Comprehensive Nursing Report: CRC, SMART Goals for Osteoporosis Care
VerifiedAdded on 2022/10/03
|9
|2216
|30
Report
AI Summary
This report presents a comprehensive analysis of a nursing case study involving a 75-year-old patient with osteoporosis, hypertension, and a history of depression. The report meticulously follows the Clinical Reasoning Cycle (CRC) to address the patient's needs. It begins by identifying key issues such as osteoporosis, low blood pressure, and pain, followed by the establishment of Specific, Measurable, Achievable, Relevant, and Time-bound (SMART) goals. These goals focus on reducing fall risk, pain relief, addressing body image concerns, minimizing fracture risk, and addressing knowledge deficits. The report then details the nursing interventions implemented, including assessments, repositioning, medication, dietary adjustments, and recreational activities, along with the rationale behind each intervention. Finally, the report evaluates the expected patient outcomes, such as improved knowledge, increased blood pressure, pain management, and enhanced social engagement, alongside a reflection on the learning experience. The references used in this report provide evidence-based support for the nursing interventions and care provided.

1
Title:
Student’s name:
Student’s id:
Title:
Student’s name:
Student’s id:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
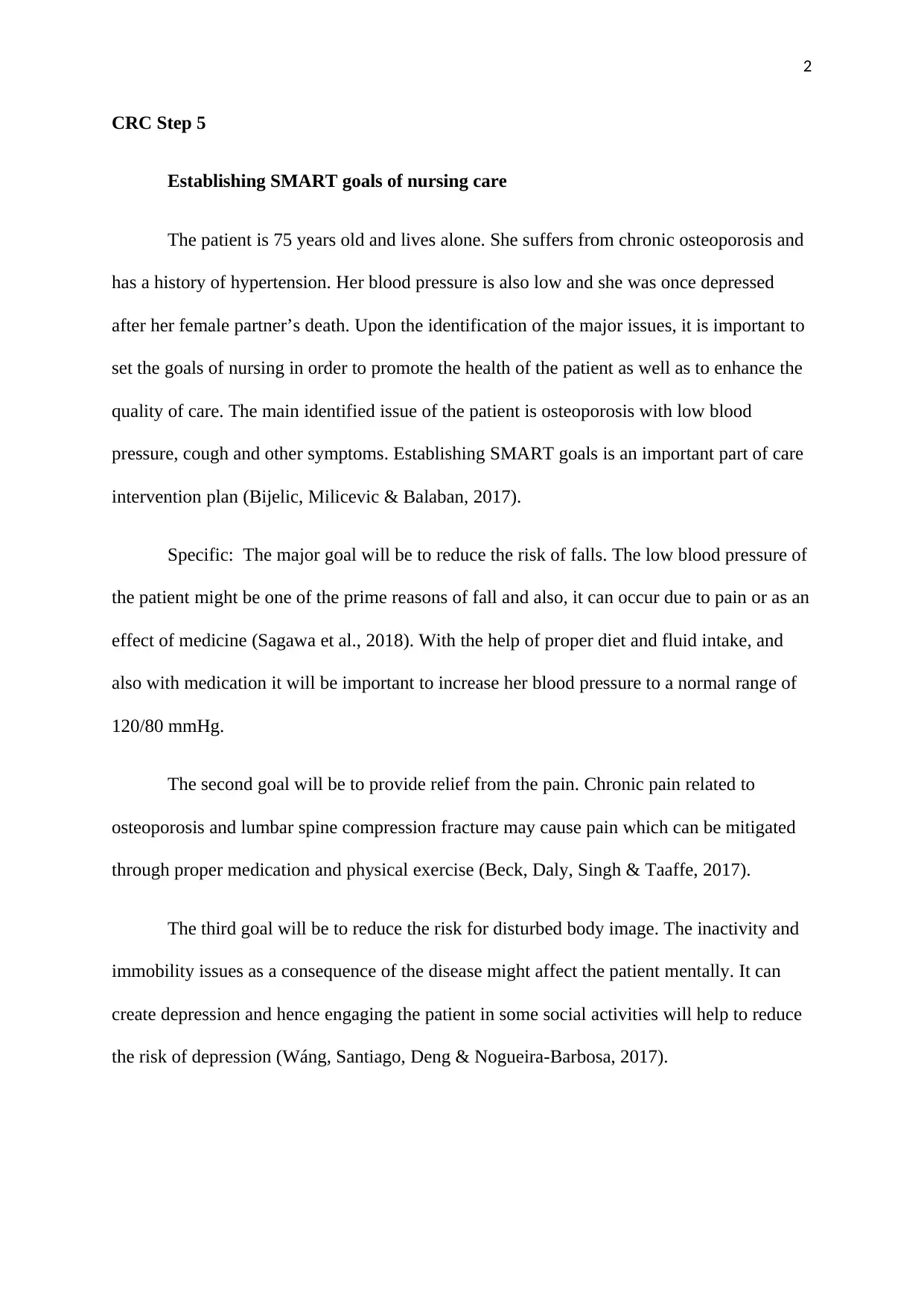
CRC Step 5
Establishing SMART goals of nursing care
The patient is 75 years old and lives alone. She suffers from chronic osteoporosis and
has a history of hypertension. Her blood pressure is also low and she was once depressed
after her female partner’s death. Upon the identification of the major issues, it is important to
set the goals of nursing in order to promote the health of the patient as well as to enhance the
quality of care. The main identified issue of the patient is osteoporosis with low blood
pressure, cough and other symptoms. Establishing SMART goals is an important part of care
intervention plan (Bijelic, Milicevic & Balaban, 2017).
