Analysing Oral Health Disparities in Indigenous Australians
VerifiedAdded on 2022/09/17
|12
|2728
|24
Essay
AI Summary
This essay provides an overview of oral health problems and their development within the Aboriginal community of Australia, comparing this community to non-Aboriginal Torres and Strait Islander Australians to analyze the burden of oral health issues. It explores how colonization has contributed to these issues, examines various social determinants affecting oral health, and identifies barriers faced by medical practitioners in addressing these concerns. The essay highlights the prevalence of oral diseases in Aboriginal communities, linking it to factors such as lack of access to oral health services, poor sanitation, and lifestyle differences. Furthermore, it discusses the impact of social and economic disparities, structural changes, and the challenges faced by Aboriginal Community Controlled Health Services (ACCHS) in providing adequate oral healthcare due to financial constraints and workforce shortages. The conclusion emphasizes the importance of oral wellbeing and the need to address the disparities in oral healthcare access for Indigenous Australians.
Running Head: NURSING
0
ORAL HEALTH
Essay
Student
8/28/2019
0
ORAL HEALTH
Essay
Student
8/28/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
1
Oral health denotes the overall wellbeing of an individual. For oral hygiene, dental care is
essential. However, lack of oral care can result in dental cavities and gums related infections.
Heart diseases, oral cancer, and diabetes are some terminal illnesses, which can occur due to lack
of oral care (Kisley, 2016, p. 277). The prevalence of this infection can be observed in the
Aboriginal community of Australia. Through the essay, brief information about the oral health
problem and its development in the Aboriginal community will be provided. Moreover, the
comparison of this community will be conducted to Non-Aboriginal Torres and Strait Islander
Australia to identify and analyse the burden of this issue, how colonization has played role in the
development of the issue, various social determinants and what is a kind of barriers observed by
medical practitioners in dealing with the issue.
According to the definition provided by World Health Organization, “oral health is a
condition where the individual is free from the chronic illness of mouth or any kind of dental
infection which restrain the ability to bite, smile, speak and other psychological capabilities.
However, when the individuals do not maintain oral health, it develops into an infection.
Oral infection or dental illness is a prolonged non-transferable disorder, which causes
unbearable pain into the mouth, affects the facial movements as well and even causes death. In
2016 Global Burden of the study was conducted in which it was identified that the oral infection
has been widespread and affected about 50% of the world’s population (3.58 billion people) in
which it was observed that dental cavities are the most prevalent condition in the society (World
Health Organization , 2018). One of the major reasons for its development is the lack of oral
sanitation and usage of Fluoride mineral, which is present in toothpaste and mouth-rinses to
protect, teethes from decay. In addition to this, it prevents oral infection. As per the research
conducted by WHO in 2016, about 2.4 billion people suffered from cavities. Besides this, about
1
Oral health denotes the overall wellbeing of an individual. For oral hygiene, dental care is
essential. However, lack of oral care can result in dental cavities and gums related infections.
Heart diseases, oral cancer, and diabetes are some terminal illnesses, which can occur due to lack
of oral care (Kisley, 2016, p. 277). The prevalence of this infection can be observed in the
Aboriginal community of Australia. Through the essay, brief information about the oral health
problem and its development in the Aboriginal community will be provided. Moreover, the
comparison of this community will be conducted to Non-Aboriginal Torres and Strait Islander
Australia to identify and analyse the burden of this issue, how colonization has played role in the
development of the issue, various social determinants and what is a kind of barriers observed by
medical practitioners in dealing with the issue.
According to the definition provided by World Health Organization, “oral health is a
condition where the individual is free from the chronic illness of mouth or any kind of dental
infection which restrain the ability to bite, smile, speak and other psychological capabilities.
However, when the individuals do not maintain oral health, it develops into an infection.
