University Report: Pathophysiology and Treatment of Diabetes Type 2
VerifiedAdded on 2022/11/26
|21
|4308
|491
Report
AI Summary
This report delves into the multifaceted aspects of Type 2 Diabetes, encompassing its definition, epidemiology, and the intricate aetiology and pathophysiology, including the roles of obesity, genetics, and lifestyle factors. It explores the clinical signs and symptoms, differential diagnosis, and investigative procedures. The report then examines both orthodox medical treatments, detailing various medications and their mechanisms of action and side effects, and natural medicine approaches, highlighting herbal remedies like cinnamon and fenugreek. Furthermore, it addresses the prognosis and potential complications associated with Type 2 Diabetes, providing a comprehensive overview of this chronic condition. The report is a valuable resource for understanding the disease and its management.

Running head: PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Name of the Student:
Name of the University:
Author Note:
PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Table of Contents
Definition...................................................................................................................................2
Epidemiology.............................................................................................................................2
Aetiology and Pathophysiology.................................................................................................3
Clinical Signs and Symptoms....................................................................................................7
Differential Diagnosis................................................................................................................7
Investigation...............................................................................................................................9
Orthodox Medical Treatment.....................................................................................................9
Natural Medicine......................................................................................................................11
Prognosis and Complications...................................................................................................13
Resource List............................................................................................................................14
References................................................................................................................................17
Table of Contents
Definition...................................................................................................................................2
Epidemiology.............................................................................................................................2
Aetiology and Pathophysiology.................................................................................................3
Clinical Signs and Symptoms....................................................................................................7
Differential Diagnosis................................................................................................................7
Investigation...............................................................................................................................9
Orthodox Medical Treatment.....................................................................................................9
Natural Medicine......................................................................................................................11
Prognosis and Complications...................................................................................................13
Resource List............................................................................................................................14
References................................................................................................................................17
2PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Definition
Diabetes is a complex disorder of carbohydrate, fat, and protein metabolism which is
a result of a deficiency of insulin secretion by the beta cell of the pancreas or resistance to
insulin.This is a chronic condition that affects the way the body metabolises glucose causing
hyperglycaemia (Mosby 2017). Type 2 diabetes (T2D) was previously known as non-insulin
dependent and adult-onset diabetes mellitus and is the most common form-accounting for
about 90% of cases (Mayo Clinic 2019).
Epidemiology
International Diabetes Federation (IDF) has estimated, 451 million people among 18-
99 years of age, are affected with Diabetes in 2017, with a prevalence of 8.4% and speculated
that the rate of prevalence is likely to arise up to 9.9% by 2045 (Cho et al. 2018).
Epidemiological survey among populations of UK, found 90.4% of British population are
affected with type 2 diabetes with a prevalence rate of 4.5% (Holman, Young and Gadsby
2015). Occurrence of type 2 diabetes depends on several factors like obesity, glucose
tolerance, and high carbohydrate meal. Higher prevalence of diabetes type 2 has been found
among African women of sub-Sahara province, due to excess obesity (Mbanya et al. 2014).
Data suggests, an overall prevalence of 5.5% among men and 5.9% among women, regarding
diabetes type 2 (Hilawe et al. 2013). Type 2 diabetes has been found to be strongly related
with parental inheritance.
Furthermore, over the past decade, diabetes prevalence has risen faster in low and
middle-income countries than in high-income countries (WHO 2016).
Definition
Diabetes is a complex disorder of carbohydrate, fat, and protein metabolism which is
a result of a deficiency of insulin secretion by the beta cell of the pancreas or resistance to
insulin.This is a chronic condition that affects the way the body metabolises glucose causing
hyperglycaemia (Mosby 2017). Type 2 diabetes (T2D) was previously known as non-insulin
dependent and adult-onset diabetes mellitus and is the most common form-accounting for
about 90% of cases (Mayo Clinic 2019).
Epidemiology
International Diabetes Federation (IDF) has estimated, 451 million people among 18-
99 years of age, are affected with Diabetes in 2017, with a prevalence of 8.4% and speculated
that the rate of prevalence is likely to arise up to 9.9% by 2045 (Cho et al. 2018).
Epidemiological survey among populations of UK, found 90.4% of British population are
affected with type 2 diabetes with a prevalence rate of 4.5% (Holman, Young and Gadsby
2015). Occurrence of type 2 diabetes depends on several factors like obesity, glucose
tolerance, and high carbohydrate meal. Higher prevalence of diabetes type 2 has been found
among African women of sub-Sahara province, due to excess obesity (Mbanya et al. 2014).
Data suggests, an overall prevalence of 5.5% among men and 5.9% among women, regarding
diabetes type 2 (Hilawe et al. 2013). Type 2 diabetes has been found to be strongly related
with parental inheritance.
