Patient Quality and Safety Indicators: Analysis of Patient Falls
VerifiedAdded on 2023/06/05
|18
|3956
|442
Report
AI Summary
This report comprehensively examines patient falls as a critical patient quality and safety concern within healthcare settings. It begins by defining patient falls, differentiating between intrinsic and extrinsic factors, and highlighting the importance of understanding risk factors for effective prevention. The report then explores the measurement of patient falls as a patient safety indicator, referencing guidelines from organizations such as the Australian Commission on Safety and Quality in Health Care (ACSQHC) and the Agency for Healthcare Research and Quality (AHRQ). A literature review provides an overview of the prevalence, risk factors, and consequences of patient falls, drawing on studies from various countries and healthcare systems. The report then discusses potential solutions, emphasizing the importance of interdisciplinary approaches and the use of Plan-Do-Study-Act (PDSA) quality cycles to improve patient outcomes. Three small-scale PDSA cycles are presented to address patient falls in a mental health unit, focusing on improved communication, staff training, and environmental modifications. The report concludes by highlighting the importance of systematic, data-driven strategies in minimizing patient falls and enhancing overall patient quality and safety.

Running Head: PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 1
Patient Quality and Safety Indicators: Patient Falls
Name
Institution
Date
Patient Quality and Safety Indicators: Patient Falls
Name
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 2
Patient Quality and Safety Indicators: Patient Falls
Introduction
Sammer, et al., (2010) sort to find out what is patient safety culture and indeed contends
that despite the remarkable efforts healthcare stakeholders take to elevate patients’ healthcare
outcomes, there are concerns as to whether these care efforts meet minimum quality and safety
standards for patients. With a team of healthcare experts, McLoughlin, et al., (2006) developed a
comparable patient safety and quality indicator framework to assist nations under the
Organization for Economic Co-operation and Development (OECD) track and monitor the same
in their healthcare systems. McLoughlin, et al., (2006) deduced that patient falls is one of the
most fundamental yet detrimental patient quality and safety concern. Healthcare institutions
ought to make efforts to minimize patient falls since quality care is critical to both patients and
the organizations. Against this backdrop, this paper will comprehensively extrapolate patient
falls as a patient quality and safety concern and how it can be used as an indicator of the same in
a given healthcare setting. Additionally, this paper will endeavor to utilize 3 small-scale PDSA
quality cycles to solve patient falls and injuries and subsequently improve patient quality and
safety outcomes in the mental health unit.
Patient Falls; Definition
Many definitions of falls and associated injuries have been advanced with many scholars
attributing falls to intrinsic and extrinsic factors. Intrinsic factors are associated with a
physiologic origin while extrinsic factors originate from the environment and other hazards
(Rheaume & Fruh, 2015). Comprehensively understanding these risk factors is critical at
facilitating the formulation of preventive strategies to patient falls. Agostini, Baker, Inouye, and
Bogardus (2001) define patient falls in inpatient settings as “Unintentionally coming to rest on
Patient Quality and Safety Indicators: Patient Falls
Introduction
Sammer, et al., (2010) sort to find out what is patient safety culture and indeed contends
that despite the remarkable efforts healthcare stakeholders take to elevate patients’ healthcare
outcomes, there are concerns as to whether these care efforts meet minimum quality and safety
standards for patients. With a team of healthcare experts, McLoughlin, et al., (2006) developed a
comparable patient safety and quality indicator framework to assist nations under the
Organization for Economic Co-operation and Development (OECD) track and monitor the same
in their healthcare systems. McLoughlin, et al., (2006) deduced that patient falls is one of the
most fundamental yet detrimental patient quality and safety concern. Healthcare institutions
ought to make efforts to minimize patient falls since quality care is critical to both patients and
the organizations. Against this backdrop, this paper will comprehensively extrapolate patient
falls as a patient quality and safety concern and how it can be used as an indicator of the same in
a given healthcare setting. Additionally, this paper will endeavor to utilize 3 small-scale PDSA
quality cycles to solve patient falls and injuries and subsequently improve patient quality and
safety outcomes in the mental health unit.
Patient Falls; Definition
Many definitions of falls and associated injuries have been advanced with many scholars
attributing falls to intrinsic and extrinsic factors. Intrinsic factors are associated with a
physiologic origin while extrinsic factors originate from the environment and other hazards
(Rheaume & Fruh, 2015). Comprehensively understanding these risk factors is critical at
facilitating the formulation of preventive strategies to patient falls. Agostini, Baker, Inouye, and
Bogardus (2001) define patient falls in inpatient settings as “Unintentionally coming to rest on
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 3
the ground, floor, or other lower level, but not as a result of syncope or overwhelming external
force.” However, an all-inclusive definition of a ‘fall’ that takes care of both intrinsic and
extrinsic factors is provided by American Nurses Association-National Database for Nursing
Quality Indicators (ANA-NDNQI) that define a ‘fall’ as “An unplanned descent to the floor with
or without injury”[American Nurses Association, 2005].
From this later definition, falls can either result to injuries or not with incident reports
using different terminologies to describe the levels of injuries. The ANA-NDNQI categorize fall-
related injuries as none-no injury, minor-slight injury requiring simple intervention, moderate-
considerably serious requiring splints or sutures, major- significantly serious requiring surgery
casting and other examinations and death-fatal. Having a formidable definition of patient falls
and levels of injury resulting from the fall is instrumental in determining what constitute a fall
and subsequently helping in calculating rates of patient falls (Healey & Darowski 2012).
