Patient-Specific Surgical Guides: A Literature Review Analysis
VerifiedAdded on 2023/05/12
|21
|14384
|170
Report
AI Summary
This report presents a systematic literature review on the application of rapid prototyping (RP) in the creation of patient-specific surgical guides (PSGs) for various orthopaedic procedures. The review analyzes clinical and experimental studies, focusing on quantifiable outcomes, design details, and manufacturing processes of RP-PSGs. The research addresses key questions regarding the increasing use of RP-PSGs, their efficiency in terms of accuracy, time-saving, and cost-effectiveness, the preferred RP processes, and the critical design aspects. The findings highlight the advantages of RP-PSGs, such as reduced operating times and improved surgical accuracy, while also discussing potential disadvantages and sources of error. Stereolithography is identified as the primary RP process, with emerging applications in complex extremity surgeries, including spinal surgery and procedures on the forearm and foot. The review underscores the importance of cooperation between engineers and medical specialists in the development and use of RP-PSGs and aims to provide a comprehensive understanding of their use, design, manufacturing process, and potential for future enhancements in surgical applications. The review excluded studies on TKA and cranio-maxillofacial applications due to the availability of comprehensive surveys.
Review Article
Proc IMechE Part H:
J Engineering in Medicine
2016, Vol. 230(6) 495–515
Ó IMechE 2016
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/0954411916636919
pih.sagepub.com
Rapid prototyping for patient-specific
surgical orthopaedics guides: A
systematic literature review
Diana Popescu and Dan Laptoiu
Abstract
There has been a lot of hype surrounding the advantages to be gained from rapid prototyping processes in
fields,including medicine.Our literature review aims objectively to assess how effective patient-specific surgicalguides
manufactured using rapid prototyping are in a number of orthopaedic surgical applications. To this end, we
systematic review to identify and analyse clinicaland experimentalliterature studies in which rapid prototyping patient-
specific surgical guides are used, focusing especially on those that entail quantifiable outcomes and, at the
viding details on the guides’design and type ofmanufacturing process.Here,it should be mentioned that in this field
there are not yet medium- or long-term data,and no information on revisions.In the reviewed studies,the reported
positive opinions on the use of rapid prototyping patient-specific surgicalguides relate to the following main advantages:
reduction in operating times, low costs and improvements in the accuracy of surgical interventions thanks
sonalisation.However,disadvantages and sources of errors which can cause patient-specific surgicalguide failures are as
well discussed by authors.Stereolithography is the main rapid prototyping process employed in these applicat
although fused deposition modelling or selective laser sintering processes can also satisfy the requirementthese
applications in terms of materialproperties,manufacturing accuracy and construction time.Another of our findings was
that individualised drill guides for spinal surgery are currently the favourite candidates for manufacture us
typing.Other emerging applications relate to complex orthopaedic surgery ofthe extremities:the forearm and foot.
Severalprocedures such as osteotomies for radius malunions or tarsalcoalition could become standard,thanks to the
significantassistance provided by rapid prototyping patient-specific surgicalguides in planning and performing such
operations.
Keywords
Patient-specific guide, rapid prototyping, orthopaedic instrumentation, computer-aided surgery
Date received: 1 October 2015; accepted: 3 February 2016
Introduction
Rapid prototyping (RP)is a group of manufacturing
processes that can build physicalobjects directly from
three-dimensional(3D) virtualmodeldata in an addi-
tive way,which is to say,by superimposing layers of
material one on top of the other. Other terms used for
this kind of processes are layer manufacturing,layer
fabrication,solid freeform fabrication and layer-by-
layer fabrication. Since 2013, the standard name, addi-
tive manufacturing (AM) has been defined as ‘the pro-
cessof joining materialsto make objectsfrom 3D
modeldata,usually layer upon layer,as opposed to
subtractive manufacturing technologies’.1 However, the
analysiscarried outfor this article showed thatthe
term RP is used more often in the medical literature, as
the advantages offered by such processes are in direct
correlation to surgical guides’ individualisation, that is,
the concept of a prototype.
Personalised healthcare is becoming an increasingly
salientapproach to medicine,2 and advances in both
medicaland technicalfields are being focused on pro-
viding solutions for medicalinterventions and devices
Politehnica University of Bucharest, Bucharest, Romania
Orthopaedics, Clinical Hospital Colentina, Bucharest, Romania
Chelariu Clinic, Bacau, Romania
Corresponding author:
Dan Laptoiu, Orthopaedics, Clinical Hospital Colentina, Sos. Stefan cel
Mare, 19-21, code 020125 Sector 2, Bucharest, Romania.
Email: danlaptoiu@yahoo.com
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Proc IMechE Part H:
J Engineering in Medicine
2016, Vol. 230(6) 495–515
Ó IMechE 2016
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/0954411916636919
pih.sagepub.com
Rapid prototyping for patient-specific
surgical orthopaedics guides: A
systematic literature review
Diana Popescu and Dan Laptoiu
Abstract
There has been a lot of hype surrounding the advantages to be gained from rapid prototyping processes in
fields,including medicine.Our literature review aims objectively to assess how effective patient-specific surgicalguides
manufactured using rapid prototyping are in a number of orthopaedic surgical applications. To this end, we
systematic review to identify and analyse clinicaland experimentalliterature studies in which rapid prototyping patient-
specific surgical guides are used, focusing especially on those that entail quantifiable outcomes and, at the
viding details on the guides’design and type ofmanufacturing process.Here,it should be mentioned that in this field
there are not yet medium- or long-term data,and no information on revisions.In the reviewed studies,the reported
positive opinions on the use of rapid prototyping patient-specific surgicalguides relate to the following main advantages:
reduction in operating times, low costs and improvements in the accuracy of surgical interventions thanks
sonalisation.However,disadvantages and sources of errors which can cause patient-specific surgicalguide failures are as
well discussed by authors.Stereolithography is the main rapid prototyping process employed in these applicat
although fused deposition modelling or selective laser sintering processes can also satisfy the requirementthese
applications in terms of materialproperties,manufacturing accuracy and construction time.Another of our findings was
that individualised drill guides for spinal surgery are currently the favourite candidates for manufacture us
typing.Other emerging applications relate to complex orthopaedic surgery ofthe extremities:the forearm and foot.
Severalprocedures such as osteotomies for radius malunions or tarsalcoalition could become standard,thanks to the
significantassistance provided by rapid prototyping patient-specific surgicalguides in planning and performing such
operations.
Keywords
Patient-specific guide, rapid prototyping, orthopaedic instrumentation, computer-aided surgery
Date received: 1 October 2015; accepted: 3 February 2016
Introduction
Rapid prototyping (RP)is a group of manufacturing
processes that can build physicalobjects directly from
three-dimensional(3D) virtualmodeldata in an addi-
tive way,which is to say,by superimposing layers of
material one on top of the other. Other terms used for
this kind of processes are layer manufacturing,layer
fabrication,solid freeform fabrication and layer-by-
layer fabrication. Since 2013, the standard name, addi-
tive manufacturing (AM) has been defined as ‘the pro-
cessof joining materialsto make objectsfrom 3D
modeldata,usually layer upon layer,as opposed to
subtractive manufacturing technologies’.1 However, the
analysiscarried outfor this article showed thatthe
term RP is used more often in the medical literature, as
the advantages offered by such processes are in direct
correlation to surgical guides’ individualisation, that is,
the concept of a prototype.
Personalised healthcare is becoming an increasingly
salientapproach to medicine,2 and advances in both
medicaland technicalfields are being focused on pro-
viding solutions for medicalinterventions and devices
Politehnica University of Bucharest, Bucharest, Romania
Orthopaedics, Clinical Hospital Colentina, Bucharest, Romania
Chelariu Clinic, Bacau, Romania
Corresponding author:
Dan Laptoiu, Orthopaedics, Clinical Hospital Colentina, Sos. Stefan cel
Mare, 19-21, code 020125 Sector 2, Bucharest, Romania.
Email: danlaptoiu@yahoo.com
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
tailored to the patient’s bone morphology and individ-
ual needs.Patient-specific surgicalguides (PSGs)are
part of this approach,thus representing a subjectof
interest for both surgeons and engineers.
The use of RP processesto manufacture patient-
specific surgicalguides(RP-PSGs) specially designed
for a specific patient can be traced back in 1997, when
Van Brusselet al.3 reported the design,manufacture
and use of the first individualised template for drilling
trajectories when inserting pedicle screws into the verte-
bra of a human spine.In 1998,Radermacher etal.4
employed the stereolithography (SL) process to obtain
the physical prototype of a PSG for pelvic osteotomies.
Berry et al.5 also engaged in studies of image processing
methods, data conversion and manufacturing using the
selective laser sintering (SLS) process.Ever since then,
the number ofsuch applications has been increasing
thanks to a greater awareness of the advantages offered
by RP processes in manufacturing objects with compli-
cated geometricalfeatures (freeform features).This is
the case of PSGs designed to exactly fit the patient’s
anatomical structures, thus supporting increased preci-
sion in a number of surgical procedures.
The improvement in the accuracy of screw implanta-
tion techniques and other orthopaedic surgicalproce-
dures has been possible through the use of radiological
examination during surgery.The irradiation during
such proceduresis higher in percutaneoussurgery,
where,in order to make as small as possible incisions,
the use of interventionalradiology isrequired when
identifying anatomicallandmarks.Therefore, in recent
years,intra-operativenavigation systemshave been
developed and implemented in operating theatresin
order to visualisethe patient’sanatomicalstructure
without resortingto interventionalradiology.This
approach is based on pre-operative image acquisition
and on the use of an anatomical landmarks system cali-
brated atthe beginning ofthe surgicalintervention.
However, performing this calibration process is a com-
plicated task.Moreover,the static landmarksestab-
lished at the beginningof surgerydo not always
maintain thesameposition throughoutthe surgical
procedure,which obviously leadsto imprecision.In
this context,PSGs can representan alternative when
used for guiding surgicalactions such as drilling,tap-
ping, cutting or axis alignment, since they transfer to a
physicalobject (called guide,jig or template)the
planned trajectories required in order to prepare the
bones for the implantation and fixation of screws, rods
and plates.6 These guides can also help to identify the
correctposition/orientation ofinstrumentsor substi-
tute for an instrument,as is the case in totalknee
arthroplasty (TKA) applications,7 for instance.
The personalisation of surgical guides implies coop-
eration between engineers and medical specialists8 when
obtaining patient’s scan data, modelling the anatomical
areas of interest, planning the surgery/tool trajectories,
designing the guide,choosing the materialand manu-
facturing process,building the guide,and sterilising
and utilising it.The flow is similar for allPSGs, but
what differs is the design of the guides,which is dic-
tated by the patient’s anatomy, the type of intervention
and surgicalapproach,as well as by the anatomical
landmarks selected by the surgeon in the pre-operative
stage.Other requirements,such as transparency9 or
multi-level guides10,11for spinal applications, may also
be considered convenientsolutionsin some medical
cases.
However, despite reported cases of orthopaedic sur-
gicaloperations in which PSGs manufactured via RP
processes have been used, to the best of our knowledge
literaturereviews have been conductedonly for
TKA 7,12,13
and cranio-maxillofacialapplications.14 No
systematic information is yet available for other ortho-
paedic applications such as spinalsurgery or correc-
tions of malunions or deformitiespresentedin
literature.
In this context,this review addresses these applica-
tions, the information in the article being organised so
that to answer four questions. This approach represents
a modality to organise the information found when
querying the literature databases, the questions provid-
ing a structured and systematic manner to analyse the
data presented in RP-PSGsliterature studies.Thus,
these questions can be considered as filters applied for
screening the literature in the field. Moreover, these are
the questions that engineers and surgeons are first ask-
ing themselves when decide to start build and use such
devices.
These questions are as follows:
Q1. Has there been a significantconstantincrease in
the use of RP-PSGs in the last couple of years?
Q2. What is the reported efficiency (in terms of accu-
racy, operation time saving and costs) of RP-PSGs use
in orthopaedic surgery?
Q3. Is there a preferred RP process for manufacturing
such guides and, if so, why?
Q4. What are the main aspects taken into account dur-
ing the RP-PSGs design process?
The answers offered by our article aim to provide the
basisfor a more accurate understanding ofthe use,
design and manufacturing process, on one hand, and of
the advantages and pitfalls of RP-PSGs in several ortho-
paedicsurgeryinterventions,on other hand. Thus,
knowledge can be gathered and hopefully used for fur-
ther studies and enhancements in the field by providing
possible suggestions for improvements in PSGs and for
their use in other types of surgical applications.
