HLTENN015: Case Study on Applying Nursing Practice in Primary Health
VerifiedAdded on 2023/04/21
|14
|6012
|409
Case Study
AI Summary
This HLTENN015 case study explores the application of nursing practice in a primary health care setting, focusing on two patients: Mr. Jones, who requires wound care for a leg ulcer, and Mr. Smith, who has COPD and struggles with self-care. The assignment includes identifying specific care needs and goals for each patient, such as wound management, smoking cessation, and respiratory support. It also provides pre-visit checklists to identify potential risks and ensure comprehensive care. The case study emphasizes client-focused care, collaboration with healthcare professionals, and the importance of evidence-based practice in achieving positive patient outcomes. Desklib offers a range of similar solved assignments and study resources for nursing students.
Student Name:
Student Signature:
Trainer Name:
Trainer Signature:
Student Outcome: Satisfactory Not Satisfactory
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 1
HLTENN015 Apply nursing practice in
the primary health care setting
Case Study
Student Signature:
Trainer Name:
Trainer Signature:
Student Outcome: Satisfactory Not Satisfactory
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 1
HLTENN015 Apply nursing practice in
the primary health care setting
Case Study
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Assessment Instructions
Achieving competency
This assessment task contains a Case Study. In order for you to meet the requirements of this
assessment task you are to providing satisfactory answer to the related questions.
The task is to be completed in your own time using available reliable sources such as the course
text books provided to you at orientation, credible internet sources such as the department of
health and other text and online journals available to you through the online library service
offered to all students and discussed at orientation.
It is important that you reference all sources of information that you use to obtain information
used in your answers. Referencing must be included and failure to adhere to this requirement will
result in a not satisfactory outcome for the assessment.
The case study is available in the Student Portal. You will need to download the case study and
complete it then submit it through the Student Portal
Plagiarism will result in an immediate Not yet Competent – all copied material MUST be
referenced accordingly. See you Student Handbook for more information.
Reassessment
If you receive a Not Yet Satisfactory result for this Assessment Task, it will be due to you not
satisfying the requirements of one, multiple or all aspects of the task. Your Assessor will provide
you with feedback as to where you did not meet the requirement. You will have another
opportunity to resubmit your assessment work addressing the areas as identified in your assessor
feedback.
Should the student wish to appeal any decision relating to outcome of this assessment task, the
student should follow the Academic-Non Academic Grievance policy and procedure available in
the Student Handbook and Skills Training Australia website.
Assessment Extension Request:
All assessments are due on the assessment due date as identified on the assessment task
document and confirmed by your Trainer/Assessor on the first day of the unit.
If you are unable, due to exceptional circumstances, to submit your assessment tasks on the
required due date, you MUST submit a completed Assessment Extension Form to your
Trainer/Assessor.
Extensions may be granted by your trainer under exceptional circumstances and will only be
granted for a maximum of 2 weeks.
Adjustment in assessment
Flexibility in assessment will be considered where the integrity of the assessment and learning
outcome is maintained. For example, a written assessment may be administered as a verbal
assessment and recorded by a STA staff member where a student has sustained an injury
preventing them from writing. Any agreement for an adjustment to assessment must be
documented in the space provided in the assessment task document (or in writing to the program
manager in the event of an electronically submitted assessment task and placed in your student
file).
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 2
Achieving competency
This assessment task contains a Case Study. In order for you to meet the requirements of this
assessment task you are to providing satisfactory answer to the related questions.
The task is to be completed in your own time using available reliable sources such as the course
text books provided to you at orientation, credible internet sources such as the department of
health and other text and online journals available to you through the online library service
offered to all students and discussed at orientation.
It is important that you reference all sources of information that you use to obtain information
used in your answers. Referencing must be included and failure to adhere to this requirement will
result in a not satisfactory outcome for the assessment.
The case study is available in the Student Portal. You will need to download the case study and
complete it then submit it through the Student Portal
Plagiarism will result in an immediate Not yet Competent – all copied material MUST be
referenced accordingly. See you Student Handbook for more information.
Reassessment
If you receive a Not Yet Satisfactory result for this Assessment Task, it will be due to you not
satisfying the requirements of one, multiple or all aspects of the task. Your Assessor will provide
you with feedback as to where you did not meet the requirement. You will have another
opportunity to resubmit your assessment work addressing the areas as identified in your assessor
feedback.
Should the student wish to appeal any decision relating to outcome of this assessment task, the
student should follow the Academic-Non Academic Grievance policy and procedure available in
the Student Handbook and Skills Training Australia website.
Assessment Extension Request:
All assessments are due on the assessment due date as identified on the assessment task
document and confirmed by your Trainer/Assessor on the first day of the unit.
If you are unable, due to exceptional circumstances, to submit your assessment tasks on the
required due date, you MUST submit a completed Assessment Extension Form to your
Trainer/Assessor.
Extensions may be granted by your trainer under exceptional circumstances and will only be
granted for a maximum of 2 weeks.
Adjustment in assessment
Flexibility in assessment will be considered where the integrity of the assessment and learning
outcome is maintained. For example, a written assessment may be administered as a verbal
assessment and recorded by a STA staff member where a student has sustained an injury
preventing them from writing. Any agreement for an adjustment to assessment must be
documented in the space provided in the assessment task document (or in writing to the program
manager in the event of an electronically submitted assessment task and placed in your student
file).
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 2
Please type your responses in the spaces provided below each question and submit as per the
instructions in the assessment document.
Please note: The space below is not indicative to the required length of the response; you are to
ensure that you thoroughly answer the question.
Task 2
Case Study
A final grade will be applied on successful completion of tasks 1, 2 and 3 This task will represent 50% of
the final grade
The case study is to be completed in your own time using available reliable sources such as the course
text books provided to you at orientation, credible internet sources such as the department of health and
other text and online journals available to you through the online library service offered to all students
and discussed at orientation.
It is important that you reference all sources of information that you use to obtain information used in
your answers. Referencing must be included and failure to adhere to this requirement will result in a not
satisfactory outcome for the assessment.
Use the following Case information for each Part of your case study.
Mr. Jones and Mr. Smith have both been referred for home nursing.
Mr. Jones is married and has a supportive wife and family but requires home visits for wound care due
to a lower leg ulcer. He cannot attend the wound clinic because his wife does not drive. Mrs. Jones
provides nutritious meals and helps him in the shower.
Mr. Smith is single, lives alone. He has a large dog on the premises and is a bit of a recluse.
There is evidence he also does not eat properly and is reluctant to shower unassisted. He continues to
smoke.
Has been referred for home nursing as he has Chronic Obstructive Pulmonary Disease(COPD) and has
had 2 recent admissions to hospital for exacerbation of COPD. Mr Smith has appointments to attend
the hospital’s outpatient clinic to assess his lung function and provide him with physiotherapy. Mr
Smith does not want to attend the outpatient clinic.
PART A: The Nursing Process.
The nursing Process begins with a thorough client assessment to provide the information needed to plan
appropriate care. It also provides a baseline for evaluation of nursing care that has been provided.
Conducting a nursing assessment means getting to know the client and their family, their environment
and lifestyle as well as their goals and perception of care. Assessment in this context includes an
assessment of the client’s needs and a risk assessment. The information you gather enables you and the
client and responsible family members to identify actual and potential problems.
