Patient Assessment Report: Barry West Case Study Analysis
VerifiedAdded on 2020/05/08
|10
|2013
|59
Report
AI Summary
This report presents a comprehensive assessment of a 64-year-old male patient, Barry West, who suffered a stroke and is currently undergoing treatment for type 2 diabetes and hypertension. The report meticulously separates subjective data, derived from the patient and family's perspectives, from objective data, obtained through medical examinations and tests. It details assessments prepared by a virtual nurse, including respiratory rate, glucose levels, Glasgow Coma Scale (GCS), and blood pressure readings. Furthermore, the report suggests additional objective assessments such as motor function, auditory symptoms, and speech/swallowing evaluations. It also outlines nursing care plans, client goals, and interventions, providing rationales and evaluation methods for improving mobility, preventing deformities, and managing the patient's condition. The report concludes with a summary of the patient's medical history, data analysis, nursing concerns, and care plan components, supported by a list of cited references.
Name of student:
Registration number:
Unit Title:
Unit Code:
Name of supervisor:
Date due:
Registration number:
Unit Title:
Unit Code:
Name of supervisor:
Date due:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Description of the client
The patient going by the name Barry West is a 64 year old male who had his first
stroke in the year 2006. He is currently being treated for type 2diabetes and
hypertension. It all started with West feeling unwell just a few months before he was
admitted to the hospital. He complained of low energy levels, lethargy and hearing
impairment. West was diagnosed and told that he had nerve problems. However, the
lack of energy and the hearing impairment continued and that when he was taken to
hospital. He collapsed at the hospital door. After assessment by a medical officer,
West was found to have GCS of 10/15 and the blood pressure was 185/110mmHg and
other tests also showed abnormal results. West has recently been described as not
being able to move his arms nor speak. He has since been taken to a rehabilitation
center to help take care of his condition.
Separation of subjective from objective data
Subjective data is the information from the patient’s point of view. The subjective
data is used by a medical officer in trying to assess the illness or the medical problem
that a patient may be having and hence help them to diagnose the disease (Bhalla&
Birns, 2015, pg-87-92). Subjective data include the feelings, perceptions, and
concerns of the patient. The subjective data obtained from West and his close family
members include;
Barry West complained of lack of energy, lethargy, and hearing impairment. Mr.
West indicates that he is not capable of moving to move his toes, arms, and legs. The
patient is also not able to talk and he also indicates that his private parts were affected.
The wife indicates that Mr. West was feeling very unwell before he suffered stroke.
Mr. West physician concluded that Mr. West had bad nerves without taking any tests.
Description of the client
The patient going by the name Barry West is a 64 year old male who had his first
stroke in the year 2006. He is currently being treated for type 2diabetes and
hypertension. It all started with West feeling unwell just a few months before he was
admitted to the hospital. He complained of low energy levels, lethargy and hearing
impairment. West was diagnosed and told that he had nerve problems. However, the
lack of energy and the hearing impairment continued and that when he was taken to
hospital. He collapsed at the hospital door. After assessment by a medical officer,
West was found to have GCS of 10/15 and the blood pressure was 185/110mmHg and
other tests also showed abnormal results. West has recently been described as not
being able to move his arms nor speak. He has since been taken to a rehabilitation
center to help take care of his condition.
Separation of subjective from objective data
Subjective data is the information from the patient’s point of view. The subjective
data is used by a medical officer in trying to assess the illness or the medical problem
that a patient may be having and hence help them to diagnose the disease (Bhalla&
Birns, 2015, pg-87-92). Subjective data include the feelings, perceptions, and
concerns of the patient. The subjective data obtained from West and his close family
members include;
Barry West complained of lack of energy, lethargy, and hearing impairment. Mr.
West indicates that he is not capable of moving to move his toes, arms, and legs. The
patient is also not able to talk and he also indicates that his private parts were affected.
The wife indicates that Mr. West was feeling very unwell before he suffered stroke.
