Capstone Project: Quality Improvement Proposal on Pressure Injuries
VerifiedAdded on 2022/09/29
|14
|3357
|39
Project
AI Summary
This quality improvement project proposal focuses on reducing the incidence of pressure injuries in hospitalized patients. The project begins with an introduction to the problem, emphasizing the significance of pressure injuries as a measure of patient care quality and referencing the National Safety and Quality Healthcare Service (NSQHS) standards. The background section provides a detailed overview of pressure injuries, including their causes, risk factors (such as immobility, malnutrition, sensory loss, and medication use), and the classification of pressure injuries according to the National Pressure Ulcer Advisory Panel (NPUAP). The proposal outlines a baseline measurement strategy using the Braden Scale for risk assessment, followed by an ethical considerations section. The core of the project is an educational intervention for nurses, designed to improve their knowledge of pressure injury prevention and management. The strategy employs a three-cycle PDSA (Plan-Do-Study-Act) approach, targeting education, awareness, and implementation. The proposal also discusses the project's limitations and strengths and concludes with a call to action for improved patient care outcomes. The proposal includes an introduction, background and rationale, baseline measurement, ethical considerations, design, strategy, and limitations and strengths.

Running head: QUALITY IMPROVEMENT PROJECT 1
Quality improvement project
Name of Student
Name of Institution
Author note
Quality improvement project
Name of Student
Name of Institution
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
QUALITY IMPROVEMENT PROJECT 2
Table of Contents
Introduction....................................................................................................................................3
Background....................................................................................................................................3
Baseline measurement...................................................................................................................7
Ethics...............................................................................................................................................8
Design..............................................................................................................................................8
Strategy Limitations and strengths..............................................................................................8
Lessons and limitation...................................................................................................................9
Conclusion......................................................................................................................................9
References......................................................................................................................................11
Table of Contents
Introduction....................................................................................................................................3
Background....................................................................................................................................3
Baseline measurement...................................................................................................................7
Ethics...............................................................................................................................................8
Design..............................................................................................................................................8
Strategy Limitations and strengths..............................................................................................8
Lessons and limitation...................................................................................................................9
Conclusion......................................................................................................................................9
References......................................................................................................................................11

QUALITY IMPROVEMENT PROJECT 3
Quality Improvement Project
Introduction
The frequency of pressure injuries in patients is often used as a measure of patient care
quality. Pressure injuries are injuries that occur on soft tissues when they are compressed by a
bony or hard structure. They are caused by friction or long-term pressure. Pressure injuries are
common in patients who are bedridden and patients who are immobilized. The National Safety
and Quality Healthcare Service (NHQHS) has provided a clinical governance standard to help
decrease the total figure of patients in hospital who get pressure injuries
(Safetyandquality.gov.au., 2012).
The goal of this project is to determine the causative factors and help prevent patients
from acquiring pressure injuries during their stay in hospital. Currently, the total sum of patients
who are diagnosed with patient injuries is very high. Determining the causative factors will in
developing strategies that will prevent pressure injuries and improve the overall patient care
quality
Background
Pressure injuries are described as a localized damage to the soft tissue. The injury could
be presented as an open ulcer or an intact skin injury. Tissue have a certain tolerance to pressure.
The skin acts a s a cushion and protects the skeleton during a shift in pressure. Prolonged
exposure to pressure reduces the tissue tolerance. Pressure ulcers are usually very pain and
uncomfortable. Pressure wounds are often confused by Moisture Associated skin Damage
(MASD), frictional burns, Medical Adhesive Related Skin Injury (MARSI), Intertriginous
Dermatitis (ITD) and Incontinence Associated Dermatitis (IAD). Localized soft tissue that are
exposed to pressure for a prolonged duration result in the occlusion of blood flow. Nutrients and
Quality Improvement Project
Introduction
The frequency of pressure injuries in patients is often used as a measure of patient care
quality. Pressure injuries are injuries that occur on soft tissues when they are compressed by a
bony or hard structure. They are caused by friction or long-term pressure. Pressure injuries are
common in patients who are bedridden and patients who are immobilized. The National Safety
and Quality Healthcare Service (NHQHS) has provided a clinical governance standard to help
decrease the total figure of patients in hospital who get pressure injuries
(Safetyandquality.gov.au., 2012).
