Paramedics: Assessment of Cardiovascular and Neurological Conditions
VerifiedAdded on 2023/06/10
|20
|4810
|57
Homework Assignment
AI Summary
This document presents solutions to a paramedics assignment, encompassing a short answer quiz and a case study. The quiz covers key aspects of cardiovascular assessment, including recording patient history, identifying pulse sites, and understanding blood pressure measurement. It also addresses the importance of perfusion assessment and interpreting vital signs. The case study focuses on a patient experiencing chest pain, simulating a potential heart attack scenario. It explores initial patient assessment, including symptom identification, the PQRST pain assessment method, and interpretation of vital signs such as heart rate, blood pressure, and oxygen saturation. Furthermore, the document includes a neurological assessment section, covering the neurological exam, common causes of altered mental status, the Glasgow Coma Scale, the Romberg test, and the significance of pupillary reactivity and Cushing's triad. This comprehensive resource provides valuable insights into critical aspects of paramedic practice and patient care.

Running head: PARAMEDICS
PARAMEDICS
Name of the Student:
Name of the University:
Author Note:
PARAMEDICS
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PARAMEDICS
CP2 8.6 - SHORT ANSWER QUIZ
1. Important information required for recording history of the cardiovascular diseases
include noting down of the onset time of the symptom, its duration, the severity of the
symptom, its course, whether the symptoms are continuous or intermittent and its
associated features such as fever or malaise. Finally consideration should be given to
whether the patient has experienced similar symptom previously or not.
2. Commonly palpated pulse sites are carotid artery, brachial artery, radial artery,
femoral artery and popliteal artery. The carotid artery is palpated on the neck below
the jaw and lateral to the larynx/trachea using the middle and index fingers. The
brachial artery papates on the anterior side of the elbow by applying pressure gently
on the artery against the underlying bone with the middle and index fingers. The
radial pulse is palpated immediately above the wrist joint near the base of the thumb
or in the anatomical snuff box, by applying pressure gently against the underlying
bone with the middle and index fingers. The femoral pulse is palpated over the ventral
thigh between the pubic symphysis and anterior superior iliac spine with the middle
and index fingers and the popliteal pulse is palpated on the posterior knee with the
middle and index fingers; the palpation of this pulse is more difficult as compared to
other pulse sites.
3. It is required to assess the palpating pulse for full 60 seconds as it highlights the
abnormalities which are not detected during the shorter assessment interval. This is
required as using shorter time period increases the errors of calculation up to four to
six fold. A patient possessing atrial fibrillation, is generally seen to have a regular
pulse when 9t is being assessed for a period of 30seconds or less than that.
CP2 8.6 - SHORT ANSWER QUIZ
1. Important information required for recording history of the cardiovascular diseases
include noting down of the onset time of the symptom, its duration, the severity of the
symptom, its course, whether the symptoms are continuous or intermittent and its
associated features such as fever or malaise. Finally consideration should be given to
whether the patient has experienced similar symptom previously or not.
2. Commonly palpated pulse sites are carotid artery, brachial artery, radial artery,
femoral artery and popliteal artery. The carotid artery is palpated on the neck below
the jaw and lateral to the larynx/trachea using the middle and index fingers. The
brachial artery papates on the anterior side of the elbow by applying pressure gently
on the artery against the underlying bone with the middle and index fingers. The
radial pulse is palpated immediately above the wrist joint near the base of the thumb
or in the anatomical snuff box, by applying pressure gently against the underlying
bone with the middle and index fingers. The femoral pulse is palpated over the ventral
thigh between the pubic symphysis and anterior superior iliac spine with the middle
and index fingers and the popliteal pulse is palpated on the posterior knee with the
middle and index fingers; the palpation of this pulse is more difficult as compared to
other pulse sites.
3. It is required to assess the palpating pulse for full 60 seconds as it highlights the
abnormalities which are not detected during the shorter assessment interval. This is
required as using shorter time period increases the errors of calculation up to four to
six fold. A patient possessing atrial fibrillation, is generally seen to have a regular
pulse when 9t is being assessed for a period of 30seconds or less than that.
2PARAMEDICS
4. With the beating of the heart, there is pumping of blood round the body to give it the
needed energy and oxygen. On blood movement, it pushes against the sides of the
blood vessels. Blood pressure is this pressure with which these blood vessels are
pushed.
