NRSG374 Assessment 1: Pain Management in Palliative Care Report
VerifiedAdded on 2023/02/02
|13
|2132
|30
Report
AI Summary
This report provides a comprehensive overview of pain management in palliative care. It begins by defining pain in palliative care, highlighting its prevalence and the challenges in managing it. The report then delves into pain assessment, discussing various methods and tools suitable for different patient populations, including children and those with cognitive impairments. It emphasizes the importance of a systematic approach to pain assessment, considering the location, characteristics, and impact of pain on daily activities. The report also explores pain management strategies, including the WHO analgesic ladder, adjuvant analgesics, and non-pharmacological therapies. Furthermore, it examines the National Palliative Care Standards and how effective pain management upholds these standards. The report emphasizes the importance of person-centered care, assessment of needs, care planning, and support for carers. Finally, it addresses concerns about using analgesics and the importance of addressing patient fears and misconceptions. The report is designed for undergraduate nursing students and graduate registered nurses.

2021
Assessment 1
NRSG374
Assessment 1
NRSG374
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Panchyayatguide, 2016)
Pain Management
in Palliative Care
1
Pain Management
in Palliative Care
1
Contents
Intended audience and learning objectives--------------------------------------------------------------3
Pain in Palliative Care------------------------------------------------------------------------------------------3
Pain assessment in Palliative Care--------------------------------------------------------------------------4
Pain management----------------------------------------------------------------------------------------------5
National Palliative Care Standard----------------------------------------------------------------------------5
How does pain management uphold the National palliative Care Standard----------------------6
2
Intended audience and learning objectives--------------------------------------------------------------3
Pain in Palliative Care------------------------------------------------------------------------------------------3
Pain assessment in Palliative Care--------------------------------------------------------------------------4
Pain management----------------------------------------------------------------------------------------------5
National Palliative Care Standard----------------------------------------------------------------------------5
How does pain management uphold the National palliative Care Standard----------------------6
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Intended audience
The intended audience of this resource is third year undergraduate
students and graduate Registered Nurses.
Learning outcomes and objectives
Upon completion of this resources, the readers will be able to:
Understand pain in palliative care
Understand how to assess pain in palliative care
Understand what pain management is and issues related to pain
management
How pain management uphold the National palliative care
standard
Pain in Palliative Care
Pain, a common symptom of many diseases, is often experienced by
patients who need palliative care (Givler et.al., 2021). Research shows
that 80% of cancer or AIDS patients, 67% of cardiovascular patients or
COPD will go through mild to severe pain during their final few months
(WHO, 2020). Even though pain relieving medicine can work effectively
for majority of conditions, it is still a challenge for health professional to
manage pain complexity for patients (The Royal Children’s Hospital
Melbourne, 2021).
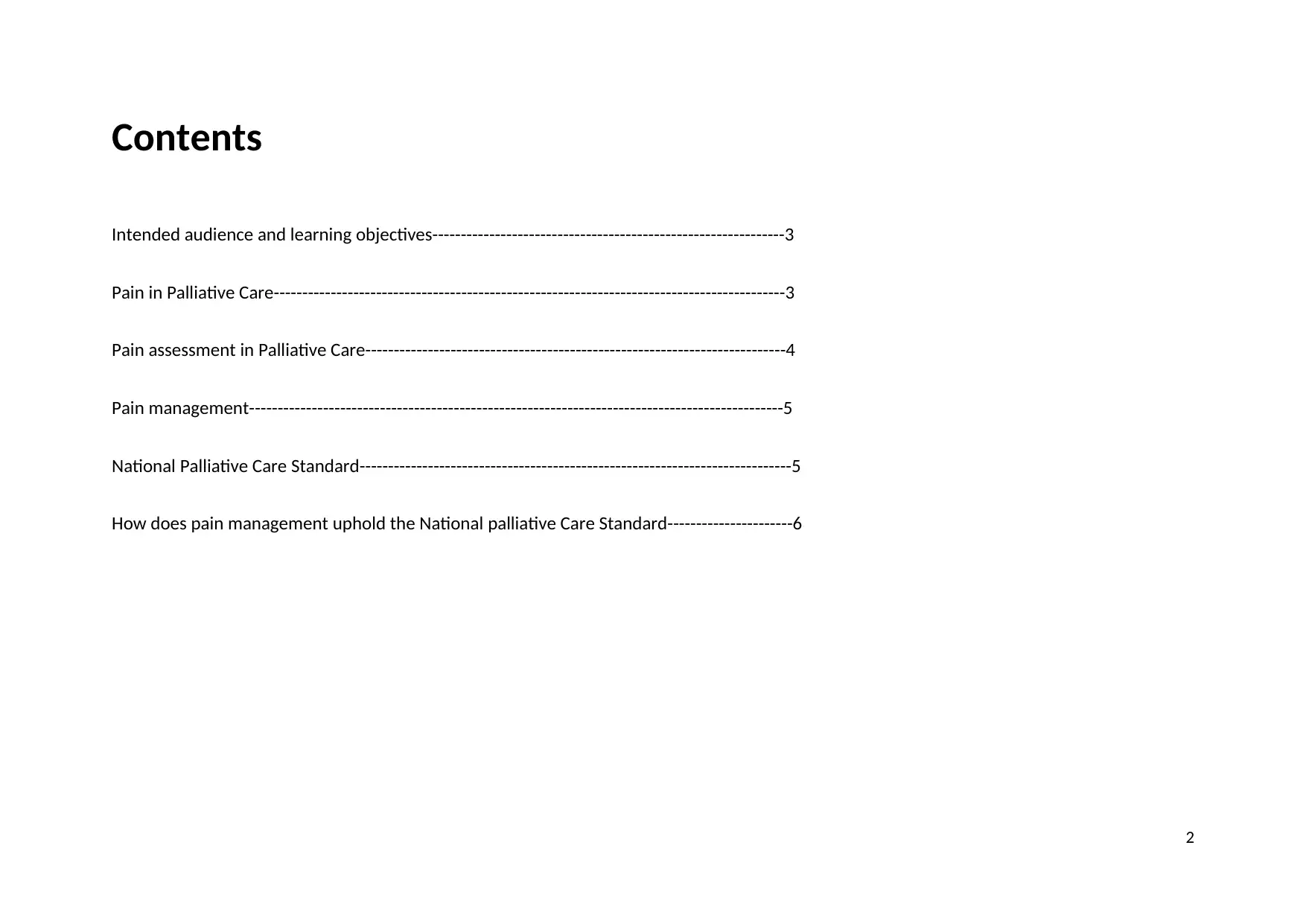
Every individual experience pain differently. Both, Severity of illness and
patient discomfort level contribute to formation of one’s experience to
pain. (Sholjakova, et.al., 2018) Physical, emotional, Social, spiritual, and
Informational are interconnected components contributing to pain.
