Bigby, et al., 2017).
patient in the context of mitigating the physical, emotional
and social constraints that he might experience while
attempting to climb stairs and travel to the local shops.
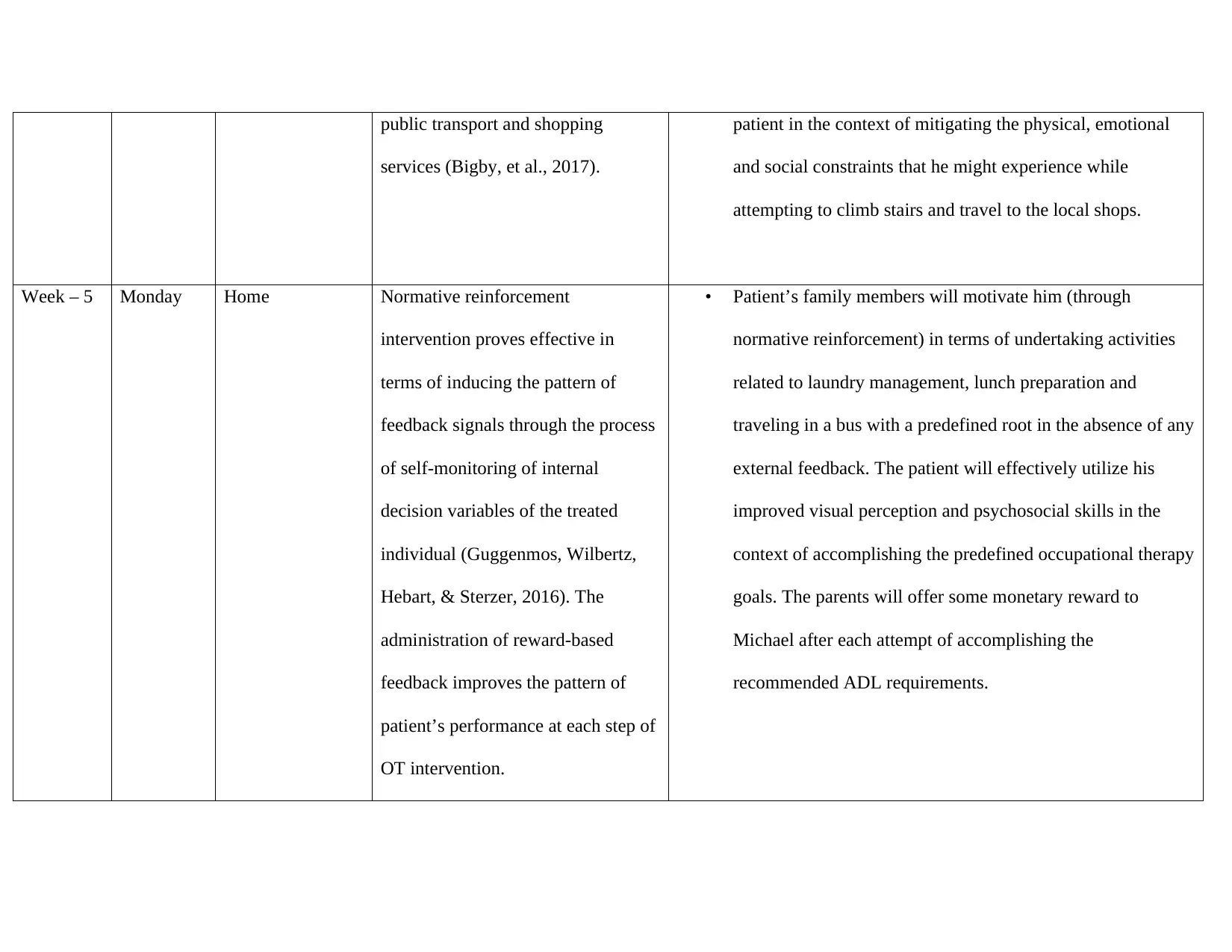
Week – 5 Monday Home Normative reinforcement
intervention proves effective in
terms of inducing the pattern of
feedback signals through the process
of self-monitoring of internal
decision variables of the treated
individual (Guggenmos, Wilbertz,
Hebart, & Sterzer, 2016). The
administration of reward-based
feedback improves the pattern of
patient’s performance at each step of
OT intervention.
