Essay on Peptic Ulcer Disease: A Comprehensive Overview
VerifiedAdded on 2022/09/15
|11
|2453
|17
Essay
AI Summary
This essay provides a comprehensive overview of peptic ulcer disease, also known as gastric ulcer. It begins with an introduction to the disease, its prevalence, and the factors that contribute to its development, including aggressive and protective factors within the stomach. The essay delves into the pathogenesis of peptic ulcers, exploring the role of acid secretion, reactive oxygen species, bacteria like Helicobacter pylori (H. pylori), and the use of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). It discusses the gastric protective factors, the impact of H. pylori, and the mechanisms by which NSAIDs damage the gastroduodenal mucosa. The essay further examines the symptoms, complications, and treatment options, including medical therapies like PPIs and antibiotics, lifestyle choices, and surgical interventions. Finally, it highlights the significance of factors such as smoking, stress, alcohol use, and genetic predisposition in the development of peptic ulcer disease, providing a well-rounded understanding of the condition.

Running head: ULCER INFECTION 1
Peptic Ulcer Disease
Student:
Professor:
Institution Affiliation:
Date:
Peptic Ulcer Disease
Student:
Professor:
Institution Affiliation:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ULCER INFECTION 2
Introduction
The stomach ulcer is also known as the gastric ulcer. The infection affects the normal
functioning of the muscularis mucosa, gastric mucosa, and the inner submucosa. The ulcers
occur along the digestive tract, such as the esophagus, duodenum, jejunum, and at the margin of
the gastroenterostomy. The infection can cause complications such as hemorrhages,
gastrointestinal blockage, perforations, and malignancy. The disease is a health problem
worldwide with high mortality and morbidity and differs with age, gender, and geographic
environment. The mucosa of the stomach controls the balancing between the aggressive and
protective factors. The hostile elements include; pepsin, alcohol usage, anomalous motility,
nonsteroidal anti-inflammatory drugs (NSAID), gastric acid, bile salts, and infections related to
helicobacter pylori (H. Pylori) and other microorganisms. The protecting factors include
secretion of mucus, production of gastro-protective prostaglandin, normal tissue
microcirculation, and bicarbonate production. This essay will discuss the pathogenesis, causes,
symptoms, treatment functions of the protective factors.
Gastric Defensive Factors
The stomach is lining is composed of intricate epithelium that creates a discriminatory
barrier between the lumen and the body. The epithelium consists of pre-epithelial mucus-
bicarbonate, Subepithelial, components). It folds into several tube-like intestinal glands with
several branching that extends to muscularis mucosa. The gastric epithelial performs its diverse
functions in an aggressive luminal environment that can accommodate around 150 mm of HCL
and other aggressive proteases. These aggressive proteases have the ability to digest a variety of
toxic pathogens and stomach tissue itself. Many defensive mechanisms under normal conditions
prevent local destruction of the mucosal integrity from maintaining its structural functions
Introduction
The stomach ulcer is also known as the gastric ulcer. The infection affects the normal
functioning of the muscularis mucosa, gastric mucosa, and the inner submucosa. The ulcers
occur along the digestive tract, such as the esophagus, duodenum, jejunum, and at the margin of
the gastroenterostomy. The infection can cause complications such as hemorrhages,
gastrointestinal blockage, perforations, and malignancy. The disease is a health problem
worldwide with high mortality and morbidity and differs with age, gender, and geographic
environment. The mucosa of the stomach controls the balancing between the aggressive and
protective factors. The hostile elements include; pepsin, alcohol usage, anomalous motility,
nonsteroidal anti-inflammatory drugs (NSAID), gastric acid, bile salts, and infections related to
helicobacter pylori (H. Pylori) and other microorganisms. The protecting factors include
secretion of mucus, production of gastro-protective prostaglandin, normal tissue
microcirculation, and bicarbonate production. This essay will discuss the pathogenesis, causes,
symptoms, treatment functions of the protective factors.
