BIOP211: Pharmacology of Paracetamol - Mechanism, Uses, and Safety
VerifiedAdded on 2022/10/12
|9
|2332
|416
Report
AI Summary
This report provides a detailed analysis of paracetamol, a widely used analgesic and antipyretic drug. It explores the drug's mechanism of action, focusing on its role in inhibiting prostaglandin synthesis within the central nervous system, and discusses its therapeutic uses for conditions like headaches, pain, osteoarthritis, and fever. The report also examines the routes of administration, adverse effects, and contraindications of paracetamol, including the risks associated with high doses and long-term use, such as liver damage. Furthermore, it addresses the importance of considering potential drug interactions, particularly with Chinese herbs and nutritional supplements, to ensure patient safety and maximize therapeutic efficacy. The report also touches on the human physiology of the disease to which the drug is indicated, focusing on pain management in osteoporosis. Overall, the report emphasizes the need for appropriate dosing, patient education, and monitoring to promote the safe and effective use of paracetamol.

Running head: PHARMACOLOGY
Pharmacology
Name of the student:
Name of the University:
Author’s note
Pharmacology
Name of the student:
Name of the University:
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PHARMACOLOGY
Paracetamol or Acetaminophen is a drug that belongs to the drug class of analgesics and
antipyretics. It is indicated for use in patients with fever and mild to moderate pain such as
migraine. Although it is a weaker analgesic compared to NSAIDs (non-steroidal anti-
inflammatory drugs) or COX-2 selective inhibitors, it is used because of better tolerance
(Graham et al., 2013). The essay gives better understanding of the therapeutic action and
pharmacology of the drug by discussing by discussing about the mechanism of action, route of
administration, adverse effects and contraindications of the drug. It also gives idea regarding the
human physiology of the disease to which the drug is indicated. The essay discusses about
interactions between paracetamol and Chinese herbs and suggests strategies to prevent adverse