Mr. West physician concluded that Mr. West had bad nerves without taking any tests.
3
He also says that Mr. West was very quiet and wanted to stay in the beach and talk
funny little tunes. The statements made by the patient, Mr. West and his wife
comprises the subjective data for this assessment.
The objective data is collected based on evidence through measurement and
conducting of tests, or can be observed through physical examination and laboratory
results. The objective data that was collected in the assessment of Mr. West include;
Glasgow Coma scale (GCS) reading at 10/15 and a blood pressure of 185/110mmHg.
The doctor also measured his respiratory rate and he found it was at 30breaths/min
and O2 saturation of 100% on 2L per minute. The blood glucose levels were
16.5mmol/L at the time of the stroke.
Assessments prepared/prepared by the nurse
The virtual nurse prepared several assessments after the patient arrived at the hospital.
The assessment were meant to enable the nurse understand the health condition of the
patient in order to be able to administer the right medication and save the patient.
The first assessment that the virtual nurse prepared for based on the information from
the assessment is measurement of the respiratory rate of the patient. This is used o
determine breathing inadequacy as a result of respiratory muscles being unable to
work properly. A respiratory rate is below 29 breaths per minute, it means that the
patient is in gross danger (Cooper & Gosnell, 2015, pg-56-57). Mr. West respiratory
rate was found to be 30 breaths per minute.
The other assessment prepared by the nurse is the test of glucose levels. The normal
glucose level in the human body ranges between 3.9 and 5.5mmol/L. This level
however fluctuates from time to time depending on whether a person is on fasting or
He also says that Mr. West was very quiet and wanted to stay in the beach and talk
funny little tunes. The statements made by the patient, Mr. West and his wife
comprises the subjective data for this assessment.
The objective data is collected based on evidence through measurement and
conducting of tests, or can be observed through physical examination and laboratory
results. The objective data that was collected in the assessment of Mr. West include;
Glasgow Coma scale (GCS) reading at 10/15 and a blood pressure of 185/110mmHg.
The doctor also measured his respiratory rate and he found it was at 30breaths/min
and O2 saturation of 100% on 2L per minute. The blood glucose levels were
16.5mmol/L at the time of the stroke.
Assessments prepared/prepared by the nurse
The virtual nurse prepared several assessments after the patient arrived at the hospital.
The assessment were meant to enable the nurse understand the health condition of the
patient in order to be able to administer the right medication and save the patient.
The first assessment that the virtual nurse prepared for based on the information from
the assessment is measurement of the respiratory rate of the patient. This is used o
determine breathing inadequacy as a result of respiratory muscles being unable to
work properly. A respiratory rate is below 29 breaths per minute, it means that the
patient is in gross danger (Cooper & Gosnell, 2015, pg-56-57). Mr. West respiratory
rate was found to be 30 breaths per minute.
The other assessment prepared by the nurse is the test of glucose levels. The normal
glucose level in the human body ranges between 3.9 and 5.5mmol/L. This level
however fluctuates from time to time depending on whether a person is on fasting or
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
has diabetes. Upon carrying out tests, it was found out that Mr. West glucose level
was very high at 16.5mmol/L. The blood sugar needs to be lowered in order to save
the patient on time. Insulin should be administered to the patient as the nurse may
deem appropriate (Cooper & Gosnell, 2015, pg-30-31).
The nurse also prepared for the Glasgow Comma Scale. GCS provides a practical
method of measuring the impairment of consciousness of a person in response to
particular stimuli. The GCS is conducted on the eyes, nerves, and motor. The
recordings of eyes response is recorded as spontaneous, to sound, to pressure and
none. The verbal test is recorded either as oriented, confused, words, sounds or none.
Test on the motor is recorded as obeying commands, localizing, normal flexion,
abnormal flexion, or none. The three elements are combined to determine the level of
responsiveness of a patient (Harris, 2016, pg- 70-74). Mr. West GSC was found to be
10/15. This means that the effect that the stroke has had on the brain is moderate. At
this level, it means that the stroke is serious and emergency medical action need to be
taken. A GCS scale between 8-9/15 is fatal and can easily cause death to the patient.