Furthermore, over the past decade, diabetes prevalence has risen faster in low and
middle-income countries than in high-income countries (WHO 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Aetiology and Pathophysiology
According to Ross and Wilson (2018), the onset of type 2 diabetes is gradual and it
frequently goes undetected until signs are found on routine investigations or a complication
occurs. The causes are multifactorial and predisposing factors include:
Obesity
Sedentary lifestyle
Increasing age, predominantly affecting middle-aged and older adults
Genetic factors
Gestational diabetes
Obesity is one of the major contributing factors of type 2 diabetes. Adiponectin, a
hormone produced especially by adipocytes, regulates insulin sensitivity. Adiponectin
activates AMPK (AMP-activated protein kinase), which phosphorylates downstream targets,
ultimately stimulating ‘Eat’ response or appetite, glucose uptake, glycolysis and inhibiting
biosynthesis of fatty acids. In patients with obesity and type 2 diabetes, adiponection
mediated AMPK response is altered along with decreased glucose tolerance, causing a rise in
blood glucose level. Hence, type 2 diabetes results in slower removal of glucose from
circulatory blood and cells become insulin-insensitive developing hyperglycemia (Breslavsky
et al. 2013).
Mayo Clinic (2019), the risk of type 2 diabetes increases with age, mostly because
people tend to exercise less, lose muscle mass and gain weight as they age. Physical activity
helps to control an individual's weight, uses up glucose as energy and makes the cells more
sensitive to insulin.
Epigenetic study by Omar (2013) elicited that risk of T2D is approximately 40% in
case one of the parent has type 2 diabetes, and chances increases to 70% if both parents have
Aetiology and Pathophysiology
According to Ross and Wilson (2018), the onset of type 2 diabetes is gradual and it
frequently goes undetected until signs are found on routine investigations or a complication
occurs. The causes are multifactorial and predisposing factors include:
Obesity
Sedentary lifestyle
Increasing age, predominantly affecting middle-aged and older adults
Genetic factors
Gestational diabetes
Obesity is one of the major contributing factors of type 2 diabetes. Adiponectin, a
hormone produced especially by adipocytes, regulates insulin sensitivity. Adiponectin
activates AMPK (AMP-activated protein kinase), which phosphorylates downstream targets,
ultimately stimulating ‘Eat’ response or appetite, glucose uptake, glycolysis and inhibiting
biosynthesis of fatty acids. In patients with obesity and type 2 diabetes, adiponection
mediated AMPK response is altered along with decreased glucose tolerance, causing a rise in
blood glucose level. Hence, type 2 diabetes results in slower removal of glucose from
circulatory blood and cells become insulin-insensitive developing hyperglycemia (Breslavsky
et al. 2013).
Mayo Clinic (2019), the risk of type 2 diabetes increases with age, mostly because
people tend to exercise less, lose muscle mass and gain weight as they age. Physical activity
helps to control an individual's weight, uses up glucose as energy and makes the cells more
sensitive to insulin.
Epigenetic study by Omar (2013) elicited that risk of T2D is approximately 40% in
case one of the parent has type 2 diabetes, and chances increases to 70% if both parents have
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
the same. Study suggests, monozygotic twins have a 60-70% concordant chance of
developing T2D, where both the parents have T2D (Kaprio et al. 1992). Several hereditary
genes like peroxisome proliferator-activated receptor gamma (PPARG), insulin receptor
substrate 1 and 2 (IRS-1, IRS-2), HNF-1A, HNF-1B, TP53 are associated with progression of
type 2 diabetes (Gaulton et al. 2008; Kung, Basu and Murphy 2016).
Anti-diabetic drugs, such as Metformin, which is widely used for T2D treatment, can
exert several side effects in humans. Most significant of them is hypoglycemia or insulin
shock. A lowered blood glucose level and higher intracellular glucose is typically associated
with drug-induced hypoglycemia. Glucose is the principal source of energy for functioning of
brain. Hence, hypoglycemia can affect by lessening energy supply to the neurons, leading to
a variety of health complications like depression, coma, seizure, arythmia or irregular
heartbeat, myocardial ischemia, and even death (Goldstein and Müller-Wieland 2016). A case
study by Al-Abri et al. (2013) has found, metformin overdose causes lactic acidosis including
decreased glucose production and absorption in liver.
Proper diet is another factor corresponding T2D manifestation. People with no
breakfast or poor breakfast are likely to develop type 2 diabetes, in contrast to those who
have proper breakfast daily, due to higher food intake during lunch. These candidates have
higher Body Mass Index (BMI), which could contribute into obesity, thus T2D (Mekary et al.
2013).