reactions between the two.
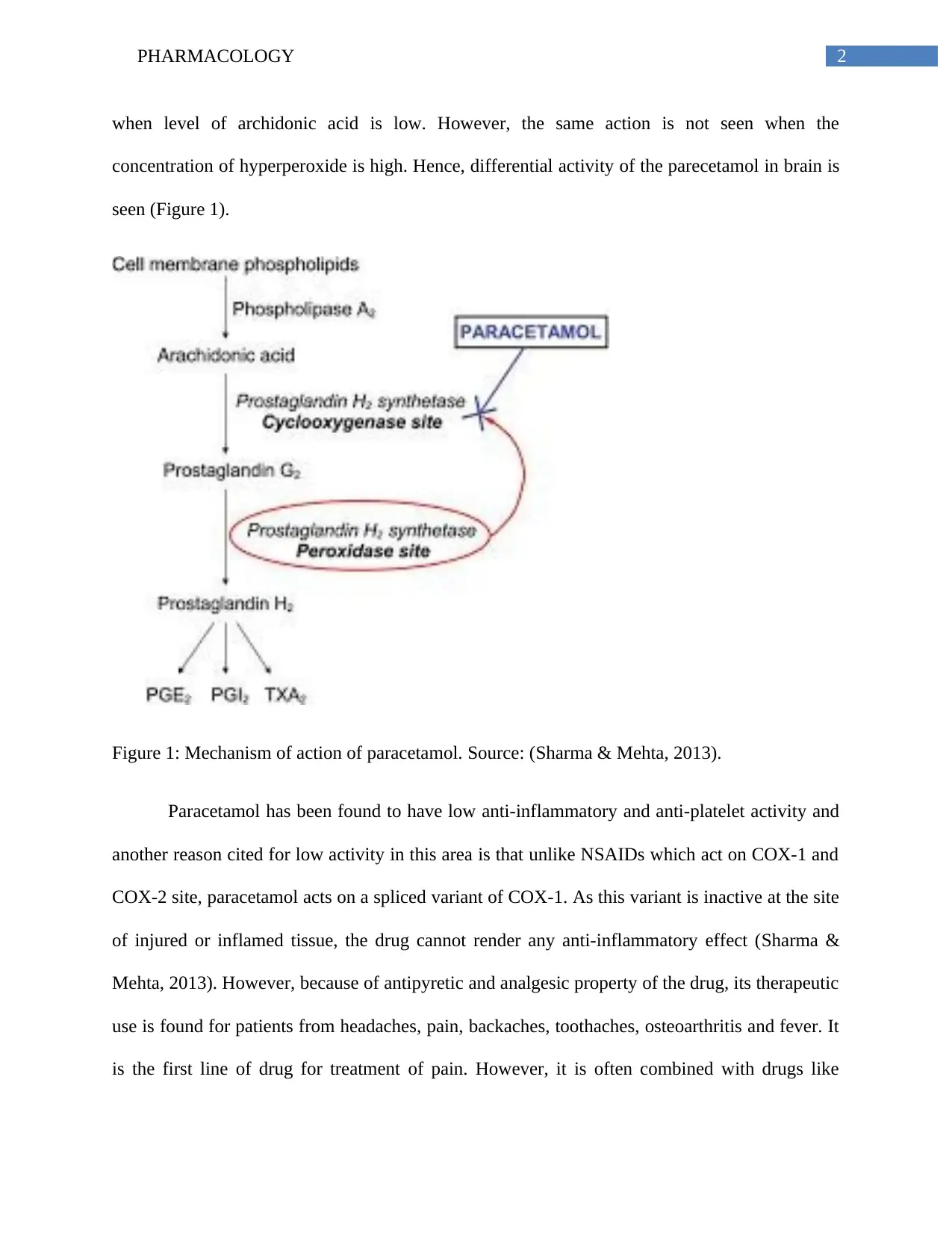
Parecetamol is renowned as one of the widely used non-prescribed medication of its
therapeutic effect on pain and fever related outcomes. The main factor involved in the
therapeutic action of the drug is the function of paracetamol in inhibiting prostanglandin
synthesis within the central nervous system. However, unlike other drugs, it has no anti-
inflammatory benefits (Mallet, Eschalier & Daulhac, 2017). Although the exact mechanism of
the drug of action is not fully established in research literature, most research study show the
function of the drug in inhibiting the COX pathways and exerting central actions to provide relief
from pain symptoms. Sharma and Mehta (2013) gives the evidence regarding the detailed action
of the drug in inhibiting production of prostaglandins. Cyclooxygenase or prostaglandin H2
synthetase is an enzyme responsible for the metabolism of arachidonic acid to prostanoids and it
contain two active sites namely COX and the peroxidase. The enzymatic activity of COX occurs
in the oxidized form. However, paracetamol forms co-substrate at the POX site to interfere with
the function of the COX enzyme. Parecetamol act as a potent inhibitor of prostaglandin synthesis
Paracetamol or Acetaminophen is a drug that belongs to the drug class of analgesics and
antipyretics. It is indicated for use in patients with fever and mild to moderate pain such as
migraine. Although it is a weaker analgesic compared to NSAIDs (non-steroidal anti-
inflammatory drugs) or COX-2 selective inhibitors, it is used because of better tolerance
(Graham et al., 2013). The essay gives better understanding of the therapeutic action and
pharmacology of the drug by discussing by discussing about the mechanism of action, route of
administration, adverse effects and contraindications of the drug. It also gives idea regarding the
human physiology of the disease to which the drug is indicated. The essay discusses about
interactions between paracetamol and Chinese herbs and suggests strategies to prevent adverse
reactions between the two.
