Pierre Robin Syndrome Case Study: A Reverse Case Study Analysis
VerifiedAdded on 2022/11/13
|6
|1800
|192
Case Study
AI Summary
This case study examines Pierre Robin Syndrome (PRS), a congenital condition characterized by micrognathia, cleft palate, and glossoptosis, presenting a reverse case study approach. The assignment traces the diagnosis backward, exploring the aetiology, pathophysiology, diagnostic tests, symptoms, and test results observed in an infant. The study delves into the embryological origins of the condition, detailing normal development and deviations in PRS. The case study outlines the mechanical theory, neurological maturation, and rhombencephalic dysneurulation as contributing factors to the pathophysiology of PRS. It includes a case presentation of a 7-month-old infant, detailing symptoms, performed tests, and treatment approaches. Dental management, including caries prevention and orthodontic intervention, is also discussed, emphasizing the need for multidisciplinary care and early intervention for improved quality of life.
Pierre Robin syndrome Case Study Assessment
By
Student’s Name
Course
Tutor
Institution
Date
By
Student’s Name
Course
Tutor
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Introduction about the disease
Pierre Robin syndrome was first described by Menard and Lannelongue in 1891 among two patients
reported with micrognathia, cleft palate, and occurrence of retroglossoptosis. In the year 1926, author
Pierre Robin made the first case publication on an infant with complete syndrome infestation. In the
year 1974, the triad transformed to Pierre Robin syndrome, being synonymous with morphogenesis
errors which are present and caused by single etiology. A study published by Breugem and
Courtemanche (2009), showed the classical confusion occurring in the classification of this sequence.
The survey was undertaken in his study entailed various aspects such as the difference between
retrognathia and micrognathia and occurrence of cleft type entail the U versus the V-shaped
occurrences. The various definition of this sequence has been published with varied opinions on Robin
Sequence classification (Oliveira &Domingues, 2015).
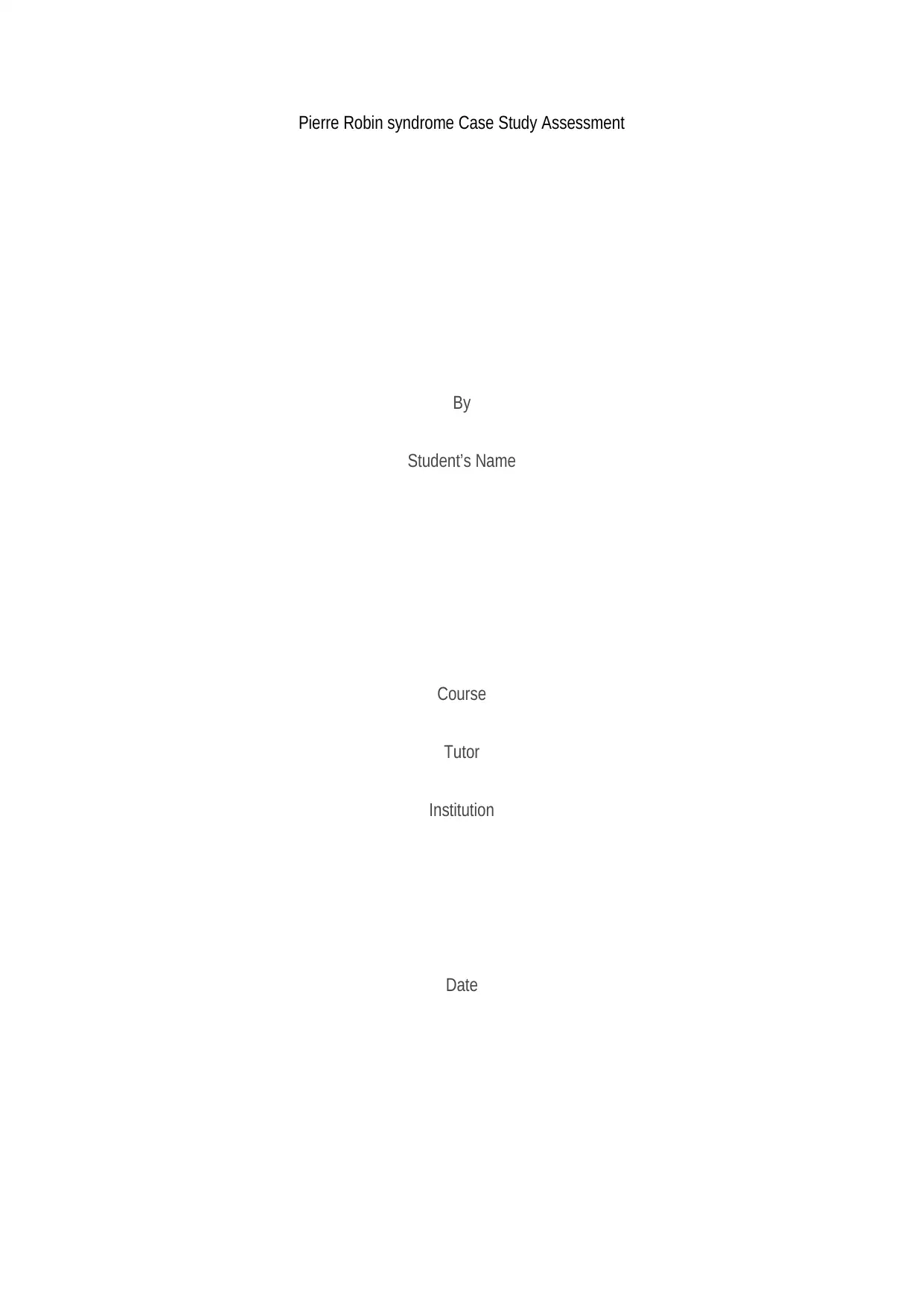
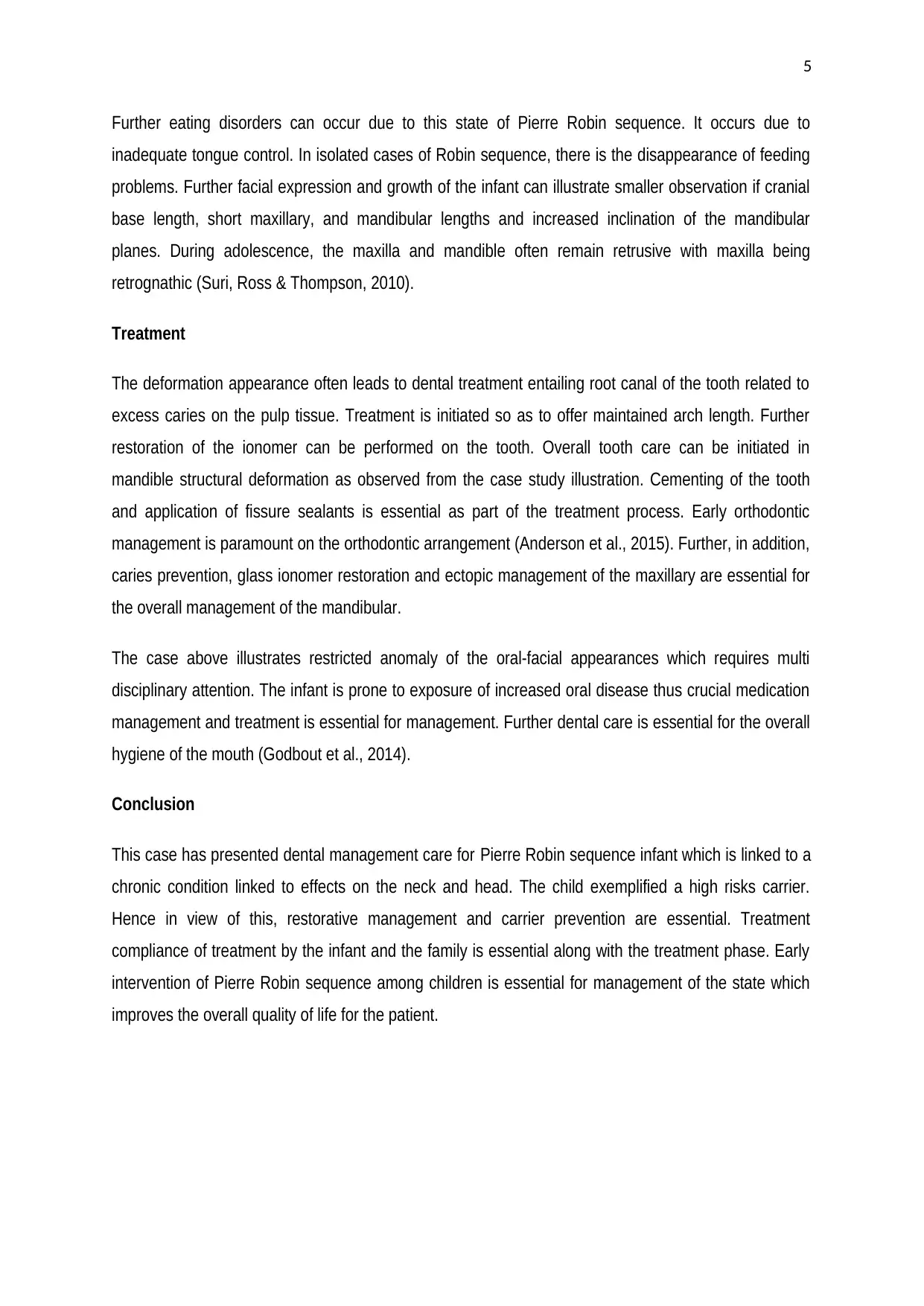
A typical image depicting this disease can be shown in figure 1 image showcasing a 5-month old baby
with the occurrence of severe micrognathia
courtesy of Tewfik, Der & Kaloustian (2003). The
heterogeneity of the birth defect has an occurrence
of approximately 1 per 8500 live births with a male:
female ratio. Its etiological background underpins
the autosomal recessive inheritances with X-linked
variance been associated with cardiac
malformation and club feet.
