NUR272 Literature Review: Compassion's Role in Palliative Care (USC)
VerifiedAdded on 2022/08/08
|5
|1623
|12
Report
AI Summary
This report presents a literature review focusing on the core value of compassion within palliative care, as required for the NUR272 course. The review explores the significance of compassion for patients, their families, and carers, examining its impact on the quality of care provided. The report analyzes various studies and research papers, highlighting key findings and themes related to compassion, including the importance of professional attitudes, the need for self-care among healthcare providers, and the influence of socio-political factors on the implementation of compassionate care. The review also discusses the existing literature gaps and the need for further research to improve the understanding and application of compassion in palliative care settings. The analysis includes a table summarizing key themes and authors, and concludes by emphasizing the crucial role of compassion in reducing suffering and creating a peaceful environment for patients and their families during end-of-life care. The assignment meets the requirements set by the University of the Sunshine Coast for the specified course, and provides a comprehensive overview of the topic.

Running head: NUR272
INTRODUCTION
Palliative Care can be defined as the approach of caregiving in which optimized and
quality care to individuals suffering from severe, complicated or terminal diseases is provided
(Kelley and Morrison 2015). According to the statement of the World Health Organization it
is the process by which critical and life-threatening illnesses are prevented or the suffering is
lowered by the early detection and treatment of the diseases and the quality of life can be
improved (Centeno 2016). There are eight core values according to the National Palliative
Care Standards which the professionals should follow (Palliative Care Australia 2020). In this
paper, one of the core value which states ‘Act with compassion towards the individual, their
near family and carers’ will be analysed elaborately. The family and carers of the suffering
individual have a very important role in providing mental, emotional, physical support to the
sufferer. So, it is a crucial point that the palliative care professional should value their efforts
as well, by treating the individual suffering and his or her family with the utmost compassion
and respect to ease their pain and distress.
BODY
Compassion is an important factor that palliative care professionals should keep in
mind to provide good quality healthcare to the patient. A research was conducted to show the
understanding of the importance of compassion and to identify various initiatives taken to
improve the compassion level in palliative care. The result showed that in some cases, the
suffering individuals and their family and carers understood the concept of compassion but
often could not implement it during the treatment as the professionals had limited idea about
this. Whereas in other cases, it was seen that the palliative care professionals who
implemented compassion, received better results as the patient and their family responded
positively to it. There are also a few methods by which compassion could be enhanced at
professional, community and organizational level which would, in turn, improve the
satisfaction of the healthcare individual and the palliative care quality (Brito-Pons and
Librada-Flores 2018).
Another study was conducted to understand the attitude of palliative care
professionals towards the dying and terminally ill individuals. The result showed that a higher
percentage of the professionals showed a negative attitude towards the protocol of palliative
care and the professionals stated that existent protocols are far from practicality. Whereas the
senior professionals showed a positive attitude towards the protocol stating the need for
INTRODUCTION
Palliative Care can be defined as the approach of caregiving in which optimized and
quality care to individuals suffering from severe, complicated or terminal diseases is provided
(Kelley and Morrison 2015). According to the statement of the World Health Organization it
is the process by which critical and life-threatening illnesses are prevented or the suffering is
lowered by the early detection and treatment of the diseases and the quality of life can be
improved (Centeno 2016). There are eight core values according to the National Palliative
Care Standards which the professionals should follow (Palliative Care Australia 2020). In this
paper, one of the core value which states ‘Act with compassion towards the individual, their
near family and carers’ will be analysed elaborately. The family and carers of the suffering
individual have a very important role in providing mental, emotional, physical support to the
sufferer. So, it is a crucial point that the palliative care professional should value their efforts
as well, by treating the individual suffering and his or her family with the utmost compassion
and respect to ease their pain and distress.
