Osteoarthritis: A Clinical Update on Causes, Diagnosis, and Treatments
VerifiedAdded on 2022/08/23
|12
|3093
|26
Report
AI Summary
This report provides a comprehensive clinical update on osteoarthritis, the most prevalent musculoskeletal disease globally. It delves into the disease's epidemiology, highlighting its impact worldwide and in Australia, including the burden of disease and the role of genetic and acquired risk factors. The report explores the aetiology and pathogenesis, detailing the causes, risk factors, and disease progression, including the impact on public health. Clinical manifestations, diagnostic processes, and treatment options are also covered, including pharmacological, non-pharmacological, and surgical interventions, along with nursing and inter-professional care implications. The report also discusses self-care and community care aspects, providing a holistic overview of osteoarthritis management.

Running Head: OSTEOARTHRITIS 1
Osteoarthritis
Name
Institutional Affiliation
Osteoarthritis
Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
OSTEOATHRITIS 2
Introduction
Osteoarthritis is the most prevalent musculoskeletal disease in the world. It is a group of
heterogeneous conditions and affects primarily the articular joints. There is cartilage
deterioration in joints which leads to pain, stiffness as well as impaired movement. According to
the World Health Organization, it is the leading cause of disability in older individuals. Men
make up 9.6% of those who are 60 years and above with symptomatic Osteoarthritis globally
while women make up 18.0% of this population. It is estimated that by 2050, 20% of the global
population will be aging. Of this, 15% will have osteoarthritis (Wittenauer, Smith & Aden,
2013).The National Institute of Health and Welfare in Australia estimates that about 2.2 million
people in Australia had Osteoarthritis from 2017 to 2018. This made up 9.3% of the country’s
population. As of 2015, Osteoarthritis made up 19% of the burden from musculoskeletal
conditions in Australia. 3 out of 5 people with the disease were female (Australian Institute of
Health and Welfare, 2019). There are more men with the disease below the age of
40. Women make the bulk of those with Osteoarthritis above 50 years of age. With
improvements in healthcare and an increase of such conditions as obesity, Osteoarthritis is
expected to be a major health issue in the future in all countries. Data on Osteoarthritis is limited
by the different definitions given to the disease as well as the measures used for its study and
management. The focus of this paper will be on the causes, treatments, and diagnosis of the
disease (Xing et al., 2016).
Aetiology and pathogenesis
Osteoarthritis generally progresses slowly and might a long time before chronic symptoms
appear. Genetic, biomechanical and biological factors influence the epidemiology of the disease.
Introduction
Osteoarthritis is the most prevalent musculoskeletal disease in the world. It is a group of
heterogeneous conditions and affects primarily the articular joints. There is cartilage
deterioration in joints which leads to pain, stiffness as well as impaired movement. According to
the World Health Organization, it is the leading cause of disability in older individuals. Men
make up 9.6% of those who are 60 years and above with symptomatic Osteoarthritis globally
while women make up 18.0% of this population. It is estimated that by 2050, 20% of the global
population will be aging. Of this, 15% will have osteoarthritis (Wittenauer, Smith & Aden,
2013).The National Institute of Health and Welfare in Australia estimates that about 2.2 million
people in Australia had Osteoarthritis from 2017 to 2018. This made up 9.3% of the country’s
population. As of 2015, Osteoarthritis made up 19% of the burden from musculoskeletal
conditions in Australia. 3 out of 5 people with the disease were female (Australian Institute of
Health and Welfare, 2019). There are more men with the disease below the age of
40. Women make the bulk of those with Osteoarthritis above 50 years of age. With
improvements in healthcare and an increase of such conditions as obesity, Osteoarthritis is
expected to be a major health issue in the future in all countries. Data on Osteoarthritis is limited
by the different definitions given to the disease as well as the measures used for its study and
management. The focus of this paper will be on the causes, treatments, and diagnosis of the
disease (Xing et al., 2016).
Aetiology and pathogenesis
Osteoarthritis generally progresses slowly and might a long time before chronic symptoms
appear. Genetic, biomechanical and biological factors influence the epidemiology of the disease.
OSTEOATHRITIS 3
Osteoarthritis is classified into either primary or secondary form. The primary type is also called
the idiopathic kind. It occurs in aging individuals. There may be many causes for the disease
such as genetic predisposition. The secondary form is as a result of disease or a condition. This
changes the internal cartilage environment. The causes can be endocrine, for trauma, infection,
and congenital abnormalities or metabolic. Conditions that can lead to secondary Osteoarthritis
include Williams syndrome and gout. Despite the different etiology of the two types, the
pathology and symptoms are similar (Allen & Golightly, 2015).
Osteoarthritis can affect any joints in the body. It, however, mainly affects the joints of thumb
carpometacarpal, first metatarsophalangeal, knee, hip, zygapophyseal of the lumbar and cervical
vertebrae and proximal and distal interphalangeal joints. Articular cartilage is mostly affected. A
large number of other close tissues are also affected (periarticular tissues). The main factors that
may lead to the development of the disease are aging, obesity, increased bone density, trauma,
occupational injury, genetics, race, ethnicity, and gender (Palazzo et al.,2016).