Patient Falls; Measurement as a Patient Safety Indicator
Australian Commission on Safety and Quality in Health Care (ACSQHC) [2012]
recognize patient falls as one of the primary hospital-acquired complications which therefore
become a formidable quality and safety indicator in the Australian health care system. Patient
falls are a federal priority in improving patient quality and safety and they are measured through
the National Health Performance Framework (NHPF) [ACSQHC, 2012]. The main focus of the
ACSQHC, (2012) falls measurement are falls that result to general bone fractures, neck and
femur fractures, and intracranial hemorrhage. The Agency for Healthcare Research and Quality
(AHRQ) [2018] point out that the most optimal measure of patient falls in inpatient settings is
one that comparisons can be made over time and across different healthcare facility units to
determine whether change is improving.
the ground, floor, or other lower level, but not as a result of syncope or overwhelming external
force.” However, an all-inclusive definition of a ‘fall’ that takes care of both intrinsic and
extrinsic factors is provided by American Nurses Association-National Database for Nursing
Quality Indicators (ANA-NDNQI) that define a ‘fall’ as “An unplanned descent to the floor with
or without injury”[American Nurses Association, 2005].
From this later definition, falls can either result to injuries or not with incident reports
using different terminologies to describe the levels of injuries. The ANA-NDNQI categorize fall-
related injuries as none-no injury, minor-slight injury requiring simple intervention, moderate-
considerably serious requiring splints or sutures, major- significantly serious requiring surgery
casting and other examinations and death-fatal. Having a formidable definition of patient falls
and levels of injury resulting from the fall is instrumental in determining what constitute a fall
and subsequently helping in calculating rates of patient falls (Healey & Darowski 2012).
Patient Falls; Measurement as a Patient Safety Indicator
Australian Commission on Safety and Quality in Health Care (ACSQHC) [2012]
recognize patient falls as one of the primary hospital-acquired complications which therefore
become a formidable quality and safety indicator in the Australian health care system. Patient
falls are a federal priority in improving patient quality and safety and they are measured through
the National Health Performance Framework (NHPF) [ACSQHC, 2012]. The main focus of the
ACSQHC, (2012) falls measurement are falls that result to general bone fractures, neck and
femur fractures, and intracranial hemorrhage. The Agency for Healthcare Research and Quality
(AHRQ) [2018] point out that the most optimal measure of patient falls in inpatient settings is
one that comparisons can be made over time and across different healthcare facility units to
determine whether change is improving.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 4
The agency recommends that patient falls be determined as a rate, specifically, the rate of
falls per 1000 occupied bed days. In the same way, healthcare practitioners can determine the
rate of injurious falls per 1000 occupied bed days. Patients’ falls specific details must be
comprehensively documented and measurement literally emanates after the actual physical
counting of the number of falls as well as number of occupied bed days in a specific timespan
like a month [AHRQ, 2018]. According to the Joint Commission on Accreditation of Healthcare
Organizations (JCAHO) [2015] patient falls are categorized under the sentinel events with the
numerator being the number of falls resulting in injuries and the denominator being all hospital
admissions.
Patient Falls Literature Review
Patient falls are by and large some of the commonest yet preventable adverse facets of
inpatient and acute hospital care. A survey conducted on England’s National Health Service
(NHS) and whose results were notified in the NHS’s National Reporting and Learning System,
indicated that there were 314,314 patient falls in NHS hospitals. This figure accounted for 19%
of all incidents the system was notified of [NHS National Reporting and Learning System,
2015]. In the U.S. health facility system, patients falls incidents have been deduced to be
between 700,000 and 1000, 000 annually with 30-50 % associated with injuries [Agency for
Healthcare Research and Quality, 2013].
The Australian Institute of Health and Welfare, (2014) reported that patient falls in both
the public and the private healthcare facilities were 298,709 while in New South Wales (NSW)
public hospitals alone there were 27,073 patient falls in 2013. In the period between 2015 and
2016, the Australian healthcare system reported 34,000 falls which happened at the rate of 3.2
per 1000 separations. The public sector hospitals reported more falls per 1000 separations which
The agency recommends that patient falls be determined as a rate, specifically, the rate of
falls per 1000 occupied bed days. In the same way, healthcare practitioners can determine the
rate of injurious falls per 1000 occupied bed days. Patients’ falls specific details must be
comprehensively documented and measurement literally emanates after the actual physical
counting of the number of falls as well as number of occupied bed days in a specific timespan
like a month [AHRQ, 2018]. According to the Joint Commission on Accreditation of Healthcare
Organizations (JCAHO) [2015] patient falls are categorized under the sentinel events with the
numerator being the number of falls resulting in injuries and the denominator being all hospital
admissions.
Patient Falls Literature Review
Patient falls are by and large some of the commonest yet preventable adverse facets of
inpatient and acute hospital care. A survey conducted on England’s National Health Service
(NHS) and whose results were notified in the NHS’s National Reporting and Learning System,
indicated that there were 314,314 patient falls in NHS hospitals. This figure accounted for 19%
of all incidents the system was notified of [NHS National Reporting and Learning System,
2015]. In the U.S. health facility system, patients falls incidents have been deduced to be
between 700,000 and 1000, 000 annually with 30-50 % associated with injuries [Agency for
Healthcare Research and Quality, 2013].
The Australian Institute of Health and Welfare, (2014) reported that patient falls in both
the public and the private healthcare facilities were 298,709 while in New South Wales (NSW)
public hospitals alone there were 27,073 patient falls in 2013. In the period between 2015 and
2016, the Australian healthcare system reported 34,000 falls which happened at the rate of 3.2
per 1000 separations. The public sector hospitals reported more falls per 1000 separations which
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 5
happened at the rate of 4.6 per 1000 separations while the private hospitals reported a rate of 1.3
per 1000 separations [Australian Institute of Health and Welfare, 2017].
Healey, et al., (2013) observe that the old age, severity of illness as well as unfamiliar
surroundings in healthcare facilities are the major predisposing risk factors of patient falls and
falls’ consequences. However, elderly and frail patients are not the only ones that are vulnerable
to falls in healthcare settings. Any patient that is perceived to be of considerable health stature is
also prone to a fall particularly due to physiological changes, medications effect, medical
condition, diagnostic testing, and surgical procedures which have the potential of weakening the
patient or leaving them confused. Patients are likely to suffer harms such as soft tissue injuries,
fractures, psychological trauma, head injuries, death, extended hospital stays and cost of
healthcare escalations (Dunne, Gaboury, & Ashe, 2014; Ambutas, Lamb & Quigley 2017).