The goal of this project is to determine the causative factors and help prevent patients
from acquiring pressure injuries during their stay in hospital. Currently, the total sum of patients
who are diagnosed with patient injuries is very high. Determining the causative factors will in
developing strategies that will prevent pressure injuries and improve the overall patient care
quality
Background
Pressure injuries are described as a localized damage to the soft tissue. The injury could
be presented as an open ulcer or an intact skin injury. Tissue have a certain tolerance to pressure.
The skin acts a s a cushion and protects the skeleton during a shift in pressure. Prolonged
exposure to pressure reduces the tissue tolerance. Pressure ulcers are usually very pain and
uncomfortable. Pressure wounds are often confused by Moisture Associated skin Damage
(MASD), frictional burns, Medical Adhesive Related Skin Injury (MARSI), Intertriginous
Dermatitis (ITD) and Incontinence Associated Dermatitis (IAD). Localized soft tissue that are
exposed to pressure for a prolonged duration result in the occlusion of blood flow. Nutrients and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
QUALITY IMPROVEMENT PROJECT 4
oxygen fail to reach the surrounding tissues and ischemia occurs. Re perfusion injury follows
and the cell undergoes obliteration and eventually necrosis occurs.
There are various threats and the key risk factor is immobility. Patients who hardly move
from their bed or their wheelchair have a high probability of forming pressure injuries. Children
who ae younger than the age of 36 moths usually have a head that is larger in comparison to the
rest of the body. Such children have a higher probability of acquiring a pressure injury in the
occipital region if the lie for long durations. Prolonged stay in an operating theater, mechanical
ventilation, intensive care unit, or in a non-invasive ventilation machine increase the chance of
forming a localized damage to the soft tissues.
Malnutrition is also a causative factor, especially in African countries like Botswana and
Zimbabwe. It is important to assess the patient’s dietary needs. A lower body mass intake
increases the probability of the development of pressure injuries. Individuals who are
underweight have a low muscle to bone ratio and the bones may exert unwanted pressure on the
soft tissue. Patients who are also overweight have a high probability of developing this condition.
Patients who are overweight are prone to experiencing friction between the various organs
especially in the limbs and at the joints. Patient who experience rapid weight loss either due to a
diet or a medical condition such as diuresis, are also at risk of acquiring a pressure injury.
Another threat is sensory loss. Patients who suffer from neurological diseases like spinal
cord injuries, delirium, dementia and neuropathy have a higher probability of forming pressure
injuries. Loss of the sensory neurons inhibit the patient form feeling pain. Most patients with
neurological diseases, are not aware that that they have pressure injuries until they develop into
stage 3 or four. Routine check ups are recommended for these patients to detect pressure injuries
oxygen fail to reach the surrounding tissues and ischemia occurs. Re perfusion injury follows
and the cell undergoes obliteration and eventually necrosis occurs.
There are various threats and the key risk factor is immobility. Patients who hardly move
from their bed or their wheelchair have a high probability of forming pressure injuries. Children
who ae younger than the age of 36 moths usually have a head that is larger in comparison to the
rest of the body. Such children have a higher probability of acquiring a pressure injury in the
occipital region if the lie for long durations. Prolonged stay in an operating theater, mechanical
ventilation, intensive care unit, or in a non-invasive ventilation machine increase the chance of
forming a localized damage to the soft tissues.
Malnutrition is also a causative factor, especially in African countries like Botswana and
Zimbabwe. It is important to assess the patient’s dietary needs. A lower body mass intake
increases the probability of the development of pressure injuries. Individuals who are
underweight have a low muscle to bone ratio and the bones may exert unwanted pressure on the
soft tissue. Patients who are also overweight have a high probability of developing this condition.
Patients who are overweight are prone to experiencing friction between the various organs
especially in the limbs and at the joints. Patient who experience rapid weight loss either due to a
diet or a medical condition such as diuresis, are also at risk of acquiring a pressure injury.