Diagram reflects the contribution factors from each component.
3
The intended audience of this resource is third year undergraduate
students and graduate Registered Nurses.
Learning outcomes and objectives
Upon completion of this resources, the readers will be able to:
Understand pain in palliative care
Understand how to assess pain in palliative care
Understand what pain management is and issues related to pain
management
How pain management uphold the National palliative care
standard
Pain in Palliative Care
Pain, a common symptom of many diseases, is often experienced by
patients who need palliative care (Givler et.al., 2021). Research shows
that 80% of cancer or AIDS patients, 67% of cardiovascular patients or
COPD will go through mild to severe pain during their final few months
(WHO, 2020). Even though pain relieving medicine can work effectively
for majority of conditions, it is still a challenge for health professional to
manage pain complexity for patients (The Royal Children’s Hospital
Melbourne, 2021).
Every individual experience pain differently. Both, Severity of illness and
patient discomfort level contribute to formation of one’s experience to
pain. (Sholjakova, et.al., 2018) Physical, emotional, Social, spiritual, and
Informational are interconnected components contributing to pain.
Diagram reflects the contribution factors from each component.
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Hui, et.al., 2018)
Pain Assessment in Palliative Care
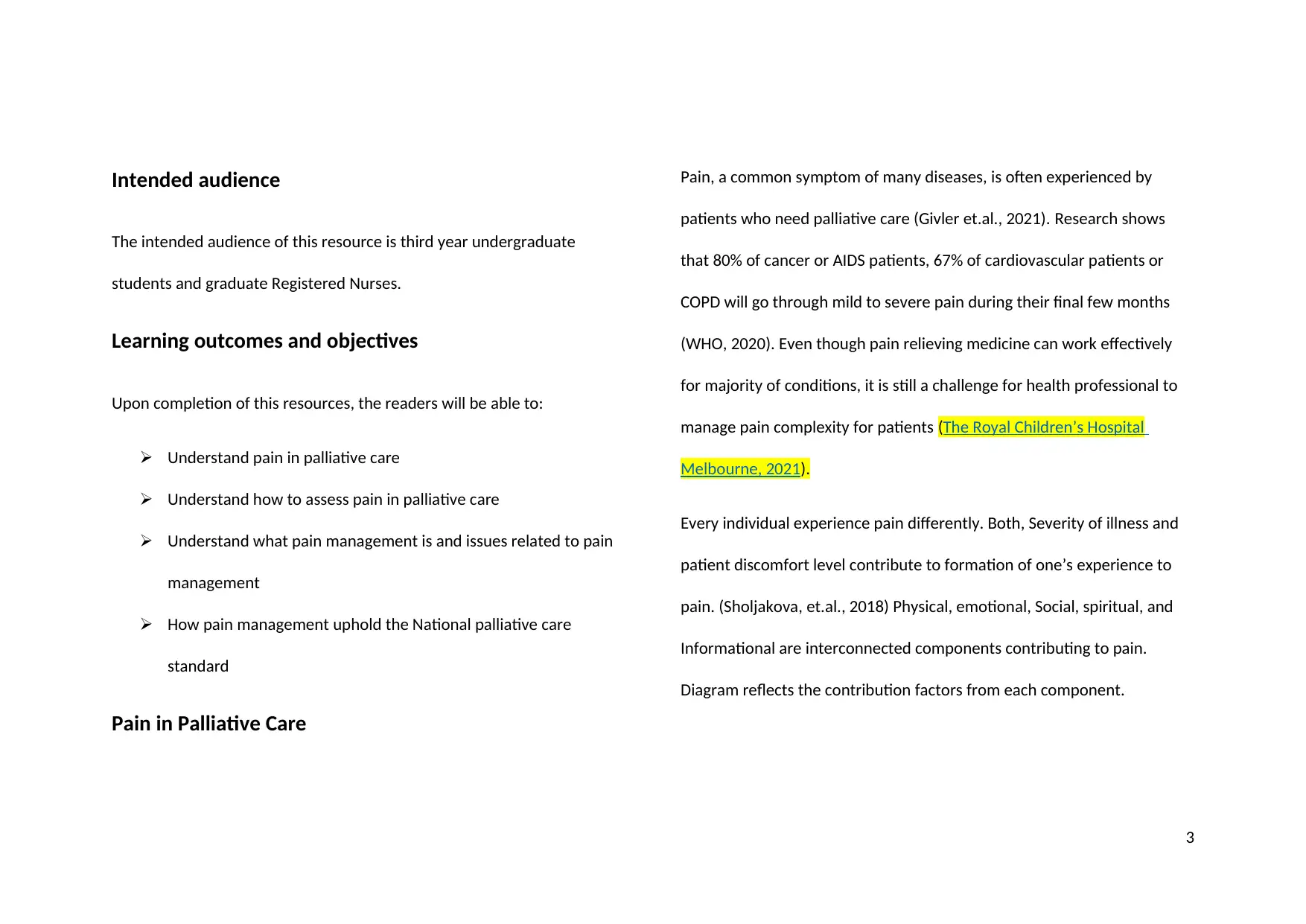
It is vital for health professionals have a good understanding of patients’
pain to develop a treatment plan. Patients can have more than one types
of pain and in different location which is very important to be identified
before medications are started (GPonline, 2015). A systematic pain
assessment should include several components including previous pain
assessment or treatments (Moore, 2018).