Specific: The major goal will be to reduce the risk of falls. The low blood pressure of
the patient might be one of the prime reasons of fall and also, it can occur due to pain or as an
effect of medicine (Sagawa et al., 2018). With the help of proper diet and fluid intake, and
also with medication it will be important to increase her blood pressure to a normal range of
120/80 mmHg.
The second goal will be to provide relief from the pain. Chronic pain related to
osteoporosis and lumbar spine compression fracture may cause pain which can be mitigated
through proper medication and physical exercise (Beck, Daly, Singh & Taaffe, 2017).
The third goal will be to reduce the risk for disturbed body image. The inactivity and
immobility issues as a consequence of the disease might affect the patient mentally. It can
create depression and hence engaging the patient in some social activities will help to reduce
the risk of depression (Wáng, Santiago, Deng & Nogueira-Barbosa, 2017).
CRC Step 5
Establishing SMART goals of nursing care
The patient is 75 years old and lives alone. She suffers from chronic osteoporosis and
has a history of hypertension. Her blood pressure is also low and she was once depressed
after her female partner’s death. Upon the identification of the major issues, it is important to
set the goals of nursing in order to promote the health of the patient as well as to enhance the
quality of care. The main identified issue of the patient is osteoporosis with low blood
pressure, cough and other symptoms. Establishing SMART goals is an important part of care
intervention plan (Bijelic, Milicevic & Balaban, 2017).
Specific: The major goal will be to reduce the risk of falls. The low blood pressure of
the patient might be one of the prime reasons of fall and also, it can occur due to pain or as an
effect of medicine (Sagawa et al., 2018). With the help of proper diet and fluid intake, and
also with medication it will be important to increase her blood pressure to a normal range of
120/80 mmHg.
The second goal will be to provide relief from the pain. Chronic pain related to
osteoporosis and lumbar spine compression fracture may cause pain which can be mitigated
through proper medication and physical exercise (Beck, Daly, Singh & Taaffe, 2017).
The third goal will be to reduce the risk for disturbed body image. The inactivity and
immobility issues as a consequence of the disease might affect the patient mentally. It can
create depression and hence engaging the patient in some social activities will help to reduce
the risk of depression (Wáng, Santiago, Deng & Nogueira-Barbosa, 2017).
3
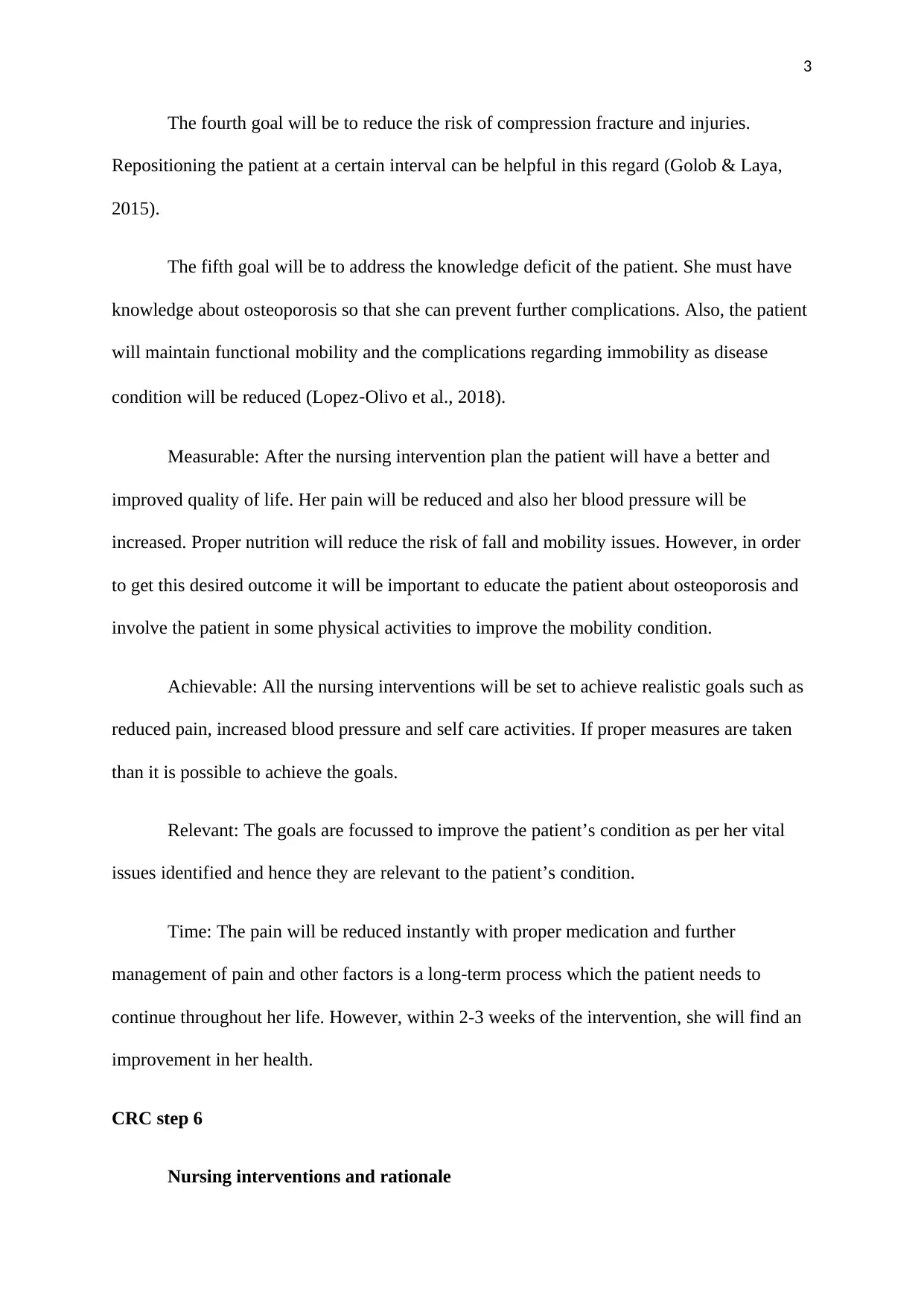
The fourth goal will be to reduce the risk of compression fracture and injuries.