Another threat is sensory loss. Patients who suffer from neurological diseases like spinal
cord injuries, delirium, dementia and neuropathy have a higher probability of forming pressure
injuries. Loss of the sensory neurons inhibit the patient form feeling pain. Most patients with
neurological diseases, are not aware that that they have pressure injuries until they develop into
stage 3 or four. Routine check ups are recommended for these patients to detect pressure injuries
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
QUALITY IMPROVEMENT PROJECT 5
early. Patients who have recently suffered a stroke, trauma or multiple sclerosis are also at a high
probability of acquiring a pressure injury (Corbett, Funk, Fortunato & O'Sullivan, 2017)
Using certain medications reduces the sensation in the extremities which increases the
probability of acquiring a pressure wound. Medications such as muscle relaxants, nerve blocks,
analgesics, epidurals, hypnotics and sedatives reduce the patient’s sensation (Metsalu & Vilo,
2015).
The microclimate also holds a major role in the development of pressure injuries. High
humidity and temperature at the surface of the skin increases the probability of forming pressure
wounds. Countries that experience high temperatures like India and the United Arab Emirated,
have individuals who are at a high probability of forming a pressure injury. Nurses should ensure
that patient sleep of dry beddings and the temperatures in the patient wards are regulated
appropriately. There should be proper airflow into the rooms of the patients. Patients should not
be left to sit in a wet nappy or a wet bed for a long duration (Gefen, Kottner & Santamaria,
2016).
There are other intrinsic factors which increase the possibility of fostering a pressure
injury. Most of these intrinsic factors impairs, sensation, lymphatic functions, sensation and
oxygen delivery. They include, smoking, cardiopulmonary diseases, anemia, depressed immune
system, low blood pressures peripheral arterial diseases, diabetes, carcinoma, lymphomas, renal
failures, fever, and dehydration (Roberts, 2015).
Pressure injuries have major implications; they result in pain, delayed recovery, increased
hospital stays, increased medical costs, probability of infection among others. Without
forgetting, pressure injurie s that have developed into stage four are not covered by most medical
insurance policies thus increasing the medical cost (Razmus & Bergquist-Beringer, 2017).
early. Patients who have recently suffered a stroke, trauma or multiple sclerosis are also at a high
probability of acquiring a pressure injury (Corbett, Funk, Fortunato & O'Sullivan, 2017)
Using certain medications reduces the sensation in the extremities which increases the
probability of acquiring a pressure wound. Medications such as muscle relaxants, nerve blocks,
analgesics, epidurals, hypnotics and sedatives reduce the patient’s sensation (Metsalu & Vilo,
2015).
The microclimate also holds a major role in the development of pressure injuries. High
humidity and temperature at the surface of the skin increases the probability of forming pressure
wounds. Countries that experience high temperatures like India and the United Arab Emirated,
have individuals who are at a high probability of forming a pressure injury. Nurses should ensure
that patient sleep of dry beddings and the temperatures in the patient wards are regulated
appropriately. There should be proper airflow into the rooms of the patients. Patients should not
be left to sit in a wet nappy or a wet bed for a long duration (Gefen, Kottner & Santamaria,
2016).
There are other intrinsic factors which increase the possibility of fostering a pressure
injury. Most of these intrinsic factors impairs, sensation, lymphatic functions, sensation and
oxygen delivery. They include, smoking, cardiopulmonary diseases, anemia, depressed immune
system, low blood pressures peripheral arterial diseases, diabetes, carcinoma, lymphomas, renal
failures, fever, and dehydration (Roberts, 2015).
Pressure injuries have major implications; they result in pain, delayed recovery, increased
hospital stays, increased medical costs, probability of infection among others. Without
forgetting, pressure injurie s that have developed into stage four are not covered by most medical
insurance policies thus increasing the medical cost (Razmus & Bergquist-Beringer, 2017).
QUALITY IMPROVEMENT PROJECT 6
The National Pressure Ulcer Advisory Panel (NPUAP) developed a classification system
for pressure injury. Using this classification, it is possible to categorize pressure injuries based on
their severity. It is no recommended to change the stage of the pressure injury as healing occurs.