Oral infection or dental illness is a prolonged non-transferable disorder, which causes
unbearable pain into the mouth, affects the facial movements as well and even causes death. In
2016 Global Burden of the study was conducted in which it was identified that the oral infection
has been widespread and affected about 50% of the world’s population (3.58 billion people) in
which it was observed that dental cavities are the most prevalent condition in the society (World
Health Organization , 2018). One of the major reasons for its development is the lack of oral
sanitation and usage of Fluoride mineral, which is present in toothpaste and mouth-rinses to
protect, teethes from decay. In addition to this, it prevents oral infection. As per the research
conducted by WHO in 2016, about 2.4 billion people suffered from cavities. Besides this, about
NURSING
2
486 million children were infected from the decay of deciduous teeth (Health People
Government , 2019). As per the statistics presented by Global Oral Health Data Bank in 2018,
the presence of dental carries differs from 49% to 83% in different countries. The major impacts
of dental issues can be observed in under-developed countries, wherewith the emergence of
urbanization, transformation living conditions and inadequate quality of health service has
increased the prevalence of oral disorders. Besides this oral issues can be occurred due to the
excessive consumption of tobacco, liquor and lack of nutrition. Ulcers, bleeding gums, plaque
which gets deposit on the teeth, bad smell, tooth sensitivity are symptoms upon which immediate
action must be taken to avoid the infection. On the daily biases, teeth come in contact of various
bacteria and fungus, which can harm the oral health in the end ( Butten, Johnson, Hall, Toombs,
King, & O’Grady, 2019).
Therefore, it can be said that taking the care of teeth from any kind disorder must be a
duty and a commitment for a lifetime.
Oral infection is a liability on Aboriginal and Torres and Strait Islander Australians in
comparison to non-aboriginal Torres and Strait Islander Australia, as oral illness is mostly found
in Indigenous Australian, which are known as Aboriginal and Torres Strait Islander citizens of
Australia than the non-Indigenous people of Australia.
2