Repositioning the patient at a certain interval can be helpful in this regard (Golob & Laya,
2015).
The fifth goal will be to address the knowledge deficit of the patient. She must have
knowledge about osteoporosis so that she can prevent further complications. Also, the patient
will maintain functional mobility and the complications regarding immobility as disease
condition will be reduced (Lopez‐Olivo et al., 2018).
Measurable: After the nursing intervention plan the patient will have a better and
improved quality of life. Her pain will be reduced and also her blood pressure will be
increased. Proper nutrition will reduce the risk of fall and mobility issues. However, in order
to get this desired outcome it will be important to educate the patient about osteoporosis and
involve the patient in some physical activities to improve the mobility condition.
Achievable: All the nursing interventions will be set to achieve realistic goals such as
reduced pain, increased blood pressure and self care activities. If proper measures are taken
than it is possible to achieve the goals.
Relevant: The goals are focussed to improve the patient’s condition as per her vital
issues identified and hence they are relevant to the patient’s condition.
Time: The pain will be reduced instantly with proper medication and further
management of pain and other factors is a long-term process which the patient needs to
continue throughout her life. However, within 2-3 weeks of the intervention, she will find an
improvement in her health.
CRC step 6
Nursing interventions and rationale
The fourth goal will be to reduce the risk of compression fracture and injuries.
Repositioning the patient at a certain interval can be helpful in this regard (Golob & Laya,
2015).
The fifth goal will be to address the knowledge deficit of the patient. She must have
knowledge about osteoporosis so that she can prevent further complications. Also, the patient
will maintain functional mobility and the complications regarding immobility as disease
condition will be reduced (Lopez‐Olivo et al., 2018).
Measurable: After the nursing intervention plan the patient will have a better and
improved quality of life. Her pain will be reduced and also her blood pressure will be
increased. Proper nutrition will reduce the risk of fall and mobility issues. However, in order
to get this desired outcome it will be important to educate the patient about osteoporosis and
involve the patient in some physical activities to improve the mobility condition.
Achievable: All the nursing interventions will be set to achieve realistic goals such as
reduced pain, increased blood pressure and self care activities. If proper measures are taken
than it is possible to achieve the goals.