The blood pressure of the patient was also tested by the nurse. Blood pressure of Mr.
West was found to be 185/110mmHg. This means that the blood pressure is very high
above the normal 145/110mmHg. The patient with such high blood pressure is at the
risk of blood vessels in the heart busting and hence resulting to death of the patient.
Additional objective assessments that could be done
There are several assessment that the virtual nurse could have prepared for the patient
apart from the ones indicated in the report. One of these is the assessment of signs of
motor dysfunction. A bedside neuron assessment of motor functions helps to
determine the extent to which the patient’s brain cells have been damaged by the
has diabetes. Upon carrying out tests, it was found out that Mr. West glucose level
was very high at 16.5mmol/L. The blood sugar needs to be lowered in order to save
the patient on time. Insulin should be administered to the patient as the nurse may
deem appropriate (Cooper & Gosnell, 2015, pg-30-31).
The nurse also prepared for the Glasgow Comma Scale. GCS provides a practical
method of measuring the impairment of consciousness of a person in response to
particular stimuli. The GCS is conducted on the eyes, nerves, and motor. The
recordings of eyes response is recorded as spontaneous, to sound, to pressure and
none. The verbal test is recorded either as oriented, confused, words, sounds or none.
Test on the motor is recorded as obeying commands, localizing, normal flexion,
abnormal flexion, or none. The three elements are combined to determine the level of
responsiveness of a patient (Harris, 2016, pg- 70-74). Mr. West GSC was found to be
10/15. This means that the effect that the stroke has had on the brain is moderate. At
this level, it means that the stroke is serious and emergency medical action need to be
taken. A GCS scale between 8-9/15 is fatal and can easily cause death to the patient.
The blood pressure of the patient was also tested by the nurse. Blood pressure of Mr.
West was found to be 185/110mmHg. This means that the blood pressure is very high
above the normal 145/110mmHg. The patient with such high blood pressure is at the
risk of blood vessels in the heart busting and hence resulting to death of the patient.
Additional objective assessments that could be done
There are several assessment that the virtual nurse could have prepared for the patient
apart from the ones indicated in the report. One of these is the assessment of signs of
motor dysfunction. A bedside neuron assessment of motor functions helps to
determine the extent to which the patient’s brain cells have been damaged by the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
stroke (Wong, 2017, pg-40-45). The assessment will involve examining the ability to
move under command and the ability of the patient to understand what you’re telling
them even thou they are not able to respond by speaking. The nurse can have the
patient flex their hand against the arm of the patient, squeezing their fingers or lifting
the leg while holding the thigh.
The nurse can also conduct an auditory symptoms test. This test is done to test the
responsiveness of the patient to sound (Schweizer & Macdonald, 2014, pg-122). It
can be done by making a loud unexpected clap away from the sight of the patient. The
response is evoked by the auditory brainstem and it may be necessary to fully
examine the responsiveness of the patients` brain.
The other objective assessment that could be conducted by the nurse is the speech and
swallowing assessment. The nurse should have examined the ability of the patient to
speak when something interesting is said to them. If the patient is completely mum, it
means that the attack is severe.
Psychogenic myoclonus can be conducted on the patient. It has variable amplitude
and frequency. This assessment can be done by eliciting of deep reflexes of the
tendon (Doenges, Moorhouse & Murr, 2014, pg-56-59). Laborious research methods
may demonstrate a reaction around 20ms before the movement.