The first category is Stage 1. In this stage there is non blanchable erythema and the skin appears
darker or pigmented. At this stage the skin is intact. The second category is Stage 2. At this
stage, the epidermis is exposed, and the area is pink and moist. The skin may be ruptured or
intact. The third category, Stage 3, occurs when there is full skin lose. The granulation tissues
and adipose layer are visible. In some cases, slough or eschar is present. The last category is
stage 4. At this stage, bone, muscles, ligament or tendons may be visible in the ulcer. Eschar and
slough are resent. Without proper interventions, the pressure injury can progress rapidly from
one stage to the next (Icn.ch., 2013).
NPUAP has also classified wound care according the various stages. Pressure injurie stat
are in stage 1 should be clean regularly then covered with a transparent film. For stage 2 pressure
wounds, it is recommended that absorptive dressing should be used to absorb any excess fluid.
Stage three and four wounds should be treated for infection. Necrotic tissues should eb debrided
and covered with the appropriate dressing. If necessary, surgery may be done to debride
extensive necrotic tissues (Latimer, Gillespie & Chaboyer, 2017).
Previous strategies developed by the NSQHS to manage pressure injuries involved
conducting a risk assessment on all patients who are hospitalized. Dressings should be managed
appropriately. The wound size is then documented. For patients who are in mild pain, oral non
opioid medications are administered. Patients that are in moderate to severe pain are
administered with opioid analgesics. Pain medication is administered before a dressing change or
debridement. Infected wounds are treated with antibiotics and additional culture should be done.
The National Pressure Ulcer Advisory Panel (NPUAP) developed a classification system
for pressure injury. Using this classification, it is possible to categorize pressure injuries based on
their severity. It is no recommended to change the stage of the pressure injury as healing occurs.
The first category is Stage 1. In this stage there is non blanchable erythema and the skin appears
darker or pigmented. At this stage the skin is intact. The second category is Stage 2. At this
stage, the epidermis is exposed, and the area is pink and moist. The skin may be ruptured or
intact. The third category, Stage 3, occurs when there is full skin lose. The granulation tissues
and adipose layer are visible. In some cases, slough or eschar is present. The last category is
stage 4. At this stage, bone, muscles, ligament or tendons may be visible in the ulcer. Eschar and
slough are resent. Without proper interventions, the pressure injury can progress rapidly from
one stage to the next (Icn.ch., 2013).
NPUAP has also classified wound care according the various stages. Pressure injurie stat
are in stage 1 should be clean regularly then covered with a transparent film. For stage 2 pressure
wounds, it is recommended that absorptive dressing should be used to absorb any excess fluid.
Stage three and four wounds should be treated for infection. Necrotic tissues should eb debrided
and covered with the appropriate dressing. If necessary, surgery may be done to debride
extensive necrotic tissues (Latimer, Gillespie & Chaboyer, 2017).
Previous strategies developed by the NSQHS to manage pressure injuries involved
conducting a risk assessment on all patients who are hospitalized. Dressings should be managed
appropriately. The wound size is then documented. For patients who are in mild pain, oral non
opioid medications are administered. Patients that are in moderate to severe pain are
administered with opioid analgesics. Pain medication is administered before a dressing change or
debridement. Infected wounds are treated with antibiotics and additional culture should be done.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
QUALITY IMPROVEMENT PROJECT 7
The patients progress is monitored and documented. Psychosocial support is provided to the
patient if need be (Jackson et al., 2017).
Baseline measurement
By comparison of the previous strategies, it is possible to develop a new solution for
preventing pressure injuries. Previous strategies involved developing a palliative care. The
patients are treated once the symptoms arise. The pressure wound is treated once it has
developed. In most scenarios the patient seeks medical attention after the pressure injury has
progressed and it in stage three or four. The strategy used is to conduct a risk assessment for
pressure injury. By conducting a risk assessment, it is possible to foresee the possibility of the
patient acquiring a pressure injury during their hospital stay. Appropriate measures can be taken
to ensure that the patient does not develop a pressure injury. The Braden Scale can be used as a
risk assessment tool to identify patients who are at a high probability of forming a pressure
injury. The risk assessment tool is used within 8 hours of admission. Additional threats are also
be identified, for example, fragile skin, previously healed or existing pressure injuries, impaired
perfusion to the extremities due to diabetes or vascular diseases, pain in areas that have been
exposed to pressure. Chairfast and bed fast patients are at a high probability of forming pressure
injurie and are examined regularly. Risk assessment is repeated during every shift for patients in
acute care, weekly for patients who are in long term care and every visit for patients who are in
home care. after the risk assessment the healthcare worker develops a nursing care plan based on
the assessment and prioritize address issues (Usher et al., 2018).