Components Examples
Pain characteristics Location, temporal, quality,
triggers
Symptoms associated Changes in strength or mobility
Pain impact Daily activities in life
Documents Documents or pain intensity
However, the severity of pain is not the same for all palliative patients.
Cancer patients often experience pain in “Multiple sites and of different
etiologies and underlying mechanisms” (Caraceni & Shkodra, 2019). It is
vital to know concepts such as neuropathic and mixed pain while
assessing pain in cancer patients (Caraceni & Shkodra, 2019). In addition,
diversity among patients should also be considered while assessing pains.
4
Pain Assessment in Palliative Care
It is vital for health professionals have a good understanding of patients’
pain to develop a treatment plan. Patients can have more than one types
of pain and in different location which is very important to be identified
before medications are started (GPonline, 2015). A systematic pain
assessment should include several components including previous pain
assessment or treatments (Moore, 2018).
Components Examples
Pain characteristics Location, temporal, quality,
triggers
Symptoms associated Changes in strength or mobility
Pain impact Daily activities in life
Documents Documents or pain intensity
However, the severity of pain is not the same for all palliative patients.
Cancer patients often experience pain in “Multiple sites and of different
etiologies and underlying mechanisms” (Caraceni & Shkodra, 2019). It is
vital to know concepts such as neuropathic and mixed pain while
assessing pain in cancer patients (Caraceni & Shkodra, 2019). In addition,
diversity among patients should also be considered while assessing pains.
4
Children, non-verbal, and cognitive impaired patients might not rate the
exact severity of their pain (Hauer & Hautrow, 2017).
There are variety of pain assessment tools in use by clinical assessment
teams. Below are the most common pain assessing tools used for ongoing
monitoring of pain in specific groups:
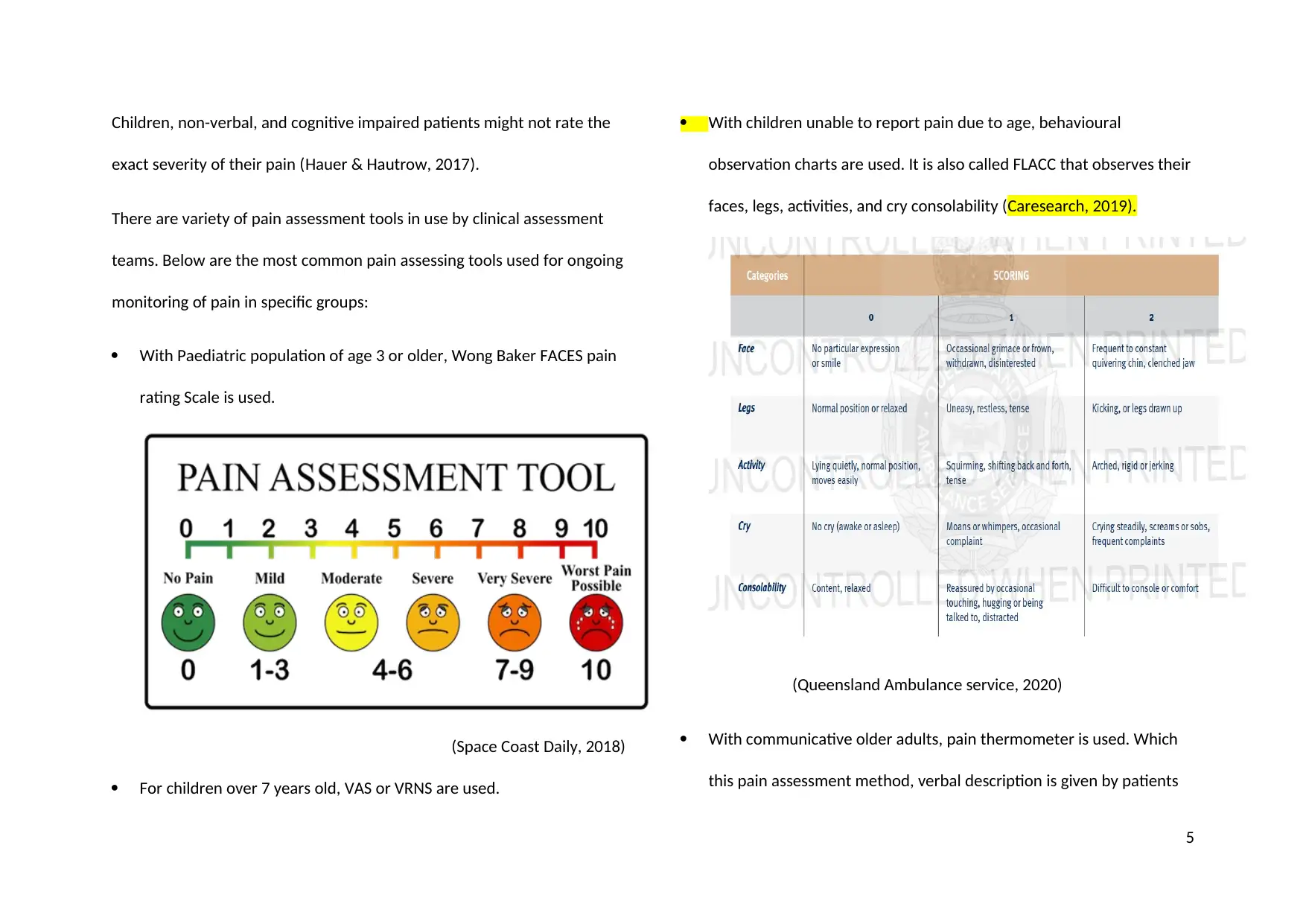
With Paediatric population of age 3 or older, Wong Baker FACES pain
rating Scale is used.
