Effect of Oral Care Program on Prevention of VAP in ICU Patients
VerifiedAdded on 2022/09/14
|6
|4853
|17
Report
AI Summary
This report presents the findings of a randomized controlled trial investigating the impact of an oral care program on the prevention of ventilator-associated pneumonia (VAP) in intensive care unit (ICU) patients. The study involved 80 participants, randomly assigned to intervention and control groups. The intervention group received a comprehensive oral care program, while the control group received routine care. Data was collected using questionnaires and the Clinical Pulmonary Infection Score (CPIS). The results indicated that while the oral care program showed a trend towards reducing pneumonia frequency, the difference was not statistically significant. The report concludes that further research with larger sample sizes and longer durations is needed to definitively assess the program's effectiveness. The study highlights the importance of oral hygiene in ICU patients, given their increased susceptibility to oral problems and the risk of VAP, a common nosocomial infection associated with high mortality rates and increased healthcare costs.
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/328066970
Effect of Oral Care Program on Prevention of Ventilator-associated Pneumonia
in Intensive Care Unit Patients: A Randomized Controlled Trial
Article in Iranian journal of nursing and midwifery research · November 2018
DOI: 10.4103/ijnmr.IJNMR_164_17
CITATIONS
2
READS
778
5 authors, including:
Some of the authors of this publication are also working on these related projects:
The effect of designer respiratory care program on the VAP IN the ICUView project
Effect of six sigma program on the number of surgeries cancellationView project
Vajihe Atashi
Isfahan University of Medical Sciences
16PUBLICATIONS35CITATIONS
SEE PROFILE
Hojatollah Yousefi
Isfahan University of Medical Sciences
43PUBLICATIONS231CITATIONS
SEE PROFILE
Hosein Mahjobipoor
6 PUBLICATIONS10CITATIONS
SEE PROFILE
Reza Bekhradi
Barijessence
47PUBLICATIONS490CITATIONS
SEE PROFILE
All content following this page was uploaded by Hojatollah Yousefi on 20 November 2018.
The user has requested enhancement of the downloaded file.
Effect of Oral Care Program on Prevention of Ventilator-associated Pneumonia
in Intensive Care Unit Patients: A Randomized Controlled Trial
Article in Iranian journal of nursing and midwifery research · November 2018
DOI: 10.4103/ijnmr.IJNMR_164_17
CITATIONS
2
READS
778
5 authors, including:
Some of the authors of this publication are also working on these related projects:
The effect of designer respiratory care program on the VAP IN the ICUView project
Effect of six sigma program on the number of surgeries cancellationView project
Vajihe Atashi
Isfahan University of Medical Sciences
16PUBLICATIONS35CITATIONS
SEE PROFILE
Hojatollah Yousefi
Isfahan University of Medical Sciences
43PUBLICATIONS231CITATIONS
SEE PROFILE
Hosein Mahjobipoor
6 PUBLICATIONS10CITATIONS
SEE PROFILE
Reza Bekhradi
Barijessence
47PUBLICATIONS490CITATIONS
SEE PROFILE
All content following this page was uploaded by Hojatollah Yousefi on 20 November 2018.
The user has requested enhancement of the downloaded file.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
486 © 2018 Iranian Journal of Nursing and Midwifery Research | Published by Wolters Kluwer - Medknow
Introduction
One of the common problems of patients
undergoing mechanical ventilation is
poor oral health.[1] Patients in intensive
care units (ICUs) quickly develop oral
problems for various reasons such as
malnutrition, presence of the tracheal tube
and nasogastric tube that is placed in the
mouth of patients for treatment purposes,
reduced fluid intake, and reduced salivation
caused by fever, diarrhea, burns, and drug
usage such as opiates.[2‑4]
In patients in ICUs, dental plaques
are formed more and faster than other
patients.[5] Oral flora changes in the course
of 48 h after hospitalization in favor of
gram‑negative organisms, which grow in
the oral cavity resulting in the formation
of dental plaque.[6] Plaque mass is
increased with an accumulation of aerobic
and anaerobic microorganisms and its
colonization by Gram‑negative bacteria is
an important factor in the accumulation of
Address for correspondence:
Dr. Ahmadreza Yazdannik,
Critical Care Nursing
Department, Nursing and
Midwifery School, Nursing
and Midwifery Care Research
Center, Isfahan University of
Medical Sciences, Isfahan, Iran.
E-mail: yazdannik@nm.mui.ac.ir
Access this article online
Website: www.ijnmrjournal.net
DOI: 10.4103/ijnmr.IJNMR_164_17
Quick Response Code:
Abstract
Background: Ventilator‑associated pneumonia (VAP) is one of the most common nosocomial
infections that increase mortality rate and the length of hospitalization. Oral care can improve
patient’s oral health, however, the role of oral care in the reduction in incidence
indisputable. The aim of this study was to investigate the effect of oral care
VAP of patients in intensive care unit. Materials and Methods: This clinical trial was conducted
on 80 participants who were randomly assigned to a control group and an inte
2016 to 2017. Data were collected at the first, third, and fifth days of the study
and clinical characteristics questionnaire and the Clinical Pulmonary Infection Score for detecting
pneumonia. Data analysis was performed using descriptive and inferential statistics in SPSS
software. Results: The results of this study showed that the frequency of pneumonia on
fifth days was 15.80% (6) and 23.70% (9) in the control group and 10.50% (4) and
intervention group, respectively. Chi‑square test did not show a significant difference
however, the frequency of pneumonia in the intervention group reduced compared with
group. Conclusions: Accordingto the results of this study, the oral care program could not
significantly decrease the incidence of VAP in critically ill patients compared with rout
practices. Similar studies with a larger sample size and longer duration should be conducted for
better results.
Keywords: Intensive care unit, oral hygiene, ventilator-associated pneumonia
Effect of Oral Care Program on Prevention of Ventilator-associated
Pneumonia in Intensive Care Unit Patients: A Randomized Controlled Trial
Vajihe Atashi1,
Hojatollah Yousefi2,
Hosein
Mahjobipoor3,
Reza Bekhradi4,
Ahmadreza
Yazdannik5
1Student Research Committee,
Faculty of Nursing and
Midwifery, Isfahan University
of Medical Sciences, Isfahan,
Iran, 2Ulcer Repair Research
Center, School of Nursing and
Midwifery, Isfahan University of
Medical Sciences, Isfahan, Iran,
3Anesthesiology and Critical
Care Department, Medicine
School, Critical Care Research
Center, Isfahan University of
Medical Sciences, Isfahan,
Iran, 4Barij Medicinal Plants
Research Center, Kashan,
Iran, 5Critical Care Nursing
Department, Nursing and
Midwifery School, Nursing
and Midwifery Care Research
Center, Isfahan University of
Medical Sciences, Isfahan, Iran
How to cite this article: Atashi V, Yousefi H,
Mahjobipoor H, Bekhradi R, Yazdannik A. Effect
of oral care program on prevention of ventilator-
associated pneumonia in intensive care unit patients:
A randomized controlled trial. Iranian J Nursing
Midwifery Res 2018;23:486-90.