Pathophysiology
The occurrence of this disease has been explained in three pathophysiological theories. The first theory
refers to the Mechanical Theory, exhibiting the most accepted theory. The occurrence of mandibular
hypoplasia often occurs during the 7th and 11th week of the gestation period. This allows the tongue to
be on the high side of the oral cavity leading to a cleft in the palate thus preventing palatal shelves
closure. This elaborates the U shaped cleft with the absence of associated cleft lip. In this case,
Oligohydramnios could have a significant role in this process due to the lack of amniotic fluid leading to
deformation of the china and impact action between the palatal shelves of the tongue.
The second theory entails the neurological maturation. The accruing delay in the maturation process
has been observed on electromyography occurring on the tongue muscles, the pharyngeal sites and
the palate leading to delay on hypoglossal conduction nerves.
Figure 1Image of Robin sequence patient and severe
micrognathia
Introduction about the disease
Pierre Robin syndrome was first described by Menard and Lannelongue in 1891 among two patients
reported with micrognathia, cleft palate, and occurrence of retroglossoptosis. In the year 1926, author
Pierre Robin made the first case publication on an infant with complete syndrome infestation. In the
year 1974, the triad transformed to Pierre Robin syndrome, being synonymous with morphogenesis
errors which are present and caused by single etiology. A study published by Breugem and
Courtemanche (2009), showed the classical confusion occurring in the classification of this sequence.
The survey was undertaken in his study entailed various aspects such as the difference between
retrognathia and micrognathia and occurrence of cleft type entail the U versus the V-shaped
occurrences. The various definition of this sequence has been published with varied opinions on Robin
Sequence classification (Oliveira &Domingues, 2015).
A typical image depicting this disease can be shown in figure 1 image showcasing a 5-month old baby
with the occurrence of severe micrognathia
courtesy of Tewfik, Der & Kaloustian (2003). The
heterogeneity of the birth defect has an occurrence
of approximately 1 per 8500 live births with a male:
female ratio. Its etiological background underpins
the autosomal recessive inheritances with X-linked
variance been associated with cardiac
malformation and club feet.
Pathophysiology
The occurrence of this disease has been explained in three pathophysiological theories. The first theory
refers to the Mechanical Theory, exhibiting the most accepted theory. The occurrence of mandibular
hypoplasia often occurs during the 7th and 11th week of the gestation period. This allows the tongue to
be on the high side of the oral cavity leading to a cleft in the palate thus preventing palatal shelves
closure. This elaborates the U shaped cleft with the absence of associated cleft lip. In this case,
Oligohydramnios could have a significant role in this process due to the lack of amniotic fluid leading to
deformation of the china and impact action between the palatal shelves of the tongue.
The second theory entails the neurological maturation. The accruing delay in the maturation process
has been observed on electromyography occurring on the tongue muscles, the pharyngeal sites and
the palate leading to delay on hypoglossal conduction nerves.
Figure 1Image of Robin sequence patient and severe
micrognathia
3
The last theory explaining the pathophysiology entails the rhombencephalic dysneurulation, this
explains the functional process of motor regulation occurring on the rhombencephalon linked to
ontogenesis (Højland et al., 2018).
Case study; case presentation
This case study involves 7 months old infant referred with cleft lip and palate. The infant was born at
29th gestation week with a weight of 1.118 kg and diagnosed with Pierre Robin Syndrome. In the initial
screening of the body, the overall ultrasound examination showed small and mandible backward.
During birth, he was netibulated and admitted to the neonatal intensive care unit admitted there for 3
months. A surgical tracheotomy was performed after twenty days after birth due to the severe
respiratory occurrence. At 3 months post birth, the infant was inserted with gasostrom due to feeding
difficulties and the first year of life she developed various complications related to fever spurts and
challenges on breathing. Surgery process was undertaken for cleft palate. At 18 months, respiratory
tubes were removed and at 2 years, gastrostomy was removed. The infant has been experiencing
hearing loss and underwent various surgical tubing challenges.
The infant dental history brushing of has on been well till age 7. Habitual habits entail regular intake of
sweets and sugary drinks.