Nursing care in the primary health environment is client focused and includes understanding and using
available family and resources. Expected outcomes are identified; this provides a guide for implementing
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 3
instructions in the assessment document.
Please note: The space below is not indicative to the required length of the response; you are to
ensure that you thoroughly answer the question.
Task 2
Case Study
A final grade will be applied on successful completion of tasks 1, 2 and 3 This task will represent 50% of
the final grade
The case study is to be completed in your own time using available reliable sources such as the course
text books provided to you at orientation, credible internet sources such as the department of health and
other text and online journals available to you through the online library service offered to all students
and discussed at orientation.
It is important that you reference all sources of information that you use to obtain information used in
your answers. Referencing must be included and failure to adhere to this requirement will result in a not
satisfactory outcome for the assessment.
Use the following Case information for each Part of your case study.
Mr. Jones and Mr. Smith have both been referred for home nursing.
Mr. Jones is married and has a supportive wife and family but requires home visits for wound care due
to a lower leg ulcer. He cannot attend the wound clinic because his wife does not drive. Mrs. Jones
provides nutritious meals and helps him in the shower.
Mr. Smith is single, lives alone. He has a large dog on the premises and is a bit of a recluse.
There is evidence he also does not eat properly and is reluctant to shower unassisted. He continues to
smoke.
Has been referred for home nursing as he has Chronic Obstructive Pulmonary Disease(COPD) and has
had 2 recent admissions to hospital for exacerbation of COPD. Mr Smith has appointments to attend
the hospital’s outpatient clinic to assess his lung function and provide him with physiotherapy. Mr
Smith does not want to attend the outpatient clinic.
PART A: The Nursing Process.
The nursing Process begins with a thorough client assessment to provide the information needed to plan
appropriate care. It also provides a baseline for evaluation of nursing care that has been provided.
Conducting a nursing assessment means getting to know the client and their family, their environment
and lifestyle as well as their goals and perception of care. Assessment in this context includes an
assessment of the client’s needs and a risk assessment. The information you gather enables you and the
client and responsible family members to identify actual and potential problems.
Nursing care in the primary health environment is client focused and includes understanding and using
available family and resources. Expected outcomes are identified; this provides a guide for implementing
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
care and the achievement of goals. Goals need to be set in partnership with the client and appropriate
family members.
Care plans are individualised and incorporate clinical pathways and best practice objectives to ensure that
care is evidence based and meets quality standards.
When formulating nursing care plans the Primary Health Care Nurse (PHCN) should consult and
collaborate with the client, registered nurse and /or case manager.
It is important to consider who will be involved in providing the planned care. If a partner or relative or
appropriate other person is to be significantly involved, then the plan will need to include provision of
adequate information to ensure safe, relevant care is delivered. Care providers roles need to be clearly
defined. Planning of care for clients in a home environment also incorporates identifying relevant
referrals and accessing additional services.
A care plan should also include appropriate education of the client and family.
You must prepare thoroughly before your visit. An organisational pre visit check list is completed to
ensure aspects associated with the client, family and the specific environment have been identified.
Questions and Assessment Part A:
Use the above client scenario information as a guide to complete the following:-: (Refer to Marking
criteria Part A)
1 Identify 3 specific care needs (Nursing Diagnoses) and 3 Goals for each client.
2. Provide individual pre-visit check lists for each scenario. Your pre-visit check lists should include
identification of any risks
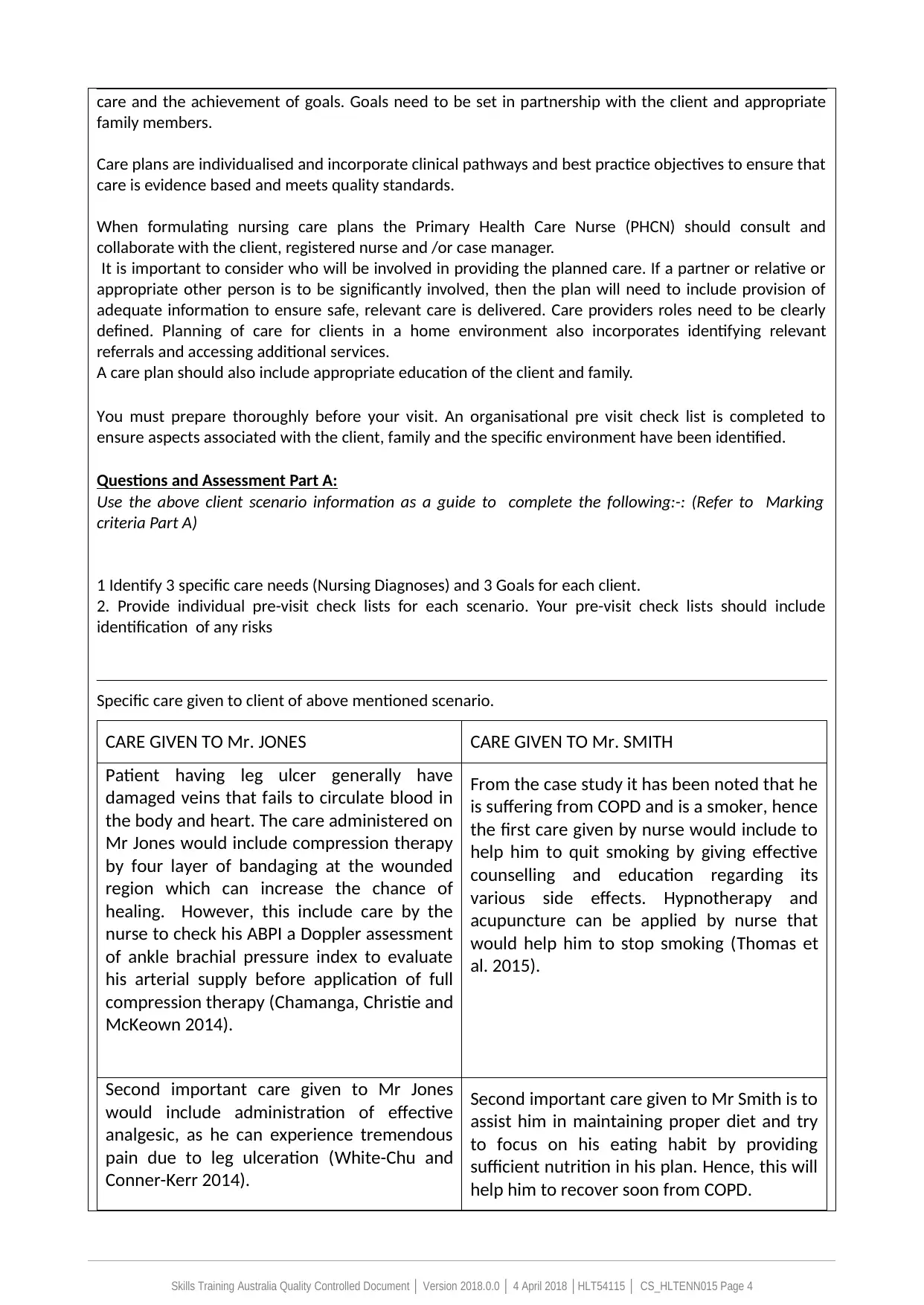
Specific care given to client of above mentioned scenario.
