Palliative Care: Origins, Core Principles and Delivery Methods
VerifiedAdded on 2024/06/05
|10
|2018
|72
Essay
AI Summary
This essay provides a thorough understanding of palliative care, beginning with its origins and development, highlighting Cicely Sanders' role in the modern hospice movement and the evolution from traditional hospice care to a comprehensive approach addressing patient needs from diagnosis through end-of-life. It details the core principles of palliative care, including pain management, holistic assessment of physical, psychological, spiritual, and social needs, and support for both patients and their families. Furthermore, the essay critically examines various delivery models, such as home-based, outpatient, inpatient, and specialist settings, discussing their strengths and limitations, and emphasizing the shift towards specialist-level palliative care programs in the UK. The essay concludes by affirming the benefits of palliative care in enhancing the quality of life for terminally ill patients, relieving pain and distressing symptoms, and providing essential support to families during bereavement.
Contents
Introduction...........................................................................................................................................1
1. Demonstrate the thorough understanding of the origins and development of palliative care.....1
2. Demonstrate the principle of palliative care.................................................................................2
3. Demonstrate a critical understanding of the delivery of palliative care........................................3
Conclusion.............................................................................................................................................7
References.............................................................................................................................................9
1
Introduction...........................................................................................................................................1
1. Demonstrate the thorough understanding of the origins and development of palliative care.....1
2. Demonstrate the principle of palliative care.................................................................................2
3. Demonstrate a critical understanding of the delivery of palliative care........................................3
Conclusion.............................................................................................................................................7
References.............................................................................................................................................9
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Palliative care is the term first coined by Cicely Sanders in 1959, it refers to the care
provided by allied health services for the terminally ill patient and their families the main
role of palliative care is to improve the quality of life of the patient for remaining lifespan. As
the life-limiting diseases encounter the most of resources of the family in taking care of the
diseased the health and social services provide palliative care that helps the families of the
patient too (Alliance, W.P.C. and World Health Organization, 2014).
2
Palliative care is the term first coined by Cicely Sanders in 1959, it refers to the care
provided by allied health services for the terminally ill patient and their families the main
role of palliative care is to improve the quality of life of the patient for remaining lifespan. As
the life-limiting diseases encounter the most of resources of the family in taking care of the
diseased the health and social services provide palliative care that helps the families of the
patient too (Alliance, W.P.C. and World Health Organization, 2014).
2
1. Demonstrate the thorough understanding of the origins and
development of palliative care.
Over the years the palliative care services have changed their face hugely and are not only
confined to the wordy meanings but are advocated by almost all of the healthcare services
and professionals. At first the origin of palliative care was in traditional and holistic
approaches but later it was identified to be of good scientific use and the utilization of
palliative care was started in health and social care (Zimmermann et al, 2014). Cicely
Sanders is known as founder of modern hospice movement that is who introduced the need
of palliative care (Clark, 2018). There was the time when hospice care was practised widely
that is the care provided after the treatment of life-threatening diseases. The founder of
palliative care identified the need for an approach that can be utilized to provide care since
the person is diagnosed with the disease and it can also prove to be an effective treatment
and thus the palliative care originated as widely used practice now-a-days (Connor, 2017).
The understanding for palliative care is essential as the term when heard mostly denotes
that the individual is dying but palliative care is not only for people who are dyeing it can be
provided as a treatment for people who are to die but can prolong their quality of life or
remaining span. Palliative care means to cloak or mask the disease that is a process where
we do not cure it but mask its effects. The development of palliative care over time since the
hospice movement of 1970's to the introduction and use of palliative care in the 19th
century there was very first development by the setting of various homes and centres
dedicated to the care of dying. St Joseph's Hospice for the Dying, Hackney London (opened
1905) was some of the institutes introduced then for caring for dying people. Later the
qualified healthcare professionals identified the need for the introduction of methods and
modalities to relieve the pain for dying patient and this was the outbreak in the palliative
care development. There were many women working in the same direction in nineteenth-
century unaware of each other's work. Jeanne Garnier was one of the earliest founders of
hospice homes in Europe and work for providing care for the dying. She started very first
home to help and care for people who were dying with respite care and services for caring
for people who are going to die (Guirimand et al, 2014). Her work based in establishment of
many other developments in order of palliative care for terminally ill patient. Rose
Hawthorn Lathrop was another nurse who trained for care for cancer patient and later
established the services to develop the care for impoverished cancer patients for their
3
development of palliative care.