5. Blood pressure is measured by using two numbers. The first of which is called
systolic blood pressure. This is used to measure the pressure in the blood vessels
when the heart beats. The number of the top in 120/80 blood pressure reading is
systolic blood pressure.
6. The second number used for measuring blood pressure is called diastolic blood
pressure. This measures the pressure in the blood vessels when the heart rests in-
between the beats. The number of the bottom in 120/80 blood pressure reading is
systolic blood pressure.
7. Patient assessment is of great importance for determination of what management
therapies need to be provided. Perfusion is part of vital sign assessment. With the
deficiency of systemic perfusion there is usually a loss of initial blood flow and
pressure to the organs that are less crucial like the skin and the gastro-intestinal
system. This is needed to maintain more flow of blood to the vital organs like the
brain and the heart.
8. For determining the patient perfusion, various easily measurable evaluations are
made. These include the pulse rate, blood pressure, skin appearance and conscious
state assessment.
9. a. Pulse 50-100 bpm, 60-80 mmHg systolic, altered conscious status in relation to
time - Adequate perfusion
b. Skin – cool, pale, clammy, alert, BP 50-100bpm – Borderline perfusion
c. Unconscious, no pulses, unrecordable BP – No perfusion
4. With the beating of the heart, there is pumping of blood round the body to give it the
needed energy and oxygen. On blood movement, it pushes against the sides of the
blood vessels. Blood pressure is this pressure with which these blood vessels are
pushed.
5. Blood pressure is measured by using two numbers. The first of which is called
systolic blood pressure. This is used to measure the pressure in the blood vessels
when the heart beats. The number of the top in 120/80 blood pressure reading is
systolic blood pressure.
6. The second number used for measuring blood pressure is called diastolic blood
pressure. This measures the pressure in the blood vessels when the heart rests in-
between the beats. The number of the bottom in 120/80 blood pressure reading is
systolic blood pressure.
7. Patient assessment is of great importance for determination of what management
therapies need to be provided. Perfusion is part of vital sign assessment. With the
deficiency of systemic perfusion there is usually a loss of initial blood flow and
pressure to the organs that are less crucial like the skin and the gastro-intestinal
system. This is needed to maintain more flow of blood to the vital organs like the
brain and the heart.
8. For determining the patient perfusion, various easily measurable evaluations are
made. These include the pulse rate, blood pressure, skin appearance and conscious
state assessment.
9. a. Pulse 50-100 bpm, 60-80 mmHg systolic, altered conscious status in relation to
time - Adequate perfusion
b. Skin – cool, pale, clammy, alert, BP 50-100bpm – Borderline perfusion
c. Unconscious, no pulses, unrecordable BP – No perfusion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PARAMEDICS
8.9: Short Answer Quiz
1. Maintenance of privacy and confidentiality
2. Neurological assessment is also known as neuro exam is an assessment of evaluation of the
nervous system of a person and is done via instrument like lights and reflex hammers. Some
areas tested in the neurological assessment include measurement of the head circumference,
mental status of the person (patient’s level of awareness and interaction with the surrounding
environment); motor function or balance of the patients (via pushing or pulling the patient
against the hands of healthcare provider via his or her legs or arms); detection of the sensory
function (done via dull needles, alcohol swabs, tuning forks or other objects); evaluation of
the functioning of the 12 different cranial nerves originating from the brain and assessment of
the hand-eye co-ordination.
3. Common cause behind the alteration of the patient’s mental status include psychiatric
illness like schizophrenia or depression and acute brain dysfunction.