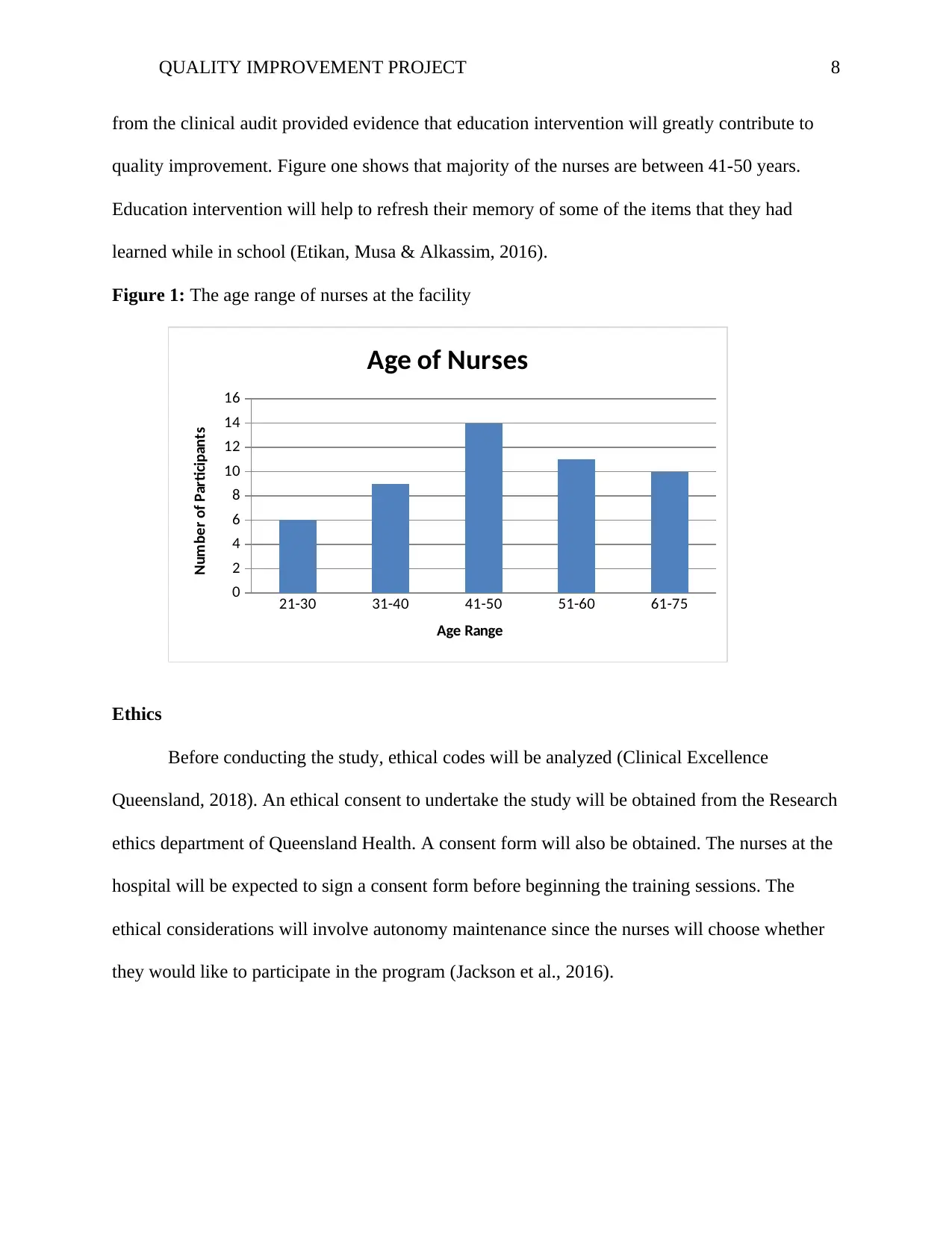
According to the data collected in the clinical audit, educating the nurses on the risk
factors, it is possible to prevent pressure injury. The clinical audit provided results showing that
most nurses were not aware of the possible threats that lead to pressure injuries. The information
The patients progress is monitored and documented. Psychosocial support is provided to the
patient if need be (Jackson et al., 2017).