CARE GIVEN TO Mr. JONES CARE GIVEN TO Mr. SMITH
Patient having leg ulcer generally have
damaged veins that fails to circulate blood in
the body and heart. The care administered on
Mr Jones would include compression therapy
by four layer of bandaging at the wounded
region which can increase the chance of
healing. However, this include care by the
nurse to check his ABPI a Doppler assessment
of ankle brachial pressure index to evaluate
his arterial supply before application of full
compression therapy (Chamanga, Christie and
McKeown 2014).
From the case study it has been noted that he
is suffering from COPD and is a smoker, hence
the first care given by nurse would include to
help him to quit smoking by giving effective
counselling and education regarding its
various side effects. Hypnotherapy and
acupuncture can be applied by nurse that
would help him to stop smoking (Thomas et
al. 2015).
Second important care given to Mr Jones
would include administration of effective
analgesic, as he can experience tremendous
pain due to leg ulceration (White-Chu and
Conner-Kerr 2014).
Second important care given to Mr Smith is to
assist him in maintaining proper diet and try
to focus on his eating habit by providing
sufficient nutrition in his plan. Hence, this will
help him to recover soon from COPD.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 4
family members.
Care plans are individualised and incorporate clinical pathways and best practice objectives to ensure that
care is evidence based and meets quality standards.
When formulating nursing care plans the Primary Health Care Nurse (PHCN) should consult and
collaborate with the client, registered nurse and /or case manager.
It is important to consider who will be involved in providing the planned care. If a partner or relative or
appropriate other person is to be significantly involved, then the plan will need to include provision of
adequate information to ensure safe, relevant care is delivered. Care providers roles need to be clearly
defined. Planning of care for clients in a home environment also incorporates identifying relevant
referrals and accessing additional services.
A care plan should also include appropriate education of the client and family.
You must prepare thoroughly before your visit. An organisational pre visit check list is completed to
ensure aspects associated with the client, family and the specific environment have been identified.
Questions and Assessment Part A:
Use the above client scenario information as a guide to complete the following:-: (Refer to Marking
criteria Part A)
1 Identify 3 specific care needs (Nursing Diagnoses) and 3 Goals for each client.
2. Provide individual pre-visit check lists for each scenario. Your pre-visit check lists should include
identification of any risks
Specific care given to client of above mentioned scenario.
CARE GIVEN TO Mr. JONES CARE GIVEN TO Mr. SMITH
Patient having leg ulcer generally have
damaged veins that fails to circulate blood in
the body and heart. The care administered on
Mr Jones would include compression therapy
by four layer of bandaging at the wounded
region which can increase the chance of
healing. However, this include care by the
nurse to check his ABPI a Doppler assessment
of ankle brachial pressure index to evaluate
his arterial supply before application of full
compression therapy (Chamanga, Christie and
McKeown 2014).
From the case study it has been noted that he
is suffering from COPD and is a smoker, hence
the first care given by nurse would include to
help him to quit smoking by giving effective
counselling and education regarding its
various side effects. Hypnotherapy and
acupuncture can be applied by nurse that
would help him to stop smoking (Thomas et
al. 2015).
Second important care given to Mr Jones
would include administration of effective
analgesic, as he can experience tremendous
pain due to leg ulceration (White-Chu and
Conner-Kerr 2014).
Second important care given to Mr Smith is to
assist him in maintaining proper diet and try
to focus on his eating habit by providing
sufficient nutrition in his plan. Hence, this will
help him to recover soon from COPD.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
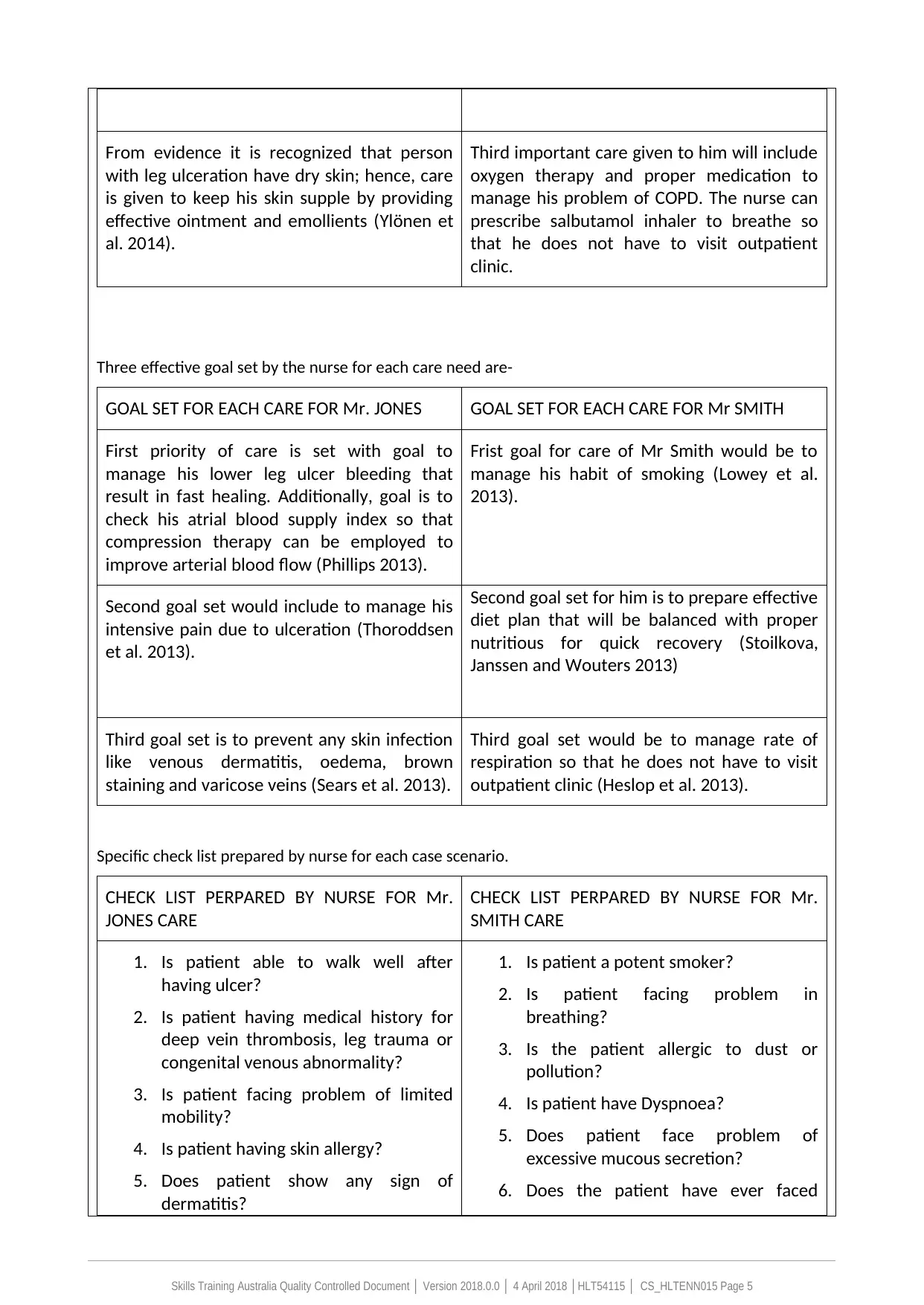
From evidence it is recognized that person
with leg ulceration have dry skin; hence, care
is given to keep his skin supple by providing
effective ointment and emollients (Ylönen et
al. 2014).