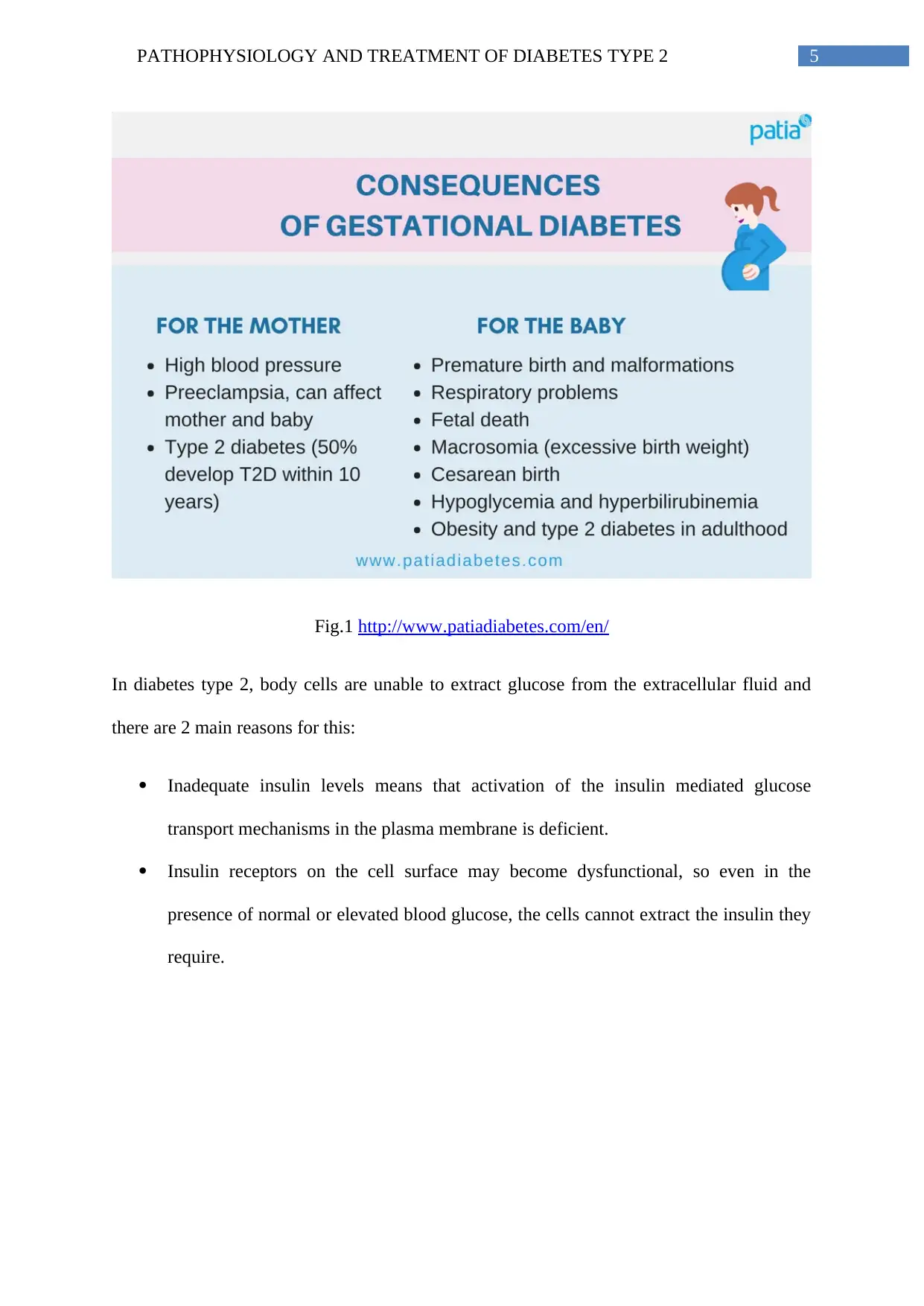
Several studies have demonstrated that women who have had gestational diabetes
have a 20% to 50% increased risk for developing type 2 diabetes later in life.
the same. Study suggests, monozygotic twins have a 60-70% concordant chance of
developing T2D, where both the parents have T2D (Kaprio et al. 1992). Several hereditary
genes like peroxisome proliferator-activated receptor gamma (PPARG), insulin receptor
substrate 1 and 2 (IRS-1, IRS-2), HNF-1A, HNF-1B, TP53 are associated with progression of
type 2 diabetes (Gaulton et al. 2008; Kung, Basu and Murphy 2016).
Anti-diabetic drugs, such as Metformin, which is widely used for T2D treatment, can
exert several side effects in humans. Most significant of them is hypoglycemia or insulin
shock. A lowered blood glucose level and higher intracellular glucose is typically associated
with drug-induced hypoglycemia. Glucose is the principal source of energy for functioning of
brain. Hence, hypoglycemia can affect by lessening energy supply to the neurons, leading to
a variety of health complications like depression, coma, seizure, arythmia or irregular
heartbeat, myocardial ischemia, and even death (Goldstein and Müller-Wieland 2016). A case
study by Al-Abri et al. (2013) has found, metformin overdose causes lactic acidosis including
decreased glucose production and absorption in liver.
Proper diet is another factor corresponding T2D manifestation. People with no
breakfast or poor breakfast are likely to develop type 2 diabetes, in contrast to those who
have proper breakfast daily, due to higher food intake during lunch. These candidates have
higher Body Mass Index (BMI), which could contribute into obesity, thus T2D (Mekary et al.
2013).
Several studies have demonstrated that women who have had gestational diabetes
have a 20% to 50% increased risk for developing type 2 diabetes later in life.
5PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Fig.1 http://www.patiadiabetes.com/en/
In diabetes type 2, body cells are unable to extract glucose from the extracellular fluid and
there are 2 main reasons for this:
Inadequate insulin levels means that activation of the insulin mediated glucose
transport mechanisms in the plasma membrane is deficient.
Insulin receptors on the cell surface may become dysfunctional, so even in the
presence of normal or elevated blood glucose, the cells cannot extract the insulin they
require.
Fig.1 http://www.patiadiabetes.com/en/
In diabetes type 2, body cells are unable to extract glucose from the extracellular fluid and
there are 2 main reasons for this:
Inadequate insulin levels means that activation of the insulin mediated glucose
transport mechanisms in the plasma membrane is deficient.