Relevant: The goals are focussed to improve the patient’s condition as per her vital
issues identified and hence they are relevant to the patient’s condition.
Time: The pain will be reduced instantly with proper medication and further
management of pain and other factors is a long-term process which the patient needs to
continue throughout her life. However, within 2-3 weeks of the intervention, she will find an
improvement in her health.
CRC step 6
Nursing interventions and rationale
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
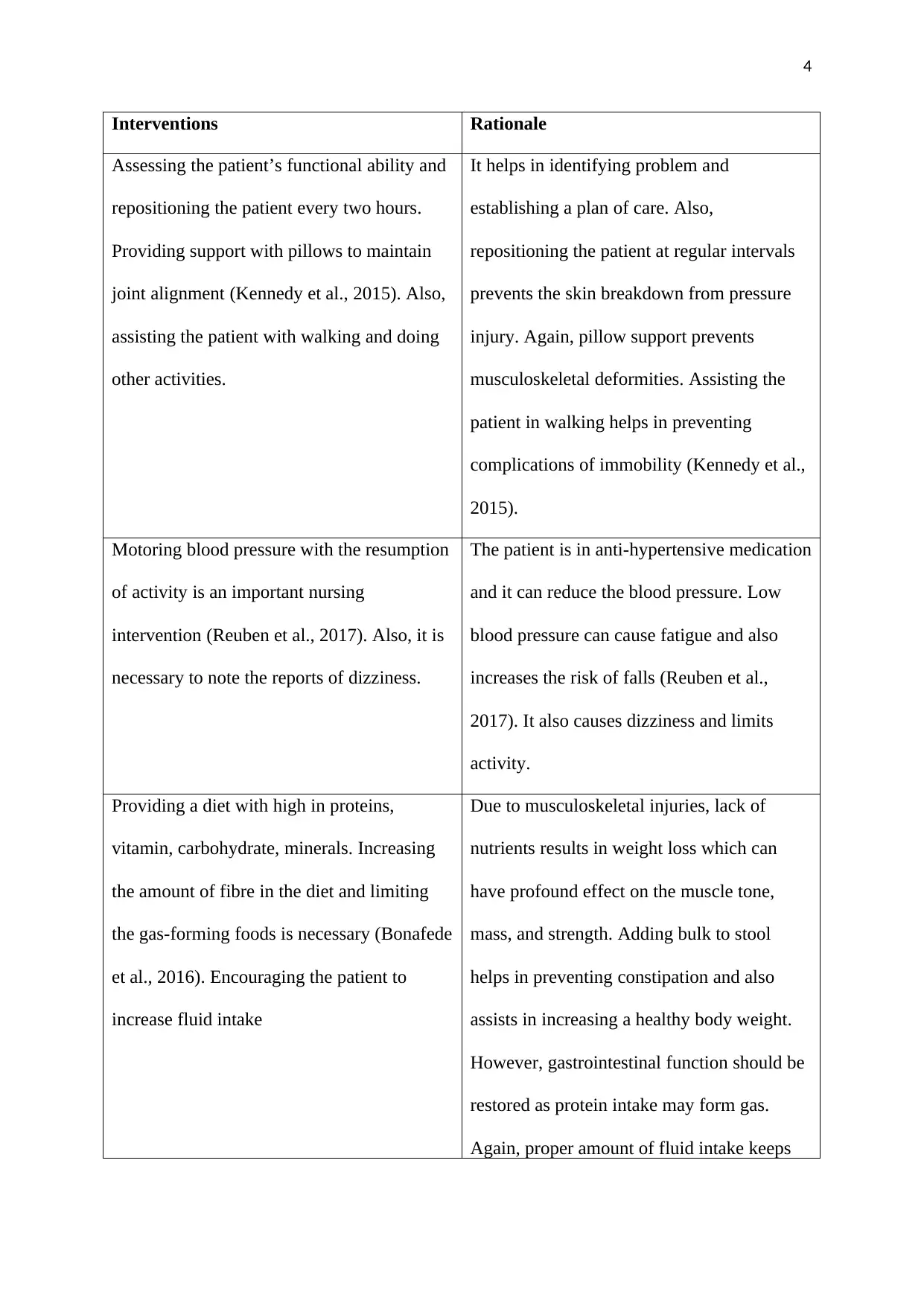
Interventions Rationale
Assessing the patient’s functional ability and
repositioning the patient every two hours.
Providing support with pillows to maintain
joint alignment (Kennedy et al., 2015). Also,
assisting the patient with walking and doing
other activities.
It helps in identifying problem and
establishing a plan of care. Also,
repositioning the patient at regular intervals
prevents the skin breakdown from pressure
injury. Again, pillow support prevents
musculoskeletal deformities. Assisting the
patient in walking helps in preventing
complications of immobility (Kennedy et al.,
2015).
