An Advocacy Report on Poor Health Services Amongst Indigenous Society
VerifiedAdded on 2022/10/04
|17
|4588
|15
Report
AI Summary
This report examines the poor health services experienced by Indigenous communities in Australia, highlighting significant disparities in health outcomes compared to the non-Indigenous population. It delves into the social determinants of health, including socioeconomic factors, environmental influences, and cultural behaviors, which contribute to health inequalities. The report discusses the barriers to effective healthcare, such as prejudice, intercultural misunderstandings, and inadequate transport. It explores health outcomes, including poor mental health, communicable diseases, malnutrition, and increased disaster vulnerability. The report also analyzes the impact of these inequalities on life expectancy and child mortality rates, referencing data from the Australian Institute of Health and Welfare. It concludes by emphasizing the need for improved healthcare access and culturally sensitive services to address the significant health challenges faced by Indigenous Australians.

Running head: POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 1
Poor Health Services Amongst Indigenous Society
Students Name
Institution Affiliation
Poor Health Services Amongst Indigenous Society
Students Name
Institution Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 2
Introduction
Different mortality and morbidity rates among the indigenous and non-indigenous
communities in Australia have been well documented and continue to exist despite government
funding that was dedicated to solving the challenge. The life expectancy of the indigenous
Australian communities is about ten years less compared to that of other Australians. The
disparity in the life expectancy and the health status between the two is attributed to various
complex issues including, social-economic influences, racism, and dispossession, as well as
transgenerational negative impacts of colonization. This paper will discuss poor health services
amongst Indigenous society in Australia.
Social Determinants of Health the Indigenous Population
The health of the Aboriginal and Torres Strait Islander families of Australia is influenced
by complex interactions ranging from their behavior, biological, environmental factors, and
social-cultural context that they live in (Waterworth, Pescud, Braham, Dimmock & Rosenberg,
2015). The factors have significant consequences for the health of these populations as they
serve as enablers and barriers to the health and wellbeing of the communities (Gibson et al.,
2015). It is essential to define the influences of the health disparities among the populations to
put into place measures that can solve the issue (Mitrou, Cooke, Lawrence, Povah, Mobilia,
Guimond & Zubrick, 2014).
Socioeconomic influence is the primary factor that is associated with health disparity in
the indigenous communities in Australia. The social, economic status of this population is
identified by the state in which the community dwells in, education levels, unemployment, poor
housing and inadequate income that are determined to correlate with the level of health
Introduction
Different mortality and morbidity rates among the indigenous and non-indigenous
communities in Australia have been well documented and continue to exist despite government
funding that was dedicated to solving the challenge. The life expectancy of the indigenous
Australian communities is about ten years less compared to that of other Australians. The
disparity in the life expectancy and the health status between the two is attributed to various
complex issues including, social-economic influences, racism, and dispossession, as well as
transgenerational negative impacts of colonization. This paper will discuss poor health services
amongst Indigenous society in Australia.
Social Determinants of Health the Indigenous Population
The health of the Aboriginal and Torres Strait Islander families of Australia is influenced
by complex interactions ranging from their behavior, biological, environmental factors, and
social-cultural context that they live in (Waterworth, Pescud, Braham, Dimmock & Rosenberg,
2015). The factors have significant consequences for the health of these populations as they
serve as enablers and barriers to the health and wellbeing of the communities (Gibson et al.,
2015). It is essential to define the influences of the health disparities among the populations to
put into place measures that can solve the issue (Mitrou, Cooke, Lawrence, Povah, Mobilia,
Guimond & Zubrick, 2014).
Socioeconomic influence is the primary factor that is associated with health disparity in
the indigenous communities in Australia. The social, economic status of this population is
identified by the state in which the community dwells in, education levels, unemployment, poor
housing and inadequate income that are determined to correlate with the level of health
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 3
challenges and further influence lifestyles that dispose the communities to injuries and illnesses
(Reading & Greenwood, 2018). The indigenous community lost sovereignty, land, waterways,
and customary laws that have contributed to the oppression of material and spiritual with
increased disease susceptibility.
The lack of a healthy environment in terms of water supply, housing, infrastructure,
personal hygiene waste disposal, food security, among others, are significant health determinants
of an individual (Reading & Greenwood, 2018: Greenwood, De Leeuw, Lindsay & Reading,
2015). The indigenous communities of Australia dwell in a rural environment where there are
limited policies that govern the management of the environment, which puts the population at
risk of disease and injury. The lack of amenities and facilities that promote and influence better
healthy living is attributed to e development of disorders that are linked to the environmental
factors.
The social, cultural, and health behaviors of an individual contribute significantly to their
health. Due to lack of employment and economic development among the indigenous groups, the
members are likely to indulge in activities that are considered the risk or have significant health
implications to the individuals (Clifford, McCalman, Bainbridge & Tsey, 2015). Substances use,
for instance, alcohol and smoking, have significant impacts on the health of not only user but
also the family and society at large (Greenwood et al., 2015). The indigenous communities have
limited access to facilities that ensures immunization against extreme conditions, which
consequently affects their health (Neumayer, 2013).
The indigenous societies are likely to be impacted by disasters, unlike the rest of the
population due to unsustainable development practices, poverty, environmental degradation, and
climate variability (Eversole, McNeish & Cimadamore, 2013). The factors are attributed to an
challenges and further influence lifestyles that dispose the communities to injuries and illnesses
(Reading & Greenwood, 2018). The indigenous community lost sovereignty, land, waterways,
and customary laws that have contributed to the oppression of material and spiritual with
increased disease susceptibility.