Received: October, 2017. Accepted: April, 2018.
This is an open access journal, and articles are
distributed under the terms of the Creative Commons
Attribution-NonCommercial-ShareAlike 4.0 License, which
allows others to remix, tweak, and build upon the work
non-commercially, as long as appropriate credit is given and the
new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
oral and pharyngeal bacteria.[7,8] The results
of several studies have revealed that bacteria
present in dental plaque are causes of
ventilator‑associated pneumonia (VAP).[5,9]
VAP develops within 48 h of intubation
and mechanical ventilation. VAP is the
second most prevalent nosocomial infection
among patients in ICUs.[10] The prevalence
rate of VAP in patients undergoing
mechanical ventilation is 9%–68%,[11]
and its resulting mortality is reported to
be 30%–70%.[12] It extends hospital and
ICU stay by 6–7 days, raises healthcare
costs by $40,000 per patient, increases
the length of mechanical ventilation, and
increases morbidity, mortality, and patient
suffering.[13‑15] Various studies have shown
that optimum oral care was accompanied
by a reduction in the occurrence of VAP
ICUs.[2,16] For instance, a study showed that
the implementation of an oral care program
in ICUs could significantly decrease
the relative risk of VAP and reduce its
Original Article
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Introduction
One of the common problems of patients
undergoing mechanical ventilation is
poor oral health.[1] Patients in intensive
care units (ICUs) quickly develop oral
problems for various reasons such as
malnutrition, presence of the tracheal tube
and nasogastric tube that is placed in the
mouth of patients for treatment purposes,
reduced fluid intake, and reduced salivation
caused by fever, diarrhea, burns, and drug
usage such as opiates.[2‑4]
In patients in ICUs, dental plaques
are formed more and faster than other
patients.[5] Oral flora changes in the course
of 48 h after hospitalization in favor of
gram‑negative organisms, which grow in
the oral cavity resulting in the formation
of dental plaque.[6] Plaque mass is
increased with an accumulation of aerobic
and anaerobic microorganisms and its
colonization by Gram‑negative bacteria is
an important factor in the accumulation of
Address for correspondence:
Dr. Ahmadreza Yazdannik,
Critical Care Nursing
Department, Nursing and
Midwifery School, Nursing
and Midwifery Care Research
Center, Isfahan University of
Medical Sciences, Isfahan, Iran.
E-mail: yazdannik@nm.mui.ac.ir
Access this article online
Website: www.ijnmrjournal.net
DOI: 10.4103/ijnmr.IJNMR_164_17
Quick Response Code:
Abstract
Background: Ventilator‑associated pneumonia (VAP) is one of the most common nosocomial
infections that increase mortality rate and the length of hospitalization. Oral care can improve
patient’s oral health, however, the role of oral care in the reduction in incidence
indisputable. The aim of this study was to investigate the effect of oral care
VAP of patients in intensive care unit. Materials and Methods: This clinical trial was conducted
on 80 participants who were randomly assigned to a control group and an inte
2016 to 2017. Data were collected at the first, third, and fifth days of the study
and clinical characteristics questionnaire and the Clinical Pulmonary Infection Score for detecting
pneumonia. Data analysis was performed using descriptive and inferential statistics in SPSS
software. Results: The results of this study showed that the frequency of pneumonia on
fifth days was 15.80% (6) and 23.70% (9) in the control group and 10.50% (4) and
intervention group, respectively. Chi‑square test did not show a significant difference
however, the frequency of pneumonia in the intervention group reduced compared with
group. Conclusions: Accordingto the results of this study, the oral care program could not
significantly decrease the incidence of VAP in critically ill patients compared with rout
practices. Similar studies with a larger sample size and longer duration should be conducted for
better results.
Keywords: Intensive care unit, oral hygiene, ventilator-associated pneumonia
Effect of Oral Care Program on Prevention of Ventilator-associated
Pneumonia in Intensive Care Unit Patients: A Randomized Controlled Trial
Vajihe Atashi1,
Hojatollah Yousefi2,
Hosein
Mahjobipoor3,
Reza Bekhradi4,
Ahmadreza
Yazdannik5
1Student Research Committee,
Faculty of Nursing and
Midwifery, Isfahan University
of Medical Sciences, Isfahan,
Iran, 2Ulcer Repair Research
Center, School of Nursing and
Midwifery, Isfahan University of
Medical Sciences, Isfahan, Iran,
3Anesthesiology and Critical
Care Department, Medicine
School, Critical Care Research
Center, Isfahan University of
Medical Sciences, Isfahan,
Iran, 4Barij Medicinal Plants
Research Center, Kashan,
Iran, 5Critical Care Nursing
Department, Nursing and
Midwifery School, Nursing
and Midwifery Care Research
Center, Isfahan University of
Medical Sciences, Isfahan, Iran
How to cite this article: Atashi V, Yousefi H,
Mahjobipoor H, Bekhradi R, Yazdannik A. Effect
of oral care program on prevention of ventilator-
associated pneumonia in intensive care unit patients:
A randomized controlled trial. Iranian J Nursing
Midwifery Res 2018;23:486-90.
Received: October, 2017. Accepted: April, 2018.
This is an open access journal, and articles are
distributed under the terms of the Creative Commons
Attribution-NonCommercial-ShareAlike 4.0 License, which
allows others to remix, tweak, and build upon the work
non-commercially, as long as appropriate credit is given and the
new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
oral and pharyngeal bacteria.[7,8] The results
of several studies have revealed that bacteria
present in dental plaque are causes of
ventilator‑associated pneumonia (VAP).[5,9]
VAP develops within 48 h of intubation
and mechanical ventilation. VAP is the
second most prevalent nosocomial infection
among patients in ICUs.[10] The prevalence
rate of VAP in patients undergoing
mechanical ventilation is 9%–68%,[11]
and its resulting mortality is reported to
be 30%–70%.[12] It extends hospital and
ICU stay by 6–7 days, raises healthcare
costs by $40,000 per patient, increases
the length of mechanical ventilation, and
increases morbidity, mortality, and patient
suffering.[13‑15] Various studies have shown
that optimum oral care was accompanied
by a reduction in the occurrence of VAP
ICUs.[2,16] For instance, a study showed that
the implementation of an oral care program
in ICUs could significantly decrease
the relative risk of VAP and reduce its
Original Article
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Atashi, et al.: Effect of oral care program on prevention of ventilator-associated pneumonia
Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018 487
prevalence from 10.4 to 3.9 cases per 1000 ventilator
days.[17]
Therefore, providing oral care and hygiene should be
considered as a fundamental aspect of nursing care in
ICUs.[3] However, despite the importance of oral care
in patients in ICUs, some studies mainly focus on the
pathophysiology of VAP and discuss the importance of oral
care when examining the physiology of oral cavity.[2] Other
studies have assessed nurses’ performance in oral care
through self‑report questionnaires and investigated nurses’
opinion on the number of oral care sessions through reports
attached to records of patients in ICUs.[18] Some studies
have investigated oral‑care‑related tools such as toothbrush
and mouthwashes.[19] According to a meta‑analysis, the
use of chlorhexidine mouthwash in patients in ICUs
significantly reduced the incidence of VAP.[20] Some studies
show that brushing is an effective way of reducing dental
plaque and VAP.[16] Therefore, studies have recommended
that further researches be conducted on oral care in patients
in ICUs.[21] Therefore, the aim of this study was to evaluate
the effect of an oral care program on the incidence of VAP
in patients in ICUs.