Gastric Defensive Factors
The stomach is lining is composed of intricate epithelium that creates a discriminatory
barrier between the lumen and the body. The epithelium consists of pre-epithelial mucus-
bicarbonate, Subepithelial, components). It folds into several tube-like intestinal glands with
several branching that extends to muscularis mucosa. The gastric epithelial performs its diverse
functions in an aggressive luminal environment that can accommodate around 150 mm of HCL
and other aggressive proteases. These aggressive proteases have the ability to digest a variety of
toxic pathogens and stomach tissue itself. Many defensive mechanisms under normal conditions
prevent local destruction of the mucosal integrity from maintaining its structural functions
ULCER INFECTION 3
despite exposure to the injurious factors. The gastric protective mechanism has a stomach
mucosal obstruction, which is a multilayered system that consists of a pre-epithelia mucus
barrier, the epithelial barrier which connects to tight junctions and sub-epithelial components that
compose nerves and the blood flow (Chai, 2011).
Peptic Ulcer Pathology
Erosions are superficial mucosal defects. The erosion defects in the ulcers outspread
through the musularis mucosa, up to the muscularis propria. Acute lesions are caused by aspirin
injury. They are many and shallow, occurring with minimal surrounding fibrosis or
inflammation, thus heal very fast. On the other hand, chronic ulcers occur singly, surrounded by
inflammation and fibrosis.
Causes and Pathophysiology
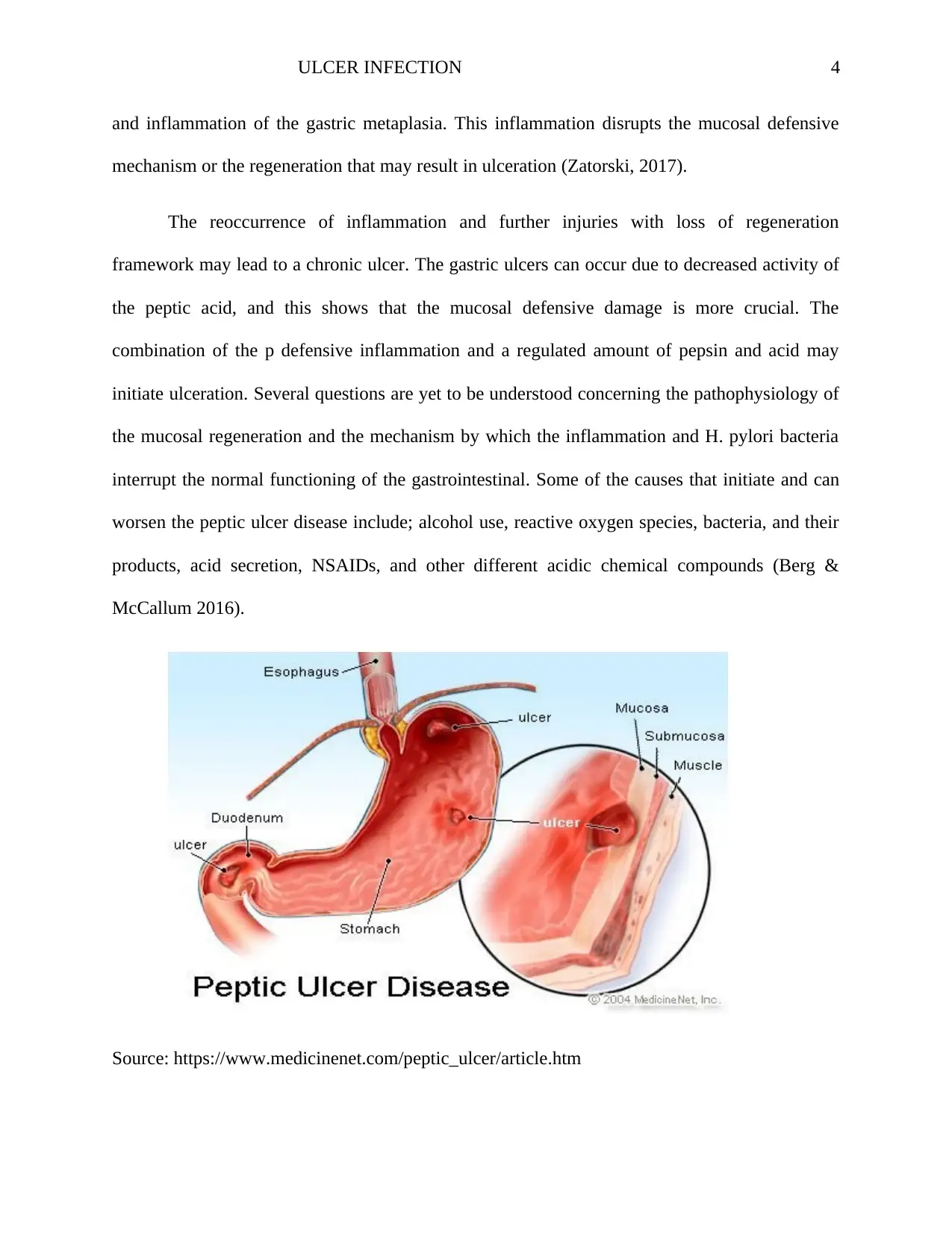
Acid secretion, reactive oxygen species, bacteria, NSAID, and other aggressive factors
impair the mucosal defense, thus altering the epithelial barrier, and this leads to the formation of
mucosal injury. The impacts of the gastric obstruction show the pathogenesis mechanism of
gastric ulcers, gastric disease, and long-lasting gastritis. These mechanisms are generated by the
imbalance between the defensive and the aggressive factors. Recent studies have shown that
familial and genetic factors in the duodenal ulcer and the increase of acid-pepsin secretion is due
to a response to several stimuli. The duodenal ulcer is characterized by duodenitis and H. pylori
contagion, and in several incidences, the secretion of compromised duodenal bicarbonate in the