Materials and methods
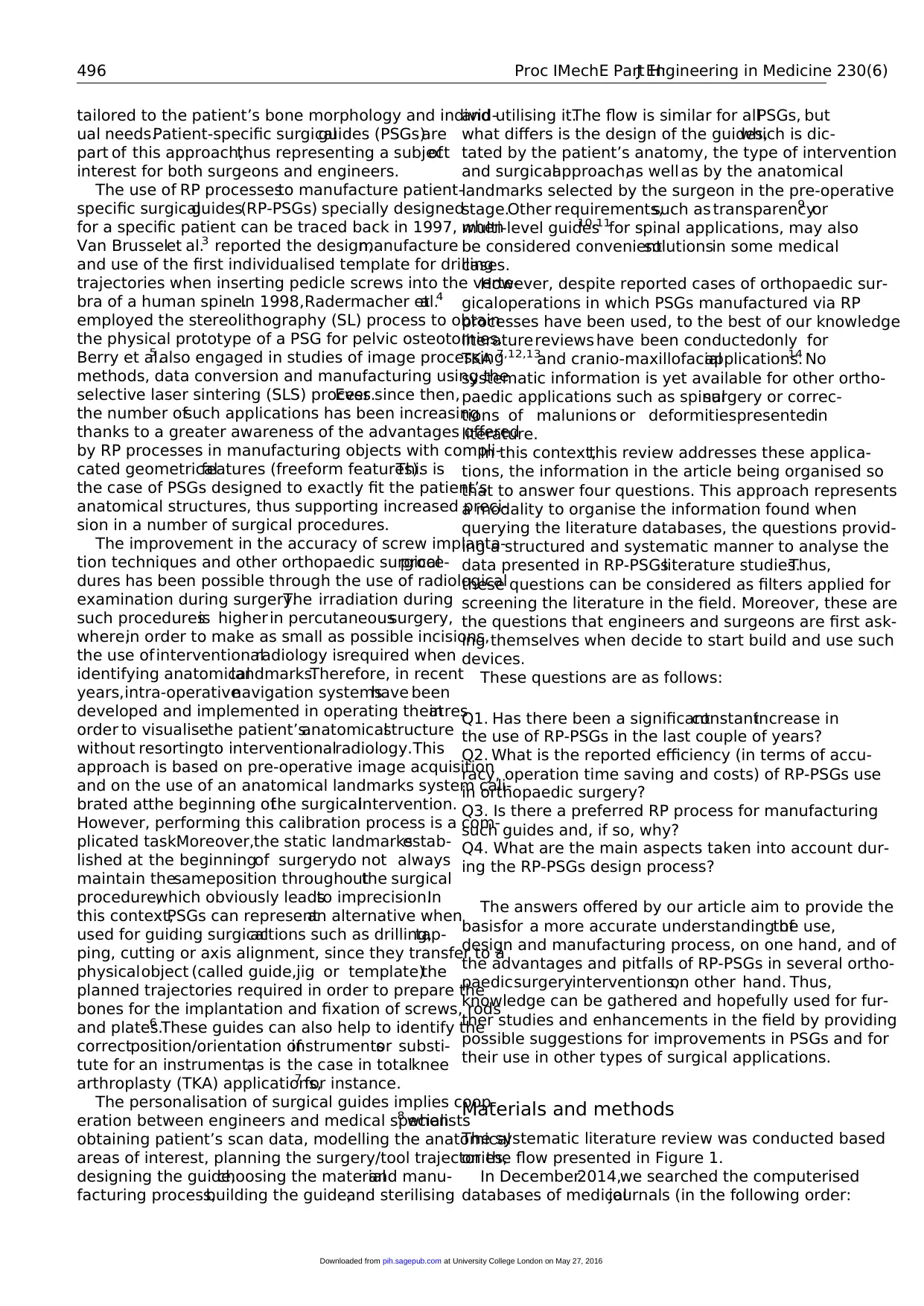
The systematic literature review was conducted based
on the flow presented in Figure 1.
In December2014,we searched the computerised
databases of medicaljournals (in the following order:
496 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
ual needs.Patient-specific surgicalguides (PSGs)are
part of this approach,thus representing a subjectof
interest for both surgeons and engineers.
The use of RP processesto manufacture patient-
specific surgicalguides(RP-PSGs) specially designed
for a specific patient can be traced back in 1997, when
Van Brusselet al.3 reported the design,manufacture
and use of the first individualised template for drilling
trajectories when inserting pedicle screws into the verte-
bra of a human spine.In 1998,Radermacher etal.4
employed the stereolithography (SL) process to obtain
the physical prototype of a PSG for pelvic osteotomies.
Berry et al.5 also engaged in studies of image processing
methods, data conversion and manufacturing using the
selective laser sintering (SLS) process.Ever since then,
the number ofsuch applications has been increasing
thanks to a greater awareness of the advantages offered
by RP processes in manufacturing objects with compli-
cated geometricalfeatures (freeform features).This is
the case of PSGs designed to exactly fit the patient’s
anatomical structures, thus supporting increased preci-
sion in a number of surgical procedures.
The improvement in the accuracy of screw implanta-
tion techniques and other orthopaedic surgicalproce-
dures has been possible through the use of radiological
examination during surgery.The irradiation during
such proceduresis higher in percutaneoussurgery,
where,in order to make as small as possible incisions,
the use of interventionalradiology isrequired when
identifying anatomicallandmarks.Therefore, in recent
years,intra-operativenavigation systemshave been
developed and implemented in operating theatresin
order to visualisethe patient’sanatomicalstructure
without resortingto interventionalradiology.This
approach is based on pre-operative image acquisition
and on the use of an anatomical landmarks system cali-
brated atthe beginning ofthe surgicalintervention.
However, performing this calibration process is a com-
plicated task.Moreover,the static landmarksestab-
lished at the beginningof surgerydo not always
maintain thesameposition throughoutthe surgical
procedure,which obviously leadsto imprecision.In
this context,PSGs can representan alternative when
used for guiding surgicalactions such as drilling,tap-
ping, cutting or axis alignment, since they transfer to a
physicalobject (called guide,jig or template)the
planned trajectories required in order to prepare the
bones for the implantation and fixation of screws, rods
and plates.6 These guides can also help to identify the
correctposition/orientation ofinstrumentsor substi-
tute for an instrument,as is the case in totalknee
arthroplasty (TKA) applications,7 for instance.
The personalisation of surgical guides implies coop-
eration between engineers and medical specialists8 when
obtaining patient’s scan data, modelling the anatomical
areas of interest, planning the surgery/tool trajectories,
designing the guide,choosing the materialand manu-
facturing process,building the guide,and sterilising
and utilising it.The flow is similar for allPSGs, but
what differs is the design of the guides,which is dic-
tated by the patient’s anatomy, the type of intervention
and surgicalapproach,as well as by the anatomical
landmarks selected by the surgeon in the pre-operative
stage.Other requirements,such as transparency9 or
multi-level guides10,11for spinal applications, may also
be considered convenientsolutionsin some medical
cases.
However, despite reported cases of orthopaedic sur-
gicaloperations in which PSGs manufactured via RP
processes have been used, to the best of our knowledge
literaturereviews have been conductedonly for
TKA 7,12,13
and cranio-maxillofacialapplications.14 No
systematic information is yet available for other ortho-
paedic applications such as spinalsurgery or correc-
tions of malunions or deformitiespresentedin
literature.
In this context,this review addresses these applica-
tions, the information in the article being organised so
that to answer four questions. This approach represents
a modality to organise the information found when
querying the literature databases, the questions provid-
ing a structured and systematic manner to analyse the
data presented in RP-PSGsliterature studies.Thus,
these questions can be considered as filters applied for
screening the literature in the field. Moreover, these are
the questions that engineers and surgeons are first ask-
ing themselves when decide to start build and use such
devices.
These questions are as follows:
Q1. Has there been a significantconstantincrease in
the use of RP-PSGs in the last couple of years?
Q2. What is the reported efficiency (in terms of accu-
racy, operation time saving and costs) of RP-PSGs use
in orthopaedic surgery?
Q3. Is there a preferred RP process for manufacturing
such guides and, if so, why?
Q4. What are the main aspects taken into account dur-
ing the RP-PSGs design process?
The answers offered by our article aim to provide the
basisfor a more accurate understanding ofthe use,
design and manufacturing process, on one hand, and of
the advantages and pitfalls of RP-PSGs in several ortho-
paedicsurgeryinterventions,on other hand. Thus,
knowledge can be gathered and hopefully used for fur-
ther studies and enhancements in the field by providing
possible suggestions for improvements in PSGs and for
their use in other types of surgical applications.
Materials and methods
The systematic literature review was conducted based
on the flow presented in Figure 1.
In December2014,we searched the computerised
databases of medicaljournals (in the following order:
496 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
PubMed, Springer, Elsevier and SearchMedica) for the
following typesof English-languagestudies:clinical
trials,comparative studies,evaluation studies,journal
articles,meta-analysis,reviews,systematic reviews and
validation studies.
The timeframe we selected for the search was 2005–
2014.Although initially we intended to focus only on
research carried outafter 2009,we subsequently rea-
lised that a review of a longer period (10 years) would
be more appropriate if we were to identify a growing
trend.We thoughtto consider 2009 as our reference
point, because this was the year when the patent for the
fused deposition modelling (FDM)processexpired,
bringing abouta ‘democratisation’of the field and a
substantialincrease in the number of applications and
manufactured parts,which could also have an impact
on the use of RP in medical applications.
Combinations of the following keywords were used
in the search on PubMed:‘rapid prototyping’and
‘guide’,‘template’,‘patient-specificinstrumentation’,
‘cutting’, ‘drill’ and ‘osteotomies’(all fields).
Combinations of words containing the terms: ‘additive
manufacturing’, ‘jigs’ and ‘3D printing’ were also used,
but they did not generate new results,that is,results
other than those presented below.
Thus, we identified 344 potentially eligible studies, as
follows:
Rapid prototyping AND guide: 95 results;
Rapid prototyping AND cutting: 23 results;
Rapid prototyping AND drill: 34 results;
Rapid prototypingAND patient-specificinstru-
mentation: 27 results;
Rapid prototyping AND osteotomies: 72 results;
Rapid prototyping AND template: 93 results.
The searcheson SearchMedica,Springer and
Elsevierproduced mostly duplicateresultsof those
from PubMed, while additional referenceswere
obtained through examination ofthe bibliography of
the articles using a shortlist obtained after two screen-
ings, as we detailed below.
In order to eliminate duplicates, the results were fil-
tered, first using the functionalities offered by PubMed
and then by ordering all the search outcomes by author.
We were left with 224 papers to provide our focus.
The nextstep was to apply exclusion criteria.We
decided to remove from the systematic literature review
paperson RP general applicationsin medicine and
papers that related RP processes to implants manufac-
turing or scaffolds fabrication,as these were not ger-
mane to our questionsand selected field ofinterest
(orthopaedic surgery). In addition, studies on the use of
RP-PSGs in TKA and cranio-maxillofacial applications
were also excluded,given the existence ofnew and
Figure 1. Flowchart for studies selection.
Popescu and Laptoiu 497
at University College London on May 27, 2016pih.sagepub.comDownloaded from
following typesof English-languagestudies:clinical
trials,comparative studies,evaluation studies,journal
articles,meta-analysis,reviews,systematic reviews and
validation studies.
The timeframe we selected for the search was 2005–
2014.Although initially we intended to focus only on
research carried outafter 2009,we subsequently rea-
lised that a review of a longer period (10 years) would
be more appropriate if we were to identify a growing
trend.We thoughtto consider 2009 as our reference
point, because this was the year when the patent for the
fused deposition modelling (FDM)processexpired,
bringing abouta ‘democratisation’of the field and a
substantialincrease in the number of applications and
manufactured parts,which could also have an impact
on the use of RP in medical applications.
Combinations of the following keywords were used
in the search on PubMed:‘rapid prototyping’and
‘guide’,‘template’,‘patient-specificinstrumentation’,
‘cutting’, ‘drill’ and ‘osteotomies’(all fields).
Combinations of words containing the terms: ‘additive
manufacturing’, ‘jigs’ and ‘3D printing’ were also used,
but they did not generate new results,that is,results
other than those presented below.
Thus, we identified 344 potentially eligible studies, as
follows:
Rapid prototyping AND guide: 95 results;
Rapid prototyping AND cutting: 23 results;
Rapid prototyping AND drill: 34 results;
Rapid prototypingAND patient-specificinstru-
mentation: 27 results;
Rapid prototyping AND osteotomies: 72 results;
Rapid prototyping AND template: 93 results.
The searcheson SearchMedica,Springer and
Elsevierproduced mostly duplicateresultsof those
from PubMed, while additional referenceswere
obtained through examination ofthe bibliography of
the articles using a shortlist obtained after two screen-
ings, as we detailed below.
In order to eliminate duplicates, the results were fil-
tered, first using the functionalities offered by PubMed
and then by ordering all the search outcomes by author.
We were left with 224 papers to provide our focus.
The nextstep was to apply exclusion criteria.We
decided to remove from the systematic literature review
paperson RP general applicationsin medicine and
papers that related RP processes to implants manufac-
turing or scaffolds fabrication,as these were not ger-
mane to our questionsand selected field ofinterest
(orthopaedic surgery). In addition, studies on the use of
RP-PSGs in TKA and cranio-maxillofacial applications
were also excluded,given the existence ofnew and
Figure 1. Flowchart for studies selection.
Popescu and Laptoiu 497
at University College London on May 27, 2016pih.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
comprehensivesurveys.Nor werestudiespresenting
TKA surgical guide applications from companies such
as Smith and Nephew, Biomet and Zimmer included in
the survey in order to avoid presentation of potentially
biased information, and also because they are not offer-
ing too many technical details on the design aspects and
manufacturing process.Moreover,Thienpontet al.15
already presented a comprehensive survey (Europe and
worldwide)on patient-specificinstrumentationfor
TKA (including RP guides), based on information from
orthopaedic companies (2011–2012 volumes ofsales).
Therefore, we focused our review only on the cases pre-
sented in the literature as we consider that they can pro-
vide documented technicalinformation on different
aspects ofthe development,use and evaluation pro-
cesses of this type of surgical guides.
Papers with English titles that came up in the search
results,but which werewritten in other languages
(German,Chinese and Japanese) were also eliminated
from our list. We assumed that it was more than likely
that the results laid out in these papers had also been
published in English in various journals.
In the end, 52 studies were retained for further anal-
ysis. When filtering titles and abstracts, we noticed the
very large number of RP applications in manufacturing
PSGs for dental applications, an area better developed
than that of orthopaedic surgery.
In the next stageof filtering,the articleswere
reviewed in full by both authors independently,in
order to establish mutualagreement,especially given
that their separate fields of specialisation (engineering
and medicine)mightdetermine differentperspectives
on and understandings of the same subject. In addition,
a supplementary search was carried out using the refer-
ences found in the 52 articles,thereby generating nine
further papers relating to the subject.
Thus, a total of 61 studies presenting applications of
RP processes in the manufacturing of PSGs for ortho-
paedic surgery,in both clinicalcases and experiments
on cadavers, were selected for ‘List 1’. However, not all
of thesearticlescontained sufficientinformation or
outcomes(i.e. radiologicaldata for PSG usefulness
assessment,information on guide design,information
on computed tomography (CT)scanning protocols,
typesof RP process and materials)to answer our
questions.Furthermore,some of the articles presented
information or preliminary information that was later
repeated, in a more detailed manner, in other papers or
book chapters. For these reasons, 23 papers were elimi-
nated from ‘List 1’, and the remaining 38 articles
(named as ‘List 2’) are discussed separately in section
‘Discussion’.The articles in ‘List 2’were divided into
two broad categories:RP-PSGs for spinal surgery
applications (discussed in section ‘RP-PSGs for spinal
surgery applications’) and RP-PSGs for other general
orthopaedic surgery applications (osteotomies,tumour
resections, etc., discussed in section ‘RP-PSGs for gen-
eral orthopaedic surgery applications’).