Baseline measurement
By comparison of the previous strategies, it is possible to develop a new solution for
preventing pressure injuries. Previous strategies involved developing a palliative care. The
patients are treated once the symptoms arise. The pressure wound is treated once it has
developed. In most scenarios the patient seeks medical attention after the pressure injury has
progressed and it in stage three or four. The strategy used is to conduct a risk assessment for
pressure injury. By conducting a risk assessment, it is possible to foresee the possibility of the
patient acquiring a pressure injury during their hospital stay. Appropriate measures can be taken
to ensure that the patient does not develop a pressure injury. The Braden Scale can be used as a
risk assessment tool to identify patients who are at a high probability of forming a pressure
injury. The risk assessment tool is used within 8 hours of admission. Additional threats are also
be identified, for example, fragile skin, previously healed or existing pressure injuries, impaired
perfusion to the extremities due to diabetes or vascular diseases, pain in areas that have been
exposed to pressure. Chairfast and bed fast patients are at a high probability of forming pressure
injurie and are examined regularly. Risk assessment is repeated during every shift for patients in
acute care, weekly for patients who are in long term care and every visit for patients who are in
home care. after the risk assessment the healthcare worker develops a nursing care plan based on
the assessment and prioritize address issues (Usher et al., 2018).
According to the data collected in the clinical audit, educating the nurses on the risk
factors, it is possible to prevent pressure injury. The clinical audit provided results showing that
most nurses were not aware of the possible threats that lead to pressure injuries. The information
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
QUALITY IMPROVEMENT PROJECT 8
from the clinical audit provided evidence that education intervention will greatly contribute to
quality improvement. Figure one shows that majority of the nurses are between 41-50 years.
Education intervention will help to refresh their memory of some of the items that they had
learned while in school (Etikan, Musa & Alkassim, 2016).
Figure 1: The age range of nurses at the facility
21-30 31-40 41-50 51-60 61-75
0
2
4
6
8
10
12
14
16
Age of Nurses
Age Range
Number of Participants
Ethics
Before conducting the study, ethical codes will be analyzed (Clinical Excellence
Queensland, 2018). An ethical consent to undertake the study will be obtained from the Research
ethics department of Queensland Health. A consent form will also be obtained. The nurses at the
hospital will be expected to sign a consent form before beginning the training sessions. The
ethical considerations will involve autonomy maintenance since the nurses will choose whether
they would like to participate in the program (Jackson et al., 2016).
from the clinical audit provided evidence that education intervention will greatly contribute to
quality improvement. Figure one shows that majority of the nurses are between 41-50 years.
Education intervention will help to refresh their memory of some of the items that they had
learned while in school (Etikan, Musa & Alkassim, 2016).
Figure 1: The age range of nurses at the facility
21-30 31-40 41-50 51-60 61-75
0
2
4
6
8
10
12
14
16
Age of Nurses
Age Range
Number of Participants
Ethics
Before conducting the study, ethical codes will be analyzed (Clinical Excellence
Queensland, 2018). An ethical consent to undertake the study will be obtained from the Research
ethics department of Queensland Health. A consent form will also be obtained. The nurses at the
hospital will be expected to sign a consent form before beginning the training sessions. The
ethical considerations will involve autonomy maintenance since the nurses will choose whether
they would like to participate in the program (Jackson et al., 2016).
QUALITY IMPROVEMENT PROJECT 9
Design
The intervention for pressure injuries is education intervention. The nurses will undergo a
training program where they will be educated on pressure injuries, the causative factors and the
preventive measures. The reason behind developing this intervention is most nurses do not know
the causative factors for pressure injuries and the preventive actions that can be taken. The
assumption made in this design is that majority of the nurses have very little information on
pressure injuries. This strategy is expected to work because evidence-based research has shown
that educational intervention has been very helpful in improving quality care. Through education
intervention, quality issues such as healthcare associated infection were resolved. This
intervention can be made long term by including a routing training session every financial year.