face of controlled acid and peptic activity. These facts show that increased peptic activity is
accompanied by the reduced duodenal buffering capability that leads to increased mucosal injury
and may result in gastric metaplasia. The presence of antral H. pylori can lead to colonization
despite exposure to the injurious factors. The gastric protective mechanism has a stomach
mucosal obstruction, which is a multilayered system that consists of a pre-epithelia mucus
barrier, the epithelial barrier which connects to tight junctions and sub-epithelial components that
compose nerves and the blood flow (Chai, 2011).
Peptic Ulcer Pathology
Erosions are superficial mucosal defects. The erosion defects in the ulcers outspread
through the musularis mucosa, up to the muscularis propria. Acute lesions are caused by aspirin
injury. They are many and shallow, occurring with minimal surrounding fibrosis or
inflammation, thus heal very fast. On the other hand, chronic ulcers occur singly, surrounded by
inflammation and fibrosis.
Causes and Pathophysiology
Acid secretion, reactive oxygen species, bacteria, NSAID, and other aggressive factors
impair the mucosal defense, thus altering the epithelial barrier, and this leads to the formation of
mucosal injury. The impacts of the gastric obstruction show the pathogenesis mechanism of
gastric ulcers, gastric disease, and long-lasting gastritis. These mechanisms are generated by the
imbalance between the defensive and the aggressive factors. Recent studies have shown that
familial and genetic factors in the duodenal ulcer and the increase of acid-pepsin secretion is due
to a response to several stimuli. The duodenal ulcer is characterized by duodenitis and H. pylori
contagion, and in several incidences, the secretion of compromised duodenal bicarbonate in the
face of controlled acid and peptic activity. These facts show that increased peptic activity is
accompanied by the reduced duodenal buffering capability that leads to increased mucosal injury
and may result in gastric metaplasia. The presence of antral H. pylori can lead to colonization
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ULCER INFECTION 4
and inflammation of the gastric metaplasia. This inflammation disrupts the mucosal defensive
mechanism or the regeneration that may result in ulceration (Zatorski, 2017).