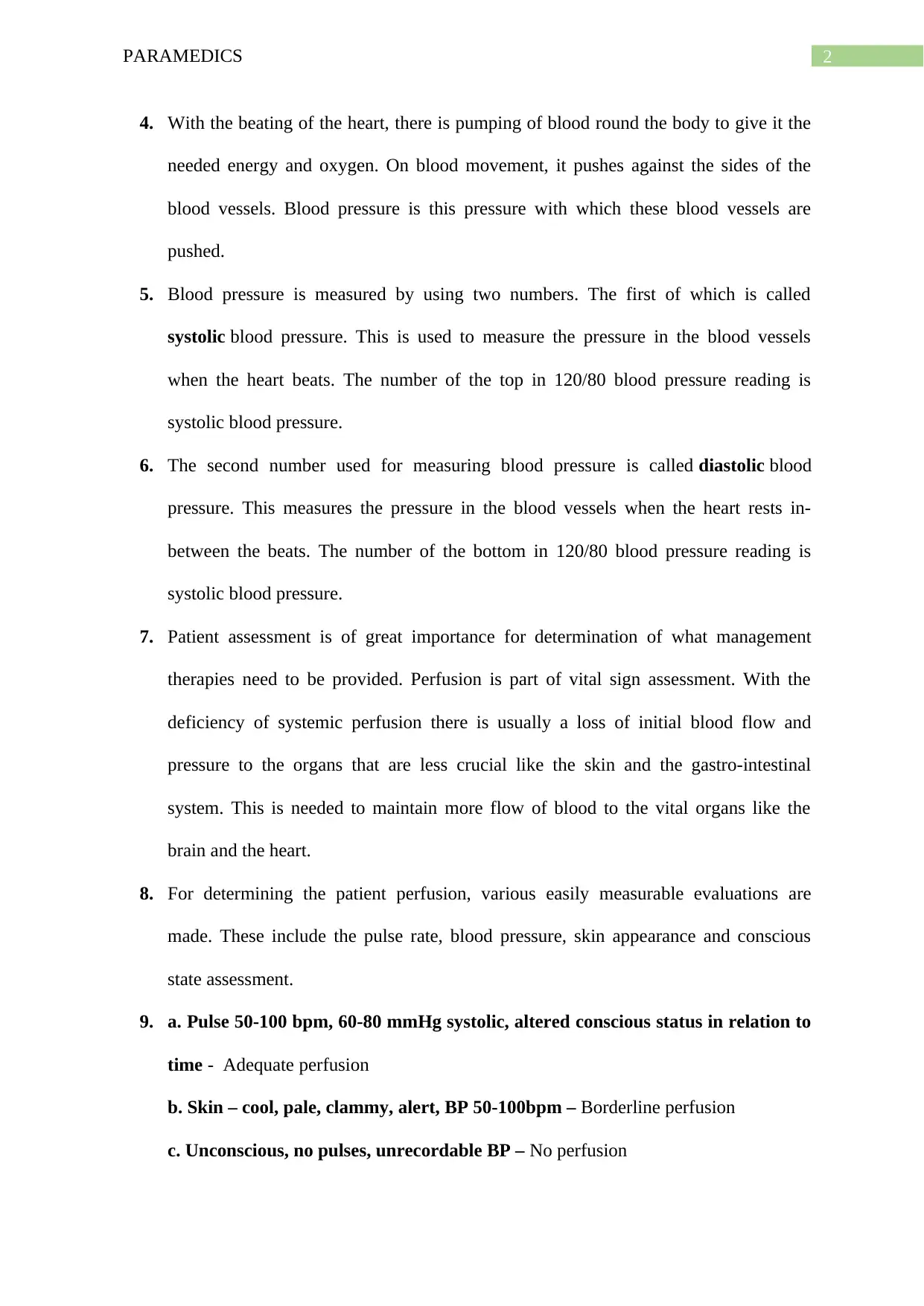
4.
Serial number Eye opening
Response
Best verbal
response
Best motor
response
Total score
a 2 4 5 11
b 4 3 6 13
c 8 or less
(Comatose
client)
d 1 1 1 3 (totally un
responsive)
8.9: Short Answer Quiz
1. Maintenance of privacy and confidentiality
2. Neurological assessment is also known as neuro exam is an assessment of evaluation of the
nervous system of a person and is done via instrument like lights and reflex hammers. Some
areas tested in the neurological assessment include measurement of the head circumference,
mental status of the person (patient’s level of awareness and interaction with the surrounding
environment); motor function or balance of the patients (via pushing or pulling the patient
against the hands of healthcare provider via his or her legs or arms); detection of the sensory
function (done via dull needles, alcohol swabs, tuning forks or other objects); evaluation of
the functioning of the 12 different cranial nerves originating from the brain and assessment of
the hand-eye co-ordination.
3. Common cause behind the alteration of the patient’s mental status include psychiatric
illness like schizophrenia or depression and acute brain dysfunction.
4.
