HEAS 1000 Clinical Integration: Practical Nurse Health History Form
VerifiedAdded on 2023/05/30
|18
|4420
|390
Practical Assignment
AI Summary
This assignment presents a comprehensive health history form completed by a practical nurse student, encompassing the client's biographical data and detailed health information. The health history includes current health status, past health history (childhood illnesses, injuries, surgeries, and mental health concerns), family history (including hereditary diseases and causes of death), allergies, prescribed and over-the-counter medications, and a thorough review of systems. The review of systems covers respiratory, cardiovascular, gastrointestinal, neurological, urinary, genital, musculoskeletal, and peripheral vascular systems, with specific questions and documented concerns. The assignment also includes the assignment brief and marking guide.
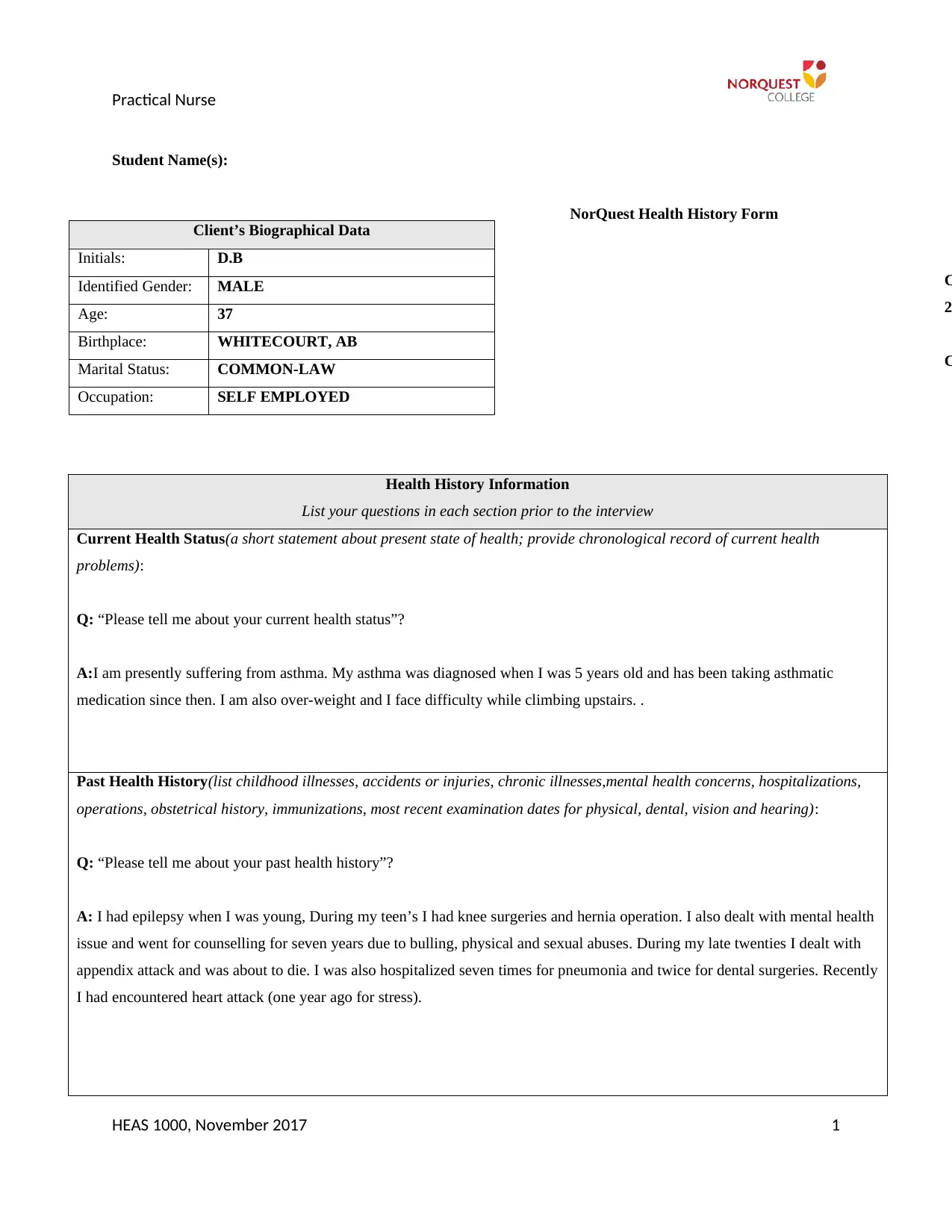
Practical Nurse
Student Name(s):
NorQuest Health History Form
Health History Information
List your questions in each section prior to the interview
Current Health Status(a short statement about present state of health; provide chronological record of current health
problems):
Q: “Please tell me about your current health status”?
A:I am presently suffering from asthma. My asthma was diagnosed when I was 5 years old and has been taking asthmatic
medication since then. I am also over-weight and I face difficulty while climbing upstairs. .
Past Health History(list childhood illnesses, accidents or injuries, chronic illnesses,mental health concerns, hospitalizations,
operations, obstetrical history, immunizations, most recent examination dates for physical, dental, vision and hearing):
Q: “Please tell me about your past health history”?
A: I had epilepsy when I was young, During my teen’s I had knee surgeries and hernia operation. I also dealt with mental health
issue and went for counselling for seven years due to bulling, physical and sexual abuses. During my late twenties I dealt with
appendix attack and was about to die. I was also hospitalized seven times for pneumonia and twice for dental surgeries. Recently
I had encountered heart attack (one year ago for stress).
HEAS 1000, November 2017 1
C
2
C
Client’s Biographical Data
Initials: D.B
Identified Gender: MALE
Age: 37
Birthplace: WHITECOURT, AB
Marital Status: COMMON-LAW
Occupation: SELF EMPLOYED
Student Name(s):
NorQuest Health History Form
Health History Information
List your questions in each section prior to the interview
Current Health Status(a short statement about present state of health; provide chronological record of current health
problems):
Q: “Please tell me about your current health status”?
A:I am presently suffering from asthma. My asthma was diagnosed when I was 5 years old and has been taking asthmatic
medication since then. I am also over-weight and I face difficulty while climbing upstairs. .
Past Health History(list childhood illnesses, accidents or injuries, chronic illnesses,mental health concerns, hospitalizations,
operations, obstetrical history, immunizations, most recent examination dates for physical, dental, vision and hearing):
Q: “Please tell me about your past health history”?
A: I had epilepsy when I was young, During my teen’s I had knee surgeries and hernia operation. I also dealt with mental health
issue and went for counselling for seven years due to bulling, physical and sexual abuses. During my late twenties I dealt with
appendix attack and was about to die. I was also hospitalized seven times for pneumonia and twice for dental surgeries. Recently
I had encountered heart attack (one year ago for stress).