Parecetamol is renowned as one of the widely used non-prescribed medication of its
therapeutic effect on pain and fever related outcomes. The main factor involved in the
therapeutic action of the drug is the function of paracetamol in inhibiting prostanglandin
synthesis within the central nervous system. However, unlike other drugs, it has no anti-
inflammatory benefits (Mallet, Eschalier & Daulhac, 2017). Although the exact mechanism of
the drug of action is not fully established in research literature, most research study show the
function of the drug in inhibiting the COX pathways and exerting central actions to provide relief
from pain symptoms. Sharma and Mehta (2013) gives the evidence regarding the detailed action
of the drug in inhibiting production of prostaglandins. Cyclooxygenase or prostaglandin H2
synthetase is an enzyme responsible for the metabolism of arachidonic acid to prostanoids and it
contain two active sites namely COX and the peroxidase. The enzymatic activity of COX occurs
in the oxidized form. However, paracetamol forms co-substrate at the POX site to interfere with
the function of the COX enzyme. Parecetamol act as a potent inhibitor of prostaglandin synthesis
2PHARMACOLOGY
when level of archidonic acid is low. However, the same action is not seen when the
concentration of hyperperoxide is high. Hence, differential activity of the parecetamol in brain is
seen (Figure 1).
Figure 1: Mechanism of action of paracetamol. Source: (Sharma & Mehta, 2013).
Paracetamol has been found to have low anti-inflammatory and anti-platelet activity and
another reason cited for low activity in this area is that unlike NSAIDs which act on COX-1 and
COX-2 site, paracetamol acts on a spliced variant of COX-1. As this variant is inactive at the site
of injured or inflamed tissue, the drug cannot render any anti-inflammatory effect (Sharma &
Mehta, 2013). However, because of antipyretic and analgesic property of the drug, its therapeutic
use is found for patients from headaches, pain, backaches, toothaches, osteoarthritis and fever. It
is the first line of drug for treatment of pain. However, it is often combined with drugs like
when level of archidonic acid is low. However, the same action is not seen when the
concentration of hyperperoxide is high. Hence, differential activity of the parecetamol in brain is
seen (Figure 1).
Figure 1: Mechanism of action of paracetamol. Source: (Sharma & Mehta, 2013).
Paracetamol has been found to have low anti-inflammatory and anti-platelet activity and
another reason cited for low activity in this area is that unlike NSAIDs which act on COX-1 and
COX-2 site, paracetamol acts on a spliced variant of COX-1. As this variant is inactive at the site
of injured or inflamed tissue, the drug cannot render any anti-inflammatory effect (Sharma &
Mehta, 2013). However, because of antipyretic and analgesic property of the drug, its therapeutic
use is found for patients from headaches, pain, backaches, toothaches, osteoarthritis and fever. It
is the first line of drug for treatment of pain. However, it is often combined with drugs like
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PHARMACOLOGY
ibuprofen to improve analgesic efficacy. For example, Paolucci, Saraceni and Piccinini (2016)
give the evidence regarding the wide use of paracetmol for mild pain in patients with
osteoporosis. In case of strong pain, treatment with opioids as well as paracetamol is done for
patients with osteoporosis. Such adjuvant drugs contribute to pain relief as well as increase in
analgesic effects. Similarly, acetaminophen is recommended as the first choice of drug for
people with non-specific low back pain (Saragiotto et al., 2016).
Hence, the clinical efficacy of the drug for treating pain is proved and it is safe to be used
when appropriate dose is taken. While administering this drug to patient, considering appropriate
dose consideration is important because high dose or long-term use of the drug has been found to
lead to liver failure, cardiovascular events and even deaths for some patient (Saragiotto et al.,
2016). A dose of 10-15 may cause severe liver damage and dose of 50 tablets can be fatal unless
acteylcysteine, an antidote is immediately provided to patient (Sandilands, Morrison & Bateman,
2016). Because of adverse effects due to large dose of paracetamol, fixed dose combination of
analgesic product is often used to treat pain. For example, paracetamol is found to be widely
used in combination with drugs like oxycodone, tramadol and codeine. The advantage of such
combination is that such dose reduces pill burden and require lower doses. They reduce the
challenges of opioid overdose in pain management too as such drug combination provides
analgesia at lower dose compared to opioid taken alone (Morón Merchante et al., 2013).