In conclusion,the articles in ‘List1’ were used to
answer Q1 and Q2,and,in part,the other questions,
while the articles in ‘List 2’ provided a detailed exami-
nation of specific RP-PSGs design and manufacturing
criteria, diverse methods and approaches, reported effi-
ciency, thereby providing answers to Q3 and Q4.
Results
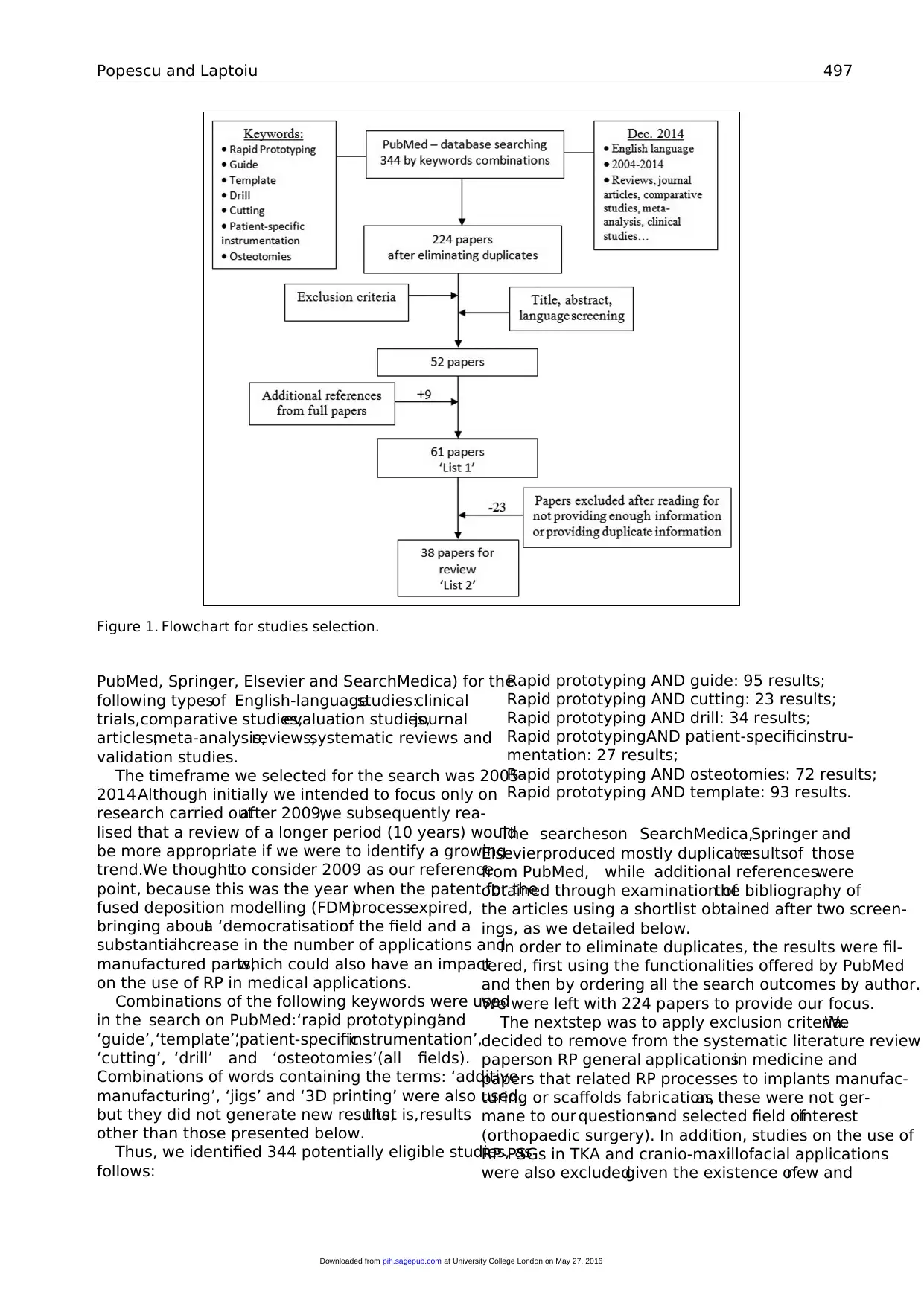
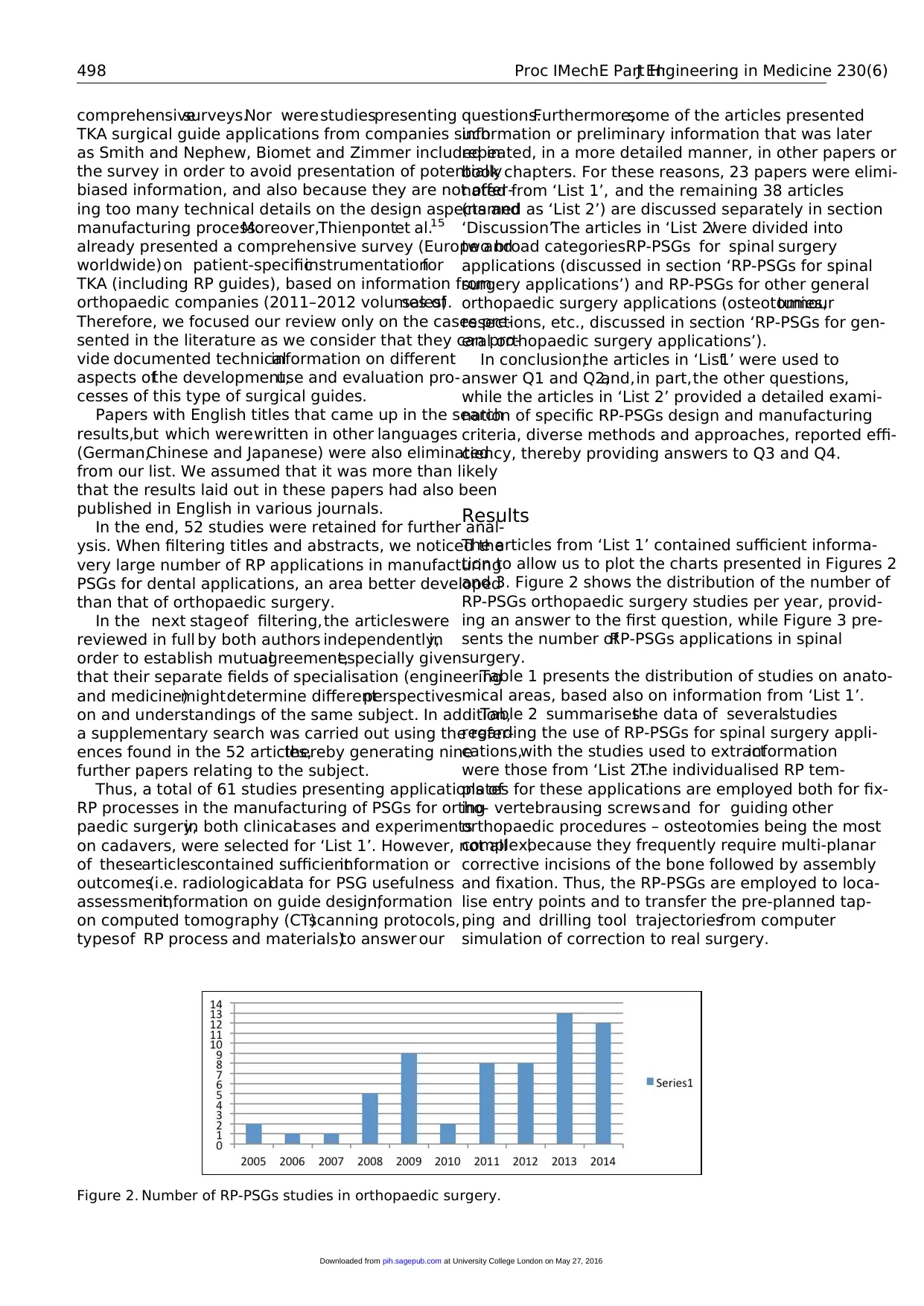
The articles from ‘List 1’ contained sufficient informa-
tion to allow us to plot the charts presented in Figures 2
and 3. Figure 2 shows the distribution of the number of
RP-PSGs orthopaedic surgery studies per year, provid-
ing an answer to the first question, while Figure 3 pre-
sents the number ofRP-PSGs applications in spinal
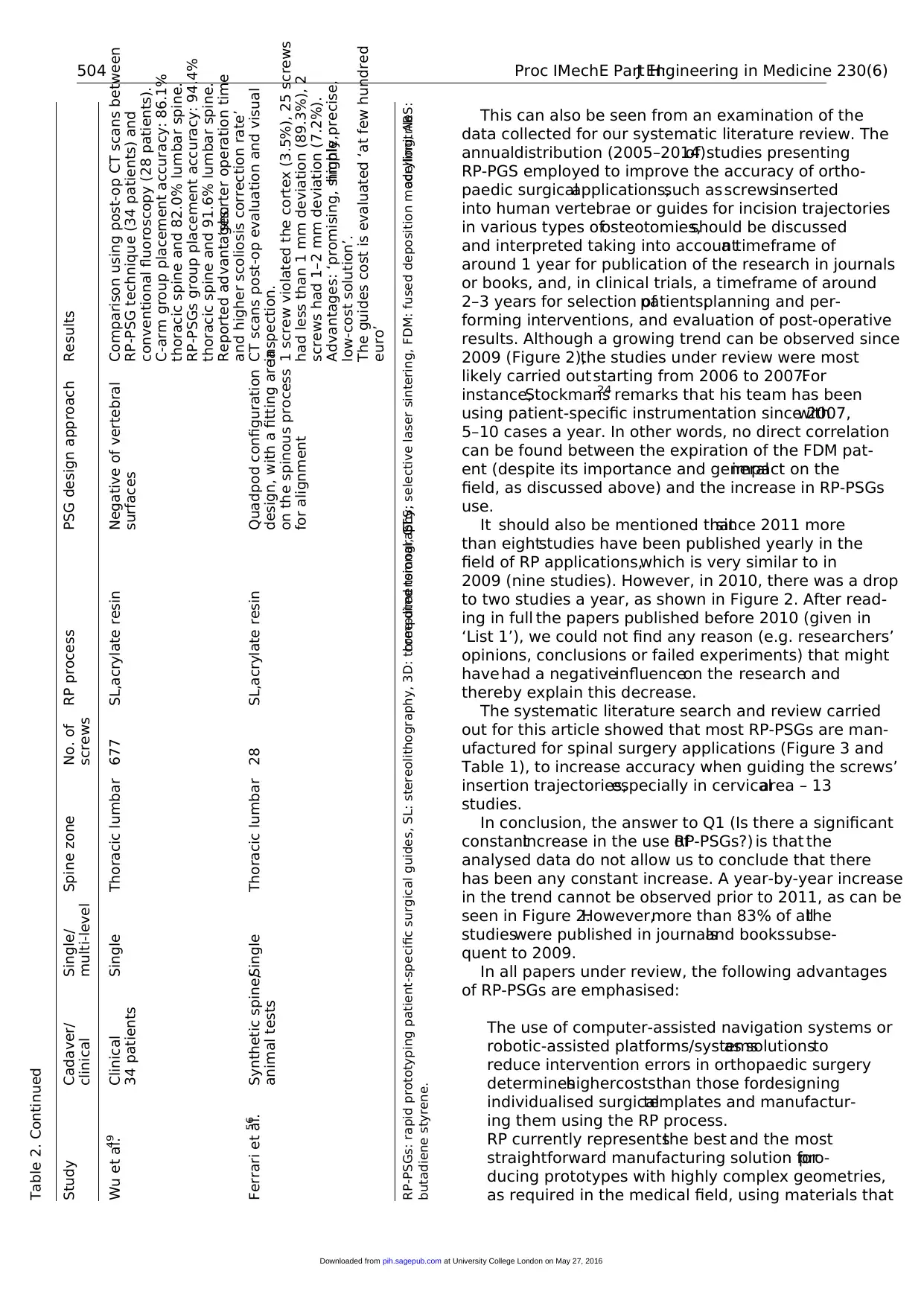
surgery.
Table 1 presents the distribution of studies on anato-
mical areas, based also on information from ‘List 1’.
Table 2 summarisesthe data of severalstudies
regarding the use of RP-PSGs for spinal surgery appli-
cations,with the studies used to extractinformation
were those from ‘List 2’.The individualised RP tem-
plates for these applications are employed both for fix-
ing vertebrausing screwsand for guiding other
orthopaedic procedures – osteotomies being the most
complex,because they frequently require multi-planar
corrective incisions of the bone followed by assembly
and fixation. Thus, the RP-PSGs are employed to loca-
lise entry points and to transfer the pre-planned tap-
ping and drilling tool trajectoriesfrom computer
simulation of correction to real surgery.
Figure 2. Number of RP-PSGs studies in orthopaedic surgery.
498 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
TKA surgical guide applications from companies such
as Smith and Nephew, Biomet and Zimmer included in
the survey in order to avoid presentation of potentially
biased information, and also because they are not offer-
ing too many technical details on the design aspects and
manufacturing process.Moreover,Thienpontet al.15
already presented a comprehensive survey (Europe and
worldwide)on patient-specificinstrumentationfor
TKA (including RP guides), based on information from
orthopaedic companies (2011–2012 volumes ofsales).
Therefore, we focused our review only on the cases pre-
sented in the literature as we consider that they can pro-
vide documented technicalinformation on different
aspects ofthe development,use and evaluation pro-
cesses of this type of surgical guides.
Papers with English titles that came up in the search
results,but which werewritten in other languages
(German,Chinese and Japanese) were also eliminated
from our list. We assumed that it was more than likely
that the results laid out in these papers had also been
published in English in various journals.
In the end, 52 studies were retained for further anal-
ysis. When filtering titles and abstracts, we noticed the
very large number of RP applications in manufacturing
PSGs for dental applications, an area better developed
than that of orthopaedic surgery.