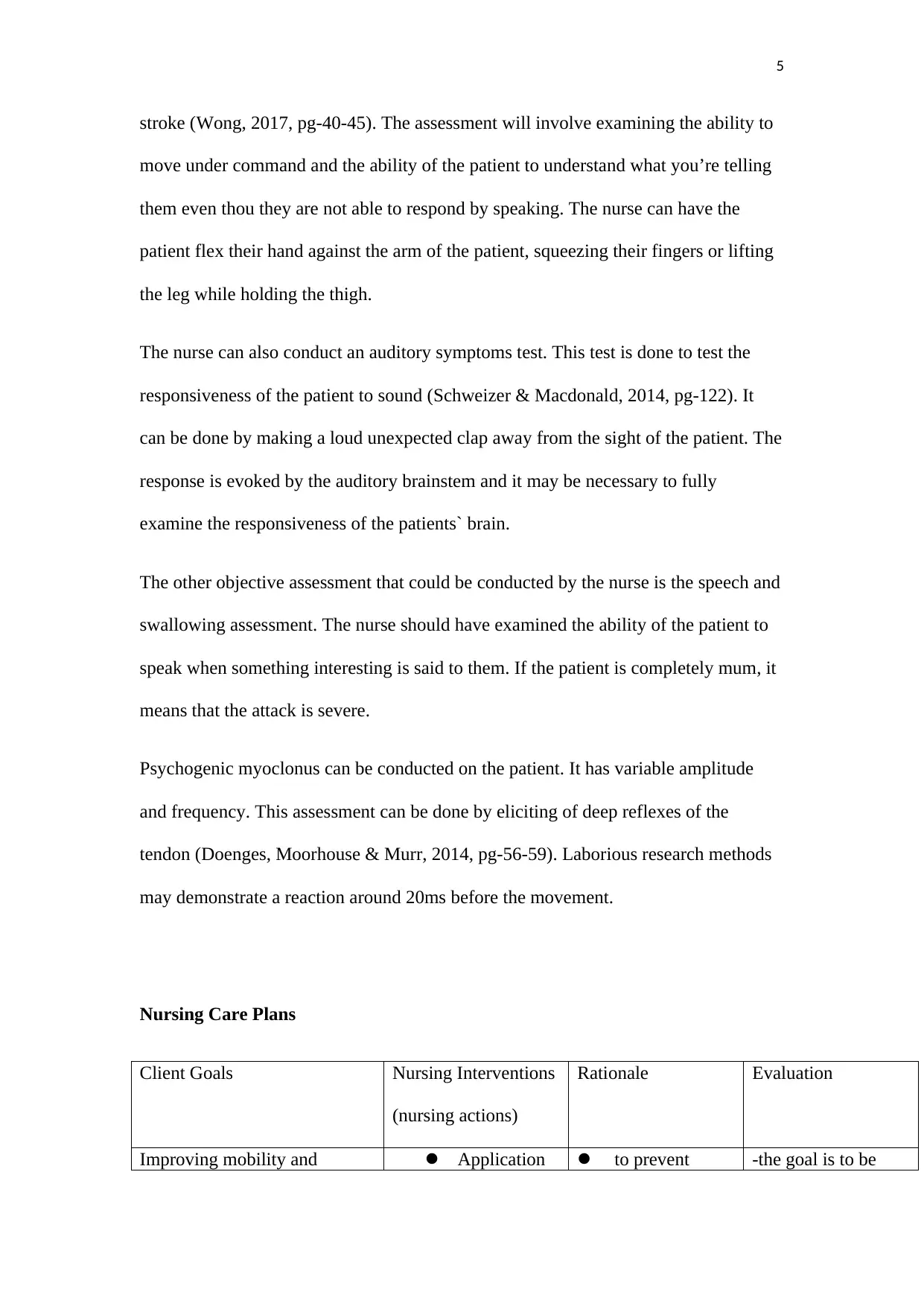
Nursing Care Plans
Client Goals Nursing Interventions
(nursing actions)
Rationale Evaluation
Improving mobility and Application to prevent -the goal is to be
stroke (Wong, 2017, pg-40-45). The assessment will involve examining the ability to
move under command and the ability of the patient to understand what you’re telling
them even thou they are not able to respond by speaking. The nurse can have the
patient flex their hand against the arm of the patient, squeezing their fingers or lifting
the leg while holding the thigh.