• Patient’s family members will motivate him (through
normative reinforcement) in terms of undertaking activities
related to laundry management, lunch preparation and
traveling in a bus with a predefined root in the absence of any
external feedback. The patient will effectively utilize his
improved visual perception and psychosocial skills in the
context of accomplishing the predefined occupational therapy
goals. The parents will offer some monetary reward to
Michael after each attempt of accomplishing the
recommended ADL requirements.
services (Bigby, et al., 2017).
patient in the context of mitigating the physical, emotional
and social constraints that he might experience while
attempting to climb stairs and travel to the local shops.
Week – 5 Monday Home Normative reinforcement
intervention proves effective in
terms of inducing the pattern of
feedback signals through the process
of self-monitoring of internal
decision variables of the treated
individual (Guggenmos, Wilbertz,
Hebart, & Sterzer, 2016). The
administration of reward-based
feedback improves the pattern of
patient’s performance at each step of
OT intervention.
• Patient’s family members will motivate him (through
normative reinforcement) in terms of undertaking activities
related to laundry management, lunch preparation and
traveling in a bus with a predefined root in the absence of any
external feedback. The patient will effectively utilize his
improved visual perception and psychosocial skills in the
context of accomplishing the predefined occupational therapy
goals. The parents will offer some monetary reward to
Michael after each attempt of accomplishing the
recommended ADL requirements.
Answer 5
The occupational therapist would require utilizing MBI (Modified Barthel Index) outcome measurement tool for objectively
measuring patient’s improvement in terms of undertaking the activities of daily living and personal care (including lunch preparation,
laundry management and travel to local shops from school through bus). MBI is a reliable tool for assessing the activities of daily
living (Ohura, Hase, Nakajima, & Nakayama, 2017). Scores retrieved through direct observation will define the extent of patient’s
improvement in the context of predefined occupational therapy goals. In terms of ambulation measurement, score-0 will indicate
patient’s complete ambulation dependence. However, score-3 will reveal the requirement of taking assistance from another person for
ambulation. Score-8 will indicate the requirement of physical aids for movement. Score-12 will indicate patient’s movement
independence; however, he might require external assistance for improving the pattern of his confidence and safety during travel.
Score-15 will emphasize the requirement of wearing braces during sitting and walking in the absence of external supervision with the
objective of facilitating hassle free movement of the patient. Similarly, lunch and laundry management tasks will require evaluation
through different scores for evaluating the pattern of overall improvement in Michael’s activities after the occupational therapy
intervention. Scores 0- 20, 21-60, 61-90, 91-99 will indicate the pattern of total, severe, moderate and slight dependence of patient on
the activities of daily living (ADL) (SV, 2017). However, score 100 will reveal complete independence of the patient in terms of
undertaking the pattern of ADL.
Answer 6
The occupational therapist would require utilizing MBI (Modified Barthel Index) outcome measurement tool for objectively
measuring patient’s improvement in terms of undertaking the activities of daily living and personal care (including lunch preparation,
laundry management and travel to local shops from school through bus). MBI is a reliable tool for assessing the activities of daily
living (Ohura, Hase, Nakajima, & Nakayama, 2017). Scores retrieved through direct observation will define the extent of patient’s
improvement in the context of predefined occupational therapy goals. In terms of ambulation measurement, score-0 will indicate
patient’s complete ambulation dependence. However, score-3 will reveal the requirement of taking assistance from another person for
ambulation. Score-8 will indicate the requirement of physical aids for movement. Score-12 will indicate patient’s movement
independence; however, he might require external assistance for improving the pattern of his confidence and safety during travel.
Score-15 will emphasize the requirement of wearing braces during sitting and walking in the absence of external supervision with the
objective of facilitating hassle free movement of the patient. Similarly, lunch and laundry management tasks will require evaluation
through different scores for evaluating the pattern of overall improvement in Michael’s activities after the occupational therapy
intervention. Scores 0- 20, 21-60, 61-90, 91-99 will indicate the pattern of total, severe, moderate and slight dependence of patient on
the activities of daily living (ADL) (SV, 2017). However, score 100 will reveal complete independence of the patient in terms of
undertaking the pattern of ADL.