Over the years the palliative care services have changed their face hugely and are not only
confined to the wordy meanings but are advocated by almost all of the healthcare services
and professionals. At first the origin of palliative care was in traditional and holistic
approaches but later it was identified to be of good scientific use and the utilization of
palliative care was started in health and social care (Zimmermann et al, 2014). Cicely
Sanders is known as founder of modern hospice movement that is who introduced the need
of palliative care (Clark, 2018). There was the time when hospice care was practised widely
that is the care provided after the treatment of life-threatening diseases. The founder of
palliative care identified the need for an approach that can be utilized to provide care since
the person is diagnosed with the disease and it can also prove to be an effective treatment
and thus the palliative care originated as widely used practice now-a-days (Connor, 2017).
The understanding for palliative care is essential as the term when heard mostly denotes
that the individual is dying but palliative care is not only for people who are dyeing it can be
provided as a treatment for people who are to die but can prolong their quality of life or
remaining span. Palliative care means to cloak or mask the disease that is a process where
we do not cure it but mask its effects. The development of palliative care over time since the
hospice movement of 1970's to the introduction and use of palliative care in the 19th
century there was very first development by the setting of various homes and centres
dedicated to the care of dying. St Joseph's Hospice for the Dying, Hackney London (opened
1905) was some of the institutes introduced then for caring for dying people. Later the
qualified healthcare professionals identified the need for the introduction of methods and
modalities to relieve the pain for dying patient and this was the outbreak in the palliative
care development. There were many women working in the same direction in nineteenth-
century unaware of each other's work. Jeanne Garnier was one of the earliest founders of
hospice homes in Europe and work for providing care for the dying. She started very first
home to help and care for people who were dying with respite care and services for caring
for people who are going to die (Guirimand et al, 2014). Her work based in establishment of
many other developments in order of palliative care for terminally ill patient. Rose
Hawthorn Lathrop was another nurse who trained for care for cancer patient and later
established the services to develop the care for impoverished cancer patients for their
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

terminal illness. At first, she used to visit patients at their houses and deliver care but later
she started a small care home for dying cancer patients.
2. Demonstrate the principle of palliative care.
The principles of care are also followed while delivering palliative services to the patient and
his family. The principles of palliative care includes provide relief from pain and other
distressing symptoms, affirms life and regards dyeing as a normal process, intends neither to
hastened not to postpone death, integrates the psychological and spiritual aspects of the
patient, offer services and support that will help patient live actively till death, offer the
family of patient the support to cope with patient’s illness and in time of bereavement, try
to enhance the quality of life through the course of illness, palliative care should be
provided with other therapies for prolonging life as chemo and radiotherapy. The most
important aspect of palliative care is pain management and avoiding distressing symptoms
(Kelley and Morrison, 2015). The control and relief from pain are essential as it will provide a
better quality of life for an individual in terminal stages. The palliative care does not work to
prolong any sort of lifespan or treat the disease but it helps in promoting better quality life
and less suffering from the symptoms of disease (Al Qadire, 2014.). The holistic needs of a
patient including physical, psychological, spiritual and social needs should be assessed
during palliative care. the physical needs may include physical status, relief from symptoms,
nutrition and hydration and safety. Psychological needs include mood, coping styles,
cognition, dimension etc. spiritual needs like meaning of life and death, acceptance of death
and illness etc. social dimensions include social interactions, prevention of isolation,
community environment, burden on family etc. these all needs are to be taken care of while
delivering palliative care. For pain relief, the morphine administration is most widely used
measure for palliative care cases. Benefits of palliative care are huge to patient, families and
healthcare professionals. It helps in reducing the distress to the patient and families,
involving the patient and their families in decision making, encourage discussion on proper
acceptance on death and dying, offering the patient and families the consistent care,
provide quality of life it also helps in supporting families during bereavement (Jones, 2015).
3. Demonstrate a critical understanding of the delivery of palliative care.
The palliative care can be delivered in various kinds of models as per the care settings and
requirement of the care. the various models of care can be home based clinic, roadside
4
she started a small care home for dying cancer patients.