McCrae et al. (2018) explains long-term use of paracetamol should be restricted because
of the adverse effect of gastrointestinal bleeding and increase in blood pressure for patients. This
evidence gives the implication that to promote patient safety, giving patients knowledge about
adverse effects and contraindications of the drug is important. Although there are no serious
side-effects of this drug, however in very rare cases allergic reaction is seen evidenced by
ibuprofen to improve analgesic efficacy. For example, Paolucci, Saraceni and Piccinini (2016)
give the evidence regarding the wide use of paracetmol for mild pain in patients with
osteoporosis. In case of strong pain, treatment with opioids as well as paracetamol is done for
patients with osteoporosis. Such adjuvant drugs contribute to pain relief as well as increase in
analgesic effects. Similarly, acetaminophen is recommended as the first choice of drug for
people with non-specific low back pain (Saragiotto et al., 2016).
Hence, the clinical efficacy of the drug for treating pain is proved and it is safe to be used
when appropriate dose is taken. While administering this drug to patient, considering appropriate
dose consideration is important because high dose or long-term use of the drug has been found to
lead to liver failure, cardiovascular events and even deaths for some patient (Saragiotto et al.,
2016). A dose of 10-15 may cause severe liver damage and dose of 50 tablets can be fatal unless
acteylcysteine, an antidote is immediately provided to patient (Sandilands, Morrison & Bateman,
2016). Because of adverse effects due to large dose of paracetamol, fixed dose combination of
analgesic product is often used to treat pain. For example, paracetamol is found to be widely
used in combination with drugs like oxycodone, tramadol and codeine. The advantage of such
combination is that such dose reduces pill burden and require lower doses. They reduce the
challenges of opioid overdose in pain management too as such drug combination provides
analgesia at lower dose compared to opioid taken alone (Morón Merchante et al., 2013).
McCrae et al. (2018) explains long-term use of paracetamol should be restricted because
of the adverse effect of gastrointestinal bleeding and increase in blood pressure for patients. This
evidence gives the implication that to promote patient safety, giving patients knowledge about
adverse effects and contraindications of the drug is important. Although there are no serious
side-effects of this drug, however in very rare cases allergic reaction is seen evidenced by
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PHARMACOLOGY
symptoms of rashes, dizziness and itching. Patients must be notified regarding this and asked to
contact clinician or pharmacist when they witness adverse side-effects of the drug. Knowledge
about contraindication of the drug is critical to patient safety too. Conditions like liver problem,
renal impairment, shock and acute inflammation of the liver are contraindicated with
paracetamol. Therefore, use of drug in this group of patients should be avoided.
Paracetamol has therapeutic use for providing pain relief to patients with headaches, pain,
backaches, toothaches, osteoarthritis and fever. Osteoporosis is a condition where skeletal bone
mass is affected and it results in changes in bone resorption and bone formation. It is systematic
skeletal disorder resulting in imbalance in bone remodeling and reduction in bone strengths.
Bone pain is the most serious issue in patients with osteoporosis. Although the mechanism of
pain is not clear, one explanation for pain is hypermodelling of bone resulting in changes in bone
innervations and osteoclasts. Bone innervation is responsible for maintaining homeostasis.
However, with decline in age, bone mass and bone strength is decreased resulting in changes in
bone innervations (Mediati, Vellucci & Dodaro, 2014). Hence, paracetamol is indicated in the
management of pain in patients with osteoporosis as it relieved pain by exerting action on the
central nervous system. The drug is also used to treat back pain in elderly patients and
osteoporosis is the main cause behind lower back pain.
To ensure maximum therapeutic effect and reduce any risk of patient safety event for
patient, it is crucial to monitor if patients are taking any western herb or Chinese herb or
nutritional supplements along with Paracetamol. This is because the drug has serious interactions
with traditional drugs taken by patient. Some common Chinese herb includes leaves, roots,
flowers and seeds of different plants like cinnamon, ginger, rhubarb and tai chi. Cinnamon is
often used by patients to manage pain in arthritis and other chronic disease because of its
symptoms of rashes, dizziness and itching. Patients must be notified regarding this and asked to
contact clinician or pharmacist when they witness adverse side-effects of the drug. Knowledge
about contraindication of the drug is critical to patient safety too. Conditions like liver problem,
renal impairment, shock and acute inflammation of the liver are contraindicated with
paracetamol. Therefore, use of drug in this group of patients should be avoided.