Insulin receptors on the cell surface may become dysfunctional, so even in the
presence of normal or elevated blood glucose, the cells cannot extract the insulin they
require.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Fig.2: https://www.thermofisher.com/blog/proteomics/type-2-
diabetesmetabolomicsreveals-lipid-dysregulation/
In case of diabetic patients, decreased amount of pancreatic insulin and insulin
insensitivity prevents glucose uptake in cells, and formation of glycogen via glycogen
synthase (inhibition of GSK3 by protein kinase B) is also hampered. Insulin, works as a
signal that promotes cellular localization of glucose transporter GLUT4, which is the
principal transmembrane channel required for glucose intake inside cells. Impairment of
utilizing glucose as energy source, cells deplete protein and fat as an alternative, to
accomplish the energy requirement (Ross and Wilson 2018).
Hyperglycaemia causes long term damage to the blood vessels and nerves and the
eyes, kidneys, nervous system and skin may be affected by the complications of the disease
(Mosby 2017).
Fig.2: https://www.thermofisher.com/blog/proteomics/type-2-
diabetesmetabolomicsreveals-lipid-dysregulation/
In case of diabetic patients, decreased amount of pancreatic insulin and insulin
insensitivity prevents glucose uptake in cells, and formation of glycogen via glycogen
synthase (inhibition of GSK3 by protein kinase B) is also hampered. Insulin, works as a
signal that promotes cellular localization of glucose transporter GLUT4, which is the
principal transmembrane channel required for glucose intake inside cells. Impairment of
utilizing glucose as energy source, cells deplete protein and fat as an alternative, to
accomplish the energy requirement (Ross and Wilson 2018).
Hyperglycaemia causes long term damage to the blood vessels and nerves and the
eyes, kidneys, nervous system and skin may be affected by the complications of the disease
(Mosby 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Clinical Signs and Symptoms
According to Mosby (2017), these are the following signs and symptoms:
Glycosuria
Polyuria
Polydipsia
Polyphagia
Hyperglycaemia
Ketoacidosis (in severe cases)
Poor wound healing
Chronic infection
The concentration of glucose in the glomerular filtrate is the same as in the blood and
it is not all reabsorbed by the tubules. The glucose remaining in the filtrate raises its osmotic
pressure, water reabsorption is reduced and the volume of urine is increased. This results in
electrolytes imbalance, dehydration, and extreme thirst (Ross and Wilson 2018).
Diabetic Ketoacidosis is a medical emergency, indicating severely deranged cell
metabolism secondary to insulin deficiency. This causes harmful substances called ketones to
build up in the body, which can be life-threatening if not treated quickly (NHS 2017).
Differential Diagnosis
Clinical Signs and Symptoms
According to Mosby (2017), these are the following signs and symptoms:
Glycosuria
Polyuria
Polydipsia
Polyphagia
Hyperglycaemia
Ketoacidosis (in severe cases)
Poor wound healing
Chronic infection
The concentration of glucose in the glomerular filtrate is the same as in the blood and