2. Demonstrate the principle of palliative care.
The principles of care are also followed while delivering palliative services to the patient and
his family. The principles of palliative care includes provide relief from pain and other
distressing symptoms, affirms life and regards dyeing as a normal process, intends neither to
hastened not to postpone death, integrates the psychological and spiritual aspects of the
patient, offer services and support that will help patient live actively till death, offer the
family of patient the support to cope with patient’s illness and in time of bereavement, try
to enhance the quality of life through the course of illness, palliative care should be
provided with other therapies for prolonging life as chemo and radiotherapy. The most
important aspect of palliative care is pain management and avoiding distressing symptoms
(Kelley and Morrison, 2015). The control and relief from pain are essential as it will provide a
better quality of life for an individual in terminal stages. The palliative care does not work to
prolong any sort of lifespan or treat the disease but it helps in promoting better quality life
and less suffering from the symptoms of disease (Al Qadire, 2014.). The holistic needs of a
patient including physical, psychological, spiritual and social needs should be assessed
during palliative care. the physical needs may include physical status, relief from symptoms,
nutrition and hydration and safety. Psychological needs include mood, coping styles,
cognition, dimension etc. spiritual needs like meaning of life and death, acceptance of death
and illness etc. social dimensions include social interactions, prevention of isolation,
community environment, burden on family etc. these all needs are to be taken care of while
delivering palliative care. For pain relief, the morphine administration is most widely used
measure for palliative care cases. Benefits of palliative care are huge to patient, families and
healthcare professionals. It helps in reducing the distress to the patient and families,
involving the patient and their families in decision making, encourage discussion on proper
acceptance on death and dying, offering the patient and families the consistent care,
provide quality of life it also helps in supporting families during bereavement (Jones, 2015).
3. Demonstrate a critical understanding of the delivery of palliative care.
The palliative care can be delivered in various kinds of models as per the care settings and
requirement of the care. the various models of care can be home based clinic, roadside
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
clinics, outpatient care, inpatient care, facility-based care, Daycare etc. the palliative care
can be provided in general as well as specialist setting as per the requirement and the
palliative care team will take extra care of palliative care patients (Partridge et al, 2014).
Hospice care- a programme providing people prognosis of six months or less and providing
care for this duration
Outpatient care- provided in ambulatory care setting to provide care to terminally ill
patients
Community patient care- occurs in collaboration of community services in community
settings to support seriously ill patients. it is better served as it can reach patient with life-
threatening illness easily, meet all dimensions of needs of the patients, provide care in care
homes and residential homes that reduce unnecessary hospital admissions and also support
family and carers in bereavement stages.
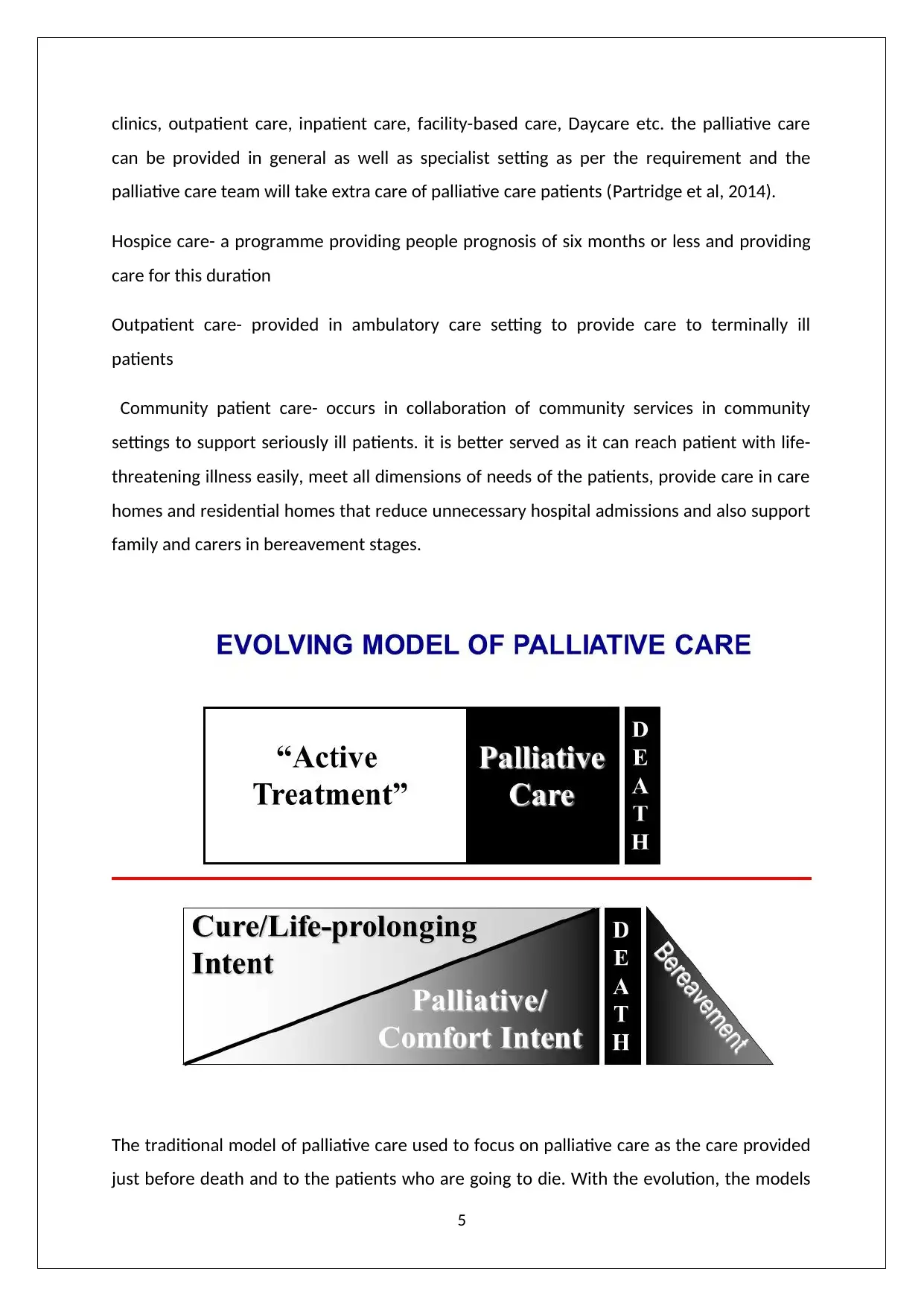
The traditional model of palliative care used to focus on palliative care as the care provided
just before death and to the patients who are going to die. With the evolution, the models
5
can be provided in general as well as specialist setting as per the requirement and the
palliative care team will take extra care of palliative care patients (Partridge et al, 2014).