The lack of a healthy environment in terms of water supply, housing, infrastructure,
personal hygiene waste disposal, food security, among others, are significant health determinants
of an individual (Reading & Greenwood, 2018: Greenwood, De Leeuw, Lindsay & Reading,
2015). The indigenous communities of Australia dwell in a rural environment where there are
limited policies that govern the management of the environment, which puts the population at
risk of disease and injury. The lack of amenities and facilities that promote and influence better
healthy living is attributed to e development of disorders that are linked to the environmental
factors.
The social, cultural, and health behaviors of an individual contribute significantly to their
health. Due to lack of employment and economic development among the indigenous groups, the
members are likely to indulge in activities that are considered the risk or have significant health
implications to the individuals (Clifford, McCalman, Bainbridge & Tsey, 2015). Substances use,
for instance, alcohol and smoking, have significant impacts on the health of not only user but
also the family and society at large (Greenwood et al., 2015). The indigenous communities have
limited access to facilities that ensures immunization against extreme conditions, which
consequently affects their health (Neumayer, 2013).
The indigenous societies are likely to be impacted by disasters, unlike the rest of the
population due to unsustainable development practices, poverty, environmental degradation, and
climate variability (Eversole, McNeish & Cimadamore, 2013). The factors are attributed to an
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 4
increased risk of injuries. The environment influences are linked to diseases and complications
that lead to health deterioration of the community.
Health Inequalities in Indigenous Communities
There various factors that have been defined as barriers to effective and efficient health
promotion services to the indigenous communities. According to healthcare practitioners,
standards of values and care are meant to offer equity and social proficiency (Browne et al.,
2016). However, there is conclusive evidence that indicates that medical practitioners are not
excepted from prejudice, which leads to culturally incentive healthcare services (Artuso, Cargo,
Brown & Daniel, 2013). The negative prejudice against the minority communities is a
significant barrier to the indigenous communities (Gibson et al., 2015). Intercultural
misunderstandings are also attributed to barriers to adequate health among the indigenous groups
in Australia. The infrequency of public transport, inadequate transport networks, and distance
from healthcare facilities is a significant barrier to the health inequalities among the indigenous
groups (Gibson et al., 2015). Due to the poor state of the communities, the members have
limited access to effective transport networks as the populations live in very remote localities.
The success of adequate healthcare services delivery is highly dependent on the quality of
communication between healthcare practitioners and patients. Due to inadequate culturally
sensitive health promotion strategies in the healthcare sector within the indigenous population,
infective communication by the healthcare workers is attributed to poor healthcare delivery
(Conway, Tsourtos & Lawn, 2017). The use of a language that the individuals cannot
comprehend is likely to cause communication barriers within the community (Gibson et al.,
2015). The medical practitioners use complex, medically orientated language that is not simple
to comprehend. Due to social-economic classes, medical practitioners are likely to behave
increased risk of injuries. The environment influences are linked to diseases and complications
that lead to health deterioration of the community.
Health Inequalities in Indigenous Communities
There various factors that have been defined as barriers to effective and efficient health
promotion services to the indigenous communities. According to healthcare practitioners,
standards of values and care are meant to offer equity and social proficiency (Browne et al.,
2016). However, there is conclusive evidence that indicates that medical practitioners are not
excepted from prejudice, which leads to culturally incentive healthcare services (Artuso, Cargo,
Brown & Daniel, 2013). The negative prejudice against the minority communities is a
significant barrier to the indigenous communities (Gibson et al., 2015). Intercultural
misunderstandings are also attributed to barriers to adequate health among the indigenous groups
in Australia. The infrequency of public transport, inadequate transport networks, and distance
from healthcare facilities is a significant barrier to the health inequalities among the indigenous
groups (Gibson et al., 2015). Due to the poor state of the communities, the members have
limited access to effective transport networks as the populations live in very remote localities.
The success of adequate healthcare services delivery is highly dependent on the quality of
communication between healthcare practitioners and patients. Due to inadequate culturally
sensitive health promotion strategies in the healthcare sector within the indigenous population,
infective communication by the healthcare workers is attributed to poor healthcare delivery
(Conway, Tsourtos & Lawn, 2017). The use of a language that the individuals cannot
comprehend is likely to cause communication barriers within the community (Gibson et al.,
2015). The medical practitioners use complex, medically orientated language that is not simple
to comprehend. Due to social-economic classes, medical practitioners are likely to behave
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 5
negatively when dealing with patients. The indigenous communities are likely to feel
uncomfortable to access medical health facilities due to the anxiety and shame when consulting
with medical practitioners (Conway et al., 2017). The use of complicated medical terminologies
by the physicians is attributed to misunderstanding, compounded with the lack of follow up or
seeking clarification due to embarrassment.
Inadequate healthcare providers of the indigenous community’s origin also contribute to
the challenges faced by the minority communities (Thomas, Bainbridge & Tsey, 2014). Having
healthcare providers from the same ethnic orientation is attributed to improved health outcomes
of the community (Durey, McEvoy, Swift-Otero, Taylor, Katzenellenbogen, & Bessarab, 2016).
However, in the indigenous communities, there is limited progress that has been made to correct
the present shortage of indigenous healthcare providers.
There is a high scarcity of health-related information among the indigenous communities
in Australia, which is a significant hindrance in targeting a unique approach that is likely to
improve and enhance health among the indigenous population (Durey et al., 2016). Inadequate
data leads to a limited analysis of the aspects that can be carried out to promote health. The
geographical isolation of the communities also limits data collection of the community.
Health Outcomes Due to Inequalities
Indigenous communities are affected by numerous health issues and complications.