The nurse can also conduct an auditory symptoms test. This test is done to test the
responsiveness of the patient to sound (Schweizer & Macdonald, 2014, pg-122). It
can be done by making a loud unexpected clap away from the sight of the patient. The
response is evoked by the auditory brainstem and it may be necessary to fully
examine the responsiveness of the patients` brain.
The other objective assessment that could be conducted by the nurse is the speech and
swallowing assessment. The nurse should have examined the ability of the patient to
speak when something interesting is said to them. If the patient is completely mum, it
means that the attack is severe.
Psychogenic myoclonus can be conducted on the patient. It has variable amplitude
and frequency. This assessment can be done by eliciting of deep reflexes of the
tendon (Doenges, Moorhouse & Murr, 2014, pg-56-59). Laborious research methods
may demonstrate a reaction around 20ms before the movement.
Nursing Care Plans
Client Goals Nursing Interventions
(nursing actions)
Rationale Evaluation
Improving mobility and Application to prevent -the goal is to be
6
prevention of deformities of splint on the patient
Elevating
affected limbs
Changing the
position of the patient
after every 2-3 hours
with the patient being
placed in a prone
position for about 10
minutes a day.
Positioning
the patient to prevent
contractures
flexion to
extremity.
To prevent
edema and
fibrosis
Changing
position helps to