Paracetamol has therapeutic use for providing pain relief to patients with headaches, pain,
backaches, toothaches, osteoarthritis and fever. Osteoporosis is a condition where skeletal bone
mass is affected and it results in changes in bone resorption and bone formation. It is systematic
skeletal disorder resulting in imbalance in bone remodeling and reduction in bone strengths.
Bone pain is the most serious issue in patients with osteoporosis. Although the mechanism of
pain is not clear, one explanation for pain is hypermodelling of bone resulting in changes in bone
innervations and osteoclasts. Bone innervation is responsible for maintaining homeostasis.
However, with decline in age, bone mass and bone strength is decreased resulting in changes in
bone innervations (Mediati, Vellucci & Dodaro, 2014). Hence, paracetamol is indicated in the
management of pain in patients with osteoporosis as it relieved pain by exerting action on the
central nervous system. The drug is also used to treat back pain in elderly patients and
osteoporosis is the main cause behind lower back pain.
To ensure maximum therapeutic effect and reduce any risk of patient safety event for
patient, it is crucial to monitor if patients are taking any western herb or Chinese herb or
nutritional supplements along with Paracetamol. This is because the drug has serious interactions
with traditional drugs taken by patient. Some common Chinese herb includes leaves, roots,
flowers and seeds of different plants like cinnamon, ginger, rhubarb and tai chi. Cinnamon is
often used by patients to manage pain in arthritis and other chronic disease because of its
5PHARMACOLOGY
inflammation lowering effect (Gharaiy et al., 2017). Chen et al. (2013) argues that despite
advance medical treatment, patients preference for Chinese herbal product is a major challenge
in disease treatment and prevention. As Chinese herb interferes with the pharmacokinetics of the
conventional drug, it is essential to monitor the effect of Chinese herb use in patients taking
paracetamol too. (Chen et al., 2013) gives the evidence that acetaminophen is the top five drug
that is often combined with conventional drugs. Izzo (2012) highlighted about the several
interactions of chinese herb with conventional drugs. For example, use of garlic with
paracetamol was found to induce changes in paracetamol pharmacokinetics and symptoms of
hypoglycemia. Hence, monitoring the potential drug-herb interaction is critical in the initial
phase of treatment only.
Paracetamol is known to have adverse effects or interaction with food or nutritional
supplements too. For example, patients taking vitamin supplements should avoid taking the drug
because it affects the metabolism of the drug in the patient body and increase the possibility of
adverse effects for patient. Hence, avoiding that nutritional supplement is critical to promote
clinical efficacy of the drug. In case any patients need to take the herbal drugs or nutritional
supplements, another action that can be taken to reduce the adverse effect of the drugs include
adjusting the dose of paracetamol (Wu et al., 2018).
To conclude, from the comprehensive discussion regarding the pharmacology of
paracetamol, it can be concluded that the drug is an efficient drug for management of pain in
patients. It shows analgesic effect by inhibition of the action of prostaglandin, however it has no
anti-inflammatory effects. The essay revealed therapeutic efficacy of the drugs in pain
management and also revealed increased clinical effectiveness when used with fixed dose
combination. This combination promotes safety of patient. The essay gave indications regarding
inflammation lowering effect (Gharaiy et al., 2017). Chen et al. (2013) argues that despite
advance medical treatment, patients preference for Chinese herbal product is a major challenge
in disease treatment and prevention. As Chinese herb interferes with the pharmacokinetics of the
conventional drug, it is essential to monitor the effect of Chinese herb use in patients taking
paracetamol too. (Chen et al., 2013) gives the evidence that acetaminophen is the top five drug
that is often combined with conventional drugs. Izzo (2012) highlighted about the several
interactions of chinese herb with conventional drugs. For example, use of garlic with
paracetamol was found to induce changes in paracetamol pharmacokinetics and symptoms of
hypoglycemia. Hence, monitoring the potential drug-herb interaction is critical in the initial
phase of treatment only.