According to research, the communities have poor mental health outcomes and significant rates
of disability attributed to accidents and injuries compared to that of non-indigenous. Social
disparities and inequalities are interlinked and have negative implications regarding the right to
health (Greenwood et al., 2015). Incidences of depression are high amongst the indigenous
negatively when dealing with patients. The indigenous communities are likely to feel
uncomfortable to access medical health facilities due to the anxiety and shame when consulting
with medical practitioners (Conway et al., 2017). The use of complicated medical terminologies
by the physicians is attributed to misunderstanding, compounded with the lack of follow up or
seeking clarification due to embarrassment.
Inadequate healthcare providers of the indigenous community’s origin also contribute to
the challenges faced by the minority communities (Thomas, Bainbridge & Tsey, 2014). Having
healthcare providers from the same ethnic orientation is attributed to improved health outcomes
of the community (Durey, McEvoy, Swift-Otero, Taylor, Katzenellenbogen, & Bessarab, 2016).
However, in the indigenous communities, there is limited progress that has been made to correct
the present shortage of indigenous healthcare providers.
There is a high scarcity of health-related information among the indigenous communities
in Australia, which is a significant hindrance in targeting a unique approach that is likely to
improve and enhance health among the indigenous population (Durey et al., 2016). Inadequate
data leads to a limited analysis of the aspects that can be carried out to promote health. The
geographical isolation of the communities also limits data collection of the community.
Health Outcomes Due to Inequalities
Indigenous communities are affected by numerous health issues and complications.
According to research, the communities have poor mental health outcomes and significant rates
of disability attributed to accidents and injuries compared to that of non-indigenous. Social
disparities and inequalities are interlinked and have negative implications regarding the right to
health (Greenwood et al., 2015). Incidences of depression are high amongst the indigenous
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 6
communities, mainly from the young population. The depression is attributed to the experience
that this group undergoes in their daily activities, for instance, experiences of colonization,
racism, ethnic, and cultural marginalization, which puts the communities at significant risk of
depression (Neumayer, 2013).
Poverty is a significant issue among the indigenous communities, which is highly
associated with communicable illnesses such as tuberculosis and malaria (Eversole et al., 2013).
Lack of proper housing facilities, access to health care and medications, language differences,
and geographic inaccessibility (Reading & Greenwood, 2018). Their environmental setting is
mainly located in the rural setting where there are forests and bushes which are highly associated
with malaria prevalence due to mosquitoes breeding. Lack of knowledge and education
regarding the prevention and protection against the vectors is also a significant contributor to the
health outcomes of the communities (Jones et al., 2019).
Poor nutrition and malnutrition are significant issues that affect the indigenous
communities in Australia, leading to poor health (Neumayer, 2013: Brimblecombe et al., 2014).
Poverty circumstances are attributed to the intake of poor diets that do not meet the needs of the
body (Eversole et al., 2013). Also, malnutrition due to environmental dilapidation and pollution
of the environment in which the indigenous societies dwell in, loss of farming land and decline
inaccessibility and abundance of traditional food sources is linked to poor nutrition in this
communities (Brimblecombe et al., 2014)
Many of the indigenous communities of Australia dwell in poverty-stricken rural areas
where there are likely to encounter disasters due to their economic activities. The communities
are likely to be affected by varying disasters based on different influences, including
unsustainable practices, environmental degradation, poverty, and variability in climate and
communities, mainly from the young population. The depression is attributed to the experience
that this group undergoes in their daily activities, for instance, experiences of colonization,
racism, ethnic, and cultural marginalization, which puts the communities at significant risk of
depression (Neumayer, 2013).
Poverty is a significant issue among the indigenous communities, which is highly
associated with communicable illnesses such as tuberculosis and malaria (Eversole et al., 2013).
Lack of proper housing facilities, access to health care and medications, language differences,
and geographic inaccessibility (Reading & Greenwood, 2018). Their environmental setting is
mainly located in the rural setting where there are forests and bushes which are highly associated
with malaria prevalence due to mosquitoes breeding. Lack of knowledge and education
regarding the prevention and protection against the vectors is also a significant contributor to the
health outcomes of the communities (Jones et al., 2019).
Poor nutrition and malnutrition are significant issues that affect the indigenous
communities in Australia, leading to poor health (Neumayer, 2013: Brimblecombe et al., 2014).
Poverty circumstances are attributed to the intake of poor diets that do not meet the needs of the
body (Eversole et al., 2013). Also, malnutrition due to environmental dilapidation and pollution
of the environment in which the indigenous societies dwell in, loss of farming land and decline
inaccessibility and abundance of traditional food sources is linked to poor nutrition in this
communities (Brimblecombe et al., 2014)
Many of the indigenous communities of Australia dwell in poverty-stricken rural areas
where there are likely to encounter disasters due to their economic activities. The communities
are likely to be affected by varying disasters based on different influences, including
unsustainable practices, environmental degradation, poverty, and variability in climate and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 7
extremes (Eversole et al., 2013). The factors contribute to an increase in the risk of disaster
encounters that contribute to the health outcomes of the indigenous communities.
