Ethics and Professional Practice: PAD Ethical Dilemma Report
VerifiedAdded on 2022/10/17
|11
|2669
|173
Report
AI Summary
This report examines the ethical issues surrounding Physician-Assisted Death (PAD), focusing on the perspectives of a doctor and a legal advisor. It defines PAD, poses an ethical question about allowing it for those with chronic diseases, and explores differing viewpoints, including the belief that life is sacred versus the right to end suffering. The report analyzes the positions of a physician who supports PAD to respect patient autonomy and a legal advisor who expresses reservations but acknowledges potential exceptions. It applies ethical theories like deontology and virtue ethics to these positions. The report also articulates the professional and personal stances of physicians, highlighting emotional and legal challenges in making PAD decisions, while emphasizing the importance of high-quality palliative care. The report includes a participant information sheet and consent form as an appendix.

Running Head: Ethics And Professional Practice
ETHICS AND PROFESSIONAL PRACTICE
ETHICS AND PROFESSIONAL PRACTICE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Ethics And Professional Practice
Table of Contents
1. Defining ethical issue: Allowing Physician-Assisted Death (PAD)......................................3
2. Ethical question......................................................................................................................3
3. Different perspective of the issue...........................................................................................3
4. Describing and analyzing positions adopted by two selected individuals (1 Doctor and 1
legal advisor)..............................................................................................................................4
5. Articulating professional and personal position, and potential challenges............................6
Reference list..............................................................................................................................8
Appendix..................................................................................................................................11
Ethics And Professional Practice
Table of Contents
1. Defining ethical issue: Allowing Physician-Assisted Death (PAD)......................................3
2. Ethical question......................................................................................................................3
3. Different perspective of the issue...........................................................................................3
4. Describing and analyzing positions adopted by two selected individuals (1 Doctor and 1
legal advisor)..............................................................................................................................4
5. Articulating professional and personal position, and potential challenges............................6
Reference list..............................................................................................................................8
Appendix..................................................................................................................................11
3
Ethics And Professional Practice
1. Defining ethical issue: Allowing Physician-Assisted Death (PAD)
Physician-assisted dying is legal in different regions of the world like California. However, at
the same time, a question arises regarding the ethical acceptability of the support activity. As
opined by Battin, Rhodes & Silvers (2015), PAD is considered as support as baby boomers
are growing older. Survey shows that near about 50 percent of doctors support this activity
because it helps to provide relief to the patients from their sufferings. PAD can be defined as
a physician providing a lethal dose on a patient request to end life (Appelbaum, 2016). Some
group of people thinks that harming patients cannot be supported while providing care. This
creates an ethical dilemma.
2. Ethical question
Should a person suffering from chronic disease be allowed for physician-assisted death
(PAD)?
3. Different perspective of the issue
Two different perspectives are associated with this ethical issue. As mentioned by Petrillo et
al. (2017), a group of people thinks that PAD is a right of an individual and it helps them to
get rid of their painful life as per their consent. On the other hand, another group of people
believes that life is a gift of God and it must not be ended by human beings. This argument is
very old and legal system of different countries has been framed with different perspectives.
As stated by Hudson, Hudson, Philip, Boughey, Kelly & Hertogh (2015), ethics differs from
moral to morality. In terms of morality, ethics deals with a well-known standard of rightness.
However, moral is a belief about a stereotypic consideration. These two perspectives are very
common in terms of argument with PAD. in many countries, PAD is legal and it is easier for
Ethics And Professional Practice
1. Defining ethical issue: Allowing Physician-Assisted Death (PAD)
Physician-assisted dying is legal in different regions of the world like California. However, at
the same time, a question arises regarding the ethical acceptability of the support activity. As
opined by Battin, Rhodes & Silvers (2015), PAD is considered as support as baby boomers
are growing older. Survey shows that near about 50 percent of doctors support this activity
because it helps to provide relief to the patients from their sufferings. PAD can be defined as
a physician providing a lethal dose on a patient request to end life (Appelbaum, 2016). Some
group of people thinks that harming patients cannot be supported while providing care. This
creates an ethical dilemma.