Third important care given to him will include
oxygen therapy and proper medication to
manage his problem of COPD. The nurse can
prescribe salbutamol inhaler to breathe so
that he does not have to visit outpatient
clinic.
Three effective goal set by the nurse for each care need are-
GOAL SET FOR EACH CARE FOR Mr. JONES GOAL SET FOR EACH CARE FOR Mr SMITH
First priority of care is set with goal to
manage his lower leg ulcer bleeding that
result in fast healing. Additionally, goal is to
check his atrial blood supply index so that
compression therapy can be employed to
improve arterial blood flow (Phillips 2013).
Frist goal for care of Mr Smith would be to
manage his habit of smoking (Lowey et al.
2013).
Second goal set would include to manage his
intensive pain due to ulceration (Thoroddsen
et al. 2013).
Second goal set for him is to prepare effective
diet plan that will be balanced with proper
nutritious for quick recovery (Stoilkova,
Janssen and Wouters 2013)
Third goal set is to prevent any skin infection
like venous dermatitis, oedema, brown
staining and varicose veins (Sears et al. 2013).
Third goal set would be to manage rate of
respiration so that he does not have to visit
outpatient clinic (Heslop et al. 2013).
Specific check list prepared by nurse for each case scenario.
CHECK LIST PERPARED BY NURSE FOR Mr.
JONES CARE
CHECK LIST PERPARED BY NURSE FOR Mr.
SMITH CARE
1. Is patient able to walk well after
having ulcer?
2. Is patient having medical history for
deep vein thrombosis, leg trauma or
congenital venous abnormality?
3. Is patient facing problem of limited
mobility?
4. Is patient having skin allergy?
5. Does patient show any sign of
dermatitis?
1. Is patient a potent smoker?
2. Is patient facing problem in
breathing?
3. Is the patient allergic to dust or
pollution?
4. Is patient have Dyspnoea?
5. Does patient face problem of
excessive mucous secretion?
6. Does the patient have ever faced
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 5
with leg ulceration have dry skin; hence, care
is given to keep his skin supple by providing
effective ointment and emollients (Ylönen et
al. 2014).
Third important care given to him will include
oxygen therapy and proper medication to
manage his problem of COPD. The nurse can
prescribe salbutamol inhaler to breathe so
that he does not have to visit outpatient
clinic.
Three effective goal set by the nurse for each care need are-
GOAL SET FOR EACH CARE FOR Mr. JONES GOAL SET FOR EACH CARE FOR Mr SMITH
First priority of care is set with goal to
manage his lower leg ulcer bleeding that
result in fast healing. Additionally, goal is to
check his atrial blood supply index so that
compression therapy can be employed to
improve arterial blood flow (Phillips 2013).
Frist goal for care of Mr Smith would be to
manage his habit of smoking (Lowey et al.
2013).
Second goal set would include to manage his
intensive pain due to ulceration (Thoroddsen
et al. 2013).
Second goal set for him is to prepare effective
diet plan that will be balanced with proper
nutritious for quick recovery (Stoilkova,
Janssen and Wouters 2013)
Third goal set is to prevent any skin infection
like venous dermatitis, oedema, brown
staining and varicose veins (Sears et al. 2013).
Third goal set would be to manage rate of
respiration so that he does not have to visit
outpatient clinic (Heslop et al. 2013).
Specific check list prepared by nurse for each case scenario.
CHECK LIST PERPARED BY NURSE FOR Mr.
JONES CARE
CHECK LIST PERPARED BY NURSE FOR Mr.
SMITH CARE
1. Is patient able to walk well after
having ulcer?
2. Is patient having medical history for
deep vein thrombosis, leg trauma or
congenital venous abnormality?
3. Is patient facing problem of limited
mobility?
4. Is patient having skin allergy?
5. Does patient show any sign of
dermatitis?
1. Is patient a potent smoker?
2. Is patient facing problem in
breathing?
3. Is the patient allergic to dust or
pollution?
4. Is patient have Dyspnoea?
5. Does patient face problem of
excessive mucous secretion?
6. Does the patient have ever faced
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 5
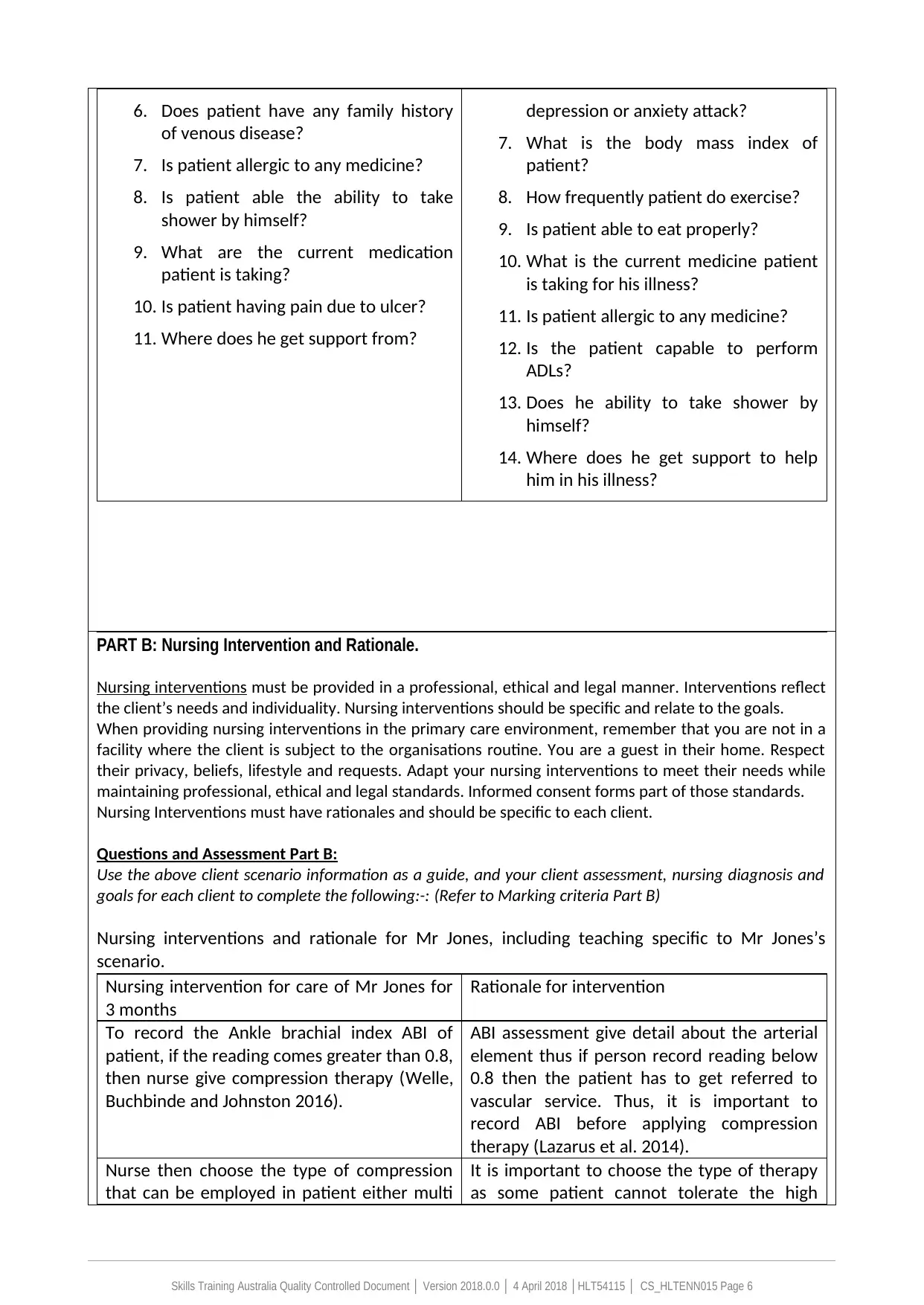
6. Does patient have any family history
of venous disease?