it is not all reabsorbed by the tubules. The glucose remaining in the filtrate raises its osmotic
pressure, water reabsorption is reduced and the volume of urine is increased. This results in
electrolytes imbalance, dehydration, and extreme thirst (Ross and Wilson 2018).
Diabetic Ketoacidosis is a medical emergency, indicating severely deranged cell
metabolism secondary to insulin deficiency. This causes harmful substances called ketones to
build up in the body, which can be life-threatening if not treated quickly (NHS 2017).
Differential Diagnosis
8PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
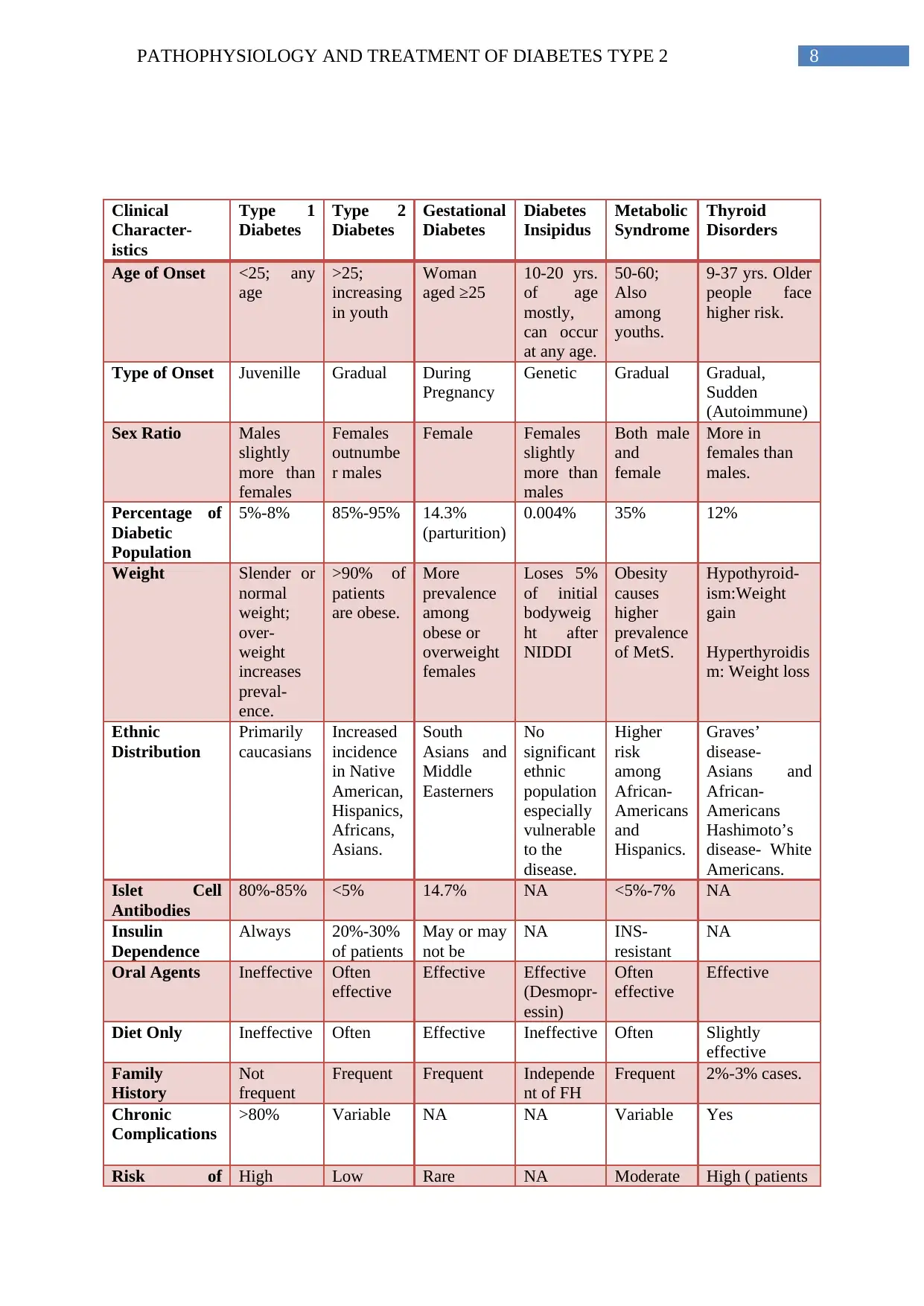
Clinical
Character-
istics
Type 1
Diabetes
Type 2
Diabetes
Gestational
Diabetes
Diabetes
Insipidus
Metabolic
Syndrome
Thyroid
Disorders
Age of Onset <25; any
age
>25;
increasing
in youth
Woman
aged ≥25
10-20 yrs.
of age
mostly,
can occur
at any age.
50-60;
Also
among
youths.
9-37 yrs. Older
people face
higher risk.
Type of Onset Juvenille Gradual During
Pregnancy
Genetic Gradual Gradual,
Sudden
(Autoimmune)
Sex Ratio Males
slightly
more than
females
Females
outnumbe
r males
Female Females
slightly
more than
males
Both male
and
female
More in
females than
males.
Percentage of
Diabetic
Population
5%-8% 85%-95% 14.3%
(parturition)
0.004% 35% 12%
Weight Slender or
normal
weight;
over-
weight
increases
preval-
ence.
>90% of
patients
are obese.
More
prevalence
among
obese or
overweight
females
Loses 5%
of initial
bodyweig
ht after
NIDDI
Obesity
causes
higher
prevalence
of MetS.
Hypothyroid-
ism:Weight
gain
Hyperthyroidis
m: Weight loss
Ethnic
Distribution
Primarily
caucasians
Increased
incidence
in Native
American,
Hispanics,
Africans,
Asians.
South
Asians and
Middle
Easterners
No
significant
ethnic
population
especially
vulnerable
to the
disease.
Higher
risk
among
African-
Americans
and
Hispanics.
Graves’
disease-
Asians and
African-
Americans
Hashimoto’s
disease- White
Americans.
Islet Cell
Antibodies
80%-85% <5% 14.7% NA <5%-7% NA
Insulin
Dependence
Always 20%-30%
of patients
May or may
not be
NA INS-
resistant
NA
Oral Agents Ineffective Often
effective
Effective Effective
(Desmopr-
essin)
Often
effective
Effective
Diet Only Ineffective Often Effective Ineffective Often Slightly
effective
Family
History
Not
frequent
Frequent Frequent Independe
nt of FH
Frequent 2%-3% cases.
Chronic
Complications
>80% Variable NA NA Variable Yes
Risk of High Low Rare NA Moderate High ( patients
Clinical
Character-
istics
Type 1
Diabetes
Type 2
Diabetes
Gestational
Diabetes
Diabetes
Insipidus
Metabolic
Syndrome
Thyroid
Disorders
Age of Onset <25; any
age
>25;
increasing
in youth
Woman
aged ≥25
10-20 yrs.
of age
mostly,
can occur
at any age.
50-60;
Also
among
youths.
9-37 yrs. Older
people face
higher risk.
Type of Onset Juvenille Gradual During
Pregnancy
Genetic Gradual Gradual,
Sudden
(Autoimmune)
Sex Ratio Males
slightly
more than
females
Females
outnumbe
r males
Female Females
slightly
more than
males
Both male
and
female
More in
females than
males.
Percentage of
Diabetic
Population
5%-8% 85%-95% 14.3%
(parturition)
0.004% 35% 12%
Weight Slender or
normal
weight;
over-
weight
increases
preval-
ence.
>90% of
patients
are obese.