486 million children were infected from the decay of deciduous teeth (Health People
Government , 2019). As per the statistics presented by Global Oral Health Data Bank in 2018,
the presence of dental carries differs from 49% to 83% in different countries. The major impacts
of dental issues can be observed in under-developed countries, wherewith the emergence of
urbanization, transformation living conditions and inadequate quality of health service has
increased the prevalence of oral disorders. Besides this oral issues can be occurred due to the
excessive consumption of tobacco, liquor and lack of nutrition. Ulcers, bleeding gums, plaque
which gets deposit on the teeth, bad smell, tooth sensitivity are symptoms upon which immediate
action must be taken to avoid the infection. On the daily biases, teeth come in contact of various
bacteria and fungus, which can harm the oral health in the end ( Butten, Johnson, Hall, Toombs,
King, & O’Grady, 2019).
Therefore, it can be said that taking the care of teeth from any kind disorder must be a
duty and a commitment for a lifetime.
Oral infection is a liability on Aboriginal and Torres and Strait Islander Australians in
comparison to non-aboriginal Torres and Strait Islander Australia, as oral illness is mostly found
in Indigenous Australian, which are known as Aboriginal and Torres Strait Islander citizens of
Australia than the non-Indigenous people of Australia.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING
3
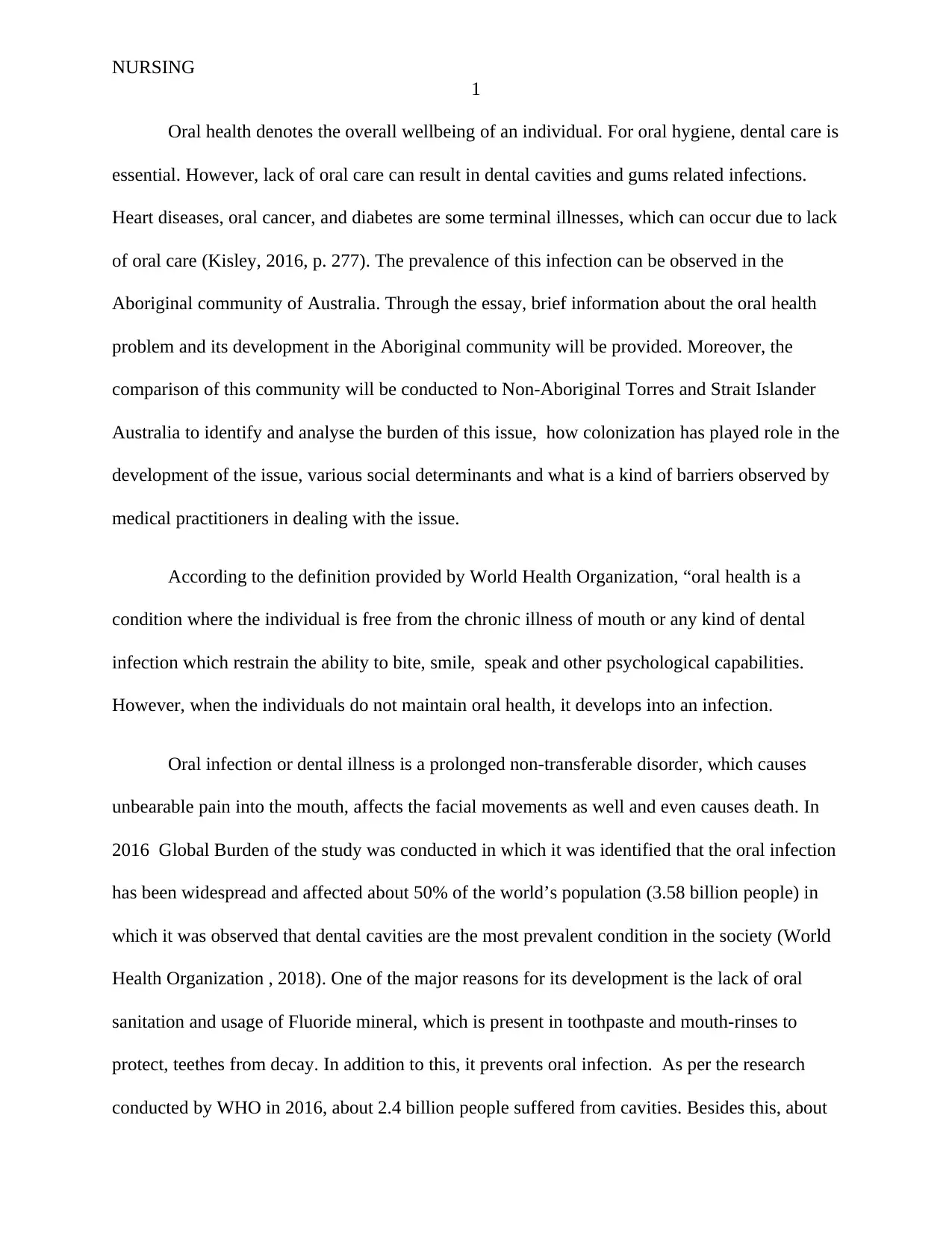
Figure 1
Source: (South Australia’s Oral Health Plan , 2019)
Due to lack of oral health services and facilities, oral diseases has life-threatening issue
among the people of Aboriginal and Torres Strait Islander, which are regarded as an Australia ‘s
first people (Health Performance Report , 2017).
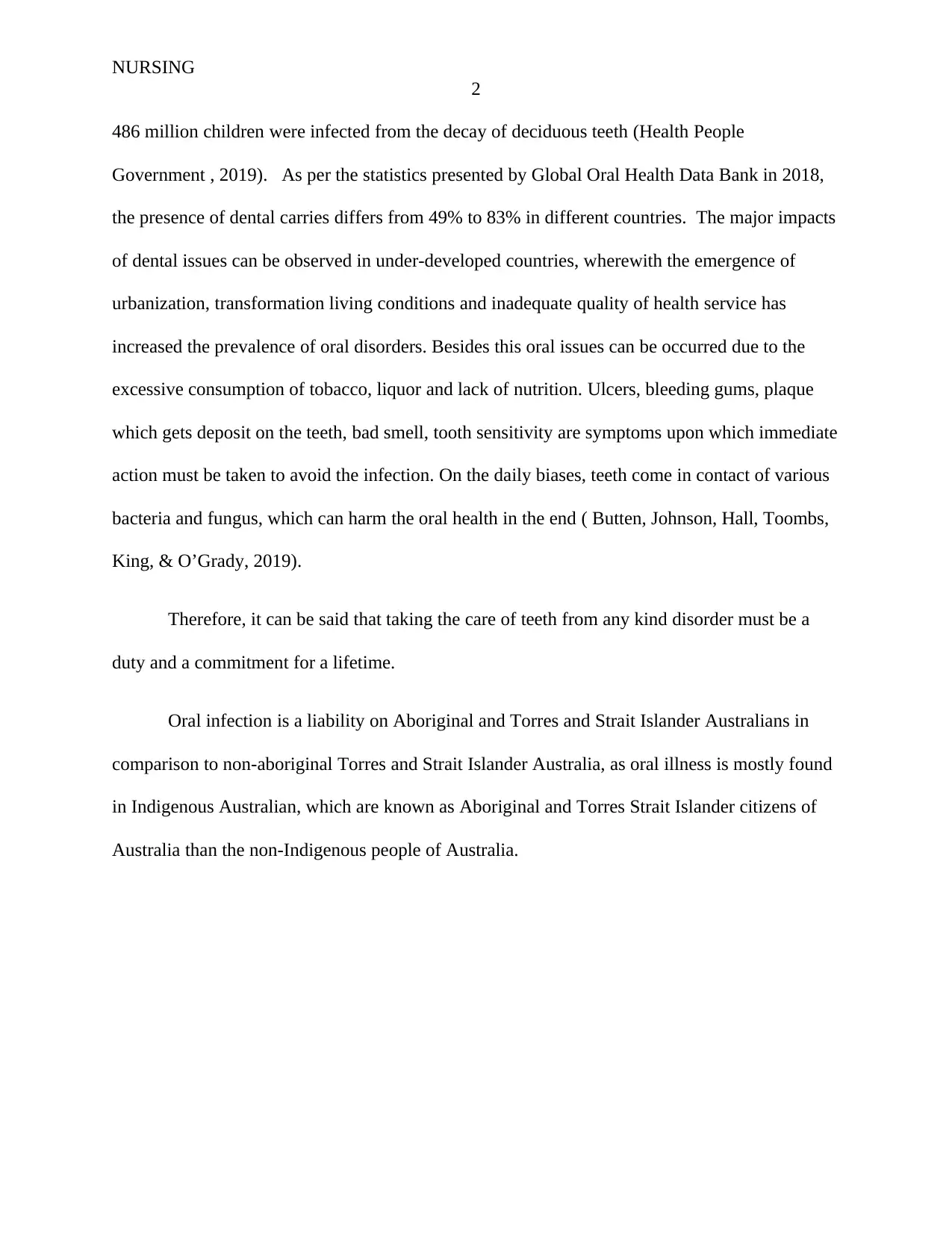
Figure 2
Source: (Health Performance Report , 2017)
3
Figure 1
Source: (South Australia’s Oral Health Plan , 2019)
Due to lack of oral health services and facilities, oral diseases has life-threatening issue
among the people of Aboriginal and Torres Strait Islander, which are regarded as an Australia ‘s
first people (Health Performance Report , 2017).
Figure 2
Source: (Health Performance Report , 2017)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
4