7. Is patient allergic to any medicine?
8. Is patient able the ability to take
shower by himself?
9. What are the current medication
patient is taking?
10. Is patient having pain due to ulcer?
11. Where does he get support from?
depression or anxiety attack?
7. What is the body mass index of
patient?
8. How frequently patient do exercise?
9. Is patient able to eat properly?
10. What is the current medicine patient
is taking for his illness?
11. Is patient allergic to any medicine?
12. Is the patient capable to perform
ADLs?
13. Does he ability to take shower by
himself?
14. Where does he get support to help
him in his illness?
PART B: Nursing Intervention and Rationale.
Nursing interventions must be provided in a professional, ethical and legal manner. Interventions reflect
the client’s needs and individuality. Nursing interventions should be specific and relate to the goals.
When providing nursing interventions in the primary care environment, remember that you are not in a
facility where the client is subject to the organisations routine. You are a guest in their home. Respect
their privacy, beliefs, lifestyle and requests. Adapt your nursing interventions to meet their needs while
maintaining professional, ethical and legal standards. Informed consent forms part of those standards.
Nursing Interventions must have rationales and should be specific to each client.
Questions and Assessment Part B:
Use the above client scenario information as a guide, and your client assessment, nursing diagnosis and
goals for each client to complete the following:-: (Refer to Marking criteria Part B)
Nursing interventions and rationale for Mr Jones, including teaching specific to Mr Jones’s
scenario.
Nursing intervention for care of Mr Jones for
3 months
Rationale for intervention
To record the Ankle brachial index ABI of
patient, if the reading comes greater than 0.8,
then nurse give compression therapy (Welle,
Buchbinde and Johnston 2016).
ABI assessment give detail about the arterial
element thus if person record reading below
0.8 then the patient has to get referred to
vascular service. Thus, it is important to
record ABI before applying compression
therapy (Lazarus et al. 2014).
Nurse then choose the type of compression
that can be employed in patient either multi
It is important to choose the type of therapy
as some patient cannot tolerate the high
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 6
of venous disease?
7. Is patient allergic to any medicine?
8. Is patient able the ability to take
shower by himself?
9. What are the current medication
patient is taking?
10. Is patient having pain due to ulcer?
11. Where does he get support from?
depression or anxiety attack?
7. What is the body mass index of
patient?
8. How frequently patient do exercise?
9. Is patient able to eat properly?
10. What is the current medicine patient
is taking for his illness?
11. Is patient allergic to any medicine?
12. Is the patient capable to perform
ADLs?
13. Does he ability to take shower by
himself?
14. Where does he get support to help
him in his illness?
PART B: Nursing Intervention and Rationale.
Nursing interventions must be provided in a professional, ethical and legal manner. Interventions reflect
the client’s needs and individuality. Nursing interventions should be specific and relate to the goals.
When providing nursing interventions in the primary care environment, remember that you are not in a
facility where the client is subject to the organisations routine. You are a guest in their home. Respect
their privacy, beliefs, lifestyle and requests. Adapt your nursing interventions to meet their needs while
maintaining professional, ethical and legal standards. Informed consent forms part of those standards.
Nursing Interventions must have rationales and should be specific to each client.
Questions and Assessment Part B:
Use the above client scenario information as a guide, and your client assessment, nursing diagnosis and
goals for each client to complete the following:-: (Refer to Marking criteria Part B)
Nursing interventions and rationale for Mr Jones, including teaching specific to Mr Jones’s
scenario.
Nursing intervention for care of Mr Jones for
3 months
Rationale for intervention
To record the Ankle brachial index ABI of
patient, if the reading comes greater than 0.8,
then nurse give compression therapy (Welle,
Buchbinde and Johnston 2016).
ABI assessment give detail about the arterial
element thus if person record reading below
0.8 then the patient has to get referred to
vascular service. Thus, it is important to
record ABI before applying compression
therapy (Lazarus et al. 2014).
Nurse then choose the type of compression
that can be employed in patient either multi
It is important to choose the type of therapy
as some patient cannot tolerate the high
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
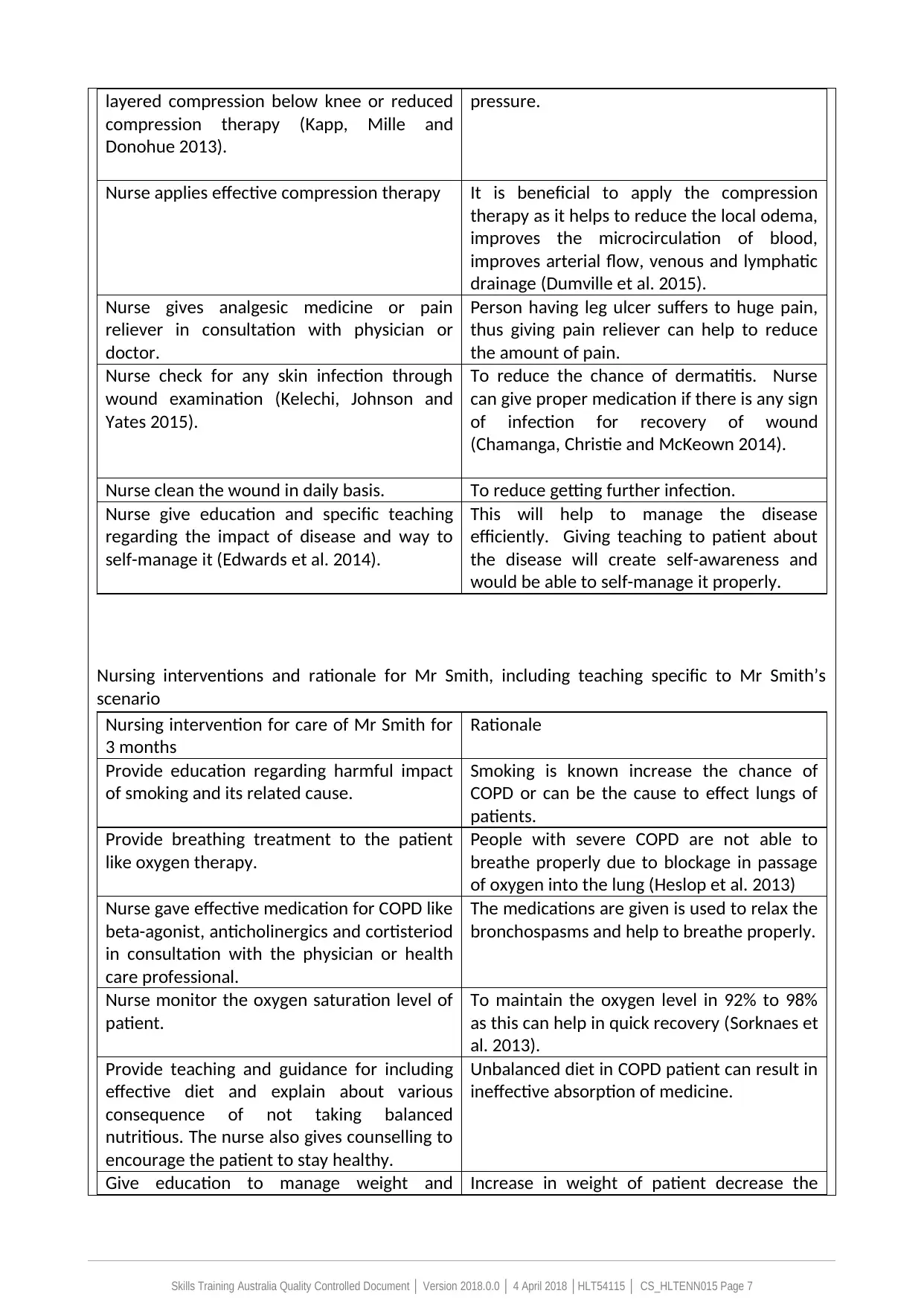
layered compression below knee or reduced
compression therapy (Kapp, Mille and
Donohue 2013).