The reoccurrence of inflammation and further injuries with loss of regeneration
framework may lead to a chronic ulcer. The gastric ulcers can occur due to decreased activity of
the peptic acid, and this shows that the mucosal defensive damage is more crucial. The
combination of the p defensive inflammation and a regulated amount of pepsin and acid may
initiate ulceration. Several questions are yet to be understood concerning the pathophysiology of
the mucosal regeneration and the mechanism by which the inflammation and H. pylori bacteria
interrupt the normal functioning of the gastrointestinal. Some of the causes that initiate and can
worsen the peptic ulcer disease include; alcohol use, reactive oxygen species, bacteria, and their
products, acid secretion, NSAIDs, and other different acidic chemical compounds (Berg &
McCallum 2016).
Source: https://www.medicinenet.com/peptic_ulcer/article.htm
and inflammation of the gastric metaplasia. This inflammation disrupts the mucosal defensive
mechanism or the regeneration that may result in ulceration (Zatorski, 2017).
The reoccurrence of inflammation and further injuries with loss of regeneration
framework may lead to a chronic ulcer. The gastric ulcers can occur due to decreased activity of
the peptic acid, and this shows that the mucosal defensive damage is more crucial. The
combination of the p defensive inflammation and a regulated amount of pepsin and acid may
initiate ulceration. Several questions are yet to be understood concerning the pathophysiology of
the mucosal regeneration and the mechanism by which the inflammation and H. pylori bacteria
interrupt the normal functioning of the gastrointestinal. Some of the causes that initiate and can
worsen the peptic ulcer disease include; alcohol use, reactive oxygen species, bacteria, and their
products, acid secretion, NSAIDs, and other different acidic chemical compounds (Berg &
McCallum 2016).
Source: https://www.medicinenet.com/peptic_ulcer/article.htm
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ULCER INFECTION 5
Helicobacter pylori (H. pylori)
Helicobacter pylori have been a common public health concern related to the
pathogenesis of peptic and gastric ulcers. The incidence of the bacteria is around 90% of the
developing ulcer cases in the populations. It is the second most prevalent human pathogen
associated with the public health problem. H. pylori is a gram-negative bacteria and a significant
contributing aspect in the pathogenesis of peptic ulcers and gastritis. It sometimes attaches itself
to the superficial epithelial cells with no significant invasion of the host tissue. The bacteria
induce severe gastritis in the infected subjects, which contribute to around 10to 15 % of the
peptic ulcer progression. H. pylori catalyze the hydrolysis of urea, leading to the formation of
ammonium (NH3), which counterbalances the gastric acid and defends itself from the aggressive
acids in the stomach. The bacteria enter the mucosa layer of the stomach, stabilize in the
superficial of the epithelial cells, and finally proliferate to form the center of the infection. The
gastric lesions occur due to the destruction of the mucosa that causes the inflammation and death
of the mucosal cell (Alpers & Yamada, 2009).
Nonsteroidal Anti-Inflammatory Drugs
The mechanism by which the NSAIDs damages the gastroduodenal mucosa is by the
systemic hindrance of constitutively articulated cyclooxygenase-1 (COX-1), which is involved in
prostaglandin production. It decreases the blood flow in the mucosal, secretion of mucus and
bicarbonate and inhibits proliferation of the cell. The NSAIDs prevent the enzyme reversibility
in a concentration-dependent way such that the use of co-administration of cyclooxygenase- 2
(COX- 2)- selective NSAIDs and exogenous prostaglandins to reduce the risk of ulcers and
Helicobacter pylori (H. pylori)
Helicobacter pylori have been a common public health concern related to the
pathogenesis of peptic and gastric ulcers. The incidence of the bacteria is around 90% of the
developing ulcer cases in the populations. It is the second most prevalent human pathogen
associated with the public health problem. H. pylori is a gram-negative bacteria and a significant
contributing aspect in the pathogenesis of peptic ulcers and gastritis. It sometimes attaches itself
to the superficial epithelial cells with no significant invasion of the host tissue. The bacteria
induce severe gastritis in the infected subjects, which contribute to around 10to 15 % of the
peptic ulcer progression. H. pylori catalyze the hydrolysis of urea, leading to the formation of
ammonium (NH3), which counterbalances the gastric acid and defends itself from the aggressive
acids in the stomach. The bacteria enter the mucosa layer of the stomach, stabilize in the
superficial of the epithelial cells, and finally proliferate to form the center of the infection. The
gastric lesions occur due to the destruction of the mucosa that causes the inflammation and death
of the mucosal cell (Alpers & Yamada, 2009).