Materials and Methods
This was a parallel randomized clinical trial
(IRCT2017101631200N2) with an intervention group and
a control group. The study population consisted of all
intubated patients hospitalized from November 2016 to
August 2017 in the ICU of hospitals affiliated to Isfahan
University of Medical Sciences, Iran. The participants were
selected using convenience sampling. The inclusion criteria
were an age of 18–65 years, an endotracheal tube in
place through the mouth, ICU hospitalization of less than
24 h, lack of hospitalization in other hospital wards before
ICU admission, lack of history of autoimmune disorders,
pneumonia, or sepsis, lack of pregnancy, lack of known
sensitivity to herbal ingredients, lack of denture, and lack
of evident oral or perioral lesions. Patients were excluded
if they died, were transferred from ICU to other settings,
developed severe oral lesions, or their legal guardian chose
to withdraw from the study.
Using the results of an earlier study[2] and with a type II
error of 0.05 and a power of 0.80, the necessary number
of patients for each study group was calculated to be
35. Considering an attrition rate of 10%, 40 patients
were recruited to each group. Simple randomization
was performed based on a random numbers tables by
an independent person who was unaware of the study.
All randomization numbers were concealed in separate
envelopes that were sealed, opaque, and serially numbered.
However, blinding was not used because of the nature of
intervention.
In the intervention group, oral care was carried out by two
research assistants who had a long work experience in the
ICU. They received necessary training on oral car
from the researcher. The intervention started from the
first day of admission to the ICU an
5 consecutive days. It should be noted tha
planned based on previous studies and arrangedas fol
adjusting the pressure of the cuff of th
between 20 and 25 mmHg using a special m
Elevating the head of the bed from 30
and throat suctioning; brushing all internal an
surfaces of the teeth, gums, and tongue for 2
a baby toothbrush and antimicrobial chlorhexid
moisturizing all surfaces of the oral mucosa, gu
tongue of the patient using swabs and moisturizin
containing aloe vera and peppermint essential
a thin layer of petroleum jelly to th
cleaning any airway obstruction; and reinserting the
the patient’s mouth.[2,3,21‑23]
In the intervention group, the patient’s or
scored using Beck Oral Assessment Scale, and ba
score, the frequency of care was determined
and 4 h for patients with no, mild, m
disorders, respectively.[22] In the control group, rou
was provided which included elevation of
bed from 30° to 45° and use of sw
0.2% solution every 12 h by nurses. The da
instruments included a demographic questionnaire
and Clinical Pulmonary Infection Score (CPIS). The
demographic questionnaire included age, gender,
underlying diseases,reasons for hospitalization, drugs use
and history of smoking, which were measured
day of the study.
The CPIS is used to detect VAP. It consists of six
components of temperature, volume of respiratory
secretions, changes in white blood cell count, pr
infiltration in chest radiograph, hypoxemia, an
culture results. The overall score of this scale ranges
between 0 and 10. Scores of 6 and hi
presenceof VAP.[17] The validity and reliability o
have been approved in various studies.[2,6] This scale wa
completed and its score was recordedby an
on the first, third, and fifth days of the
Data analysis was performed using SPSS (version 16
Inc., Chicago, IL, USA). Fisher’s exact test, C
and t‑test were used for demographic variables.
test was used to examine the differences
groups in terms of qualitative variables. t‑T
examine the two groups in terms of quantitativ
Mann–Whitney U test was used for comparison
between control and intervention groups. The level of
statistical significance was set at p < 0.05.
Ethical considerations
This study was approved by the Institutiona
and the Ethics Committee of Isfahan University
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018 487
prevalence from 10.4 to 3.9 cases per 1000 ventilator
days.[17]
Therefore, providing oral care and hygiene should be
considered as a fundamental aspect of nursing care in
ICUs.[3] However, despite the importance of oral care
in patients in ICUs, some studies mainly focus on the
pathophysiology of VAP and discuss the importance of oral
care when examining the physiology of oral cavity.[2] Other
studies have assessed nurses’ performance in oral care
through self‑report questionnaires and investigated nurses’
opinion on the number of oral care sessions through reports
attached to records of patients in ICUs.[18] Some studies
have investigated oral‑care‑related tools such as toothbrush
and mouthwashes.[19] According to a meta‑analysis, the
use of chlorhexidine mouthwash in patients in ICUs
significantly reduced the incidence of VAP.[20] Some studies
show that brushing is an effective way of reducing dental
plaque and VAP.[16] Therefore, studies have recommended
that further researches be conducted on oral care in patients
in ICUs.[21] Therefore, the aim of this study was to evaluate
the effect of an oral care program on the incidence of VAP
in patients in ICUs.
Materials and Methods
This was a parallel randomized clinical trial
(IRCT2017101631200N2) with an intervention group and
a control group. The study population consisted of all
intubated patients hospitalized from November 2016 to
August 2017 in the ICU of hospitals affiliated to Isfahan
University of Medical Sciences, Iran. The participants were
selected using convenience sampling. The inclusion criteria
were an age of 18–65 years, an endotracheal tube in
place through the mouth, ICU hospitalization of less than
24 h, lack of hospitalization in other hospital wards before
ICU admission, lack of history of autoimmune disorders,
pneumonia, or sepsis, lack of pregnancy, lack of known
sensitivity to herbal ingredients, lack of denture, and lack
of evident oral or perioral lesions. Patients were excluded
if they died, were transferred from ICU to other settings,
developed severe oral lesions, or their legal guardian chose
to withdraw from the study.
Using the results of an earlier study[2] and with a type II
error of 0.05 and a power of 0.80, the necessary number
of patients for each study group was calculated to be
35. Considering an attrition rate of 10%, 40 patients
were recruited to each group. Simple randomization
was performed based on a random numbers tables by
an independent person who was unaware of the study.
All randomization numbers were concealed in separate
envelopes that were sealed, opaque, and serially numbered.