This will enable the nurses to refresh their knowledge and will enable new nurses to learn about
patient care quality improvement (South West Hospital and Health Service, 2019).
Strategy Limitations and strengths
Three PDSA cycle will be used in this design. The first cycle the aim will be to educate
the nurses on the probability factors of pressure injuries and the preventive measures. The
hypothesis is there are several factors that result in pressure injuries. The strategy for this cycle is
to hold a workshop or a training session where the nurses will be educated on the causative
factors for pressure injuries. The second PDSA cycle will have an aim of creating awareness on
pressure injuries. The strategy for this PDSA cycle is to create posters and billboards that explain
pressure injuries. The third PDSA cycle will have an aim of implementing the information
learned from the education intervention into daily practice the hypothesis of this cycle is through
implementation the knowledge learned will be retained the nurses. The strategy for this cycle is
Design
The intervention for pressure injuries is education intervention. The nurses will undergo a
training program where they will be educated on pressure injuries, the causative factors and the
preventive measures. The reason behind developing this intervention is most nurses do not know
the causative factors for pressure injuries and the preventive actions that can be taken. The
assumption made in this design is that majority of the nurses have very little information on
pressure injuries. This strategy is expected to work because evidence-based research has shown
that educational intervention has been very helpful in improving quality care. Through education
intervention, quality issues such as healthcare associated infection were resolved. This
intervention can be made long term by including a routing training session every financial year.
This will enable the nurses to refresh their knowledge and will enable new nurses to learn about
patient care quality improvement (South West Hospital and Health Service, 2019).
Strategy Limitations and strengths
Three PDSA cycle will be used in this design. The first cycle the aim will be to educate
the nurses on the probability factors of pressure injuries and the preventive measures. The
hypothesis is there are several factors that result in pressure injuries. The strategy for this cycle is
to hold a workshop or a training session where the nurses will be educated on the causative
factors for pressure injuries. The second PDSA cycle will have an aim of creating awareness on
pressure injuries. The strategy for this PDSA cycle is to create posters and billboards that explain
pressure injuries. The third PDSA cycle will have an aim of implementing the information
learned from the education intervention into daily practice the hypothesis of this cycle is through
implementation the knowledge learned will be retained the nurses. The strategy for this cycle is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
QUALITY IMPROVEMENT PROJECT 10
nursing the nurses create awareness about pressure injury to the patients (Gray & Giuliano,
2018).
The key learning from the first cycle is that education intervention was very effective.
The nurses were more knowledgeable on the causative factors and could explain to a patient. the
key learning from the second PDSA cycle is that posters are more effective I creating awareness
as compared to billboards. The key learning from the third cycle is that creating awareness to the
patient using the nurse was not as effective. This was not anticipated during the study (Roberts et
al., 2016)
Lessons and limitation
The major lesson is that educating the nurses helps to improve patient care. Through
understanding the risk factors, the nurses can prevent more cases of pressure injuries form
arising. The major limitation of this study is that the education intervention will have to be
repeated each time a new staff joins the healthcare facility (Nguyen, Chaboyer & Whitty, 2015).
Conclusion
In conclusion, pressure injuries are caused by several factors; they include, malnutrition,
physical immobility, chronic illnesses among others. The purpose of this project was to ascertain
the causative factors and help prevent patients from acquiring pressure injuries during their stay
in hospital. The strategy chosen, helped to achieve the aim. To ensure that this work continues, it
is recommended that the strategy should be implemented in other healthcare facilities. It is
recommended that for future projects, the education intervention should be included to patients
and their family members to help reduce the probability of pressure injuries and appropriate
interventions when they occur. Individuals are also encouraged to improve on their nutritional
nursing the nurses create awareness about pressure injury to the patients (Gray & Giuliano,
2018).
The key learning from the first cycle is that education intervention was very effective.
The nurses were more knowledgeable on the causative factors and could explain to a patient. the
key learning from the second PDSA cycle is that posters are more effective I creating awareness
as compared to billboards. The key learning from the third cycle is that creating awareness to the
patient using the nurse was not as effective. This was not anticipated during the study (Roberts et
al., 2016)
Lessons and limitation
The major lesson is that educating the nurses helps to improve patient care. Through
understanding the risk factors, the nurses can prevent more cases of pressure injuries form
arising. The major limitation of this study is that the education intervention will have to be
repeated each time a new staff joins the healthcare facility (Nguyen, Chaboyer & Whitty, 2015).