Serial number Eye opening
Response
Best verbal
response
Best motor
response
Total score
a 2 4 5 11
b 4 3 6 13
c 8 or less
(Comatose
client)
d 1 1 1 3 (totally un
responsive)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PARAMEDICS
5. Romberg Test is use to examine the neurological function for balance and also use to text
driving under the influence of certain intoxication. The overall examination is based on the
premise that the person requires minimum two out of three senses to maintain the body
balance while in a standing position. Three main senses include proprioception, vestibular
function and vision
6. Examination limb strength of the patients helps in the assessment of the sensory modalities
of the limb and this help in the further assessment of the body balance. It provides additional
information about the motor movement and provide vital information about the developing
hemiparesis in the leg or arm in one side of the body that is either left or right.
7.
a. Space-occupying lesions: occurs in brain because of malignancy or other abnormal
pathological condition including haematoma or abscess. Majority of the intracerebral tumours
are primary and the remaining mainly originates outside the CNS. Examples: brain tumours
(primary of metastatic)
b. Oedema: characterised by excess accumulation of watery fluid in the cavities or tissues of
the body. Examples for oedema include cerebral oedema (extracellular fluid accumulation in
brain)
8. Pupillary reactivity is an early indicator which indicates increase of intracranial pressure
and is common among patients having severe traumatic brain injury There exist an inversely
proportional relationship between the intracranial pressure and papillary reactivity. Increase
intracranial pressure signifies decreased papillary activity.
9. ‘Cushing’s triad’ should not be confused with Cushing reflex. ‘Cushing’s triad’ is a sign
of increased intracranial pressure. The Triad mainly consists of hypertension (progressive
5. Romberg Test is use to examine the neurological function for balance and also use to text
driving under the influence of certain intoxication. The overall examination is based on the
premise that the person requires minimum two out of three senses to maintain the body
balance while in a standing position. Three main senses include proprioception, vestibular
function and vision
6. Examination limb strength of the patients helps in the assessment of the sensory modalities
of the limb and this help in the further assessment of the body balance. It provides additional
information about the motor movement and provide vital information about the developing
hemiparesis in the leg or arm in one side of the body that is either left or right.
7.
a. Space-occupying lesions: occurs in brain because of malignancy or other abnormal
pathological condition including haematoma or abscess. Majority of the intracerebral tumours
are primary and the remaining mainly originates outside the CNS. Examples: brain tumours
(primary of metastatic)
b. Oedema: characterised by excess accumulation of watery fluid in the cavities or tissues of
the body. Examples for oedema include cerebral oedema (extracellular fluid accumulation in
brain)
8. Pupillary reactivity is an early indicator which indicates increase of intracranial pressure
and is common among patients having severe traumatic brain injury There exist an inversely
proportional relationship between the intracranial pressure and papillary reactivity. Increase
intracranial pressure signifies decreased papillary activity.
9. ‘Cushing’s triad’ should not be confused with Cushing reflex. ‘Cushing’s triad’ is a sign
of increased intracranial pressure. The Triad mainly consists of hypertension (progressive
5PARAMEDICS
increase in the systolic pressure), bradycardia and widening pulse pressure (progressive
increase in the differential relation between the systolic and diastolic pressure).
10. Vital signs of neurological assessment includes
Level of consciousness
Blood pressure
Heart rate
11. Assessment of pupil response and size in relation to light is not directly a part of the
Glasgow Coma Scale but is regarded as vital addition to the GCS assessment. Assessment of
pupil is done in both conscious and unconscious patients. The main process of assessment
involves
Looking at the size of both the pupils
Observation of shape of both the pupils
Observation of whether both the pupils react to light in equal manner
12. A low Glasgow Coma Scale score does not always accurately led to the determination of
severe traumatic brain injury. Proper examination of the verbal score is also important to
detect the presence of severe traumatic brain injury.
increase in the systolic pressure), bradycardia and widening pulse pressure (progressive
increase in the differential relation between the systolic and diastolic pressure).
10. Vital signs of neurological assessment includes
Level of consciousness
Blood pressure
Heart rate
11. Assessment of pupil response and size in relation to light is not directly a part of the
Glasgow Coma Scale but is regarded as vital addition to the GCS assessment. Assessment of
pupil is done in both conscious and unconscious patients. The main process of assessment
involves
Looking at the size of both the pupils
Observation of shape of both the pupils
Observation of whether both the pupils react to light in equal manner
12. A low Glasgow Coma Scale score does not always accurately led to the determination of
severe traumatic brain injury. Proper examination of the verbal score is also important to
detect the presence of severe traumatic brain injury.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PARAMEDICS
CP2 8.7 - CASE STUDY
1. The first reaction on seeing the patient in this condition will be to try to comfort him
possibly by laying him down. The next step will be trying to identify his signs and
symptoms in order to make out the cause of his distress. There is a chance trying to
get to know of his problems by asking him when such symptoms started occurring.