In the next stageof filtering,the articleswere
reviewed in full by both authors independently,in
order to establish mutualagreement,especially given
that their separate fields of specialisation (engineering
and medicine)mightdetermine differentperspectives
on and understandings of the same subject. In addition,
a supplementary search was carried out using the refer-
ences found in the 52 articles,thereby generating nine
further papers relating to the subject.
Thus, a total of 61 studies presenting applications of
RP processes in the manufacturing of PSGs for ortho-
paedic surgery,in both clinicalcases and experiments
on cadavers, were selected for ‘List 1’. However, not all
of thesearticlescontained sufficientinformation or
outcomes(i.e. radiologicaldata for PSG usefulness
assessment,information on guide design,information
on computed tomography (CT)scanning protocols,
typesof RP process and materials)to answer our
questions.Furthermore,some of the articles presented
information or preliminary information that was later
repeated, in a more detailed manner, in other papers or
book chapters. For these reasons, 23 papers were elimi-
nated from ‘List 1’, and the remaining 38 articles
(named as ‘List 2’) are discussed separately in section
‘Discussion’.The articles in ‘List 2’were divided into
two broad categories:RP-PSGs for spinal surgery
applications (discussed in section ‘RP-PSGs for spinal
surgery applications’) and RP-PSGs for other general
orthopaedic surgery applications (osteotomies,tumour
resections, etc., discussed in section ‘RP-PSGs for gen-
eral orthopaedic surgery applications’).
In conclusion,the articles in ‘List1’ were used to
answer Q1 and Q2,and,in part,the other questions,
while the articles in ‘List 2’ provided a detailed exami-
nation of specific RP-PSGs design and manufacturing
criteria, diverse methods and approaches, reported effi-
ciency, thereby providing answers to Q3 and Q4.
Results
The articles from ‘List 1’ contained sufficient informa-
tion to allow us to plot the charts presented in Figures 2
and 3. Figure 2 shows the distribution of the number of
RP-PSGs orthopaedic surgery studies per year, provid-
ing an answer to the first question, while Figure 3 pre-
sents the number ofRP-PSGs applications in spinal
surgery.
Table 1 presents the distribution of studies on anato-
mical areas, based also on information from ‘List 1’.
Table 2 summarisesthe data of severalstudies
regarding the use of RP-PSGs for spinal surgery appli-
cations,with the studies used to extractinformation
were those from ‘List 2’.The individualised RP tem-
plates for these applications are employed both for fix-
ing vertebrausing screwsand for guiding other
orthopaedic procedures – osteotomies being the most
complex,because they frequently require multi-planar
corrective incisions of the bone followed by assembly
and fixation. Thus, the RP-PSGs are employed to loca-
lise entry points and to transfer the pre-planned tap-
ping and drilling tool trajectoriesfrom computer
simulation of correction to real surgery.
Figure 2. Number of RP-PSGs studies in orthopaedic surgery.
498 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
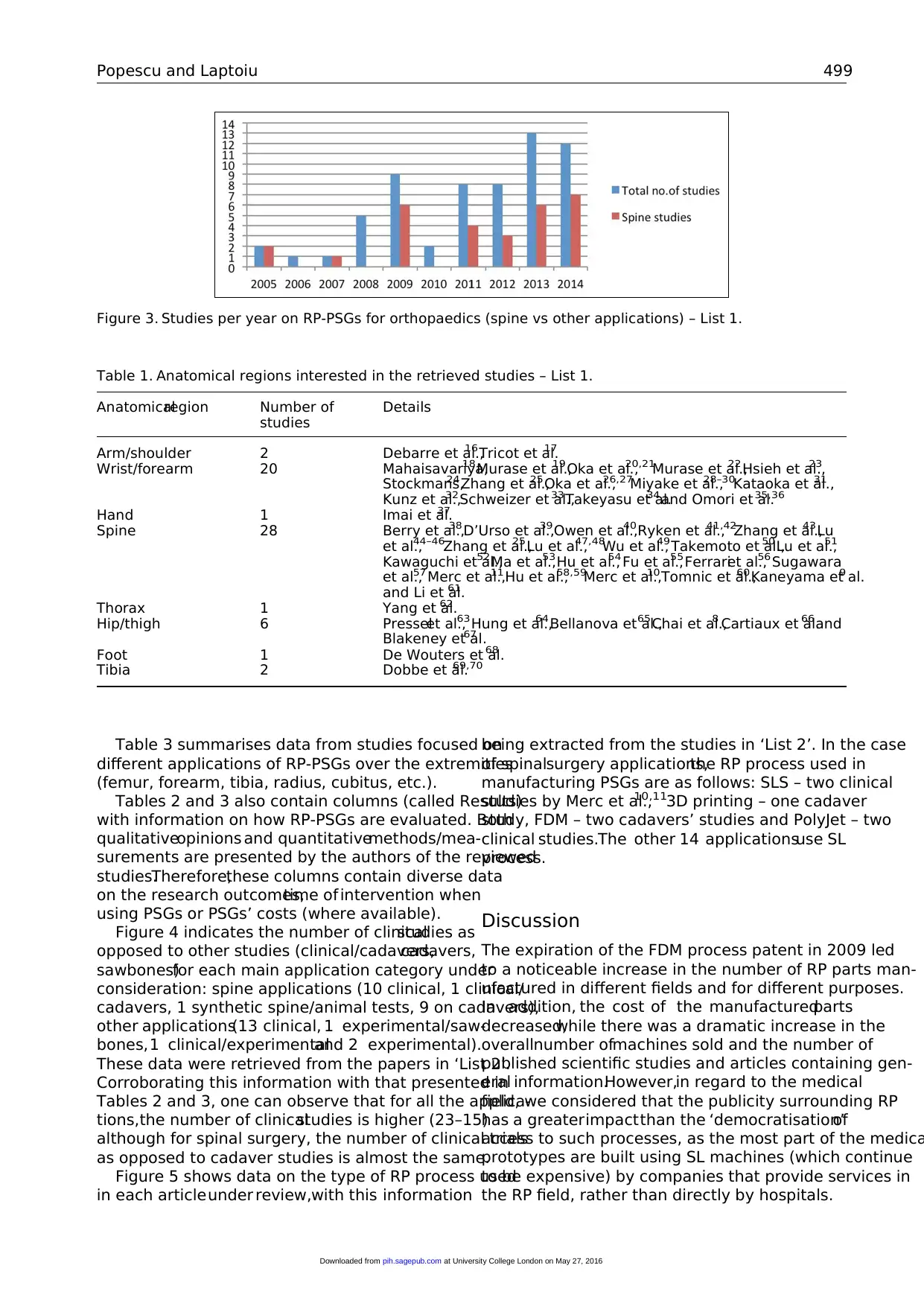
Table 3 summarises data from studies focused on
different applications of RP-PSGs over the extremities
(femur, forearm, tibia, radius, cubitus, etc.).
Tables 2 and 3 also contain columns (called Results)
with information on how RP-PSGs are evaluated. Both
qualitativeopinions and quantitativemethods/mea-
surements are presented by the authors of the reviewed
studies.Therefore,these columns contain diverse data
on the research outcomes,time of intervention when
using PSGs or PSGs’ costs (where available).
Figure 4 indicates the number of clinicalstudies as
opposed to other studies (clinical/cadavers,cadavers,
sawbones)for each main application category under
consideration: spine applications (10 clinical, 1 clinical/
cadavers, 1 synthetic spine/animal tests, 9 on cadavers),
other applications(13 clinical, 1 experimental/saw-
bones,1 clinical/experimentaland 2 experimental).
These data were retrieved from the papers in ‘List 2’.
Corroborating this information with that presented in
Tables 2 and 3, one can observe that for all the applica-
tions,the number of clinicalstudies is higher (23–15)
although for spinal surgery, the number of clinical trials
as opposed to cadaver studies is almost the same.
Figure 5 shows data on the type of RP process used
in each articleunder review,with this information
being extracted from the studies in ‘List 2’. In the case
of spinalsurgery applications,the RP process used in
manufacturing PSGs are as follows: SLS – two clinical
studies by Merc et al.,10,113D printing – one cadaver
study, FDM – two cadavers’ studies and PolyJet – two
clinical studies.The other 14 applicationsuse SL
process.
Discussion
The expiration of the FDM process patent in 2009 led
to a noticeable increase in the number of RP parts man-
ufactured in different fields and for different purposes.
In addition, the cost of the manufacturedparts
decreased,while there was a dramatic increase in the
overallnumber ofmachines sold and the number of
published scientific studies and articles containing gen-
eral information.However,in regard to the medical
field, we considered that the publicity surrounding RP
has a greaterimpactthan the ‘democratisation’of
access to such processes, as the most part of the medica
prototypes are built using SL machines (which continue
to be expensive) by companies that provide services in
the RP field, rather than directly by hospitals.
Table 1. Anatomical regions interested in the retrieved studies – List 1.
Anatomicalregion Number of
studies
Details
Arm/shoulder 2 Debarre et al.,16 Tricot et al.17
Wrist/forearm 20 Mahaisavariya,18 Murase et al.,19 Oka et al.,20,21
Murase et al.,22 Hsieh et al.,23
Stockmans,24Zhang et al.,25Oka et al.,26,27
Miyake et al.,28–30Kataoka et al.,31
Kunz et al.,32 Schweizer et al.,33 Takeyasu et al.34 and Omori et al.35,36
Hand 1 Imai et al.37
Spine 28 Berry et al.,38 D’Urso et al.,39 Owen et al.,40 Ryken et al.,41,42
Zhang et al.,43 Lu
et al.,44–46Zhang et al.,25 Lu et al.,47,48
Wu et al.,49 Takemoto et al.,50 Lu et al.,51
Kawaguchi et al.,52 Ma et al.,53 Hu et al.,54 Fu et al.,55Ferrariet al.,56 Sugawara
et al.,57 Merc et al.,11 Hu et al.,58,59
Merc et al.,10 Tomnic et al.,60Kaneyama et al.9
and Li et al.61
Thorax 1 Yang et al.62
Hip/thigh 6 Presselet al.,63Hung et al.,64 Bellanova et al.,65 Chai et al.,8 Cartiaux et al.66and
Blakeney et al.67
Foot 1 De Wouters et al.68
Tibia 2 Dobbe et al.69,70
Figure 3. Studies per year on RP-PSGs for orthopaedics (spine vs other applications) – List 1.
Popescu and Laptoiu 499
at University College London on May 27, 2016pih.sagepub.comDownloaded from
different applications of RP-PSGs over the extremities
(femur, forearm, tibia, radius, cubitus, etc.).
Tables 2 and 3 also contain columns (called Results)
with information on how RP-PSGs are evaluated. Both
qualitativeopinions and quantitativemethods/mea-
surements are presented by the authors of the reviewed
studies.Therefore,these columns contain diverse data
on the research outcomes,time of intervention when
using PSGs or PSGs’ costs (where available).
Figure 4 indicates the number of clinicalstudies as
opposed to other studies (clinical/cadavers,cadavers,
sawbones)for each main application category under
consideration: spine applications (10 clinical, 1 clinical/
cadavers, 1 synthetic spine/animal tests, 9 on cadavers),
other applications(13 clinical, 1 experimental/saw-
bones,1 clinical/experimentaland 2 experimental).
These data were retrieved from the papers in ‘List 2’.
Corroborating this information with that presented in
Tables 2 and 3, one can observe that for all the applica-
tions,the number of clinicalstudies is higher (23–15)
although for spinal surgery, the number of clinical trials
as opposed to cadaver studies is almost the same.
Figure 5 shows data on the type of RP process used
in each articleunder review,with this information
being extracted from the studies in ‘List 2’. In the case
of spinalsurgery applications,the RP process used in
manufacturing PSGs are as follows: SLS – two clinical
studies by Merc et al.,10,113D printing – one cadaver
study, FDM – two cadavers’ studies and PolyJet – two
clinical studies.The other 14 applicationsuse SL
process.
Discussion
The expiration of the FDM process patent in 2009 led
to a noticeable increase in the number of RP parts man-
ufactured in different fields and for different purposes.
In addition, the cost of the manufacturedparts
decreased,while there was a dramatic increase in the
overallnumber ofmachines sold and the number of
published scientific studies and articles containing gen-
eral information.However,in regard to the medical
field, we considered that the publicity surrounding RP
has a greaterimpactthan the ‘democratisation’of
access to such processes, as the most part of the medica
prototypes are built using SL machines (which continue
to be expensive) by companies that provide services in
the RP field, rather than directly by hospitals.
Table 1. Anatomical regions interested in the retrieved studies – List 1.
Anatomicalregion Number of
studies
Details
Arm/shoulder 2 Debarre et al.,16 Tricot et al.17
Wrist/forearm 20 Mahaisavariya,18 Murase et al.,19 Oka et al.,20,21
Murase et al.,22 Hsieh et al.,23
Stockmans,24Zhang et al.,25Oka et al.,26,27
Miyake et al.,28–30Kataoka et al.,31
Kunz et al.,32 Schweizer et al.,33 Takeyasu et al.34 and Omori et al.35,36
Hand 1 Imai et al.37
Spine 28 Berry et al.,38 D’Urso et al.,39 Owen et al.,40 Ryken et al.,41,42
Zhang et al.,43 Lu
et al.,44–46Zhang et al.,25 Lu et al.,47,48
Wu et al.,49 Takemoto et al.,50 Lu et al.,51
Kawaguchi et al.,52 Ma et al.,53 Hu et al.,54 Fu et al.,55Ferrariet al.,56 Sugawara
et al.,57 Merc et al.,11 Hu et al.,58,59
Merc et al.,10 Tomnic et al.,60Kaneyama et al.9
and Li et al.61
Thorax 1 Yang et al.62
Hip/thigh 6 Presselet al.,63Hung et al.,64 Bellanova et al.,65 Chai et al.,8 Cartiaux et al.66and
Blakeney et al.67
Foot 1 De Wouters et al.68
Tibia 2 Dobbe et al.69,70
Figure 3. Studies per year on RP-PSGs for orthopaedics (spine vs other applications) – List 1.