–Tests performed
Facial asymmetry did
Intra oral soft tissue analysis
Dentition assessment
–Test Result
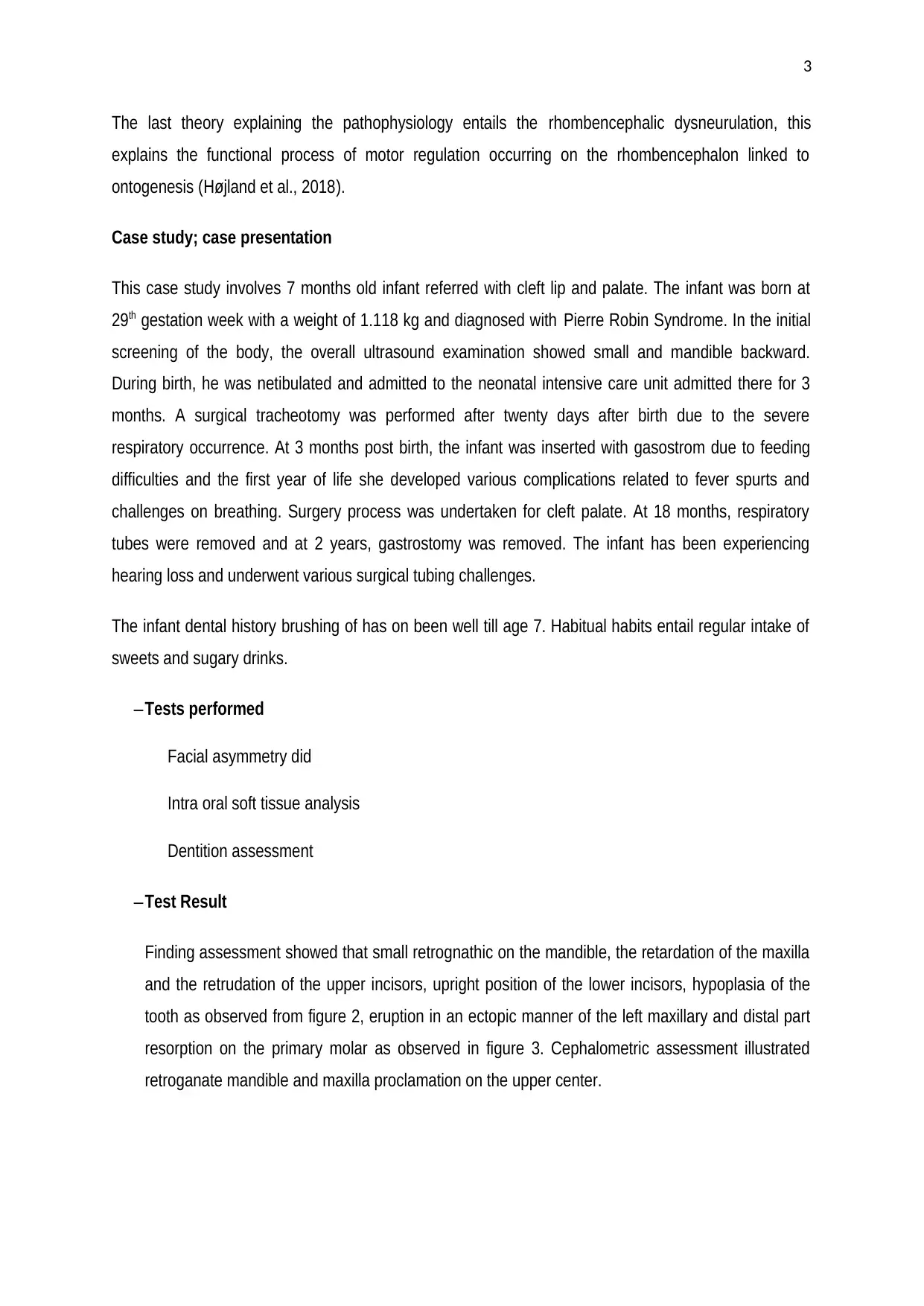
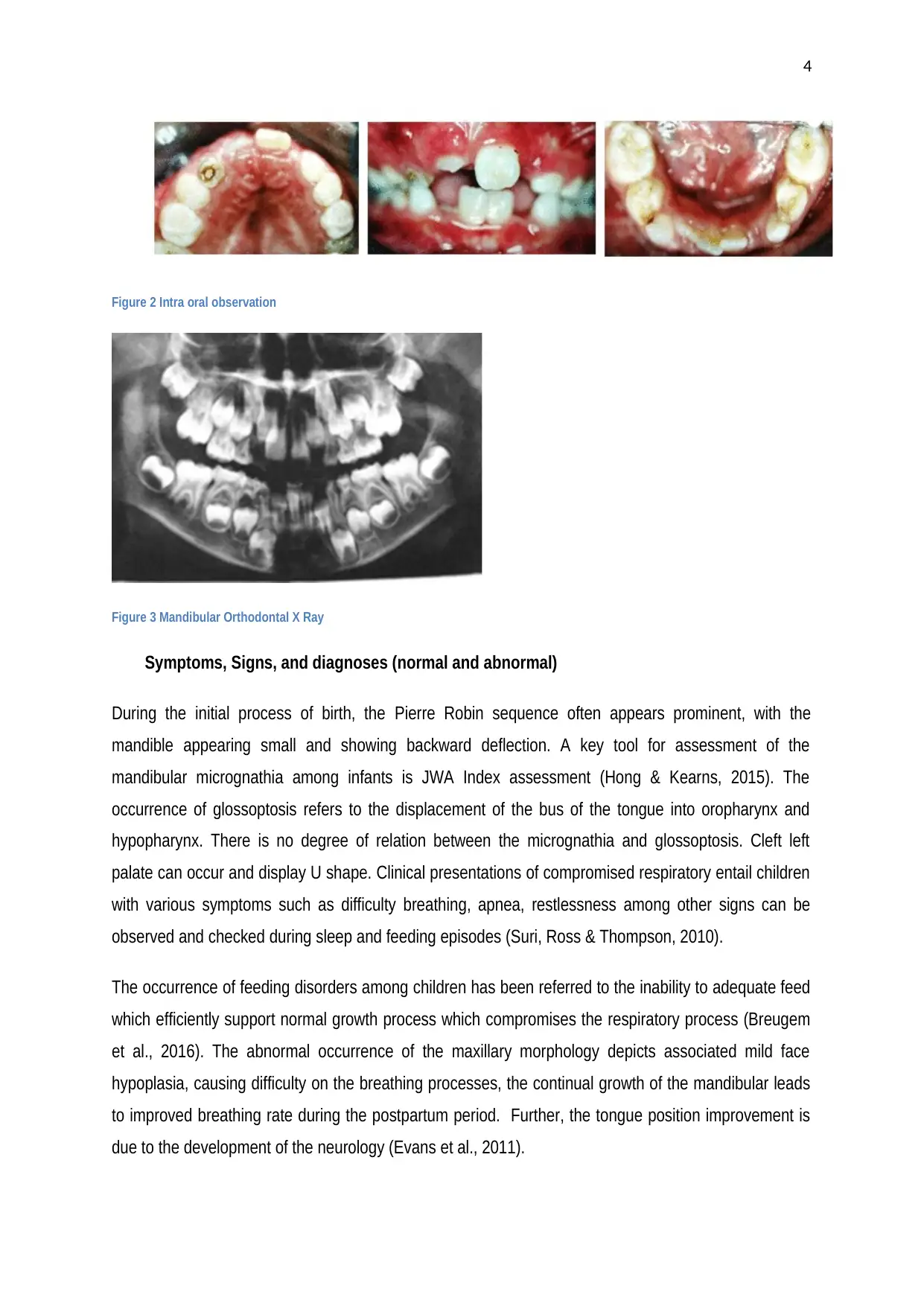
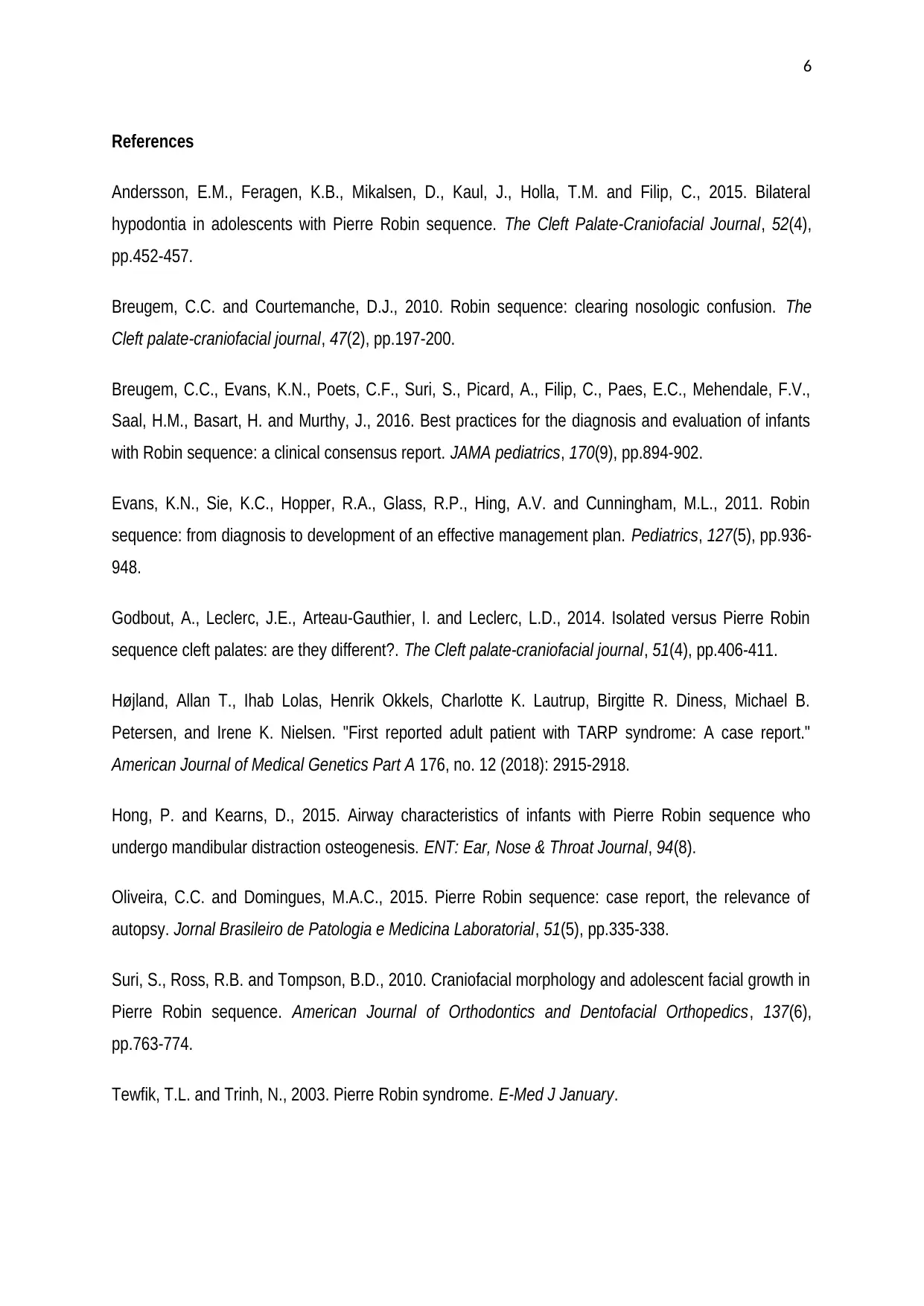
Finding assessment showed that small retrognathic on the mandible, the retardation of the maxilla
and the retrudation of the upper incisors, upright position of the lower incisors, hypoplasia of the
tooth as observed from figure 2, eruption in an ectopic manner of the left maxillary and distal part
resorption on the primary molar as observed in figure 3. Cephalometric assessment illustrated
retroganate mandible and maxilla proclamation on the upper center.
The last theory explaining the pathophysiology entails the rhombencephalic dysneurulation, this
explains the functional process of motor regulation occurring on the rhombencephalon linked to
ontogenesis (Højland et al., 2018).
Case study; case presentation
This case study involves 7 months old infant referred with cleft lip and palate. The infant was born at
29th gestation week with a weight of 1.118 kg and diagnosed with Pierre Robin Syndrome. In the initial
screening of the body, the overall ultrasound examination showed small and mandible backward.
During birth, he was netibulated and admitted to the neonatal intensive care unit admitted there for 3