Hyaline cartilage can be described as alymphatic, avascular and aneural. Osteoarthritis starts
through the injury of tissues through mechanical means, defects of cartilage metabolism or
inflammatory mediators. Repair then occurs. A result is that collagen and proteoglycans are
produced. Enzymes degrade the cartilage with cytokine being produced. The chondrocytes then
undergo apoptosis. Subchondral cysts develop from subchondral bone stiffening and subsequent
infarction. It is the bone repair mechanisms that lead to the development of osteophytes and
subchondral sclerosis. Synovial fluid is produced in larger quantities and is less viscous due to
synovium inflammation and thickening. The stress on ligaments and periarticular tendons lead to
contractures and tendinitis. The joint thus becomes less mobile with the muscles becoming thin
and providing less support. In the spine, posterior longitudinal ligaments proliferate and thicken
Osteoarthritis is classified into either primary or secondary form. The primary type is also called
the idiopathic kind. It occurs in aging individuals. There may be many causes for the disease
such as genetic predisposition. The secondary form is as a result of disease or a condition. This
changes the internal cartilage environment. The causes can be endocrine, for trauma, infection,
and congenital abnormalities or metabolic. Conditions that can lead to secondary Osteoarthritis
include Williams syndrome and gout. Despite the different etiology of the two types, the
pathology and symptoms are similar (Allen & Golightly, 2015).
Osteoarthritis can affect any joints in the body. It, however, mainly affects the joints of thumb
carpometacarpal, first metatarsophalangeal, knee, hip, zygapophyseal of the lumbar and cervical
vertebrae and proximal and distal interphalangeal joints. Articular cartilage is mostly affected. A
large number of other close tissues are also affected (periarticular tissues). The main factors that
may lead to the development of the disease are aging, obesity, increased bone density, trauma,
occupational injury, genetics, race, ethnicity, and gender (Palazzo et al.,2016).
Hyaline cartilage can be described as alymphatic, avascular and aneural. Osteoarthritis starts
through the injury of tissues through mechanical means, defects of cartilage metabolism or
inflammatory mediators. Repair then occurs. A result is that collagen and proteoglycans are
produced. Enzymes degrade the cartilage with cytokine being produced. The chondrocytes then
undergo apoptosis. Subchondral cysts develop from subchondral bone stiffening and subsequent
infarction. It is the bone repair mechanisms that lead to the development of osteophytes and
subchondral sclerosis. Synovial fluid is produced in larger quantities and is less viscous due to
synovium inflammation and thickening. The stress on ligaments and periarticular tendons lead to
contractures and tendinitis. The joint thus becomes less mobile with the muscles becoming thin
and providing less support. In the spine, posterior longitudinal ligaments proliferate and thicken
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
OSTEOATHRITIS 4
as a result. Transverse bars thus encroach the spinal cord. Lumbar Spinal Stenosis results from
the compression of the posterior canal due to ligamenta flava undergoing hyperplasia and
hypertrophy (Kontzias, 2018).
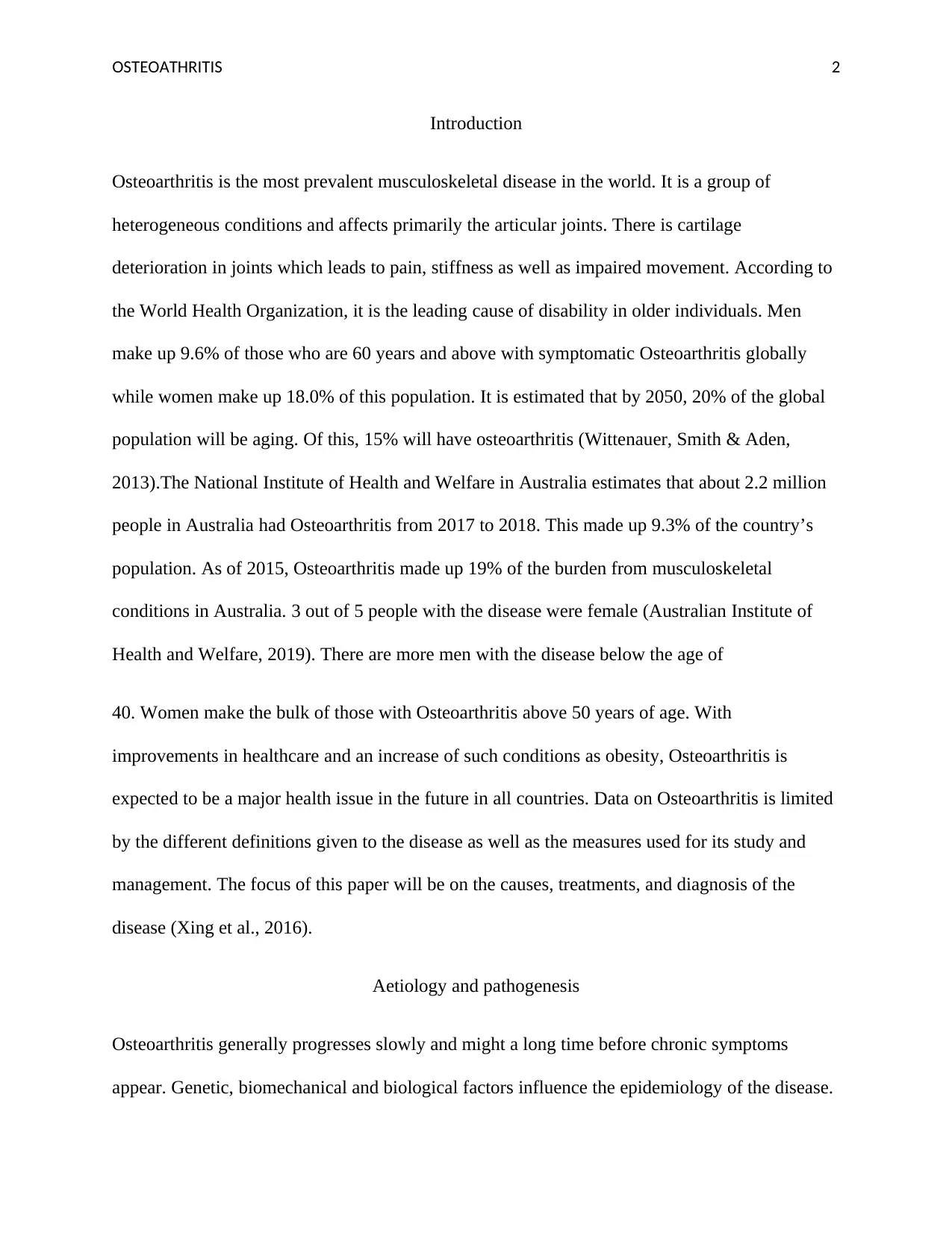
It has also been established that Inflammatory agents such as lipid derivatives, cytokines, and
reactive oxygen and nitrogen species lead to cell activation at cartilage, synovium as well as
subchondral bone. (Haseeb & Haqqi, 2013). Matrix metalloproteinases are then released which
degraded the cartilage. Higher concentrations of leptin and serum lipids levels are also linked to
osteoarthritis. The incidences of individuals with obesity having hand osteoarthritis imply
another role of obesity other than putting pressure on joints. This is through adipose tissue.