prevent the
patient from
developing bed
sores and
becoming more
immobile (Lee,
2017, pg)
evaluated by
assessing the
progress of the
patient every week.
The ability of the
patient to move their
hands and to
communicate better
through speech will
be an important
means of evaluation.
The blood glucose
level and the blood
pressure need to be
evaluated on a
regular basis.
prevention of deformities of splint on the patient
Elevating
affected limbs
Changing the
position of the patient
after every 2-3 hours
with the patient being
placed in a prone
position for about 10
minutes a day.
Positioning
the patient to prevent
contractures
flexion to
extremity.
To prevent
edema and
fibrosis
Changing
position helps to
prevent the
patient from
developing bed
sores and
becoming more
immobile (Lee,
2017, pg)
evaluated by
assessing the
progress of the
patient every week.
The ability of the
patient to move their
hands and to
communicate better
through speech will
be an important
means of evaluation.
The blood glucose
level and the blood
pressure need to be
evaluated on a
regular basis.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
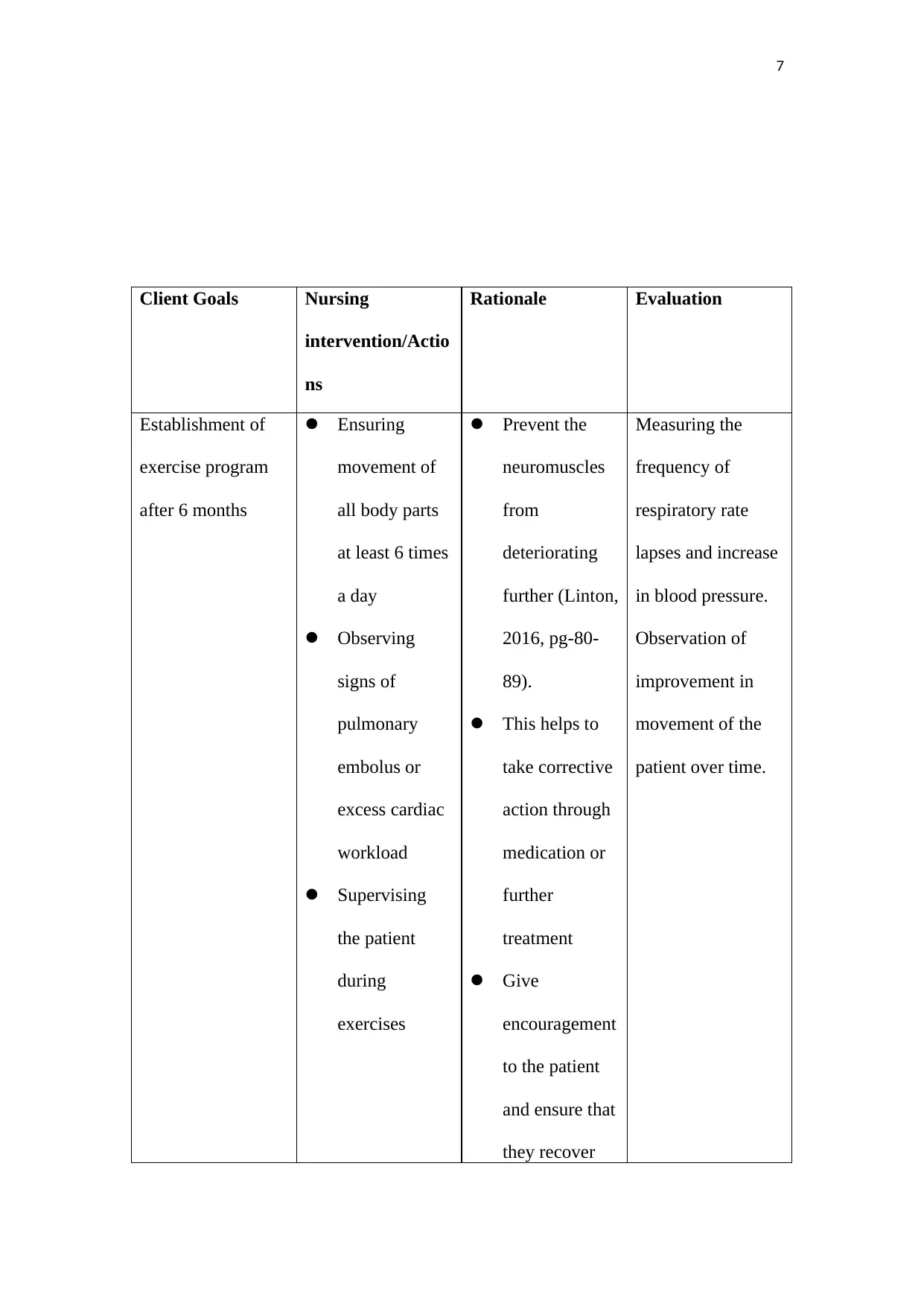
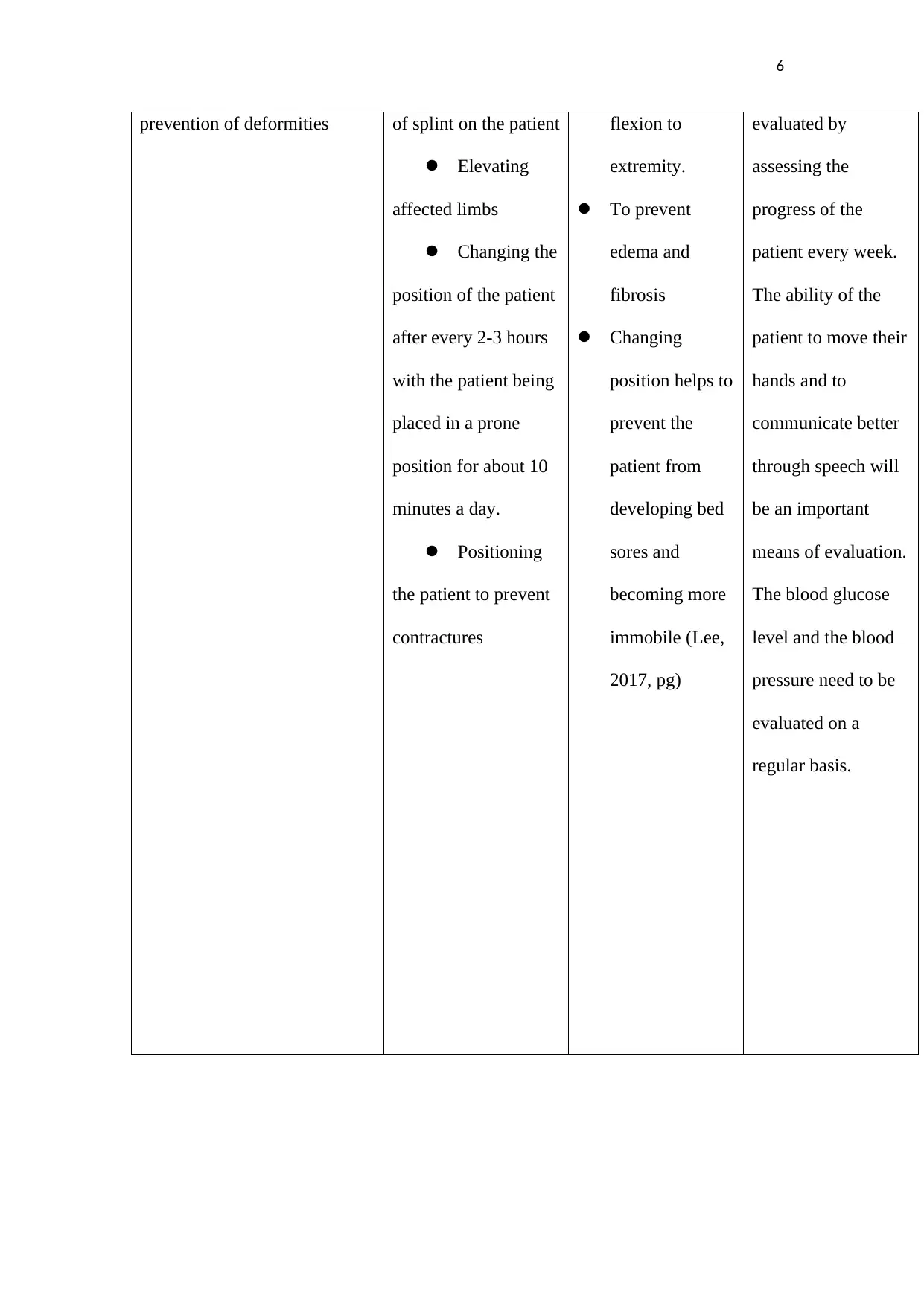
7
Client Goals Nursing
intervention/Actio
ns
Rationale Evaluation
Establishment of
exercise program
after 6 months
Ensuring
movement of
all body parts
at least 6 times
a day
Observing
signs of
pulmonary
embolus or
excess cardiac
workload
Supervising
the patient