BODY
Compassion is an important factor that palliative care professionals should keep in
mind to provide good quality healthcare to the patient. A research was conducted to show the
understanding of the importance of compassion and to identify various initiatives taken to
improve the compassion level in palliative care. The result showed that in some cases, the
suffering individuals and their family and carers understood the concept of compassion but
often could not implement it during the treatment as the professionals had limited idea about
this. Whereas in other cases, it was seen that the palliative care professionals who
implemented compassion, received better results as the patient and their family responded
positively to it. There are also a few methods by which compassion could be enhanced at
professional, community and organizational level which would, in turn, improve the
satisfaction of the healthcare individual and the palliative care quality (Brito-Pons and
Librada-Flores 2018).
Another study was conducted to understand the attitude of palliative care
professionals towards the dying and terminally ill individuals. The result showed that a higher
percentage of the professionals showed a negative attitude towards the protocol of palliative
care and the professionals stated that existent protocols are far from practicality. Whereas the
senior professionals showed a positive attitude towards the protocol stating the need for
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

2
NUR272
compassion towards the patients. Thus the researchers concluded that the healthcare workers’
attitudes should be looked after and in case they should be put under training to develop
values in them (Leclerc 2014).
A study was conducted to discuss the available literature on the need for self-care and
compassion in palliative care. Investigation resulted in the identification four themes
including the importance of self-care; planning and awareness; self-care dimensions and
balanced compassion. The review also stated that even after such a widespread discussion
and knowledge about the need of self-care of the carers and compassion in palliative care
there are not enough literature or methodologies designed so that it can be widely accepted.
There is a considerable need for further research on this topic to make it easier to adapt
(Mills, Wand and Fraser 2017).
Zaman et al. (2018) examined the position and need for compassion in palliative care
and the discussion going on about it. The study states that even after a widespread discussion
and teaching the need for compassion in palliative care, professionals complain about the
difficulties in adapting it. The researchers report that it is the socio-political factors that
prevent the professionals from adapting it which includes closed health systems, sense of
individualism and privacy, increased mistrust in the global politics and anxiety about the
legal proceedings on health grounds. The report concludes that the value of compassion in
palliative care discussed should be revised by building a proper structure and incorporation of
much more realistic and practical concepts.
DISCUSSION
In the first literature, it was seen that though the majority of the palliative care
professionals had an about compassion and its need but owing to their limited knowledge in
this field they could not implement it during treatment. This could be overcome by a more
widespread campaign about this and by creating awareness among the professionals. It
should also be introduced as a compulsory part in their course of study so that young carers
can act with more compassion with the patient as well as his or her family and carers. This
rationale is taken from a study conducted by Centeno et al. (2016).
The next study shows that professionals exhibit a negative view of compassion as a
crucial aspect of palliative care. This is the result of stringent rules that might make them face
NUR272
compassion towards the patients. Thus the researchers concluded that the healthcare workers’
attitudes should be looked after and in case they should be put under training to develop
values in them (Leclerc 2014).
A study was conducted to discuss the available literature on the need for self-care and
compassion in palliative care. Investigation resulted in the identification four themes
including the importance of self-care; planning and awareness; self-care dimensions and
balanced compassion. The review also stated that even after such a widespread discussion
and knowledge about the need of self-care of the carers and compassion in palliative care
there are not enough literature or methodologies designed so that it can be widely accepted.
There is a considerable need for further research on this topic to make it easier to adapt
(Mills, Wand and Fraser 2017).
Zaman et al. (2018) examined the position and need for compassion in palliative care
and the discussion going on about it. The study states that even after a widespread discussion
and teaching the need for compassion in palliative care, professionals complain about the
difficulties in adapting it. The researchers report that it is the socio-political factors that
prevent the professionals from adapting it which includes closed health systems, sense of
individualism and privacy, increased mistrust in the global politics and anxiety about the
legal proceedings on health grounds. The report concludes that the value of compassion in
palliative care discussed should be revised by building a proper structure and incorporation of
much more realistic and practical concepts.
DISCUSSION
In the first literature, it was seen that though the majority of the palliative care
professionals had an about compassion and its need but owing to their limited knowledge in
this field they could not implement it during treatment. This could be overcome by a more
widespread campaign about this and by creating awareness among the professionals. It
should also be introduced as a compulsory part in their course of study so that young carers
can act with more compassion with the patient as well as his or her family and carers. This
rationale is taken from a study conducted by Centeno et al. (2016).