2. Ethical question
Should a person suffering from chronic disease be allowed for physician-assisted death
(PAD)?
3. Different perspective of the issue
Two different perspectives are associated with this ethical issue. As mentioned by Petrillo et
al. (2017), a group of people thinks that PAD is a right of an individual and it helps them to
get rid of their painful life as per their consent. On the other hand, another group of people
believes that life is a gift of God and it must not be ended by human beings. This argument is
very old and legal system of different countries has been framed with different perspectives.
As stated by Hudson, Hudson, Philip, Boughey, Kelly & Hertogh (2015), ethics differs from
moral to morality. In terms of morality, ethics deals with a well-known standard of rightness.
However, moral is a belief about a stereotypic consideration. These two perspectives are very
common in terms of argument with PAD. in many countries, PAD is legal and it is easier for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Ethics And Professional Practice
a person to opt for PAD. For example, people of Belgium, Switzerland, The Netherlands,
Canada, Colombia, six states of US including Washington, Oregon, California, Colorado, and
Montana, are able to make their decision about their life. Frey & Hans (2016) have described
that, as per the legal system of these countries, people have autonomy to make their decision
about end of life and healthcare professionals faceless ethical dilemma in assisting suicide.
Other countries are still facing an ethical dilemma regarding PAD. As mentioned by Karsoho,
Fishman, Wright & Macdonald (2016), doctors, nurses and healthcare practitioners are liable
to save lives of people. They are morally bound to perform this duty. This aspect has become
a part of their mindset. Hence, it is difficult for them to assist in suicide. These kind of
personalities are holding the moral belief that a person cannot get assistance in dying. As
contradicted by Petrillo et al. (2017), development of society is allowing people to focus on
morality. They understand that the right decision must be taken even if it is hard. Based on
this perspective, legal system of several countries is allowing physicians to assist in the
suicide of patient with non-curable diseases. It can be seen that some of the physicians
believe in the concept of virtue ethics. Aim of this kind of people is to maintain good public
relations by focusing on virtues. Another group of physicians rely on deontological ethics and
make decisions according to the situation. This kind of physicians is able to assist in suicide
after evaluating poor condition of the patient. Both of these perspectives are partially correct
and one of these can be chosen after evaluating all related aspects in case of PAD.
4. Describing and analyzing positions adopted by two selected individuals (1 Doctor and
1 legal advisor)
Response about the question was collected from two people who are involved in this process
of PAD. A doctor and a legal advisor were involved in the study.
Response from doctor:
Ethics And Professional Practice
a person to opt for PAD. For example, people of Belgium, Switzerland, The Netherlands,
Canada, Colombia, six states of US including Washington, Oregon, California, Colorado, and
Montana, are able to make their decision about their life. Frey & Hans (2016) have described
that, as per the legal system of these countries, people have autonomy to make their decision
about end of life and healthcare professionals faceless ethical dilemma in assisting suicide.
Other countries are still facing an ethical dilemma regarding PAD. As mentioned by Karsoho,
Fishman, Wright & Macdonald (2016), doctors, nurses and healthcare practitioners are liable
to save lives of people. They are morally bound to perform this duty. This aspect has become
a part of their mindset. Hence, it is difficult for them to assist in suicide. These kind of
personalities are holding the moral belief that a person cannot get assistance in dying. As
contradicted by Petrillo et al. (2017), development of society is allowing people to focus on
morality. They understand that the right decision must be taken even if it is hard. Based on
this perspective, legal system of several countries is allowing physicians to assist in the
suicide of patient with non-curable diseases. It can be seen that some of the physicians
believe in the concept of virtue ethics. Aim of this kind of people is to maintain good public
relations by focusing on virtues. Another group of physicians rely on deontological ethics and
make decisions according to the situation. This kind of physicians is able to assist in suicide
after evaluating poor condition of the patient. Both of these perspectives are partially correct
and one of these can be chosen after evaluating all related aspects in case of PAD.
4. Describing and analyzing positions adopted by two selected individuals (1 Doctor and
1 legal advisor)
Response about the question was collected from two people who are involved in this process
of PAD. A doctor and a legal advisor were involved in the study.