Motoring blood pressure with the resumption
of activity is an important nursing
intervention (Reuben et al., 2017). Also, it is
necessary to note the reports of dizziness.
The patient is in anti-hypertensive medication
and it can reduce the blood pressure. Low
blood pressure can cause fatigue and also
increases the risk of falls (Reuben et al.,
2017). It also causes dizziness and limits
activity.
Providing a diet with high in proteins,
vitamin, carbohydrate, minerals. Increasing
the amount of fibre in the diet and limiting
the gas-forming foods is necessary (Bonafede
et al., 2016). Encouraging the patient to
increase fluid intake
Due to musculoskeletal injuries, lack of
nutrients results in weight loss which can
have profound effect on the muscle tone,
mass, and strength. Adding bulk to stool
helps in preventing constipation and also
assists in increasing a healthy body weight.
However, gastrointestinal function should be
restored as protein intake may form gas.
Again, proper amount of fluid intake keeps
Interventions Rationale
Assessing the patient’s functional ability and
repositioning the patient every two hours.
Providing support with pillows to maintain
joint alignment (Kennedy et al., 2015). Also,
assisting the patient with walking and doing
other activities.
It helps in identifying problem and
establishing a plan of care. Also,
repositioning the patient at regular intervals
prevents the skin breakdown from pressure
injury. Again, pillow support prevents
musculoskeletal deformities. Assisting the
patient in walking helps in preventing
complications of immobility (Kennedy et al.,
2015).
Motoring blood pressure with the resumption
of activity is an important nursing
intervention (Reuben et al., 2017). Also, it is
necessary to note the reports of dizziness.
The patient is in anti-hypertensive medication
and it can reduce the blood pressure. Low
blood pressure can cause fatigue and also
increases the risk of falls (Reuben et al.,
2017). It also causes dizziness and limits
activity.
Providing a diet with high in proteins,
vitamin, carbohydrate, minerals. Increasing
the amount of fibre in the diet and limiting
the gas-forming foods is necessary (Bonafede
et al., 2016). Encouraging the patient to
increase fluid intake
Due to musculoskeletal injuries, lack of
nutrients results in weight loss which can
have profound effect on the muscle tone,
mass, and strength. Adding bulk to stool
helps in preventing constipation and also
assists in increasing a healthy body weight.
However, gastrointestinal function should be
restored as protein intake may form gas.
Again, proper amount of fluid intake keeps
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
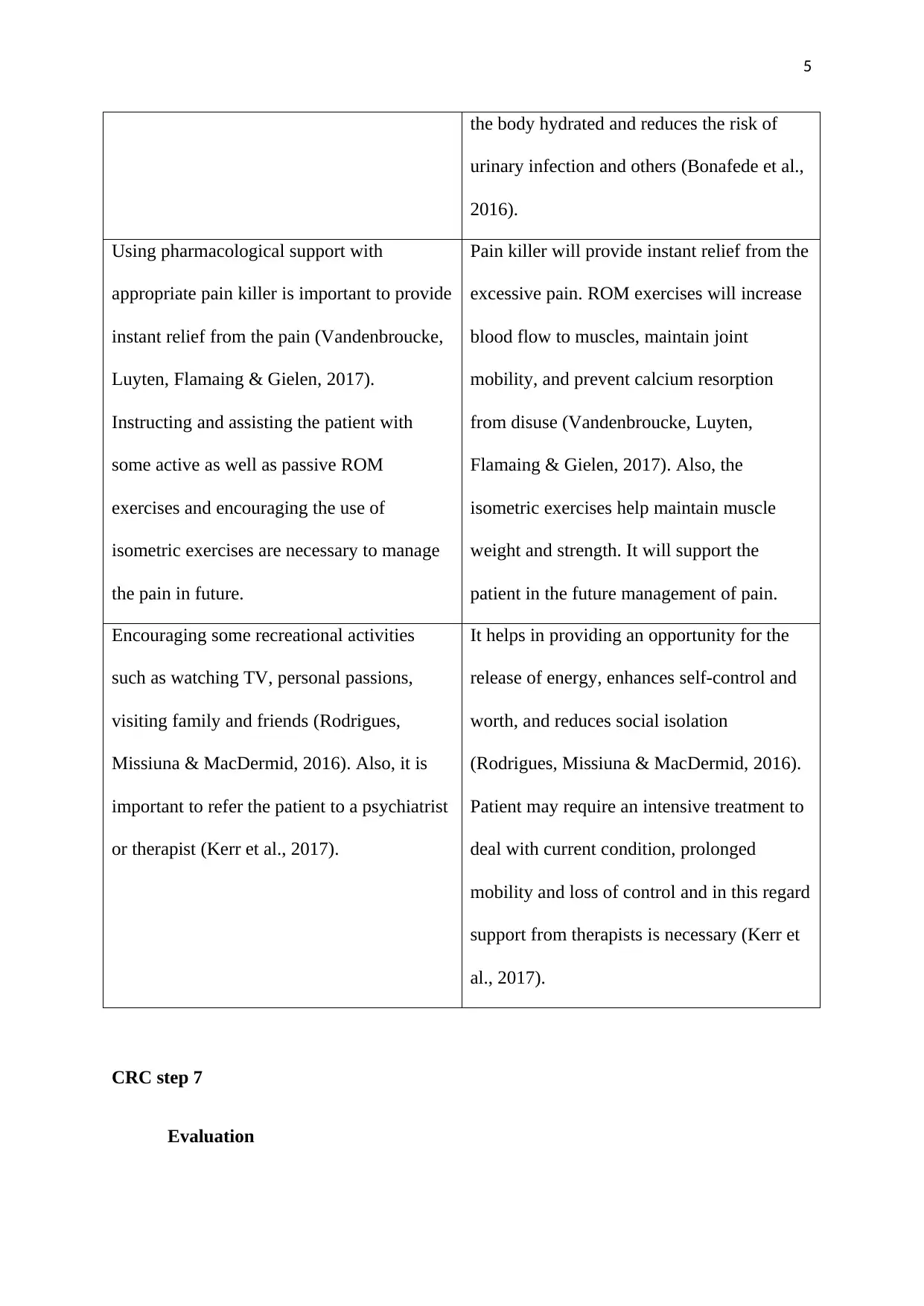
the body hydrated and reduces the risk of
urinary infection and others (Bonafede et al.,
2016).
Using pharmacological support with
appropriate pain killer is important to provide
instant relief from the pain (Vandenbroucke,
Luyten, Flamaing & Gielen, 2017).
Instructing and assisting the patient with
some active as well as passive ROM
exercises and encouraging the use of
isometric exercises are necessary to manage
the pain in future.