More
prevalence
among
obese or
overweight
females
Loses 5%
of initial
bodyweig
ht after
NIDDI
Obesity
causes
higher
prevalence
of MetS.
Hypothyroid-
ism:Weight
gain
Hyperthyroidis
m: Weight loss
Ethnic
Distribution
Primarily
caucasians
Increased
incidence
in Native
American,
Hispanics,
Africans,
Asians.
South
Asians and
Middle
Easterners
No
significant
ethnic
population
especially
vulnerable
to the
disease.
Higher
risk
among
African-
Americans
and
Hispanics.
Graves’
disease-
Asians and
African-
Americans
Hashimoto’s
disease- White
Americans.
Islet Cell
Antibodies
80%-85% <5% 14.7% NA <5%-7% NA
Insulin
Dependence
Always 20%-30%
of patients
May or may
not be
NA INS-
resistant
NA
Oral Agents Ineffective Often
effective
Effective Effective
(Desmopr-
essin)
Often
effective
Effective
Diet Only Ineffective Often Effective Ineffective Often Slightly
effective
Family
History
Not
frequent
Frequent Frequent Independe
nt of FH
Frequent 2%-3% cases.
Chronic
Complications
>80% Variable NA NA Variable Yes
Risk of High Low Rare NA Moderate High ( patients
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Diabetic
Ketoacidosis
having both
Diabetes+TD)
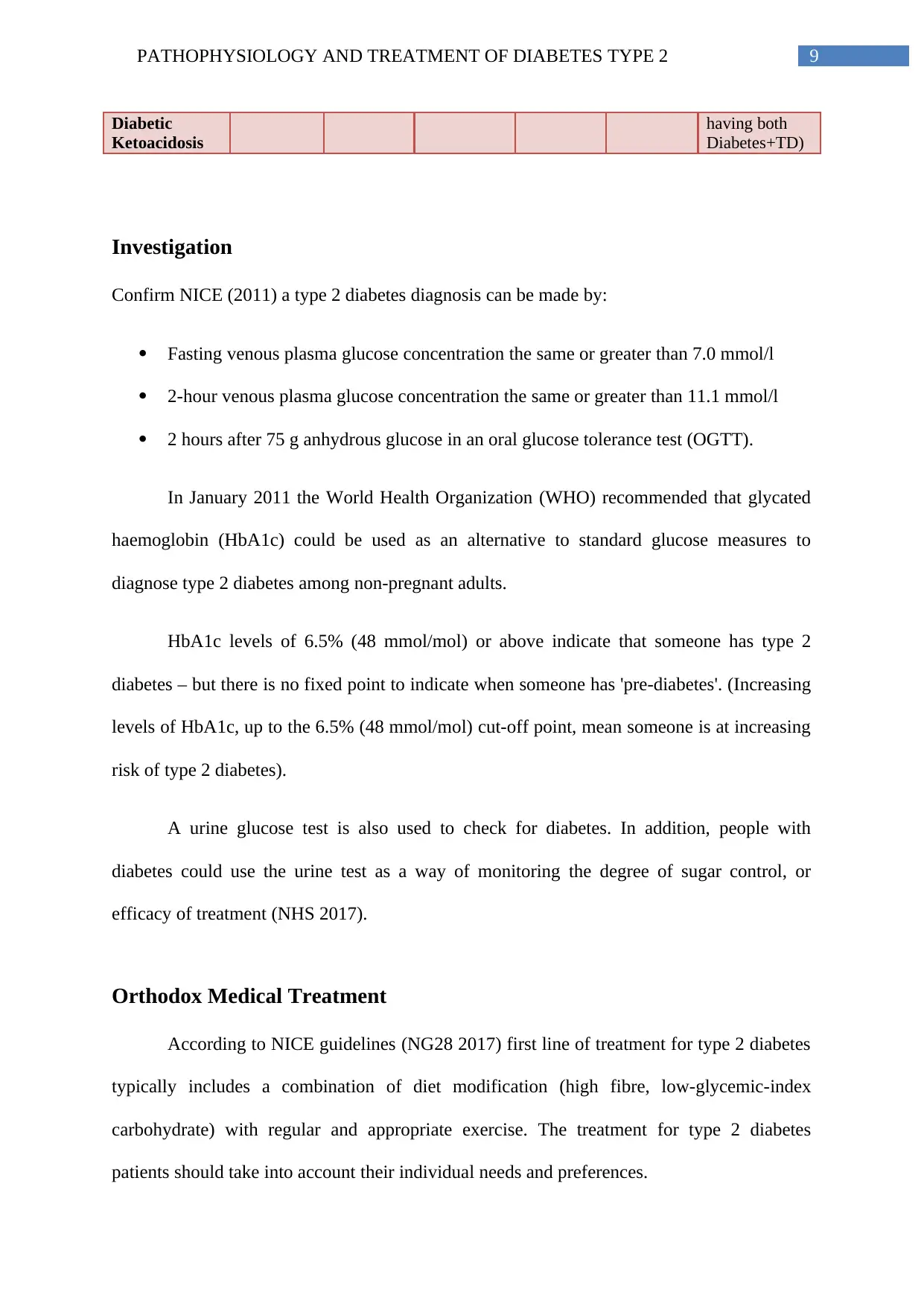
Investigation
Confirm NICE (2011) a type 2 diabetes diagnosis can be made by:
Fasting venous plasma glucose concentration the same or greater than 7.0 mmol/l
2-hour venous plasma glucose concentration the same or greater than 11.1 mmol/l
2 hours after 75 g anhydrous glucose in an oral glucose tolerance test (OGTT).