Response from doctor:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Ethics And Professional Practice
It is a question of ethical dilemma and different views can be gained regarding this matter.
However, I think PAD is an essential tool of end of life care. As a physician, it is my duty to
support and respect the autonomy of a patient and provide relief from all kinds of sufferings.
Moreover, the decision of PAD can be supported after analysis of patients clinical reports by
a third party government organization. It can only be implemented if no chance of revival is
left. However, in many incidents, it was seen that patients request death due to the pain of
continuous suffering, stress, and depression. Hence, firstly, it is the ethical duty of a
professional to provide proper care to reduce some pain.
Response from a legal advisor
It is a question of a serious ethical dilemma that occurs due to the nature of patient-physician
relationship. In society, the role of physician is to support a patient during illness rather than
devising strategies to kill them. However, this decision can be taken on the basis of the
patient's request, legal consent of court and vulnerability of the disease. It is the duty of
health professionals to provide high-quality palliative care and try to reduce suffering of
patients. A vital point in this ethical question is medicines cannot eliminate death rather it
cannot reduce all the sufferings.
Description and analysis of response
It can be seen that both selected professionals have provided different answers with respect to
the ethical question. Physician has supported this concept of death due to respecting the
patient's autonomy. This view can be supported by concepts of deontological theory. As
opined by Heintz et al. (2015), deontological theory states that humans need to be treated
with dignity and respect must be provided to everyone's views. Hence, request of patient
needs to be analyzed after evaluation of the request proper steps can be taken to fulfill the
wishes of patients. According to this ethical theory, it is the duty of a person to respect other
people's rights. Moreover, Molewijk, Hem & Pedersen (2015) contradicted that conflicts can
Ethics And Professional Practice
It is a question of ethical dilemma and different views can be gained regarding this matter.
However, I think PAD is an essential tool of end of life care. As a physician, it is my duty to
support and respect the autonomy of a patient and provide relief from all kinds of sufferings.
Moreover, the decision of PAD can be supported after analysis of patients clinical reports by
a third party government organization. It can only be implemented if no chance of revival is
left. However, in many incidents, it was seen that patients request death due to the pain of
continuous suffering, stress, and depression. Hence, firstly, it is the ethical duty of a
professional to provide proper care to reduce some pain.
Response from a legal advisor
It is a question of a serious ethical dilemma that occurs due to the nature of patient-physician
relationship. In society, the role of physician is to support a patient during illness rather than
devising strategies to kill them. However, this decision can be taken on the basis of the
patient's request, legal consent of court and vulnerability of the disease. It is the duty of
health professionals to provide high-quality palliative care and try to reduce suffering of
patients. A vital point in this ethical question is medicines cannot eliminate death rather it
cannot reduce all the sufferings.
Description and analysis of response
It can be seen that both selected professionals have provided different answers with respect to
the ethical question. Physician has supported this concept of death due to respecting the
patient's autonomy. This view can be supported by concepts of deontological theory. As
opined by Heintz et al. (2015), deontological theory states that humans need to be treated
with dignity and respect must be provided to everyone's views. Hence, request of patient
needs to be analyzed after evaluation of the request proper steps can be taken to fulfill the
wishes of patients. According to this ethical theory, it is the duty of a person to respect other
people's rights. Moreover, Molewijk, Hem & Pedersen (2015) contradicted that conflicts can
6
Ethics And Professional Practice
occur between duties and principles. The doctor has also mentioned that it is his its duty to
provide proper care. However, in the case of any conflicting situation, proper analysis of the
present condition of the patient and legal guidance from any government third party can also
be sought. This can help to eliminate any situation of dilemma.
The legal professional has given a very diplomatic answer regarding this ethical question. He
opposed the process of PAD but on the other hand, suggested that decisions can be taken on
the basis of physical condition of the patient. This is can be related to the theory of virtue
ethics. According to this ethical theory, decision-makers need to understand the virtue of
proper public relations and decisions must be made according to those virtues
(Pagecentertraining.psu.edu, 2018). Hence, a professional needs to approve the request of
PAD after proper analysis of vulnerability of the disease and achieving legal consent.