Pain killer will provide instant relief from the
excessive pain. ROM exercises will increase
blood flow to muscles, maintain joint
mobility, and prevent calcium resorption
from disuse (Vandenbroucke, Luyten,
Flamaing & Gielen, 2017). Also, the
isometric exercises help maintain muscle
weight and strength. It will support the
patient in the future management of pain.
Encouraging some recreational activities
such as watching TV, personal passions,
visiting family and friends (Rodrigues,
Missiuna & MacDermid, 2016). Also, it is
important to refer the patient to a psychiatrist
or therapist (Kerr et al., 2017).
It helps in providing an opportunity for the
release of energy, enhances self-control and
worth, and reduces social isolation
(Rodrigues, Missiuna & MacDermid, 2016).
Patient may require an intensive treatment to
deal with current condition, prolonged
mobility and loss of control and in this regard
support from therapists is necessary (Kerr et
al., 2017).
CRC step 7
Evaluation
the body hydrated and reduces the risk of
urinary infection and others (Bonafede et al.,
2016).
Using pharmacological support with
appropriate pain killer is important to provide
instant relief from the pain (Vandenbroucke,
Luyten, Flamaing & Gielen, 2017).
Instructing and assisting the patient with
some active as well as passive ROM
exercises and encouraging the use of
isometric exercises are necessary to manage
the pain in future.
Pain killer will provide instant relief from the
excessive pain. ROM exercises will increase
blood flow to muscles, maintain joint
mobility, and prevent calcium resorption
from disuse (Vandenbroucke, Luyten,
Flamaing & Gielen, 2017). Also, the
isometric exercises help maintain muscle
weight and strength. It will support the
patient in the future management of pain.
Encouraging some recreational activities
such as watching TV, personal passions,
visiting family and friends (Rodrigues,
Missiuna & MacDermid, 2016). Also, it is
important to refer the patient to a psychiatrist
or therapist (Kerr et al., 2017).
It helps in providing an opportunity for the
release of energy, enhances self-control and
worth, and reduces social isolation
(Rodrigues, Missiuna & MacDermid, 2016).
Patient may require an intensive treatment to
deal with current condition, prolonged
mobility and loss of control and in this regard
support from therapists is necessary (Kerr et
al., 2017).
CRC step 7
Evaluation
6
Upon the successful implementation of the nursing interventions, the patient’s desired
condition can be evaluated. Expected patient’s outcome may include some important
improvements. The patient will acquire a clear knowledge about osteoporosis and its self-
management techniques. Also, the patient’s body weight and blood pressure will be increased
which will provide additional muscles strength and support to the mobility (Smart, Dermody,
Coronado & Wilson, 2018). The intervention plans will help the patient in managing pain in
future. Also, she will be able to engage herself in some social activities to increase her mental
support. Consultation with the therapists will help in gaining moral support in her physical
condition.