Coutinho, Bloch, and Coeli (2012) in a study involving older persons above the age of 60
observed a one-year cumulative mortality of 25.2% amongst all older persons with fall
associated fractures. Wong, et al., (2011) estimated that injured patients from falls are likely to
spend an additional 6.3 days in the hospital while Galbraith, et al., (2011); Haines, et al., (2013)
estimated that it can cost up to $14,000 per fall with injury.
JCAHO [2015] through its Sentinel Alert Event publication contend that falls with severe
injury are persistently amongst the top 10 sentinel events which are reported to the commission’s
Sentinel Event database. Since 2009, 465 falls reports with injuries have been reported with
many of these injuries occurring in healthcare settings of which 63% resulting in death and the
rest sustaining injuries. The JCAHO [2015] further indicate that the most contributing factors to
patient falls include communication failures, lack of effective leadership, physical environment
deficiencies, ineffective staff management practices, inadequate assessments and failure to
happened at the rate of 4.6 per 1000 separations while the private hospitals reported a rate of 1.3
per 1000 separations [Australian Institute of Health and Welfare, 2017].
Healey, et al., (2013) observe that the old age, severity of illness as well as unfamiliar
surroundings in healthcare facilities are the major predisposing risk factors of patient falls and
falls’ consequences. However, elderly and frail patients are not the only ones that are vulnerable
to falls in healthcare settings. Any patient that is perceived to be of considerable health stature is
also prone to a fall particularly due to physiological changes, medications effect, medical
condition, diagnostic testing, and surgical procedures which have the potential of weakening the
patient or leaving them confused. Patients are likely to suffer harms such as soft tissue injuries,
fractures, psychological trauma, head injuries, death, extended hospital stays and cost of
healthcare escalations (Dunne, Gaboury, & Ashe, 2014; Ambutas, Lamb & Quigley 2017).
Coutinho, Bloch, and Coeli (2012) in a study involving older persons above the age of 60
observed a one-year cumulative mortality of 25.2% amongst all older persons with fall
associated fractures. Wong, et al., (2011) estimated that injured patients from falls are likely to
spend an additional 6.3 days in the hospital while Galbraith, et al., (2011); Haines, et al., (2013)
estimated that it can cost up to $14,000 per fall with injury.
JCAHO [2015] through its Sentinel Alert Event publication contend that falls with severe
injury are persistently amongst the top 10 sentinel events which are reported to the commission’s
Sentinel Event database. Since 2009, 465 falls reports with injuries have been reported with
many of these injuries occurring in healthcare settings of which 63% resulting in death and the
rest sustaining injuries. The JCAHO [2015] further indicate that the most contributing factors to
patient falls include communication failures, lack of effective leadership, physical environment
deficiencies, ineffective staff management practices, inadequate assessments and failure to
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 6
adhere to protocols and safety practices. To this end, there is a need to come up with patient
quality and safety improvement strategies that can minimize falls and its adverse effects.
Potential Solutions to Patient Falls
JCAHO [2015]; [ACSQHC, 2012] has suggested several actions that healthcare
institutions can utilize to prevent and minimize falls and injuries related to falls. These include
