Pharmacy Practice 17: Hospital System Challenges Analysis
VerifiedAdded on 2020/04/29
|21
|5415
|1047
Report
AI Summary
This report, focusing on Pharmacy Practice 17, investigates the challenges faced by pharmacy professionals and healthcare managers within large hospital systems. Utilizing a literature review, the report identifies key obstacles such as the need to convince stakeholders of the problem, lack of expertise, inadequate financial support, and insufficient organizational capacity. The report explores the roles of pharmacy professionals in implementing healthcare innovations, pharmacogenomics, and evidence-based medicine, highlighting challenges like lack of exposure to pharmacy informatics and the need for adequate role models. The methodology includes a PICO framework and searches of Medline, CINAHL, and SCOPUS databases to formulate a research question and analyze existing literature. The study emphasizes the importance of addressing these challenges to ensure quality patient care, maintain fiscal responsibility, and adapt to the rapidly evolving healthcare landscape. The report also touches upon the need for improved teamwork designs and the impact of technology on healthcare management.

Running head: PHARMACY PRACTICE
Challenges for pharmacy professionals in large hospital systems
Name of the Student
Name of the University
Author Note
Challenges for pharmacy professionals in large hospital systems
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PHARMACY PRACTICE
Abstract
The primary responsibility of health care managers is fostering an environment, which will
provide quality and necessary health care interventions to patients at maximum profit. They are
involved in determining health budgets, ordering and receiving supplies, administering benefits
and payrolls, and distributing regular communication among the hospital authorities and their
patients. They work by keeping up with relevant health care policies and laws, technologies and
standards. The pharmacy professionals and healthcare managers also have the responsibility of
representing their healthcare organization at external meetings, such as investor gatherings and
community forums. In order to determine the health care needs, they should take medical
decisions that will affect the finances of their hospital facilities. However, there are several
challenges and barriers that they face during implementation of their duties. Their duties vary
according to the title and function of the healthcare facilities. This report will aim to investigate
the several challenges that arise in health sector by using secondary data sources. It will use a
literature review to identify the challenges and will finally recommend measures that can be
adopted by them to ensure that patients receive necessary services and the costs are minimized.
Abstract
The primary responsibility of health care managers is fostering an environment, which will
provide quality and necessary health care interventions to patients at maximum profit. They are
involved in determining health budgets, ordering and receiving supplies, administering benefits
and payrolls, and distributing regular communication among the hospital authorities and their
patients. They work by keeping up with relevant health care policies and laws, technologies and
standards. The pharmacy professionals and healthcare managers also have the responsibility of
representing their healthcare organization at external meetings, such as investor gatherings and
community forums. In order to determine the health care needs, they should take medical
decisions that will affect the finances of their hospital facilities. However, there are several
challenges and barriers that they face during implementation of their duties. Their duties vary
according to the title and function of the healthcare facilities. This report will aim to investigate
the several challenges that arise in health sector by using secondary data sources. It will use a
literature review to identify the challenges and will finally recommend measures that can be
adopted by them to ensure that patients receive necessary services and the costs are minimized.
2PHARMACY PRACTICE
Introduction
Quality management is a critical requirement across all healthcare organizations.
Building patient centric quality management is considered of utmost importance. Several tools
and standards are imposed by healthcare managers to achieve quality management. The primary
role of pharmacy professionals and healthcare managers is to provide high quality healthcare,
while ensuring that the patient is taken care of (Lee et al., 2012). The managers are responsible
for ensuring that the regulations and processes are being adhered to. They keep a check on
adaptation of the standards and instill the processes into the healthcare setting, with the aim of
assuring patient safety and satisfaction. The job of a healthcare manager is undoubtedly
demanding and difficult (Batalden et al., 2015). The topic is essential in IT industry owing to the
fact that healthcare management is one of the fastest growing industries. The need for
comprehensive healthcare practices is ever-increasing due to population explosion and
development in science.
Thus, the practices involved in healthcare management need to be continuously improved
to satisfy the ever-increasing market. With rise in health expenses and increase in competition,
managers must be prepared to effectively lead the hospital settings. Managers combine a sound
understanding of healthcare system with business expertise and work toward increasing
effectiveness and efficiency. Rapid reforms and innovation have made delivery of quality care
central to hospital management (Kirkpatrick et al., 2013). This can be accounted for the fact that
the federal government and the patients expect delivery of results by skilled management
professionals.