CRC step 8
Reflection
Being a nurse, I need to face lost of situations daily and all help me in gaining more
knowledge about my profession. After the completion of this clinical reasoning cycle on the
case study of a patient with osteoporosis, I learned a lot of new things about my practice.
However, initially I was nervous and I felt issues while assessing the vital signs and making
nursing intervention plans due to lack of experience. But later on, I became confident and
applied my theoretical knowledge in handling the patient’s issue. I learned that repositioning
the patient after a certain interval is highly necessary in order to avoid compression injuries.
Also, I realized that physical injuries may create mental instability and patient might become
depressed which requires additional mental support. However, it was a learning opportunity
for me but I also felt, things could have been better if I could overcome my nervousness. But,
I think I will able to overcome all the issues after gaining experience in this field. In future, I
will also take support from the seniors if required.
Upon the successful implementation of the nursing interventions, the patient’s desired
condition can be evaluated. Expected patient’s outcome may include some important
improvements. The patient will acquire a clear knowledge about osteoporosis and its self-
management techniques. Also, the patient’s body weight and blood pressure will be increased
which will provide additional muscles strength and support to the mobility (Smart, Dermody,
Coronado & Wilson, 2018). The intervention plans will help the patient in managing pain in
future. Also, she will be able to engage herself in some social activities to increase her mental
support. Consultation with the therapists will help in gaining moral support in her physical
condition.
CRC step 8
Reflection
Being a nurse, I need to face lost of situations daily and all help me in gaining more
knowledge about my profession. After the completion of this clinical reasoning cycle on the
case study of a patient with osteoporosis, I learned a lot of new things about my practice.
However, initially I was nervous and I felt issues while assessing the vital signs and making
nursing intervention plans due to lack of experience. But later on, I became confident and
applied my theoretical knowledge in handling the patient’s issue. I learned that repositioning
the patient after a certain interval is highly necessary in order to avoid compression injuries.
Also, I realized that physical injuries may create mental instability and patient might become
depressed which requires additional mental support. However, it was a learning opportunity
for me but I also felt, things could have been better if I could overcome my nervousness. But,
I think I will able to overcome all the issues after gaining experience in this field. In future, I
will also take support from the seniors if required.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
References
Beck, B. R., Daly, R. M., Singh, M. A. F., & Taaffe, D. R. (2017). Exercise and Sports
Science Australia (ESSA) position statement on exercise prescription for the
prevention and management of osteoporosis. Journal of science and medicine in
sport, 20(5), 438-445.
Bijelic, R., Milicevic, S., & Balaban, J. (2017). Risk factors for osteoporosis in
postmenopausal women. Medical Archives, 71(1), 25.
Bonafede, M., Shi, N., Barron, R., Li, X., Crittenden, D. B., & Chandler, D. (2016).
Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis
using US claims data. Archives of osteoporosis, 11(1), 26.
Golob, A. L., & Laya, M. B. (2015). Osteoporosis: screening, prevention, and
management. Medical Clinics, 99(3), 587-606.
Kennedy, C. C., Ioannidis, G., Thabane, L., Adachi, J. D., O’Donnell, D., Giangregorio, L.
M., ... & Papaioannou, A. (2015). Osteoporosis prescribing in long-term care: impact
of a provincial knowledge translation strategy. Canadian Journal on Aging/La Revue
canadienne du vieillissement, 34(2), 137-148.
Kerr, C., Bottomley, C., Shingler, S., Giangregorio, L., de Freitas, H. M., Patel, C., ... &
Gold, D. T. (2017). The importance of physical function to people with
osteoporosis. Osteoporosis International, 28(5), 1597-1607.
Lopez‐Olivo, M. A., Ingleshwar, A., Volk, R. J., Jibaja‐Weiss, M., Barbo, A., Saag, K., ... &
Suarez‐Almazor, M. E. (2018). Development and pilot testing of multimedia patient
education tools for patients with knee osteoarthritis, osteoporosis, and rheumatoid
arthritis. Arthritis care & research, 70(2), 213-220.
References
Beck, B. R., Daly, R. M., Singh, M. A. F., & Taaffe, D. R. (2017). Exercise and Sports
Science Australia (ESSA) position statement on exercise prescription for the
prevention and management of osteoporosis. Journal of science and medicine in
sport, 20(5), 438-445.
Bijelic, R., Milicevic, S., & Balaban, J. (2017). Risk factors for osteoporosis in
postmenopausal women. Medical Archives, 71(1), 25.