(Space Coast Daily, 2018)
For children over 7 years old, VAS or VRNS are used.
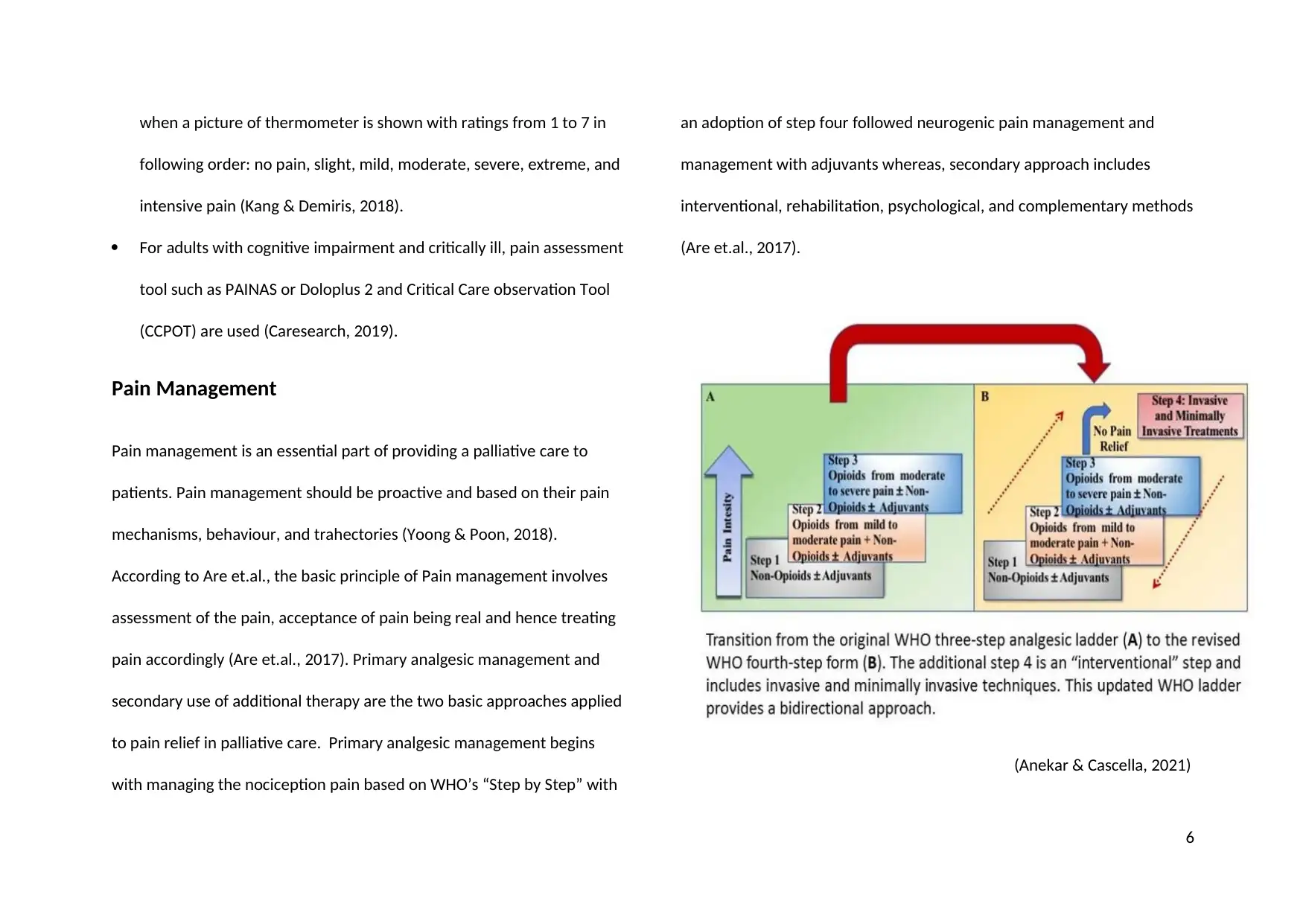
With children unable to report pain due to age, behavioural
observation charts are used. It is also called FLACC that observes their
faces, legs, activities, and cry consolability (Caresearch, 2019).
(Queensland Ambulance service, 2020)
With communicative older adults, pain thermometer is used. Which
this pain assessment method, verbal description is given by patients
5
exact severity of their pain (Hauer & Hautrow, 2017).
There are variety of pain assessment tools in use by clinical assessment
teams. Below are the most common pain assessing tools used for ongoing
monitoring of pain in specific groups:
With Paediatric population of age 3 or older, Wong Baker FACES pain
rating Scale is used.
(Space Coast Daily, 2018)
For children over 7 years old, VAS or VRNS are used.
With children unable to report pain due to age, behavioural
observation charts are used. It is also called FLACC that observes their
faces, legs, activities, and cry consolability (Caresearch, 2019).
(Queensland Ambulance service, 2020)
With communicative older adults, pain thermometer is used. Which
this pain assessment method, verbal description is given by patients
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
when a picture of thermometer is shown with ratings from 1 to 7 in
following order: no pain, slight, mild, moderate, severe, extreme, and
intensive pain (Kang & Demiris, 2018).