HEAS 1000, November 2017 1
C
2
C
Client’s Biographical Data
Initials: D.B
Identified Gender: MALE
Age: 37
Birthplace: WHITECOURT, AB
Marital Status: COMMON-LAW
Occupation: SELF EMPLOYED
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Practical Nurse
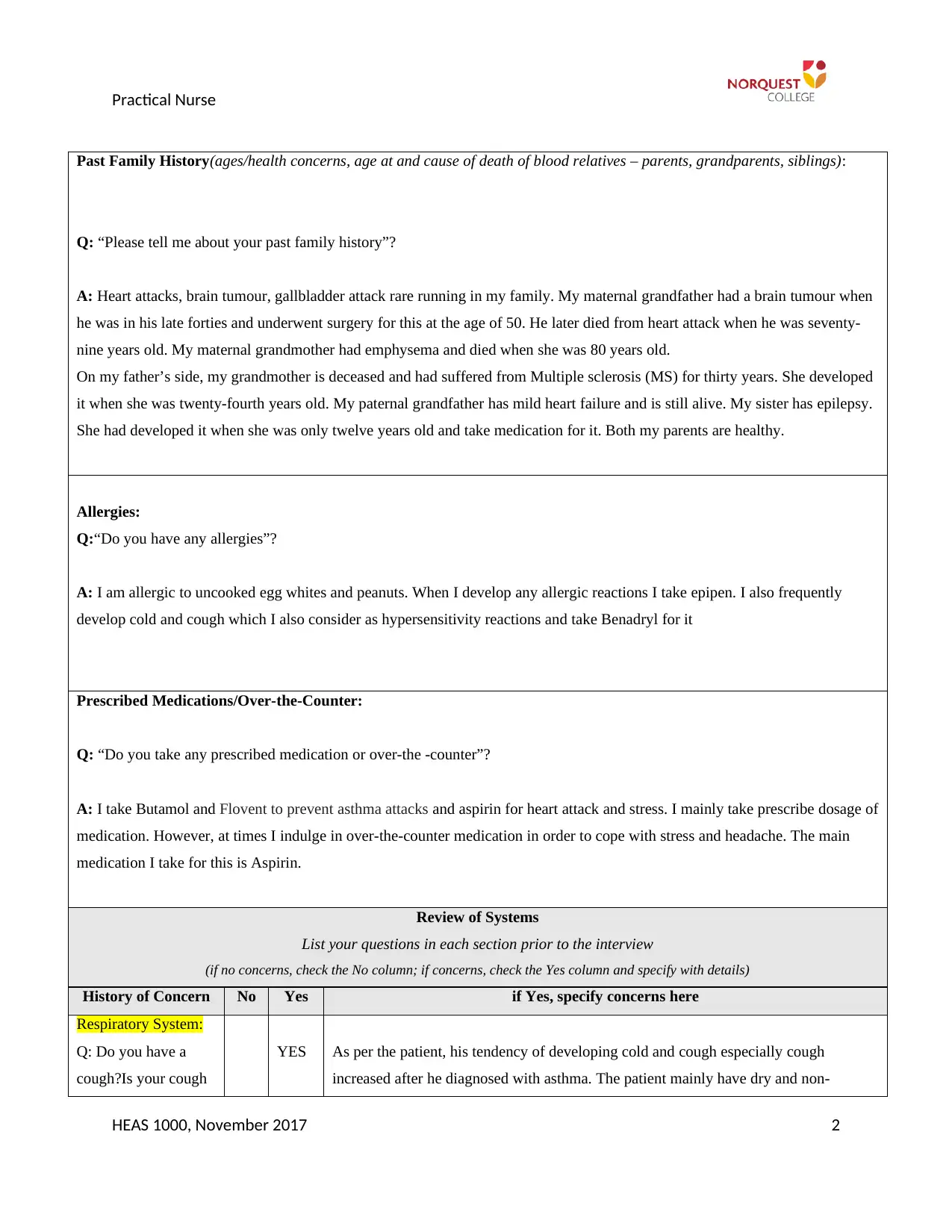
Past Family History(ages/health concerns, age at and cause of death of blood relatives – parents, grandparents, siblings):
Q: “Please tell me about your past family history”?
A: Heart attacks, brain tumour, gallbladder attack rare running in my family. My maternal grandfather had a brain tumour when
he was in his late forties and underwent surgery for this at the age of 50. He later died from heart attack when he was seventy-
nine years old. My maternal grandmother had emphysema and died when she was 80 years old.
On my father’s side, my grandmother is deceased and had suffered from Multiple sclerosis (MS) for thirty years. She developed
it when she was twenty-fourth years old. My paternal grandfather has mild heart failure and is still alive. My sister has epilepsy.
She had developed it when she was only twelve years old and take medication for it. Both my parents are healthy.
Allergies:
Q:“Do you have any allergies”?
A: I am allergic to uncooked egg whites and peanuts. When I develop any allergic reactions I take epipen. I also frequently
develop cold and cough which I also consider as hypersensitivity reactions and take Benadryl for it
Prescribed Medications/Over-the-Counter:
Q: “Do you take any prescribed medication or over-the -counter”?
A: I take Butamol and Flovent to prevent asthma attacks and aspirin for heart attack and stress. I mainly take prescribe dosage of
medication. However, at times I indulge in over-the-counter medication in order to cope with stress and headache. The main
medication I take for this is Aspirin.
Review of Systems
List your questions in each section prior to the interview
(if no concerns, check the No column; if concerns, check the Yes column and specify with details)
History of Concern No Yes if Yes, specify concerns here
Respiratory System:
Q: Do you have a
cough?Is your cough
YES As per the patient, his tendency of developing cold and cough especially cough
increased after he diagnosed with asthma. The patient mainly have dry and non-
HEAS 1000, November 2017 2
Past Family History(ages/health concerns, age at and cause of death of blood relatives – parents, grandparents, siblings):
Q: “Please tell me about your past family history”?
A: Heart attacks, brain tumour, gallbladder attack rare running in my family. My maternal grandfather had a brain tumour when
he was in his late forties and underwent surgery for this at the age of 50. He later died from heart attack when he was seventy-
nine years old. My maternal grandmother had emphysema and died when she was 80 years old.
On my father’s side, my grandmother is deceased and had suffered from Multiple sclerosis (MS) for thirty years. She developed
it when she was twenty-fourth years old. My paternal grandfather has mild heart failure and is still alive. My sister has epilepsy.
She had developed it when she was only twelve years old and take medication for it. Both my parents are healthy.
Allergies:
Q:“Do you have any allergies”?
A: I am allergic to uncooked egg whites and peanuts. When I develop any allergic reactions I take epipen. I also frequently
develop cold and cough which I also consider as hypersensitivity reactions and take Benadryl for it
Prescribed Medications/Over-the-Counter:
Q: “Do you take any prescribed medication or over-the -counter”?
A: I take Butamol and Flovent to prevent asthma attacks and aspirin for heart attack and stress. I mainly take prescribe dosage of
medication. However, at times I indulge in over-the-counter medication in order to cope with stress and headache. The main
medication I take for this is Aspirin.
Review of Systems
List your questions in each section prior to the interview
(if no concerns, check the No column; if concerns, check the Yes column and specify with details)
History of Concern No Yes if Yes, specify concerns here
Respiratory System:
Q: Do you have a
cough?Is your cough
YES As per the patient, his tendency of developing cold and cough especially cough
increased after he diagnosed with asthma. The patient mainly have dry and non-
HEAS 1000, November 2017 2
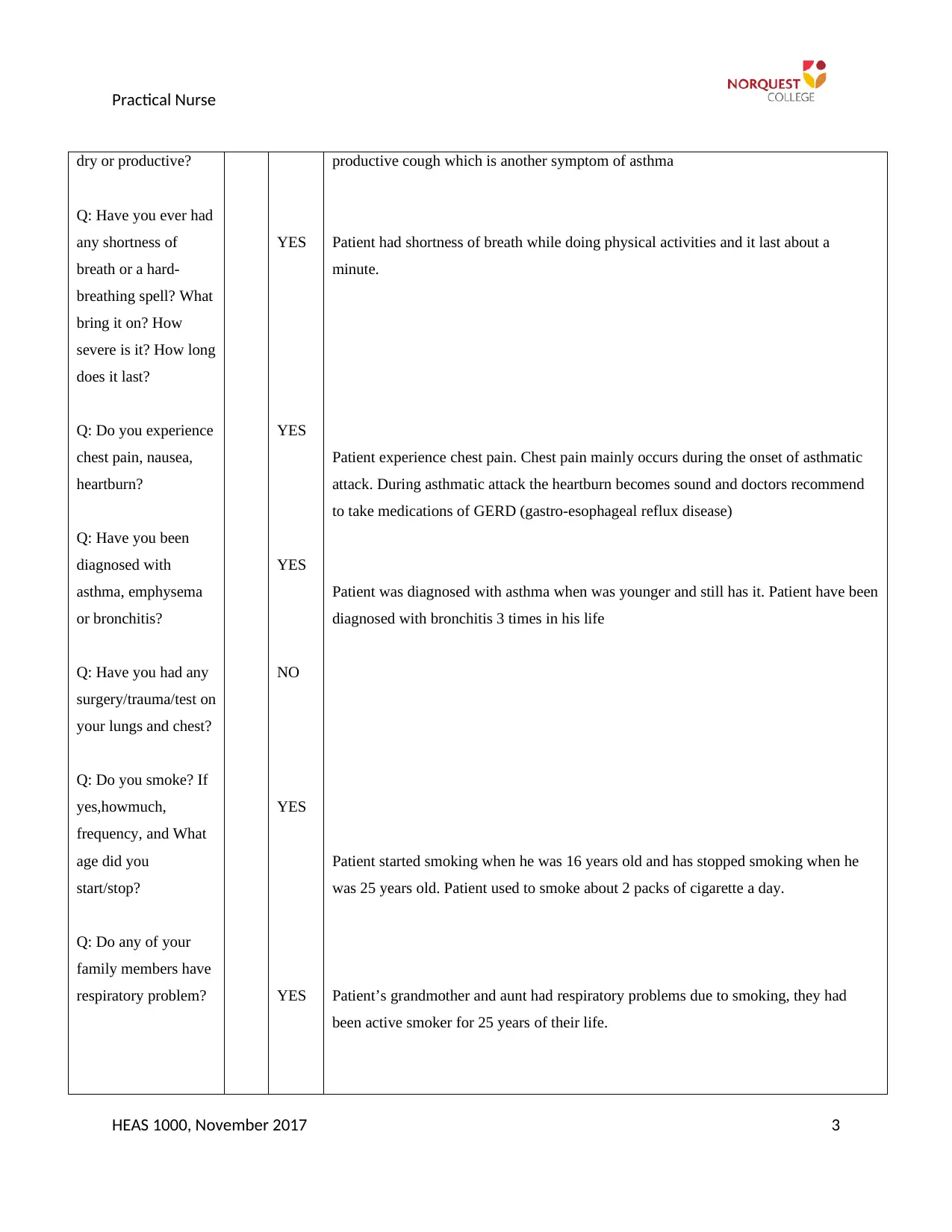
Practical Nurse
dry or productive?
