Case Study: Paediatric Scabies Patient and Nursing Interventions
VerifiedAdded on 2023/01/03
|1
|1567
|3
Case Study
AI Summary
This case study presents the case of a 1-year-old Aboriginal female, K, diagnosed with scabies. It provides an overview of the condition, including its causative agent (Sarcoptes scabei), pathophysiology, prevalence in Indigenous communities, and clinical symptoms like itching and rashes. The case study details K's presentation to the clinic, her mother's concerns, and the patient's background. It emphasizes the importance of culturally safe nursing interventions, including referrals to an Aboriginal RN and Health Counsellor, as well as the use of benzyl benzoate or malathion for treatment. The study also discusses the relevance of NSQHS Standards in providing effective care to Aboriginal and Torres Strait Islander communities, highlighting the need for appropriate diagnosis, patient education, and precautionary measures to prevent the spread of infection. References from various research studies support the discussed points.
CASE STUDY OF A PAEDIATRIC PATIENT SUFFERING FROM SCABIES - Student Name:
Tammi Knight and student ID: 1130139
Introduction:
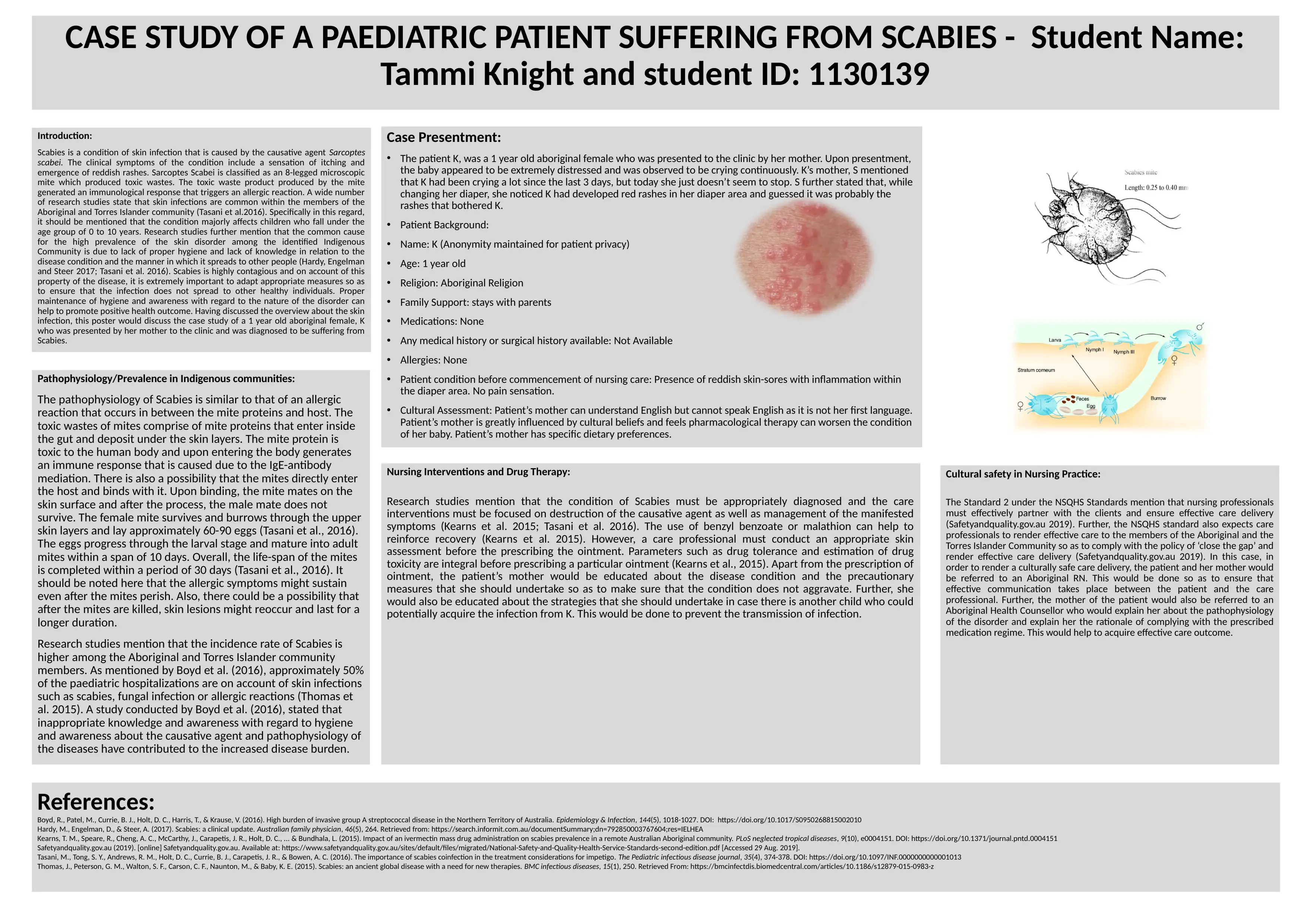
Scabies is a condition of skin infection that is caused by the causative agent Sarcoptes
scabei. The clinical symptoms of the condition include a sensation of itching and
emergence of reddish rashes. Sarcoptes Scabei is classified as an 8-legged microscopic
mite which produced toxic wastes. The toxic waste product produced by the mite
generated an immunological response that triggers an allergic reaction. A wide number
of research studies state that skin infections are common within the members of the
Aboriginal and Torres Islander community (Tasani et al.2016). Specifically in this regard,
it should be mentioned that the condition majorly affects children who fall under the
age group of 0 to 10 years. Research studies further mention that the common cause
for the high prevalence of the skin disorder among the identified Indigenous
Community is due to lack of proper hygiene and lack of knowledge in relation to the
disease condition and the manner in which it spreads to other people (Hardy, Engelman
and Steer 2017; Tasani et al. 2016). Scabies is highly contagious and on account of this