leading efforts to raise falls prevention awareness; establishment of an interdisciplinary falls
injury prevention team; institution of standardized tools to identify falls’ risk factors. Moreover,
the commission deems coming up with patient-specific plans of care such as effective
communication and one-to-one patient education as very instrumental. Furthermore, conducting
effective post-fall management practices such as transparent reporting of falls and falls’ analysis
can inform further improvement. JCAHO [2015] asserts that preventing hospital falls calls for
the commitment of healthcare facility's leaders as well as the formulation of systematic and data-
driven strategies targeting particular health care settings and specific patient populations. The
Plan-Do-Study-Act (PDSA) quality cycles framework is such one systematic and data-driven
approach instrumental in the improvement of patient quality and safety indicators (Varkey, et al.,
2009).
PDSA Small-Scale quality cycles
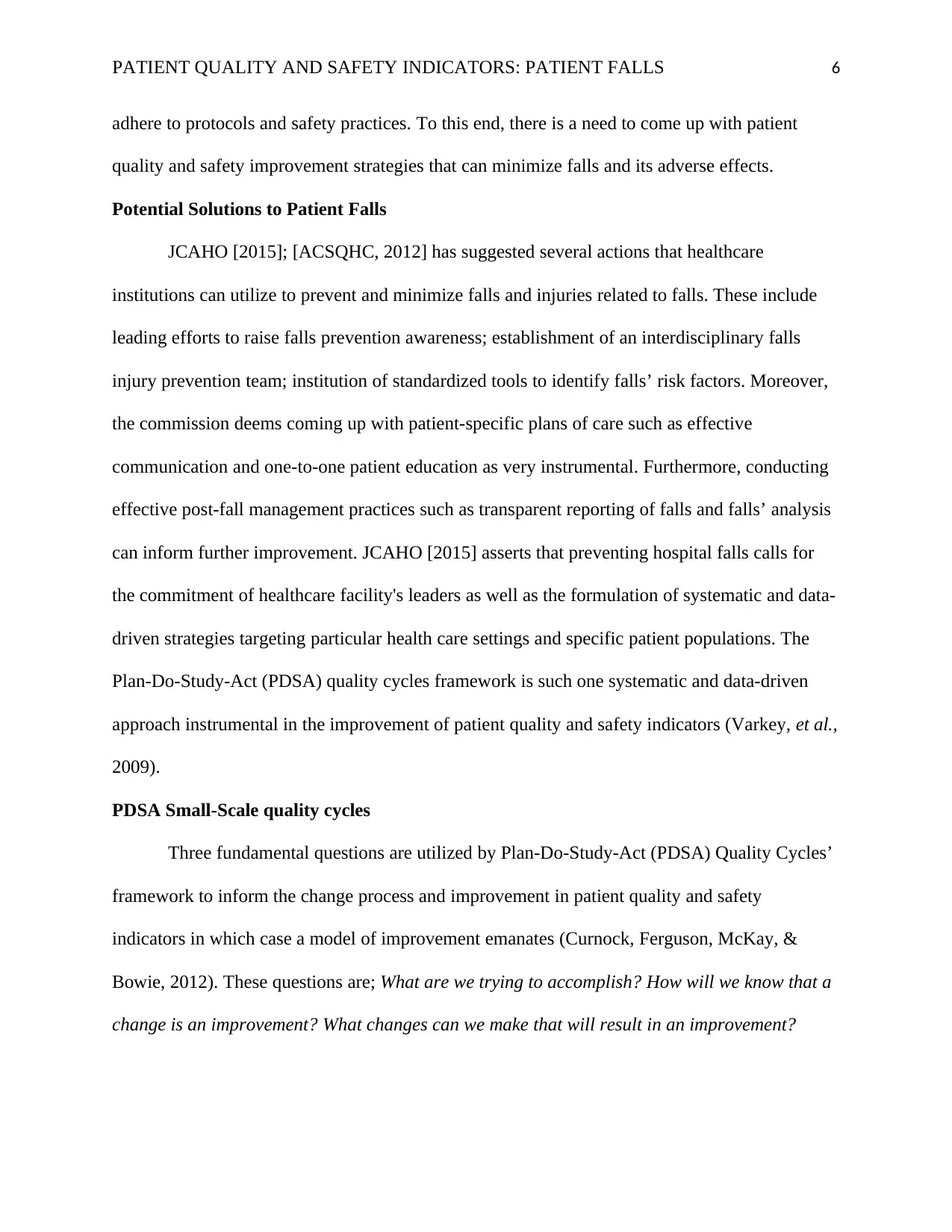
Three fundamental questions are utilized by Plan-Do-Study-Act (PDSA) Quality Cycles’
framework to inform the change process and improvement in patient quality and safety
indicators in which case a model of improvement emanates (Curnock, Ferguson, McKay, &
Bowie, 2012). These questions are; What are we trying to accomplish? How will we know that a
change is an improvement? What changes can we make that will result in an improvement?
adhere to protocols and safety practices. To this end, there is a need to come up with patient
quality and safety improvement strategies that can minimize falls and its adverse effects.
Potential Solutions to Patient Falls
JCAHO [2015]; [ACSQHC, 2012] has suggested several actions that healthcare
institutions can utilize to prevent and minimize falls and injuries related to falls. These include
leading efforts to raise falls prevention awareness; establishment of an interdisciplinary falls
injury prevention team; institution of standardized tools to identify falls’ risk factors. Moreover,
the commission deems coming up with patient-specific plans of care such as effective
communication and one-to-one patient education as very instrumental. Furthermore, conducting
effective post-fall management practices such as transparent reporting of falls and falls’ analysis
can inform further improvement. JCAHO [2015] asserts that preventing hospital falls calls for
the commitment of healthcare facility's leaders as well as the formulation of systematic and data-
driven strategies targeting particular health care settings and specific patient populations. The
Plan-Do-Study-Act (PDSA) quality cycles framework is such one systematic and data-driven
approach instrumental in the improvement of patient quality and safety indicators (Varkey, et al.,
2009).
PDSA Small-Scale quality cycles
Three fundamental questions are utilized by Plan-Do-Study-Act (PDSA) Quality Cycles’
framework to inform the change process and improvement in patient quality and safety
indicators in which case a model of improvement emanates (Curnock, Ferguson, McKay, &
Bowie, 2012). These questions are; What are we trying to accomplish? How will we know that a
change is an improvement? What changes can we make that will result in an improvement?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 7
The Improvement Guide, API, 2009.
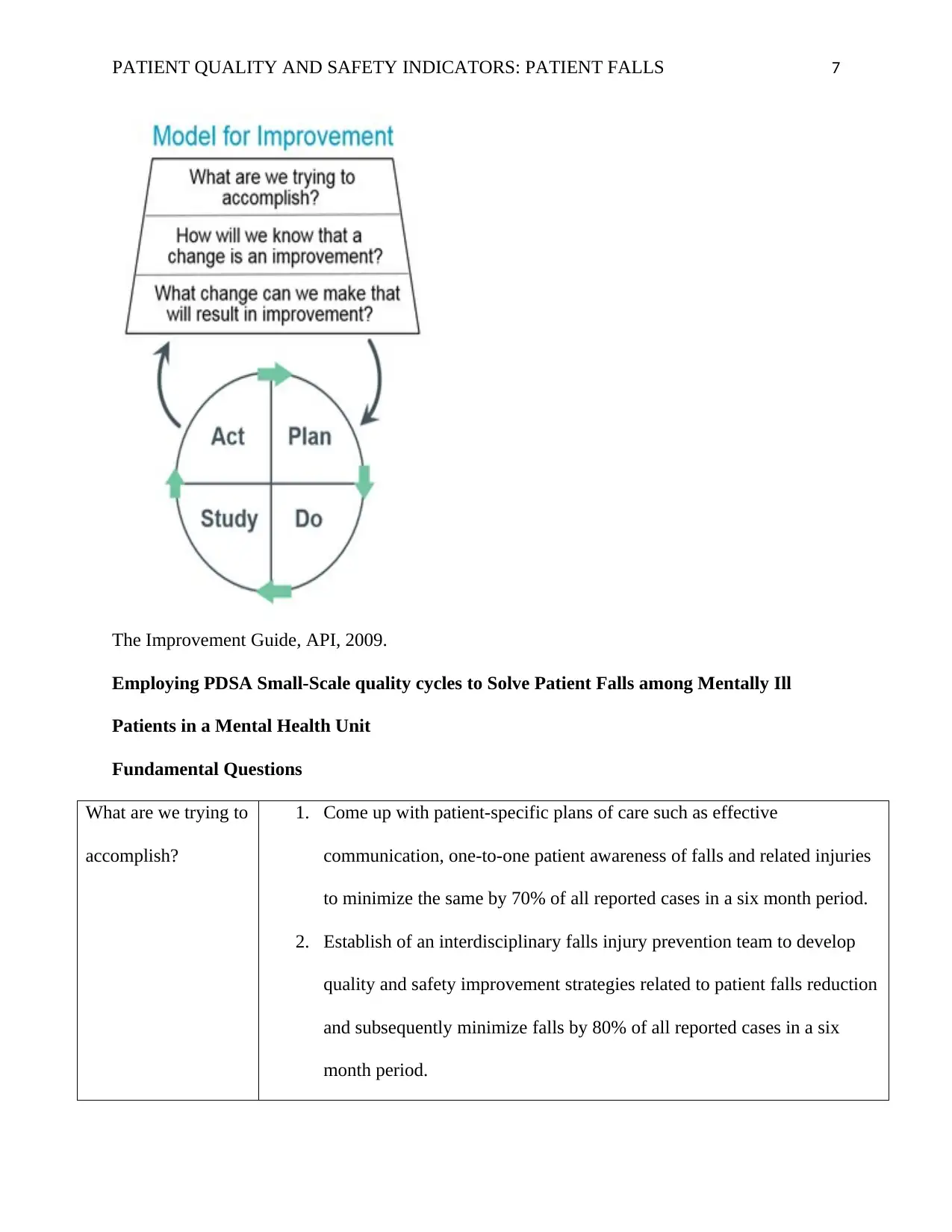
Employing PDSA Small-Scale quality cycles to Solve Patient Falls among Mentally Ill
Patients in a Mental Health Unit
Fundamental Questions
What are we trying to
accomplish?