Health Disparity Impacting the Indigenous Communities of Australia
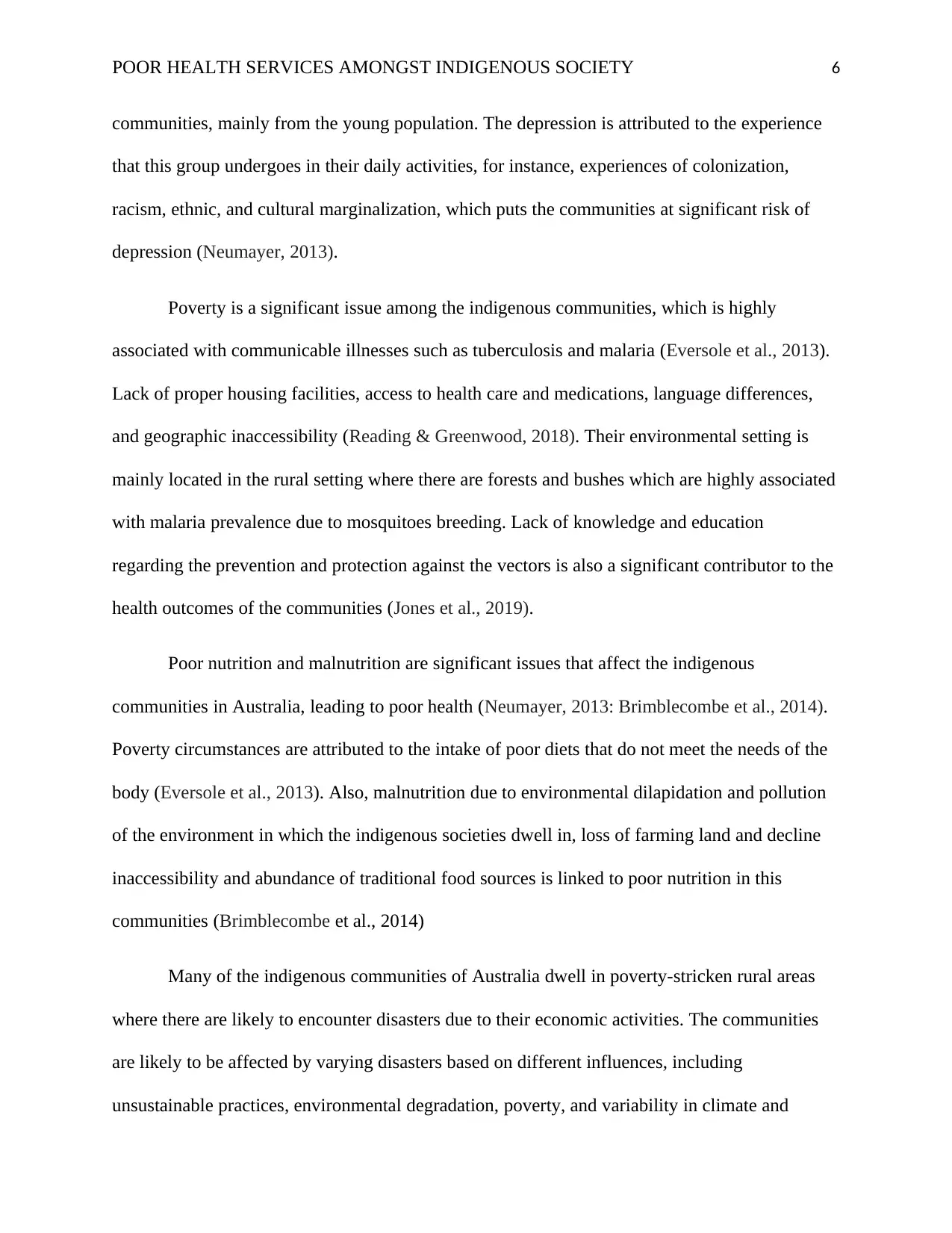
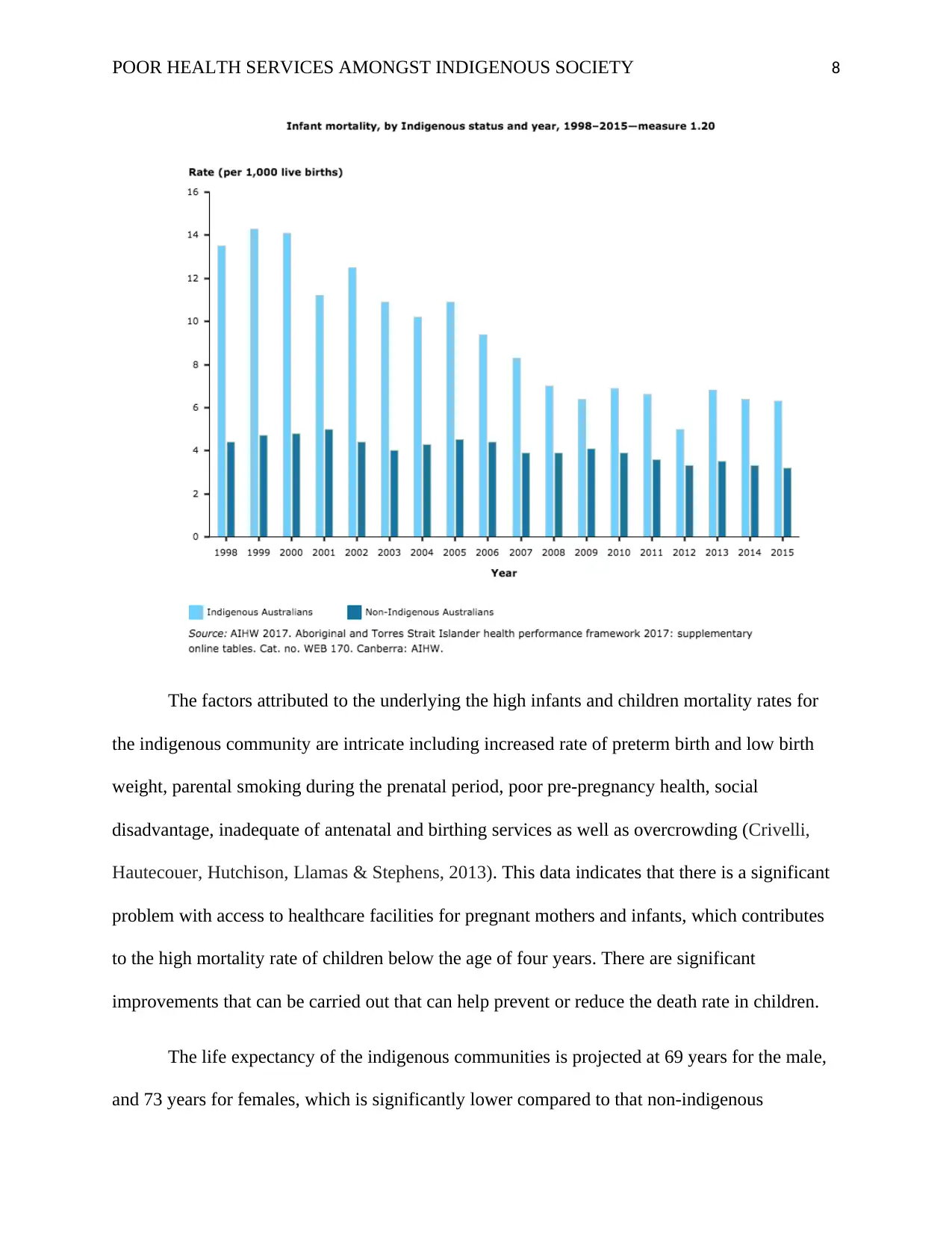
Life expectancy and child mortality are extensively utilized as general indicators of
community health. In Australia, the overall life expectancy is considerably higher and child
mortality rates are low compared to other nations (Thomas et al., 2014). However, there are
significant differences in both measures between the non-indigenous and indigenous
communities. According to an Australian study by (AIHW) Australian Institute of Health and
Welfare in 2016, the mortality rate of infants was indicated at 146 for every 100,000 indigenous
children and 70 for every 100,000 for the non-indigenous children population (DOH, 2017). The
data indicates a gap of at least 76 deaths for every 100,00 children, whereby the likelihood of
indigenous children to die was double that of the non-indigenous children (Thomas et al., 2014).
AIHW highlighted that the risk of child mortality varied with age, with death in the first of life
accounts for approximately 82 percent of all indigenous children's death and 84 percent for non-
indigenous populations.
The child mortality gap was attributed to three major causes, which accounted for 85
percent of the difference in child death among the non-indigenous and indigenous children below
four years between the years 2011 and 2015. The causes included birth and pregnancy-related
problems that accounted for 40 percent of the gap, (SIDS) sudden infant death syndrome and
other unidentified reasons accounting for 26 percent and injuries, accidents and other
environmental reasons accounting for 19% of the gap (DOH, 2017).
extremes (Eversole et al., 2013). The factors contribute to an increase in the risk of disaster
encounters that contribute to the health outcomes of the indigenous communities.
Health Disparity Impacting the Indigenous Communities of Australia
Life expectancy and child mortality are extensively utilized as general indicators of
community health. In Australia, the overall life expectancy is considerably higher and child