during
exercises
Prevent the
neuromuscles
from
deteriorating
further (Linton,
2016, pg-80-
89).
This helps to
take corrective
action through
medication or
further
treatment
Give
encouragement
to the patient
and ensure that
they recover
Measuring the
frequency of
respiratory rate
lapses and increase
in blood pressure.
Observation of
improvement in
movement of the
patient over time.
Client Goals Nursing
intervention/Actio
ns
Rationale Evaluation
Establishment of
exercise program
after 6 months
Ensuring
movement of
all body parts
at least 6 times
a day
Observing
signs of
pulmonary
embolus or
excess cardiac
workload
Supervising
the patient
during
exercises
Prevent the
neuromuscles
from
deteriorating
further (Linton,
2016, pg-80-
89).
This helps to
take corrective
action through
medication or
further
treatment
Give
encouragement
to the patient
and ensure that
they recover
Measuring the
frequency of
respiratory rate
lapses and increase
in blood pressure.
Observation of
improvement in
movement of the
patient over time.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
gradually
(Baird &
Bethel,2011,
pg- 122)
Conclusion
This assessment evaluates the medical condition of the virtual patient who in this case
is Mr. West. The report begins with an introduction of the patient. The medical
history of the patient from the time immediately he suffered first stroke until now.
This is followed separation of objective patient data from the subjective patient data.