pressure.
Nurse applies effective compression therapy It is beneficial to apply the compression
therapy as it helps to reduce the local odema,
improves the microcirculation of blood,
improves arterial flow, venous and lymphatic
drainage (Dumville et al. 2015).
Nurse gives analgesic medicine or pain
reliever in consultation with physician or
doctor.
Person having leg ulcer suffers to huge pain,
thus giving pain reliever can help to reduce
the amount of pain.
Nurse check for any skin infection through
wound examination (Kelechi, Johnson and
Yates 2015).
To reduce the chance of dermatitis. Nurse
can give proper medication if there is any sign
of infection for recovery of wound
(Chamanga, Christie and McKeown 2014).
Nurse clean the wound in daily basis. To reduce getting further infection.
Nurse give education and specific teaching
regarding the impact of disease and way to
self-manage it (Edwards et al. 2014).
This will help to manage the disease
efficiently. Giving teaching to patient about
the disease will create self-awareness and
would be able to self-manage it properly.
Nursing interventions and rationale for Mr Smith, including teaching specific to Mr Smith’s
scenario
Nursing intervention for care of Mr Smith for
3 months
Rationale
Provide education regarding harmful impact
of smoking and its related cause.
Smoking is known increase the chance of
COPD or can be the cause to effect lungs of
patients.
Provide breathing treatment to the patient
like oxygen therapy.
People with severe COPD are not able to
breathe properly due to blockage in passage
of oxygen into the lung (Heslop et al. 2013)
Nurse gave effective medication for COPD like
beta-agonist, anticholinergics and cortisteriod
in consultation with the physician or health
care professional.
The medications are given is used to relax the
bronchospasms and help to breathe properly.
Nurse monitor the oxygen saturation level of
patient.
To maintain the oxygen level in 92% to 98%
as this can help in quick recovery (Sorknaes et
al. 2013).
Provide teaching and guidance for including
effective diet and explain about various
consequence of not taking balanced
nutritious. The nurse also gives counselling to
encourage the patient to stay healthy.
Unbalanced diet in COPD patient can result in
ineffective absorption of medicine.
Give education to manage weight and Increase in weight of patient decrease the
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 7
compression therapy (Kapp, Mille and
Donohue 2013).
pressure.
Nurse applies effective compression therapy It is beneficial to apply the compression
therapy as it helps to reduce the local odema,
improves the microcirculation of blood,
improves arterial flow, venous and lymphatic
drainage (Dumville et al. 2015).
Nurse gives analgesic medicine or pain
reliever in consultation with physician or
doctor.
Person having leg ulcer suffers to huge pain,
thus giving pain reliever can help to reduce
the amount of pain.
Nurse check for any skin infection through
wound examination (Kelechi, Johnson and
Yates 2015).
To reduce the chance of dermatitis. Nurse
can give proper medication if there is any sign
of infection for recovery of wound
(Chamanga, Christie and McKeown 2014).
Nurse clean the wound in daily basis. To reduce getting further infection.
Nurse give education and specific teaching
regarding the impact of disease and way to
self-manage it (Edwards et al. 2014).
This will help to manage the disease
efficiently. Giving teaching to patient about
the disease will create self-awareness and
would be able to self-manage it properly.
Nursing interventions and rationale for Mr Smith, including teaching specific to Mr Smith’s
scenario
Nursing intervention for care of Mr Smith for
3 months
Rationale
Provide education regarding harmful impact
of smoking and its related cause.
Smoking is known increase the chance of
COPD or can be the cause to effect lungs of
patients.
Provide breathing treatment to the patient
like oxygen therapy.
People with severe COPD are not able to
breathe properly due to blockage in passage
of oxygen into the lung (Heslop et al. 2013)
Nurse gave effective medication for COPD like
beta-agonist, anticholinergics and cortisteriod
in consultation with the physician or health
care professional.
The medications are given is used to relax the
bronchospasms and help to breathe properly.
Nurse monitor the oxygen saturation level of
patient.
To maintain the oxygen level in 92% to 98%
as this can help in quick recovery (Sorknaes et
al. 2013).
Provide teaching and guidance for including
effective diet and explain about various
consequence of not taking balanced
nutritious. The nurse also gives counselling to
encourage the patient to stay healthy.
Unbalanced diet in COPD patient can result in
ineffective absorption of medicine.