mortality rates are low compared to other nations (Thomas et al., 2014). However, there are
significant differences in both measures between the non-indigenous and indigenous
communities. According to an Australian study by (AIHW) Australian Institute of Health and
Welfare in 2016, the mortality rate of infants was indicated at 146 for every 100,000 indigenous
children and 70 for every 100,000 for the non-indigenous children population (DOH, 2017). The
data indicates a gap of at least 76 deaths for every 100,00 children, whereby the likelihood of
indigenous children to die was double that of the non-indigenous children (Thomas et al., 2014).
AIHW highlighted that the risk of child mortality varied with age, with death in the first of life
accounts for approximately 82 percent of all indigenous children's death and 84 percent for non-
indigenous populations.
The child mortality gap was attributed to three major causes, which accounted for 85
percent of the difference in child death among the non-indigenous and indigenous children below
four years between the years 2011 and 2015. The causes included birth and pregnancy-related
problems that accounted for 40 percent of the gap, (SIDS) sudden infant death syndrome and
other unidentified reasons accounting for 26 percent and injuries, accidents and other
environmental reasons accounting for 19% of the gap (DOH, 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 8
The factors attributed to the underlying the high infants and children mortality rates for
the indigenous community are intricate including increased rate of preterm birth and low birth
weight, parental smoking during the prenatal period, poor pre-pregnancy health, social
disadvantage, inadequate of antenatal and birthing services as well as overcrowding (Crivelli,
Hautecouer, Hutchison, Llamas & Stephens, 2013). This data indicates that there is a significant
problem with access to healthcare facilities for pregnant mothers and infants, which contributes
to the high mortality rate of children below the age of four years. There are significant
improvements that can be carried out that can help prevent or reduce the death rate in children.