As per the study showcased through the above graph, it can be analysed that in June
2015, 6.9% of Aboriginal children from 0-4 age were detected and hospitalized for dental
infections, which is twice the rate of children living in other parts of Australia. It depicts the lack
of availability of an efficient health care system in underprivileged localities ( Butten, Johnson,
Hall, Toombs, King, & O’Grady, 2019).
In comparison to non- Aboriginal and Torres Strait Islander children, the probability of
oral decay and dental issues are higher in Aboriginal children. The issues related to the oral care
has been multiplied in the towns as the native people are not able to access timely dental
treatments to cure the infection. Moreover, they lack the knowledge to deal with the issue
( Butten, Johnson, Hall, Toombs, King, & O’Grady, 2019, p. 1). In addition to this, Due to
negligence, many Aboriginal youths have lost their teeth at an early age as compared to the
immigrant. Prolonged diseases like diabetes, consumption of tobacco, and poor dental sanitation
are some of the common issues that are among the native citizens (Australian Dental Association
, 2019). Such health problem has led to the rapid growth of Periodontitis (Gum infection that
damages the jawline). With the progress of periodontal diseases, the effectiveness of treatment
has been reduced. Besides this, in New South Wales, the development of oral caries or cavities is
twice among the local children as comparative to non-local infants. However, it is curable, but its
evolvement is worsening the situation in NSW. According to the sources, 57% of the native
people are suffering from chronic dental diseases whereas in urban cites 25% of adults are
infected to dental caries (Williams, 2011, p. 549). Dental cavities and Periodontitis results in
severe pain, infection and tooth loss and eventually deteriorate the health of the people (Shearer
& Jamieson , 2012, p. 319).
4
As per the study showcased through the above graph, it can be analysed that in June
2015, 6.9% of Aboriginal children from 0-4 age were detected and hospitalized for dental
infections, which is twice the rate of children living in other parts of Australia. It depicts the lack
of availability of an efficient health care system in underprivileged localities ( Butten, Johnson,
Hall, Toombs, King, & O’Grady, 2019).