1. Come up with patient-specific plans of care such as effective
communication, one-to-one patient awareness of falls and related injuries
to minimize the same by 70% of all reported cases in a six month period.
2. Establish of an interdisciplinary falls injury prevention team to develop
quality and safety improvement strategies related to patient falls reduction
and subsequently minimize falls by 80% of all reported cases in a six
month period.
The Improvement Guide, API, 2009.
Employing PDSA Small-Scale quality cycles to Solve Patient Falls among Mentally Ill
Patients in a Mental Health Unit
Fundamental Questions
What are we trying to
accomplish?
1. Come up with patient-specific plans of care such as effective
communication, one-to-one patient awareness of falls and related injuries
to minimize the same by 70% of all reported cases in a six month period.
2. Establish of an interdisciplinary falls injury prevention team to develop
quality and safety improvement strategies related to patient falls reduction
and subsequently minimize falls by 80% of all reported cases in a six
month period.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 8
3. Improve the physical mental health unit environment by removing patient
falls risk factors and subsequently minimize falls by 90% of all reported
cases in a six month period.
How will we know
that a change is an
improvement?
1. Patient falls reduction with patient being more aware falls’ dangers and
falls’ risk factors.
2. Healthcare practitioners demonstrate skilled abilities of handling mentally
ill patients requirements including falls’ cases
3. Mental health patients' abilities to locate falls risk factors in the mental
health unit
What changes can we
make that will result
in an improvement?
1. Streamline communication between healthcare practitioners and institute
passionate one-to-one patient education.
2. Healthcare providers’ training on the how to handle falls among mentally
ill patients.
3. Having low-beds, non-slippery floors and supporting gadgets especially in
washing rooms.
PDSA quality cycles
3. Improve the physical mental health unit environment by removing patient
falls risk factors and subsequently minimize falls by 90% of all reported