Q: Have you ever had
any shortness of
breath or a hard-
breathing spell? What
bring it on? How
severe is it? How long
does it last?
Q: Do you experience
chest pain, nausea,
heartburn?
Q: Have you been
diagnosed with
asthma, emphysema
or bronchitis?
Q: Have you had any
surgery/trauma/test on
your lungs and chest?
Q: Do you smoke? If
yes,howmuch,
frequency, and What
age did you
start/stop?
Q: Do any of your
family members have
respiratory problem?
YES
YES
YES
NO
YES
YES
productive cough which is another symptom of asthma
Patient had shortness of breath while doing physical activities and it last about a
minute.
Patient experience chest pain. Chest pain mainly occurs during the onset of asthmatic
attack. During asthmatic attack the heartburn becomes sound and doctors recommend
to take medications of GERD (gastro-esophageal reflux disease)
Patient was diagnosed with asthma when was younger and still has it. Patient have been
diagnosed with bronchitis 3 times in his life
Patient started smoking when he was 16 years old and has stopped smoking when he
was 25 years old. Patient used to smoke about 2 packs of cigarette a day.
Patient’s grandmother and aunt had respiratory problems due to smoking, they had
been active smoker for 25 years of their life.
HEAS 1000, November 2017 3
dry or productive?
Q: Have you ever had
any shortness of
breath or a hard-
breathing spell? What
bring it on? How
severe is it? How long
does it last?
Q: Do you experience
chest pain, nausea,
heartburn?
Q: Have you been
diagnosed with
asthma, emphysema
or bronchitis?
Q: Have you had any
surgery/trauma/test on
your lungs and chest?
Q: Do you smoke? If
yes,howmuch,
frequency, and What
age did you
start/stop?
Q: Do any of your
family members have
respiratory problem?
YES
YES
YES
NO
YES
YES
productive cough which is another symptom of asthma
Patient had shortness of breath while doing physical activities and it last about a
minute.
Patient experience chest pain. Chest pain mainly occurs during the onset of asthmatic
attack. During asthmatic attack the heartburn becomes sound and doctors recommend
to take medications of GERD (gastro-esophageal reflux disease)
Patient was diagnosed with asthma when was younger and still has it. Patient have been
diagnosed with bronchitis 3 times in his life
Patient started smoking when he was 16 years old and has stopped smoking when he
was 25 years old. Patient used to smoke about 2 packs of cigarette a day.
Patient’s grandmother and aunt had respiratory problems due to smoking, they had
been active smoker for 25 years of their life.
HEAS 1000, November 2017 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Practical Nurse
Cardiovascular
System:
Q: Do you experience
any chest pain?
Q: Do you experience
heart palpitation
/irregular heart beat?
Q: Do you experience
any dizziness?
Q: Do you have a
history of heart
problems such as
heart defect/murmur?
Q: Have you had
rheumatic fever
Q: When did you last
have your cholesterol
test?
Q: Haves any of your
family been
diagnosed with high
blood pressure
(hypertension); heart
defect; high
cholesterol or heart
attack (myocardial
infection)?
Q: When was your
last BP/pulse
checked?
YES
YES
YES
YES
YES
Patient’s experience heart burn especially after the onset of asthma and then take
medications of GERD
Just after mild to moderate exercise or while climbing upstairs, when experience heart
palpitation along with shortness of breadth
Patient has encountered heart attack last year and the reason highlighted behind heart
attack is stress
Patient once had rheumatic fever when he was 10 years old and was under antibiotic
medication and Denadryl.
Patient has last checked his cholesterol one moth back. The test reported 140 mg/dL
cholesterol which is borderline high (normal range: less than 100 mg/dL) (Hall, 2015)
Patient reported that his grandfather had hypertension and died of heart attack
Last week and it recorded 130/90. It is higher than the normal range (normal range:
120/80) (Hall, 2015)
HEAS 1000, November 2017 4
Cardiovascular
System:
Q: Do you experience
any chest pain?
Q: Do you experience
heart palpitation
/irregular heart beat?
Q: Do you experience
any dizziness?
Q: Do you have a
history of heart
problems such as
heart defect/murmur?
Q: Have you had
rheumatic fever
Q: When did you last
have your cholesterol
test?
Q: Haves any of your
family been
diagnosed with high
blood pressure
(hypertension); heart
defect; high
cholesterol or heart
attack (myocardial
infection)?
Q: When was your
last BP/pulse
checked?
YES
YES
YES
YES
YES
Patient’s experience heart burn especially after the onset of asthma and then take
medications of GERD
Just after mild to moderate exercise or while climbing upstairs, when experience heart
palpitation along with shortness of breadth
Patient has encountered heart attack last year and the reason highlighted behind heart
attack is stress
Patient once had rheumatic fever when he was 10 years old and was under antibiotic
medication and Denadryl.