Introduction
Quality management is a critical requirement across all healthcare organizations.
Building patient centric quality management is considered of utmost importance. Several tools
and standards are imposed by healthcare managers to achieve quality management. The primary
role of pharmacy professionals and healthcare managers is to provide high quality healthcare,
while ensuring that the patient is taken care of (Lee et al., 2012). The managers are responsible
for ensuring that the regulations and processes are being adhered to. They keep a check on
adaptation of the standards and instill the processes into the healthcare setting, with the aim of
assuring patient safety and satisfaction. The job of a healthcare manager is undoubtedly
demanding and difficult (Batalden et al., 2015). The topic is essential in IT industry owing to the
fact that healthcare management is one of the fastest growing industries. The need for
comprehensive healthcare practices is ever-increasing due to population explosion and
development in science.
Thus, the practices involved in healthcare management need to be continuously improved
to satisfy the ever-increasing market. With rise in health expenses and increase in competition,
managers must be prepared to effectively lead the hospital settings. Managers combine a sound
understanding of healthcare system with business expertise and work toward increasing
effectiveness and efficiency. Rapid reforms and innovation have made delivery of quality care
central to hospital management (Kirkpatrick et al., 2013). This can be accounted for the fact that
the federal government and the patients expect delivery of results by skilled management
professionals.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PHARMACY PRACTICE
However, the managers need to overcome several challenges to improve patient care and
maintain fiscal responsibility. This report will therefore illustrate on the different challenges
faced by pharmacy professionals and healthcare managers in hospital settings. The report will
focus on a literature review to illustrate the several challenges faced by healthcare managers
across large hospitals.
Literature review
A particular study aimed to formally evaluate the healthcare programs to understand the
challenges that occur in healthcare settings while improving care quality. The study further tried
to identify the ways by which the challenges could be addressed. Lessons from the Health
Foundation’s improvement programmes were integrated with relevant literature. Several reports
were read and carefully analysed. NVivo software was used to undertake the analysis. This was
followed by conduction of a narrative review of the organizational factors that would likely
hinder efforts of improvement. The analysis helped in the identification of 10 key challenges that
were related to improvement interventions and professional context. The fundamental challenge
identified was failure to convince people that there was a need to address the real problem. While
planning and designing interventions, the healthcare managers must carefully target the problems
that are more likely to be accepted across the hospital setting. The study identified other
challenges at the planning stage, which included contest of the chosen interventions due to lack
of sufficient evidence, poor data collection and lack of adequate monitoring, lack of expertise
and inadequate financial support, managerial skills and infrastructure. The findings also provided
evidence that lack of work culture, inadequate organizational capacity can create emotional
exhaustion create adverse outcomes. Lack of engagement of staff and failure to overcome lack of
However, the managers need to overcome several challenges to improve patient care and
maintain fiscal responsibility. This report will therefore illustrate on the different challenges
faced by pharmacy professionals and healthcare managers in hospital settings. The report will
focus on a literature review to illustrate the several challenges faced by healthcare managers
across large hospitals.
Literature review
A particular study aimed to formally evaluate the healthcare programs to understand the
challenges that occur in healthcare settings while improving care quality. The study further tried
to identify the ways by which the challenges could be addressed. Lessons from the Health
Foundation’s improvement programmes were integrated with relevant literature. Several reports
were read and carefully analysed. NVivo software was used to undertake the analysis. This was
followed by conduction of a narrative review of the organizational factors that would likely
hinder efforts of improvement. The analysis helped in the identification of 10 key challenges that
were related to improvement interventions and professional context. The fundamental challenge
identified was failure to convince people that there was a need to address the real problem. While
planning and designing interventions, the healthcare managers must carefully target the problems
that are more likely to be accepted across the hospital setting. The study identified other
challenges at the planning stage, which included contest of the chosen interventions due to lack
of sufficient evidence, poor data collection and lack of adequate monitoring, lack of expertise
and inadequate financial support, managerial skills and infrastructure. The findings also provided
evidence that lack of work culture, inadequate organizational capacity can create emotional
exhaustion create adverse outcomes. Lack of engagement of staff and failure to overcome lack of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PHARMACY PRACTICE
ownership and low leadership skills were also recognized by the study as one of the biggest
challenges (Dixon-Woods, McNicol & Martin, 2012).