Paracetamol is known to have adverse effects or interaction with food or nutritional
supplements too. For example, patients taking vitamin supplements should avoid taking the drug
because it affects the metabolism of the drug in the patient body and increase the possibility of
adverse effects for patient. Hence, avoiding that nutritional supplement is critical to promote
clinical efficacy of the drug. In case any patients need to take the herbal drugs or nutritional
supplements, another action that can be taken to reduce the adverse effect of the drugs include
adjusting the dose of paracetamol (Wu et al., 2018).
To conclude, from the comprehensive discussion regarding the pharmacology of
paracetamol, it can be concluded that the drug is an efficient drug for management of pain in
patients. It shows analgesic effect by inhibition of the action of prostaglandin, however it has no
anti-inflammatory effects. The essay revealed therapeutic efficacy of the drugs in pain
management and also revealed increased clinical effectiveness when used with fixed dose
combination. This combination promotes safety of patient. The essay gave indications regarding
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PHARMACOLOGY
considering the impact of drugs on patient outcome by providing appropriate dose and limiting
overdose of drugs. The drug is found to beneficial for use of initial pain management because of
limited drug-drug interactions. There drug was found to have no severe adverse reaction.
However, research literature gave evidence regarding the hazards of long-term use of the drug.
Hence, long-term used should be strictly monitored and adequate patient education should be
prioritized to ensure safe use of the drug.
considering the impact of drugs on patient outcome by providing appropriate dose and limiting
overdose of drugs. The drug is found to beneficial for use of initial pain management because of
limited drug-drug interactions. There drug was found to have no severe adverse reaction.
However, research literature gave evidence regarding the hazards of long-term use of the drug.
Hence, long-term used should be strictly monitored and adequate patient education should be
prioritized to ensure safe use of the drug.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PHARMACOLOGY
References:
Chen, M. C., Lai, J. N., Chen, P. C., & Wang, J. D. (2013). Concurrent use of conventional drugs with
Chinese herbal products in Taiwan: a population-based study. Journal of traditional and
complementary medicine, 3(4), 256-262.
Gharaiy, N. R., Shahnazi, M., Kia, P. Y., & Javadzadeh, Y. (2017). The Effect of Cinnamon on Cyclical
Breast Pain. Iranian Red Crescent Medical Journal, 19(6).
Graham, G. G., Davies, M. J., Day, R. O., Mohamudally, A., & Scott, K. F. (2013). The modern
pharmacology of paracetamol: therapeutic actions, mechanism of action, metabolism, toxicity
and recent pharmacological findings. Inflammopharmacology, 21(3), 201-232.
Izzo, A. A. (2012). Interactions between herbs and conventional drugs: overview of the clinical
data. Medical Principles and Practice, 21(5), 404-428.
Mallet, C., Eschalier, A., & Daulhac, L. (2017). Paracetamol: update on its analgesic mechanism of
action. Pain relief–From analgesics to alternative therapies.
McCrae, J. C., Morrison, E. E., MacIntyre, I. M., Dear, J. W., & Webb, D. J. (2018). Long‐term adverse
effects of paracetamol–a review. British journal of clinical pharmacology, 84(10), 2218-2230.
Mediati, R. D., Vellucci, R., & Dodaro, L. (2014). Pathogenesis and clinical aspects of pain in patients
with osteoporosis. Clinical Cases in Mineral and Bone Metabolism, 11(3), 169.
Morón Merchante, I., Pergolizzi, J. V., van de Laar, M., Mellinghoff, H. U., Nalamachu, S., O'Brien,
J., ... & Raffa, R. B. (2013). Tramadol/Paracetamol fixed-dose combination for chronic pain
management in family practice: a clinical review. ISRN family medicine, 2013.
References:
Chen, M. C., Lai, J. N., Chen, P. C., & Wang, J. D. (2013). Concurrent use of conventional drugs with
Chinese herbal products in Taiwan: a population-based study. Journal of traditional and
complementary medicine, 3(4), 256-262.