cases in a six month period.
How will we know
that a change is an
improvement?
1. Patient falls reduction with patient being more aware falls’ dangers and
falls’ risk factors.
2. Healthcare practitioners demonstrate skilled abilities of handling mentally
ill patients requirements including falls’ cases
3. Mental health patients' abilities to locate falls risk factors in the mental
health unit
What changes can we
make that will result
in an improvement?
1. Streamline communication between healthcare practitioners and institute
passionate one-to-one patient education.
2. Healthcare providers’ training on the how to handle falls among mentally
ill patients.
3. Having low-beds, non-slippery floors and supporting gadgets especially in
washing rooms.
PDSA quality cycles
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 9
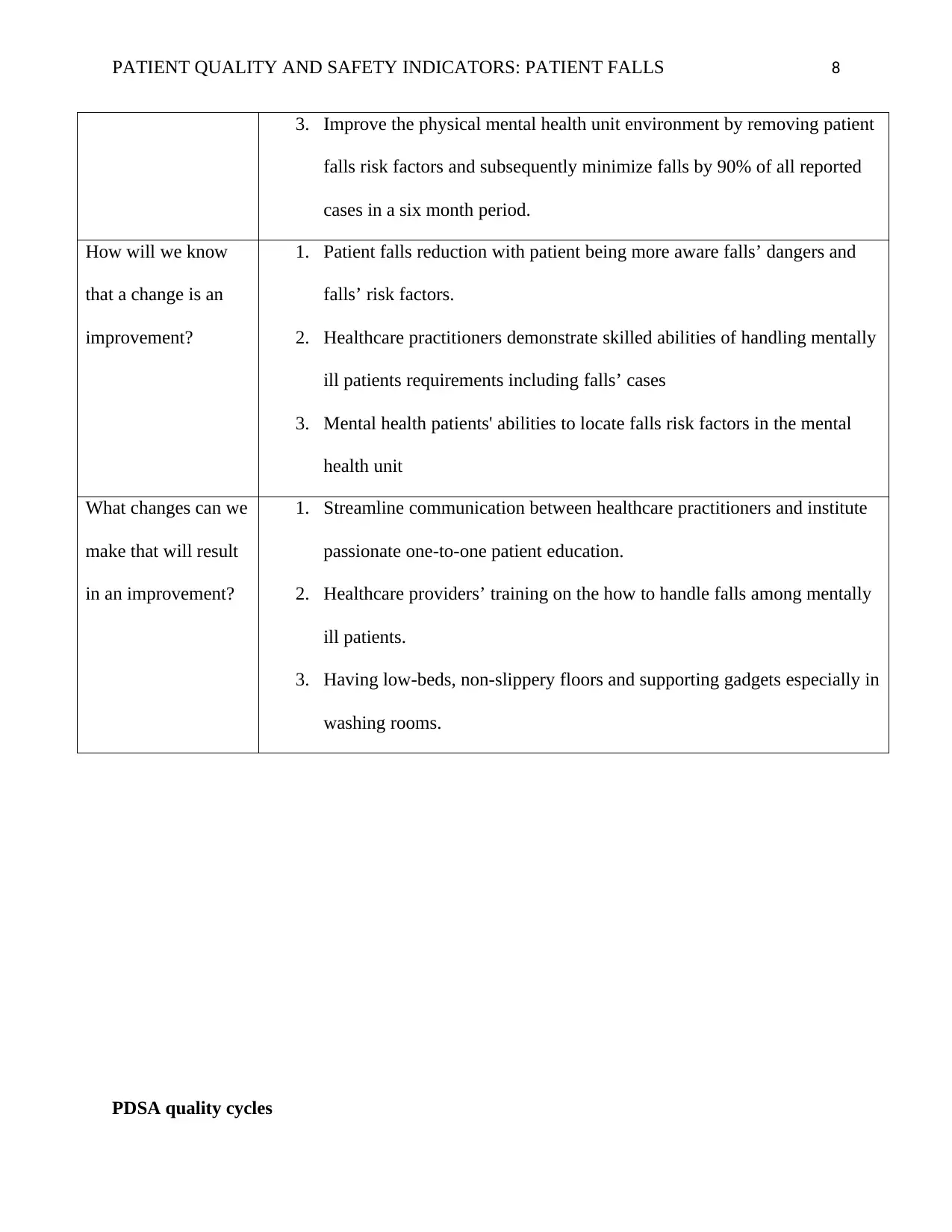
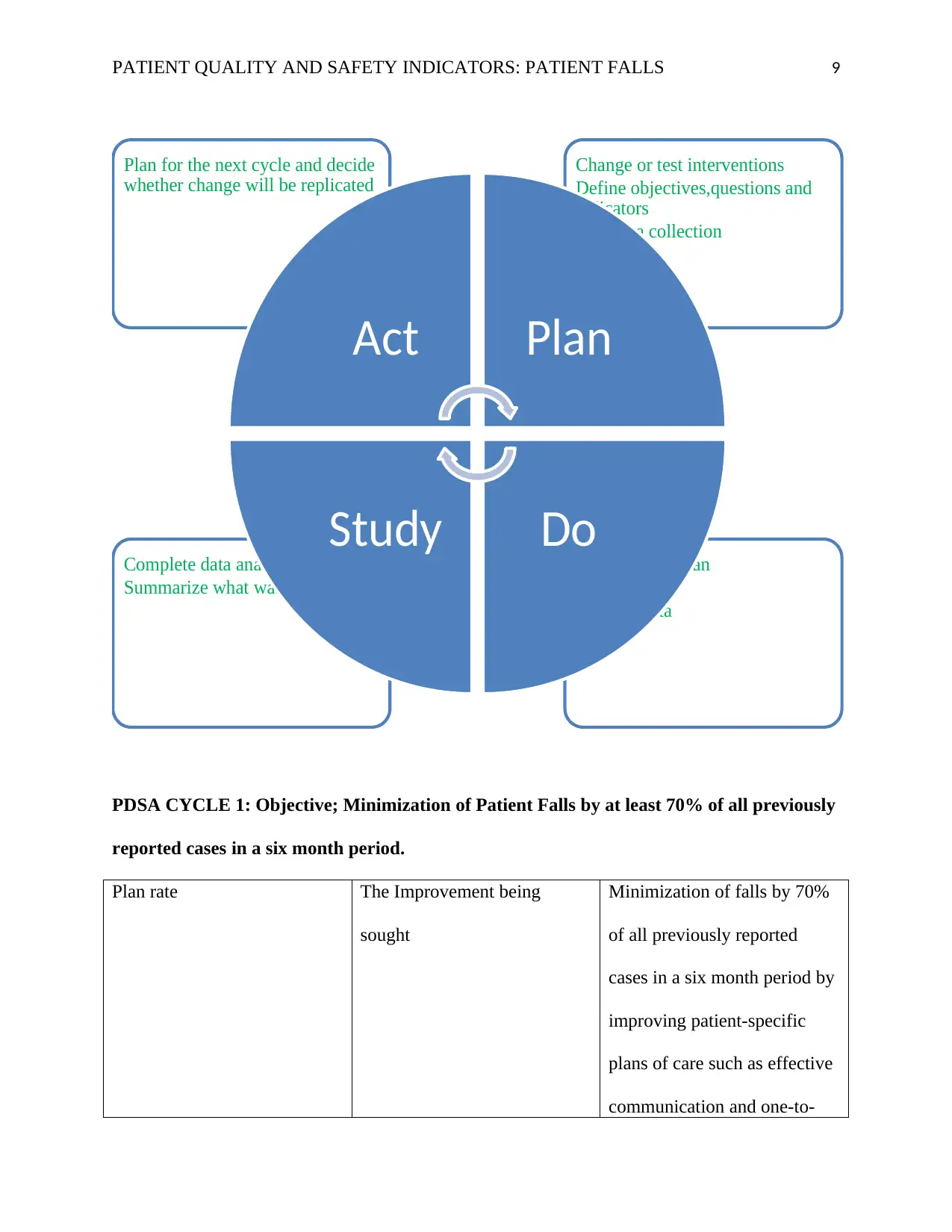
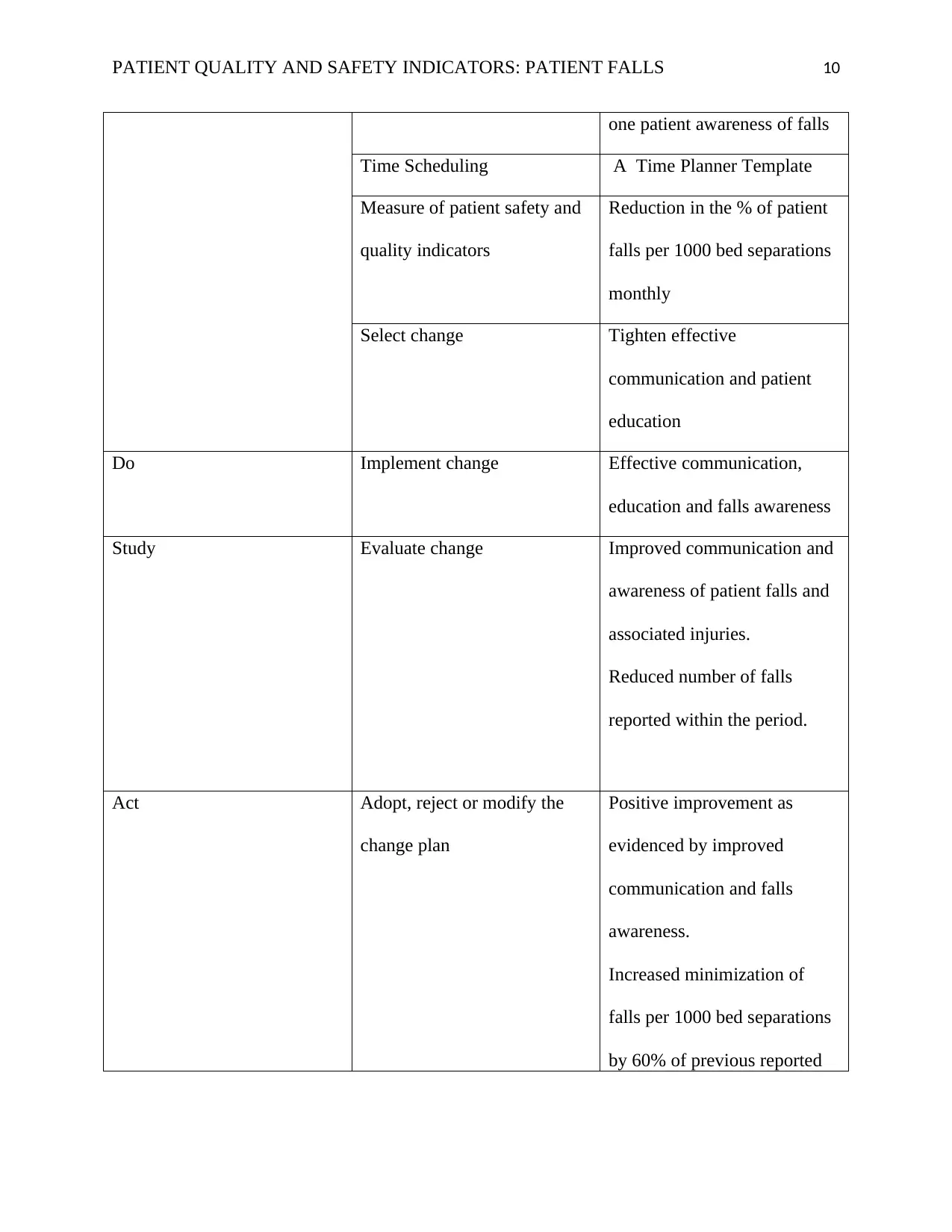
PDSA CYCLE 1: Objective; Minimization of Patient Falls by at least 70% of all previously
reported cases in a six month period.
Plan rate The Improvement being
sought
Minimization of falls by 70%
of all previously reported
cases in a six month period by
improving patient-specific
plans of care such as effective
communication and one-to-
Carry out the plan
Collect data
Analyse data
Complete data analysis
Summarize what was learned
Change or test interventions
Define objectives,questions and
indicators
Plan data collection
Plan for the next cycle and decide
whether change will be replicated
Act Plan
DoStudy
PDSA CYCLE 1: Objective; Minimization of Patient Falls by at least 70% of all previously
reported cases in a six month period.
Plan rate The Improvement being
sought
Minimization of falls by 70%
of all previously reported
cases in a six month period by
improving patient-specific
plans of care such as effective
communication and one-to-
Carry out the plan
Collect data
Analyse data
Complete data analysis
Summarize what was learned
Change or test interventions
Define objectives,questions and
indicators
Plan data collection
Plan for the next cycle and decide
whether change will be replicated
Act Plan
DoStudy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 10
