Nursing Patient Assessment: Skin Cancer Risk Factors Report
VerifiedAdded on 2022/10/17
|5
|947
|34
Report
AI Summary
This report focuses on the risk factors associated with skin cancer, providing a detailed analysis for patient assessment within a nursing context. The report identifies key factors such as exposure to ultraviolet (UV) light from sunlight and tanning beds, which is highlighted as the primary risk. It also dis...

Running head: PATIENT ASSESSMENT NURSING 1
Patient Assessment Nursing
Student’s Name
Institutional Affiliation
Patient Assessment Nursing
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Patient Assessment Nursing
Following the patient at hand, I shall explain the risk factors of skin cancer through
detailed description. Skin cancer has plenty of risk factors which call for note taking before
explaining to the patient. The fundamental risk for skin cancer is exposure to ultraviolet (UV)
light (Nahar et al., 2016). This includes tanning beds and sunlight. The risk intensifies with the
duration of exposure to the light. Individuals who live in areas with intensive sunlight and those
who spent most of their time outdoors are at higher risk. Early exposure, for instance, individuals
who had sunburns while still young are at higher risk for developing skin cancer.
Immune suppression is also a vital risk factor. Conditions which weaken the immune
system of the body like diseases, viruses and immune suppression therapy linked to organ
transplant increase the risk of developing skin cancer Garrett et al., 2017). Gender also plays a
significant role. Men are two times more likely to develop skin cancer compared to women.
With respect to the human body, plenty of moles increase the likelihood of developing
skin cancer. Thus individuals with moles are advised to seek dermatologist regularly for
examination (Seebode, Lehmann, & Emmert, 2016). Caucasians are also at a higher risk in
developing skin cancer when compared to non-white. The risk increases for individuals who
possess red or blond hair.
Following genetic make-up, family history plays a significant role. Individuals with one
or more siblings or parents with skin cancer are at higher risk of developing the disease.
Furthermore, presence of inherited conditions (xeroderma pigmentation), which hinder the skin
from preserving itself from UV light, increases the likelihood of developing skin cancer.
Patient Assessment Nursing
Following the patient at hand, I shall explain the risk factors of skin cancer through
detailed description. Skin cancer has plenty of risk factors which call for note taking before
explaining to the patient. The fundamental risk for skin cancer is exposure to ultraviolet (UV)
light (Nahar et al., 2016). This includes tanning beds and sunlight. The risk intensifies with the
duration of exposure to the light. Individuals who live in areas with intensive sunlight and those
who spent most of their time outdoors are at higher risk. Early exposure, for instance, individuals
who had sunburns while still young are at higher risk for developing skin cancer.
Immune suppression is also a vital risk factor. Conditions which weaken the immune
system of the body like diseases, viruses and immune suppression therapy linked to organ
transplant increase the risk of developing skin cancer Garrett et al., 2017). Gender also plays a
significant role. Men are two times more likely to develop skin cancer compared to women.
With respect to the human body, plenty of moles increase the likelihood of developing
skin cancer. Thus individuals with moles are advised to seek dermatologist regularly for
examination (Seebode, Lehmann, & Emmert, 2016). Caucasians are also at a higher risk in
developing skin cancer when compared to non-white. The risk increases for individuals who
possess red or blond hair.
Following genetic make-up, family history plays a significant role. Individuals with one
or more siblings or parents with skin cancer are at higher risk of developing the disease.
Furthermore, presence of inherited conditions (xeroderma pigmentation), which hinder the skin
from preserving itself from UV light, increases the likelihood of developing skin cancer.
3
Lifestyle activities are also potential risk factors. Smokers are likely to develop skin
cancer especially on the lips. Exposure to sunlight, as already mentioned, is a potential risk
factor. Chemical exposure may hinder with biochemical properties of the skin hence increasing
its risk for developing cancer.
The most important prevention measure to use is to impose lifestyle changes. For
instance, it is advisable to reduce time of exposure to UV light (Queen, 2017). As viewed under
the risk factors, it is clear that prolonged exposure to UV light causes the condition. Therefore, it
is vital for an individual to reduce the time of exposure to UV light as a strategic approach in
preventing adverse conditions of skin cancer. Also, it is significant to seek medication regarding
inherited conditions that pose a challenge on the skin. The skin deserves to be maintained healthy
so as to overcome the impact of UV. Therefore, seeking treatment for inherited skin diseases
serve a significant role in preventing the occurrence of skin cancer. Furthermore, it is significant
to maintain the body immune system through proper nutrition and exercise (Gordon, & Rowell,
2015). Proper nutrition provides the body with vitamins which serve a significant role in
maintaining the body immune system. In so doing, the body maintains resistance to conditions
that cause skin cancer. Proper nutrition also helps in providing the skin with appropriate nutrients
that are significant in maintaining its biochemical properties. Lastly, I shall impose restrictions
such as prevention of using UV tanning beds.