However, blinding was not used because of the nature of
intervention.
In the intervention group, oral care was carried out by two
research assistants who had a long work experience in the
ICU. They received necessary training on oral car
from the researcher. The intervention started from the
first day of admission to the ICU an
5 consecutive days. It should be noted tha
planned based on previous studies and arrangedas fol
adjusting the pressure of the cuff of th
between 20 and 25 mmHg using a special m
Elevating the head of the bed from 30
and throat suctioning; brushing all internal an
surfaces of the teeth, gums, and tongue for 2
a baby toothbrush and antimicrobial chlorhexid
moisturizing all surfaces of the oral mucosa, gu
tongue of the patient using swabs and moisturizin
containing aloe vera and peppermint essential
a thin layer of petroleum jelly to th
cleaning any airway obstruction; and reinserting the
the patient’s mouth.[2,3,21‑23]
In the intervention group, the patient’s or
scored using Beck Oral Assessment Scale, and ba
score, the frequency of care was determined
and 4 h for patients with no, mild, m
disorders, respectively.[22] In the control group, rou
was provided which included elevation of
bed from 30° to 45° and use of sw
0.2% solution every 12 h by nurses. The da
instruments included a demographic questionnaire
and Clinical Pulmonary Infection Score (CPIS). The
demographic questionnaire included age, gender,
underlying diseases,reasons for hospitalization, drugs use
and history of smoking, which were measured
day of the study.
The CPIS is used to detect VAP. It consists of six
components of temperature, volume of respiratory
secretions, changes in white blood cell count, pr
infiltration in chest radiograph, hypoxemia, an
culture results. The overall score of this scale ranges
between 0 and 10. Scores of 6 and hi
presenceof VAP.[17] The validity and reliability o
have been approved in various studies.[2,6] This scale wa
completed and its score was recordedby an
on the first, third, and fifth days of the
Data analysis was performed using SPSS (version 16
Inc., Chicago, IL, USA). Fisher’s exact test, C
and t‑test were used for demographic variables.
test was used to examine the differences
groups in terms of qualitative variables. t‑T
examine the two groups in terms of quantitativ
Mann–Whitney U test was used for comparison
between control and intervention groups. The level of
statistical significance was set at p < 0.05.
Ethical considerations
This study was approved by the Institutiona
and the Ethics Committee of Isfahan University
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Atashi, et al.: Effect of oral care program on prevention of ventilator-associated pneumonia
488 Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018
Sciences (code IR.MUI.REC.1395.3.361). The study aim
was explained to patients’ legal guardians and they were
ensured that the data would be handled confidentially,
participation in the study would be voluntarily, and they
could withdraw from the study at any stage. All participants
signed an informed consent form.
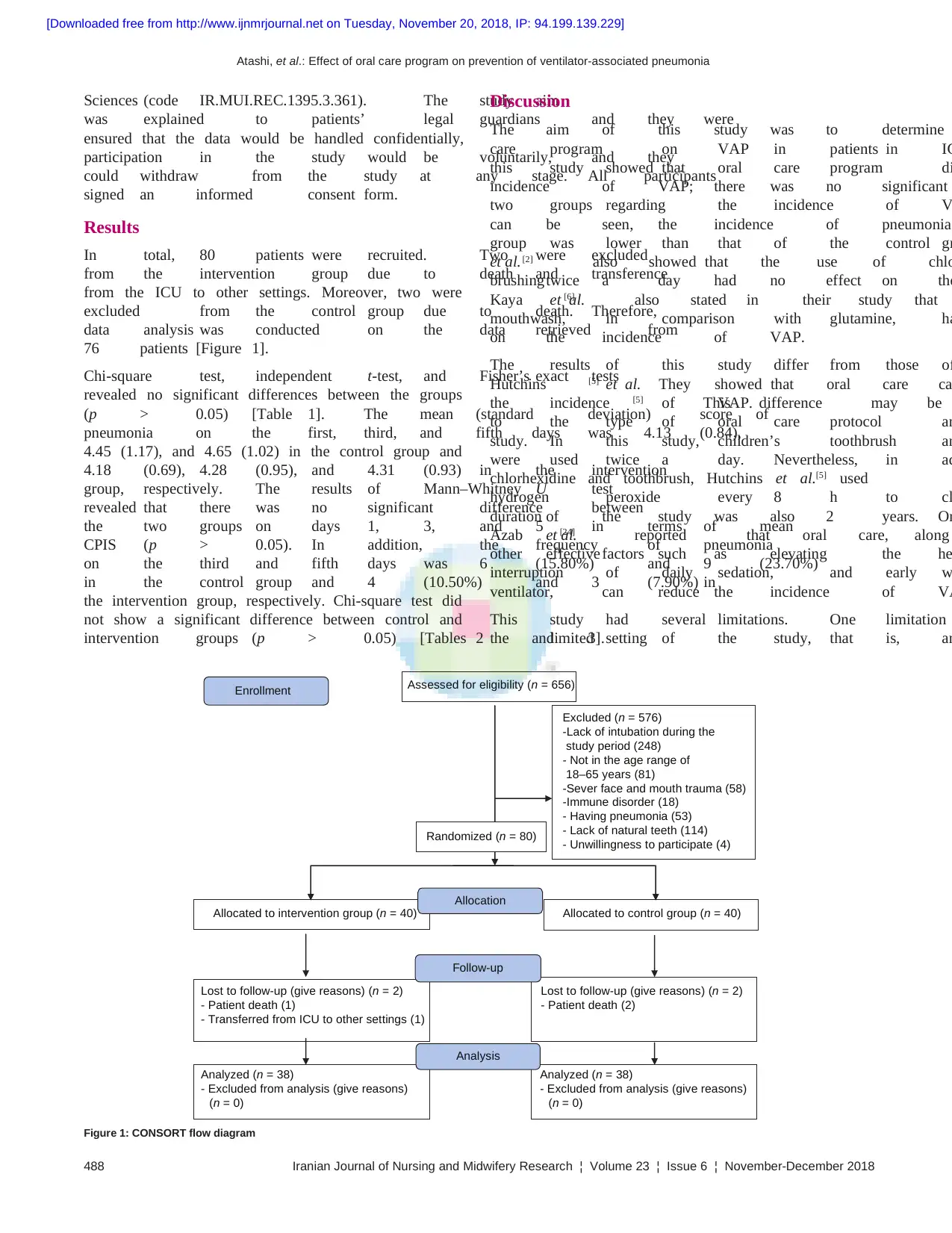
Results
In total, 80 patients were recruited. Two were excluded
from the intervention group due to death and transference
from the ICU to other settings. Moreover, two were
excluded from the control group due to death. Therefore,
data analysis was conducted on the data retrieved from
76 patients [Figure 1].