Inflammation results from nutrient overload with the production of adipokines and cytokines.
The deregulation of microRNAs results in activation of the compliment system-T lymphocytes,
B-lymphocytes and macrophages are sensitized. All this leads to tissue degradation (Wang et al.,
2015).
Besides, some loci are linked to osteoarthritis of the hip. These are VEGF and COL11A1 genes
and one close to the NCOA3 gene (nuclear receptor coactivator 3). Studies have also associated
different genes with apoptosis and pathogenesis. Individuals with parents with osteoarthritis are
more likely to develop the disease (Tsezou, 2014). It has been observed that knee pain is
prevalent or worsening of symptoms for those who have a parent who had a knee replacement.
There are other explanations offered for the development of the disease. Aging is thought to lead
to osteoarthritis through a decline of cellular mechanisms responsible for tissue homeostasis
which lowers responses to joint injury and loss, as well as stress. Thinning of cartilage, oxidative
damage, and muscle weakness are contributors to osteoarthritis in older individuals. Obesity, on
as a result. Transverse bars thus encroach the spinal cord. Lumbar Spinal Stenosis results from
the compression of the posterior canal due to ligamenta flava undergoing hyperplasia and
hypertrophy (Kontzias, 2018).
It has also been established that Inflammatory agents such as lipid derivatives, cytokines, and
reactive oxygen and nitrogen species lead to cell activation at cartilage, synovium as well as
subchondral bone. (Haseeb & Haqqi, 2013). Matrix metalloproteinases are then released which
degraded the cartilage. Higher concentrations of leptin and serum lipids levels are also linked to
osteoarthritis. The incidences of individuals with obesity having hand osteoarthritis imply
another role of obesity other than putting pressure on joints. This is through adipose tissue.
Inflammation results from nutrient overload with the production of adipokines and cytokines.
The deregulation of microRNAs results in activation of the compliment system-T lymphocytes,
B-lymphocytes and macrophages are sensitized. All this leads to tissue degradation (Wang et al.,
2015).
Besides, some loci are linked to osteoarthritis of the hip. These are VEGF and COL11A1 genes
and one close to the NCOA3 gene (nuclear receptor coactivator 3). Studies have also associated
different genes with apoptosis and pathogenesis. Individuals with parents with osteoarthritis are
more likely to develop the disease (Tsezou, 2014). It has been observed that knee pain is
prevalent or worsening of symptoms for those who have a parent who had a knee replacement.
There are other explanations offered for the development of the disease. Aging is thought to lead
to osteoarthritis through a decline of cellular mechanisms responsible for tissue homeostasis
which lowers responses to joint injury and loss, as well as stress. Thinning of cartilage, oxidative
damage, and muscle weakness are contributors to osteoarthritis in older individuals. Obesity, on
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
OSTEOATHRITIS 5
the other hand, exerts pressure on weight-bearing joints of the body such as in the knee. Normal
biomechanics and load distribution are thus disrupted (Berenbaum, Eymard& Houard, 2013).
Vascular disease may also possibly hasten or initiate osteoarthritis. This is via venous occlusion,
microemboli or Stasis. There is thus a reduced blood flow in the small vessels of subchondral
bone. The subchondral ischaemia can lead to nutrient and gas exchange reduction to the cartilage
and bone. Diabetes is also linked to osteoarthritis possibly through reactive free radicals (oxygen
species) from elevated glucose concentrations. These along with advanced end-products of
glycation lead to degradation and degeneration of cartilage. Kneeling, putting joints under stress
or injury in work-related activities has also been shown to the development of the disease.
Figure 1. Metabolic triggers of Osteoarthritis (Wang et al., 2015).
the other hand, exerts pressure on weight-bearing joints of the body such as in the knee. Normal
biomechanics and load distribution are thus disrupted (Berenbaum, Eymard& Houard, 2013).
Vascular disease may also possibly hasten or initiate osteoarthritis. This is via venous occlusion,
microemboli or Stasis. There is thus a reduced blood flow in the small vessels of subchondral
bone. The subchondral ischaemia can lead to nutrient and gas exchange reduction to the cartilage
and bone. Diabetes is also linked to osteoarthritis possibly through reactive free radicals (oxygen
species) from elevated glucose concentrations. These along with advanced end-products of
glycation lead to degradation and degeneration of cartilage. Kneeling, putting joints under stress
or injury in work-related activities has also been shown to the development of the disease.