The next study shows that professionals exhibit a negative view of compassion as a
crucial aspect of palliative care. This is the result of stringent rules that might make them face
3
NUR272
problems or make them uncomfortable and the senior professionals should look into this
matter and solve the problems by easing their thought process.
The other two works of literature show that there is a wide literature gap in this field
that needs to be filled. Innovative research and newer procedures are very much in need to
make the approaches more acceptable (Huynh, Henry and Dosani 2015). It is also seen that
sociopolitical factors affect the adaption of compassion in palliative care professionals. This
can be overcome by careful handling of the reasons leading to non-adaption of compassion to
avoid any outrage among the professionals regarding their belief. This case can be improved
by counselling the professionals and also making them realize the importance of compassion.
They should be given real-life scenarios regarding their personal lives which would bring
their conscience and make them tenacious in providing compassion while treating the
patients.
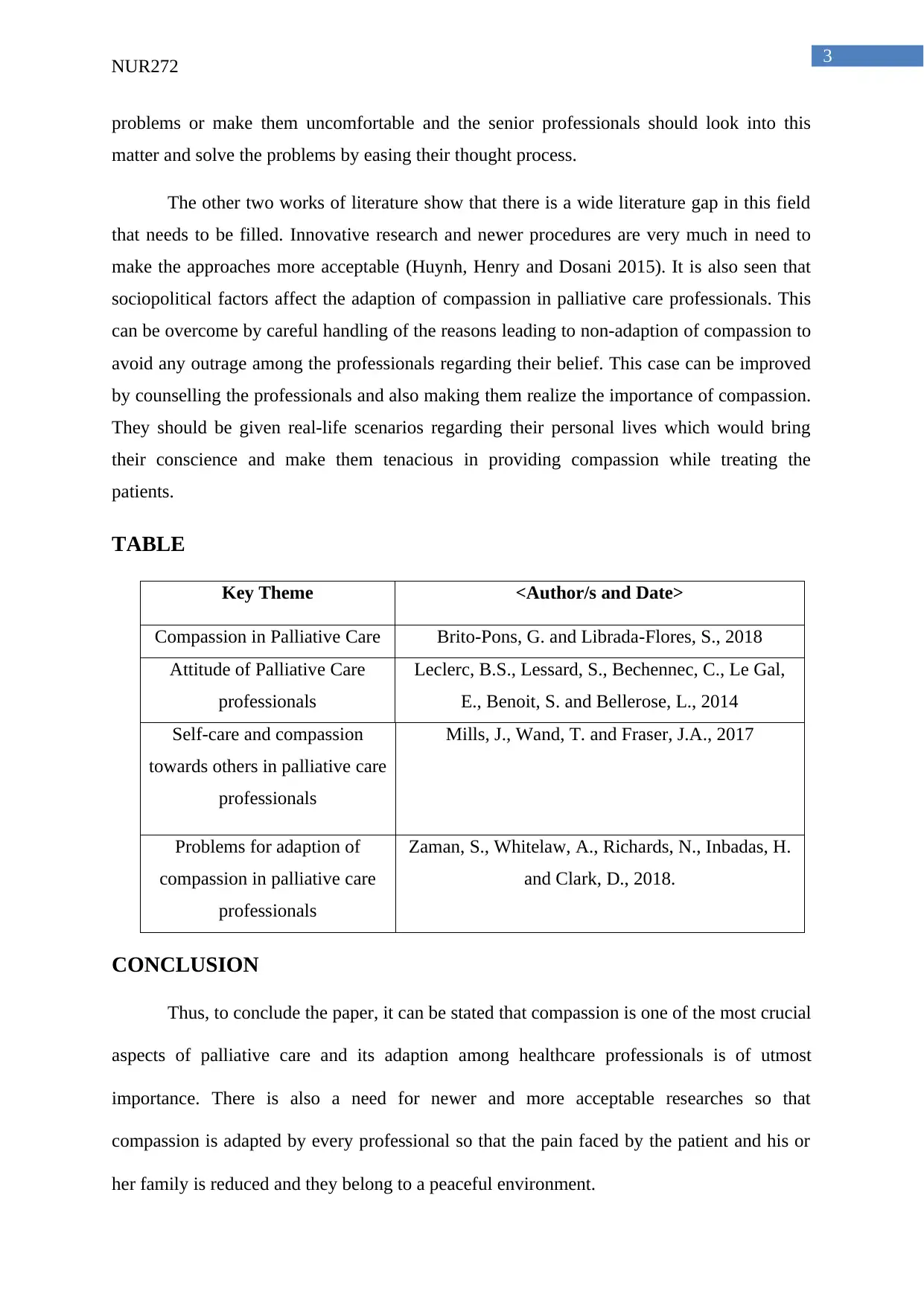
TABLE
Key Theme <Author/s and Date>
Compassion in Palliative Care Brito-Pons, G. and Librada-Flores, S., 2018
Attitude of Palliative Care
professionals
Leclerc, B.S., Lessard, S., Bechennec, C., Le Gal,
E., Benoit, S. and Bellerose, L., 2014
Self-care and compassion
towards others in palliative care
professionals
Mills, J., Wand, T. and Fraser, J.A., 2017
Problems for adaption of
compassion in palliative care
professionals
Zaman, S., Whitelaw, A., Richards, N., Inbadas, H.
and Clark, D., 2018.
CONCLUSION
Thus, to conclude the paper, it can be stated that compassion is one of the most crucial
aspects of palliative care and its adaption among healthcare professionals is of utmost
importance. There is also a need for newer and more acceptable researches so that
compassion is adapted by every professional so that the pain faced by the patient and his or
her family is reduced and they belong to a peaceful environment.
NUR272
problems or make them uncomfortable and the senior professionals should look into this
matter and solve the problems by easing their thought process.