Patient has last checked his cholesterol one moth back. The test reported 140 mg/dL
cholesterol which is borderline high (normal range: less than 100 mg/dL) (Hall, 2015)
Patient reported that his grandfather had hypertension and died of heart attack
Last week and it recorded 130/90. It is higher than the normal range (normal range:
120/80) (Hall, 2015)
HEAS 1000, November 2017 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Practical Nurse
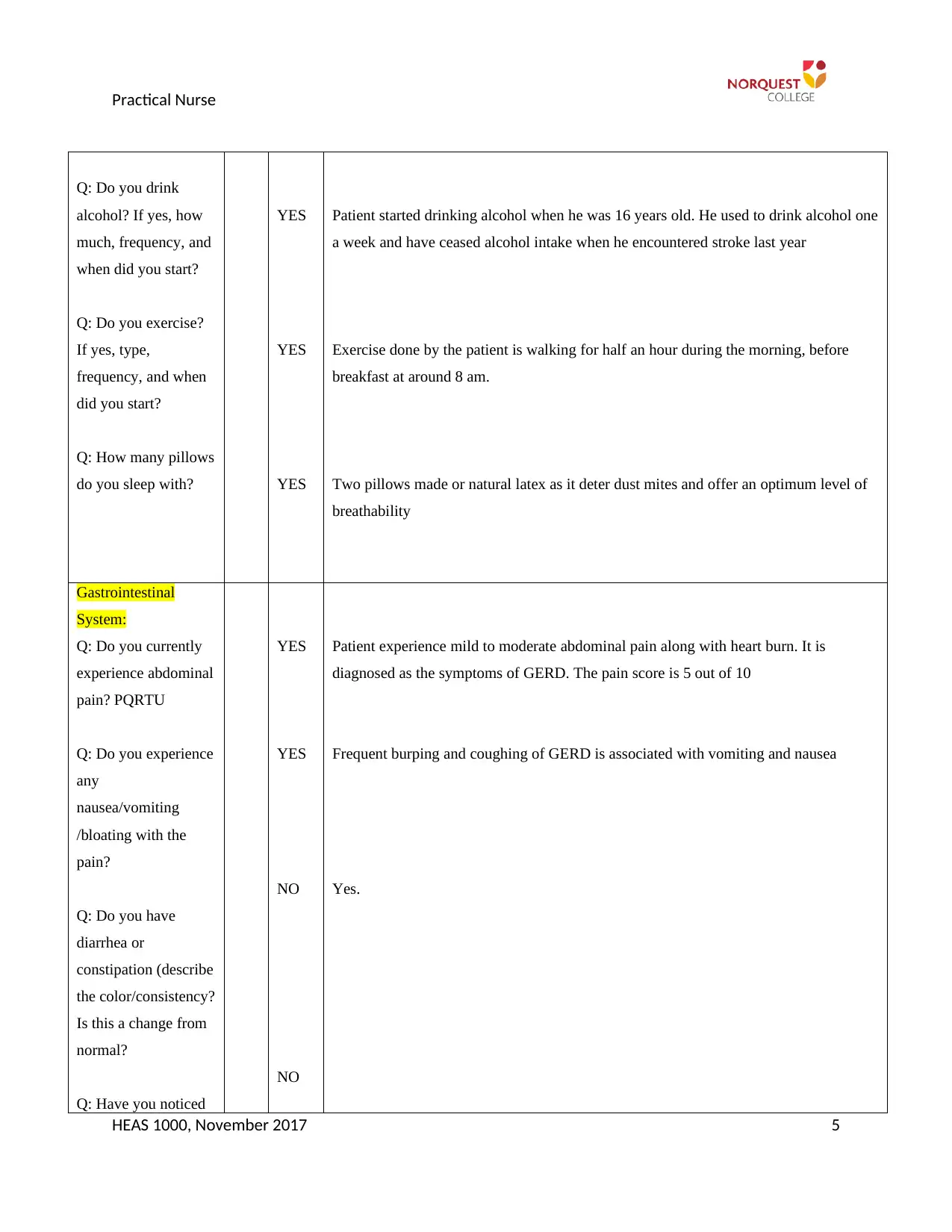
Q: Do you drink
alcohol? If yes, how
much, frequency, and
when did you start?
Q: Do you exercise?
If yes, type,
frequency, and when
did you start?
Q: How many pillows
do you sleep with?
YES
YES
YES
Patient started drinking alcohol when he was 16 years old. He used to drink alcohol one
a week and have ceased alcohol intake when he encountered stroke last year
Exercise done by the patient is walking for half an hour during the morning, before
breakfast at around 8 am.
Two pillows made or natural latex as it deter dust mites and offer an optimum level of
breathability
Gastrointestinal
System:
Q: Do you currently
experience abdominal
pain? PQRTU
Q: Do you experience
any
nausea/vomiting
/bloating with the
pain?
Q: Do you have
diarrhea or
constipation (describe
the color/consistency?
Is this a change from
normal?
Q: Have you noticed
YES
YES
NO
NO
Patient experience mild to moderate abdominal pain along with heart burn. It is
diagnosed as the symptoms of GERD. The pain score is 5 out of 10
Frequent burping and coughing of GERD is associated with vomiting and nausea
Yes.
HEAS 1000, November 2017 5
Q: Do you drink
alcohol? If yes, how
much, frequency, and
when did you start?
Q: Do you exercise?
If yes, type,
frequency, and when
did you start?
Q: How many pillows
do you sleep with?
YES
YES
YES
Patient started drinking alcohol when he was 16 years old. He used to drink alcohol one
a week and have ceased alcohol intake when he encountered stroke last year
Exercise done by the patient is walking for half an hour during the morning, before
breakfast at around 8 am.
Two pillows made or natural latex as it deter dust mites and offer an optimum level of
breathability
Gastrointestinal
System:
Q: Do you currently
experience abdominal
pain? PQRTU
Q: Do you experience
any
nausea/vomiting
/bloating with the
pain?
Q: Do you have
diarrhea or
constipation (describe
the color/consistency?
Is this a change from
normal?
Q: Have you noticed
YES
YES
NO
NO
Patient experience mild to moderate abdominal pain along with heart burn. It is
diagnosed as the symptoms of GERD. The pain score is 5 out of 10
Frequent burping and coughing of GERD is associated with vomiting and nausea
Yes.
HEAS 1000, November 2017 5
Practical Nurse
a change in your
urine?
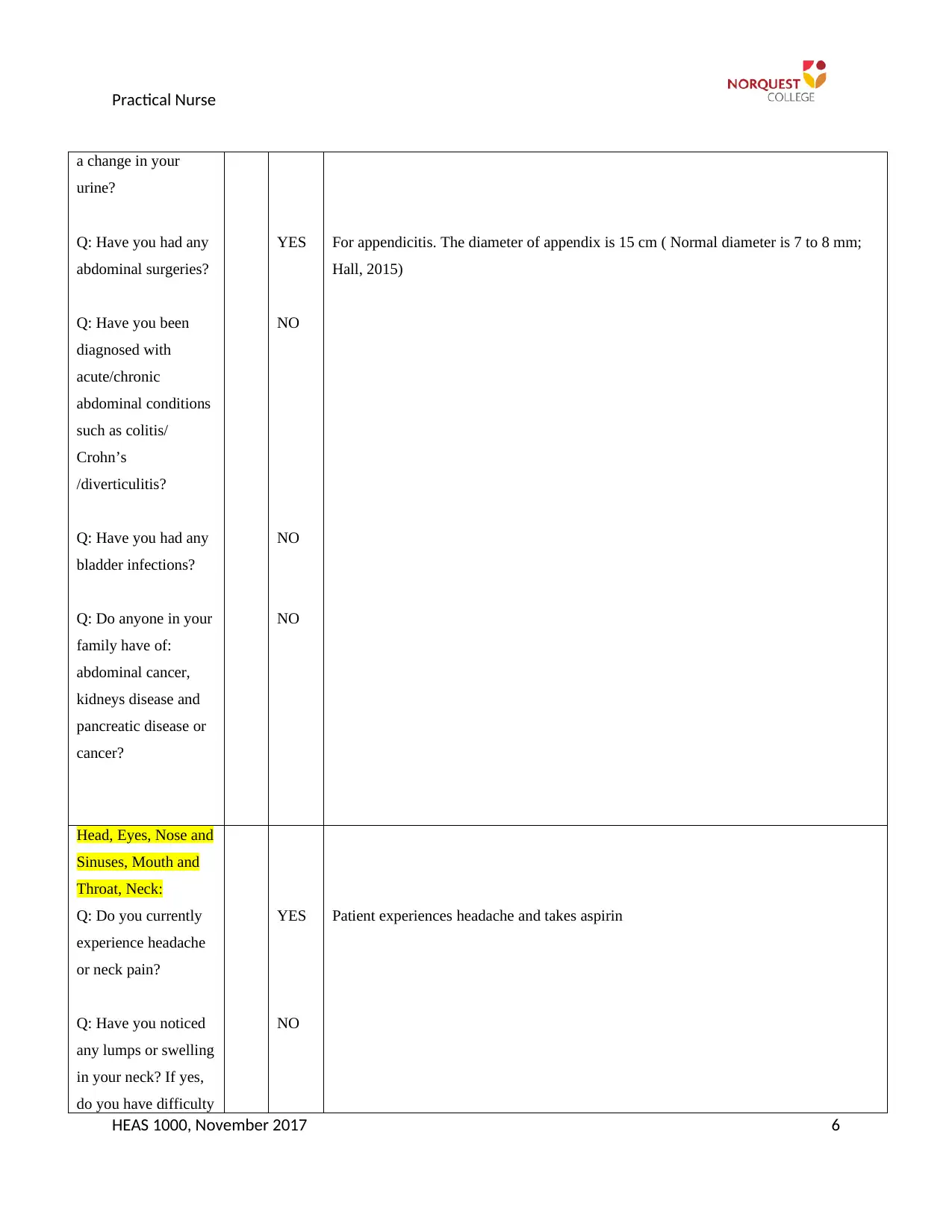
Q: Have you had any
abdominal surgeries?