Figure 1. Metabolic triggers of Osteoarthritis (Wang et al., 2015).
OSTEOATHRITIS 6
Osteoarthritis is thus a complex disease with multifactorial causes (Glyn-Jones et al., 2015).
Research, however, is ongoing to adopt the understanding of the pathology of the disease into
treatment methods. Patients with the disease suffer from distress and other psychological
conditions. Furthermore, the disease leads to expenses from surgery, purchase of medicine and
adaptive devices. Osteoarthritis also leads individuals to stop working. This then leads to
socioeconomic hardship. Pain and disability are the main triggers. The use of medication and
inactivity can lead to other diseases (Neogi, 2013). These include cardiovascular diseases such as
hypertension.
Clinical Manifestation
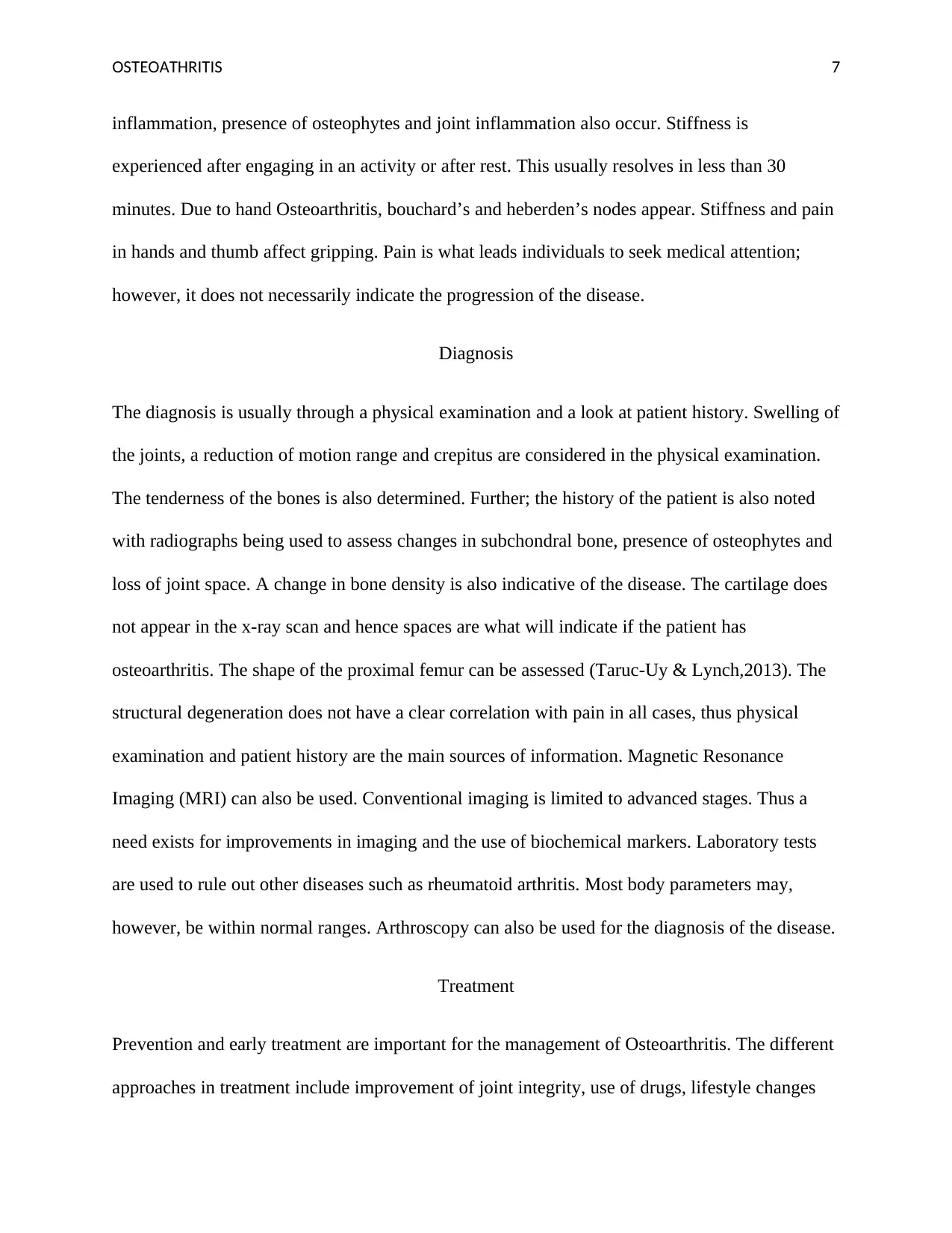
Figure 2. (Kontzias, 2018)
Common symptoms are swelling of the joints, pain, stiffness, and crepitus. Joint deformity,
subarticular bone remodeling periarticular muscle weakening, ligamentous laxity, synovial
Osteoarthritis is thus a complex disease with multifactorial causes (Glyn-Jones et al., 2015).
Research, however, is ongoing to adopt the understanding of the pathology of the disease into
treatment methods. Patients with the disease suffer from distress and other psychological
conditions. Furthermore, the disease leads to expenses from surgery, purchase of medicine and
adaptive devices. Osteoarthritis also leads individuals to stop working. This then leads to
socioeconomic hardship. Pain and disability are the main triggers. The use of medication and
inactivity can lead to other diseases (Neogi, 2013). These include cardiovascular diseases such as
hypertension.