Another study was conducted to identify the roles of pharmacists in pharmacogenomics
implementation. The specific resources and responsibilities needed for pharmacy professionals to
execute their roles had not yet been defined. The study identified the roles of pharmacy
professionals by summarizing the results obtained from a clopidogrel-CYP2C19 pilot project.
The project involved administration of antiplatelet therapies for patients who had undergone
percutaneous coronary intervention and stent placement. More than 1000 patients were
genotyped. The results revealed the essential roles of pharmacy professionals. These roles and
responsibilities included expertise in developing electronic medical records and clinical decision
support system (pharmacy informatics), implementing medication safety, adhering to medication
regulations and policies, developing educational strategies and logistically using all drug related
information and database management approaches in patient care centres. Pharmacy
professionals are also involved in solving ethical issues related to patient care. The results
suggested that 14 pharmacists were involved in the program during the first 2 years of study and
needed to develop an expertise in pharmacokinetics, pharmacogenomics and informatics to
achieve holistic patient care (Owusu‐Obeng et al., 2014).
The role of healthcare managers in implementation of innovative healthcare was
demonstrated by another study. The study results proved that these managers play a key role in
implementing healthcare innovation. The gap that existed between practice and effective care
evidences was attributed to poor implementation of healthcare innovations. The study suggested
that managers are involved in influencing healthcare innovation implementation by actively
synthesizing and diffusing information, mediating between daily activities and strategies, and
ownership and low leadership skills were also recognized by the study as one of the biggest
challenges (Dixon-Woods, McNicol & Martin, 2012).
Another study was conducted to identify the roles of pharmacists in pharmacogenomics
implementation. The specific resources and responsibilities needed for pharmacy professionals to
execute their roles had not yet been defined. The study identified the roles of pharmacy
professionals by summarizing the results obtained from a clopidogrel-CYP2C19 pilot project.
The project involved administration of antiplatelet therapies for patients who had undergone
percutaneous coronary intervention and stent placement. More than 1000 patients were
genotyped. The results revealed the essential roles of pharmacy professionals. These roles and
responsibilities included expertise in developing electronic medical records and clinical decision
support system (pharmacy informatics), implementing medication safety, adhering to medication
regulations and policies, developing educational strategies and logistically using all drug related
information and database management approaches in patient care centres. Pharmacy
professionals are also involved in solving ethical issues related to patient care. The results
suggested that 14 pharmacists were involved in the program during the first 2 years of study and
needed to develop an expertise in pharmacokinetics, pharmacogenomics and informatics to
achieve holistic patient care (Owusu‐Obeng et al., 2014).
The role of healthcare managers in implementation of innovative healthcare was
demonstrated by another study. The study results proved that these managers play a key role in
implementing healthcare innovation. The gap that existed between practice and effective care
evidences was attributed to poor implementation of healthcare innovations. The study suggested
that managers are involved in influencing healthcare innovation implementation by actively
synthesizing and diffusing information, mediating between daily activities and strategies, and
5PHARMACY PRACTICE
selling the innovations to important stakeholders. It emphasized on the fact that teamwork
designs are essential for the functioning of healthcare organizations. It showed that healthcare
managers are entitled with the responsibility of overseeing team initiatives. This enhances their
potential to influence implementation of innovative techniques (Birken, Lee & Weiner, 2012).
Another study attempted to evaluate the attitude, knowledge, and proficiency of
pharmacy graduates in the practice of evidence based medicine. Pre and post survey studies and
skill tests were conducted among the sample with the help of a valid questionnaire with the aim
of comprehending the transformation in the knowledge of pharmacy professionals during their
transition to a hospital setting. The skills gained by pharmacy undergraduates were assessed and
statistically analysed. A series of Problem Based Learning were conducted followed by
administration of pre and post-test and the competencies were assessed. On analysis of the data
using IBM SPSS v20.0 ANCOVA software, it was found that majority of the students could
formulate PICO questions and apply them in the healthcare setting after taking the pharmacy
course. One of the major challenges identified was the lack of adequate role models who would
promote the culture of evidence based practice on the hospital wards. A change in the behavior
of senior pharmacists on the use of EBP methods was needed to create a significant impact in the
minds of junior pharmacy professionals that would in turn improve the quality of patient care in
near future. Another challenge that pharmacy professionals face is the lack of exposure to
pharmacy informatics. This weakens their approach to searching for drug information. Moreover,
they are often unable to handle statistical information in large hospital settings (Abu-Gharbieh et
al., 2015).