The other two works of literature show that there is a wide literature gap in this field
that needs to be filled. Innovative research and newer procedures are very much in need to
make the approaches more acceptable (Huynh, Henry and Dosani 2015). It is also seen that
sociopolitical factors affect the adaption of compassion in palliative care professionals. This
can be overcome by careful handling of the reasons leading to non-adaption of compassion to
avoid any outrage among the professionals regarding their belief. This case can be improved
by counselling the professionals and also making them realize the importance of compassion.
They should be given real-life scenarios regarding their personal lives which would bring
their conscience and make them tenacious in providing compassion while treating the
patients.
TABLE
Key Theme <Author/s and Date>
Compassion in Palliative Care Brito-Pons, G. and Librada-Flores, S., 2018
Attitude of Palliative Care
professionals
Leclerc, B.S., Lessard, S., Bechennec, C., Le Gal,
E., Benoit, S. and Bellerose, L., 2014
Self-care and compassion
towards others in palliative care
professionals
Mills, J., Wand, T. and Fraser, J.A., 2017
Problems for adaption of
compassion in palliative care
professionals
Zaman, S., Whitelaw, A., Richards, N., Inbadas, H.
and Clark, D., 2018.
CONCLUSION
Thus, to conclude the paper, it can be stated that compassion is one of the most crucial
aspects of palliative care and its adaption among healthcare professionals is of utmost
importance. There is also a need for newer and more acceptable researches so that
compassion is adapted by every professional so that the pain faced by the patient and his or
her family is reduced and they belong to a peaceful environment.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
NUR272
REFERENCES
Brito-Pons, G. and Librada-Flores, S., 2018. Compassion in palliative care: a review. Current
opinion in supportive and palliative care, 12(4), pp.472-479.
Centeno C, Lynch T, Garralda E, Carrasco JM, Guillen-Grima F, Clark D. Coverage and
development of specialist palliative care services across the World Health Organization
European Region (2005–2012): Results from a European Association for Palliative Care Task
Force survey of 53 Countries. Palliative Medicine. 2016;30(4):351-362.
doi:10.1177/0269216315598671.