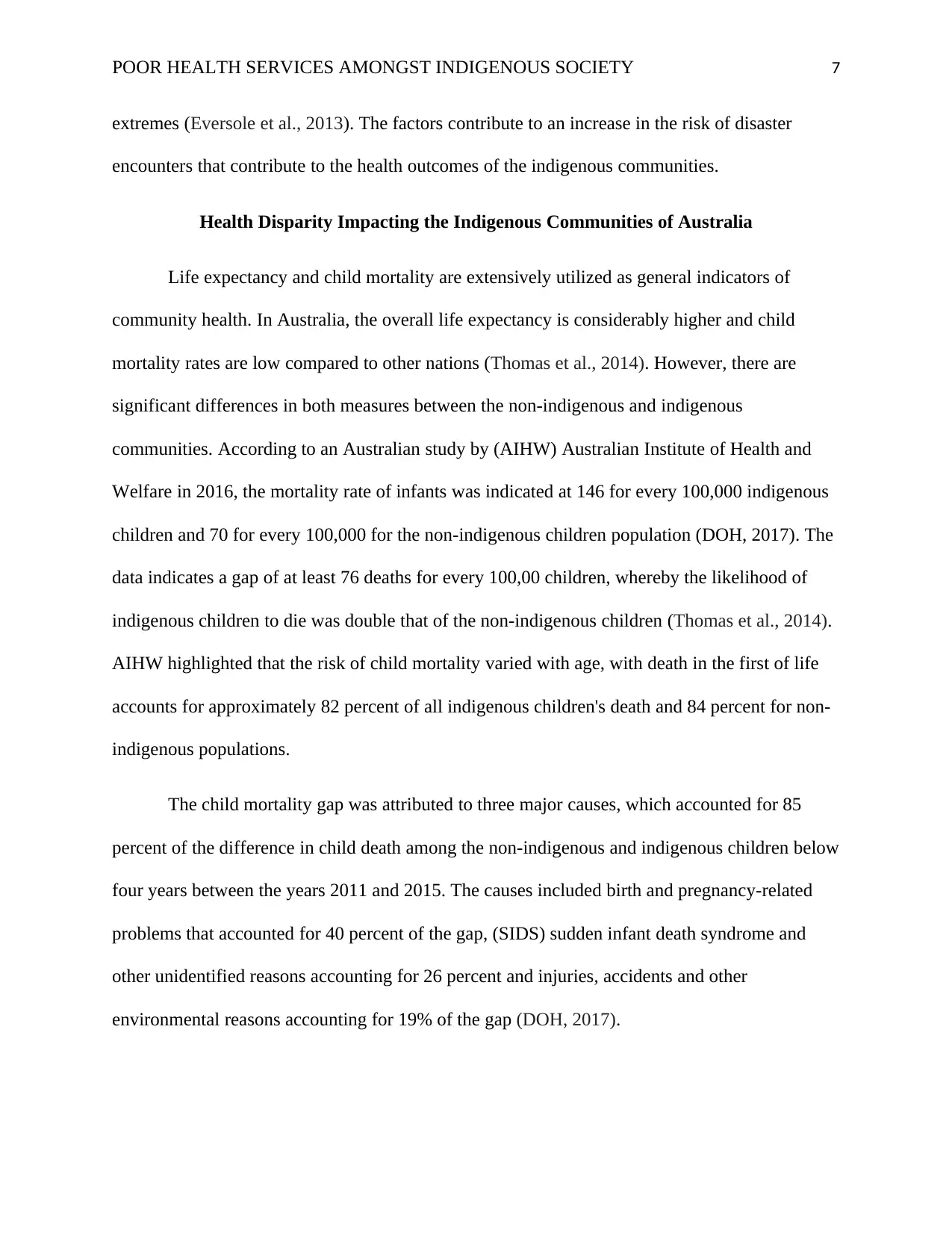
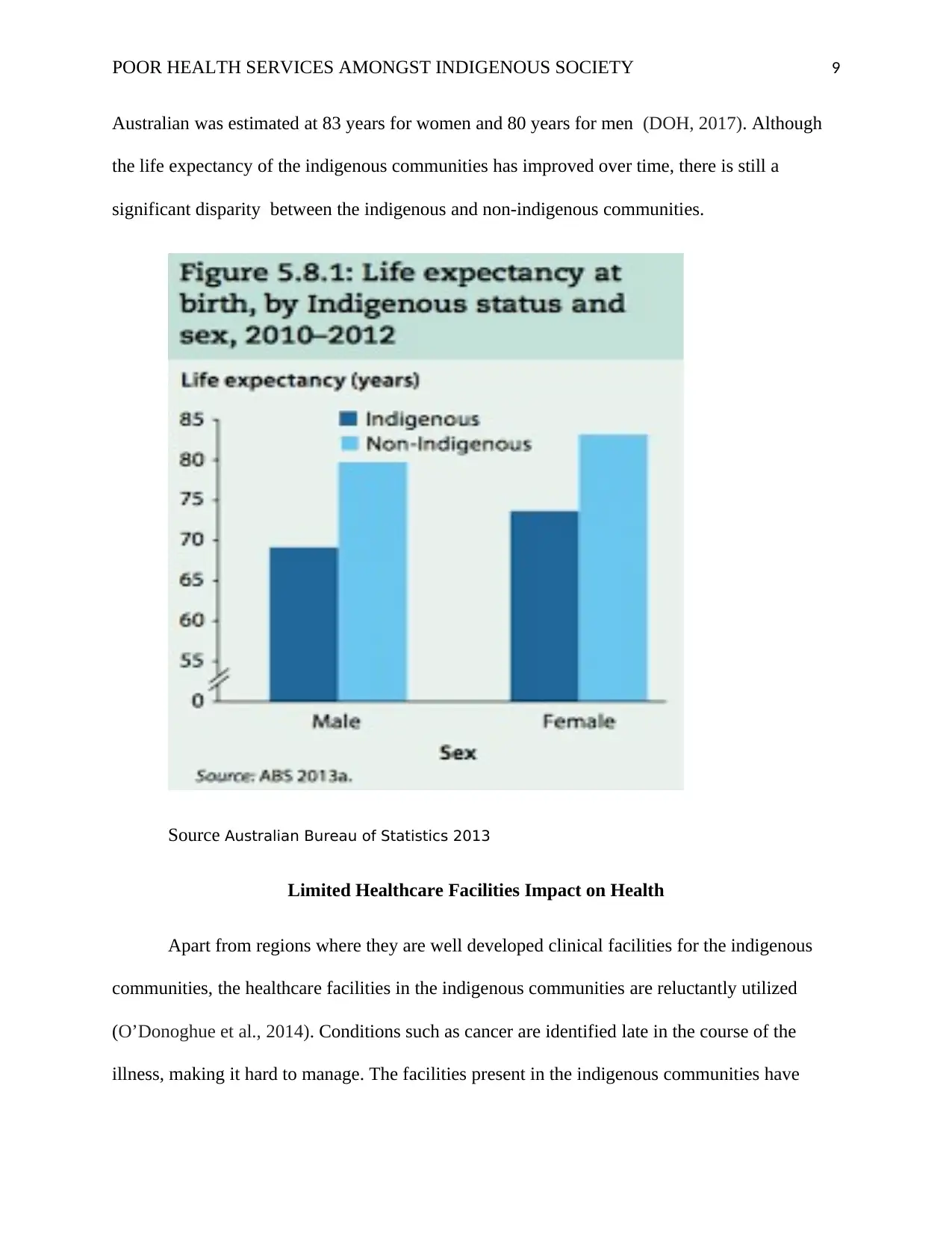
The life expectancy of the indigenous communities is projected at 69 years for the male,
and 73 years for females, which is significantly lower compared to that non-indigenous
The factors attributed to the underlying the high infants and children mortality rates for
the indigenous community are intricate including increased rate of preterm birth and low birth
weight, parental smoking during the prenatal period, poor pre-pregnancy health, social
disadvantage, inadequate of antenatal and birthing services as well as overcrowding (Crivelli,
Hautecouer, Hutchison, Llamas & Stephens, 2013). This data indicates that there is a significant
problem with access to healthcare facilities for pregnant mothers and infants, which contributes
to the high mortality rate of children below the age of four years. There are significant
improvements that can be carried out that can help prevent or reduce the death rate in children.