In comparison to non- Aboriginal and Torres Strait Islander children, the probability of
oral decay and dental issues are higher in Aboriginal children. The issues related to the oral care
has been multiplied in the towns as the native people are not able to access timely dental
treatments to cure the infection. Moreover, they lack the knowledge to deal with the issue
( Butten, Johnson, Hall, Toombs, King, & O’Grady, 2019, p. 1). In addition to this, Due to
negligence, many Aboriginal youths have lost their teeth at an early age as compared to the
immigrant. Prolonged diseases like diabetes, consumption of tobacco, and poor dental sanitation
are some of the common issues that are among the native citizens (Australian Dental Association
, 2019). Such health problem has led to the rapid growth of Periodontitis (Gum infection that
damages the jawline). With the progress of periodontal diseases, the effectiveness of treatment
has been reduced. Besides this, in New South Wales, the development of oral caries or cavities is
twice among the local children as comparative to non-local infants. However, it is curable, but its
evolvement is worsening the situation in NSW. According to the sources, 57% of the native
people are suffering from chronic dental diseases whereas in urban cites 25% of adults are
infected to dental caries (Williams, 2011, p. 549). Dental cavities and Periodontitis results in
severe pain, infection and tooth loss and eventually deteriorate the health of the people (Shearer
& Jamieson , 2012, p. 319).
NURSING
5
One of the major reason of high prevalence of oral diseases in Aboriginal communities is
colonization. Due to the colonization, today Aboriginal communities of Australia are deprived of
basic needs and currently suffering from various social problems like poverty, low life
expectancy and financial support from the government (Behrendt, 2016). The majority of the
people of these communities have no shelter and have a high prevalence of violence and physical
abuse. In spite of government efforts, the occurrence of dental infections in local communities is
very much higher in comparison to Non-Aboriginal communities (Dudgeon , Wright, Paradies,
Garvey, & Walker, 2019). One of the major reasons for such ineffectiveness is orthodox
thinking and discrimination against native people of Australia, whose presence can be witnessed
in the healthcare system of the nation ( Riggs, et al., 2015, p. 241).
Colonization is one of the major factors, which has created disparities among the people
of the nation and has led the path of injustice, as they are not accepted by the society (Sherwood,
2013, p. 28). Such bias attitude has resulted in unbalanced health of Indigenous individuals. In
the history of colonization, Indigenous citizens of Australia used to have small tribe, living in a
definite area. Currently, the situation of Aboriginal people is so worse that they are not able to
cure the prolonged diseases ( Griffiths, Coleman, Lee, & Madden, 2016, p. 9). Decreased
awareness of the high degree of oral infection and lack of dental care describe the biasedness of
the society towards the native people. Addition to the colonization, urbanization, difference in
the lifestyle has created a gap between two communities.
They are two major determinants of health, which affect the development of oral health is
Social Culture. It depicts the impact Social economic status over the overall health of the
individuals. A study was conducted in which it has been identified that social and economic
disparities are connected with the dental care status. Monitoring the social-economic status in
5
One of the major reason of high prevalence of oral diseases in Aboriginal communities is
colonization. Due to the colonization, today Aboriginal communities of Australia are deprived of
basic needs and currently suffering from various social problems like poverty, low life
expectancy and financial support from the government (Behrendt, 2016). The majority of the
people of these communities have no shelter and have a high prevalence of violence and physical
abuse. In spite of government efforts, the occurrence of dental infections in local communities is
very much higher in comparison to Non-Aboriginal communities (Dudgeon , Wright, Paradies,
Garvey, & Walker, 2019). One of the major reasons for such ineffectiveness is orthodox
thinking and discrimination against native people of Australia, whose presence can be witnessed
in the healthcare system of the nation ( Riggs, et al., 2015, p. 241).
Colonization is one of the major factors, which has created disparities among the people
of the nation and has led the path of injustice, as they are not accepted by the society (Sherwood,
2013, p. 28). Such bias attitude has resulted in unbalanced health of Indigenous individuals. In
the history of colonization, Indigenous citizens of Australia used to have small tribe, living in a
definite area. Currently, the situation of Aboriginal people is so worse that they are not able to
cure the prolonged diseases ( Griffiths, Coleman, Lee, & Madden, 2016, p. 9). Decreased
awareness of the high degree of oral infection and lack of dental care describe the biasedness of
the society towards the native people. Addition to the colonization, urbanization, difference in
the lifestyle has created a gap between two communities.
They are two major determinants of health, which affect the development of oral health is
Social Culture. It depicts the impact Social economic status over the overall health of the
individuals. A study was conducted in which it has been identified that social and economic
disparities are connected with the dental care status. Monitoring the social-economic status in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING
6
oral care is critical to describe the differences in the treatment and medications. Moreover, on the
bases of the differences, medical professional discriminates between the patients. Earlier it was
perceived the social and economic position of any individual negatively affects the treatment of
oral health infections as it suggests that higher the economic status, better quality services to cure
the oral infections and prior attention than the rest of the patients. In the medical system,
financial status and academic standards are utilizing to measure the status of patients (Tellez ,
Zini , & Estupiñan-Day, 2014, p. 148).