Conclusion
In conclusion, pressure injuries are caused by several factors; they include, malnutrition,
physical immobility, chronic illnesses among others. The purpose of this project was to ascertain
the causative factors and help prevent patients from acquiring pressure injuries during their stay
in hospital. The strategy chosen, helped to achieve the aim. To ensure that this work continues, it
is recommended that the strategy should be implemented in other healthcare facilities. It is
recommended that for future projects, the education intervention should be included to patients
and their family members to help reduce the probability of pressure injuries and appropriate
interventions when they occur. Individuals are also encouraged to improve on their nutritional
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
QUALITY IMPROVEMENT PROJECT 11
status and improve their overall weight. This will help to reduce cases of malnutrition. Patients
are also encouraged to adopt heath lifestyles such as tobacco cessation (Edsberg et al., 2016).
status and improve their overall weight. This will help to reduce cases of malnutrition. Patients
are also encouraged to adopt heath lifestyles such as tobacco cessation (Edsberg et al., 2016).
QUALITY IMPROVEMENT PROJECT 12
References
Clinical Excellence Queensland. (2018). Audit tools for National Safety and Quality Health
Service Standards. Retrieved 27 August 2019, from
https://clinicalexcellence.qld.gov.au/resources/audit-tools-national-safety-and-quality-
health-service-standards
Corbett, L. Q., Funk, M., Fortunato, G., & O'Sullivan, D. M. (2017). Pressure injury in a
community population. Journal of Wound, Ostomy and Continence Nursing, 44(3), 221-
227.
Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016).
Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised
pressure injury staging system. Journal of Wound, Ostomy, and Continence
Nursing, 43(6), 585.
Etikan, I., Musa, S. A., & Alkassim, R. S. (2016). Comparison of convenience sampling and
purposive sampling. American journal of theoretical and applied statistics, 5(1), 1-4.
Gefen, A., Kottner, J., & Santamaria, N. (2016). Clinical and biomechanical perspectives on
pressure injury prevention research: the case of prophylactic dressings. Clinical
Biomechanics, 38, 29-34.
Gray, M., & Giuliano, K. K. (2018). Incontinence-associated dermatitis, characteristics and
relationship to pressure injury: a multisite epidemiologic analysis. Journal of Wound,
Ostomy, and Continence Nursing, 45(1), 63.
Icn.ch. (2013). Pressure Ulcer Prevention. Retrieved 27 August 2019, from
https://www.icn.ch/sites/default/files/inline-files/Pressure_Ulcer_Prevention.pdf
References
Clinical Excellence Queensland. (2018). Audit tools for National Safety and Quality Health
Service Standards. Retrieved 27 August 2019, from
https://clinicalexcellence.qld.gov.au/resources/audit-tools-national-safety-and-quality-
health-service-standards
Corbett, L. Q., Funk, M., Fortunato, G., & O'Sullivan, D. M. (2017). Pressure injury in a
community population. Journal of Wound, Ostomy and Continence Nursing, 44(3), 221-
227.
Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016).
Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised
pressure injury staging system. Journal of Wound, Ostomy, and Continence
Nursing, 43(6), 585.
Etikan, I., Musa, S. A., & Alkassim, R. S. (2016). Comparison of convenience sampling and
purposive sampling. American journal of theoretical and applied statistics, 5(1), 1-4.
Gefen, A., Kottner, J., & Santamaria, N. (2016). Clinical and biomechanical perspectives on
pressure injury prevention research: the case of prophylactic dressings. Clinical
Biomechanics, 38, 29-34.
Gray, M., & Giuliano, K. K. (2018). Incontinence-associated dermatitis, characteristics and
relationship to pressure injury: a multisite epidemiologic analysis. Journal of Wound,
Ostomy, and Continence Nursing, 45(1), 63.
Icn.ch. (2013). Pressure Ulcer Prevention. Retrieved 27 August 2019, from
https://www.icn.ch/sites/default/files/inline-files/Pressure_Ulcer_Prevention.pdf
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