Next step will be to call 911 or a local emergency contact number of the patient if
such is available. In case aspirin is available, the patient can be made to chew and
swallow an aspirin. If the patient is able to inform that there was a history of heart
attack earlier, and if the doctor had prescribed nitro-glycerine for the patient, make the
patient take it as directed by the doctor (Pasqualucci et al., 2015).
2. Looking at the visible symptoms of the patient the most probable guess would be a
heart attack as the patient tends to clutch his chest and looks pale, sweaty and anxious
and breathing at a fast rate. An additional information is that the patient is a quite
aged, which increases the chances of heart attack. The symptoms of heart attack
generally involves:
Uncomfortable pressure, fullness or squeezing pain in the centre of the chest
Spreading of discomfort or pain beyond the chest to the shoulders, back, neck, jaw,
teeth, or one or both arms, or occasionally upper abdomen
Shortness of breath
Light-headedness, dizziness, fainting
Sweating
Nausea (Patra, & Mishra, 2017).
CP2 8.7 - CASE STUDY
1. The first reaction on seeing the patient in this condition will be to try to comfort him
possibly by laying him down. The next step will be trying to identify his signs and
symptoms in order to make out the cause of his distress. There is a chance trying to
get to know of his problems by asking him when such symptoms started occurring.
Next step will be to call 911 or a local emergency contact number of the patient if
such is available. In case aspirin is available, the patient can be made to chew and
swallow an aspirin. If the patient is able to inform that there was a history of heart
attack earlier, and if the doctor had prescribed nitro-glycerine for the patient, make the
patient take it as directed by the doctor (Pasqualucci et al., 2015).
2. Looking at the visible symptoms of the patient the most probable guess would be a
heart attack as the patient tends to clutch his chest and looks pale, sweaty and anxious
and breathing at a fast rate. An additional information is that the patient is a quite
aged, which increases the chances of heart attack. The symptoms of heart attack
generally involves:
Uncomfortable pressure, fullness or squeezing pain in the centre of the chest
Spreading of discomfort or pain beyond the chest to the shoulders, back, neck, jaw,
teeth, or one or both arms, or occasionally upper abdomen
Shortness of breath
Light-headedness, dizziness, fainting
Sweating
Nausea (Patra, & Mishra, 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PARAMEDICS
3. In such situations of chest pain occurring in a patient, performance of an accurate
assessment is an important requirement. Although there are various methods of
assessing the chest pain, one of the most popular methods is ‘PQRST’ pain
assessment which involves the following: P for Position/Provoking Factors, Q for
Quality, R for Radiation, S for Severity/Symptoms and T for Time. The questions
involved for Position/Provoking Factors includes “when the pain started what were
your actions? How did it take place? Is there anything that makes it better or worse?
Does any stimuli trigger it like Stress or a certain Position or maybe certain
activities?” For Quality/Quantity, the questions are “How does it feel? Words can be
used to describe the pain such as sharp, dull, stabbing, burning, crushing, throbbing,
nauseating, shooting, twisting or stretching”, for Region/Radiation it is “Where does
the pain seen to be located? Does the pain seem to be radiating? If so, where? Does
the pain feel to be travelling or moving? was the pain focused when it started?”, for
Severity Scale, “
4. Mention the severity of the pain on a scale of 0 to 10 where zero is no pain and 10 is
the worst pain ever? Does the pain interfere with the daily activities? How bad is it at
its worst? Does the pain force you to sit down or slow down? For how much time
does the episode last?” and for Timing the questions are “When did the pain start?for
how long did it last ? How often does the pain does it occur? Is the pain sudden or
gradual? When the pain was fists experienced, what were you doing? When do you
usually experience it? Are you ever awakened by the severity of the pain? Does the
pain lead to any other symptom? When does the pain occur the most? Is it during or
after meals? Is the occurence seasonally?” (Ioannidis & Khoury, 2014).
3. In such situations of chest pain occurring in a patient, performance of an accurate
assessment is an important requirement. Although there are various methods of
assessing the chest pain, one of the most popular methods is ‘PQRST’ pain
assessment which involves the following: P for Position/Provoking Factors, Q for
Quality, R for Radiation, S for Severity/Symptoms and T for Time. The questions
involved for Position/Provoking Factors includes “when the pain started what were
your actions? How did it take place? Is there anything that makes it better or worse?