one patient awareness of falls
Time Scheduling A Time Planner Template
Measure of patient safety and
quality indicators
Reduction in the % of patient
falls per 1000 bed separations
monthly
Select change Tighten effective
communication and patient
education
Do Implement change Effective communication,
education and falls awareness
Study Evaluate change Improved communication and
awareness of patient falls and
associated injuries.
Reduced number of falls
reported within the period.
Act Adopt, reject or modify the
change plan
Positive improvement as
evidenced by improved
communication and falls
awareness.
Increased minimization of
falls per 1000 bed separations
by 60% of previous reported
one patient awareness of falls
Time Scheduling A Time Planner Template
Measure of patient safety and
quality indicators
Reduction in the % of patient
falls per 1000 bed separations
monthly
Select change Tighten effective
communication and patient
education
Do Implement change Effective communication,
education and falls awareness
Study Evaluate change Improved communication and
awareness of patient falls and
associated injuries.
Reduced number of falls
reported within the period.
Act Adopt, reject or modify the
change plan
Positive improvement as
evidenced by improved
communication and falls
awareness.
Increased minimization of
falls per 1000 bed separations
by 60% of previous reported
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 11
incidences.
PDSA CYCLE 2: Objective; Minimization of Patient Falls by at least 80% of all previously
reported cases in a six month period.
Plan The Improvement being
sought
Enhance healthcare providers’
skills and capacity to
minimize patient falls by 80%
of previously reported cases in
a six month’s period
Time Scheduling A Time Planner Template
Measure of patient safety and
quality indicators
Reduction in the % of patient
falls per 1000 bed separations
monthly
Select change Capacitating healthcare
providers through training and
education on handling
mentally ill patient falls
Do Implement change Train and educate healthcare
practitioners
Study Evaluate change % of healthcare practitioners
that can correctly handle
mentally ill patient’s falls and
injuries resulting from those
incidences.