Clinical Manifestation
Figure 2. (Kontzias, 2018)
Common symptoms are swelling of the joints, pain, stiffness, and crepitus. Joint deformity,
subarticular bone remodeling periarticular muscle weakening, ligamentous laxity, synovial
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
OSTEOATHRITIS 7
inflammation, presence of osteophytes and joint inflammation also occur. Stiffness is
experienced after engaging in an activity or after rest. This usually resolves in less than 30
minutes. Due to hand Osteoarthritis, bouchard’s and heberden’s nodes appear. Stiffness and pain
in hands and thumb affect gripping. Pain is what leads individuals to seek medical attention;
however, it does not necessarily indicate the progression of the disease.
Diagnosis
The diagnosis is usually through a physical examination and a look at patient history. Swelling of
the joints, a reduction of motion range and crepitus are considered in the physical examination.
The tenderness of the bones is also determined. Further; the history of the patient is also noted
with radiographs being used to assess changes in subchondral bone, presence of osteophytes and
loss of joint space. A change in bone density is also indicative of the disease. The cartilage does
not appear in the x-ray scan and hence spaces are what will indicate if the patient has
osteoarthritis. The shape of the proximal femur can be assessed (Taruc-Uy & Lynch,2013). The
structural degeneration does not have a clear correlation with pain in all cases, thus physical
examination and patient history are the main sources of information. Magnetic Resonance
Imaging (MRI) can also be used. Conventional imaging is limited to advanced stages. Thus a
need exists for improvements in imaging and the use of biochemical markers. Laboratory tests
are used to rule out other diseases such as rheumatoid arthritis. Most body parameters may,
however, be within normal ranges. Arthroscopy can also be used for the diagnosis of the disease.
Treatment
Prevention and early treatment are important for the management of Osteoarthritis. The different
approaches in treatment include improvement of joint integrity, use of drugs, lifestyle changes
inflammation, presence of osteophytes and joint inflammation also occur. Stiffness is
experienced after engaging in an activity or after rest. This usually resolves in less than 30
minutes. Due to hand Osteoarthritis, bouchard’s and heberden’s nodes appear. Stiffness and pain
in hands and thumb affect gripping. Pain is what leads individuals to seek medical attention;
however, it does not necessarily indicate the progression of the disease.
Diagnosis
The diagnosis is usually through a physical examination and a look at patient history. Swelling of
the joints, a reduction of motion range and crepitus are considered in the physical examination.
The tenderness of the bones is also determined. Further; the history of the patient is also noted
with radiographs being used to assess changes in subchondral bone, presence of osteophytes and
loss of joint space. A change in bone density is also indicative of the disease. The cartilage does
not appear in the x-ray scan and hence spaces are what will indicate if the patient has
osteoarthritis. The shape of the proximal femur can be assessed (Taruc-Uy & Lynch,2013). The
structural degeneration does not have a clear correlation with pain in all cases, thus physical
examination and patient history are the main sources of information. Magnetic Resonance
Imaging (MRI) can also be used. Conventional imaging is limited to advanced stages. Thus a
need exists for improvements in imaging and the use of biochemical markers. Laboratory tests
are used to rule out other diseases such as rheumatoid arthritis. Most body parameters may,
however, be within normal ranges. Arthroscopy can also be used for the diagnosis of the disease.
Treatment
Prevention and early treatment are important for the management of Osteoarthritis. The different
approaches in treatment include improvement of joint integrity, use of drugs, lifestyle changes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
OSTEOATHRITIS 8
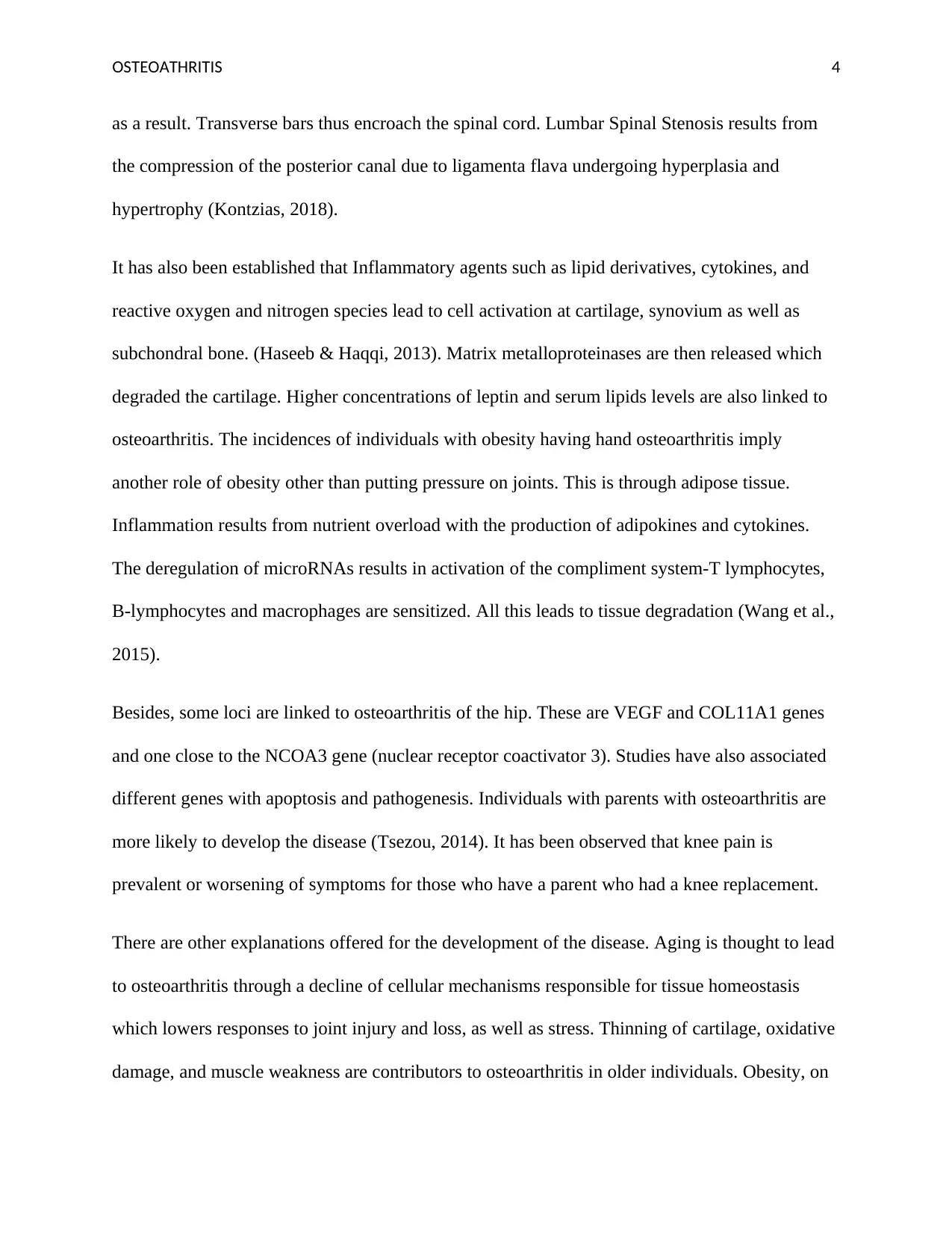
and surgery. There is currently no cure for Osteoarthritis. The goals of treatment are alleviation
of symptoms and improvement of functional status. Symptom severity is varied with pain being