Give education to manage weight and Increase in weight of patient decrease the
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
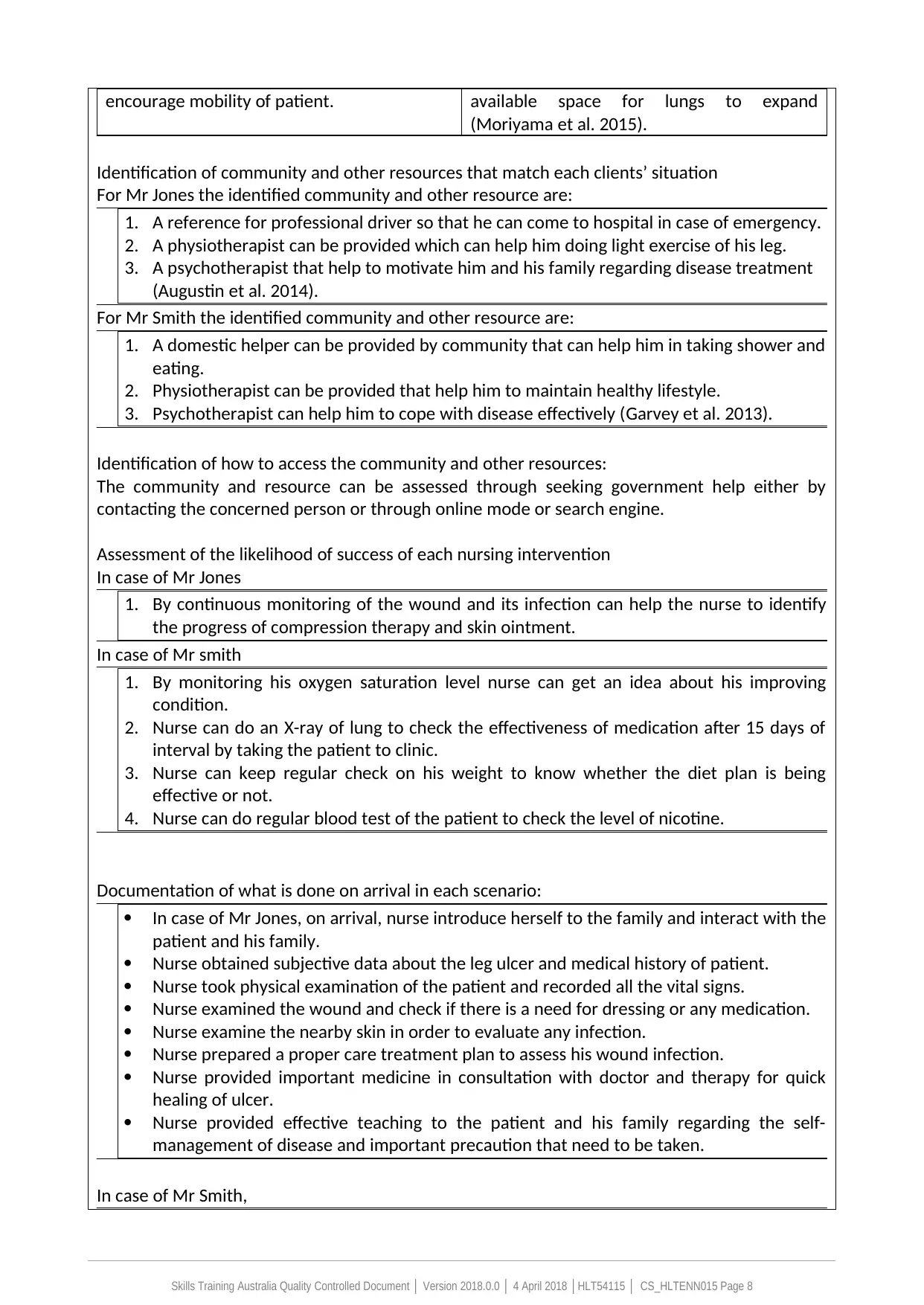
encourage mobility of patient. available space for lungs to expand
(Moriyama et al. 2015).
Identification of community and other resources that match each clients’ situation
For Mr Jones the identified community and other resource are:
1. A reference for professional driver so that he can come to hospital in case of emergency.
2. A physiotherapist can be provided which can help him doing light exercise of his leg.
3. A psychotherapist that help to motivate him and his family regarding disease treatment
(Augustin et al. 2014).
For Mr Smith the identified community and other resource are:
1. A domestic helper can be provided by community that can help him in taking shower and
eating.
2. Physiotherapist can be provided that help him to maintain healthy lifestyle.
3. Psychotherapist can help him to cope with disease effectively (Garvey et al. 2013).
Identification of how to access the community and other resources:
The community and resource can be assessed through seeking government help either by
contacting the concerned person or through online mode or search engine.
Assessment of the likelihood of success of each nursing intervention
In case of Mr Jones
1. By continuous monitoring of the wound and its infection can help the nurse to identify
the progress of compression therapy and skin ointment.
In case of Mr smith
1. By monitoring his oxygen saturation level nurse can get an idea about his improving
condition.
2. Nurse can do an X-ray of lung to check the effectiveness of medication after 15 days of
interval by taking the patient to clinic.
3. Nurse can keep regular check on his weight to know whether the diet plan is being
effective or not.
4. Nurse can do regular blood test of the patient to check the level of nicotine.
Documentation of what is done on arrival in each scenario:
In case of Mr Jones, on arrival, nurse introduce herself to the family and interact with the
patient and his family.
Nurse obtained subjective data about the leg ulcer and medical history of patient.
Nurse took physical examination of the patient and recorded all the vital signs.
Nurse examined the wound and check if there is a need for dressing or any medication.
Nurse examine the nearby skin in order to evaluate any infection.
Nurse prepared a proper care treatment plan to assess his wound infection.
Nurse provided important medicine in consultation with doctor and therapy for quick
healing of ulcer.
Nurse provided effective teaching to the patient and his family regarding the self-
management of disease and important precaution that need to be taken.
In case of Mr Smith,
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 8
(Moriyama et al. 2015).
Identification of community and other resources that match each clients’ situation
For Mr Jones the identified community and other resource are:
1. A reference for professional driver so that he can come to hospital in case of emergency.
2. A physiotherapist can be provided which can help him doing light exercise of his leg.
3. A psychotherapist that help to motivate him and his family regarding disease treatment
(Augustin et al. 2014).
For Mr Smith the identified community and other resource are:
1. A domestic helper can be provided by community that can help him in taking shower and
eating.
2. Physiotherapist can be provided that help him to maintain healthy lifestyle.
3. Psychotherapist can help him to cope with disease effectively (Garvey et al. 2013).
Identification of how to access the community and other resources:
The community and resource can be assessed through seeking government help either by
contacting the concerned person or through online mode or search engine.
Assessment of the likelihood of success of each nursing intervention
In case of Mr Jones
1. By continuous monitoring of the wound and its infection can help the nurse to identify
the progress of compression therapy and skin ointment.
In case of Mr smith
1. By monitoring his oxygen saturation level nurse can get an idea about his improving
condition.
2. Nurse can do an X-ray of lung to check the effectiveness of medication after 15 days of
interval by taking the patient to clinic.
3. Nurse can keep regular check on his weight to know whether the diet plan is being
effective or not.
4. Nurse can do regular blood test of the patient to check the level of nicotine.
Documentation of what is done on arrival in each scenario:
In case of Mr Jones, on arrival, nurse introduce herself to the family and interact with the
patient and his family.
Nurse obtained subjective data about the leg ulcer and medical history of patient.
Nurse took physical examination of the patient and recorded all the vital signs.
Nurse examined the wound and check if there is a need for dressing or any medication.
Nurse examine the nearby skin in order to evaluate any infection.
Nurse prepared a proper care treatment plan to assess his wound infection.
Nurse provided important medicine in consultation with doctor and therapy for quick
healing of ulcer.
Nurse provided effective teaching to the patient and his family regarding the self-
management of disease and important precaution that need to be taken.
In case of Mr Smith,
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 8
Nurse first need to introduce herself and create an environment of effective
communication.