A systematic content analysis was performed to identify the challenges and opportunities
in social pharmacy and pharmacy practice. Narrowly focused pharmacy services, lack of
selling the innovations to important stakeholders. It emphasized on the fact that teamwork
designs are essential for the functioning of healthcare organizations. It showed that healthcare
managers are entitled with the responsibility of overseeing team initiatives. This enhances their
potential to influence implementation of innovative techniques (Birken, Lee & Weiner, 2012).
Another study attempted to evaluate the attitude, knowledge, and proficiency of
pharmacy graduates in the practice of evidence based medicine. Pre and post survey studies and
skill tests were conducted among the sample with the help of a valid questionnaire with the aim
of comprehending the transformation in the knowledge of pharmacy professionals during their
transition to a hospital setting. The skills gained by pharmacy undergraduates were assessed and
statistically analysed. A series of Problem Based Learning were conducted followed by
administration of pre and post-test and the competencies were assessed. On analysis of the data
using IBM SPSS v20.0 ANCOVA software, it was found that majority of the students could
formulate PICO questions and apply them in the healthcare setting after taking the pharmacy
course. One of the major challenges identified was the lack of adequate role models who would
promote the culture of evidence based practice on the hospital wards. A change in the behavior
of senior pharmacists on the use of EBP methods was needed to create a significant impact in the
minds of junior pharmacy professionals that would in turn improve the quality of patient care in
near future. Another challenge that pharmacy professionals face is the lack of exposure to
pharmacy informatics. This weakens their approach to searching for drug information. Moreover,
they are often unable to handle statistical information in large hospital settings (Abu-Gharbieh et
al., 2015).
A systematic content analysis was performed to identify the challenges and opportunities
in social pharmacy and pharmacy practice. Narrowly focused pharmacy services, lack of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PHARMACY PRACTICE
consensus, pressure on publishing the research results and reduction in research funding add to
the challenges. The study suggested that creating provisions for patient-oriented healthcare
services and dispensing medication in a proper manner are some of the key issues that are faced
by pharmacy professionals and healthcare managers (Almarsdóttir, Kaae & Traulsen, 2014).
The research challenges faced in context awareness and computation communication for
ubiquitious healthcare were investigated by another study. The study stated that specialized
instructions and rising costs of hospitalizations created major problems for healthcare manages in
real-time hospital settings. The major challenges faced by them as identified by the research are
the discovery and provision of computing resources and wireless grid computing. The
unpredictability and high mobility of the device acts as a barrier in the interaction between data
providers. Reliable transmission and prioritization of vital signs of the patients posed another
challenge. Additional interference occurs due to proliferation of electronic devices that are used
in the hospitals. Thus, the study provided an overview of the factors that create difficulty for
healthcare managers to deliver personalized healthcare solutions in large hospital settings
(Viswanathan, Chen & Pompili, 2012).
Methodology
Development of a researchable question is one of the major challenging tasks that are
encountered while initiating a project. A researchable question can therefore be defined as an
uncertainty about a particular problem, which can be examined, challenged, and analyzed with
the aim of providing useful information. Thus, a successful research depends upon good
formulation of the research question based on the several problems that are faced in research
activities (Lang et al., 2012).
consensus, pressure on publishing the research results and reduction in research funding add to
the challenges. The study suggested that creating provisions for patient-oriented healthcare
services and dispensing medication in a proper manner are some of the key issues that are faced
by pharmacy professionals and healthcare managers (Almarsdóttir, Kaae & Traulsen, 2014).
The research challenges faced in context awareness and computation communication for
ubiquitious healthcare were investigated by another study. The study stated that specialized
instructions and rising costs of hospitalizations created major problems for healthcare manages in
real-time hospital settings. The major challenges faced by them as identified by the research are
the discovery and provision of computing resources and wireless grid computing. The
unpredictability and high mobility of the device acts as a barrier in the interaction between data
providers. Reliable transmission and prioritization of vital signs of the patients posed another
challenge. Additional interference occurs due to proliferation of electronic devices that are used
in the hospitals. Thus, the study provided an overview of the factors that create difficulty for
healthcare managers to deliver personalized healthcare solutions in large hospital settings
(Viswanathan, Chen & Pompili, 2012).