PDSA CYCLE 2: Objective; Minimization of Patient Falls by at least 80% of all previously
reported cases in a six month period.
Plan The Improvement being
sought
Enhance healthcare providers’
skills and capacity to
minimize patient falls by 80%
of previously reported cases in
a six month’s period
Time Scheduling A Time Planner Template
Measure of patient safety and
quality indicators
Reduction in the % of patient
falls per 1000 bed separations
monthly
Select change Capacitating healthcare
providers through training and
education on handling
mentally ill patient falls
Do Implement change Train and educate healthcare
practitioners
Study Evaluate change % of healthcare practitioners
that can correctly handle
mentally ill patient’s falls and
injuries resulting from those
PATIENT QUALITY AND SAFETY INDICATORS: PATIENT FALLS 12
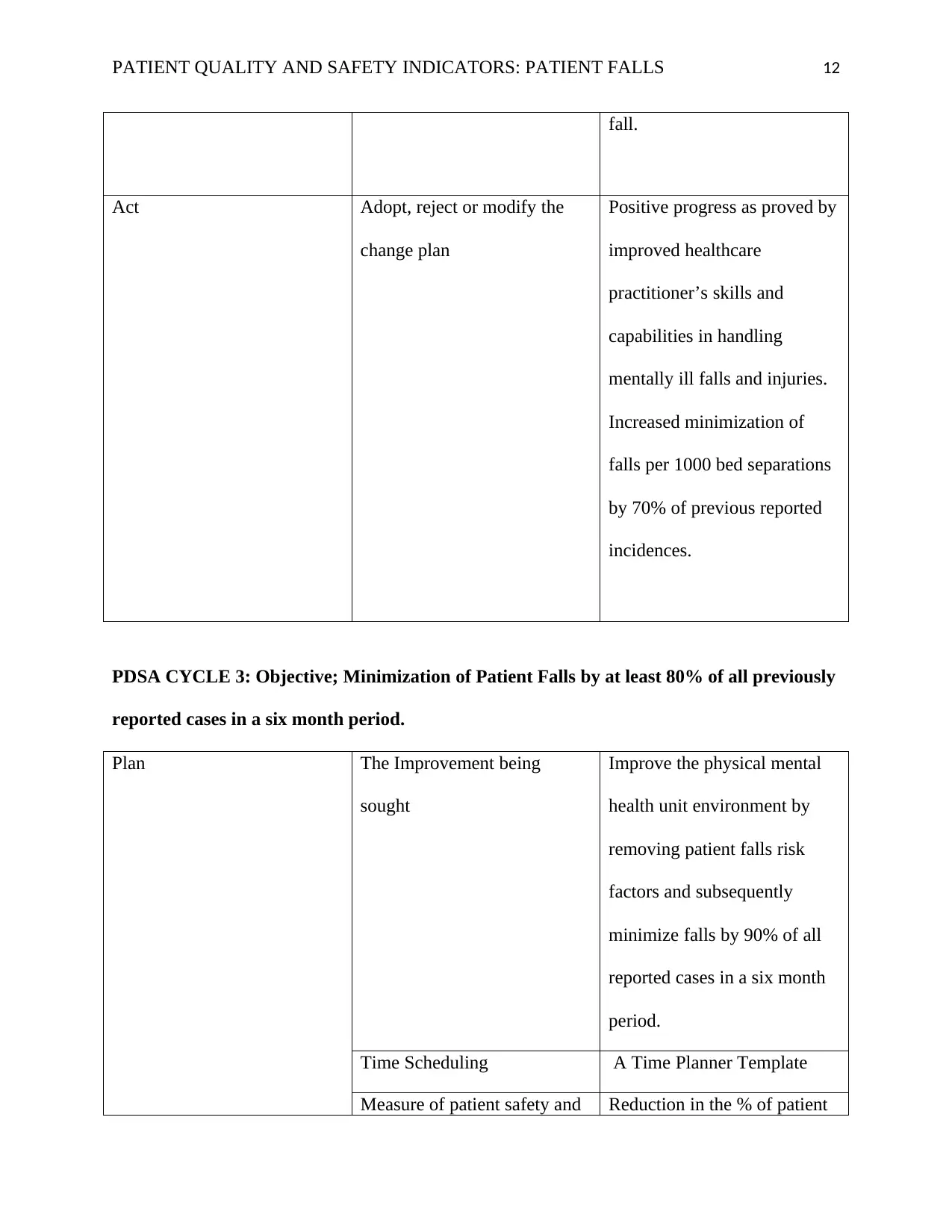
fall.
Act Adopt, reject or modify the
change plan
Positive progress as proved by
improved healthcare
practitioner’s skills and
capabilities in handling
mentally ill falls and injuries.
Increased minimization of
falls per 1000 bed separations
by 70% of previous reported
incidences.
PDSA CYCLE 3: Objective; Minimization of Patient Falls by at least 80% of all previously
reported cases in a six month period.
Plan The Improvement being
sought
Improve the physical mental
health unit environment by
removing patient falls risk
factors and subsequently
minimize falls by 90% of all
reported cases in a six month
period.
Time Scheduling A Time Planner Template
Measure of patient safety and Reduction in the % of patient
fall.
Act Adopt, reject or modify the
change plan
Positive progress as proved by
improved healthcare
practitioner’s skills and
capabilities in handling
mentally ill falls and injuries.
Increased minimization of
falls per 1000 bed separations
by 70% of previous reported
incidences.
PDSA CYCLE 3: Objective; Minimization of Patient Falls by at least 80% of all previously
reported cases in a six month period.
Plan The Improvement being
sought
Improve the physical mental
health unit environment by
removing patient falls risk
factors and subsequently
minimize falls by 90% of all
reported cases in a six month
period.
Time Scheduling A Time Planner Template
Measure of patient safety and Reduction in the % of patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