Another determinant is Structural change. A structural change like income, goods, and
services and climate affects the prevalence of Oral diseases in aboriginal communities in
Australia. It describes prevailing living conditions and social gradients. Social Gradient in
medical terms describes two situations in which individuals that are underprivileged in terms of
social-economic status, have poor oral health and low life expectancy in comparison to
advantaged sections of the society. Oral disease and lack of dental care services in the local areas
of the community are some of the impacts of a structural shift in Australia (Jamieson, et al.,
2016, p. 1375).
In the article “The oral health care experiences of NSW Aboriginal Community
Controlled Health Services” author Megan A. Campbell has stated Aboriginal communities are
suffering prolonged illness of Oral health (Campbell, Hunt, Walker, & Williams, 2015, p. 21).
To provide a cure for this illness, various health care services have been started by the
government and hospitals for the underprivileged section of the society. Services have been
provided by ACCHS (Aboriginal Community Controlled Health Service). Through the article, it
has been perceived financial assistance and lack of appropriate workforce are two major barriers,
which are disturbing the flow of Oral health services. ACCHS further stated due to insufficient
6
oral care is critical to describe the differences in the treatment and medications. Moreover, on the
bases of the differences, medical professional discriminates between the patients. Earlier it was
perceived the social and economic position of any individual negatively affects the treatment of
oral health infections as it suggests that higher the economic status, better quality services to cure
the oral infections and prior attention than the rest of the patients. In the medical system,
financial status and academic standards are utilizing to measure the status of patients (Tellez ,
Zini , & Estupiñan-Day, 2014, p. 148).
Another determinant is Structural change. A structural change like income, goods, and
services and climate affects the prevalence of Oral diseases in aboriginal communities in
Australia. It describes prevailing living conditions and social gradients. Social Gradient in
medical terms describes two situations in which individuals that are underprivileged in terms of
social-economic status, have poor oral health and low life expectancy in comparison to
advantaged sections of the society. Oral disease and lack of dental care services in the local areas
of the community are some of the impacts of a structural shift in Australia (Jamieson, et al.,
2016, p. 1375).
In the article “The oral health care experiences of NSW Aboriginal Community
Controlled Health Services” author Megan A. Campbell has stated Aboriginal communities are
suffering prolonged illness of Oral health (Campbell, Hunt, Walker, & Williams, 2015, p. 21).
To provide a cure for this illness, various health care services have been started by the
government and hospitals for the underprivileged section of the society. Services have been
provided by ACCHS (Aboriginal Community Controlled Health Service). Through the article, it
has been perceived financial assistance and lack of appropriate workforce are two major barriers,
which are disturbing the flow of Oral health services. ACCHS further stated due to insufficient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
7
funds, effective treatment of the patients has become difficult. Moreover, insufficient capital has
become a roadblock in the recruitment of medical professionals and staff. Another barrier is
private care from the CDDS (Chronic Diseases Dental Diseases) with the less availability of the
medical professionals and midwives. In addition to this, many local dentists have refused to treat
Aboriginal communities. Such a biased attitude has been experienced by ACCHS ( Durey &
Thompson, 2011, p. 1).
7
funds, effective treatment of the patients has become difficult. Moreover, insufficient capital has
become a roadblock in the recruitment of medical professionals and staff. Another barrier is
private care from the CDDS (Chronic Diseases Dental Diseases) with the less availability of the
medical professionals and midwives. In addition to this, many local dentists have refused to treat
Aboriginal communities. Such a biased attitude has been experienced by ACCHS ( Durey &
Thompson, 2011, p. 1).
NURSING
8
From the above essay, it can be inferred that maintaining Oral wellbeing is very crucial
for the overall health of the individual. However, when proper care is not taken, then various oral
care problems start developing into the mouth like infections and terminal illness. Oral diseases
cause tooth decay, unbearable pain and affects facial movements. However, such diseases can
mainly be observed in low and middle-income countries like in Australia, In Australia, the
effects of oral infection can be seen in Aboriginal and Torres and Strait Islander Australians. In
the essay, it was also discussed the burden on aboriginal communities in comparison to the non-
aboriginal community and regarding the barriers that are appearing in the treatment of the
citizens of this community.