Methodology
Development of a researchable question is one of the major challenging tasks that are
encountered while initiating a project. A researchable question can therefore be defined as an
uncertainty about a particular problem, which can be examined, challenged, and analyzed with
the aim of providing useful information. Thus, a successful research depends upon good
formulation of the research question based on the several problems that are faced in research
activities (Lang et al., 2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PHARMACY PRACTICE
The main purpose of this literature search was to evaluate the available literature and
formulate a research question that would help in future research. The research problem was of
some familiarity and a topic of interest. There was a need to channelize the question by focusing
on information that was yet to be explored. Once the problem was narrowed down, the existing
literature was analysed and seeked and it helped to straighten research approach.
The hypothesis carefully created a testimony of how the research was expected to
proceed. It acted as one of the most essential tools that assisted in answering the research
question. Although, the literature search was time-consuming and exhaustive, some simple steps
were adopted that helped in managing the process. The steps used for the methodology are stated
below:
Formulating the research question
A well-focused question was formulated and acted as a critical step for facilitating
clinical research. There were several general and patient-oriented questions that arose from
clinical issues. However, this study aimed to investigate the potential challenges that are faced by
healthcare managers and pharmacy professionals in real-time hospital settings. While
formulating a research question, the FINER criteria was considered (F-Feasible, I-Interesting, N-
Novel, E-Ethical and R-Relevant). The idea was interesting and relevant to clinical research. It
would have helped in adding information to already completed research work (Cook & West,
2012).
A PICO framework was used to develop the research question. It helped to focus on the
exact information that was needed (Cooke, Smith & Booth, 2012). The study population,
The main purpose of this literature search was to evaluate the available literature and
formulate a research question that would help in future research. The research problem was of
some familiarity and a topic of interest. There was a need to channelize the question by focusing
on information that was yet to be explored. Once the problem was narrowed down, the existing
literature was analysed and seeked and it helped to straighten research approach.
The hypothesis carefully created a testimony of how the research was expected to
proceed. It acted as one of the most essential tools that assisted in answering the research
question. Although, the literature search was time-consuming and exhaustive, some simple steps
were adopted that helped in managing the process. The steps used for the methodology are stated
below:
Formulating the research question
A well-focused question was formulated and acted as a critical step for facilitating
clinical research. There were several general and patient-oriented questions that arose from
clinical issues. However, this study aimed to investigate the potential challenges that are faced by
healthcare managers and pharmacy professionals in real-time hospital settings. While
formulating a research question, the FINER criteria was considered (F-Feasible, I-Interesting, N-
Novel, E-Ethical and R-Relevant). The idea was interesting and relevant to clinical research. It
would have helped in adding information to already completed research work (Cook & West,