months. A surgical tracheotomy was performed after twenty days after birth due to the severe
respiratory occurrence. At 3 months post birth, the infant was inserted with gasostrom due to feeding
difficulties and the first year of life she developed various complications related to fever spurts and
challenges on breathing. Surgery process was undertaken for cleft palate. At 18 months, respiratory
tubes were removed and at 2 years, gastrostomy was removed. The infant has been experiencing
hearing loss and underwent various surgical tubing challenges.
The infant dental history brushing of has on been well till age 7. Habitual habits entail regular intake of
sweets and sugary drinks.
–Tests performed
Facial asymmetry did
Intra oral soft tissue analysis
Dentition assessment
–Test Result
Finding assessment showed that small retrognathic on the mandible, the retardation of the maxilla
and the retrudation of the upper incisors, upright position of the lower incisors, hypoplasia of the
tooth as observed from figure 2, eruption in an ectopic manner of the left maxillary and distal part
resorption on the primary molar as observed in figure 3. Cephalometric assessment illustrated
retroganate mandible and maxilla proclamation on the upper center.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Figure 2 Intra oral observation
Figure 3 Mandibular Orthodontal X Ray
Symptoms, Signs, and diagnoses (normal and abnormal)
During the initial process of birth, the Pierre Robin sequence often appears prominent, with the
mandible appearing small and showing backward deflection. A key tool for assessment of the
mandibular micrognathia among infants is JWA Index assessment (Hong & Kearns, 2015). The
occurrence of glossoptosis refers to the displacement of the bus of the tongue into oropharynx and
hypopharynx. There is no degree of relation between the micrognathia and glossoptosis. Cleft left
palate can occur and display U shape. Clinical presentations of compromised respiratory entail children
with various symptoms such as difficulty breathing, apnea, restlessness among other signs can be
observed and checked during sleep and feeding episodes (Suri, Ross & Thompson, 2010).
The occurrence of feeding disorders among children has been referred to the inability to adequate feed
which efficiently support normal growth process which compromises the respiratory process (Breugem
et al., 2016). The abnormal occurrence of the maxillary morphology depicts associated mild face
hypoplasia, causing difficulty on the breathing processes, the continual growth of the mandibular leads
to improved breathing rate during the postpartum period. Further, the tongue position improvement is
due to the development of the neurology (Evans et al., 2011).