The objective data is the data collected from conducting laboratory test and
observation of physical condition of the patient by the medical officer. The subjective
data is based on the narratives of the patient on their feelings and beliefs concerning
the disease which is affecting them. The report also examines the assessments
prepared by the nurse. They include conducting blood sugar test, GCS test and blood
pressure tests. The report also analyzes the nursing concerns and sets goals with a
rationale and a method of evaluation.
gradually
(Baird &
Bethel,2011,
pg- 122)
Conclusion
This assessment evaluates the medical condition of the virtual patient who in this case
is Mr. West. The report begins with an introduction of the patient. The medical
history of the patient from the time immediately he suffered first stroke until now.
This is followed separation of objective patient data from the subjective patient data.
The objective data is the data collected from conducting laboratory test and
observation of physical condition of the patient by the medical officer. The subjective
data is based on the narratives of the patient on their feelings and beliefs concerning
the disease which is affecting them. The report also examines the assessments
prepared by the nurse. They include conducting blood sugar test, GCS test and blood
pressure tests. The report also analyzes the nursing concerns and sets goals with a
rationale and a method of evaluation.
9
References
Baird, M. S., & Bethel, S. (2011). Manual of critical care nursing: Nursing
interventions and collaborative management. St. Louis, Mo: Elsevier
Mosby.
Bhalla, A., & Birns, J. (2015). Management of post-stroke complications.
Cohen, R. A., & Gunstad, J. (2010). Neuropsychology and cardiovascular disease.
Oxford: Oxford University Press.
Cooper, K., & Gosnell, K. (2015). Foundations and adult health nursing.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2014). Nursing care plans:
Guidelines for individualizing client care across the life span.
Philadelphia: F.A. Davis Company.
Edmans, J. (2011). Occupational Therapy and Stroke. New York, NY: John Wiley &
Sons.
Foster, J. G. W., & In Prevost, S. S. (2012). Advanced practice nursing of adults in
acute care.
Harris, C. (2016). Neuromonitoring and assessment: An issue of critical care nursing
clinics of north america. Elsevier.
Lee, S.-H. (2017). Stroke revisited: Diagnosis and treatment of ischemic stroke.
Linton, A. D. (2016). Introduction to medical-surgical nursing.
Schweizer, T. A., & Macdonald, R. L. (2014.). The Behavioral Consequences of
Stroke [recurso electrónico].
References
Baird, M. S., & Bethel, S. (2011). Manual of critical care nursing: Nursing
interventions and collaborative management. St. Louis, Mo: Elsevier
Mosby.
Bhalla, A., & Birns, J. (2015). Management of post-stroke complications.
Cohen, R. A., & Gunstad, J. (2010). Neuropsychology and cardiovascular disease.
Oxford: Oxford University Press.
Cooper, K., & Gosnell, K. (2015). Foundations and adult health nursing.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2014). Nursing care plans:
Guidelines for individualizing client care across the life span.
Philadelphia: F.A. Davis Company.
Edmans, J. (2011). Occupational Therapy and Stroke. New York, NY: John Wiley &
Sons.
Foster, J. G. W., & In Prevost, S. S. (2012). Advanced practice nursing of adults in
acute care.
Harris, C. (2016). Neuromonitoring and assessment: An issue of critical care nursing
clinics of north america. Elsevier.
Lee, S.-H. (2017). Stroke revisited: Diagnosis and treatment of ischemic stroke.
Linton, A. D. (2016). Introduction to medical-surgical nursing.
Schweizer, T. A., & Macdonald, R. L. (2014.). The Behavioral Consequences of
Stroke [recurso electrónico].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

10
Wong, O. I.-C. H. I. (2017). Evidence-Based Bedside Swallowing Assessment by
Nurses For The Patients With Stroke. S.L.: Open Dissertation Press.
Wong, O. I.-C. H. I. (2017). Evidence-Based Bedside Swallowing Assessment by
Nurses For The Patients With Stroke. S.L.: Open Dissertation Press.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