For adults with cognitive impairment and critically ill, pain assessment
tool such as PAINAS or Doloplus 2 and Critical Care observation Tool
(CCPOT) are used (Caresearch, 2019).
Pain Management
Pain management is an essential part of providing a palliative care to
patients. Pain management should be proactive and based on their pain
mechanisms, behaviour, and trahectories (Yoong & Poon, 2018).
According to Are et.al., the basic principle of Pain management involves
assessment of the pain, acceptance of pain being real and hence treating
pain accordingly (Are et.al., 2017). Primary analgesic management and
secondary use of additional therapy are the two basic approaches applied
to pain relief in palliative care. Primary analgesic management begins
with managing the nociception pain based on WHO’s “Step by Step” with
an adoption of step four followed neurogenic pain management and
management with adjuvants whereas, secondary approach includes
interventional, rehabilitation, psychological, and complementary methods
(Are et.al., 2017).
(Anekar & Cascella, 2021)
6
following order: no pain, slight, mild, moderate, severe, extreme, and
intensive pain (Kang & Demiris, 2018).
For adults with cognitive impairment and critically ill, pain assessment
tool such as PAINAS or Doloplus 2 and Critical Care observation Tool
(CCPOT) are used (Caresearch, 2019).
Pain Management
Pain management is an essential part of providing a palliative care to
patients. Pain management should be proactive and based on their pain
mechanisms, behaviour, and trahectories (Yoong & Poon, 2018).
According to Are et.al., the basic principle of Pain management involves
assessment of the pain, acceptance of pain being real and hence treating
pain accordingly (Are et.al., 2017). Primary analgesic management and
secondary use of additional therapy are the two basic approaches applied
to pain relief in palliative care. Primary analgesic management begins
with managing the nociception pain based on WHO’s “Step by Step” with
an adoption of step four followed neurogenic pain management and
management with adjuvants whereas, secondary approach includes
interventional, rehabilitation, psychological, and complementary methods
(Are et.al., 2017).
(Anekar & Cascella, 2021)
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
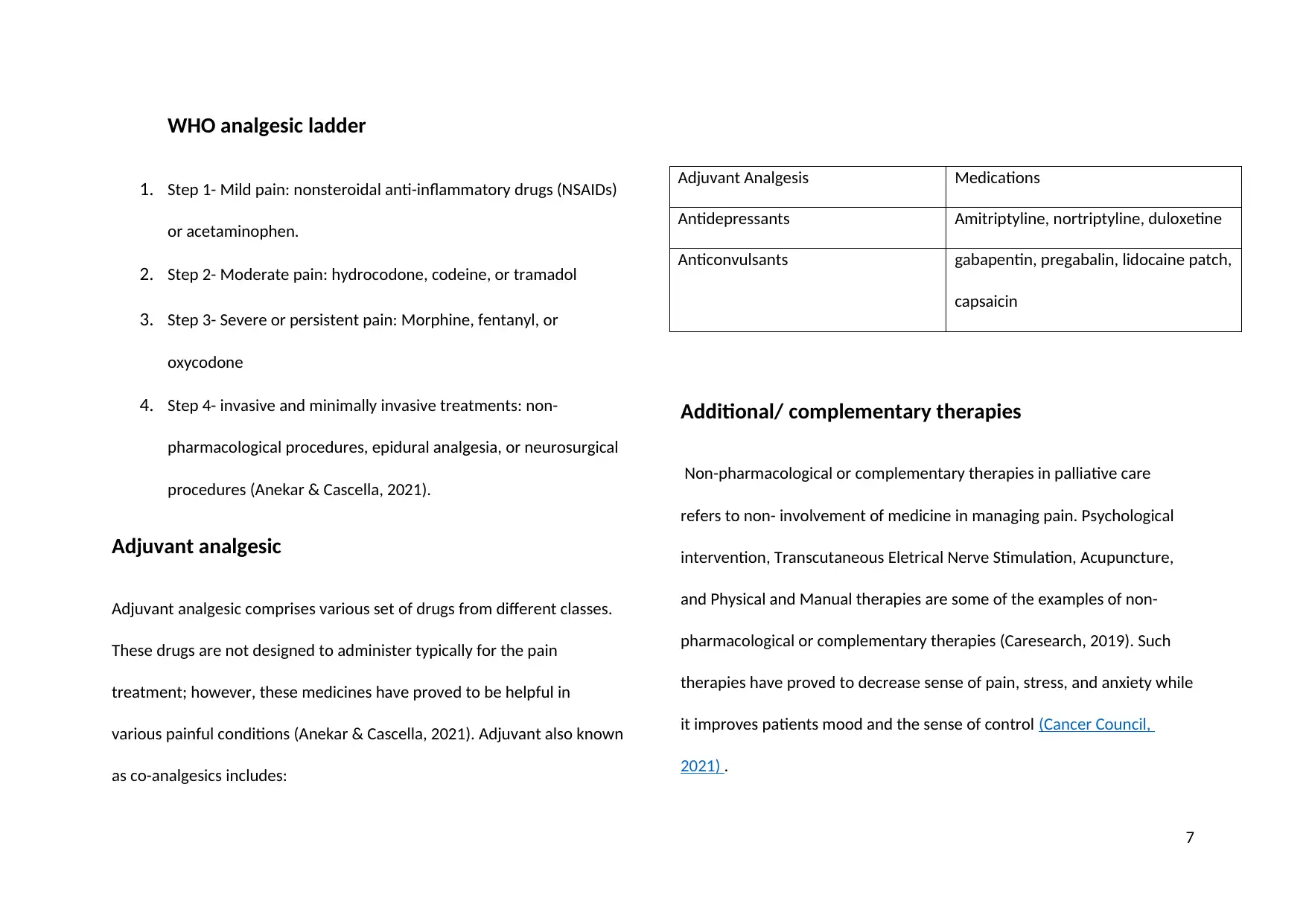
WHO analgesic ladder
1. Step 1- Mild pain: nonsteroidal anti-inflammatory drugs (NSAIDs)
or acetaminophen.