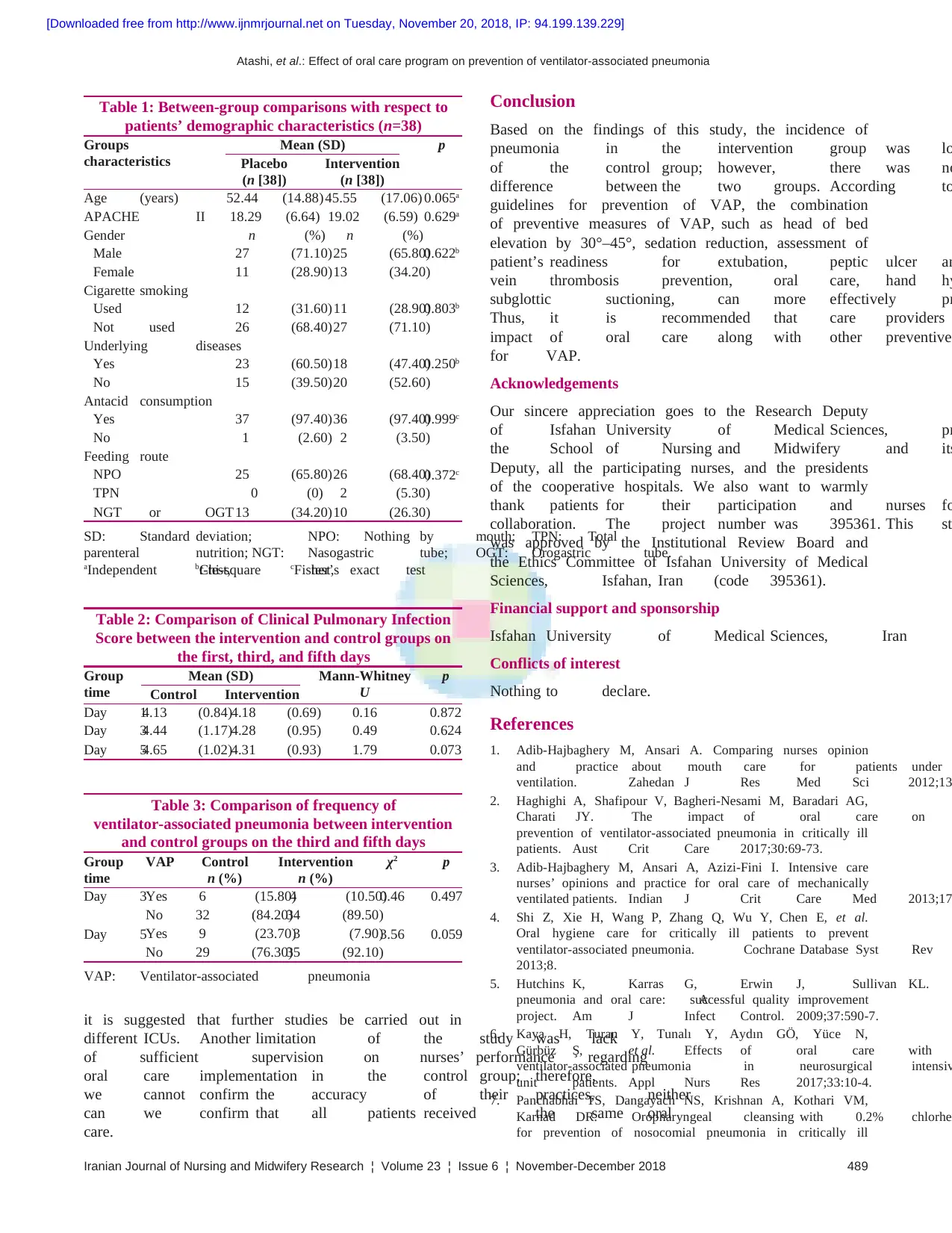
Chi‑square test, independent t‑test, and Fisher’s exact tests
revealed no significant differences between the groups
(p > 0.05) [Table 1]. The mean (standard deviation) score of
pneumonia on the first, third, and fifth days was 4.13 (0.84),
4.45 (1.17), and 4.65 (1.02) in the control group and
4.18 (0.69), 4.28 (0.95), and 4.31 (0.93) in the intervention
group, respectively. The results of Mann–Whitney U test
revealed that there was no significant difference between
the two groups on days 1, 3, and 5 in terms of mean
CPIS (p > 0.05). In addition, the frequency of pneumonia
on the third and fifth days was 6 (15.80%) and 9 (23.70%)
in the control group and 4 (10.50%) and 3 (7.90%) in
the intervention group, respectively. Chi‑square test did
not show a significant difference between control and
intervention groups (p > 0.05) [Tables 2 and 3].
Discussion
The aim of this study was to determine
care program on VAP in patients in IC
this study showed that oral care program di
incidence of VAP; there was no significant
two groups regarding the incidence of V
can be seen, the incidence of pneumonia
group was lower than that of the control gr
et al.[2] also showed that the use of chlo
brushingtwice a day had no effect on the
Kaya et al.[6] also stated in their study that
mouthwash, in comparison with glutamine, ha
on the incidence of VAP.
The results of this study differ from those of
Hutchins et al.[5] They showed that oral care ca
the incidence of VAP.[5] This difference may be
to the type of oral care protocol an
study. In this study, children’s toothbrush an
were used twice a day. Nevertheless, in ad
chlorhexidine and toothbrush, Hutchins et al.[5] used
hydrogen peroxide every 8 h to cl
duration of the study was also 2 years. On
Azab et al.[24] reported that oral care, along
other effectivefactors such as elevating the he
interruption of daily sedation, and early w
ventilator, can reduce the incidence of VA
This study had several limitations. One limitation
the limited setting of the study, that is, an
Assessed for eligibility (n = 656)
Excluded (n = 576)
-Lack of intubation during the
study period (248)
- Not in the age range of
18–65 years (81)
-Sever face and mouth trauma (58)
-Immune disorder (18)
- Having pneumonia (53)
- Lack of natural teeth (114)
- Unwillingness to participate (4)
Randomized (n = 80)
Enrollment
Allocation
Follow-up
Analysis
Allocated to intervention group (n = 40) Allocated to control group (n = 40)
Lost to follow-up (give reasons) (n = 2)
- Patient death (1)
- Transferred from ICU to other settings (1)
Lost to follow-up (give reasons) (n = 2)
- Patient death (2)
Analyzed (n = 38)
- Excluded from analysis (give reasons)
(n = 0)
Analyzed (n = 38)
- Excluded from analysis (give reasons)
(n = 0)
Figure 1: CONSORT flow diagram
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
488 Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018
Sciences (code IR.MUI.REC.1395.3.361). The study aim
was explained to patients’ legal guardians and they were
ensured that the data would be handled confidentially,
participation in the study would be voluntarily, and they
could withdraw from the study at any stage. All participants
signed an informed consent form.