In January 2011 the World Health Organization (WHO) recommended that glycated
haemoglobin (HbA1c) could be used as an alternative to standard glucose measures to
diagnose type 2 diabetes among non-pregnant adults.
HbA1c levels of 6.5% (48 mmol/mol) or above indicate that someone has type 2
diabetes – but there is no fixed point to indicate when someone has 'pre-diabetes'. (Increasing
levels of HbA1c, up to the 6.5% (48 mmol/mol) cut-off point, mean someone is at increasing
risk of type 2 diabetes).
A urine glucose test is also used to check for diabetes. In addition, people with
diabetes could use the urine test as a way of monitoring the degree of sugar control, or
efficacy of treatment (NHS 2017).
Orthodox Medical Treatment
According to NICE guidelines (NG28 2017) first line of treatment for type 2 diabetes
typically includes a combination of diet modification (high fibre, low-glycemic-index
carbohydrate) with regular and appropriate exercise. The treatment for type 2 diabetes
patients should take into account their individual needs and preferences.
Diabetic
Ketoacidosis
having both
Diabetes+TD)
Investigation
Confirm NICE (2011) a type 2 diabetes diagnosis can be made by:
Fasting venous plasma glucose concentration the same or greater than 7.0 mmol/l
2-hour venous plasma glucose concentration the same or greater than 11.1 mmol/l
2 hours after 75 g anhydrous glucose in an oral glucose tolerance test (OGTT).
In January 2011 the World Health Organization (WHO) recommended that glycated
haemoglobin (HbA1c) could be used as an alternative to standard glucose measures to
diagnose type 2 diabetes among non-pregnant adults.
HbA1c levels of 6.5% (48 mmol/mol) or above indicate that someone has type 2
diabetes – but there is no fixed point to indicate when someone has 'pre-diabetes'. (Increasing
levels of HbA1c, up to the 6.5% (48 mmol/mol) cut-off point, mean someone is at increasing
risk of type 2 diabetes).
A urine glucose test is also used to check for diabetes. In addition, people with
diabetes could use the urine test as a way of monitoring the degree of sugar control, or
efficacy of treatment (NHS 2017).
Orthodox Medical Treatment
According to NICE guidelines (NG28 2017) first line of treatment for type 2 diabetes
typically includes a combination of diet modification (high fibre, low-glycemic-index
carbohydrate) with regular and appropriate exercise. The treatment for type 2 diabetes
patients should take into account their individual needs and preferences.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
Oral anti-hyperglycaemic tablets and/or injectable medication may also be prescribed.
Metformin is one of the most commonly given drugs and helps the body to better respond to
insulin. Dose of metformin should be gradually increased over several weeks to minimise the
risk of gastrointestinal side effects. A review of the dose of metformin is necessary if the
estimated glomerular filtration rate is below 45 ml/minute/1.73m (NICE 2017).
Drug Mode of Action Side Effects
Acarbose Breakdown of complex
carbohydrate and
polysaccharides.
Inflammation
Stomach pain
Constipation
Metformin Controls glycogen synthesis
in liver, intestinal glucose
absorption, glucose uptake in
muscles.
Hypoglycemia
Lactic acidosis
Asthenia
Myalgia
Bromocriptine Agonist of DOPA receptors,
prevents cellular insulin
resistance.
Headache
Nausea
Abdominal cramp
Alogliptin Inhibits DPP-4, increases
insulin production without
developing chances of
hypoglycemia.
Increased heart rate
Nausea
Loss of appetite
Clay stool
Albiglutide B-cell proliferation and
insulin sensitivity by
incretins and regulating
appetite.
Vomiting
Nausea
Diarrhea
Oral anti-hyperglycaemic tablets and/or injectable medication may also be prescribed.
Metformin is one of the most commonly given drugs and helps the body to better respond to
insulin. Dose of metformin should be gradually increased over several weeks to minimise the
risk of gastrointestinal side effects. A review of the dose of metformin is necessary if the
estimated glomerular filtration rate is below 45 ml/minute/1.73m (NICE 2017).
Drug Mode of Action Side Effects
Acarbose Breakdown of complex
carbohydrate and
polysaccharides.
Inflammation
Stomach pain
Constipation
Metformin Controls glycogen synthesis
in liver, intestinal glucose
absorption, glucose uptake in
muscles.
Hypoglycemia
Lactic acidosis
Asthenia
Myalgia
Bromocriptine Agonist of DOPA receptors,
prevents cellular insulin
resistance.
Headache
Nausea
Abdominal cramp
Alogliptin Inhibits DPP-4, increases
insulin production without
developing chances of
hypoglycemia.
Increased heart rate
Nausea
Loss of appetite
Clay stool
Albiglutide B-cell proliferation and
insulin sensitivity by
incretins and regulating
appetite.