The life expectancy of the indigenous communities is projected at 69 years for the male,
and 73 years for females, which is significantly lower compared to that non-indigenous
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 9
Australian was estimated at 83 years for women and 80 years for men (DOH, 2017). Although
the life expectancy of the indigenous communities has improved over time, there is still a
significant disparity between the indigenous and non-indigenous communities.
Source Australian Bureau of Statistics 2013
Limited Healthcare Facilities Impact on Health
Apart from regions where they are well developed clinical facilities for the indigenous
communities, the healthcare facilities in the indigenous communities are reluctantly utilized
(O’Donoghue et al., 2014). Conditions such as cancer are identified late in the course of the
illness, making it hard to manage. The facilities present in the indigenous communities have
Australian was estimated at 83 years for women and 80 years for men (DOH, 2017). Although
the life expectancy of the indigenous communities has improved over time, there is still a
significant disparity between the indigenous and non-indigenous communities.
Source Australian Bureau of Statistics 2013
Limited Healthcare Facilities Impact on Health
Apart from regions where they are well developed clinical facilities for the indigenous
communities, the healthcare facilities in the indigenous communities are reluctantly utilized
(O’Donoghue et al., 2014). Conditions such as cancer are identified late in the course of the
illness, making it hard to manage. The facilities present in the indigenous communities have
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 10
limited association with the mainstream services and maybe unaware of what local palliative
care facilities are offered. The mainstream service providers may also have limited knowledge of
the services, special needs, network as well as social support available to them (Cliffor et al.,
2015).
The indigenous communities in Australia exhibit remarkable resilience and pride in their
culture, which consequently has implications for their health and believes. The presence of
traditional healers who have significant influence over contemporary medicine is a significant
effect on the health and wellbeing of the indigenous population (Greenwood et al., 2015).
Despite numerous programs to educate the community on seeking contemporary healthcare, the
individuals are still inclined to seeking help from the traditional healers, which is not effective as
modern medicine (Jones et al., 2019).
The current health practices and policies put in place are in favor of standardized
healthcare, where the marginalized communities are often left out. Defining the efficiency of
such programs in alleviating the disparities witnessed between the non-indigenous and
indigenous communities needs healthcare practitioners to critically reflect on whether the
existing practices and policies influence or compromise the health and wellbeing of the
marginalized groups (Mitrou et al., 2014). The lack of tailor-made health facilities for the
marginalized communities is identified as the significant impact of the health problem.
Target Audience and Project Recommendation
The Australian government is dedicated to improving the health and wellbeing of the indigenous
community and consequently reduce the gap that is present between the non-indigenous and
indigenous groups of Australia (Murphy & Reath, 2014). A lot of resources and policies have
limited association with the mainstream services and maybe unaware of what local palliative
care facilities are offered. The mainstream service providers may also have limited knowledge of
the services, special needs, network as well as social support available to them (Cliffor et al.,
2015).
The indigenous communities in Australia exhibit remarkable resilience and pride in their
culture, which consequently has implications for their health and believes. The presence of
traditional healers who have significant influence over contemporary medicine is a significant
effect on the health and wellbeing of the indigenous population (Greenwood et al., 2015).
Despite numerous programs to educate the community on seeking contemporary healthcare, the
individuals are still inclined to seeking help from the traditional healers, which is not effective as
modern medicine (Jones et al., 2019).
The current health practices and policies put in place are in favor of standardized
healthcare, where the marginalized communities are often left out. Defining the efficiency of
such programs in alleviating the disparities witnessed between the non-indigenous and
indigenous communities needs healthcare practitioners to critically reflect on whether the
existing practices and policies influence or compromise the health and wellbeing of the
marginalized groups (Mitrou et al., 2014). The lack of tailor-made health facilities for the
marginalized communities is identified as the significant impact of the health problem.
Target Audience and Project Recommendation
The Australian government is dedicated to improving the health and wellbeing of the indigenous
community and consequently reduce the gap that is present between the non-indigenous and
indigenous groups of Australia (Murphy & Reath, 2014). A lot of resources and policies have
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 11
been made with the aim of closing the indigenous disadvantages in terms of their health and
wellbeing, housing, employment, and education (Jones et al., 2019). Even with policy
formulation and resource allocation, some factors need to be considered to ensure efficiency and
equitable services are offered to the disadvantaged communities. The government should ensure
that the policies formulated are followed, and research is carried out regularly to determine
efficiency in terms of service delivery to the marginalized communities (Murphy & Reath,
2014). To reduce the disparity in these communities, the government should formulate policies
that enforce tailor-made healthcare services for the indigenous communities. The services should
be centered on the needs of the society; hence, policymakers should involve the communities in
developing the policies to ensure effective outcomes (O’Donoghue et al., 2014).