Answer 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The systematic acquisition of a P-E-O fit warrants the integration of performance, occupational and environmental factors for
generating the desirable outcomes from the occupational therapy intervention. In the presented case scenario, the accomplishment of
patient’s occupational performance will be evident by the level of improvement in his activities of daily living and personal care. The
performance components will require evaluating while assessing Michael’s motor skills and communication pattern. These
components must effectively coordinate with the environmental factors (including patient’s surroundings, societal and cultural
attributes and other natural constraints) and occupational ingredients (occupational/self-care activities, leisure time and productivity)
in the context of acquiring the desirable occupational performance. The systematic integration of the attributes including person,
environment and occupation will eventually reveal the substantial improvement in Michael’s activities of daily living. For example, he
will successfully prepare his lunch, manage the laundry task and commute to the local shops through bus in the absence of an external
assistance. Michal will indeed be able to effectively surpass the environmental constraints and prove to be a good occupational fit in
accordance with the P-E-O fit approach. Michael’s sustained adaptation to the P-E-O fit constraints will affirm the establishment of
his self-sufficiency in terms of independently undertaking the desirable activities (Lien, Steggell, & Iwarsson, 2015).
Bibliography
generating the desirable outcomes from the occupational therapy intervention. In the presented case scenario, the accomplishment of
patient’s occupational performance will be evident by the level of improvement in his activities of daily living and personal care. The
performance components will require evaluating while assessing Michael’s motor skills and communication pattern. These
components must effectively coordinate with the environmental factors (including patient’s surroundings, societal and cultural
attributes and other natural constraints) and occupational ingredients (occupational/self-care activities, leisure time and productivity)
in the context of acquiring the desirable occupational performance. The systematic integration of the attributes including person,
environment and occupation will eventually reveal the substantial improvement in Michael’s activities of daily living. For example, he
will successfully prepare his lunch, manage the laundry task and commute to the local shops through bus in the absence of an external
assistance. Michal will indeed be able to effectively surpass the environmental constraints and prove to be a good occupational fit in
accordance with the P-E-O fit approach. Michael’s sustained adaptation to the P-E-O fit constraints will affirm the establishment of
his self-sufficiency in terms of independently undertaking the desirable activities (Lien, Steggell, & Iwarsson, 2015).
Bibliography
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Bigby , C., Johnson , H., O'Halloran , R., Douglas , J., West , D., & Bould , E. (2017). Communication access on trains: a qualitative
exploration of the perspectives of passengers with communication disabilities. Disability and Rehabilitation, 1-8.
doi:10.1080/09638288.2017.1380721
Colquhoun , H. L., Letts , L. J., Law , M. C., MacDermid , J. C., & Missiuna , C. A. (2012). Administration of the Canadian
Occupational Performance Measure: effect on practice. Canadian Journal of Occupational Therapy, 79(2), 120-128. Retrieved
from https://www.ncbi.nlm.nih.gov/pubmed/22667020
Ernst, M., Daniele, T., & Frantz, K. (2011). New perspectives on adolescent motivated behavior: attention and conditioning.
Developmental Cognitive Neuroscience, 1(4), 377-389. doi:10.1016/j.dcn.2011.07.013
Fling, B. W., Dutta, G. G., Schlueter, H., Cameron, M. H., & Horak, F. B. (2014). Associations between Proprioceptive Neural
Pathway Structural Connectivity and Balance in People with Multiple Sclerosis. Frontiers in Human Neuroscience.
doi:10.3389/fnhum.2014.00814
Greenberg, G. (2010). Positive reinforcement. Can Fam Physician, 56(3), 222. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2837681/
Guggenmos, M., Wilbertz, G., Hebart, M. N., & Sterzer, P. (2016). Mesolimbic confidence signals guide perceptual learning in the
absence of external feedback. eLife. doi:10.7554/eLife.13388
exploration of the perspectives of passengers with communication disabilities. Disability and Rehabilitation, 1-8.
doi:10.1080/09638288.2017.1380721
Colquhoun , H. L., Letts , L. J., Law , M. C., MacDermid , J. C., & Missiuna , C. A. (2012). Administration of the Canadian
Occupational Performance Measure: effect on practice. Canadian Journal of Occupational Therapy, 79(2), 120-128. Retrieved
from https://www.ncbi.nlm.nih.gov/pubmed/22667020
Ernst, M., Daniele, T., & Frantz, K. (2011). New perspectives on adolescent motivated behavior: attention and conditioning.