Popescu and Laptoiu 499
at University College London on May 27, 2016pih.sagepub.comDownloaded from
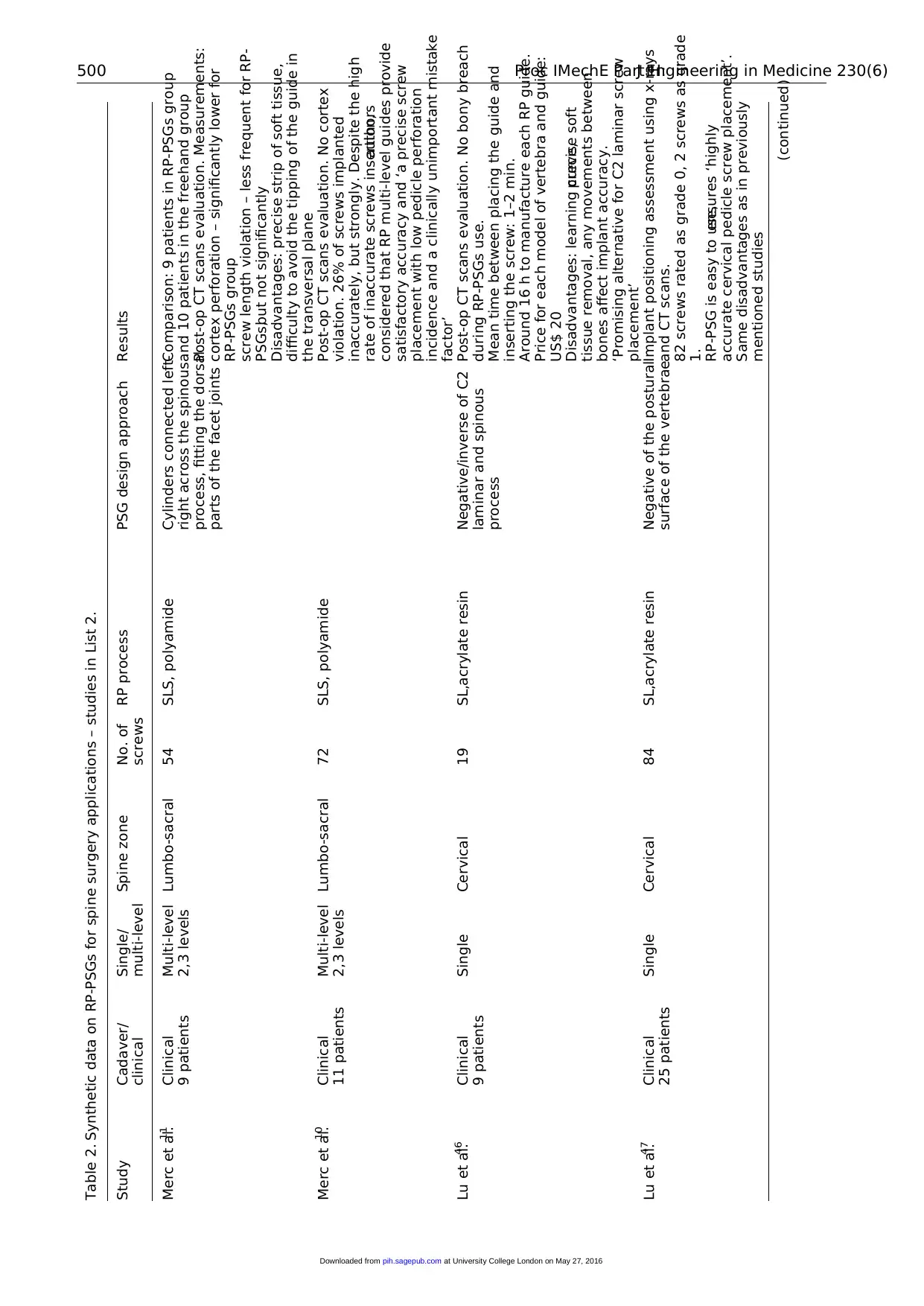
Table 2. Synthetic data on RP-PSGs for spine surgery applications – studies in List 2.
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Merc et al.11 Clinical
9 patients
Multi-level
2,3 levels
Lumbo-sacral 54 SLS, polyamide Cylinders connected left-
right across the spinous
process, fitting the dorsal
parts of the facet joints
Comparison: 9 patients in RP-PSGs group
and 10 patients in the freehand group
Post-op CT scans evaluation. Measurements:
cortex perforation – significantly lower for
RP-PSGs group
screw length violation – less frequent for RP-
PSGs,but not significantly
Disadvantages: precise strip of soft tissue,
difficulty to avoid the tipping of the guide in
the transversal plane
Merc et al.10 Clinical
11 patients
Multi-level
2,3 levels
Lumbo-sacral 72 SLS, polyamide Post-op CT scans evaluation. No cortex
violation. 26% of screws implanted
inaccurately, but strongly. Despite the high
rate of inaccurate screws insertion,authors
considered that RP multi-level guides provide
satisfactory accuracy and ‘a precise screw
placement with low pedicle perforation
incidence and a clinically unimportant mistake
factor’
Lu et al.46 Clinical
9 patients
Single Cervical 19 SL,acrylate resin Negative/inverse of C2
laminar and spinous
process
Post-op CT scans evaluation. No bony breach
during RP-PSGs use.
Mean time between placing the guide and
inserting the screw: 1–2 min.
Around 16 h to manufacture each RP guide.
Price for each model of vertebra and guide:
US$ 20
Disadvantages: learning curve,precise soft
tissue removal, any movements between
bones affect implant accuracy.
‘Promising alternative for C2 laminar screw
placement’
Lu et al.47 Clinical
25 patients
Single Cervical 84 SL,acrylate resin Negative of the postural
surface of the vertebrae
Implant positioning assessment using x-rays
and CT scans.
82 screws rated as grade 0, 2 screws as grade
1.
RP-PSG is easy to use,ensures ‘highly
accurate cervical pedicle screw placement’.
Same disadvantages as in previously
mentioned studies
(continued)500 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Merc et al.11 Clinical
9 patients
Multi-level
2,3 levels
Lumbo-sacral 54 SLS, polyamide Cylinders connected left-
right across the spinous
process, fitting the dorsal
parts of the facet joints
Comparison: 9 patients in RP-PSGs group
and 10 patients in the freehand group
Post-op CT scans evaluation. Measurements:
cortex perforation – significantly lower for
RP-PSGs group
screw length violation – less frequent for RP-
PSGs,but not significantly
Disadvantages: precise strip of soft tissue,
difficulty to avoid the tipping of the guide in
the transversal plane
Merc et al.10 Clinical
11 patients
Multi-level
2,3 levels
Lumbo-sacral 72 SLS, polyamide Post-op CT scans evaluation. No cortex
violation. 26% of screws implanted
inaccurately, but strongly. Despite the high
rate of inaccurate screws insertion,authors
considered that RP multi-level guides provide
satisfactory accuracy and ‘a precise screw
placement with low pedicle perforation
incidence and a clinically unimportant mistake
factor’
Lu et al.46 Clinical
9 patients
Single Cervical 19 SL,acrylate resin Negative/inverse of C2
laminar and spinous
process
Post-op CT scans evaluation. No bony breach
during RP-PSGs use.
Mean time between placing the guide and
inserting the screw: 1–2 min.
Around 16 h to manufacture each RP guide.
Price for each model of vertebra and guide:
US$ 20
Disadvantages: learning curve,precise soft
tissue removal, any movements between
bones affect implant accuracy.
‘Promising alternative for C2 laminar screw
placement’
Lu et al.47 Clinical
25 patients
Single Cervical 84 SL,acrylate resin Negative of the postural
surface of the vertebrae
Implant positioning assessment using x-rays
and CT scans.
82 screws rated as grade 0, 2 screws as grade
1.
RP-PSG is easy to use,ensures ‘highly
accurate cervical pedicle screw placement’.
Same disadvantages as in previously
mentioned studies
(continued)500 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
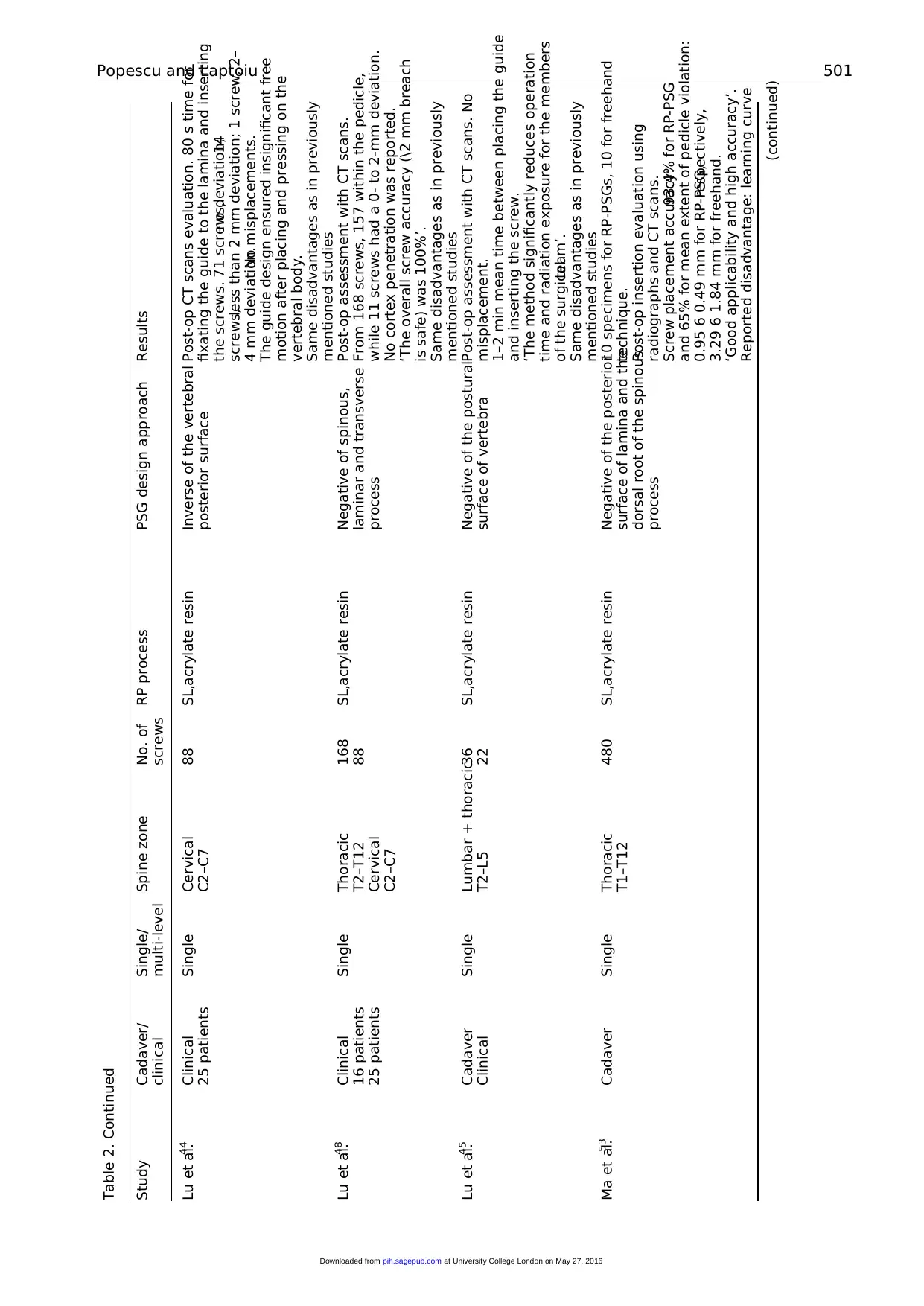
Table 2. Continued
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Lu et al.44 Clinical
25 patients
Single Cervical
C2–C7
88 SL,acrylate resin Inverse of the vertebral
posterior surface
Post-op CT scans evaluation. 80 s time for
fixating the guide to the lamina and inserting
the screws. 71 screws,no deviation;14
screws,less than 2 mm deviation; 1 screw, 2–
4 mm deviation.No misplacements.
The guide design ensured insignificant free
motion after placing and pressing on the
vertebral body.
Same disadvantages as in previously
mentioned studies
Lu et al.48 Clinical
16 patients
25 patients
Single Thoracic
T2–T12
Cervical
C2–C7
168
88
SL,acrylate resin Negative of spinous,
laminar and transverse
process
Post-op assessment with CT scans.
From 168 screws, 157 within the pedicle,
while 11 screws had a 0- to 2-mm deviation.
No cortex penetration was reported.
‘The overall screw accuracy (\2 mm breach
is safe) was 100%’.
Same disadvantages as in previously
mentioned studies
Lu et al.45 Cadaver
Clinical
Single Lumbar + thoracic
T2–L5
36
22
SL,acrylate resin Negative of the postural
surface of vertebra
Post-op assessment with CT scans. No
misplacement.
1–2 min mean time between placing the guide
and inserting the screw.
‘The method significantly reduces operation
time and radiation exposure for the members
of the surgicalteam’.
Same disadvantages as in previously
mentioned studies
Ma et al.53 Cadaver Single Thoracic
T1–T12
480 SL,acrylate resin Negative of the posterior
surface of lamina and the
dorsal root of the spinous
process
10 specimens for RP-PSGs, 10 for freehand
technique.
Post-op insertion evaluation using
radiographs and CT scans.
Screw placement accuracy:93.4% for RP-PSG
and 65% for mean extent of pedicle violation:
0.95 6 0.49 mm for RP-PSG,respectively,
3.29 6 1.84 mm for freehand.
‘Good applicability and high accuracy’.
Reported disadvantage: learning curve
(continued)Popescu and Laptoiu 501
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Lu et al.44 Clinical
25 patients
Single Cervical
C2–C7
88 SL,acrylate resin Inverse of the vertebral
posterior surface
Post-op CT scans evaluation. 80 s time for
fixating the guide to the lamina and inserting
the screws. 71 screws,no deviation;14
screws,less than 2 mm deviation; 1 screw, 2–
4 mm deviation.No misplacements.
The guide design ensured insignificant free
motion after placing and pressing on the
vertebral body.
Same disadvantages as in previously
mentioned studies
Lu et al.48 Clinical
16 patients
25 patients
Single Thoracic
T2–T12
Cervical
C2–C7
168
88
SL,acrylate resin Negative of spinous,
laminar and transverse
process
Post-op assessment with CT scans.