However, both the professionals have given priority of high-quality palliative care for
minimizing the suffering of patients. This is because many times patients, who are suffering
from chronic diseases makes, wish of death due to stress and depression. Regular
communication, proper motivation can help them to gain mental strength. This can help them
to have normal biological death rather than PAD.
5. Articulating professional and personal position, and potential challenges
Personal and professional positions of physicians are different in terms of perspectives. In
personal life, physicians understand the pain of patients who are suffering from chronic non-
curable diseases. They understand the point of view of patients towards PAD. As supported
by Amer (2019), physicians communicate with patients, who apply for PAD to understand
their ground of this decision. In-depth analysis of patients though helps them to understand
their perspectives towards death. On the other hand, their profession prevents them to assist
in suicide. As opined by Lucas, Van Wee & Maat (2016), doctors take an oath to save lives at
Ethics And Professional Practice
occur between duties and principles. The doctor has also mentioned that it is his its duty to
provide proper care. However, in the case of any conflicting situation, proper analysis of the
present condition of the patient and legal guidance from any government third party can also
be sought. This can help to eliminate any situation of dilemma.
The legal professional has given a very diplomatic answer regarding this ethical question. He
opposed the process of PAD but on the other hand, suggested that decisions can be taken on
the basis of physical condition of the patient. This is can be related to the theory of virtue
ethics. According to this ethical theory, decision-makers need to understand the virtue of
proper public relations and decisions must be made according to those virtues
(Pagecentertraining.psu.edu, 2018). Hence, a professional needs to approve the request of
PAD after proper analysis of vulnerability of the disease and achieving legal consent.
However, both the professionals have given priority of high-quality palliative care for
minimizing the suffering of patients. This is because many times patients, who are suffering
from chronic diseases makes, wish of death due to stress and depression. Regular
communication, proper motivation can help them to gain mental strength. This can help them
to have normal biological death rather than PAD.
5. Articulating professional and personal position, and potential challenges
Personal and professional positions of physicians are different in terms of perspectives. In
personal life, physicians understand the pain of patients who are suffering from chronic non-
curable diseases. They understand the point of view of patients towards PAD. As supported
by Amer (2019), physicians communicate with patients, who apply for PAD to understand
their ground of this decision. In-depth analysis of patients though helps them to understand
their perspectives towards death. On the other hand, their profession prevents them to assist
in suicide. As opined by Lucas, Van Wee & Maat (2016), doctors take an oath to save lives at
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Ethics And Professional Practice
the beginning of their career. Their dedication towards their duty and their ethics prevent
them to allow someone to die. A professional physician fights a battle in his mind before
taking part in PAD. They prioritize the pain of patients over their emotional barriers. As a
person, their morals prevent them to assist suicide and their morality allows them to take
decision on the favor of the applicant. According to Koçyiğit & Karadağ (2016), in both
personal and professional aspect, physicians respect the autonomy of patients regarding end
of their lives.
Several challenges are faced by physicians while making decision regarding PAD. Emotional
challenge is the main barrier to making a decision in favor of PAD. It can be overcome with
the cooperation from the patient and his or her family members. Another challenge is legal
consequences. Both patients and physicians face legal issues in case of PAD. As suggested by
Karsoho et al. (2016), it can be mitigated by following legal guidelines of the country.
Ethics And Professional Practice
the beginning of their career. Their dedication towards their duty and their ethics prevent
them to allow someone to die. A professional physician fights a battle in his mind before
taking part in PAD. They prioritize the pain of patients over their emotional barriers. As a
person, their morals prevent them to assist suicide and their morality allows them to take
decision on the favor of the applicant. According to Koçyiğit & Karadağ (2016), in both
personal and professional aspect, physicians respect the autonomy of patients regarding end
of their lives.