Palliative Care Australia (2020). National Palliative Care Standards. [ebook] Canberra:
Palliative Care Australia. Available at:
(https://palliativecare.org.au/wp-content/uploads/dlm_uploads/2018/11/PalliativeCare-
National-Standards-2018_Nov-web.pdf [Accessed 22 Feb. 2020]. Kelley, A.S. and Morrison,
R.S., 2015. Palliative care for the seriously ill. New England Journal of Medicine, 373(8),
pp.747-755.
Leclerc, B.S., Lessard, S., Bechennec, C., Le Gal, E., Benoit, S. and Bellerose, L., 2014.
Attitudes toward death, dying, end-of-life palliative care, and interdisciplinary practice in
long term care workers. Journal of the American Medical Directors Association, 15(3),
pp.207-213.
Mills, J., Wand, T. and Fraser, J.A., 2017. Palliative care professionals' care and compassion
for self and others: a narrative review.
Zaman, S., Whitelaw, A., Richards, N., Inbadas, H. and Clark, D., 2018. A moment for
compassion: emerging rhetorics in end-of-life care. Medical humanities, 44(2), pp.140-143.
Kelley, A.S. and Morrison, R.S., 2015. Palliative care for the seriously ill. New England
Journal of Medicine, 373(8), pp.747-755.
Centeno, C., Ballesteros, M., Carrasco, J.M. and Arantzamendi, M., 2016. Does palliative
care education matter to medical students? The experience of attending an undergraduate
course in palliative care. BMJ supportive & palliative care, 6(1), pp.128-134.
NUR272
REFERENCES
Brito-Pons, G. and Librada-Flores, S., 2018. Compassion in palliative care: a review. Current
opinion in supportive and palliative care, 12(4), pp.472-479.
Centeno C, Lynch T, Garralda E, Carrasco JM, Guillen-Grima F, Clark D. Coverage and
development of specialist palliative care services across the World Health Organization
European Region (2005–2012): Results from a European Association for Palliative Care Task
Force survey of 53 Countries. Palliative Medicine. 2016;30(4):351-362.
doi:10.1177/0269216315598671.
Palliative Care Australia (2020). National Palliative Care Standards. [ebook] Canberra:
Palliative Care Australia. Available at:
(https://palliativecare.org.au/wp-content/uploads/dlm_uploads/2018/11/PalliativeCare-
National-Standards-2018_Nov-web.pdf [Accessed 22 Feb. 2020]. Kelley, A.S. and Morrison,
R.S., 2015. Palliative care for the seriously ill. New England Journal of Medicine, 373(8),
pp.747-755.
Leclerc, B.S., Lessard, S., Bechennec, C., Le Gal, E., Benoit, S. and Bellerose, L., 2014.
Attitudes toward death, dying, end-of-life palliative care, and interdisciplinary practice in
long term care workers. Journal of the American Medical Directors Association, 15(3),
pp.207-213.
Mills, J., Wand, T. and Fraser, J.A., 2017. Palliative care professionals' care and compassion
for self and others: a narrative review.
Zaman, S., Whitelaw, A., Richards, N., Inbadas, H. and Clark, D., 2018. A moment for
compassion: emerging rhetorics in end-of-life care. Medical humanities, 44(2), pp.140-143.
Kelley, A.S. and Morrison, R.S., 2015. Palliative care for the seriously ill. New England
Journal of Medicine, 373(8), pp.747-755.
Centeno, C., Ballesteros, M., Carrasco, J.M. and Arantzamendi, M., 2016. Does palliative
care education matter to medical students? The experience of attending an undergraduate
course in palliative care. BMJ supportive & palliative care, 6(1), pp.128-134.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

5
NUR272
Huynh, L., Henry, B. and Dosani, N., 2015. Minding the gap: access to palliative care and the
homeless. BMC palliative care, 14(1), p.62.
NUR272
Huynh, L., Henry, B. and Dosani, N., 2015. Minding the gap: access to palliative care and the
homeless. BMC palliative care, 14(1), p.62.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