Figure 2 Intra oral observation
Figure 3 Mandibular Orthodontal X Ray
Symptoms, Signs, and diagnoses (normal and abnormal)
During the initial process of birth, the Pierre Robin sequence often appears prominent, with the
mandible appearing small and showing backward deflection. A key tool for assessment of the
mandibular micrognathia among infants is JWA Index assessment (Hong & Kearns, 2015). The
occurrence of glossoptosis refers to the displacement of the bus of the tongue into oropharynx and
hypopharynx. There is no degree of relation between the micrognathia and glossoptosis. Cleft left
palate can occur and display U shape. Clinical presentations of compromised respiratory entail children
with various symptoms such as difficulty breathing, apnea, restlessness among other signs can be
observed and checked during sleep and feeding episodes (Suri, Ross & Thompson, 2010).
The occurrence of feeding disorders among children has been referred to the inability to adequate feed
which efficiently support normal growth process which compromises the respiratory process (Breugem
et al., 2016). The abnormal occurrence of the maxillary morphology depicts associated mild face
hypoplasia, causing difficulty on the breathing processes, the continual growth of the mandibular leads
to improved breathing rate during the postpartum period. Further, the tongue position improvement is
due to the development of the neurology (Evans et al., 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Further eating disorders can occur due to this state of Pierre Robin sequence. It occurs due to
inadequate tongue control. In isolated cases of Robin sequence, there is the disappearance of feeding
problems. Further facial expression and growth of the infant can illustrate smaller observation if cranial
base length, short maxillary, and mandibular lengths and increased inclination of the mandibular
planes. During adolescence, the maxilla and mandible often remain retrusive with maxilla being
retrognathic (Suri, Ross & Thompson, 2010).
Treatment
The deformation appearance often leads to dental treatment entailing root canal of the tooth related to
excess caries on the pulp tissue. Treatment is initiated so as to offer maintained arch length. Further
restoration of the ionomer can be performed on the tooth. Overall tooth care can be initiated in
mandible structural deformation as observed from the case study illustration. Cementing of the tooth
and application of fissure sealants is essential as part of the treatment process. Early orthodontic
management is paramount on the orthodontic arrangement (Anderson et al., 2015). Further, in addition,
caries prevention, glass ionomer restoration and ectopic management of the maxillary are essential for
the overall management of the mandibular.
The case above illustrates restricted anomaly of the oral-facial appearances which requires multi
disciplinary attention. The infant is prone to exposure of increased oral disease thus crucial medication
management and treatment is essential for management. Further dental care is essential for the overall
hygiene of the mouth (Godbout et al., 2014).
Conclusion
This case has presented dental management care for Pierre Robin sequence infant which is linked to a
chronic condition linked to effects on the neck and head. The child exemplified a high risks carrier.
Hence in view of this, restorative management and carrier prevention are essential. Treatment
compliance of treatment by the infant and the family is essential along with the treatment phase. Early
intervention of Pierre Robin sequence among children is essential for management of the state which
improves the overall quality of life for the patient.
Further eating disorders can occur due to this state of Pierre Robin sequence. It occurs due to
inadequate tongue control. In isolated cases of Robin sequence, there is the disappearance of feeding
problems. Further facial expression and growth of the infant can illustrate smaller observation if cranial
base length, short maxillary, and mandibular lengths and increased inclination of the mandibular
planes. During adolescence, the maxilla and mandible often remain retrusive with maxilla being
retrognathic (Suri, Ross & Thompson, 2010).
Treatment
The deformation appearance often leads to dental treatment entailing root canal of the tooth related to
excess caries on the pulp tissue. Treatment is initiated so as to offer maintained arch length. Further
restoration of the ionomer can be performed on the tooth. Overall tooth care can be initiated in
mandible structural deformation as observed from the case study illustration. Cementing of the tooth
and application of fissure sealants is essential as part of the treatment process. Early orthodontic
management is paramount on the orthodontic arrangement (Anderson et al., 2015). Further, in addition,
caries prevention, glass ionomer restoration and ectopic management of the maxillary are essential for
the overall management of the mandibular.
The case above illustrates restricted anomaly of the oral-facial appearances which requires multi
disciplinary attention. The infant is prone to exposure of increased oral disease thus crucial medication
management and treatment is essential for management. Further dental care is essential for the overall
hygiene of the mouth (Godbout et al., 2014).
Conclusion
This case has presented dental management care for Pierre Robin sequence infant which is linked to a
chronic condition linked to effects on the neck and head. The child exemplified a high risks carrier.
Hence in view of this, restorative management and carrier prevention are essential. Treatment
compliance of treatment by the infant and the family is essential along with the treatment phase. Early
intervention of Pierre Robin sequence among children is essential for management of the state which
improves the overall quality of life for the patient.