Q: Have you been
diagnosed with
acute/chronic
abdominal conditions
such as colitis/
Crohn’s
/diverticulitis?
Q: Have you had any
bladder infections?
Q: Do anyone in your
family have of:
abdominal cancer,
kidneys disease and
pancreatic disease or
cancer?
YES
NO
NO
NO
For appendicitis. The diameter of appendix is 15 cm ( Normal diameter is 7 to 8 mm;
Hall, 2015)
Head, Eyes, Nose and
Sinuses, Mouth and
Throat, Neck:
Q: Do you currently
experience headache
or neck pain?
Q: Have you noticed
any lumps or swelling
in your neck? If yes,
do you have difficulty
YES
NO
Patient experiences headache and takes aspirin
HEAS 1000, November 2017 6
a change in your
urine?
Q: Have you had any
abdominal surgeries?
Q: Have you been
diagnosed with
acute/chronic
abdominal conditions
such as colitis/
Crohn’s
/diverticulitis?
Q: Have you had any
bladder infections?
Q: Do anyone in your
family have of:
abdominal cancer,
kidneys disease and
pancreatic disease or
cancer?
YES
NO
NO
NO
For appendicitis. The diameter of appendix is 15 cm ( Normal diameter is 7 to 8 mm;
Hall, 2015)
Head, Eyes, Nose and
Sinuses, Mouth and
Throat, Neck:
Q: Do you currently
experience headache
or neck pain?
Q: Have you noticed
any lumps or swelling
in your neck? If yes,
do you have difficulty
YES
NO
Patient experiences headache and takes aspirin
HEAS 1000, November 2017 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Practical Nurse
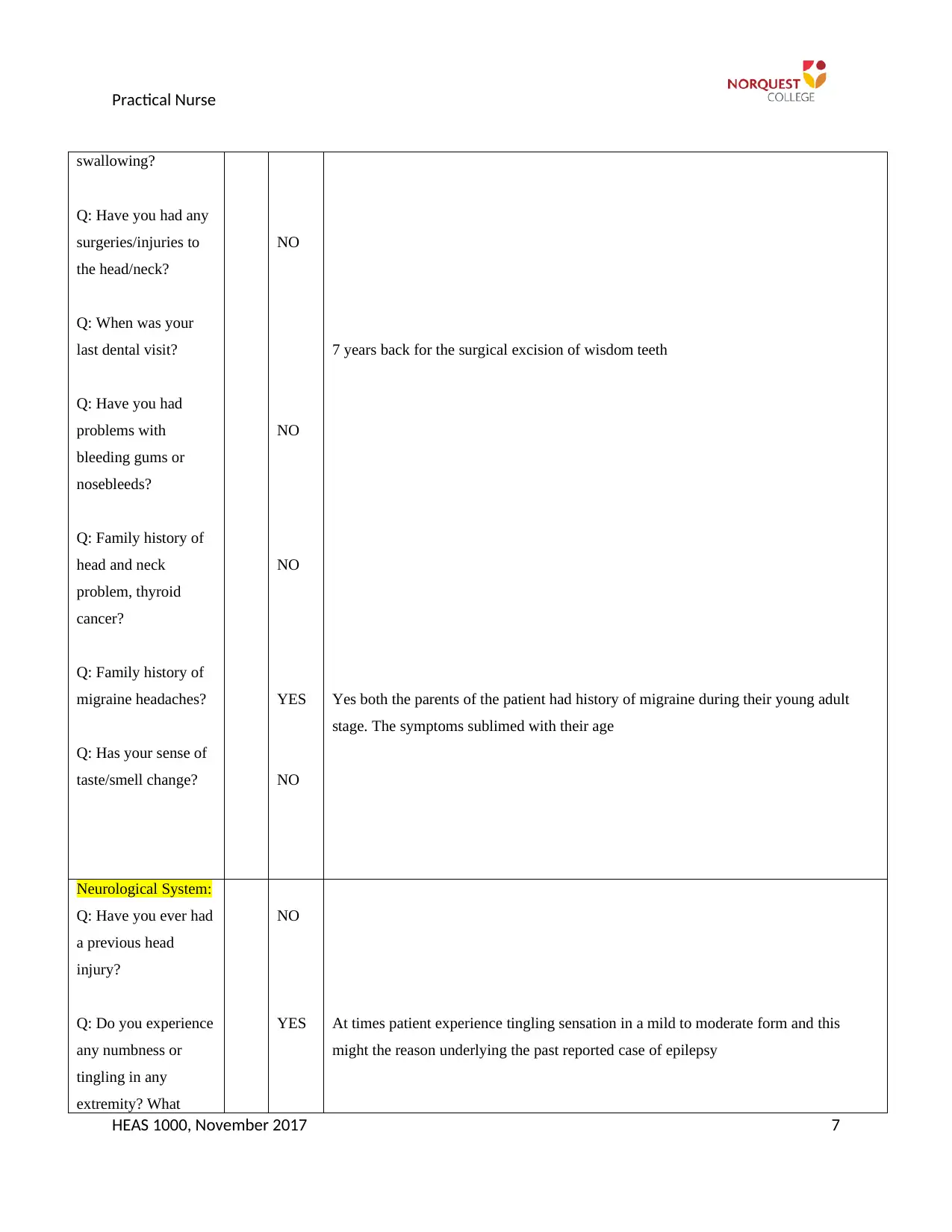
swallowing?
Q: Have you had any
surgeries/injuries to
the head/neck?
Q: When was your
last dental visit?
Q: Have you had
problems with
bleeding gums or
nosebleeds?
Q: Family history of
head and neck
problem, thyroid
cancer?
Q: Family history of
migraine headaches?
Q: Has your sense of
taste/smell change?
NO
NO
NO
YES
NO
7 years back for the surgical excision of wisdom teeth
Yes both the parents of the patient had history of migraine during their young adult
stage. The symptoms sublimed with their age
Neurological System:
Q: Have you ever had
a previous head
injury?
Q: Do you experience
any numbness or
tingling in any
extremity? What
NO
YES At times patient experience tingling sensation in a mild to moderate form and this
might the reason underlying the past reported case of epilepsy
HEAS 1000, November 2017 7
swallowing?
Q: Have you had any
surgeries/injuries to
the head/neck?
Q: When was your
last dental visit?
Q: Have you had
problems with
bleeding gums or
nosebleeds?
Q: Family history of
head and neck
problem, thyroid
cancer?
Q: Family history of
migraine headaches?
Q: Has your sense of
taste/smell change?
NO
NO
NO
YES
NO
7 years back for the surgical excision of wisdom teeth
Yes both the parents of the patient had history of migraine during their young adult
stage. The symptoms sublimed with their age
Neurological System:
Q: Have you ever had
a previous head
injury?