From 168 screws, 157 within the pedicle,
while 11 screws had a 0- to 2-mm deviation.
No cortex penetration was reported.
‘The overall screw accuracy (\2 mm breach
is safe) was 100%’.
Same disadvantages as in previously
mentioned studies
Lu et al.45 Cadaver
Clinical
Single Lumbar + thoracic
T2–L5
36
22
SL,acrylate resin Negative of the postural
surface of vertebra
Post-op assessment with CT scans. No
misplacement.
1–2 min mean time between placing the guide
and inserting the screw.
‘The method significantly reduces operation
time and radiation exposure for the members
of the surgicalteam’.
Same disadvantages as in previously
mentioned studies
Ma et al.53 Cadaver Single Thoracic
T1–T12
480 SL,acrylate resin Negative of the posterior
surface of lamina and the
dorsal root of the spinous
process
10 specimens for RP-PSGs, 10 for freehand
technique.
Post-op insertion evaluation using
radiographs and CT scans.
Screw placement accuracy:93.4% for RP-PSG
and 65% for mean extent of pedicle violation:
0.95 6 0.49 mm for RP-PSG,respectively,
3.29 6 1.84 mm for freehand.
‘Good applicability and high accuracy’.
Reported disadvantage: learning curve
(continued)Popescu and Laptoiu 501
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
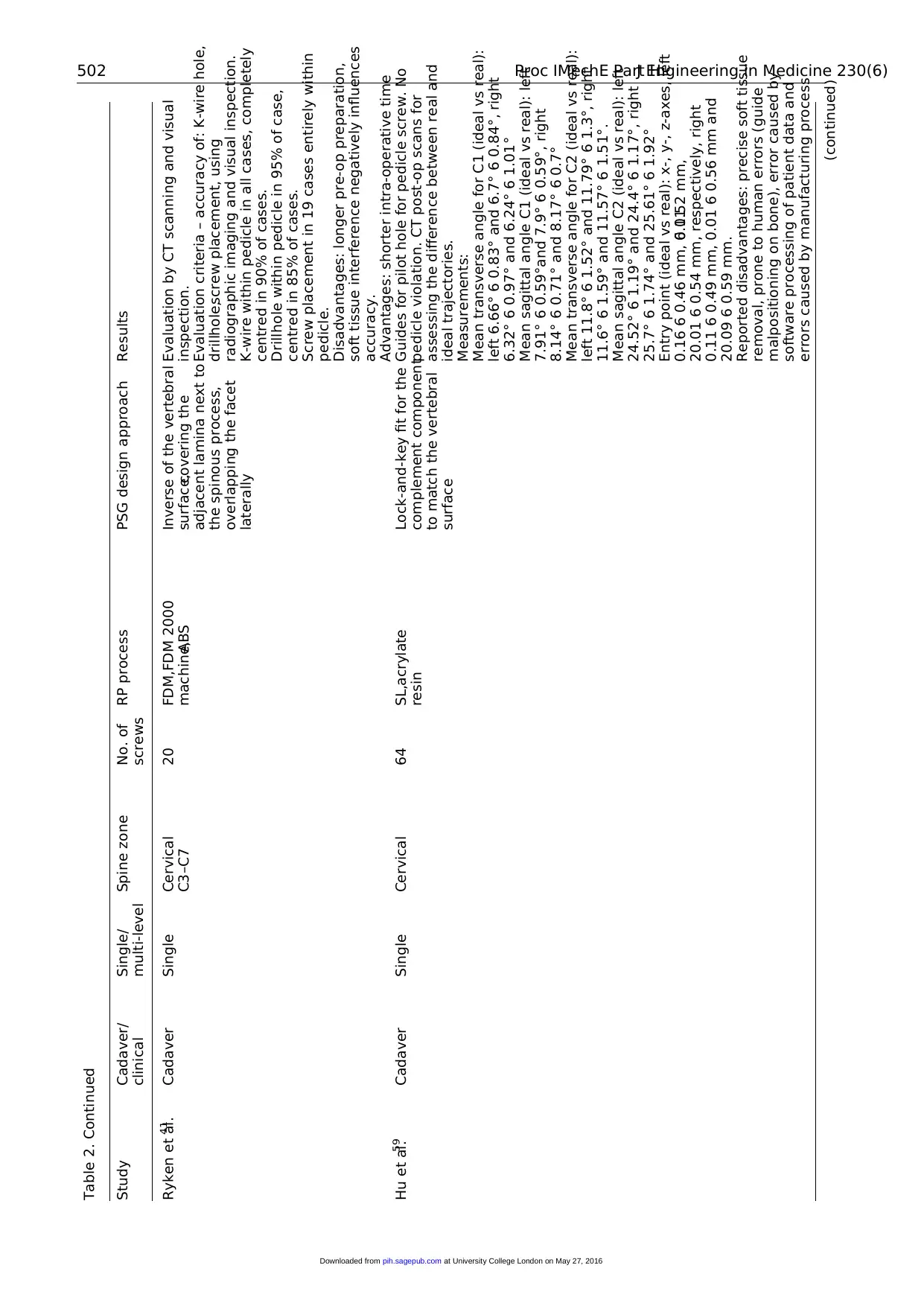
Table 2. Continued
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Ryken et al.41 Cadaver Single Cervical
C3–C7
20 FDM,FDM 2000
machine,ABS
Inverse of the vertebral
surface,covering the
adjacent lamina next to
the spinous process,
overlapping the facet
laterally
Evaluation by CT scanning and visual
inspection.
Evaluation criteria – accuracy of: K-wire hole,
drillhole,screw placement, using
radiographic imaging and visual inspection.
K-wire within pedicle in all cases, completely
centred in 90% of cases.
Drillhole within pedicle in 95% of case,
centred in 85% of cases.
Screw placement in 19 cases entirely within
pedicle.
Disadvantages: longer pre-op preparation,
soft tissue interference negatively influences
accuracy.
Advantages: shorter intra-operative time
Hu et al.59 Cadaver Single Cervical 64 SL,acrylate
resin
Lock-and-key fit for the
complement component
to match the vertebral
surface
Guides for pilot hole for pedicle screw. No
pedicle violation. CT post-op scans for
assessing the difference between real and
ideal trajectories.
Measurements:
Mean transverse angle for C1 (ideal vs real):
left 6.66° 6 0.83° and 6.7° 6 0.84°, right
6.32° 6 0.97° and 6.24° 6 1.01°
Mean sagittal angle C1 (ideal vs real): left
7.91° 6 0.59°and 7.9° 6 0.59°, right
8.14° 6 0.71° and 8.17° 6 0.7°
Mean transverse angle for C2 (ideal vs real):
left 11.8° 6 1.52° and 11.79° 6 1.3°, right
11.6° 6 1.59° and 11.57° 6 1.51°.
Mean sagittal angle C2 (ideal vs real): left
24.52° 6 1.19° and 24.4° 6 1.17°, right
25.7° 6 1.74° and 25.61° 6 1.92°
Entry point (ideal vs real): x-, y-, z-axes, left
0.16 6 0.46 mm, 0.116 0.52 mm,
20.01 6 0.54 mm, respectively, right
0.11 6 0.49 mm, 0.01 6 0.56 mm and
20.09 6 0.59 mm.
Reported disadvantages: precise soft tissue
removal, prone to human errors (guide
malpositioning on bone), error caused by
software processing of patient data and
errors caused by manufacturing process
(continued)502 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Ryken et al.41 Cadaver Single Cervical
C3–C7
20 FDM,FDM 2000
machine,ABS
Inverse of the vertebral
surface,covering the
adjacent lamina next to
the spinous process,
overlapping the facet
laterally
Evaluation by CT scanning and visual
inspection.
Evaluation criteria – accuracy of: K-wire hole,
drillhole,screw placement, using
radiographic imaging and visual inspection.
K-wire within pedicle in all cases, completely
centred in 90% of cases.
Drillhole within pedicle in 95% of case,
centred in 85% of cases.
Screw placement in 19 cases entirely within
pedicle.
Disadvantages: longer pre-op preparation,
soft tissue interference negatively influences
accuracy.
Advantages: shorter intra-operative time
Hu et al.59 Cadaver Single Cervical 64 SL,acrylate
resin
Lock-and-key fit for the
complement component
to match the vertebral
surface
Guides for pilot hole for pedicle screw. No
pedicle violation. CT post-op scans for
assessing the difference between real and
ideal trajectories.
Measurements:
Mean transverse angle for C1 (ideal vs real):
left 6.66° 6 0.83° and 6.7° 6 0.84°, right
6.32° 6 0.97° and 6.24° 6 1.01°
Mean sagittal angle C1 (ideal vs real): left
7.91° 6 0.59°and 7.9° 6 0.59°, right
8.14° 6 0.71° and 8.17° 6 0.7°
Mean transverse angle for C2 (ideal vs real):
left 11.8° 6 1.52° and 11.79° 6 1.3°, right
11.6° 6 1.59° and 11.57° 6 1.51°.
Mean sagittal angle C2 (ideal vs real): left
24.52° 6 1.19° and 24.4° 6 1.17°, right
25.7° 6 1.74° and 25.61° 6 1.92°
Entry point (ideal vs real): x-, y-, z-axes, left
0.16 6 0.46 mm, 0.116 0.52 mm,
20.01 6 0.54 mm, respectively, right
0.11 6 0.49 mm, 0.01 6 0.56 mm and
20.09 6 0.59 mm.
Reported disadvantages: precise soft tissue
removal, prone to human errors (guide
malpositioning on bone), error caused by
software processing of patient data and
errors caused by manufacturing process
(continued)502 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
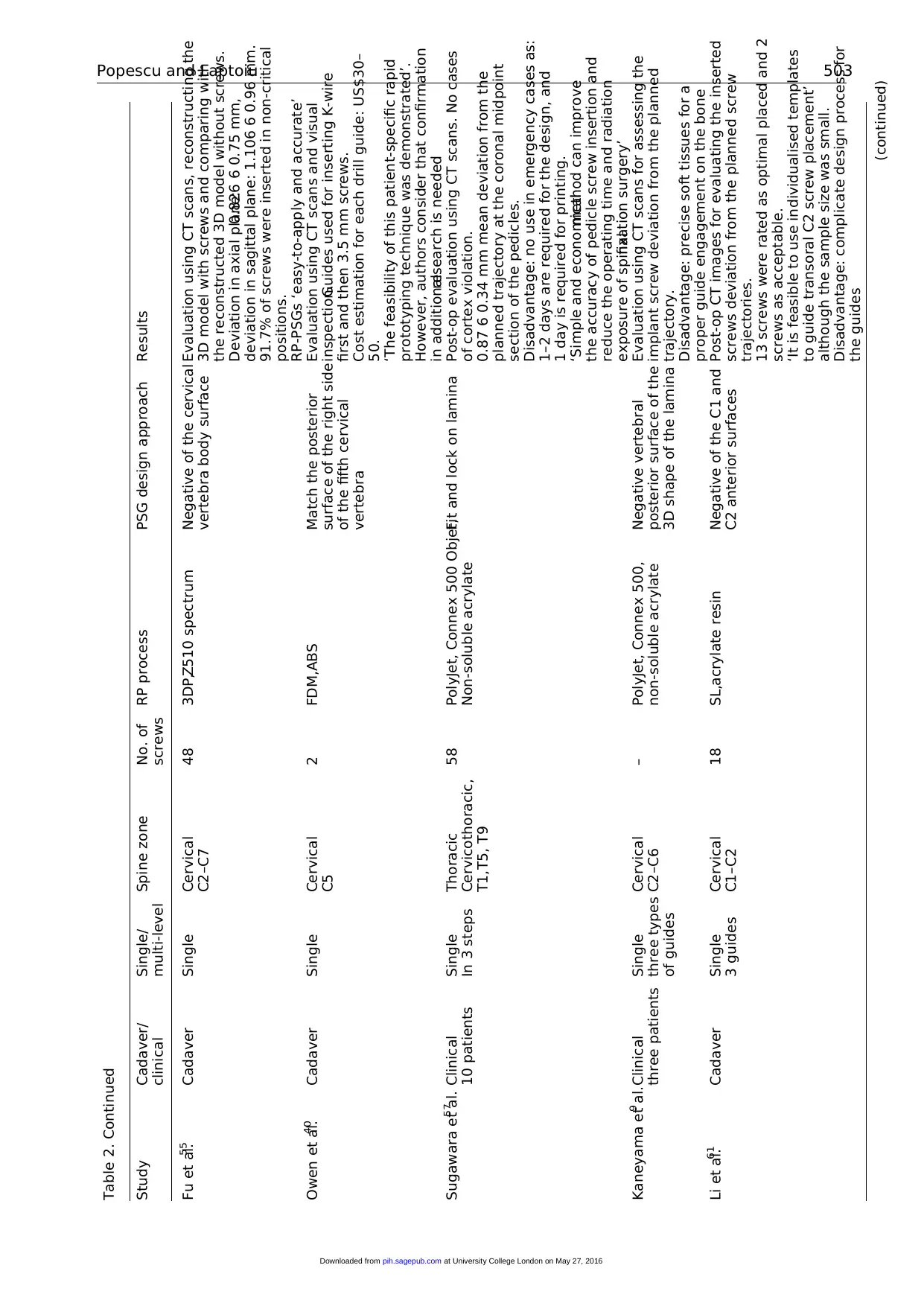
Table 2. Continued
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Fu et al.55 Cadaver Single Cervical
C2–C7
48 3DP,Z510 spectrum Negative of the cervical
vertebra body surface
Evaluation using CT scans, reconstructing the
3D model with screws and comparing with
the reconstructed 3D model without screws.
Deviation in axial plane:0.826 6 0.75 mm,
deviation in sagittal plane: 1.106 6 0.96 mm.
91.7% of screws were inserted in non-critical
positions.
RP-PSGs ‘easy-to-apply and accurate’
Owen et al.40 Cadaver Single Cervical
C5
2 FDM,ABS Match the posterior
surface of the right side
of the fifth cervical
vertebra
Evaluation using CT scans and visual
inspection.Guides used for inserting K-wire
first and then 3.5 mm screws.