Hospice care- a programme providing people prognosis of six months or less and providing
care for this duration
Outpatient care- provided in ambulatory care setting to provide care to terminally ill
patients
Community patient care- occurs in collaboration of community services in community
settings to support seriously ill patients. it is better served as it can reach patient with life-
threatening illness easily, meet all dimensions of needs of the patients, provide care in care
homes and residential homes that reduce unnecessary hospital admissions and also support
family and carers in bereavement stages.
The traditional model of palliative care used to focus on palliative care as the care provided
just before death and to the patients who are going to die. With the evolution, the models
5

of care changed and evolved model denotes palliative care with all dimensions that will help
in life-prolonging intent, comfort the patient during terminal stages and also support the
family after patient's death.
Other models include palliative care in a hospital, ambulatory setting and home. The
hospital setting involves three models that are- Palliative care consultation services,
dedicated and integrated palliative care. the ambulatory palliative services ensure
continuous care for hospital discharged patients, on-going care for symptoms distress and
complex treatments, pain management and psychosocial support for patient and families
and enhances the quality of life.
There is some critical analysis of the palliative care models as doctors are supposed to play
an active role in palliative care but in the community and home-based settings the nurses
are playing lead roles in palliative care. Teamwork can be limited in home-based care as all
the practitioners cannot be present to provide care. Pain control is also not as effective as
patients cared in hospitals than at homes. The delivery of palliative care in the UK is
moreover shifting to specialist-level palliative care programme where a care team is
supposed to have specialist professionals to advocate the care process as per patient’s
requirements (Dobrina et al, 2014).
6
in life-prolonging intent, comfort the patient during terminal stages and also support the
family after patient's death.
Other models include palliative care in a hospital, ambulatory setting and home. The
hospital setting involves three models that are- Palliative care consultation services,
dedicated and integrated palliative care. the ambulatory palliative services ensure
continuous care for hospital discharged patients, on-going care for symptoms distress and
complex treatments, pain management and psychosocial support for patient and families
and enhances the quality of life.
There is some critical analysis of the palliative care models as doctors are supposed to play
an active role in palliative care but in the community and home-based settings the nurses
are playing lead roles in palliative care. Teamwork can be limited in home-based care as all
the practitioners cannot be present to provide care. Pain control is also not as effective as
patients cared in hospitals than at homes. The delivery of palliative care in the UK is
moreover shifting to specialist-level palliative care programme where a care team is
supposed to have specialist professionals to advocate the care process as per patient’s
requirements (Dobrina et al, 2014).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Conclusion
Care at the end of life is essential and this is being demonstrated in explaining different
aspects of palliative care in this assignment. This essay reveals that the palliative care is
beneficial to the terminally ill patients in any setting that helps enhance their quality of life
and care that will provide relief from pain and distressing symptoms of the disease. It not
only helps the patient but also supports the family and carers to cope up with the disease an
treatment of the patient and during the bereavement after their death.