Q: Do you experience
any numbness or
tingling in any
extremity? What
NO
YES At times patient experience tingling sensation in a mild to moderate form and this
might the reason underlying the past reported case of epilepsy
HEAS 1000, November 2017 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Practical Nurse
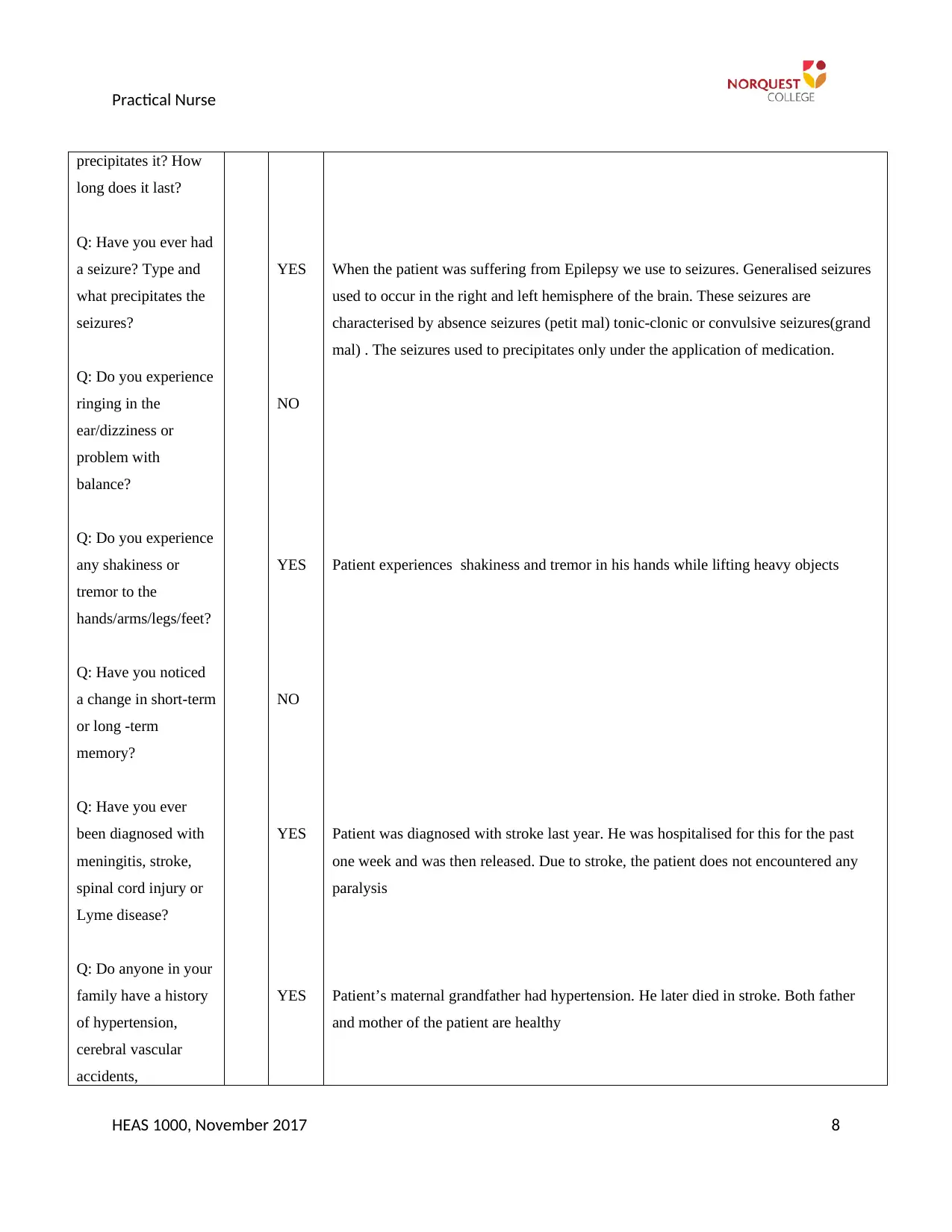
precipitates it? How
long does it last?
Q: Have you ever had
a seizure? Type and
what precipitates the
seizures?
Q: Do you experience
ringing in the
ear/dizziness or
problem with
balance?
Q: Do you experience
any shakiness or
tremor to the
hands/arms/legs/feet?
Q: Have you noticed
a change in short-term
or long -term
memory?
Q: Have you ever
been diagnosed with
meningitis, stroke,
spinal cord injury or
Lyme disease?
Q: Do anyone in your
family have a history
of hypertension,
cerebral vascular
accidents,
YES
NO
YES
NO
YES
YES
When the patient was suffering from Epilepsy we use to seizures. Generalised seizures
used to occur in the right and left hemisphere of the brain. These seizures are
characterised by absence seizures (petit mal) tonic-clonic or convulsive seizures(grand
mal) . The seizures used to precipitates only under the application of medication.
Patient experiences shakiness and tremor in his hands while lifting heavy objects
Patient was diagnosed with stroke last year. He was hospitalised for this for the past
one week and was then released. Due to stroke, the patient does not encountered any
paralysis
Patient’s maternal grandfather had hypertension. He later died in stroke. Both father
and mother of the patient are healthy
HEAS 1000, November 2017 8
precipitates it? How
long does it last?
Q: Have you ever had
a seizure? Type and
what precipitates the
seizures?
Q: Do you experience
ringing in the
ear/dizziness or
problem with
balance?
Q: Do you experience
any shakiness or
tremor to the
hands/arms/legs/feet?
Q: Have you noticed
a change in short-term
or long -term
memory?
Q: Have you ever
been diagnosed with
meningitis, stroke,
spinal cord injury or
Lyme disease?
Q: Do anyone in your
family have a history
of hypertension,
cerebral vascular
accidents,
YES
NO
YES
NO
YES
YES
When the patient was suffering from Epilepsy we use to seizures. Generalised seizures
used to occur in the right and left hemisphere of the brain. These seizures are
characterised by absence seizures (petit mal) tonic-clonic or convulsive seizures(grand
mal) . The seizures used to precipitates only under the application of medication.
Patient experiences shakiness and tremor in his hands while lifting heavy objects
Patient was diagnosed with stroke last year. He was hospitalised for this for the past
one week and was then released. Due to stroke, the patient does not encountered any
paralysis
Patient’s maternal grandfather had hypertension. He later died in stroke. Both father
and mother of the patient are healthy
HEAS 1000, November 2017 8
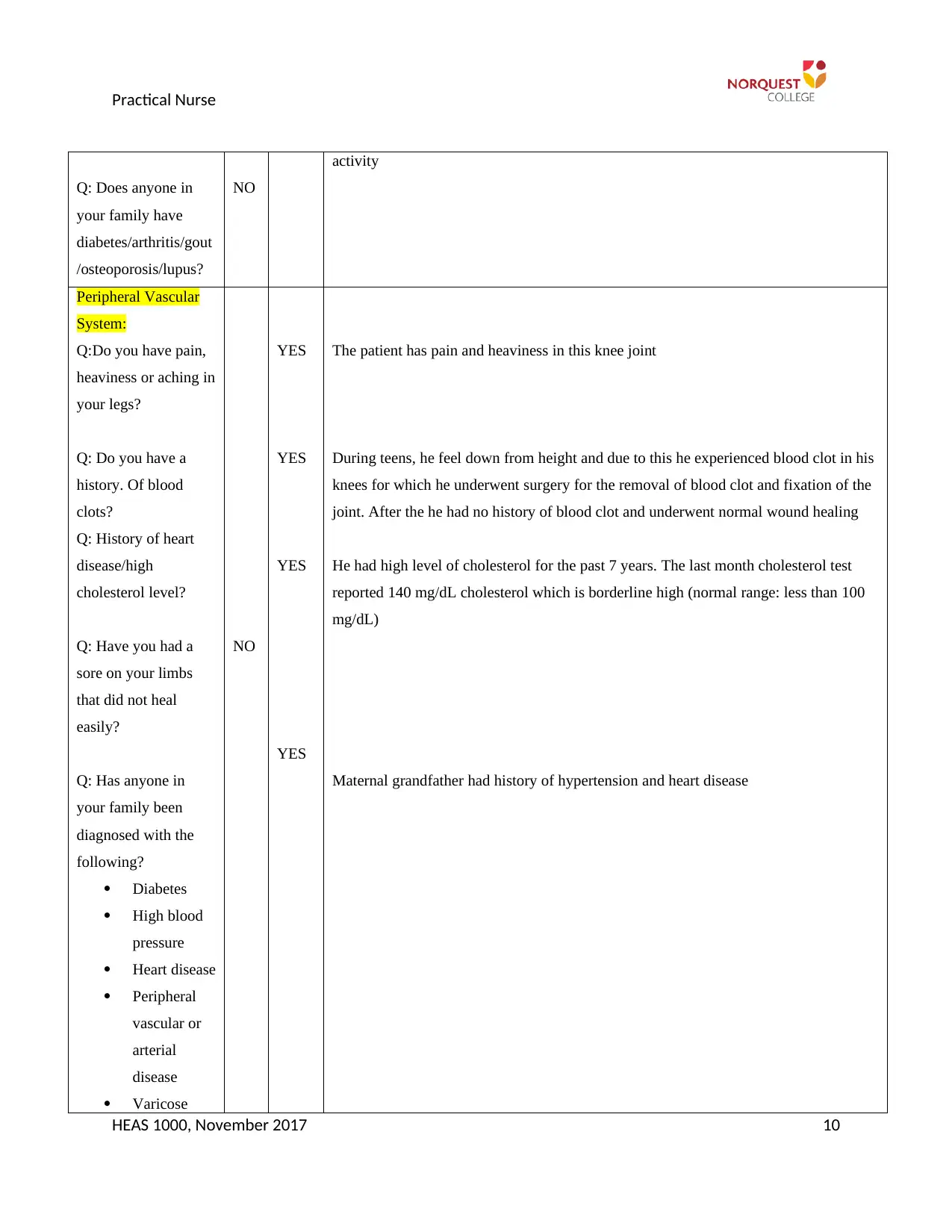
Practical Nurse
Alzheimer’s?