Developmental Cognitive Neuroscience, 1(4), 377-389. doi:10.1016/j.dcn.2011.07.013
Fling, B. W., Dutta, G. G., Schlueter, H., Cameron, M. H., & Horak, F. B. (2014). Associations between Proprioceptive Neural
Pathway Structural Connectivity and Balance in People with Multiple Sclerosis. Frontiers in Human Neuroscience.
doi:10.3389/fnhum.2014.00814
Greenberg, G. (2010). Positive reinforcement. Can Fam Physician, 56(3), 222. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2837681/
Guggenmos, M., Wilbertz, G., Hebart, M. N., & Sterzer, P. (2016). Mesolimbic confidence signals guide perceptual learning in the
absence of external feedback. eLife. doi:10.7554/eLife.13388
Hubble , R. P., Naughton, G. A., Silburn, P. A., & Cole, M. H. (2014). Trunk muscle exercises as a means of improving postural
stability in people with Parkinson's disease: a protocol for a randomised controlled trial. BMJ Open, 4(12).
doi:10.1136/bmjopen-2014-006095
Jastran, M., Bisogni, C. A., Sobal, J., Blake, C., & Devinee, C. M. (2009). Eating routines: Embedded, value based, modifiable, and
reflective. Appetite, 127–136.
Lee, S. W., Kielhofner, G., Morley, M., Heasman, D., Garnham, M., Willis, S., . . . Taylor, R. R. (2012). Impact of using the Model of
Human Occupation: a survey of occupational therapy mental health practitioners' perceptions. Scandinavain Journal of
Occupational Therapy, 19(5), 450-456.
Lien, L. L., Steggell, C. D., & Iwarsson, S. (2015). Adaptive Strategies and Person-Environment Fit among Functionally Limited
Older Adults Aging in Place: A Mixed Methods Approach. International Journal of Environmental Research and Public
Health, 12(9), 11954–11974. doi:10.3390/ijerph120911954
Morici, G., Auria, C. I., Baiamonte, P., Mazzuca, E., Castrogiovanni, A., & Bonsignore, M. R. (2016). Endurance training: is it bad
for you? Breathe, 140-147. doi:10.1183/20734735.007016
Ohura , T., Hase , K., Nakajima , Y., & Nakayama , T. (2017). Validity and reliability of a performance evaluation tool based on the
modified Barthel Index for stroke patients. BMC Medical Research Methodology, 17(1), 131. doi:10.1186/s12874-017-0409-2
stability in people with Parkinson's disease: a protocol for a randomised controlled trial. BMJ Open, 4(12).
doi:10.1136/bmjopen-2014-006095
Jastran, M., Bisogni, C. A., Sobal, J., Blake, C., & Devinee, C. M. (2009). Eating routines: Embedded, value based, modifiable, and
reflective. Appetite, 127–136.
Lee, S. W., Kielhofner, G., Morley, M., Heasman, D., Garnham, M., Willis, S., . . . Taylor, R. R. (2012). Impact of using the Model of
Human Occupation: a survey of occupational therapy mental health practitioners' perceptions. Scandinavain Journal of
Occupational Therapy, 19(5), 450-456.
Lien, L. L., Steggell, C. D., & Iwarsson, S. (2015). Adaptive Strategies and Person-Environment Fit among Functionally Limited
Older Adults Aging in Place: A Mixed Methods Approach. International Journal of Environmental Research and Public
Health, 12(9), 11954–11974. doi:10.3390/ijerph120911954
Morici, G., Auria, C. I., Baiamonte, P., Mazzuca, E., Castrogiovanni, A., & Bonsignore, M. R. (2016). Endurance training: is it bad
for you? Breathe, 140-147. doi:10.1183/20734735.007016
Ohura , T., Hase , K., Nakajima , Y., & Nakayama , T. (2017). Validity and reliability of a performance evaluation tool based on the
modified Barthel Index for stroke patients. BMC Medical Research Methodology, 17(1), 131. doi:10.1186/s12874-017-0409-2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