2012).
A PICO framework was used to develop the research question. It helped to focus on the
exact information that was needed (Cooke, Smith & Booth, 2012). The study population,
8PHARMACY PRACTICE
intervention or indicator, comparison or benchmark and the primary outcome of the anticipated
results were used for framing the question. In this particular case scenario:
intervention or indicator, comparison or benchmark and the primary outcome of the anticipated
results were used for framing the question. In this particular case scenario:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PHARMACY PRACTICE
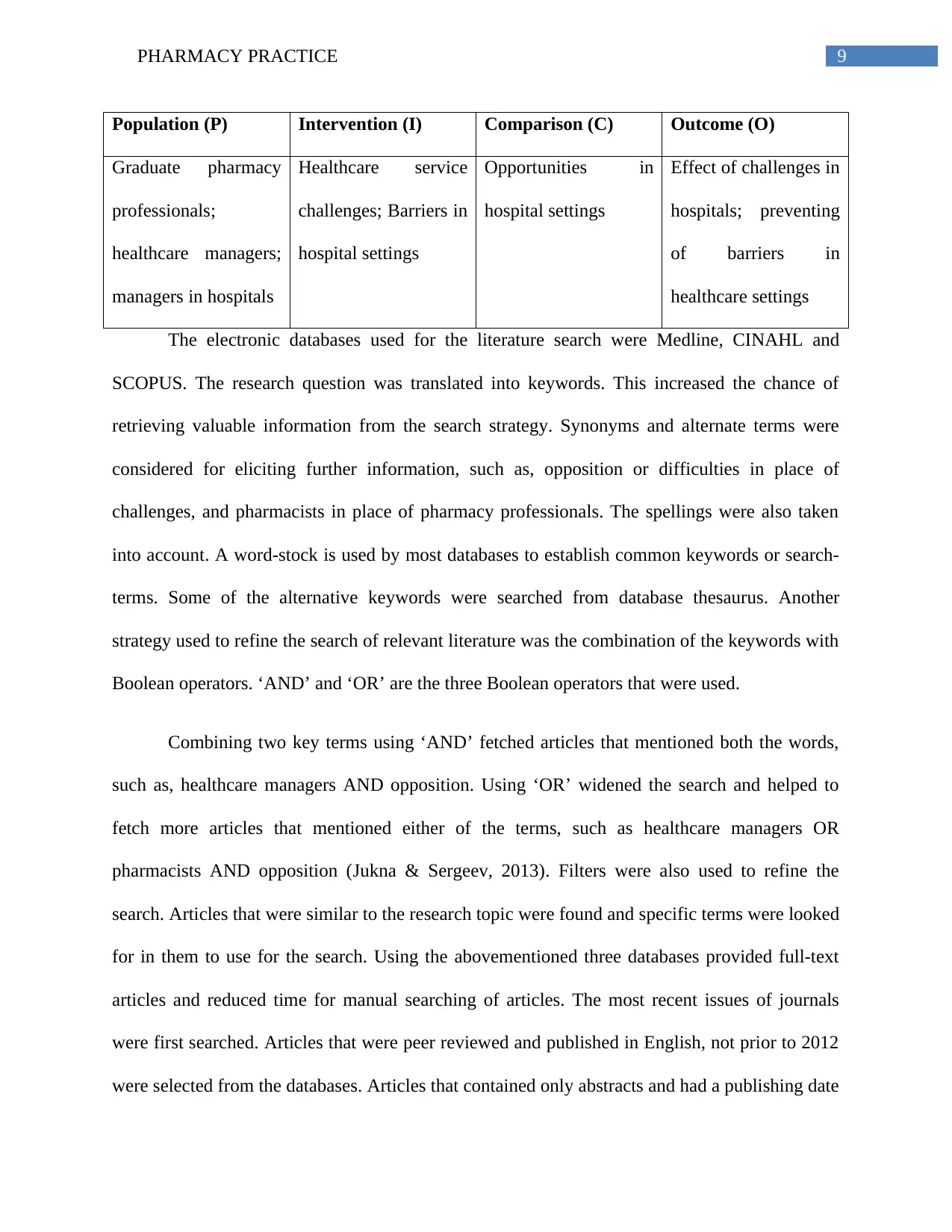
Population (P) Intervention (I) Comparison (C) Outcome (O)
Graduate pharmacy
professionals;
healthcare managers;
managers in hospitals
Healthcare service
challenges; Barriers in
hospital settings
Opportunities in
hospital settings
Effect of challenges in
hospitals; preventing
of barriers in
healthcare settings
The electronic databases used for the literature search were Medline, CINAHL and
SCOPUS. The research question was translated into keywords. This increased the chance of
retrieving valuable information from the search strategy. Synonyms and alternate terms were
considered for eliciting further information, such as, opposition or difficulties in place of
challenges, and pharmacists in place of pharmacy professionals. The spellings were also taken
into account. A word-stock is used by most databases to establish common keywords or search-
terms. Some of the alternative keywords were searched from database thesaurus. Another
strategy used to refine the search of relevant literature was the combination of the keywords with
Boolean operators. ‘AND’ and ‘OR’ are the three Boolean operators that were used.
Combining two key terms using ‘AND’ fetched articles that mentioned both the words,
such as, healthcare managers AND opposition. Using ‘OR’ widened the search and helped to
fetch more articles that mentioned either of the terms, such as healthcare managers OR
pharmacists AND opposition (Jukna & Sergeev, 2013). Filters were also used to refine the
search. Articles that were similar to the research topic were found and specific terms were looked
for in them to use for the search. Using the abovementioned three databases provided full-text
articles and reduced time for manual searching of articles. The most recent issues of journals
were first searched. Articles that were peer reviewed and published in English, not prior to 2012
were selected from the databases. Articles that contained only abstracts and had a publishing date
Population (P) Intervention (I) Comparison (C) Outcome (O)
Graduate pharmacy
professionals;
healthcare managers;
managers in hospitals
Healthcare service
challenges; Barriers in
hospital settings
Opportunities in
hospital settings
Effect of challenges in
hospitals; preventing
of barriers in
healthcare settings
The electronic databases used for the literature search were Medline, CINAHL and
SCOPUS. The research question was translated into keywords. This increased the chance of
retrieving valuable information from the search strategy. Synonyms and alternate terms were
considered for eliciting further information, such as, opposition or difficulties in place of
challenges, and pharmacists in place of pharmacy professionals. The spellings were also taken
into account. A word-stock is used by most databases to establish common keywords or search-
terms. Some of the alternative keywords were searched from database thesaurus. Another
strategy used to refine the search of relevant literature was the combination of the keywords with
Boolean operators. ‘AND’ and ‘OR’ are the three Boolean operators that were used.