Urinary System:
Genital System:
Q: Sexual
orientation?
Q: Do have any
STI’s?
Q: How many
partners had you been
with?
NO
GAY
One
Musculoskeletal
System:
Q: Do you have any
joint/muscle or bone
pain or stiffness?
Q: Do you notices
any muscle
weakness?
Q: Have you had any
problems with or
received /joint/bones
YE
S
YE
S
YE
S
Patient experiences stiffness in the knees as he knee surgery during his teens
He has muscle weakness in the knees
Patient had difficulty in folding the knees at the time of running due. The patient had
knee injury during his knees and for that he had underwent a operation by an
orthopaedic. It is due to knee injury that the patient fail to participate in the physical
HEAS 1000, November 2017 9
Alzheimer’s?
Urinary System:
Genital System:
Q: Sexual
orientation?
Q: Do have any
STI’s?
Q: How many
partners had you been
with?
NO
GAY
One
Musculoskeletal
System:
Q: Do you have any
joint/muscle or bone
pain or stiffness?
Q: Do you notices
any muscle
weakness?
Q: Have you had any
problems with or
received /joint/bones
YE
S
YE
S
YE
S
Patient experiences stiffness in the knees as he knee surgery during his teens
He has muscle weakness in the knees
Patient had difficulty in folding the knees at the time of running due. The patient had
knee injury during his knees and for that he had underwent a operation by an
orthopaedic. It is due to knee injury that the patient fail to participate in the physical
HEAS 1000, November 2017 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Practical Nurse
Q: Does anyone in
your family have
diabetes/arthritis/gout
/osteoporosis/lupus?
NO
activity
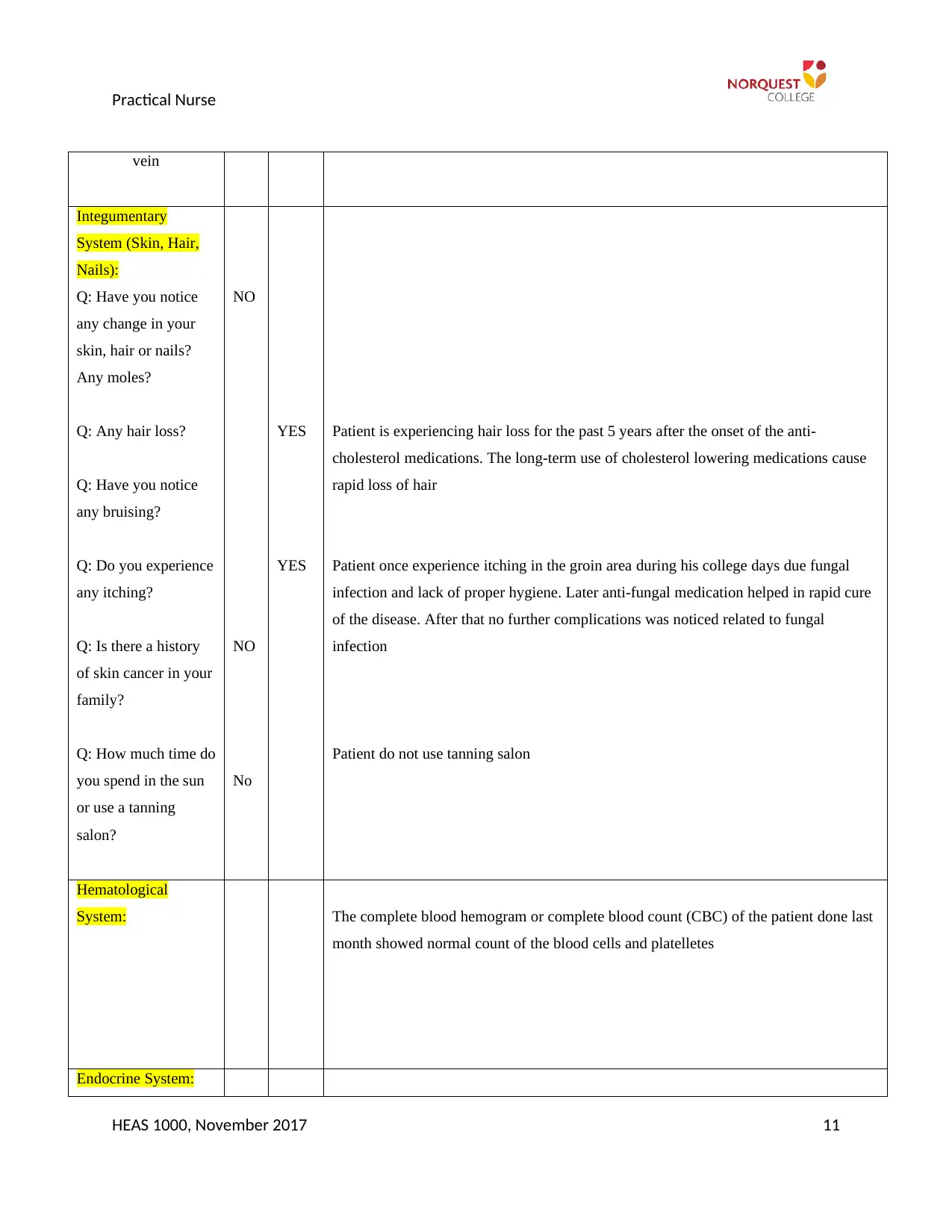
Peripheral Vascular
System:
Q:Do you have pain,
heaviness or aching in
your legs?
Q: Do you have a
history. Of blood
clots?
Q: History of heart
disease/high
cholesterol level?
Q: Have you had a
sore on your limbs
that did not heal
easily?
Q: Has anyone in
your family been
diagnosed with the
following?
Diabetes
High blood
pressure
Heart disease
Peripheral
vascular or
arterial
disease
Varicose
NO
YES
YES
YES
YES
The patient has pain and heaviness in this knee joint
During teens, he feel down from height and due to this he experienced blood clot in his
knees for which he underwent surgery for the removal of blood clot and fixation of the
joint. After the he had no history of blood clot and underwent normal wound healing
He had high level of cholesterol for the past 7 years. The last month cholesterol test
reported 140 mg/dL cholesterol which is borderline high (normal range: less than 100
mg/dL)
Maternal grandfather had history of hypertension and heart disease
HEAS 1000, November 2017 10
Q: Does anyone in
your family have
diabetes/arthritis/gout
/osteoporosis/lupus?
NO
activity
Peripheral Vascular
System:
Q:Do you have pain,
heaviness or aching in
your legs?
Q: Do you have a
history. Of blood
clots?
Q: History of heart
disease/high
cholesterol level?
Q: Have you had a
sore on your limbs
that did not heal
easily?
Q: Has anyone in
your family been
diagnosed with the
following?