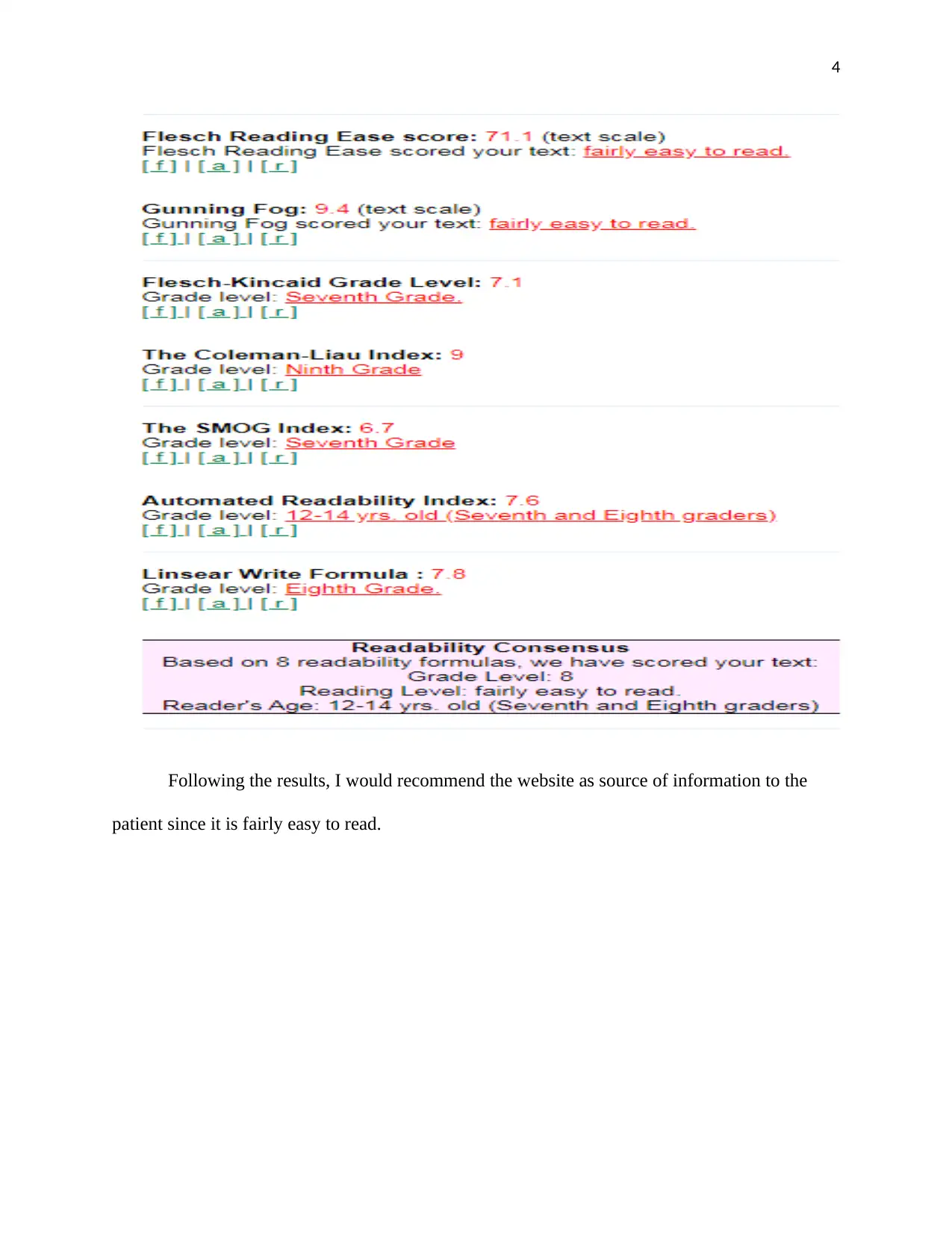
Following an intensive online research, I realized a webpage provided by The Skin
Cancer Foundation (2019) had vital information regarding early detection of skin cancer. The
figure below illustrates the results after running part of the information through the Free Text
Readability Consensus Calculator program.