Several challenges are faced by physicians while making decision regarding PAD. Emotional
challenge is the main barrier to making a decision in favor of PAD. It can be overcome with
the cooperation from the patient and his or her family members. Another challenge is legal
consequences. Both patients and physicians face legal issues in case of PAD. As suggested by
Karsoho et al. (2016), it can be mitigated by following legal guidelines of the country.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Ethics And Professional Practice
Reference list
Amer, A. B. (2019). Understanding the Ethical Theories in Medical Practice. Open Journal of
Nursing, 9(2), 188-193. Retrieved from:
Appelbaum, P. S. (2016). Physician-assisted death for patients with mental disorders—
reasons for concern. JAMA psychiatry, 73(4), 325-326.Retrieved from:
Battin, M. P., Rhodes, R., & Silvers, A. (2015). Physician assisted suicide: expanding the
debate. Routledge.Retrieved from:
Frey, L. M., & Hans, J. D. (2016). Attitudes toward assisted suicide: Does family context
matter?. Archives of suicide research, 20(2), 250-264. Retrieved from:
Heintz, E., Lintamo, L., Hultcrantz, M., Jacobson, S., Levi, R., Munthe, C., ... & Sandman, L.
(2015). Framework for systematic identification of ethical aspects of healthcare
technologies: the SBU approach. International journal of technology assessment in
health care, 31(3), 124-130. Retrieved from:
Hudson, P., Hudson, R., Philip, J., Boughey, M., Kelly, B., & Hertogh, C. (2015). Legalizing
physician-assisted suicide and/or euthanasia: Pragmatic implications. Palliative &
supportive care, 13(5), 1399-1409. Retrieved from:
Karsoho, H., Fishman, J. R., Wright, D. K., & Macdonald, M. E. (2016). Suffering and
medicalization at the end of life: the case of physician-assisted dying. Social Science
& Medicine, 170, 188-196. Retrieved from:
Koçyiğit, M., & Karadağ, E. (2016). Developing an ethical tendencies scale based on the
theories of ethics. Turkish Journal of Business Ethics, 9(2), 297-307. Retrieved from:
Lucas, K., Van Wee, B., & Maat, K. (2016). A method to evaluate equitable accessibility:
combining ethical theories and accessibility-based approaches. Transportation, 43(3),
473-490. Retrieved from:
Ethics And Professional Practice
Reference list
Amer, A. B. (2019). Understanding the Ethical Theories in Medical Practice. Open Journal of
Nursing, 9(2), 188-193. Retrieved from:
Appelbaum, P. S. (2016). Physician-assisted death for patients with mental disorders—
reasons for concern. JAMA psychiatry, 73(4), 325-326.Retrieved from:
Battin, M. P., Rhodes, R., & Silvers, A. (2015). Physician assisted suicide: expanding the
debate. Routledge.Retrieved from:
Frey, L. M., & Hans, J. D. (2016). Attitudes toward assisted suicide: Does family context
matter?. Archives of suicide research, 20(2), 250-264. Retrieved from:
Heintz, E., Lintamo, L., Hultcrantz, M., Jacobson, S., Levi, R., Munthe, C., ... & Sandman, L.
(2015). Framework for systematic identification of ethical aspects of healthcare
technologies: the SBU approach. International journal of technology assessment in
health care, 31(3), 124-130. Retrieved from:
Hudson, P., Hudson, R., Philip, J., Boughey, M., Kelly, B., & Hertogh, C. (2015). Legalizing
physician-assisted suicide and/or euthanasia: Pragmatic implications. Palliative &
supportive care, 13(5), 1399-1409. Retrieved from:
Karsoho, H., Fishman, J. R., Wright, D. K., & Macdonald, M. E. (2016). Suffering and
medicalization at the end of life: the case of physician-assisted dying. Social Science
& Medicine, 170, 188-196. Retrieved from:
Koçyiğit, M., & Karadağ, E. (2016). Developing an ethical tendencies scale based on the
theories of ethics. Turkish Journal of Business Ethics, 9(2), 297-307. Retrieved from:
Lucas, K., Van Wee, B., & Maat, K. (2016). A method to evaluate equitable accessibility:
combining ethical theories and accessibility-based approaches. Transportation, 43(3),
473-490. Retrieved from:
9
Ethics And Professional Practice
Molewijk, B., Hem, M. H., & Pedersen, R. (2015). Dealing with ethical challenges: a focus
group study with professionals in mental health care. BMC medical ethics, 16(1), 4.