property of the disease, it is extremely important to adapt appropriate measures so as
to ensure that the infection does not spread to other healthy individuals. Proper
maintenance of hygiene and awareness with regard to the nature of the disorder can
help to promote positive health outcome. Having discussed the overview about the skin
infection, this poster would discuss the case study of a 1 year old aboriginal female, K
who was presented by her mother to the clinic and was diagnosed to be suffering from
Scabies.
Pathophysiology/Prevalence in Indigenous communities:
The pathophysiology of Scabies is similar to that of an allergic
reaction that occurs in between the mite proteins and host. The
toxic wastes of mites comprise of mite proteins that enter inside
the gut and deposit under the skin layers. The mite protein is
toxic to the human body and upon entering the body generates
an immune response that is caused due to the IgE-antibody
mediation. There is also a possibility that the mites directly enter
the host and binds with it. Upon binding, the mite mates on the
skin surface and after the process, the male mate does not
survive. The female mite survives and burrows through the upper
skin layers and lay approximately 60-90 eggs (Tasani et al., 2016).
The eggs progress through the larval stage and mature into adult
mites within a span of 10 days. Overall, the life-span of the mites
is completed within a period of 30 days (Tasani et al., 2016). It
should be noted here that the allergic symptoms might sustain
even after the mites perish. Also, there could be a possibility that
after the mites are killed, skin lesions might reoccur and last for a
longer duration.
Research studies mention that the incidence rate of Scabies is
higher among the Aboriginal and Torres Islander community
members. As mentioned by Boyd et al. (2016), approximately 50%
of the paediatric hospitalizations are on account of skin infections
such as scabies, fungal infection or allergic reactions (Thomas et
al. 2015). A study conducted by Boyd et al. (2016), stated that
inappropriate knowledge and awareness with regard to hygiene
and awareness about the causative agent and pathophysiology of
the diseases have contributed to the increased disease burden.