8
Care at the end of life is essential and this is being demonstrated in explaining different
aspects of palliative care in this assignment. This essay reveals that the palliative care is
beneficial to the terminally ill patients in any setting that helps enhance their quality of life
and care that will provide relief from pain and distressing symptoms of the disease. It not
only helps the patient but also supports the family and carers to cope up with the disease an
treatment of the patient and during the bereavement after their death.
8
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Al Qadire, M., 2014. Knowledge of palliative care: An online survey. Nurse education today,
34(5), pp.714-718.
Alliance, W.P.C. and World Health Organization, 2014. Global atlas of palliative care at the
end of life. London: Worldwide Palliative Care Alliance.
Clark, D., 2018. Cicely Saunders: A Life and Legacy. Oxford University Press.
Connor, S.R., 2017. Hospice and palliative care: The essential guide. Taylor & Francis.
Dobrina, R., Tenze, M. and Palese, A., 2014. An overview of hospice and palliative care
nursing models and theories. International journal of palliative nursing, 20(2), pp.75-81.
Guirimand, F., Dubois, E., Laporte, L., Richard, J.F. and Leboul, D., 2014. Death wishes and
explicit requests for euthanasia in a palliative care hospital: an analysis of patients files. BMC
palliative care, 13(1), p.53.
Jones, J., 2015. Benefits of palliative care. Professional case management, 20(5), pp.262-
264.
Kelley, A.S. and Morrison, R.S., 2015. Palliative care for the seriously ill. New England Journal
of Medicine, 373(8), pp.747-755.
Partridge, A.H., Seah, D.S., King, T., Leighl, N.B., Hauke, R., Wollins, D.S. and Von Roenn, J.H.,
2014. Developing a service model that integrates palliative care throughout cancer care: the
time is now. Journal of Clinical Oncology, 32(29), pp.3330-3336.
Zimmermann, C., Swami, N., Krzyzanowska, M., Hannon, B., Leighl, N., Oza, A., Moore, M.,
Rydall, A., Rodin, G., Tannock, I. and Donner, A., 2014. Early palliative care for patients with
advanced cancer: a cluster-randomised controlled trial. The Lancet, 383(9930), pp.1721-
1730.
10
Al Qadire, M., 2014. Knowledge of palliative care: An online survey. Nurse education today,
34(5), pp.714-718.
Alliance, W.P.C. and World Health Organization, 2014. Global atlas of palliative care at the
end of life. London: Worldwide Palliative Care Alliance.
Clark, D., 2018. Cicely Saunders: A Life and Legacy. Oxford University Press.
Connor, S.R., 2017. Hospice and palliative care: The essential guide. Taylor & Francis.
Dobrina, R., Tenze, M. and Palese, A., 2014. An overview of hospice and palliative care
nursing models and theories. International journal of palliative nursing, 20(2), pp.75-81.
Guirimand, F., Dubois, E., Laporte, L., Richard, J.F. and Leboul, D., 2014. Death wishes and
explicit requests for euthanasia in a palliative care hospital: an analysis of patients files. BMC
palliative care, 13(1), p.53.
Jones, J., 2015. Benefits of palliative care. Professional case management, 20(5), pp.262-
264.
Kelley, A.S. and Morrison, R.S., 2015. Palliative care for the seriously ill. New England Journal
of Medicine, 373(8), pp.747-755.
Partridge, A.H., Seah, D.S., King, T., Leighl, N.B., Hauke, R., Wollins, D.S. and Von Roenn, J.H.,
2014. Developing a service model that integrates palliative care throughout cancer care: the
time is now. Journal of Clinical Oncology, 32(29), pp.3330-3336.
Zimmermann, C., Swami, N., Krzyzanowska, M., Hannon, B., Leighl, N., Oza, A., Moore, M.,
Rydall, A., Rodin, G., Tannock, I. and Donner, A., 2014. Early palliative care for patients with
advanced cancer: a cluster-randomised controlled trial. The Lancet, 383(9930), pp.1721-
1730.
10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