Diabetes
High blood
pressure
Heart disease
Peripheral
vascular or
arterial
disease
Varicose
NO
YES
YES
YES
YES
The patient has pain and heaviness in this knee joint
During teens, he feel down from height and due to this he experienced blood clot in his
knees for which he underwent surgery for the removal of blood clot and fixation of the
joint. After the he had no history of blood clot and underwent normal wound healing
He had high level of cholesterol for the past 7 years. The last month cholesterol test
reported 140 mg/dL cholesterol which is borderline high (normal range: less than 100
mg/dL)
Maternal grandfather had history of hypertension and heart disease
HEAS 1000, November 2017 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Practical Nurse
vein
Integumentary
System (Skin, Hair,
Nails):
Q: Have you notice
any change in your
skin, hair or nails?
Any moles?
Q: Any hair loss?
Q: Have you notice
any bruising?
Q: Do you experience
any itching?
Q: Is there a history
of skin cancer in your
family?
Q: How much time do
you spend in the sun
or use a tanning
salon?
NO
NO
No
YES
YES
Patient is experiencing hair loss for the past 5 years after the onset of the anti-
cholesterol medications. The long-term use of cholesterol lowering medications cause
rapid loss of hair
Patient once experience itching in the groin area during his college days due fungal
infection and lack of proper hygiene. Later anti-fungal medication helped in rapid cure
of the disease. After that no further complications was noticed related to fungal
infection
Patient do not use tanning salon
Hematological
System: The complete blood hemogram or complete blood count (CBC) of the patient done last
month showed normal count of the blood cells and platelletes
Endocrine System:
HEAS 1000, November 2017 11
vein
Integumentary
System (Skin, Hair,
Nails):
Q: Have you notice
any change in your
skin, hair or nails?
Any moles?
Q: Any hair loss?
Q: Have you notice
any bruising?
Q: Do you experience
any itching?
Q: Is there a history
of skin cancer in your
family?
Q: How much time do
you spend in the sun
or use a tanning
salon?
NO
NO
No
YES
YES
Patient is experiencing hair loss for the past 5 years after the onset of the anti-
cholesterol medications. The long-term use of cholesterol lowering medications cause
rapid loss of hair
Patient once experience itching in the groin area during his college days due fungal
infection and lack of proper hygiene. Later anti-fungal medication helped in rapid cure
of the disease. After that no further complications was noticed related to fungal
infection
Patient do not use tanning salon
Hematological
System: The complete blood hemogram or complete blood count (CBC) of the patient done last
month showed normal count of the blood cells and platelletes
Endocrine System:
HEAS 1000, November 2017 11
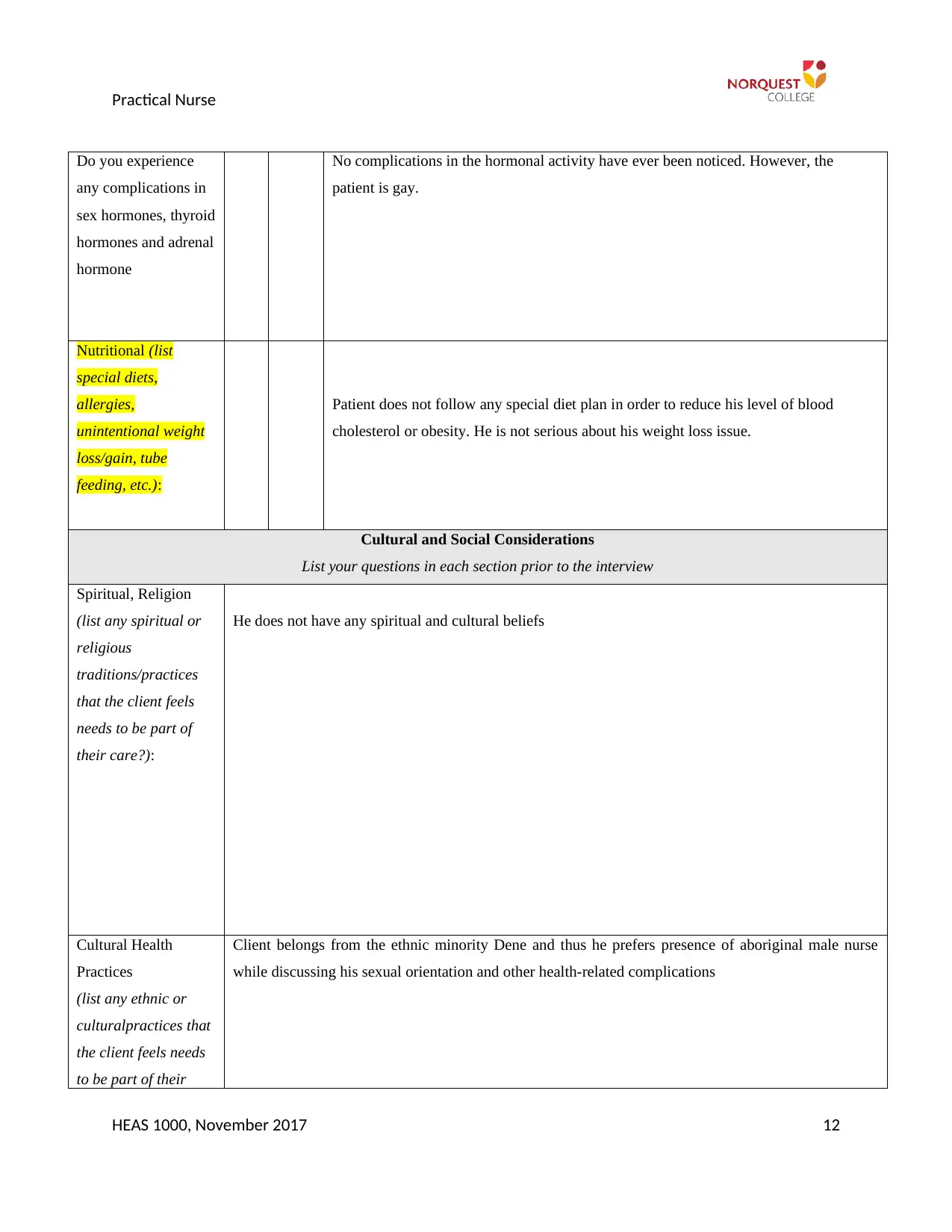
Practical Nurse
Do you experience
any complications in
sex hormones, thyroid
hormones and adrenal
hormone
No complications in the hormonal activity have ever been noticed. However, the
patient is gay.
Nutritional (list
special diets,
allergies,
unintentional weight
loss/gain, tube
feeding, etc.):
Patient does not follow any special diet plan in order to reduce his level of blood
cholesterol or obesity. He is not serious about his weight loss issue.
Cultural and Social Considerations
List your questions in each section prior to the interview
Spiritual, Religion
(list any spiritual or
religious
traditions/practices
that the client feels
needs to be part of
their care?):
He does not have any spiritual and cultural beliefs
Cultural Health
Practices
(list any ethnic or
culturalpractices that
the client feels needs
to be part of their
Client belongs from the ethnic minority Dene and thus he prefers presence of aboriginal male nurse
while discussing his sexual orientation and other health-related complications
HEAS 1000, November 2017 12
Do you experience
any complications in
sex hormones, thyroid
hormones and adrenal
hormone
No complications in the hormonal activity have ever been noticed. However, the
patient is gay.
Nutritional (list
special diets,
allergies,
unintentional weight
loss/gain, tube
feeding, etc.):
Patient does not follow any special diet plan in order to reduce his level of blood
cholesterol or obesity. He is not serious about his weight loss issue.
Cultural and Social Considerations
List your questions in each section prior to the interview
Spiritual, Religion
(list any spiritual or
religious
traditions/practices
that the client feels
needs to be part of
their care?):
He does not have any spiritual and cultural beliefs
Cultural Health
Practices
(list any ethnic or
culturalpractices that
the client feels needs
to be part of their
Client belongs from the ethnic minority Dene and thus he prefers presence of aboriginal male nurse
while discussing his sexual orientation and other health-related complications
HEAS 1000, November 2017 12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