Combining two key terms using ‘AND’ fetched articles that mentioned both the words,
such as, healthcare managers AND opposition. Using ‘OR’ widened the search and helped to
fetch more articles that mentioned either of the terms, such as healthcare managers OR
pharmacists AND opposition (Jukna & Sergeev, 2013). Filters were also used to refine the
search. Articles that were similar to the research topic were found and specific terms were looked
for in them to use for the search. Using the abovementioned three databases provided full-text
articles and reduced time for manual searching of articles. The most recent issues of journals
were first searched. Articles that were peer reviewed and published in English, not prior to 2012
were selected from the databases. Articles that contained only abstracts and had a publishing date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PHARMACY PRACTICE
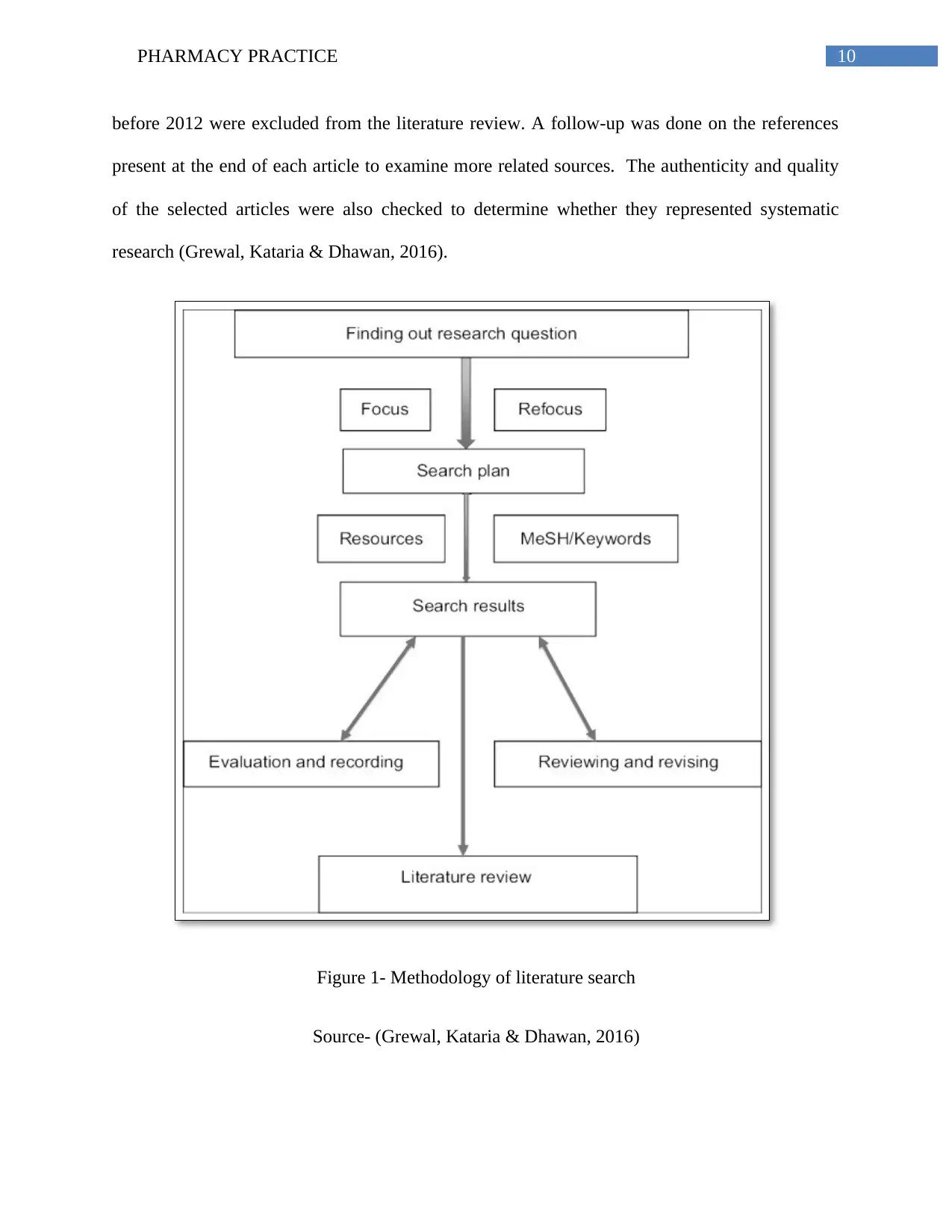
before 2012 were excluded from the literature review. A follow-up was done on the references
present at the end of each article to examine more related sources. The authenticity and quality
of the selected articles were also checked to determine whether they represented systematic
research (Grewal, Kataria & Dhawan, 2016).