Cultural safety in Nursing Practice:
The Standard 2 under the NSQHS Standards mention that nursing professionals
must effectively partner with the clients and ensure effective care delivery
(Safetyandquality.gov.au 2019). Further, the NSQHS standard also expects care
professionals to render effective care to the members of the Aboriginal and the
Torres Islander Community so as to comply with the policy of ‘close the gap’ and
render effective care delivery (Safetyandquality.gov.au 2019). In this case, in
order to render a culturally safe care delivery, the patient and her mother would
be referred to an Aboriginal RN. This would be done so as to ensure that
effective communication takes place between the patient and the care
professional. Further, the mother of the patient would also be referred to an
Aboriginal Health Counsellor who would explain her about the pathophysiology
of the disorder and explain her the rationale of complying with the prescribed
medication regime. This would help to acquire effective care outcome.
Case Presentment:
• The patient K, was a 1 year old aboriginal female who was presented to the clinic by her mother. Upon presentment,
the baby appeared to be extremely distressed and was observed to be crying continuously. K’s mother, S mentioned
that K had been crying a lot since the last 3 days, but today she just doesn’t seem to stop. S further stated that, while
changing her diaper, she noticed K had developed red rashes in her diaper area and guessed it was probably the
rashes that bothered K.
• Patient Background:
• Name: K (Anonymity maintained for patient privacy)
• Age: 1 year old
• Religion: Aboriginal Religion
• Family Support: stays with parents
• Medications: None
• Any medical history or surgical history available: Not Available
• Allergies: None
• Patient condition before commencement of nursing care: Presence of reddish skin-sores with inflammation within
the diaper area. No pain sensation.
• Cultural Assessment: Patient’s mother can understand English but cannot speak English as it is not her first language.
Patient’s mother is greatly influenced by cultural beliefs and feels pharmacological therapy can worsen the condition
of her baby. Patient’s mother has specific dietary preferences.
Nursing Interventions and Drug Therapy:
Research studies mention that the condition of Scabies must be appropriately diagnosed and the care
interventions must be focused on destruction of the causative agent as well as management of the manifested
symptoms (Kearns et al. 2015; Tasani et al. 2016). The use of benzyl benzoate or malathion can help to
reinforce recovery (Kearns et al. 2015). However, a care professional must conduct an appropriate skin
assessment before the prescribing the ointment. Parameters such as drug tolerance and estimation of drug
toxicity are integral before prescribing a particular ointment (Kearns et al., 2015). Apart from the prescription of
ointment, the patient’s mother would be educated about the disease condition and the precautionary
measures that she should undertake so as to make sure that the condition does not aggravate. Further, she
would also be educated about the strategies that she should undertake in case there is another child who could
potentially acquire the infection from K. This would be done to prevent the transmission of infection.
References:
Boyd, R., Patel, M., Currie, B. J., Holt, D. C., Harris, T., & Krause, V. (2016). High burden of invasive group A streptococcal disease in the Northern Territory of Australia. Epidemiology & Infection, 144(5), 1018-1027. DOI: https://doi.org/10.1017/S0950268815002010
Hardy, M., Engelman, D., & Steer, A. (2017). Scabies: a clinical update. Australian family physician, 46(5), 264. Retrieved from: https://search.informit.com.au/documentSummary;dn=792850003767604;res=IELHEA
Kearns, T. M., Speare, R., Cheng, A. C., McCarthy, J., Carapetis, J. R., Holt, D. C., ... & Bundhala, L. (2015). Impact of an ivermectin mass drug administration on scabies prevalence in a remote Australian Aboriginal community. PLoS neglected tropical diseases, 9(10), e0004151. DOI: https://doi.org/10.1371/journal.pntd.0004151
Safetyandquality.gov.au (2019). [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf [Accessed 29 Aug. 2019].