Results
In total, 80 patients were recruited. Two were excluded
from the intervention group due to death and transference
from the ICU to other settings. Moreover, two were
excluded from the control group due to death. Therefore,
data analysis was conducted on the data retrieved from
76 patients [Figure 1].
Chi‑square test, independent t‑test, and Fisher’s exact tests
revealed no significant differences between the groups
(p > 0.05) [Table 1]. The mean (standard deviation) score of
pneumonia on the first, third, and fifth days was 4.13 (0.84),
4.45 (1.17), and 4.65 (1.02) in the control group and
4.18 (0.69), 4.28 (0.95), and 4.31 (0.93) in the intervention
group, respectively. The results of Mann–Whitney U test
revealed that there was no significant difference between
the two groups on days 1, 3, and 5 in terms of mean
CPIS (p > 0.05). In addition, the frequency of pneumonia
on the third and fifth days was 6 (15.80%) and 9 (23.70%)
in the control group and 4 (10.50%) and 3 (7.90%) in
the intervention group, respectively. Chi‑square test did
not show a significant difference between control and
intervention groups (p > 0.05) [Tables 2 and 3].
Discussion
The aim of this study was to determine
care program on VAP in patients in IC
this study showed that oral care program di
incidence of VAP; there was no significant
two groups regarding the incidence of V
can be seen, the incidence of pneumonia
group was lower than that of the control gr
et al.[2] also showed that the use of chlo
brushingtwice a day had no effect on the
Kaya et al.[6] also stated in their study that
mouthwash, in comparison with glutamine, ha
on the incidence of VAP.
The results of this study differ from those of
Hutchins et al.[5] They showed that oral care ca
the incidence of VAP.[5] This difference may be
to the type of oral care protocol an
study. In this study, children’s toothbrush an
were used twice a day. Nevertheless, in ad
chlorhexidine and toothbrush, Hutchins et al.[5] used
hydrogen peroxide every 8 h to cl
duration of the study was also 2 years. On
Azab et al.[24] reported that oral care, along
other effectivefactors such as elevating the he
interruption of daily sedation, and early w
ventilator, can reduce the incidence of VA
This study had several limitations. One limitation
the limited setting of the study, that is, an
Assessed for eligibility (n = 656)
Excluded (n = 576)
-Lack of intubation during the
study period (248)
- Not in the age range of
18–65 years (81)
-Sever face and mouth trauma (58)
-Immune disorder (18)
- Having pneumonia (53)
- Lack of natural teeth (114)
- Unwillingness to participate (4)
Randomized (n = 80)
Enrollment
Allocation
Follow-up
Analysis
Allocated to intervention group (n = 40) Allocated to control group (n = 40)
Lost to follow-up (give reasons) (n = 2)
- Patient death (1)
- Transferred from ICU to other settings (1)
Lost to follow-up (give reasons) (n = 2)
- Patient death (2)
Analyzed (n = 38)
- Excluded from analysis (give reasons)
(n = 0)
Analyzed (n = 38)
- Excluded from analysis (give reasons)
(n = 0)
Figure 1: CONSORT flow diagram
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Atashi, et al.: Effect of oral care program on prevention of ventilator-associated pneumonia
Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018 489
Conclusion
Based on the findings of this study, the incidence of
pneumonia in the intervention group was lo
of the control group; however, there was no
difference between the two groups. According to
guidelines for prevention of VAP, the combination
of preventive measures of VAP, such as head of bed
elevation by 30°–45°, sedation reduction, assessment of
patient’s readiness for extubation, peptic ulcer an
vein thrombosis prevention, oral care, hand hy
subglottic suctioning, can more effectively pr
Thus, it is recommended that care providers
impact of oral care along with other preventive
for VAP.
Acknowledgements
Our sincere appreciation goes to the Research Deputy
of Isfahan University of Medical Sciences, pr
the School of Nursing and Midwifery and its
Deputy, all the participating nurses, and the presidents
of the cooperative hospitals. We also want to warmly
thank patients for their participation and nurses fo
collaboration. The project number was 395361. This st
was approved by the Institutional Review Board and
the Ethics Committee of Isfahan University of Medical
Sciences, Isfahan, Iran (code 395361).
Financial support and sponsorship
Isfahan University of Medical Sciences, Iran
Conflicts of interest
Nothing to declare.
References
1. Adib‑Hajbaghery M, Ansari A. Comparing nurses opinion
and practice about mouth care for patients under
ventilation. Zahedan J Res Med Sci 2012;13
2. Haghighi A, Shafipour V, Bagheri‑Nesami M, Baradari AG,
Charati JY. The impact of oral care on
prevention of ventilator‑associated pneumonia in critically ill
patients. Aust Crit Care 2017;30:69‑73.
3. Adib‑Hajbaghery M, Ansari A, Azizi‑Fini I. Intensive care
nurses’ opinions and practice for oral care of mechanically
ventilated patients. Indian J Crit Care Med 2013;17
4. Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, et al.
Oral hygiene care for critically ill patients to prevent
ventilator‑associated pneumonia. Cochrane Database Syst Rev
2013;8.
5. Hutchins K, Karras G, Erwin J, Sullivan KL.
pneumonia and oral care: Asuccessful quality improvement
project. Am J Infect Control. 2009;37:590‑7.
6. Kaya H, Turan Y, Tunalı Y, Aydın GÖ, Yüce N,
Gürbüz Ş, et al. Effects of oral care with
ventilator‑associated pneumonia in neurosurgical intensiv
unit patients. Appl Nurs Res 2017;33:10‑4.
7. Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM,
Karnad DR. Oropharyngeal cleansing with 0.2% chlorhe
for prevention of nosocomial pneumonia in critically ill
Table 1: Between‑group comparisons with respect to
patients’ demographic characteristics (n=38)
Groups
characteristics
Mean (SD) p
Placebo
(n [38])
Intervention
(n [38])
Age (years) 52.44 (14.88)45.55 (17.06) 0.065a
APACHE II 18.29 (6.64) 19.02 (6.59) 0.629a
Gender n (%) n (%)
Male 27 (71.10)25 (65.80)0.622b
Female 11 (28.90)13 (34.20)
Cigarette smoking
Used 12 (31.60)11 (28.90)0.803b
Not used 26 (68.40)27 (71.10)
Underlying diseases
Yes 23 (60.50)18 (47.40)0.250b
No 15 (39.50)20 (52.60)
Antacid consumption
Yes 37 (97.40)36 (97.40)0.999c
No 1 (2.60) 2 (3.50)
Feeding route
NPO 25 (65.80)26 (68.40)0.372c
TPN 0 (0) 2 (5.30)
NGT or OGT13 (34.20)10 (26.30)
SD: Standard deviation; NPO: Nothing by mouth; TPN: Total
parenteral nutrition; NGT: Nasogastric tube; OGT: Orogastric tube.