Retrieved from:
Pagecentertraining.psu.edu (2018), Ethical theories, [Online], Retrieved on 24th July 2019
from:
Petrillo, L. A., Dzeng, E., Harrison, K. L., Forbes, L., Scribner, B., & Koenig, B. A. (2017).
How California prepared for implementation of physician-assisted death: a
primer. American journal of public health, 107(6), 883-888.Retrieved from:
Ethics And Professional Practice
Molewijk, B., Hem, M. H., & Pedersen, R. (2015). Dealing with ethical challenges: a focus
group study with professionals in mental health care. BMC medical ethics, 16(1), 4.
Retrieved from:
Pagecentertraining.psu.edu (2018), Ethical theories, [Online], Retrieved on 24th July 2019
from:
Petrillo, L. A., Dzeng, E., Harrison, K. L., Forbes, L., Scribner, B., & Koenig, B. A. (2017).
How California prepared for implementation of physician-assisted death: a
primer. American journal of public health, 107(6), 883-888.Retrieved from:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Ethics And Professional Practice
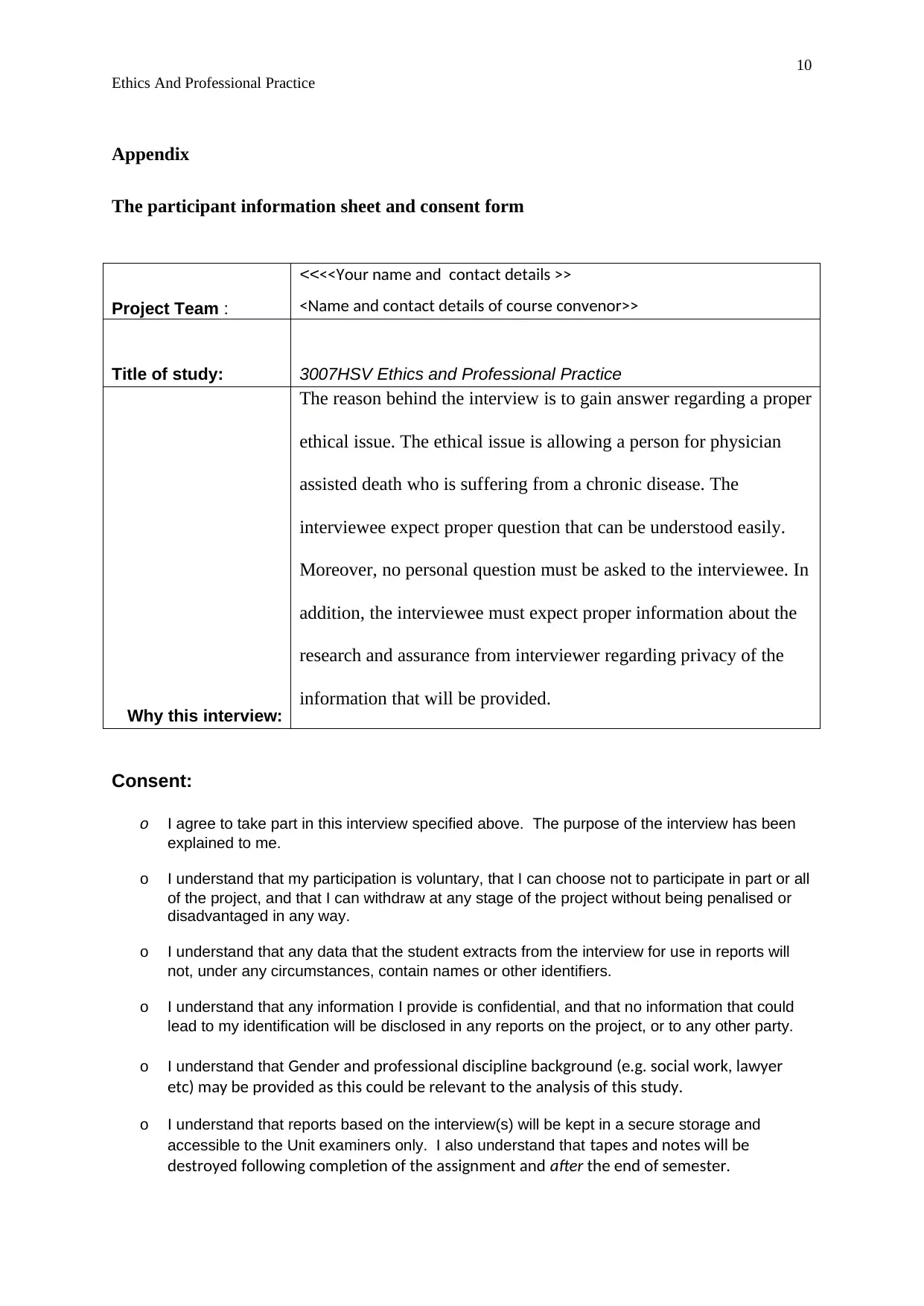
Appendix
The participant information sheet and consent form
Project Team :
<<<<Your name and contact details >>
<Name and contact details of course convenor>>
Title of study: 3007HSV Ethics and Professional Practice
Why this interview:
The reason behind the interview is to gain answer regarding a proper
ethical issue. The ethical issue is allowing a person for physician
assisted death who is suffering from a chronic disease. The
interviewee expect proper question that can be understood easily.
Moreover, no personal question must be asked to the interviewee. In
addition, the interviewee must expect proper information about the
research and assurance from interviewer regarding privacy of the
information that will be provided.
Consent:
o I agree to take part in this interview specified above. The purpose of the interview has been
explained to me.
o I understand that my participation is voluntary, that I can choose not to participate in part or all
of the project, and that I can withdraw at any stage of the project without being penalised or
disadvantaged in any way.
o I understand that any data that the student extracts from the interview for use in reports will
not, under any circumstances, contain names or other identifiers.
o I understand that any information I provide is confidential, and that no information that could
lead to my identification will be disclosed in any reports on the project, or to any other party.
o I understand that Gender and professional discipline background (e.g. social work, lawyer