Does any stimuli trigger it like Stress or a certain Position or maybe certain
activities?” For Quality/Quantity, the questions are “How does it feel? Words can be
used to describe the pain such as sharp, dull, stabbing, burning, crushing, throbbing,
nauseating, shooting, twisting or stretching”, for Region/Radiation it is “Where does
the pain seen to be located? Does the pain seem to be radiating? If so, where? Does
the pain feel to be travelling or moving? was the pain focused when it started?”, for
Severity Scale, “
4. Mention the severity of the pain on a scale of 0 to 10 where zero is no pain and 10 is
the worst pain ever? Does the pain interfere with the daily activities? How bad is it at
its worst? Does the pain force you to sit down or slow down? For how much time
does the episode last?” and for Timing the questions are “When did the pain start?for
how long did it last ? How often does the pain does it occur? Is the pain sudden or
gradual? When the pain was fists experienced, what were you doing? When do you
usually experience it? Are you ever awakened by the severity of the pain? Does the
pain lead to any other symptom? When does the pain occur the most? Is it during or
after meals? Is the occurence seasonally?” (Ioannidis & Khoury, 2014).
8PARAMEDICS
5. HR = 120 rapid, and weak – it is more than the normal range as the normal rate of
heart beat is 100 beats per minute.
BP = 180/70 – the blood pressure is also quite high compared to the normal range.
The normal range of blood pressure is 120/70 for an adult.
SaO2 = 93% - This is below the normal range as the normal is between 95 to 100%
RR = 25 with crackles heard on auscultation – This respiratory rate is normal.
6. Some of the basic symptoms of heart attack included an experience of extreme
pressure on the chest and chest pain which includes a squeezing or full sensation.
This is generally followed by pain in one or both arms, jaw, back, stomach, or neck.
Other such symptoms of heart attack include shortness of breath, nausea, vomiting,
light-headedness, and breaking in cold sweat. Although the characteristic symptoms
are chest pain and pressure, it is likely that women suffer more incidents of heart
attack than men that does not occur in the traditional way. Instead, some women with
heart attacks may experience more of the other symptoms, like light-headedness,
nausea, extreme fatigue, fainting, dizziness, or pressure in the upper back (Patra, &
Mishra, 2017).
CP2 8.10 - CASE STUDY QUIZ
1. The AVPU scale which is the acronym for alert, voice, pain and unresponsive, is a
system that is used by health care professional in order to measure and record the
level of the consciousness of the patient. According to this system, the patient is alert
as he is fully awake. The eyes are open spontaneously and he can respond to the
commands, although there may be confusion. The next is voice. Although the patient
can respond to the voice or a verbal stimulus, the patient is not able to speak. Next
there is pain. In this category the patient responds upon application of pain stimulus.
Here the patient is unable to respond to such pain stimulus. The next is
5. HR = 120 rapid, and weak – it is more than the normal range as the normal rate of
heart beat is 100 beats per minute.
BP = 180/70 – the blood pressure is also quite high compared to the normal range.
The normal range of blood pressure is 120/70 for an adult.
SaO2 = 93% - This is below the normal range as the normal is between 95 to 100%
RR = 25 with crackles heard on auscultation – This respiratory rate is normal.
6. Some of the basic symptoms of heart attack included an experience of extreme
pressure on the chest and chest pain which includes a squeezing or full sensation.
This is generally followed by pain in one or both arms, jaw, back, stomach, or neck.
Other such symptoms of heart attack include shortness of breath, nausea, vomiting,
light-headedness, and breaking in cold sweat. Although the characteristic symptoms
are chest pain and pressure, it is likely that women suffer more incidents of heart
attack than men that does not occur in the traditional way. Instead, some women with
heart attacks may experience more of the other symptoms, like light-headedness,
nausea, extreme fatigue, fainting, dizziness, or pressure in the upper back (Patra, &
Mishra, 2017).
CP2 8.10 - CASE STUDY QUIZ
1. The AVPU scale which is the acronym for alert, voice, pain and unresponsive, is a
system that is used by health care professional in order to measure and record the
level of the consciousness of the patient. According to this system, the patient is alert
as he is fully awake. The eyes are open spontaneously and he can respond to the
commands, although there may be confusion. The next is voice. Although the patient
can respond to the voice or a verbal stimulus, the patient is not able to speak. Next
there is pain. In this category the patient responds upon application of pain stimulus.