aIndependent t‑test,bChi‑square test,cFisher’s exact test
Table 2: Comparison of Clinical Pulmonary Infection
Score between the intervention and control groups on
the first, third, and fifth days
Group
time
Mean (SD) Mann‑Whitney
U
p
Control Intervention
Day 14.13 (0.84)4.18 (0.69) 0.16 0.872
Day 34.44 (1.17)4.28 (0.95) 0.49 0.624
Day 54.65 (1.02)4.31 (0.93) 1.79 0.073
Table 3: Comparison of frequency of
ventilator‑associated pneumonia between intervention
and control groups on the third and fifth days
Group
time
VAP Control
n (%)
Intervention
n (%)
χ2 p
Day 3Yes 6 (15.80)4 (10.50)0.46 0.497
No 32 (84.20)34 (89.50)
Day 5Yes 9 (23.70)3 (7.90)3.56 0.059
No 29 (76.30)35 (92.10)
VAP: Ventilator‑associated pneumonia
it is suggested that further studies be carried out in
different ICUs. Another limitation of the study was lack
of sufficient supervision on nurses’ performance regarding
oral care implementation in the control group; therefore,
we cannot confirm the accuracy of their practices, neither
can we confirm that all patients received the same oral
care.
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018 489
Conclusion
Based on the findings of this study, the incidence of
pneumonia in the intervention group was lo
of the control group; however, there was no
difference between the two groups. According to
guidelines for prevention of VAP, the combination
of preventive measures of VAP, such as head of bed
elevation by 30°–45°, sedation reduction, assessment of
patient’s readiness for extubation, peptic ulcer an
vein thrombosis prevention, oral care, hand hy
subglottic suctioning, can more effectively pr
Thus, it is recommended that care providers
impact of oral care along with other preventive
for VAP.
Acknowledgements
Our sincere appreciation goes to the Research Deputy
of Isfahan University of Medical Sciences, pr
the School of Nursing and Midwifery and its
Deputy, all the participating nurses, and the presidents
of the cooperative hospitals. We also want to warmly
thank patients for their participation and nurses fo
collaboration. The project number was 395361. This st
was approved by the Institutional Review Board and
the Ethics Committee of Isfahan University of Medical
Sciences, Isfahan, Iran (code 395361).
Financial support and sponsorship
Isfahan University of Medical Sciences, Iran
Conflicts of interest
Nothing to declare.
References
1. Adib‑Hajbaghery M, Ansari A. Comparing nurses opinion
and practice about mouth care for patients under
ventilation. Zahedan J Res Med Sci 2012;13
2. Haghighi A, Shafipour V, Bagheri‑Nesami M, Baradari AG,
Charati JY. The impact of oral care on
prevention of ventilator‑associated pneumonia in critically ill
patients. Aust Crit Care 2017;30:69‑73.
3. Adib‑Hajbaghery M, Ansari A, Azizi‑Fini I. Intensive care
nurses’ opinions and practice for oral care of mechanically
ventilated patients. Indian J Crit Care Med 2013;17
4. Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, et al.
Oral hygiene care for critically ill patients to prevent
ventilator‑associated pneumonia. Cochrane Database Syst Rev
2013;8.
5. Hutchins K, Karras G, Erwin J, Sullivan KL.
pneumonia and oral care: Asuccessful quality improvement
project. Am J Infect Control. 2009;37:590‑7.
6. Kaya H, Turan Y, Tunalı Y, Aydın GÖ, Yüce N,
Gürbüz Ş, et al. Effects of oral care with
ventilator‑associated pneumonia in neurosurgical intensiv
unit patients. Appl Nurs Res 2017;33:10‑4.
7. Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM,
Karnad DR. Oropharyngeal cleansing with 0.2% chlorhe
for prevention of nosocomial pneumonia in critically ill
Table 1: Between‑group comparisons with respect to
patients’ demographic characteristics (n=38)
Groups
characteristics
Mean (SD) p
Placebo
(n [38])
Intervention
(n [38])
Age (years) 52.44 (14.88)45.55 (17.06) 0.065a
APACHE II 18.29 (6.64) 19.02 (6.59) 0.629a
Gender n (%) n (%)
Male 27 (71.10)25 (65.80)0.622b
Female 11 (28.90)13 (34.20)
Cigarette smoking
Used 12 (31.60)11 (28.90)0.803b
Not used 26 (68.40)27 (71.10)
Underlying diseases
Yes 23 (60.50)18 (47.40)0.250b
No 15 (39.50)20 (52.60)
Antacid consumption
Yes 37 (97.40)36 (97.40)0.999c
No 1 (2.60) 2 (3.50)
Feeding route
NPO 25 (65.80)26 (68.40)0.372c
TPN 0 (0) 2 (5.30)
NGT or OGT13 (34.20)10 (26.30)
SD: Standard deviation; NPO: Nothing by mouth; TPN: Total
parenteral nutrition; NGT: Nasogastric tube; OGT: Orogastric tube.
aIndependent t‑test,bChi‑square test,cFisher’s exact test
Table 2: Comparison of Clinical Pulmonary Infection
Score between the intervention and control groups on
the first, third, and fifth days
Group
time
Mean (SD) Mann‑Whitney
U
p
Control Intervention
Day 14.13 (0.84)4.18 (0.69) 0.16 0.872
Day 34.44 (1.17)4.28 (0.95) 0.49 0.624
Day 54.65 (1.02)4.31 (0.93) 1.79 0.073
Table 3: Comparison of frequency of
ventilator‑associated pneumonia between intervention
and control groups on the third and fifth days
Group
time
VAP Control
n (%)
Intervention
n (%)
χ2 p
Day 3Yes 6 (15.80)4 (10.50)0.46 0.497
No 32 (84.20)34 (89.50)
Day 5Yes 9 (23.70)3 (7.90)3.56 0.059
No 29 (76.30)35 (92.10)
VAP: Ventilator‑associated pneumonia
it is suggested that further studies be carried out in
different ICUs. Another limitation of the study was lack
of sufficient supervision on nurses’ performance regarding
oral care implementation in the control group; therefore,
we cannot confirm the accuracy of their practices, neither
can we confirm that all patients received the same oral
care.
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
Atashi, et al.: Effect of oral care program on prevention of ventilator-associated pneumonia
490 Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018
patients: An open‑label randomized trial with 0.01% potassium
permanganate as control. Chest J 2009;135:1150‑6.
8. Pedreira ML, Kusahara DM, de Carvalho WB, Núñez SC,
Peterlini MAS. Oral care interventions and oropharyngeal
colonization in children receiving mechanical ventilation. Am J
Crit Care 2009;18:319‑28.
9. Hillier B, Wilson C, Chamberlain D, King L. Preventing
ventilator‑associated pneumonia through oral care, product
selection, and application method: A literature review. AACN
Adv Crit Care 2013;24:38‑58.