Tasani, M., Tong, S. Y., Andrews, R. M., Holt, D. C., Currie, B. J., Carapetis, J. R., & Bowen, A. C. (2016). The importance of scabies coinfection in the treatment considerations for impetigo. The Pediatric infectious disease journal, 35(4), 374-378. DOI: https://doi.org/10.1097/INF.0000000000001013
Thomas, J., Peterson, G. M., Walton, S. F., Carson, C. F., Naunton, M., & Baby, K. E. (2015). Scabies: an ancient global disease with a need for new therapies. BMC infectious diseases, 15(1), 250. Retrieved From: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-015-0983-z
Tammi Knight and student ID: 1130139
Introduction:
Scabies is a condition of skin infection that is caused by the causative agent Sarcoptes
scabei. The clinical symptoms of the condition include a sensation of itching and
emergence of reddish rashes. Sarcoptes Scabei is classified as an 8-legged microscopic
mite which produced toxic wastes. The toxic waste product produced by the mite
generated an immunological response that triggers an allergic reaction. A wide number
of research studies state that skin infections are common within the members of the
Aboriginal and Torres Islander community (Tasani et al.2016). Specifically in this regard,
it should be mentioned that the condition majorly affects children who fall under the
age group of 0 to 10 years. Research studies further mention that the common cause
for the high prevalence of the skin disorder among the identified Indigenous
Community is due to lack of proper hygiene and lack of knowledge in relation to the
disease condition and the manner in which it spreads to other people (Hardy, Engelman
and Steer 2017; Tasani et al. 2016). Scabies is highly contagious and on account of this
property of the disease, it is extremely important to adapt appropriate measures so as
to ensure that the infection does not spread to other healthy individuals. Proper
maintenance of hygiene and awareness with regard to the nature of the disorder can
help to promote positive health outcome. Having discussed the overview about the skin
infection, this poster would discuss the case study of a 1 year old aboriginal female, K
who was presented by her mother to the clinic and was diagnosed to be suffering from
Scabies.
Pathophysiology/Prevalence in Indigenous communities:
The pathophysiology of Scabies is similar to that of an allergic
reaction that occurs in between the mite proteins and host. The
toxic wastes of mites comprise of mite proteins that enter inside
the gut and deposit under the skin layers. The mite protein is
toxic to the human body and upon entering the body generates
an immune response that is caused due to the IgE-antibody
mediation. There is also a possibility that the mites directly enter
the host and binds with it. Upon binding, the mite mates on the
skin surface and after the process, the male mate does not
survive. The female mite survives and burrows through the upper
skin layers and lay approximately 60-90 eggs (Tasani et al., 2016).
The eggs progress through the larval stage and mature into adult
mites within a span of 10 days. Overall, the life-span of the mites
is completed within a period of 30 days (Tasani et al., 2016). It
should be noted here that the allergic symptoms might sustain
even after the mites perish. Also, there could be a possibility that
after the mites are killed, skin lesions might reoccur and last for a
longer duration.
Research studies mention that the incidence rate of Scabies is
higher among the Aboriginal and Torres Islander community
members. As mentioned by Boyd et al. (2016), approximately 50%
of the paediatric hospitalizations are on account of skin infections
such as scabies, fungal infection or allergic reactions (Thomas et
al. 2015). A study conducted by Boyd et al. (2016), stated that
inappropriate knowledge and awareness with regard to hygiene
and awareness about the causative agent and pathophysiology of
the diseases have contributed to the increased disease burden.
Cultural safety in Nursing Practice:
The Standard 2 under the NSQHS Standards mention that nursing professionals
must effectively partner with the clients and ensure effective care delivery
(Safetyandquality.gov.au 2019). Further, the NSQHS standard also expects care
professionals to render effective care to the members of the Aboriginal and the
Torres Islander Community so as to comply with the policy of ‘close the gap’ and
render effective care delivery (Safetyandquality.gov.au 2019). In this case, in
order to render a culturally safe care delivery, the patient and her mother would
be referred to an Aboriginal RN. This would be done so as to ensure that
effective communication takes place between the patient and the care
professional. Further, the mother of the patient would also be referred to an
Aboriginal Health Counsellor who would explain her about the pathophysiology
of the disorder and explain her the rationale of complying with the prescribed
medication regime. This would help to acquire effective care outcome.