Here the patient is unable to respond to such pain stimulus. The next is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PARAMEDICS
unresponsiveness. Here the patient is evidently unresponsiveness as there is no
response to the voice or the pain (Hoffmann et al., 2016).
2. The Glasgow coma scale (GCS), an effective neurological scale which helps in giving
an efficient and objective way for recording of the state of a person when the
individual is conscious. This is required for the initial as well as the assessments that
follow after the initial one. The elements of the GCS includes eye response, motor
response and verbal response. According to this scale the patient described here the
eye response of the patient can be recorded as 4 as the eyes are open spontaneously.
The verbal response is 2, as the patient can only moan in order to respond to a verbal
stimuli. Lastly the motor response is 2, as the patient is able to show some motor
response on the left side but not on the right side (Teasdale et al., 2014)
3. The important questions that can be asked in order to assess such conditions
indicating towards brain injury includes the occurrences and the severity of :
headaches,
‘pressure in head’,
neck pain,
nausea or vomiting,
dizziness,
blurred vision,
balance problems,
sensitivity to light,
sensitivity to noise,
feeling slowed down,
difficulty in concentrating,
difficulty remembering,
unresponsiveness. Here the patient is evidently unresponsiveness as there is no
response to the voice or the pain (Hoffmann et al., 2016).
2. The Glasgow coma scale (GCS), an effective neurological scale which helps in giving
an efficient and objective way for recording of the state of a person when the
individual is conscious. This is required for the initial as well as the assessments that
follow after the initial one. The elements of the GCS includes eye response, motor
response and verbal response. According to this scale the patient described here the
eye response of the patient can be recorded as 4 as the eyes are open spontaneously.
The verbal response is 2, as the patient can only moan in order to respond to a verbal
stimuli. Lastly the motor response is 2, as the patient is able to show some motor
response on the left side but not on the right side (Teasdale et al., 2014)
3. The important questions that can be asked in order to assess such conditions
indicating towards brain injury includes the occurrences and the severity of :
headaches,
‘pressure in head’,
neck pain,
nausea or vomiting,
dizziness,
blurred vision,
balance problems,
sensitivity to light,
sensitivity to noise,
feeling slowed down,
difficulty in concentrating,
difficulty remembering,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PARAMEDICS
fatigue or low energy,
confusion,
drowsiness,
excessive tiredness,
more emotional,
irritability,
sadness
Nervousness or anxiety (Roozenbeek, Maas & Menon, 2013).
4. The vital signs assessment required for such patient includes measuring blood
pressure, heart rate, respiratory rate and blood glucose level (Yue et al., 2013).
5. The probable disorder that the patient seems to be suffering from is stroke. Therefore
treatment should be given according to this (Jauch et al., 2013).
6. According to the clinical practice guidelines of the QAS Clinical Practice Manual , in
case of a stroke the following guidelines must be followed:
IV access considering oxygen, antiemetic, analgesia, IV fluid, and stroke
mimics
Consider acute stroke referral
7.
fatigue or low energy,
confusion,
drowsiness,
excessive tiredness,
more emotional,
irritability,
sadness
Nervousness or anxiety (Roozenbeek, Maas & Menon, 2013).
4. The vital signs assessment required for such patient includes measuring blood
pressure, heart rate, respiratory rate and blood glucose level (Yue et al., 2013).
5. The probable disorder that the patient seems to be suffering from is stroke. Therefore
treatment should be given according to this (Jauch et al., 2013).
6. According to the clinical practice guidelines of the QAS Clinical Practice Manual , in
case of a stroke the following guidelines must be followed:
IV access considering oxygen, antiemetic, analgesia, IV fluid, and stroke
mimics
Consider acute stroke referral
7.