Nonsteroidal Anti-Inflammatory Drugs
The mechanism by which the NSAIDs damages the gastroduodenal mucosa is by the
systemic hindrance of constitutively articulated cyclooxygenase-1 (COX-1), which is involved in
prostaglandin production. It decreases the blood flow in the mucosal, secretion of mucus and
bicarbonate and inhibits proliferation of the cell. The NSAIDs prevent the enzyme reversibility
in a concentration-dependent way such that the use of co-administration of cyclooxygenase- 2
(COX- 2)- selective NSAIDs and exogenous prostaglandins to reduce the risk of ulcers and
ULCER INFECTION 6
mucosal damage. The different physicochemical properties of the NSAIDs brings about
dissimilarities in their harmfulness. The NSAIDs interfere with the phospholipids leading to the
mitochondrial oxidative phosphorylation, thus mucosal destruction. The NSAIDs become
protonate when exposed to gastric acidic juice, thus crossing the lipid membrane and induce the
epithelial cells. Most of the patients who present a history of peptic ulcer disease are over 65
years. They use anticoagulants or steroids at high dosage disposing to them to high risk of
NSAID- induced ulcers.
High secretion of gastric acid
This occurs in non-NSAID and non-Hp Duodenal ulcer. The gastric acid is mostly
secreted in non- NSAIDs Duodenal ulcer and in non- Hp. The mechanism of hypersecretion of
the acid has not yet been established, while vagal cholinergic mechanisms are among the
probable that require intense study hypersecretory duodenal ulcer patients. After the NSAIDs,
Hp and gastrinoma have been excluded, and the PPI remains the only management model.
Smoking
The literature has revealed that there is a strong relationship between cigarette smoking
and the incidence rate of peptic ulcer disease. Cigarette smoking is also associated with
mortality, recurrences, stomach complications, and delay in ulcer healing. People who smoke are
two times more likely to have peptic ulcer disease than those who do not smoke. H. pylori and
cigarette smoking are the major contributors of the peptic ulcer disease. The relationship between
H. pylori infection and cigarette smoking is that smoking can increase susceptibility, weaken the
mucosal protective factors, and can provide a favorable environment for the H. pylori infection.
Stress
mucosal damage. The different physicochemical properties of the NSAIDs brings about
dissimilarities in their harmfulness. The NSAIDs interfere with the phospholipids leading to the
mitochondrial oxidative phosphorylation, thus mucosal destruction. The NSAIDs become
protonate when exposed to gastric acidic juice, thus crossing the lipid membrane and induce the
epithelial cells. Most of the patients who present a history of peptic ulcer disease are over 65
years. They use anticoagulants or steroids at high dosage disposing to them to high risk of
NSAID- induced ulcers.
High secretion of gastric acid
This occurs in non-NSAID and non-Hp Duodenal ulcer. The gastric acid is mostly
secreted in non- NSAIDs Duodenal ulcer and in non- Hp. The mechanism of hypersecretion of
the acid has not yet been established, while vagal cholinergic mechanisms are among the
probable that require intense study hypersecretory duodenal ulcer patients. After the NSAIDs,
Hp and gastrinoma have been excluded, and the PPI remains the only management model.