Lifestyle activities are also potential risk factors. Smokers are likely to develop skin
cancer especially on the lips. Exposure to sunlight, as already mentioned, is a potential risk
factor. Chemical exposure may hinder with biochemical properties of the skin hence increasing
its risk for developing cancer.
The most important prevention measure to use is to impose lifestyle changes. For
instance, it is advisable to reduce time of exposure to UV light (Queen, 2017). As viewed under
the risk factors, it is clear that prolonged exposure to UV light causes the condition. Therefore, it
is vital for an individual to reduce the time of exposure to UV light as a strategic approach in
preventing adverse conditions of skin cancer. Also, it is significant to seek medication regarding
inherited conditions that pose a challenge on the skin. The skin deserves to be maintained healthy
so as to overcome the impact of UV. Therefore, seeking treatment for inherited skin diseases
serve a significant role in preventing the occurrence of skin cancer. Furthermore, it is significant
to maintain the body immune system through proper nutrition and exercise (Gordon, & Rowell,
2015). Proper nutrition provides the body with vitamins which serve a significant role in
maintaining the body immune system. In so doing, the body maintains resistance to conditions
that cause skin cancer. Proper nutrition also helps in providing the skin with appropriate nutrients
that are significant in maintaining its biochemical properties. Lastly, I shall impose restrictions
such as prevention of using UV tanning beds.
Following an intensive online research, I realized a webpage provided by The Skin
Cancer Foundation (2019) had vital information regarding early detection of skin cancer. The
figure below illustrates the results after running part of the information through the Free Text
Readability Consensus Calculator program.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Following the results, I would recommend the website as source of information to the
patient since it is fairly easy to read.
Following the results, I would recommend the website as source of information to the
patient since it is fairly easy to read.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
References
Garrett, G. L., Blanc, P. D., Boscardin, J., Lloyd, A. A., Ahmed, R. L., Anthony, T., ... & Cheng,
J. Y. (2017). Incidence of and risk factors for skin cancer in organ transplant recipients in
the United States. JAMA dermatology, 153(3), 296-303.
Gordon, L. G., & Rowell, D. (2015). Health system costs of skin cancer and cost-effectiveness of
skin cancer prevention and screening: a systematic review. European Journal of Cancer
Prevention, 24(2), 141-149.
Nahar, V. K., Ford, M. A., Brodell, R. T., Boyas, J. F., Jacks, S. K., Biviji-Sharma, R., ... &
Bass, M. A. (2016). Skin cancer prevention practices among malignant melanoma
survivors: a systematic review. Journal of cancer research and clinical oncology, 142(6),
1273-1283.
Queen, L. (2017). Skin Cancer: Causes, Prevention, and Treatment.
Seebode, C., Lehmann, J., & Emmert, S. (2016). Photocarcinogenesis and skin cancer prevention
strategies. Anticancer research, 36(3), 1371-1378.
The Skin Cancer Foundation (2019). Early detection: Overview [online]. Retrieved from:
https://www.skincancer.org/early-detection/
References
Garrett, G. L., Blanc, P. D., Boscardin, J., Lloyd, A. A., Ahmed, R. L., Anthony, T., ... & Cheng,
J. Y. (2017). Incidence of and risk factors for skin cancer in organ transplant recipients in
the United States. JAMA dermatology, 153(3), 296-303.
Gordon, L. G., & Rowell, D. (2015). Health system costs of skin cancer and cost-effectiveness of
skin cancer prevention and screening: a systematic review. European Journal of Cancer
Prevention, 24(2), 141-149.
Nahar, V. K., Ford, M. A., Brodell, R. T., Boyas, J. F., Jacks, S. K., Biviji-Sharma, R., ... &
Bass, M. A. (2016). Skin cancer prevention practices among malignant melanoma
survivors: a systematic review. Journal of cancer research and clinical oncology, 142(6),
1273-1283.
Queen, L. (2017). Skin Cancer: Causes, Prevention, and Treatment.
Seebode, C., Lehmann, J., & Emmert, S. (2016). Photocarcinogenesis and skin cancer prevention
strategies. Anticancer research, 36(3), 1371-1378.
The Skin Cancer Foundation (2019). Early detection: Overview [online]. Retrieved from:
https://www.skincancer.org/early-detection/
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