Bonafede, M., Shi, N., Barron, R., Li, X., Crittenden, D. B., & Chandler, D. (2016).
Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis
using US claims data. Archives of osteoporosis, 11(1), 26.
Golob, A. L., & Laya, M. B. (2015). Osteoporosis: screening, prevention, and
management. Medical Clinics, 99(3), 587-606.
Kennedy, C. C., Ioannidis, G., Thabane, L., Adachi, J. D., O’Donnell, D., Giangregorio, L.
M., ... & Papaioannou, A. (2015). Osteoporosis prescribing in long-term care: impact
of a provincial knowledge translation strategy. Canadian Journal on Aging/La Revue
canadienne du vieillissement, 34(2), 137-148.
Kerr, C., Bottomley, C., Shingler, S., Giangregorio, L., de Freitas, H. M., Patel, C., ... &
Gold, D. T. (2017). The importance of physical function to people with
osteoporosis. Osteoporosis International, 28(5), 1597-1607.
Lopez‐Olivo, M. A., Ingleshwar, A., Volk, R. J., Jibaja‐Weiss, M., Barbo, A., Saag, K., ... &
Suarez‐Almazor, M. E. (2018). Development and pilot testing of multimedia patient
education tools for patients with knee osteoarthritis, osteoporosis, and rheumatoid
arthritis. Arthritis care & research, 70(2), 213-220.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Reuben, D. B., Gazarian, P., Alexander, N., Araujo, K., Baker, D., Bean, J. F., ... & Leipzig,
R. M. (2017). The STRIDE Intervention: Falls Risk Factor Assessment and
Management, Patient Engagement, and Nurse Co-management. Journal of the
American Geriatrics Society, 65(12), 2733.
Rodrigues, I., Missiuna, C., & MacDermid, J. C. (2016). A theoretical perspective on
exercise adherence and osteoporosis using the theory of planned behavior and the
social cognitive theory. Critical Reviews™ in Physical and Rehabilitation
Medicine, 28(1-2).
Sagawa, N., Marcum, Z. A., Boudreau, R. M., Hanlon, J. T., Albert, S. M., O’Hare, C., ... &
Harris, T. B. (2018). Low blood pressure levels for fall injuries in older adults: the
Health, Aging and Body Composition Study. European journal of ageing, 15(3), 321-
330.
Smart, D. A., Dermody, G., Coronado, M. E., & Wilson, M. (2018). Mobility programs for
the hospitalized older adult: a scoping review. Gerontology and Geriatric
Medicine, 4, 2333721418808146.
Vandenbroucke, A., Luyten, F. P., Flamaing, J., & Gielen, E. (2017). Pharmacological
treatment of osteoporosis in the oldest old. Clinical interventions in aging, 12, 1065.
Wáng, Y. X. J., Santiago, F. R., Deng, M., & Nogueira-Barbosa, M. H. (2017). Identifying
osteoporotic vertebral endplate and cortex fractures. Quantitative imaging in medicine
and surgery, 7(5), 555.
Reuben, D. B., Gazarian, P., Alexander, N., Araujo, K., Baker, D., Bean, J. F., ... & Leipzig,
R. M. (2017). The STRIDE Intervention: Falls Risk Factor Assessment and
Management, Patient Engagement, and Nurse Co-management. Journal of the
American Geriatrics Society, 65(12), 2733.
Rodrigues, I., Missiuna, C., & MacDermid, J. C. (2016). A theoretical perspective on
exercise adherence and osteoporosis using the theory of planned behavior and the
social cognitive theory. Critical Reviews™ in Physical and Rehabilitation
Medicine, 28(1-2).
Sagawa, N., Marcum, Z. A., Boudreau, R. M., Hanlon, J. T., Albert, S. M., O’Hare, C., ... &
Harris, T. B. (2018). Low blood pressure levels for fall injuries in older adults: the
Health, Aging and Body Composition Study. European journal of ageing, 15(3), 321-
330.
Smart, D. A., Dermody, G., Coronado, M. E., & Wilson, M. (2018). Mobility programs for
the hospitalized older adult: a scoping review. Gerontology and Geriatric
Medicine, 4, 2333721418808146.
Vandenbroucke, A., Luyten, F. P., Flamaing, J., & Gielen, E. (2017). Pharmacological
treatment of osteoporosis in the oldest old. Clinical interventions in aging, 12, 1065.
Wáng, Y. X. J., Santiago, F. R., Deng, M., & Nogueira-Barbosa, M. H. (2017). Identifying
osteoporotic vertebral endplate and cortex fractures. Quantitative imaging in medicine
and surgery, 7(5), 555.

9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