Figure 1- Methodology of literature search
Source- (Grewal, Kataria & Dhawan, 2016)
before 2012 were excluded from the literature review. A follow-up was done on the references
present at the end of each article to examine more related sources. The authenticity and quality
of the selected articles were also checked to determine whether they represented systematic
research (Grewal, Kataria & Dhawan, 2016).
Figure 1- Methodology of literature search
Source- (Grewal, Kataria & Dhawan, 2016)
11PHARMACY PRACTICE
Relevance of the topic
The topic selected for this study intersects with management and healthcare. Health care
managers are entrusted with the responsibility of overseeing the business aspects such as
operations and finances of a health care organization. Their primary responsibility is to ensure
that all patients admitted to the hospital or healthcare centre receive high quality care. This can
be only achieved by providing all necessary resources and tools that help nurses and physicians
to deliver great health care (Sanii et al., 2016). Their duties also require them to ensure that the
healthcare organization is operationally and financially sound, the personnel issues are managed
well and the community members are taught properly on the different health issues. Thus, they
play an essential role in reducing hospitalization costs while maintaining patient satisfaction.
Pharmacy professionals are also involved in dispensing medications and monitoring the health
and progress of patients by optimizing their response to medication interventions. The patients
are educated on proper use of prescriptions and are provided holistic based care in institutional
settings (Tripathi et al., 2014).
Thus, if these healthcare managers and pharmacists face challenges while carrying out
their duties in a hospital setting, the overall health of the patient will deteriorate. There will be a
delay in cure of the disease and elimination of symptoms, which in turn will create adverse
health outcomes. Thus, the research question for this study is of extreme importance to managing
patient health as identification of the key barriers or challenges on performing a literature search
would assist healthcare practitioners to work towards improving the flaws, minimizing risks and
maintaining overall patient health.
Primary sources basically provide information that is closely related to the research topic.
However, it was difficult to collect such data from interviews, surveys or questionnaires due to
Relevance of the topic
The topic selected for this study intersects with management and healthcare. Health care
managers are entrusted with the responsibility of overseeing the business aspects such as
operations and finances of a health care organization. Their primary responsibility is to ensure
that all patients admitted to the hospital or healthcare centre receive high quality care. This can
be only achieved by providing all necessary resources and tools that help nurses and physicians
to deliver great health care (Sanii et al., 2016). Their duties also require them to ensure that the
healthcare organization is operationally and financially sound, the personnel issues are managed
well and the community members are taught properly on the different health issues. Thus, they
play an essential role in reducing hospitalization costs while maintaining patient satisfaction.
Pharmacy professionals are also involved in dispensing medications and monitoring the health
and progress of patients by optimizing their response to medication interventions. The patients
are educated on proper use of prescriptions and are provided holistic based care in institutional
settings (Tripathi et al., 2014).
Thus, if these healthcare managers and pharmacists face challenges while carrying out
their duties in a hospital setting, the overall health of the patient will deteriorate. There will be a
delay in cure of the disease and elimination of symptoms, which in turn will create adverse
health outcomes. Thus, the research question for this study is of extreme importance to managing
patient health as identification of the key barriers or challenges on performing a literature search
would assist healthcare practitioners to work towards improving the flaws, minimizing risks and
maintaining overall patient health.
Primary sources basically provide information that is closely related to the research topic.
However, it was difficult to collect such data from interviews, surveys or questionnaires due to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