Gharaiy, N. R., Shahnazi, M., Kia, P. Y., & Javadzadeh, Y. (2017). The Effect of Cinnamon on Cyclical
Breast Pain. Iranian Red Crescent Medical Journal, 19(6).
Graham, G. G., Davies, M. J., Day, R. O., Mohamudally, A., & Scott, K. F. (2013). The modern
pharmacology of paracetamol: therapeutic actions, mechanism of action, metabolism, toxicity
and recent pharmacological findings. Inflammopharmacology, 21(3), 201-232.
Izzo, A. A. (2012). Interactions between herbs and conventional drugs: overview of the clinical
data. Medical Principles and Practice, 21(5), 404-428.
Mallet, C., Eschalier, A., & Daulhac, L. (2017). Paracetamol: update on its analgesic mechanism of
action. Pain relief–From analgesics to alternative therapies.
McCrae, J. C., Morrison, E. E., MacIntyre, I. M., Dear, J. W., & Webb, D. J. (2018). Long‐term adverse
effects of paracetamol–a review. British journal of clinical pharmacology, 84(10), 2218-2230.
Mediati, R. D., Vellucci, R., & Dodaro, L. (2014). Pathogenesis and clinical aspects of pain in patients
with osteoporosis. Clinical Cases in Mineral and Bone Metabolism, 11(3), 169.
Morón Merchante, I., Pergolizzi, J. V., van de Laar, M., Mellinghoff, H. U., Nalamachu, S., O'Brien,
J., ... & Raffa, R. B. (2013). Tramadol/Paracetamol fixed-dose combination for chronic pain
management in family practice: a clinical review. ISRN family medicine, 2013.
8PHARMACOLOGY
Paolucci, T., Saraceni, V. M., & Piccinini, G. (2016). Management of chronic pain in osteoporosis:
challenges and solutions. Journal of pain research, 9, 177.
Sandilands, E. A., Morrison, E. E., & Bateman, D. N. (2016). Adverse reactions to intravenous
acetylcysteine in paracetamol poisoning. Adverse drug reaction bulletin, 297(1), 1147-1150.
Saragiotto, B. T., Machado, G. C., Ferreira, M. L., Pinheiro, M. B., Shaheed, C. A., & Maher, C. G.
(2016). Paracetamol for low back pain. Cochrane Database of Systematic Reviews, (6).
Sharma, C. V., & Mehta, V. (2013). Paracetamol: mechanisms and updates. Continuing Education in
Anaesthesia, Critical Care & Pain, 14(4), 153-158.
Wu, Z., Camargo Jr, C. A., Malihi, Z., Bartley, J., Waayer, D., Lawes, C. M., ... & Scragg, R. (2018).
Monthly vitamin D supplementation, pain, and pattern of analgesic prescription: secondary
analysis from the randomized, double-blind, placebo-controlled Vitamin D Assessment
study. Pain, 159(6), 1074-1082.
Paolucci, T., Saraceni, V. M., & Piccinini, G. (2016). Management of chronic pain in osteoporosis:
challenges and solutions. Journal of pain research, 9, 177.
Sandilands, E. A., Morrison, E. E., & Bateman, D. N. (2016). Adverse reactions to intravenous
acetylcysteine in paracetamol poisoning. Adverse drug reaction bulletin, 297(1), 1147-1150.
Saragiotto, B. T., Machado, G. C., Ferreira, M. L., Pinheiro, M. B., Shaheed, C. A., & Maher, C. G.
(2016). Paracetamol for low back pain. Cochrane Database of Systematic Reviews, (6).
Sharma, C. V., & Mehta, V. (2013). Paracetamol: mechanisms and updates. Continuing Education in
Anaesthesia, Critical Care & Pain, 14(4), 153-158.
Wu, Z., Camargo Jr, C. A., Malihi, Z., Bartley, J., Waayer, D., Lawes, C. M., ... & Scragg, R. (2018).
Monthly vitamin D supplementation, pain, and pattern of analgesic prescription: secondary
analysis from the randomized, double-blind, placebo-controlled Vitamin D Assessment
study. Pain, 159(6), 1074-1082.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