Smoking
The literature has revealed that there is a strong relationship between cigarette smoking
and the incidence rate of peptic ulcer disease. Cigarette smoking is also associated with
mortality, recurrences, stomach complications, and delay in ulcer healing. People who smoke are
two times more likely to have peptic ulcer disease than those who do not smoke. H. pylori and
cigarette smoking are the major contributors of the peptic ulcer disease. The relationship between
H. pylori infection and cigarette smoking is that smoking can increase susceptibility, weaken the
mucosal protective factors, and can provide a favorable environment for the H. pylori infection.
Stress
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ULCER INFECTION 7
Many studies have demonstrated how psychological distress have influenced the natural
history and pathogenesis of peptic ulcer disease. The conclusions about the contributing factor of
the psychological factors towards the cause of peptic ulcer disease are far from being established.
There is no concluded “ulcer–type” personality. Acute stress increases the pulse rate, anxiety,
and blood pressure of the patients with duodenal ulcers leading to a significant increase in the
basal acid secretion. Typically, ulcer patient shows the same psychological makeup as in other
people, but they appear to have more degrees of stress. However, the distinctive evidence that the
occupational factors may influence the development of peptic ulcer disease is yet to be
established.
Alcohol
High concentrated alcohols destroy the gastric mucosal barrier into Hydrogen ions, which results
in acute gastric mucosal sores presented by mucosal hemorrhages. Alcohol itself initiates the
secretion of the acid, while the content of the alcoholic beverages can also stimulate the secretion
of the acid.
Genetic factors
Genetic factors play a significant role in the pathogenesis of ulcer infection. The prevalence of
developing the disease in the close relatives of the ulcer patient is three times greater than within
the general public. About 20-25% of the patients with duodenal ulcer cases have a positive
family history, while the gastric ulcer patient reports ununiformed cases of the disease in the
family history.
Symptoms
Many studies have demonstrated how psychological distress have influenced the natural
history and pathogenesis of peptic ulcer disease. The conclusions about the contributing factor of
the psychological factors towards the cause of peptic ulcer disease are far from being established.
There is no concluded “ulcer–type” personality. Acute stress increases the pulse rate, anxiety,
and blood pressure of the patients with duodenal ulcers leading to a significant increase in the
basal acid secretion. Typically, ulcer patient shows the same psychological makeup as in other
people, but they appear to have more degrees of stress. However, the distinctive evidence that the
occupational factors may influence the development of peptic ulcer disease is yet to be
established.
Alcohol
High concentrated alcohols destroy the gastric mucosal barrier into Hydrogen ions, which results
in acute gastric mucosal sores presented by mucosal hemorrhages. Alcohol itself initiates the
secretion of the acid, while the content of the alcoholic beverages can also stimulate the secretion
of the acid.
Genetic factors
Genetic factors play a significant role in the pathogenesis of ulcer infection. The prevalence of
developing the disease in the close relatives of the ulcer patient is three times greater than within
the general public. About 20-25% of the patients with duodenal ulcer cases have a positive
family history, while the gastric ulcer patient reports ununiformed cases of the disease in the
family history.
Symptoms
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ULCER INFECTION 8
Some of the symptoms linked to peptic ulcer disease are abdominal pain and discomfort
and nausea. The pain is experienced in the epigastrium. The ulcer patients describe the pain as a
gnawing, slowly building up for 1-2 hours before it starts decreasing. Gastric ulcer is aggravated
by meals while duodenal ulcers are minimized by meals. This corresponds to why gastric ulcer
patient tends to avoid meals, thus losing weight while those with duodenal do not present weight
loss.
Complications
The disease is associated with internal bleeding (Hemorrhage), perforation due to burning in the
stomach wall, gastric outlet barrier after the contraction of the pylorus. The opening of the
stomach into the small intestine is called the pylorus.