etc) may be provided as this could be relevant to the analysis of this study.
o I understand that reports based on the interview(s) will be kept in a secure storage and
accessible to the Unit examiners only. I also understand that tapes and notes will be
destroyed following completion of the assignment and after the end of semester.
Ethics And Professional Practice
Appendix
The participant information sheet and consent form
Project Team :
<<<<Your name and contact details >>
<Name and contact details of course convenor>>
Title of study: 3007HSV Ethics and Professional Practice
Why this interview:
The reason behind the interview is to gain answer regarding a proper
ethical issue. The ethical issue is allowing a person for physician
assisted death who is suffering from a chronic disease. The
interviewee expect proper question that can be understood easily.
Moreover, no personal question must be asked to the interviewee. In
addition, the interviewee must expect proper information about the
research and assurance from interviewer regarding privacy of the
information that will be provided.
Consent:
o I agree to take part in this interview specified above. The purpose of the interview has been
explained to me.
o I understand that my participation is voluntary, that I can choose not to participate in part or all
of the project, and that I can withdraw at any stage of the project without being penalised or
disadvantaged in any way.
o I understand that any data that the student extracts from the interview for use in reports will
not, under any circumstances, contain names or other identifiers.
o I understand that any information I provide is confidential, and that no information that could
lead to my identification will be disclosed in any reports on the project, or to any other party.
o I understand that Gender and professional discipline background (e.g. social work, lawyer
etc) may be provided as this could be relevant to the analysis of this study.
o I understand that reports based on the interview(s) will be kept in a secure storage and
accessible to the Unit examiners only. I also understand that tapes and notes will be
destroyed following completion of the assignment and after the end of semester.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
Ethics And Professional Practice
Participant’s name: XXXX
Signature: XXXX
Date: 25th July 2019
Interviewer’s name: XXXX
Ethics And Professional Practice
Participant’s name: XXXX
Signature: XXXX
Date: 25th July 2019
Interviewer’s name: XXXX
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