8
From the above essay, it can be inferred that maintaining Oral wellbeing is very crucial
for the overall health of the individual. However, when proper care is not taken, then various oral
care problems start developing into the mouth like infections and terminal illness. Oral diseases
cause tooth decay, unbearable pain and affects facial movements. However, such diseases can
mainly be observed in low and middle-income countries like in Australia, In Australia, the
effects of oral infection can be seen in Aboriginal and Torres and Strait Islander Australians. In
the essay, it was also discussed the burden on aboriginal communities in comparison to the non-
aboriginal community and regarding the barriers that are appearing in the treatment of the
citizens of this community.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING
9
Bibliography
Butten, K., Johnson, N. W., Hall, K. K., Toombs, M., King, N., & O’Grady, K.-A. F. (2019).
Impact of oral health on Australian urban Aboriginal and Torres Strait Islander families:
a qualitative study. International Journal for Equity in Health, 1-10.
Durey, A., & Thompson, S. C. (2011). Reducing the health disparities of Indigenous Australians:
time to change focus. Health Services Research, 1-11.
Griffiths, K., Coleman, C., Lee, V., & Madden, R. (2016). How colonisation determines social
justice and Indigenous health—a review of the literature. Journal of Popular Research,
9–30.
Riggs, E., Gibbs, L., Kilpatrick, N., Gussy, M., Gemert, C. v., Ali, S., et al. (2015). Breaking
down the barriers: a qualitative study to understand child oral health in refugee and
migrant communities in Australia. Ethnicity & Health, 241–257.
Australian Dental Association . (2019). Policy Statement 2.3.5 – Delivery of Oral Health:
Special groups: Aboriginal and Torres Strait Islander Australians. Retrieved 2019, from
Australian Dental Association:
https://www.ada.org.au/Dental-Professionals/Policies/National-Oral-Health/2-3-5-
Aboriginal-and-Torres-Strait-Islander-Austra/ADAPolicies_2-3-
5_AboriginalandTorresStraitIslande.aspx
Behrendt, L. (2016, September 22). Indigenous Australians know we're the oldest living culture
– it's in our Dreamtime. Retrieved 2019, from The Guardian :
9
Bibliography
Butten, K., Johnson, N. W., Hall, K. K., Toombs, M., King, N., & O’Grady, K.-A. F. (2019).
Impact of oral health on Australian urban Aboriginal and Torres Strait Islander families:
a qualitative study. International Journal for Equity in Health, 1-10.
Durey, A., & Thompson, S. C. (2011). Reducing the health disparities of Indigenous Australians:
time to change focus. Health Services Research, 1-11.
Griffiths, K., Coleman, C., Lee, V., & Madden, R. (2016). How colonisation determines social
justice and Indigenous health—a review of the literature. Journal of Popular Research,
9–30.
Riggs, E., Gibbs, L., Kilpatrick, N., Gussy, M., Gemert, C. v., Ali, S., et al. (2015). Breaking
down the barriers: a qualitative study to understand child oral health in refugee and
migrant communities in Australia. Ethnicity & Health, 241–257.
Australian Dental Association . (2019). Policy Statement 2.3.5 – Delivery of Oral Health:
Special groups: Aboriginal and Torres Strait Islander Australians. Retrieved 2019, from
Australian Dental Association:
https://www.ada.org.au/Dental-Professionals/Policies/National-Oral-Health/2-3-5-
Aboriginal-and-Torres-Strait-Islander-Austra/ADAPolicies_2-3-
5_AboriginalandTorresStraitIslande.aspx
Behrendt, L. (2016, September 22). Indigenous Australians know we're the oldest living culture
– it's in our Dreamtime. Retrieved 2019, from The Guardian :
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING
10
https://www.theguardian.com/commentisfree/2016/sep/22/indigenous-australians-know-
were-the-oldest-living-culture-its-in-our-dreamtime
Campbell, M. A., Hunt, J., Walker, D., & Williams, R. (2015). The oral health care experiences
of NSW Aboriginal. Australian and New Zealand Journal of Public Health, 39(1), 21-25.
Dudgeon , P., Wright, M., Paradies, Y., Garvey, D., & Walker, I. (2019). The Social, Cultural
and Historical Context of Aboriginal and Torres Strait Islander Australians. Retrieved
2019, from Working Together:
https://pdfs.semanticscholar.org/50b6/5225341222d898453e8932aafd020207f56d.pdf
Health People Government . (2019). Oral Health. Retrieved from Health People Government:
https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health
Health Performance Report . (2017). Aboriginal and Torres Strait Islander Health Performance
Framework 2017 Report. Retrieved 2019, from
https://www.pmc.gov.au/sites/default/files/publications/indigenous/hpf-2017/
tier1/111.html
Jamieson, L., Elani, H., Mejia, G., Ju, X., Kawachi, I., Thomson, W., et al. (2016). Inequalities in
Indigenous Oral Health: Findings from Australia, New Zealand, and Canada. Journal of
Dental Research, 1375–1380.