Cost estimation for each drill guide: US$30–
50.
‘The feasibility of this patient-specific rapid
prototyping technique was demonstrated’.
However, authors consider that confirmation
in additionalresearch is needed
Sugawara et al.57 Clinical
10 patients
Single
In 3 steps
Thoracic
Cervicothoracic,
T1,T5, T9
58 PolyJet, Connex 500 Objet,
Non-soluble acrylate
Fit and lock on lamina Post-op evaluation using CT scans. No cases
of cortex violation.
0.87 6 0.34 mm mean deviation from the
planned trajectory at the coronal midpoint
section of the pedicles.
Disadvantage: no use in emergency cases as:
1–2 days are required for the design, and
1 day is required for printing.
‘Simple and economicalmethod can improve
the accuracy of pedicle screw insertion and
reduce the operating time and radiation
exposure of spinalfixation surgery’
Kaneyama et al.9 Clinical
three patients
Single
three types
of guides
Cervical
C2–C6
– PolyJet, Connex 500,
non-soluble acrylate
Negative vertebral
posterior surface of the
3D shape of the lamina
Evaluation using CT scans for assessing the
implant screw deviation from the planned
trajectory.
Disadvantage: precise soft tissues for a
proper guide engagement on the bone
Li et al.61 Cadaver Single
3 guides
Cervical
C1–C2
18 SL,acrylate resin Negative of the C1 and
C2 anterior surfaces
Post-op CT images for evaluating the inserted
screws deviation from the planned screw
trajectories.
13 screws were rated as optimal placed and 2
screws as acceptable.
‘It is feasible to use individualised templates
to guide transoral C2 screw placement’
although the sample size was small.
Disadvantage: complicate design process for
the guides
(continued)Popescu and Laptoiu 503
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Fu et al.55 Cadaver Single Cervical
C2–C7
48 3DP,Z510 spectrum Negative of the cervical
vertebra body surface
Evaluation using CT scans, reconstructing the
3D model with screws and comparing with
the reconstructed 3D model without screws.
Deviation in axial plane:0.826 6 0.75 mm,
deviation in sagittal plane: 1.106 6 0.96 mm.
91.7% of screws were inserted in non-critical
positions.
RP-PSGs ‘easy-to-apply and accurate’
Owen et al.40 Cadaver Single Cervical
C5
2 FDM,ABS Match the posterior
surface of the right side
of the fifth cervical
vertebra
Evaluation using CT scans and visual
inspection.Guides used for inserting K-wire
first and then 3.5 mm screws.
Cost estimation for each drill guide: US$30–
50.
‘The feasibility of this patient-specific rapid
prototyping technique was demonstrated’.
However, authors consider that confirmation
in additionalresearch is needed
Sugawara et al.57 Clinical
10 patients
Single
In 3 steps
Thoracic
Cervicothoracic,
T1,T5, T9
58 PolyJet, Connex 500 Objet,
Non-soluble acrylate
Fit and lock on lamina Post-op evaluation using CT scans. No cases
of cortex violation.
0.87 6 0.34 mm mean deviation from the
planned trajectory at the coronal midpoint
section of the pedicles.
Disadvantage: no use in emergency cases as:
1–2 days are required for the design, and
1 day is required for printing.
‘Simple and economicalmethod can improve
the accuracy of pedicle screw insertion and
reduce the operating time and radiation
exposure of spinalfixation surgery’
Kaneyama et al.9 Clinical
three patients
Single
three types
of guides
Cervical
C2–C6
– PolyJet, Connex 500,
non-soluble acrylate
Negative vertebral
posterior surface of the
3D shape of the lamina
Evaluation using CT scans for assessing the
implant screw deviation from the planned
trajectory.
Disadvantage: precise soft tissues for a
proper guide engagement on the bone
Li et al.61 Cadaver Single
3 guides
Cervical
C1–C2
18 SL,acrylate resin Negative of the C1 and
C2 anterior surfaces
Post-op CT images for evaluating the inserted
screws deviation from the planned screw
trajectories.
13 screws were rated as optimal placed and 2
screws as acceptable.
‘It is feasible to use individualised templates
to guide transoral C2 screw placement’
although the sample size was small.
Disadvantage: complicate design process for
the guides
(continued)Popescu and Laptoiu 503
at University College London on May 27, 2016pih.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
This can also be seen from an examination of the
data collected for our systematic literature review. The
annualdistribution (2005–2014)of studies presenting
RP-PGS employed to improve the accuracy of ortho-
paedic surgicalapplications,such as screwsinserted
into human vertebrae or guides for incision trajectories
in various types ofosteotomies,should be discussed
and interpreted taking into accounta timeframe of
around 1 year for publication of the research in journals
or books, and, in clinical trials, a timeframe of around
2–3 years for selection ofpatients,planning and per-
forming interventions, and evaluation of post-operative
results. Although a growing trend can be observed since
2009 (Figure 2),the studies under review were most
likely carried outstarting from 2006 to 2007.For
instance,Stockmans24 remarks that his team has been
using patient-specific instrumentation since 2007,with
5–10 cases a year. In other words, no direct correlation
can be found between the expiration of the FDM pat-
ent (despite its importance and generalimpact on the
field, as discussed above) and the increase in RP-PSGs
use.
It should also be mentioned thatsince 2011 more
than eightstudies have been published yearly in the
field of RP applications,which is very similar to in
2009 (nine studies). However, in 2010, there was a drop
to two studies a year, as shown in Figure 2. After read-
ing in full the papers published before 2010 (given in
‘List 1’), we could not find any reason (e.g. researchers’
opinions, conclusions or failed experiments) that might
have had a negativeinfluenceon the research and
thereby explain this decrease.
The systematic literature search and review carried
out for this article showed that most RP-PSGs are man-
ufactured for spinal surgery applications (Figure 3 and
Table 1), to increase accuracy when guiding the screws’
insertion trajectories,especially in cervicalarea – 13
studies.
In conclusion, the answer to Q1 (Is there a significant
constantincrease in the use ofRP-PSGs?) is that the
analysed data do not allow us to conclude that there
has been any constant increase. A year-by-year increase
in the trend cannot be observed prior to 2011, as can be
seen in Figure 2.However,more than 83% of allthe
studieswere published in journalsand bookssubse-
quent to 2009.
In all papers under review, the following advantages
of RP-PSGs are emphasised:
The use of computer-assisted navigation systems or
robotic-assisted platforms/systemsas solutionsto
reduce intervention errors in orthopaedic surgery
determineshighercoststhan those fordesigning
individualised surgicaltemplates and manufactur-
ing them using the RP process.
RP currently representsthe best and the most
straightforward manufacturing solution forpro-
ducing prototypes with highly complex geometries,
as required in the medical field, using materials that
Table 2. Continued
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Wu et al.49 Clinical
34 patients
Single Thoracic lumbar 677 SL,acrylate resin Negative of vertebral
surfaces
Comparison using post-op CT scans between
RP-PSG technique (34 patients) and
conventional fluoroscopy (28 patients).
C-arm group placement accuracy: 86.1%
thoracic spine and 82.0% lumbar spine.
RP-PSGs group placement accuracy: 94.4%
thoracic spine and 91.6% lumbar spine.
Reported advantages:‘shorter operation time
and higher scoliosis correction rate’
Ferrari et al.56 Synthetic spine/
animal tests
Single Thoracic lumbar 28 SL,acrylate resin Quadpod configuration
design, with a fitting area
on the spinous process
for alignment
CT scans post-op evaluation and visual
inspection.
1 screw violated the cortex (3.5%), 25 screws
had less than 1 mm deviation (89.3%), 2
screws had 1–2 mm deviation (7.2%).
Advantages: ‘promising, simple,highly precise,
low-cost solution’.
The guides cost is evaluated ‘at few hundred
euro’
RP-PSGs: rapid prototyping patient-specific surgical guides, SL: stereolithography, 3D: three-dimensional, CT:computed tomography,SLS: selective laser sintering, FDM: fused deposition modelling, ABS:acrylonitrile
butadiene styrene.
504 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
data collected for our systematic literature review. The
annualdistribution (2005–2014)of studies presenting
RP-PGS employed to improve the accuracy of ortho-
paedic surgicalapplications,such as screwsinserted
into human vertebrae or guides for incision trajectories
in various types ofosteotomies,should be discussed
and interpreted taking into accounta timeframe of
around 1 year for publication of the research in journals
or books, and, in clinical trials, a timeframe of around
2–3 years for selection ofpatients,planning and per-
forming interventions, and evaluation of post-operative
results. Although a growing trend can be observed since
2009 (Figure 2),the studies under review were most
likely carried outstarting from 2006 to 2007.For
instance,Stockmans24 remarks that his team has been
using patient-specific instrumentation since 2007,with
5–10 cases a year. In other words, no direct correlation
can be found between the expiration of the FDM pat-
ent (despite its importance and generalimpact on the
field, as discussed above) and the increase in RP-PSGs
use.
It should also be mentioned thatsince 2011 more
than eightstudies have been published yearly in the
field of RP applications,which is very similar to in
2009 (nine studies). However, in 2010, there was a drop
to two studies a year, as shown in Figure 2. After read-
ing in full the papers published before 2010 (given in
‘List 1’), we could not find any reason (e.g. researchers’
opinions, conclusions or failed experiments) that might
have had a negativeinfluenceon the research and
thereby explain this decrease.
The systematic literature search and review carried
out for this article showed that most RP-PSGs are man-
ufactured for spinal surgery applications (Figure 3 and
Table 1), to increase accuracy when guiding the screws’
insertion trajectories,especially in cervicalarea – 13
studies.
In conclusion, the answer to Q1 (Is there a significant
constantincrease in the use ofRP-PSGs?) is that the
analysed data do not allow us to conclude that there
has been any constant increase. A year-by-year increase
in the trend cannot be observed prior to 2011, as can be
seen in Figure 2.However,more than 83% of allthe
studieswere published in journalsand bookssubse-
quent to 2009.
In all papers under review, the following advantages
of RP-PSGs are emphasised:
The use of computer-assisted navigation systems or
robotic-assisted platforms/systemsas solutionsto
reduce intervention errors in orthopaedic surgery
determineshighercoststhan those fordesigning
individualised surgicaltemplates and manufactur-
ing them using the RP process.
RP currently representsthe best and the most
straightforward manufacturing solution forpro-
ducing prototypes with highly complex geometries,
as required in the medical field, using materials that
Table 2. Continued
Study Cadaver/
clinical
Single/
multi-level
Spine zone No. of
screws
RP process PSG design approach Results
Wu et al.49 Clinical
34 patients
Single Thoracic lumbar 677 SL,acrylate resin Negative of vertebral
surfaces
Comparison using post-op CT scans between
RP-PSG technique (34 patients) and
conventional fluoroscopy (28 patients).
C-arm group placement accuracy: 86.1%
thoracic spine and 82.0% lumbar spine.
RP-PSGs group placement accuracy: 94.4%
thoracic spine and 91.6% lumbar spine.
Reported advantages:‘shorter operation time
and higher scoliosis correction rate’
Ferrari et al.56 Synthetic spine/
animal tests
Single Thoracic lumbar 28 SL,acrylate resin Quadpod configuration
design, with a fitting area
on the spinous process
for alignment
CT scans post-op evaluation and visual
inspection.
1 screw violated the cortex (3.5%), 25 screws
had less than 1 mm deviation (89.3%), 2
screws had 1–2 mm deviation (7.2%).
Advantages: ‘promising, simple,highly precise,
low-cost solution’.
The guides cost is evaluated ‘at few hundred
euro’
RP-PSGs: rapid prototyping patient-specific surgical guides, SL: stereolithography, 3D: three-dimensional, CT:computed tomography,SLS: selective laser sintering, FDM: fused deposition modelling, ABS:acrylonitrile
butadiene styrene.
504 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
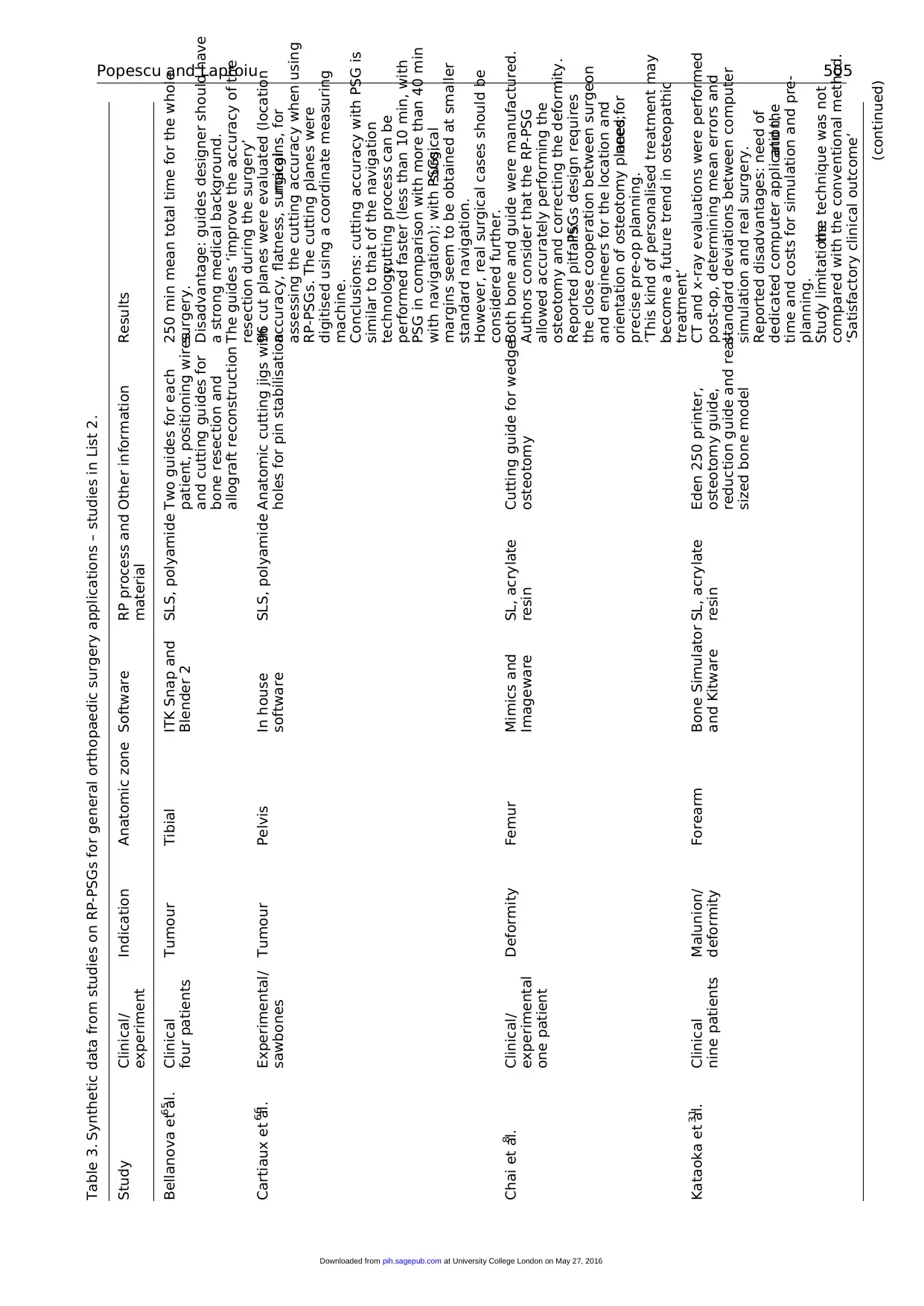
Table 3. Synthetic data from studies on RP-PSGs for general orthopaedic surgery applications – studies in List 2.