the main issue. The duration of the disease is also considered in treatment.
Physical activity, splints, acupuncture, and nerve stimulation are used for management. A
healthy diet is usually adopted which allows weight loss. The management of obesity helps
relieve pressure on weight-bearing joints, reduce inflammation and enhance the general health of
the patient. Occupational injuries are also addressed to resolve pain and impairment.
Physiotherapy is usually adopted for mild cases. There is also the use of orthotics, braces and
appropriate footwear. Individuals can also be trained in coping as well as make use of self-
management initiatives (Fransen et al., 2015).
Drugs are administered in a stepwise manner. These include acetaminophen, topical capsaicin,
inhibitors of cyclooxygenase -2 and anti-inflammatories that are not steroidal. Steroids can be
administered as injections intra-articularly. Topical capsaicin is used when dealing with
superficial joints and is used three or four times daily, with the effects occurring after some
weeks. Duloxetine is used for moderate pain relief. Intra-articular injections either hyaluronate or
corticosteroid are used in some cases. Lubrication injections are also used. Corticosteroids
provide pain relief for about 6 months. Acetaminophen (paracetamol) is used for mild and at
times moderate pain. This is usually two tablets every eight hours. There are both long term and
short term side effects but can be used up to four times a day. Non-steroidal medications like
Ibuprofen, naproxen, and aspirin which are also anti-inflammatory are more efficacious.
Diclofenac is given as 150mg daily and is shown to be more effective. However, they have
adverse effects on the gastrointestinal tract and have more toxicity. Ibuprofen, for instance, can
cause kidney and liver problems, fluid retention and raised blood pressure. Other NSAIDS drugs
and surgery. There is currently no cure for Osteoarthritis. The goals of treatment are alleviation
of symptoms and improvement of functional status. Symptom severity is varied with pain being
the main issue. The duration of the disease is also considered in treatment.
Physical activity, splints, acupuncture, and nerve stimulation are used for management. A
healthy diet is usually adopted which allows weight loss. The management of obesity helps
relieve pressure on weight-bearing joints, reduce inflammation and enhance the general health of
the patient. Occupational injuries are also addressed to resolve pain and impairment.
Physiotherapy is usually adopted for mild cases. There is also the use of orthotics, braces and
appropriate footwear. Individuals can also be trained in coping as well as make use of self-
management initiatives (Fransen et al., 2015).
Drugs are administered in a stepwise manner. These include acetaminophen, topical capsaicin,
inhibitors of cyclooxygenase -2 and anti-inflammatories that are not steroidal. Steroids can be
administered as injections intra-articularly. Topical capsaicin is used when dealing with
superficial joints and is used three or four times daily, with the effects occurring after some
weeks. Duloxetine is used for moderate pain relief. Intra-articular injections either hyaluronate or
corticosteroid are used in some cases. Lubrication injections are also used. Corticosteroids
provide pain relief for about 6 months. Acetaminophen (paracetamol) is used for mild and at
times moderate pain. This is usually two tablets every eight hours. There are both long term and
short term side effects but can be used up to four times a day. Non-steroidal medications like
Ibuprofen, naproxen, and aspirin which are also anti-inflammatory are more efficacious.
Diclofenac is given as 150mg daily and is shown to be more effective. However, they have
adverse effects on the gastrointestinal tract and have more toxicity. Ibuprofen, for instance, can
cause kidney and liver problems, fluid retention and raised blood pressure. Other NSAIDS drugs

OSTEOATHRITIS 9
could result in bleeding, kidney and liver disorders. A combination with a protectant of the
gastrointestinal tract is used. Opioids and tramadol are used for greater pain control. Tramadol is
given as 400 mg dose daily, usually 50 to 100 mg every 6 hours. Opioids have the potential for
abuse and can lead to respiratory depression as well as nausea, itching, and constipation.