2. Step 2- Moderate pain: hydrocodone, codeine, or tramadol
3. Step 3- Severe or persistent pain: Morphine, fentanyl, or
oxycodone
4. Step 4- invasive and minimally invasive treatments: non-
pharmacological procedures, epidural analgesia, or neurosurgical
procedures (Anekar & Cascella, 2021).
Adjuvant analgesic
Adjuvant analgesic comprises various set of drugs from different classes.
These drugs are not designed to administer typically for the pain
treatment; however, these medicines have proved to be helpful in
various painful conditions (Anekar & Cascella, 2021). Adjuvant also known
as co-analgesics includes:
Adjuvant Analgesis Medications
Antidepressants Amitriptyline, nortriptyline, duloxetine
Anticonvulsants gabapentin, pregabalin, lidocaine patch,
capsaicin
Additional/ complementary therapies
Non-pharmacological or complementary therapies in palliative care
refers to non- involvement of medicine in managing pain. Psychological
intervention, Transcutaneous Eletrical Nerve Stimulation, Acupuncture,
and Physical and Manual therapies are some of the examples of non-
pharmacological or complementary therapies (Caresearch, 2019). Such
therapies have proved to decrease sense of pain, stress, and anxiety while
it improves patients mood and the sense of control (Cancer Council,
2021) .
7
1. Step 1- Mild pain: nonsteroidal anti-inflammatory drugs (NSAIDs)
or acetaminophen.
2. Step 2- Moderate pain: hydrocodone, codeine, or tramadol
3. Step 3- Severe or persistent pain: Morphine, fentanyl, or
oxycodone
4. Step 4- invasive and minimally invasive treatments: non-
pharmacological procedures, epidural analgesia, or neurosurgical
procedures (Anekar & Cascella, 2021).
Adjuvant analgesic
Adjuvant analgesic comprises various set of drugs from different classes.
These drugs are not designed to administer typically for the pain
treatment; however, these medicines have proved to be helpful in
various painful conditions (Anekar & Cascella, 2021). Adjuvant also known
as co-analgesics includes:
Adjuvant Analgesis Medications
Antidepressants Amitriptyline, nortriptyline, duloxetine
Anticonvulsants gabapentin, pregabalin, lidocaine patch,
capsaicin
Additional/ complementary therapies
Non-pharmacological or complementary therapies in palliative care
refers to non- involvement of medicine in managing pain. Psychological
intervention, Transcutaneous Eletrical Nerve Stimulation, Acupuncture,
and Physical and Manual therapies are some of the examples of non-
pharmacological or complementary therapies (Caresearch, 2019). Such
therapies have proved to decrease sense of pain, stress, and anxiety while
it improves patients mood and the sense of control (Cancer Council,
2021) .
7
Concern about using Analgesic
Pain being the most common symptoms experienced by palliative care
patients, various analgesics are used by health professionals. While,
opioid analgesics give relief from pain and distress to patients, it comes
with some concerns and issues. A study showed that 43 patients out of
100 expressed concern to use opioid treatments. The common concerns
were drug addition, fear of dying, and unwanted effects (Graczyk, et.al.,
20174).
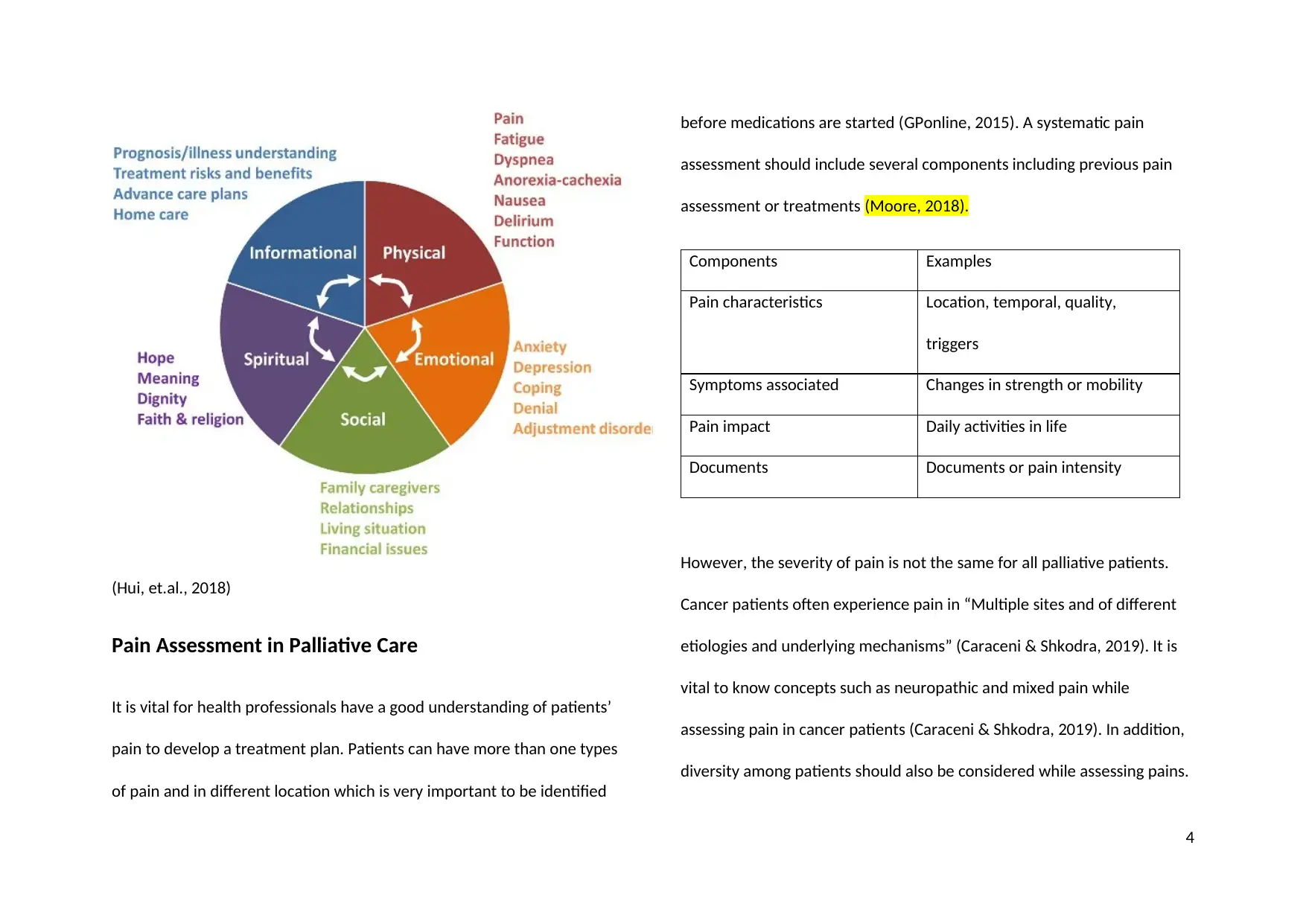
National Palliative Care Standard