10. Liao YM, Tsai JR, Chou FH. The effectiveness of an oral health
care program for preventing ventilator‑associated pneumonia.
Nurs Crit Care 2015;20:89‑97.
11. Gatell J, Rosa M, Santé Roig M, Hernández Vian Ó,
Carrillo Santín E, Turégano Duaso C, et al. Assessment of a
training programme for the prevention of ventilator‑associated
pneumonia. Nurs Crit Care 2012;17:285‑92.
12. Micik S, Besic N, Johnson N, Han M, Hamlyn S, Ball H.
Reducing risk for ventilator associated pneumonia through
nursing sensitive interventions. Intensive Crit Care Nurs
2013;29:261‑5.
13. Gallagher JA. Implementation of ventilator‑associatedpneumonia
clinical guideline (Bundle). J Nurs Pract 2012;8:377‑82.
14. Craven DE, Lei Y, Ruthazer R, Sarwar A, Hudcova J. Incidence
and outcomes of ventilator‑associated tracheobronchitis and
pneumonia. Am J Med 2013;126:542‑9.
15. Rello J, Chastre J, Cornaglia G, Masterton R. A European care
bundle for management of ventilator‑associated pneumonia.
J Crit Care 2011;26:3‑10.
16. Kiyoshi‑Teo H, Blegen M. Influence of institutional guidelines
on oral hygiene practices in intensive care units.
2015;24:309‑18.
17. Fields LB. Oral care intervention to reduce incidence of
ventilator‑associated pneumonia in the neurologic
unit. J Neurosc Nurs 2008;40:291‑8.
18. Feider LL, Mitchell P, Bridges E. Oral care
intubated critically ill adults. Am J Crit Care
19. Munro CL, Grap MJ, Jones DJ, McClish DK,
Sessler CN. Chlorhexidine, toothbrushing, and preventing
ventilator‑associated pneumonia in critically ill adults.
Care 2009;18:428‑37.
20. Longti Li ZA, Li L, Zheng X, Jie
antiseptics prevent ventilator‑associated pneumonia
receiving mechanical ventilation? An update meta‑an
17 randomized controlled trials. Int J Clin
21. Jang CS, Shin YS. Effects of combination
health, dry mouth and salivary pH of intubated patients:
A randomized controlled trial. Int J Nurs
22. Ames NJ, Sulima P, Yates JM, McCullagh L, Gollins SL,
Soeken K, et al. Effects of systematic oral
patients: A multicenter study. Am J Crit
23. Prendergast V, Jakobsson U, Renvert S,
of a standard versus comprehensive oral care
intubated neuroscience ICU patients: Results of a
controlled trial. J Neurosci Nurs 2012;44:134‑46.
24. El Azab SR, El Sayed AE, Abdelkarim
Saqabi A, El Demerdash S. Combination of ventilator care
bundle and regular oral care with chlorhexidine
with reduction in ventilator associated pneumonia. Egypt J
Anaesth 2013;29:273‑7.
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
View publication statsView publication stats
490 Iranian Journal of Nursing and Midwifery Research ¦ Volume 23 ¦ Issue 6 ¦ November-December 2018
patients: An open‑label randomized trial with 0.01% potassium
permanganate as control. Chest J 2009;135:1150‑6.
8. Pedreira ML, Kusahara DM, de Carvalho WB, Núñez SC,
Peterlini MAS. Oral care interventions and oropharyngeal
colonization in children receiving mechanical ventilation. Am J
Crit Care 2009;18:319‑28.
9. Hillier B, Wilson C, Chamberlain D, King L. Preventing
ventilator‑associated pneumonia through oral care, product
selection, and application method: A literature review. AACN
Adv Crit Care 2013;24:38‑58.
10. Liao YM, Tsai JR, Chou FH. The effectiveness of an oral health
care program for preventing ventilator‑associated pneumonia.
Nurs Crit Care 2015;20:89‑97.
11. Gatell J, Rosa M, Santé Roig M, Hernández Vian Ó,
Carrillo Santín E, Turégano Duaso C, et al. Assessment of a
training programme for the prevention of ventilator‑associated
pneumonia. Nurs Crit Care 2012;17:285‑92.
12. Micik S, Besic N, Johnson N, Han M, Hamlyn S, Ball H.
Reducing risk for ventilator associated pneumonia through
nursing sensitive interventions. Intensive Crit Care Nurs
2013;29:261‑5.
13. Gallagher JA. Implementation of ventilator‑associatedpneumonia
clinical guideline (Bundle). J Nurs Pract 2012;8:377‑82.
14. Craven DE, Lei Y, Ruthazer R, Sarwar A, Hudcova J. Incidence
and outcomes of ventilator‑associated tracheobronchitis and
pneumonia. Am J Med 2013;126:542‑9.
15. Rello J, Chastre J, Cornaglia G, Masterton R. A European care
bundle for management of ventilator‑associated pneumonia.
J Crit Care 2011;26:3‑10.
16. Kiyoshi‑Teo H, Blegen M. Influence of institutional guidelines
on oral hygiene practices in intensive care units.
2015;24:309‑18.
17. Fields LB. Oral care intervention to reduce incidence of
ventilator‑associated pneumonia in the neurologic
unit. J Neurosc Nurs 2008;40:291‑8.
18. Feider LL, Mitchell P, Bridges E. Oral care
intubated critically ill adults. Am J Crit Care
19. Munro CL, Grap MJ, Jones DJ, McClish DK,
Sessler CN. Chlorhexidine, toothbrushing, and preventing
ventilator‑associated pneumonia in critically ill adults.
Care 2009;18:428‑37.
20. Longti Li ZA, Li L, Zheng X, Jie
antiseptics prevent ventilator‑associated pneumonia
receiving mechanical ventilation? An update meta‑an
17 randomized controlled trials. Int J Clin
21. Jang CS, Shin YS. Effects of combination
health, dry mouth and salivary pH of intubated patients:
A randomized controlled trial. Int J Nurs
22. Ames NJ, Sulima P, Yates JM, McCullagh L, Gollins SL,
Soeken K, et al. Effects of systematic oral
patients: A multicenter study. Am J Crit
23. Prendergast V, Jakobsson U, Renvert S,
of a standard versus comprehensive oral care
intubated neuroscience ICU patients: Results of a
controlled trial. J Neurosci Nurs 2012;44:134‑46.
24. El Azab SR, El Sayed AE, Abdelkarim
Saqabi A, El Demerdash S. Combination of ventilator care
bundle and regular oral care with chlorhexidine
with reduction in ventilator associated pneumonia. Egypt J
Anaesth 2013;29:273‑7.
[Downloaded free from http://www.ijnmrjournal.net on Tuesday, November 20, 2018, IP: 94.199.139.229]
View publication statsView publication stats
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