Diacerein, glucosamine S-Adenosylmethionine need more analysis of their effectiveness. The
use of avocado-soybean unsaponifiables is largely effective but more studies also need to carry
out. A review indicated that viscosupplementation was not a recommended therapy.
Surgery to replace the affected joints is used when the diseases are chronic and upon failure of
drugs or non-pharmacological therapies. It can be arthroplasty, arthroscopy or fusion and joint
lavage procedures. Chondrocyte implants, osteochondral grafts, and microfractures are also used.
Implants, however, have poor functional outcomes and limited duration of the prostheses. Joint
replacement takes place in the late stages. Stem cell implants are being proposed but these are
yet to be used in clinical settings (Sierra et al., 2015). The use of these strategies to limit the
progression of the disease through delay or arrest has had little success. Joint replacement is
currently the most effective means of treatment.
Figure3. Hierarchy of treatment. (Wittenauer, Smith & Aden, 2013)
could result in bleeding, kidney and liver disorders. A combination with a protectant of the
gastrointestinal tract is used. Opioids and tramadol are used for greater pain control. Tramadol is
given as 400 mg dose daily, usually 50 to 100 mg every 6 hours. Opioids have the potential for
abuse and can lead to respiratory depression as well as nausea, itching, and constipation.
Diacerein, glucosamine S-Adenosylmethionine need more analysis of their effectiveness. The
use of avocado-soybean unsaponifiables is largely effective but more studies also need to carry
out. A review indicated that viscosupplementation was not a recommended therapy.
Surgery to replace the affected joints is used when the diseases are chronic and upon failure of
drugs or non-pharmacological therapies. It can be arthroplasty, arthroscopy or fusion and joint
lavage procedures. Chondrocyte implants, osteochondral grafts, and microfractures are also used.
Implants, however, have poor functional outcomes and limited duration of the prostheses. Joint
replacement takes place in the late stages. Stem cell implants are being proposed but these are
yet to be used in clinical settings (Sierra et al., 2015). The use of these strategies to limit the
progression of the disease through delay or arrest has had little success. Joint replacement is
currently the most effective means of treatment.
Figure3. Hierarchy of treatment. (Wittenauer, Smith & Aden, 2013)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
OSTEOATHRITIS 10
Patients will need education on how to cope with the symptoms. The plans of care must take
into consideration pain relief and ensuring the optimal condition of the joints. Deterioration of
symptoms should also be avoided or managed. The psychological distress of the patient is also to
be reduced. The patient may not have the ability to carry out necessary activities such as self-
care and working. It is this crucial to prevent the disease through education of patients, early
diagnosis and referrals of patients to services like physiotherapy to allow for recovery. The social
support system needs to be strengthened. Thus close family members need to be involved and
educated as well (Litwic et al., 2013).
Conclusion
There is a need for further research into the epidemiology, etiology, diagnosis, and treatment of
Osteoarthritis. The disease is the most prevalent disease affecting the joints. Obesity, genetic
variations, trauma, and aging processes contribute to the development of the disease. There are,
however, treatment options available that are aided by imaging, evaluation of patient history and
physical exams. These treatments include surgery, pharmacological approaches, exercise, and
physical therapy.
Patients will need education on how to cope with the symptoms. The plans of care must take
into consideration pain relief and ensuring the optimal condition of the joints. Deterioration of
symptoms should also be avoided or managed. The psychological distress of the patient is also to
be reduced. The patient may not have the ability to carry out necessary activities such as self-
care and working. It is this crucial to prevent the disease through education of patients, early
diagnosis and referrals of patients to services like physiotherapy to allow for recovery. The social
support system needs to be strengthened. Thus close family members need to be involved and
educated as well (Litwic et al., 2013).
Conclusion
There is a need for further research into the epidemiology, etiology, diagnosis, and treatment of
Osteoarthritis. The disease is the most prevalent disease affecting the joints. Obesity, genetic
variations, trauma, and aging processes contribute to the development of the disease. There are,
however, treatment options available that are aided by imaging, evaluation of patient history and
physical exams. These treatments include surgery, pharmacological approaches, exercise, and
physical therapy.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
OSTEOATHRITIS 11
References
Allen, K. D., & Golightly, Y. M. (2015). Epidemiology of osteoarthritis: State of the evidence.
Current Opinion in Rheumatology, 27(3), 276-283.
Australian Institute of Health and Welfare. (2019, August 30). Osteoarthritis. Retrieved April 18,
2020, from https://www.aihw.gov.au/reports/chronic-musculoskeletal
conditions/osteoarthritis/contents/impact-of-osteoarthritis
Berenbaum, F., Eymard, F., & Houard, X. (2013). Osteoarthritis, inflammation, and obesity.
Current Opinion in Rheumatology, 25(1), 114-118.
Fransen, M., McConnell, S., Harmer, A. R., Van der Esch, M., Simic, M., & Bennell, K. L.
(2015). Exercise for osteoarthritis of the knee. Cochrane Database of Systematic
Reviews.
Glyn-Jones, S., Palmer, A. J., Agricola, R., Price, A. J., Vincent, T. L., Weinans, H., & Carr, A.
J. (2015). Osteoarthritis. The Lancet, 386(9991), 376-387.
Haseeb, A., & Haqqi, T. M. (2013). Immunopathogenesis of osteoarthritis. Clinical Immunology,
146(3), 185-196.