Treatment
Medical Therapy
The PPIs, thought cannot kill the H. pylori infection; they help in fighting the H. pylori
infection. The medicines also reduce acid secretion and protect the lining of the duodenum and
that of the stomach. These PPIs include the esomeprazole (Nexium) and dexlansoprazole
(Dexilant). The doctor can prescribe some antibiotics that can kill H. pylori. The ways in which
the doctors prescribe these antibiotics are different throughout the world. There are specific types
of antibiotics that cannot destroy certain types of H. pylori. Histamine receptor blockers block
the biochemical histamine in the body that initiates the stomach to secrete acid. Some of the
histamine receptor blockers include the Tagmet (cimetidine) and Pepcid (famotidine). Antacids
relieve the peptic ulcer pain temporarily though it does not kill the H. pylori.
Surgical interventions; they are preferred when the ulcer creates a hole in the stomach wall
Some of the symptoms linked to peptic ulcer disease are abdominal pain and discomfort
and nausea. The pain is experienced in the epigastrium. The ulcer patients describe the pain as a
gnawing, slowly building up for 1-2 hours before it starts decreasing. Gastric ulcer is aggravated
by meals while duodenal ulcers are minimized by meals. This corresponds to why gastric ulcer
patient tends to avoid meals, thus losing weight while those with duodenal do not present weight
loss.
Complications
The disease is associated with internal bleeding (Hemorrhage), perforation due to burning in the
stomach wall, gastric outlet barrier after the contraction of the pylorus. The opening of the
stomach into the small intestine is called the pylorus.
Treatment
Medical Therapy
The PPIs, thought cannot kill the H. pylori infection; they help in fighting the H. pylori
infection. The medicines also reduce acid secretion and protect the lining of the duodenum and
that of the stomach. These PPIs include the esomeprazole (Nexium) and dexlansoprazole
(Dexilant). The doctor can prescribe some antibiotics that can kill H. pylori. The ways in which
the doctors prescribe these antibiotics are different throughout the world. There are specific types
of antibiotics that cannot destroy certain types of H. pylori. Histamine receptor blockers block
the biochemical histamine in the body that initiates the stomach to secrete acid. Some of the
histamine receptor blockers include the Tagmet (cimetidine) and Pepcid (famotidine). Antacids
relieve the peptic ulcer pain temporarily though it does not kill the H. pylori.
Surgical interventions; they are preferred when the ulcer creates a hole in the stomach wall
ULCER INFECTION 9
Endoscopy; is the most appropriate to treat some bleeding ulcers.
Lifestyle
Choice of a healthier diet
Eating a healthy diet, especially rich in vitamins A and C, like fruits, whole grains, and
vegetables. A patient who is not taking vitamin reach foods finds it difficult to heal the ulcers.
Considering foods like yogurt, miso, sauerkraut, and aged cheeses and stop the use of NSAIDs.
Elimination of the Milk
Sometimes milk can relieve ulcer pain, but later drinking milk will promote the production of
excess acid, thus increasing the ulcer pain.
Controlling of Stress and avoid Smoking
Controlling stress and avoid smoking can protect the severity of the signs and symptoms of the
disease and reduce the production of stomach acid. Smoking obstructs the stomach lining making
it more prone to ulcer development. When a patient is much stressed, the signs and symptoms of
the peptic ulcers worsen than when he/she is in a calm condition.
Minimal avoidance of alcohol usage
Limited use of alcohol is encouraged to avoid erosion of the mucosal lining in the stomach and
intestine. Too much use of alcohol can erode and aggravate the mucosal lining of the stomach
and small intestine, causing bleeding inflammation (Peptic ulcer, 2020).
Conclusion
Endoscopy; is the most appropriate to treat some bleeding ulcers.
Lifestyle
Choice of a healthier diet
Eating a healthy diet, especially rich in vitamins A and C, like fruits, whole grains, and
vegetables. A patient who is not taking vitamin reach foods finds it difficult to heal the ulcers.
Considering foods like yogurt, miso, sauerkraut, and aged cheeses and stop the use of NSAIDs.
Elimination of the Milk
Sometimes milk can relieve ulcer pain, but later drinking milk will promote the production of
excess acid, thus increasing the ulcer pain.