6
References
Andersson, E.M., Feragen, K.B., Mikalsen, D., Kaul, J., Holla, T.M. and Filip, C., 2015. Bilateral
hypodontia in adolescents with Pierre Robin sequence. The Cleft Palate-Craniofacial Journal, 52(4),
pp.452-457.
Breugem, C.C. and Courtemanche, D.J., 2010. Robin sequence: clearing nosologic confusion. The
Cleft palate-craniofacial journal, 47(2), pp.197-200.
Breugem, C.C., Evans, K.N., Poets, C.F., Suri, S., Picard, A., Filip, C., Paes, E.C., Mehendale, F.V.,
Saal, H.M., Basart, H. and Murthy, J., 2016. Best practices for the diagnosis and evaluation of infants
with Robin sequence: a clinical consensus report. JAMA pediatrics, 170(9), pp.894-902.
Evans, K.N., Sie, K.C., Hopper, R.A., Glass, R.P., Hing, A.V. and Cunningham, M.L., 2011. Robin
sequence: from diagnosis to development of an effective management plan. Pediatrics, 127(5), pp.936-
948.
Godbout, A., Leclerc, J.E., Arteau-Gauthier, I. and Leclerc, L.D., 2014. Isolated versus Pierre Robin
sequence cleft palates: are they different?. The Cleft palate-craniofacial journal, 51(4), pp.406-411.
Højland, Allan T., Ihab Lolas, Henrik Okkels, Charlotte K. Lautrup, Birgitte R. Diness, Michael B.
Petersen, and Irene K. Nielsen. "First reported adult patient with TARP syndrome: A case report."
American Journal of Medical Genetics Part A 176, no. 12 (2018): 2915-2918.
Hong, P. and Kearns, D., 2015. Airway characteristics of infants with Pierre Robin sequence who
undergo mandibular distraction osteogenesis. ENT: Ear, Nose & Throat Journal, 94(8).
Oliveira, C.C. and Domingues, M.A.C., 2015. Pierre Robin sequence: case report, the relevance of
autopsy. Jornal Brasileiro de Patologia e Medicina Laboratorial, 51(5), pp.335-338.
Suri, S., Ross, R.B. and Tompson, B.D., 2010. Craniofacial morphology and adolescent facial growth in
Pierre Robin sequence. American Journal of Orthodontics and Dentofacial Orthopedics, 137(6),
pp.763-774.
Tewfik, T.L. and Trinh, N., 2003. Pierre Robin syndrome. E-Med J January.
References
Andersson, E.M., Feragen, K.B., Mikalsen, D., Kaul, J., Holla, T.M. and Filip, C., 2015. Bilateral
hypodontia in adolescents with Pierre Robin sequence. The Cleft Palate-Craniofacial Journal, 52(4),
pp.452-457.
Breugem, C.C. and Courtemanche, D.J., 2010. Robin sequence: clearing nosologic confusion. The
Cleft palate-craniofacial journal, 47(2), pp.197-200.
Breugem, C.C., Evans, K.N., Poets, C.F., Suri, S., Picard, A., Filip, C., Paes, E.C., Mehendale, F.V.,
Saal, H.M., Basart, H. and Murthy, J., 2016. Best practices for the diagnosis and evaluation of infants
with Robin sequence: a clinical consensus report. JAMA pediatrics, 170(9), pp.894-902.
Evans, K.N., Sie, K.C., Hopper, R.A., Glass, R.P., Hing, A.V. and Cunningham, M.L., 2011. Robin
sequence: from diagnosis to development of an effective management plan. Pediatrics, 127(5), pp.936-
948.
Godbout, A., Leclerc, J.E., Arteau-Gauthier, I. and Leclerc, L.D., 2014. Isolated versus Pierre Robin
sequence cleft palates: are they different?. The Cleft palate-craniofacial journal, 51(4), pp.406-411.
Højland, Allan T., Ihab Lolas, Henrik Okkels, Charlotte K. Lautrup, Birgitte R. Diness, Michael B.
Petersen, and Irene K. Nielsen. "First reported adult patient with TARP syndrome: A case report."
American Journal of Medical Genetics Part A 176, no. 12 (2018): 2915-2918.
Hong, P. and Kearns, D., 2015. Airway characteristics of infants with Pierre Robin sequence who
undergo mandibular distraction osteogenesis. ENT: Ear, Nose & Throat Journal, 94(8).
Oliveira, C.C. and Domingues, M.A.C., 2015. Pierre Robin sequence: case report, the relevance of
autopsy. Jornal Brasileiro de Patologia e Medicina Laboratorial, 51(5), pp.335-338.
Suri, S., Ross, R.B. and Tompson, B.D., 2010. Craniofacial morphology and adolescent facial growth in
Pierre Robin sequence. American Journal of Orthodontics and Dentofacial Orthopedics, 137(6),
pp.763-774.
Tewfik, T.L. and Trinh, N., 2003. Pierre Robin syndrome. E-Med J January.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.