According to Palliative Care Australia, “Palliative care is person and
family- centred care provided for a person with an active, progressive,
advanced disease, who has little or no prospect of cure and who is
expected to die, and for whom the primary treatment goal is to optimise
the quality of life.” (2018) The main aim of palliative care is to provide
person- centred care to the patients’ and their families’ needs,
preferences, and values regardless of their diagnosis. (PCA, ?)
The National Palliative Care Standards works as a guideline for specialist
while encouraging and promoting the ideas of patient- centred and
compassionate high-quality care to patients. (PCA, 2021?) The National
Palliative Care Standards comprises nine standards as shown in picture
below:
8
Pain being the most common symptoms experienced by palliative care
patients, various analgesics are used by health professionals. While,
opioid analgesics give relief from pain and distress to patients, it comes
with some concerns and issues. A study showed that 43 patients out of
100 expressed concern to use opioid treatments. The common concerns
were drug addition, fear of dying, and unwanted effects (Graczyk, et.al.,
20174).
National Palliative Care Standard
According to Palliative Care Australia, “Palliative care is person and
family- centred care provided for a person with an active, progressive,
advanced disease, who has little or no prospect of cure and who is
expected to die, and for whom the primary treatment goal is to optimise
the quality of life.” (2018) The main aim of palliative care is to provide
person- centred care to the patients’ and their families’ needs,
preferences, and values regardless of their diagnosis. (PCA, ?)
The National Palliative Care Standards works as a guideline for specialist
while encouraging and promoting the ideas of patient- centred and
compassionate high-quality care to patients. (PCA, 2021?) The National
Palliative Care Standards comprises nine standards as shown in picture
below:
8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
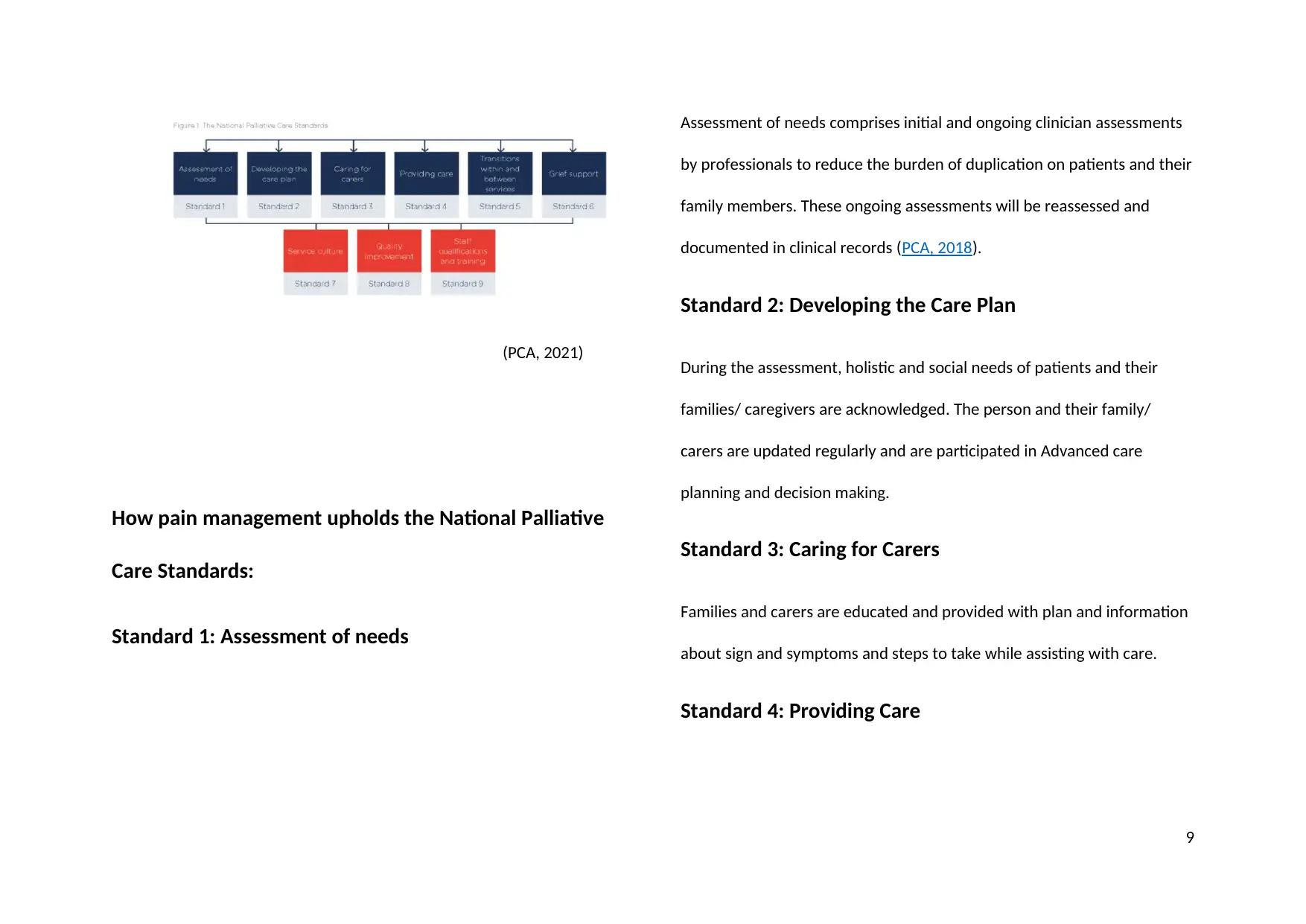
(PCA, 2021)
How pain management upholds the National Palliative
Care Standards:
Standard 1: Assessment of needs
Assessment of needs comprises initial and ongoing clinician assessments
by professionals to reduce the burden of duplication on patients and their
family members. These ongoing assessments will be reassessed and
documented in clinical records (PCA, 2018).
Standard 2: Developing the Care Plan
During the assessment, holistic and social needs of patients and their
families/ caregivers are acknowledged. The person and their family/
carers are updated regularly and are participated in Advanced care
planning and decision making.
Standard 3: Caring for Carers
Families and carers are educated and provided with plan and information
about sign and symptoms and steps to take while assisting with care.
Standard 4: Providing Care
9
How pain management upholds the National Palliative
Care Standards:
Standard 1: Assessment of needs
Assessment of needs comprises initial and ongoing clinician assessments
by professionals to reduce the burden of duplication on patients and their
family members. These ongoing assessments will be reassessed and