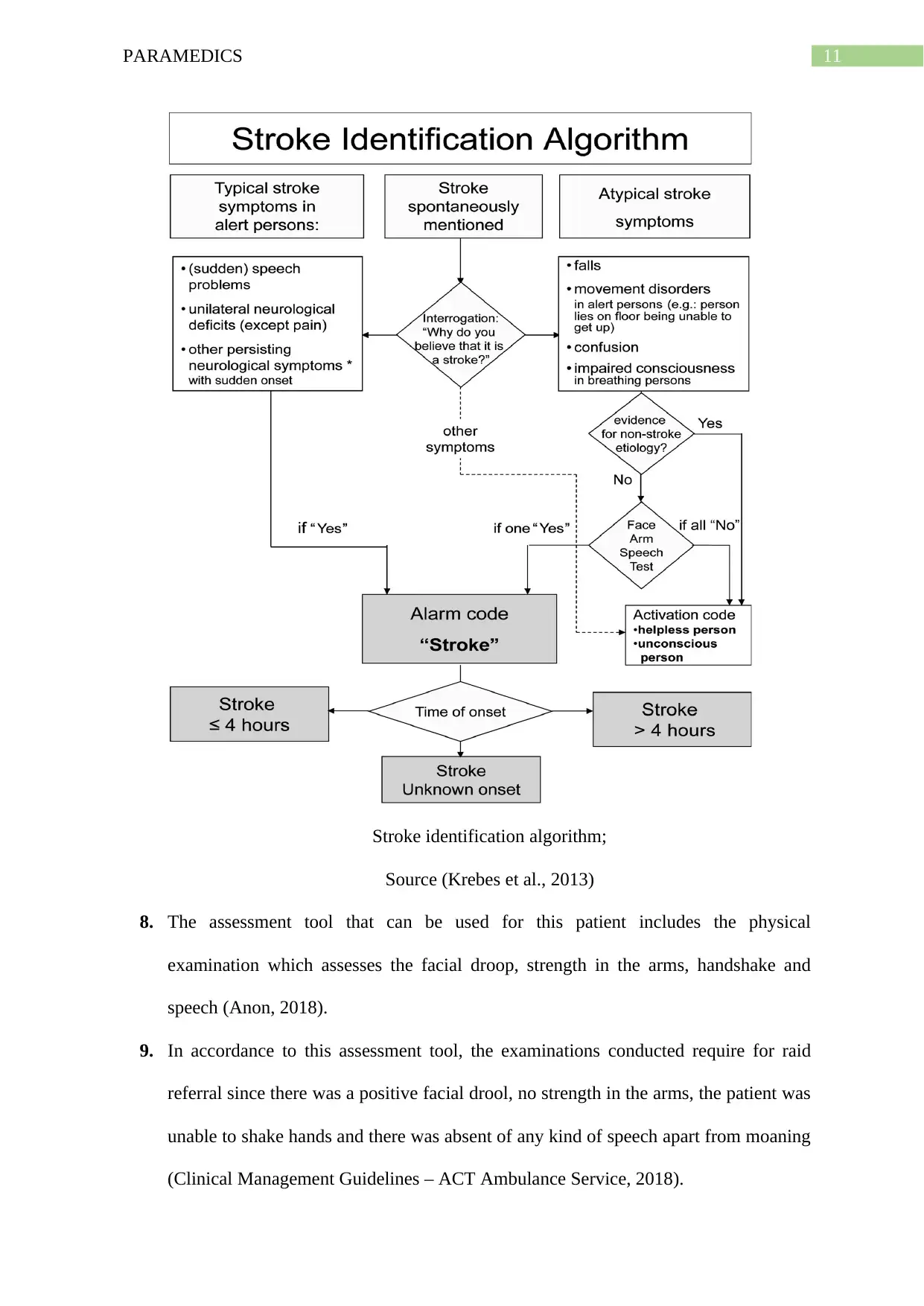
11PARAMEDICS
Stroke identification algorithm;
Source (Krebes et al., 2013)
8. The assessment tool that can be used for this patient includes the physical
examination which assesses the facial droop, strength in the arms, handshake and
speech (Anon, 2018).
9. In accordance to this assessment tool, the examinations conducted require for raid
referral since there was a positive facial drool, no strength in the arms, the patient was
unable to shake hands and there was absent of any kind of speech apart from moaning
(Clinical Management Guidelines – ACT Ambulance Service, 2018).
Stroke identification algorithm;
Source (Krebes et al., 2013)
8. The assessment tool that can be used for this patient includes the physical
examination which assesses the facial droop, strength in the arms, handshake and
speech (Anon, 2018).
9. In accordance to this assessment tool, the examinations conducted require for raid
referral since there was a positive facial drool, no strength in the arms, the patient was
unable to shake hands and there was absent of any kind of speech apart from moaning
(Clinical Management Guidelines – ACT Ambulance Service, 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