Kisley, S. (2016). No Mental Health without Oral Health. Canadian Psychiatric Association ,
277-282.
Shearer, M., & Jamieson , L. (2012). Indigenous Australians and Oral Health. Indigenous
Australians and Oral Health , 319-340.
10
https://www.theguardian.com/commentisfree/2016/sep/22/indigenous-australians-know-
were-the-oldest-living-culture-its-in-our-dreamtime
Campbell, M. A., Hunt, J., Walker, D., & Williams, R. (2015). The oral health care experiences
of NSW Aboriginal. Australian and New Zealand Journal of Public Health, 39(1), 21-25.
Dudgeon , P., Wright, M., Paradies, Y., Garvey, D., & Walker, I. (2019). The Social, Cultural
and Historical Context of Aboriginal and Torres Strait Islander Australians. Retrieved
2019, from Working Together:
https://pdfs.semanticscholar.org/50b6/5225341222d898453e8932aafd020207f56d.pdf
Health People Government . (2019). Oral Health. Retrieved from Health People Government:
https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health
Health Performance Report . (2017). Aboriginal and Torres Strait Islander Health Performance
Framework 2017 Report. Retrieved 2019, from
https://www.pmc.gov.au/sites/default/files/publications/indigenous/hpf-2017/
tier1/111.html
Jamieson, L., Elani, H., Mejia, G., Ju, X., Kawachi, I., Thomson, W., et al. (2016). Inequalities in
Indigenous Oral Health: Findings from Australia, New Zealand, and Canada. Journal of
Dental Research, 1375–1380.
Kisley, S. (2016). No Mental Health without Oral Health. Canadian Psychiatric Association ,
277-282.
Shearer, M., & Jamieson , L. (2012). Indigenous Australians and Oral Health. Indigenous
Australians and Oral Health , 319-340.
NURSING
11
Sherwood, J. (2013). Colonisation – It’s bad for your health: The context of Aboriginal health. A
Journal for Australian Nursing Profession, 28-40.
South Australia’s Oral Health Plan . (2019). Draft Saohp 2019 - 2026. Retrieved 2019, from
South Australia’s Oral Health Plan – draft 6Mar2019:
https://www.sahealth.sa.gov.au/wps/wcm/connect/6513697c-c216-417e-be20-
3ee3fa1ebcd5/draft+SOHP+proposed+for+release+for+public+consultation+6-3-19.pdf?
MOD=AJPERES&CACHEID=ROOTWORKSPACE-6513697c-c216-417e-be20-
3ee3fa1ebcd5-mNBSK4P
Tellez , M., Zini , A., & Estupiñan-Day, S. (2014). Social Determinants and Oral Health: An
Update. Current Oral Health Report , 148-152.
Williams, D. (2011). Global Oral Health Inequalities: The Research Agenda. Journal of Dental
Research, 549-551.
World Health Organization . (2018, September 24). Oral health. Retrieved 2019, from World
Health Organization: https://www.who.int/news-room/fact-sheets/detail/oral-health
11
Sherwood, J. (2013). Colonisation – It’s bad for your health: The context of Aboriginal health. A
Journal for Australian Nursing Profession, 28-40.
South Australia’s Oral Health Plan . (2019). Draft Saohp 2019 - 2026. Retrieved 2019, from
South Australia’s Oral Health Plan – draft 6Mar2019:
https://www.sahealth.sa.gov.au/wps/wcm/connect/6513697c-c216-417e-be20-
3ee3fa1ebcd5/draft+SOHP+proposed+for+release+for+public+consultation+6-3-19.pdf?
MOD=AJPERES&CACHEID=ROOTWORKSPACE-6513697c-c216-417e-be20-
3ee3fa1ebcd5-mNBSK4P
Tellez , M., Zini , A., & Estupiñan-Day, S. (2014). Social Determinants and Oral Health: An
Update. Current Oral Health Report , 148-152.
Williams, D. (2011). Global Oral Health Inequalities: The Research Agenda. Journal of Dental
Research, 549-551.
World Health Organization . (2018, September 24). Oral health. Retrieved 2019, from World
Health Organization: https://www.who.int/news-room/fact-sheets/detail/oral-health
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