Case Presentment:
• The patient K, was a 1 year old aboriginal female who was presented to the clinic by her mother. Upon presentment,
the baby appeared to be extremely distressed and was observed to be crying continuously. K’s mother, S mentioned
that K had been crying a lot since the last 3 days, but today she just doesn’t seem to stop. S further stated that, while
changing her diaper, she noticed K had developed red rashes in her diaper area and guessed it was probably the
rashes that bothered K.
• Patient Background:
• Name: K (Anonymity maintained for patient privacy)
• Age: 1 year old
• Religion: Aboriginal Religion
• Family Support: stays with parents
• Medications: None
• Any medical history or surgical history available: Not Available
• Allergies: None
• Patient condition before commencement of nursing care: Presence of reddish skin-sores with inflammation within
the diaper area. No pain sensation.
• Cultural Assessment: Patient’s mother can understand English but cannot speak English as it is not her first language.
Patient’s mother is greatly influenced by cultural beliefs and feels pharmacological therapy can worsen the condition
of her baby. Patient’s mother has specific dietary preferences.
Nursing Interventions and Drug Therapy:
Research studies mention that the condition of Scabies must be appropriately diagnosed and the care
interventions must be focused on destruction of the causative agent as well as management of the manifested
symptoms (Kearns et al. 2015; Tasani et al. 2016). The use of benzyl benzoate or malathion can help to
reinforce recovery (Kearns et al. 2015). However, a care professional must conduct an appropriate skin
assessment before the prescribing the ointment. Parameters such as drug tolerance and estimation of drug
toxicity are integral before prescribing a particular ointment (Kearns et al., 2015). Apart from the prescription of
ointment, the patient’s mother would be educated about the disease condition and the precautionary
measures that she should undertake so as to make sure that the condition does not aggravate. Further, she
would also be educated about the strategies that she should undertake in case there is another child who could
potentially acquire the infection from K. This would be done to prevent the transmission of infection.
References:
Boyd, R., Patel, M., Currie, B. J., Holt, D. C., Harris, T., & Krause, V. (2016). High burden of invasive group A streptococcal disease in the Northern Territory of Australia. Epidemiology & Infection, 144(5), 1018-1027. DOI: https://doi.org/10.1017/S0950268815002010
Hardy, M., Engelman, D., & Steer, A. (2017). Scabies: a clinical update. Australian family physician, 46(5), 264. Retrieved from: https://search.informit.com.au/documentSummary;dn=792850003767604;res=IELHEA
Kearns, T. M., Speare, R., Cheng, A. C., McCarthy, J., Carapetis, J. R., Holt, D. C., ... & Bundhala, L. (2015). Impact of an ivermectin mass drug administration on scabies prevalence in a remote Australian Aboriginal community. PLoS neglected tropical diseases, 9(10), e0004151. DOI: https://doi.org/10.1371/journal.pntd.0004151
Safetyandquality.gov.au (2019). [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf [Accessed 29 Aug. 2019].
Tasani, M., Tong, S. Y., Andrews, R. M., Holt, D. C., Currie, B. J., Carapetis, J. R., & Bowen, A. C. (2016). The importance of scabies coinfection in the treatment considerations for impetigo. The Pediatric infectious disease journal, 35(4), 374-378. DOI: https://doi.org/10.1097/INF.0000000000001013
Thomas, J., Peterson, G. M., Walton, S. F., Carson, C. F., Naunton, M., & Baby, K. E. (2015). Scabies: an ancient global disease with a need for new therapies. BMC infectious diseases, 15(1), 250. Retrieved From: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-015-0983-z
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