documented in clinical records (PCA, 2018).
Standard 2: Developing the Care Plan
During the assessment, holistic and social needs of patients and their
families/ caregivers are acknowledged. The person and their family/
carers are updated regularly and are participated in Advanced care
planning and decision making.
Standard 3: Caring for Carers
Families and carers are educated and provided with plan and information
about sign and symptoms and steps to take while assisting with care.
Standard 4: Providing Care
9
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10
References:
Anekar, A., & Cascellav, M. (2021). WHO analgesic ladder [Image]. Retrieved 5 September 2021, from
https://www.ncbi.nlm.nih.gov/books/NBK554435/figure/article-31358.image.f1/?report=objectonly.
Are, M., McIntyre, A., & Reddy, S. (2017). Global disparities in cancer pain management and palliative care. Journal of Surgical Oncology, 115(5), 637–641.
https://doi.org/10.1002/jso.24585
Caraceni, A., & Shkodra, M. (2019). Cancer Pain Assessment and Classification. Cancers, 11(4), 510. https://doi.org/10.3390/cancers11040510
CareSearch. (2019). Non Pharmacological Approaches. Retrieved 4 September 2021,
from https://www.caresearch.com.au/caresearch/tabid/751/Default.aspx
GPonline. (2015). Assessing and managing pain in palliative care | GPonline. Gponline.com. Retrieved 5 September 2021, from
https://www.gponline.com/assessing-managing-pain-palliative-care/palliative-end-of-life-care/article/1293241.
Hauer, J., & Houtrow, A. J. (2017). Pain Assessment and Treatment in Children With Significant Impairment of the Central Nervous System. Pediatrics
(Evanston), 139(6), e20171002–. https://doi.org/10.1542/peds.2017-1002
Hui, D., Hannon, B., Zimmermann, C., & Bruera, E. (2018). [Image]. Retrieved 5 September 2021, from
https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21490.
11
Anekar, A., & Cascellav, M. (2021). WHO analgesic ladder [Image]. Retrieved 5 September 2021, from
https://www.ncbi.nlm.nih.gov/books/NBK554435/figure/article-31358.image.f1/?report=objectonly.
Are, M., McIntyre, A., & Reddy, S. (2017). Global disparities in cancer pain management and palliative care. Journal of Surgical Oncology, 115(5), 637–641.
https://doi.org/10.1002/jso.24585
Caraceni, A., & Shkodra, M. (2019). Cancer Pain Assessment and Classification. Cancers, 11(4), 510. https://doi.org/10.3390/cancers11040510
CareSearch. (2019). Non Pharmacological Approaches. Retrieved 4 September 2021,
from https://www.caresearch.com.au/caresearch/tabid/751/Default.aspx
GPonline. (2015). Assessing and managing pain in palliative care | GPonline. Gponline.com. Retrieved 5 September 2021, from
https://www.gponline.com/assessing-managing-pain-palliative-care/palliative-end-of-life-care/article/1293241.
Hauer, J., & Houtrow, A. J. (2017). Pain Assessment and Treatment in Children With Significant Impairment of the Central Nervous System. Pediatrics
(Evanston), 139(6), e20171002–. https://doi.org/10.1542/peds.2017-1002
Hui, D., Hannon, B., Zimmermann, C., & Bruera, E. (2018). [Image]. Retrieved 5 September 2021, from
https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21490.
11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