Study Clinical/
experiment
Indication Anatomic zone Software RP process and
material
Other information Results
Bellanova et al.65 Clinical
four patients
Tumour Tibial ITK Snap and
Blender 2
SLS, polyamide Two guides for each
patient, positioning wires
and cutting guides for
bone resection and
allograft reconstruction
250 min mean total time for the whole
surgery.
Disadvantage: guides designer should have
a strong medical background.
The guides ‘improve the accuracy of the
resection during the surgery’
Cartiaux et al.66 Experimental/
sawbones
Tumour Pelvis In house
software
SLS, polyamide Anatomic cutting jigs with
holes for pin stabilisation
96 cut planes were evaluated (location
accuracy, flatness, surgicalmargins, for
assessing the cutting accuracy when using
RP-PSGs. The cutting planes were
digitised using a coordinate measuring
machine.
Conclusions: cutting accuracy with PSG is
similar to that of the navigation
technology;cutting process can be
performed faster (less than 10 min, with
PSG in comparison with more than 40 min
with navigation); with PSGs,surgical
margins seem to be obtained at smaller
standard navigation.
However, real surgical cases should be
considered further.
Chai et al.8 Clinical/
experimental
one patient
Deformity Femur Mimics and
Imageware
SL, acrylate
resin
Cutting guide for wedge
osteotomy
Both bone and guide were manufactured.
Authors consider that the RP-PSG
allowed accurately performing the
osteotomy and correcting the deformity.
Reported pitfalls:PSGs design requires
the close cooperation between surgeon
and engineers for the location and
orientation of osteotomy planes;need for
precise pre-op planning.
‘This kind of personalised treatment may
become a future trend in osteopathic
treatment’
Kataoka et al.31 Clinical
nine patients
Malunion/
deformity
Forearm Bone Simulator
and Kitware
SL, acrylate
resin
Eden 250 printer,
osteotomy guide,
reduction guide and real-
sized bone model
CT and x-ray evaluations were performed
post-op, determining mean errors and
standard deviations between computer
simulation and real surgery.
Reported disadvantages: need of
dedicated computer application,and the
time and costs for simulation and pre-
planning.
Study limitations:the technique was not
compared with the conventional method.
‘Satisfactory clinical outcome’
(continued)Popescu and Laptoiu 505
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Clinical/
experiment
Indication Anatomic zone Software RP process and
material
Other information Results
Bellanova et al.65 Clinical
four patients
Tumour Tibial ITK Snap and
Blender 2
SLS, polyamide Two guides for each
patient, positioning wires
and cutting guides for
bone resection and
allograft reconstruction
250 min mean total time for the whole
surgery.
Disadvantage: guides designer should have
a strong medical background.
The guides ‘improve the accuracy of the
resection during the surgery’
Cartiaux et al.66 Experimental/
sawbones
Tumour Pelvis In house
software
SLS, polyamide Anatomic cutting jigs with
holes for pin stabilisation
96 cut planes were evaluated (location
accuracy, flatness, surgicalmargins, for
assessing the cutting accuracy when using
RP-PSGs. The cutting planes were
digitised using a coordinate measuring
machine.
Conclusions: cutting accuracy with PSG is
similar to that of the navigation
technology;cutting process can be
performed faster (less than 10 min, with
PSG in comparison with more than 40 min
with navigation); with PSGs,surgical
margins seem to be obtained at smaller
standard navigation.
However, real surgical cases should be
considered further.
Chai et al.8 Clinical/
experimental
one patient
Deformity Femur Mimics and
Imageware
SL, acrylate
resin
Cutting guide for wedge
osteotomy
Both bone and guide were manufactured.
Authors consider that the RP-PSG
allowed accurately performing the
osteotomy and correcting the deformity.
Reported pitfalls:PSGs design requires
the close cooperation between surgeon
and engineers for the location and
orientation of osteotomy planes;need for
precise pre-op planning.
‘This kind of personalised treatment may
become a future trend in osteopathic
treatment’
Kataoka et al.31 Clinical
nine patients
Malunion/
deformity
Forearm Bone Simulator
and Kitware
SL, acrylate
resin
Eden 250 printer,
osteotomy guide,
reduction guide and real-
sized bone model
CT and x-ray evaluations were performed
post-op, determining mean errors and
standard deviations between computer
simulation and real surgery.
Reported disadvantages: need of
dedicated computer application,and the
time and costs for simulation and pre-
planning.
Study limitations:the technique was not
compared with the conventional method.
‘Satisfactory clinical outcome’
(continued)Popescu and Laptoiu 505
at University College London on May 27, 2016pih.sagepub.comDownloaded from
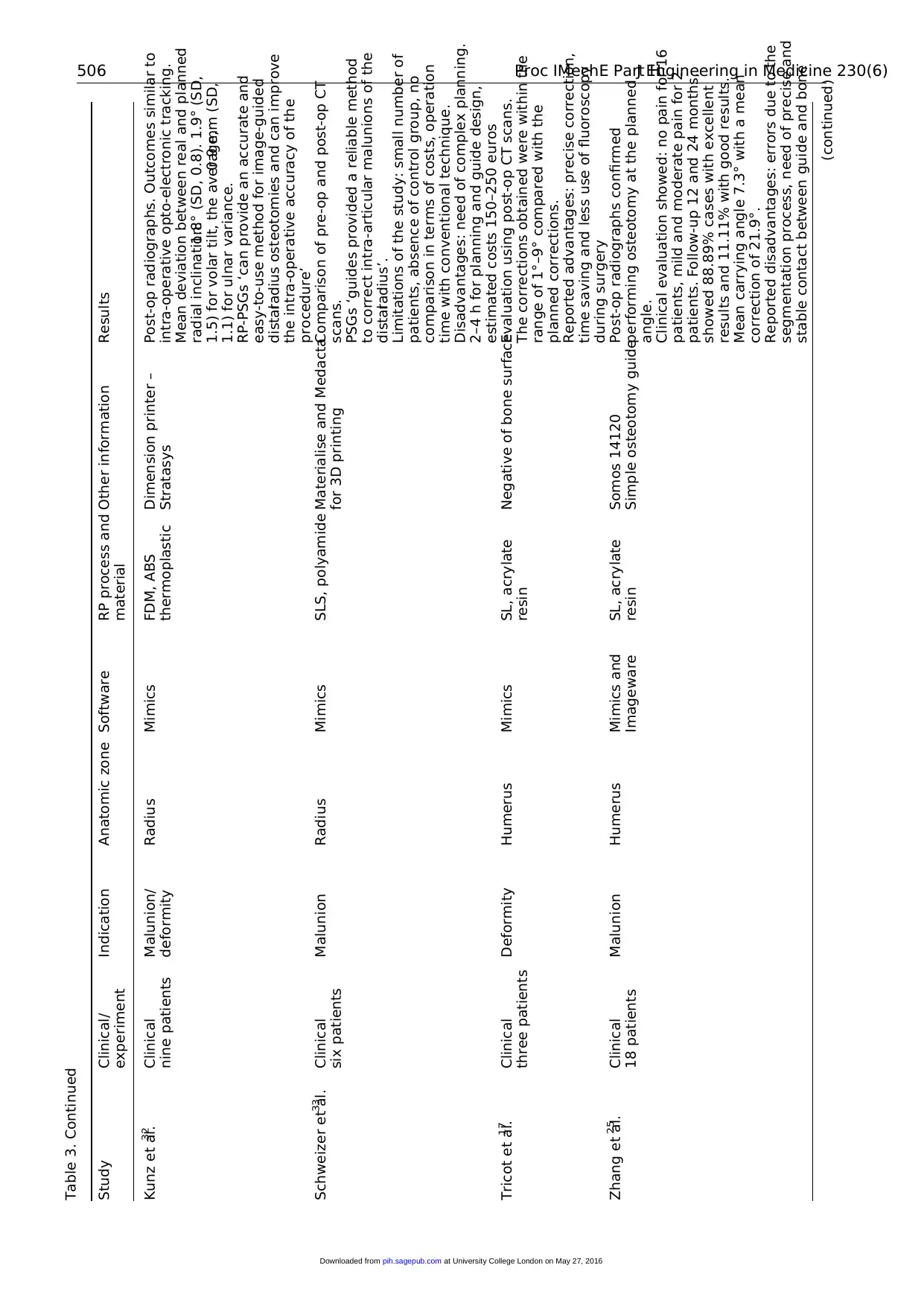
Table 3. Continued
Study Clinical/
experiment
Indication Anatomic zone Software RP process and
material
Other information Results
Kunz et al.32 Clinical
nine patients
Malunion/
deformity
Radius Mimics FDM, ABS
thermoplastic
Dimension printer –
Stratasys
Post-op radiographs. Outcomes similar to
intra-operative opto-electronic tracking.
Mean deviation between real and planned
radial inclination:1.8° (SD, 0.8). 1.9° (SD,
1.5) for volar tilt, the average,0.9 mm (SD,
1.1) for ulnar variance.
RP-PSGs ‘can provide an accurate and
easy-to-use method for image-guided
distalradius osteotomies and can improve
the intra-operative accuracy of the
procedure’
Schweizer et al.33 Clinical
six patients
Malunion Radius Mimics SLS, polyamide Materialise and Medacta
for 3D printing
Comparison of pre-op and post-op CT
scans.
PSGs ‘guides provided a reliable method
to correct intra-articular malunions of the
distalradius’.
Limitations of the study: small number of
patients, absence of control group, no
comparison in terms of costs, operation
time with conventional technique.
Disadvantages: need of complex planning.
2–4 h for planning and guide design,
estimated costs 150–250 euros
Tricot et al.17 Clinical
three patients
Deformity Humerus Mimics SL, acrylate
resin
Negative of bone surfaceEvaluation using post-op CT scans.
The corrections obtained were within the
range of 1°–9° compared with the
planned corrections.
Reported advantages: precise correction,
time saving and less use of fluoroscopy
during surgery
Zhang et al.25 Clinical
18 patients
Malunion Humerus Mimics and
Imageware
SL, acrylate
resin
Somos 14120
Simple osteotomy guide
Post-op radiographs confirmed
performing osteotomy at the planned
angle.
Clinical evaluation showed: no pain for 16
patients, mild and moderate pain for 2
patients. Follow-up 12 and 24 months,
showed 88.89% cases with excellent
results and 11.11% with good results.
Mean carrying angle 7.3° with a mean
correction of 21.9°.
Reported disadvantages: errors due to the
segmentation process, need of precise and
stable contact between guide and bone
(continued)506 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
Study Clinical/
experiment
Indication Anatomic zone Software RP process and
material
Other information Results
Kunz et al.32 Clinical
nine patients
Malunion/
deformity
Radius Mimics FDM, ABS
thermoplastic
Dimension printer –
Stratasys
Post-op radiographs. Outcomes similar to
intra-operative opto-electronic tracking.
Mean deviation between real and planned
radial inclination:1.8° (SD, 0.8). 1.9° (SD,
1.5) for volar tilt, the average,0.9 mm (SD,
1.1) for ulnar variance.
RP-PSGs ‘can provide an accurate and
easy-to-use method for image-guided
distalradius osteotomies and can improve
the intra-operative accuracy of the
procedure’
Schweizer et al.33 Clinical
six patients
Malunion Radius Mimics SLS, polyamide Materialise and Medacta
for 3D printing
Comparison of pre-op and post-op CT
scans.
PSGs ‘guides provided a reliable method
to correct intra-articular malunions of the
distalradius’.
Limitations of the study: small number of
patients, absence of control group, no
comparison in terms of costs, operation
time with conventional technique.
Disadvantages: need of complex planning.
2–4 h for planning and guide design,
estimated costs 150–250 euros
Tricot et al.17 Clinical
three patients
Deformity Humerus Mimics SL, acrylate
resin
Negative of bone surfaceEvaluation using post-op CT scans.
The corrections obtained were within the
range of 1°–9° compared with the
planned corrections.
Reported advantages: precise correction,
time saving and less use of fluoroscopy
during surgery
Zhang et al.25 Clinical
18 patients
Malunion Humerus Mimics and
Imageware
SL, acrylate
resin
Somos 14120
Simple osteotomy guide
Post-op radiographs confirmed
performing osteotomy at the planned
angle.
Clinical evaluation showed: no pain for 16
patients, mild and moderate pain for 2
patients. Follow-up 12 and 24 months,
showed 88.89% cases with excellent
results and 11.11% with good results.
Mean carrying angle 7.3° with a mean
correction of 21.9°.
Reported disadvantages: errors due to the
segmentation process, need of precise and
stable contact between guide and bone
(continued)506 Proc IMechE Part H:J Engineering in Medicine 230(6)
at University College London on May 27, 2016pih.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