Nurses and other medical practitioners working in the indigenous healthcare facilities
have a significant role to play in health literacy (Rheault, Coyer, Jones & Bonner, 2019). Health
literacy is a powerful tool in healthcare service delivery. The nurses can help educate pregnant
mothers from the indigenous communities on the importance of managing their health so as to
ensure the safety of their unborn child (Crivelli et al., 2013) Advocating for health literacy will
offer the mothers the knowledge on what to eat during their pregnancy to ensure the unborn child
develops healthily (Rheault et al., 2019). The nurses can also promote regular medical checkups
to the pregnant mothers as a way of determining the health status of the mother and child will, in
turn, reduce child mortality (Crivelli et al., 2013). Inadequate knowledge of chronic diseases and
other significant diseases are attributed to the premature deaths of community members. The
nurses should offer education to the community on the importance of regular medical checkups
and reducing substance use, for instance, tobacco, which is a major cause of death to the
indigenous communities. The medical practitioners should also be encouraged to promote a
been made with the aim of closing the indigenous disadvantages in terms of their health and
wellbeing, housing, employment, and education (Jones et al., 2019). Even with policy
formulation and resource allocation, some factors need to be considered to ensure efficiency and
equitable services are offered to the disadvantaged communities. The government should ensure
that the policies formulated are followed, and research is carried out regularly to determine
efficiency in terms of service delivery to the marginalized communities (Murphy & Reath,
2014). To reduce the disparity in these communities, the government should formulate policies
that enforce tailor-made healthcare services for the indigenous communities. The services should
be centered on the needs of the society; hence, policymakers should involve the communities in
developing the policies to ensure effective outcomes (O’Donoghue et al., 2014).
Nurses and other medical practitioners working in the indigenous healthcare facilities
have a significant role to play in health literacy (Rheault, Coyer, Jones & Bonner, 2019). Health
literacy is a powerful tool in healthcare service delivery. The nurses can help educate pregnant
mothers from the indigenous communities on the importance of managing their health so as to
ensure the safety of their unborn child (Crivelli et al., 2013) Advocating for health literacy will
offer the mothers the knowledge on what to eat during their pregnancy to ensure the unborn child
develops healthily (Rheault et al., 2019). The nurses can also promote regular medical checkups
to the pregnant mothers as a way of determining the health status of the mother and child will, in
turn, reduce child mortality (Crivelli et al., 2013). Inadequate knowledge of chronic diseases and
other significant diseases are attributed to the premature deaths of community members. The
nurses should offer education to the community on the importance of regular medical checkups
and reducing substance use, for instance, tobacco, which is a major cause of death to the
indigenous communities. The medical practitioners should also be encouraged to promote a
POOR HEALTH SERVICES AMONGST INDIGENOUS SOCIETY 12
friendly environment when intercutting with the indigenous communities. They should also
communicate in simple language that is comprehensible to the individuals to avoid
misinterpretation from the indigenous population (Artuso et al., 2013). The healthcare services
provider should also hire individuals from the community to help in communication. This will
reduce the anxiety and shame brought about by the lack of education from the community
members
Conclusion
Nurses are mandated to actively encourage a culture of safety and learning that
encompasses engaging with medical practitioners and other stakeholders to share knowledge and
practice that supports a person centered-care. The indigenous communities of Australia have
different needs compared to that of the non-indigenous majority, which makes it relevant to
handle their needs as a community and not through standardized healthcare services with the rest
of the people. The indigenous communities are vulnerable due to their cultural practices,
environmental, behavior, and social, economic activities, which constitute their poor health.
Studying the different issues that impact the health of the indigenous populations will offer data
that is important in making decisions that will promote healthy living in the community.
Consequently, they should ensure that the set policies are followed and the resources are used to
achieve individual-centered care.
The nurses, therefore, should share their knowledge of the community based on
observations and analysis of the prevalent conditions such as mortality rate in children and life
expectancy rate, which will help in formulating relevant policies and programs that are based on
the community needs. Offering advice to the indigenous community on better health and
wellbeing is key to the reduction of the health disparity presently witnessed. Learning about the
friendly environment when intercutting with the indigenous communities. They should also
communicate in simple language that is comprehensible to the individuals to avoid
misinterpretation from the indigenous population (Artuso et al., 2013). The healthcare services
provider should also hire individuals from the community to help in communication. This will
reduce the anxiety and shame brought about by the lack of education from the community
members
Conclusion
Nurses are mandated to actively encourage a culture of safety and learning that
encompasses engaging with medical practitioners and other stakeholders to share knowledge and
practice that supports a person centered-care. The indigenous communities of Australia have
different needs compared to that of the non-indigenous majority, which makes it relevant to
handle their needs as a community and not through standardized healthcare services with the rest
of the people. The indigenous communities are vulnerable due to their cultural practices,
environmental, behavior, and social, economic activities, which constitute their poor health.
Studying the different issues that impact the health of the indigenous populations will offer data
that is important in making decisions that will promote healthy living in the community.
Consequently, they should ensure that the set policies are followed and the resources are used to
achieve individual-centered care.
The nurses, therefore, should share their knowledge of the community based on
observations and analysis of the prevalent conditions such as mortality rate in children and life
expectancy rate, which will help in formulating relevant policies and programs that are based on
the community needs. Offering advice to the indigenous community on better health and
wellbeing is key to the reduction of the health disparity presently witnessed. Learning about the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