Vomiting
Nausea
Diarrhea
11PATHOPHYSIOLOGY AND TREATMENT OF DIABETES TYPE 2
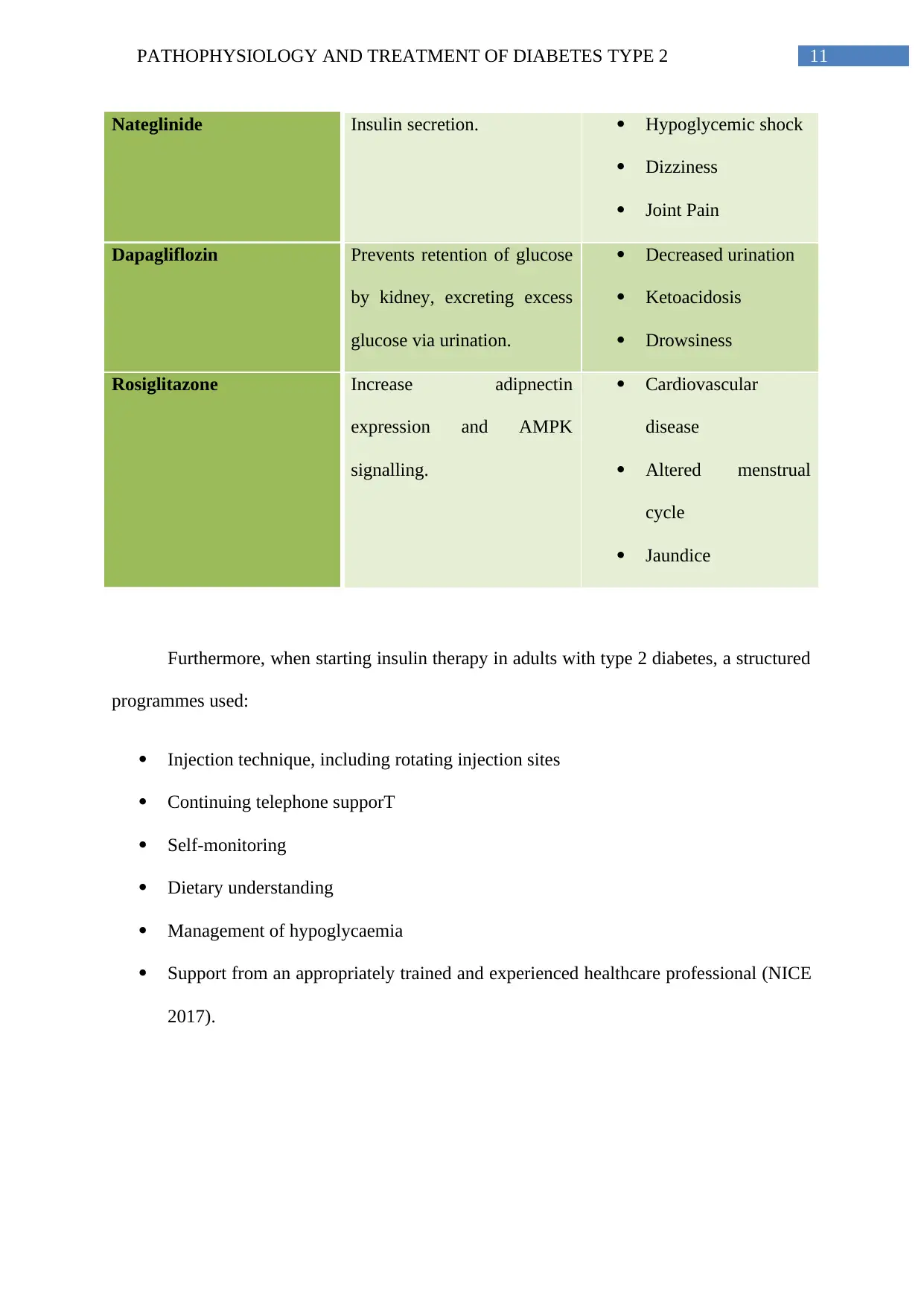
Nateglinide Insulin secretion. Hypoglycemic shock
Dizziness
Joint Pain
Dapagliflozin Prevents retention of glucose
by kidney, excreting excess
glucose via urination.
Decreased urination
Ketoacidosis
Drowsiness
Rosiglitazone Increase adipnectin
expression and AMPK
signalling.
Cardiovascular
disease
Altered menstrual
cycle
Jaundice
Furthermore, when starting insulin therapy in adults with type 2 diabetes, a structured
programmes used:
Injection technique, including rotating injection sites
Continuing telephone supporT
Self-monitoring
Dietary understanding
Management of hypoglycaemia
Support from an appropriately trained and experienced healthcare professional (NICE
2017).
Nateglinide Insulin secretion. Hypoglycemic shock
Dizziness
Joint Pain
Dapagliflozin Prevents retention of glucose
by kidney, excreting excess
glucose via urination.
Decreased urination
Ketoacidosis
Drowsiness
Rosiglitazone Increase adipnectin
expression and AMPK
signalling.
Cardiovascular
disease
Altered menstrual
cycle
Jaundice
Furthermore, when starting insulin therapy in adults with type 2 diabetes, a structured
programmes used:
Injection technique, including rotating injection sites
Continuing telephone supporT
Self-monitoring
Dietary understanding
Management of hypoglycaemia
Support from an appropriately trained and experienced healthcare professional (NICE
2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