Controlling of Stress and avoid Smoking
Controlling stress and avoid smoking can protect the severity of the signs and symptoms of the
disease and reduce the production of stomach acid. Smoking obstructs the stomach lining making
it more prone to ulcer development. When a patient is much stressed, the signs and symptoms of
the peptic ulcers worsen than when he/she is in a calm condition.
Minimal avoidance of alcohol usage
Limited use of alcohol is encouraged to avoid erosion of the mucosal lining in the stomach and
intestine. Too much use of alcohol can erode and aggravate the mucosal lining of the stomach
and small intestine, causing bleeding inflammation (Peptic ulcer, 2020).
Conclusion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

ULCER INFECTION 10
In conclusion, the essay has demonstrated the pathophysiology, causes, symptoms,
treatment, gastric protective factors, and the complications associated with peptic ulcer disease.
Gastric protective factors are the defensive mechanisms that help the lining mucosal of the small
intestine and the stomach to function normally even after the exposure to the injurious aggressive
factors. Various factors such as stress, smoking, bacteria, NSAIDs, alcohol, hypersecretion of
gastric acid, and the genetic factors enable the development of peptic ulcer disease. Some
common symptoms of the disease include abdominal bleeding, inflammation, abdominal pain,
discomfort, and nausea. The paper has demonstrated that gastric outlet obstruction, perforation,
and hemorrhage are some of the complications associated with peptic ulcer disease. The
treatment of the disease includes surgical and medical therapies, endoscopy, and changing into
healthier lifestyles ways.
In conclusion, the essay has demonstrated the pathophysiology, causes, symptoms,
treatment, gastric protective factors, and the complications associated with peptic ulcer disease.
Gastric protective factors are the defensive mechanisms that help the lining mucosal of the small
intestine and the stomach to function normally even after the exposure to the injurious aggressive
factors. Various factors such as stress, smoking, bacteria, NSAIDs, alcohol, hypersecretion of
gastric acid, and the genetic factors enable the development of peptic ulcer disease. Some
common symptoms of the disease include abdominal bleeding, inflammation, abdominal pain,
discomfort, and nausea. The paper has demonstrated that gastric outlet obstruction, perforation,
and hemorrhage are some of the complications associated with peptic ulcer disease. The
treatment of the disease includes surgical and medical therapies, endoscopy, and changing into
healthier lifestyles ways.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ULCER INFECTION 11
References
Alpers, D. H., & Yamada, T. (2009). Textbook of Gastroenterology: Vol. 5th ed. Wiley-
Blackwell
Berg, P., & McCallum, R. (2016). Dumping syndrome: a review of the current concepts of
pathophysiology, diagnosis, and treatment. Digestive diseases and sciences, 61(1), 11-18.
Chai, J. (2011). Gastric Ulcer Healing - Role of Serum Response Factor. INTECH Open Access
Publisher.
Peptic ulcer. (2020, April 3). Retrieved from
https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/diagnosis-treatment/drc-
20354229
Zatorski, H. (2017). Pathophysiology and risk factors in peptic ulcer disease. In Introduction to
Gastrointestinal Diseases Vol. 2 (pp. 7-20). Springer, Cham.
References
Alpers, D. H., & Yamada, T. (2009). Textbook of Gastroenterology: Vol. 5th ed. Wiley-
Blackwell
Berg, P., & McCallum, R. (2016). Dumping syndrome: a review of the current concepts of
pathophysiology, diagnosis, and treatment. Digestive diseases and sciences, 61(1), 11-18.
Chai, J. (2011). Gastric Ulcer Healing - Role of Serum Response Factor. INTECH Open Access
Publisher.
Peptic ulcer. (2020, April 3). Retrieved from
https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/diagnosis-treatment/drc-
20354229
Zatorski, H. (2017). Pathophysiology and risk factors in peptic ulcer disease. In Introduction to
Gastrointestinal Diseases Vol. 2 (pp. 7-20). Springer, Cham.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