Kontzias, A. (2018). Osteoarthritis (OA)-Musculoskeletal and Connective Tissue Disorders-
MSD Manual Professional Edition. Retrieved April 18, 2020, from
https://www.msdmanuals.com/professional/musculoskeletal-and-connective-tissue-
disorders/joint-disorders/osteoarthritis-oa)
Litwic, A., Edwards, M. H., Dennison, E. M., & Cooper, C. (2013). Epidemiology and burden of
osteoarthritis. British Medical Bulletin, 105(1), 185-199.
References
Allen, K. D., & Golightly, Y. M. (2015). Epidemiology of osteoarthritis: State of the evidence.
Current Opinion in Rheumatology, 27(3), 276-283.
Australian Institute of Health and Welfare. (2019, August 30). Osteoarthritis. Retrieved April 18,
2020, from https://www.aihw.gov.au/reports/chronic-musculoskeletal
conditions/osteoarthritis/contents/impact-of-osteoarthritis
Berenbaum, F., Eymard, F., & Houard, X. (2013). Osteoarthritis, inflammation, and obesity.
Current Opinion in Rheumatology, 25(1), 114-118.
Fransen, M., McConnell, S., Harmer, A. R., Van der Esch, M., Simic, M., & Bennell, K. L.
(2015). Exercise for osteoarthritis of the knee. Cochrane Database of Systematic
Reviews.
Glyn-Jones, S., Palmer, A. J., Agricola, R., Price, A. J., Vincent, T. L., Weinans, H., & Carr, A.
J. (2015). Osteoarthritis. The Lancet, 386(9991), 376-387.
Haseeb, A., & Haqqi, T. M. (2013). Immunopathogenesis of osteoarthritis. Clinical Immunology,
146(3), 185-196.
Kontzias, A. (2018). Osteoarthritis (OA)-Musculoskeletal and Connective Tissue Disorders-
MSD Manual Professional Edition. Retrieved April 18, 2020, from
https://www.msdmanuals.com/professional/musculoskeletal-and-connective-tissue-
disorders/joint-disorders/osteoarthritis-oa)
Litwic, A., Edwards, M. H., Dennison, E. M., & Cooper, C. (2013). Epidemiology and burden of
osteoarthritis. British Medical Bulletin, 105(1), 185-199.
OSTEOATHRITIS 12
Neogi, T. (2013). The epidemiology and impact of pain in osteoarthritis. Osteoarthritis and
Cartilage, 21(9), 1145-1153.
Palazzo, C., Nguyen, C., Lefevre-Colau, M., Rannou, F., & Poiraudeau, S. (2016). Risk factors
and burden of osteoarthritis. Annals of Physical and Rehabilitation Medicine, 59(3), 134-
138.
Sierra, R., Wyles, C., Houdek, M., & Behfar, A. (2015). Mesenchymal stem cell therapy for
osteoarthritis: Current perspectives. Stem Cells and Cloning: Advances and Applications,
8(2015), 117.
Taruc-Uy, R. L., & Lynch, S. A. (2013). Diagnosis and Treatment of Osteoarthritis. Primary
Care: Clinics in Office Practice, 40(4), 821-836.
Tsezou, A. (2014). Genetics/genomics in osteoarthritis. Osteoarthritis and Cartilage, 22, S4-S5.
Wang, X., Hunter, D., Xu, J., & Ding, C. (2015). Metabolic triggered inflammation in
osteoarthritis. Osteoarthritis and Cartilage, 23(1), 22-30.
Wittenauer R., Smith L., & Aden K. (2013, January 28). Update on 2004 Background Paper, BP
6.12 Osteoarthritis. Retrieved from
https://www.who.int/medicines/areas/priority_medicines/Ch6_12Osteo.pdf
Xing, D., Xu, Y., Liu, Q., Ke, Y., Wang, B., Li, Z., & Lin, J. (2016). Osteoarthritis and all-cause
mortality in worldwide populations: grading the evidence from a meta-analysis. Scientific
Reports, 6(1).
Neogi, T. (2013). The epidemiology and impact of pain in osteoarthritis. Osteoarthritis and
Cartilage, 21(9), 1145-1153.
Palazzo, C., Nguyen, C., Lefevre-Colau, M., Rannou, F., & Poiraudeau, S. (2016). Risk factors
and burden of osteoarthritis. Annals of Physical and Rehabilitation Medicine, 59(3), 134-
138.
Sierra, R., Wyles, C., Houdek, M., & Behfar, A. (2015). Mesenchymal stem cell therapy for
osteoarthritis: Current perspectives. Stem Cells and Cloning: Advances and Applications,
8(2015), 117.
Taruc-Uy, R. L., & Lynch, S. A. (2013). Diagnosis and Treatment of Osteoarthritis. Primary
Care: Clinics in Office Practice, 40(4), 821-836.
Tsezou, A. (2014). Genetics/genomics in osteoarthritis. Osteoarthritis and Cartilage, 22, S4-S5.
Wang, X., Hunter, D., Xu, J., & Ding, C. (2015). Metabolic triggered inflammation in
osteoarthritis. Osteoarthritis and Cartilage, 23(1), 22-30.
Wittenauer R., Smith L., & Aden K. (2013, January 28). Update on 2004 Background Paper, BP
6.12 Osteoarthritis. Retrieved from
https://www.who.int/medicines/areas/priority_medicines/Ch6_12Osteo.pdf
Xing, D., Xu, Y., Liu, Q., Ke, Y., Wang, B., Li, Z., & Lin, J. (2016). Osteoarthritis and all-cause
mortality in worldwide populations: grading the evidence from a meta-analysis. Scientific
Reports, 6(1).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