Nurse communicated with the patient about his medical history and social life.
Nurses took physical examination of patient to check his condition of disease.
Nurse monitored the oxygen saturation level of the patient.
Nurse provided effective medicine in consultation with doctor, to the patient for better
recovery.
Nurse encouraged the patient for doing exercise and stop smoking by providing effective
teaching.
Nurse prepared a balanced diet for his healthy lifestyle.
PART C: Evaluation
Evaluation is the final step in the nursing process. Evaluation identifies the achievement of outcomes.
Evaluation can also lead to re-assessment of care. During evaluation it becomes evident whether the
previous steps of the nursing process were effective and if the expected outcomes have been reached.
The purpose of evaluation is to monitor the client’s responses to nursing interventions and their progress
toward planned goals.
Evaluation of care should be a continuous process that occurs with every visit to the client and through
the documenting and reporting process. Each evaluation that is made depends on your ability to form a
judgement or an opinion about the data that has been collected. Evaluation findings will help to:
Determine if original assessment data still applies
Identifies further potential or actual complications
Analyse responses to nursing interventions, this may identify the need for first aid or emergency
care.
Determine if care meets standards and is evidence based
Identify opportunities to improve the quality of care
Assess outcomes from other health care team members
Questions and Assessment Part C:
Use the client scenario information as a guide and refer back to your previous client assessment and
nursing care plans to complete the following :- (Refer to Marking criteria Part C)
1. What criteria would you look for when evaluating whether you have met the goals you set for
each client?
2. As the PHCN conducting the home visits, who would you report the outcomes to?
3. What specific documentation would you complete after the home visit for Mr Jones, and Mr
Smith?
critical evaluation of Mr Jones
The nursing intervention given to the patient was for the period of three months, nurse visit to
the client home in every 15 days in order to evaluate his progress from disease and to check
whether the treatment is working effectively or not. The interventions given by nurse to the
patient with an expectation that it will bring quick recovery of the disease. In every 15-day nurse
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 9
communication.
Nurse communicated with the patient about his medical history and social life.
Nurses took physical examination of patient to check his condition of disease.
Nurse monitored the oxygen saturation level of the patient.
Nurse provided effective medicine in consultation with doctor, to the patient for better
recovery.
Nurse encouraged the patient for doing exercise and stop smoking by providing effective
teaching.
Nurse prepared a balanced diet for his healthy lifestyle.
PART C: Evaluation
Evaluation is the final step in the nursing process. Evaluation identifies the achievement of outcomes.
Evaluation can also lead to re-assessment of care. During evaluation it becomes evident whether the
previous steps of the nursing process were effective and if the expected outcomes have been reached.
The purpose of evaluation is to monitor the client’s responses to nursing interventions and their progress
toward planned goals.
Evaluation of care should be a continuous process that occurs with every visit to the client and through
the documenting and reporting process. Each evaluation that is made depends on your ability to form a
judgement or an opinion about the data that has been collected. Evaluation findings will help to:
Determine if original assessment data still applies
Identifies further potential or actual complications
Analyse responses to nursing interventions, this may identify the need for first aid or emergency
care.
Determine if care meets standards and is evidence based
Identify opportunities to improve the quality of care
Assess outcomes from other health care team members
Questions and Assessment Part C:
Use the client scenario information as a guide and refer back to your previous client assessment and
nursing care plans to complete the following :- (Refer to Marking criteria Part C)
1. What criteria would you look for when evaluating whether you have met the goals you set for
each client?
2. As the PHCN conducting the home visits, who would you report the outcomes to?
3. What specific documentation would you complete after the home visit for Mr Jones, and Mr
Smith?
critical evaluation of Mr Jones
The nursing intervention given to the patient was for the period of three months, nurse visit to
the client home in every 15 days in order to evaluate his progress from disease and to check
whether the treatment is working effectively or not. The interventions given by nurse to the
patient with an expectation that it will bring quick recovery of the disease. In every 15-day nurse
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
check the area of ulcer, its redness and make record of it. After next 15 days when nurse re-visit
client house, comparison of current situation is made with the previous wound in terms of area
of wound covered and by noticing redness and pain. If no progress is seen in the wound, then
nurse expect that the intervention given to the patient is not effective and the patient need
some extra care. The compression therapy given to patient need to be increase for next period
of time (Zarch and Jemec 2014). If the pain is still persisting, then nurse can change the
medication in consultation with the doctor. Nurse can check the mobility of leg to evaluate the
progress of disease. Nurse also do a physical examination to check any infection. If sign of
infection is noticed, medicine prescribed need to be changed. Nurse then evaluate the data that
is recorded. All record of the changes is kept and maintained. In next visit nurse check the
condition of wound by comparing the previous record. After completion of 3 months, if the ulcer
is healed, medication and therapy can be stopped.
critical evaluation of Mr Smith
The nursing intervention given to the Mr Smith focus on to quit smoking and provide effective
teaching regarding the impact of disease in his health. The expected outcome by the nurse after
giving such intervention is, patient can effectively manage his illness by maintaining healthy diet
and exercise. In order to evaluate that whether he has quit smoking or not, nurse need to take
blood test in every 15 day of period. If the level of nicotine in blood is at low level, then nurse
can predict that the patient has stopped smoking. Nurse needs to make a regular record of his
signs and symptoms to check the effectiveness of nursing intervention. In next visit, nurse can
do a test to check oxygen saturation level to know whether the medicine given to the patient
has effectively worked. If the oxygen level gets maintained for the period of 2 months, nurse can
expect that the medicine has proven to be effective (Calvo et al. 2014). If he is still facing the
problem in breathing and his oxygen level is still low, nurse in consultation with the doctor can
make changes in nursing intervention for better recovery. Thus, by continuous monitoring of his
healthy habits and diet, nurse assume that care given is being practical for his health. The
progress is seen for 3 months of continuous visit, proves that nursing teaching and education given to the
patient has been worked.
2. The outcome of the evaluation will be reported to the concerned physician who undertook the case
and responsibility of patient.
3. Specific documentation the will be completed after visiting to Mr Jones and Mr Smith is
medical briefing file highlighting his current sign and symptoms along with an information form
on the situation of the patient.
Reference
Augustin, M., Brocatti, L.K., Rustenbach, S.J., Schäfer, I. and Herberger, K., 2014. Cost of illness‐ ‐
of leg ulcers in the community. International wound journal, 11(3), pp.283-292.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 10
client house, comparison of current situation is made with the previous wound in terms of area
of wound covered and by noticing redness and pain. If no progress is seen in the wound, then
nurse expect that the intervention given to the patient is not effective and the patient need
some extra care. The compression therapy given to patient need to be increase for next period
of time (Zarch and Jemec 2014). If the pain is still persisting, then nurse can change the
medication in consultation with the doctor. Nurse can check the mobility of leg to evaluate the
progress of disease. Nurse also do a physical examination to check any infection. If sign of
infection is noticed, medicine prescribed need to be changed. Nurse then evaluate the data that
is recorded. All record of the changes is kept and maintained. In next visit nurse check the
condition of wound by comparing the previous record. After completion of 3 months, if the ulcer
is healed, medication and therapy can be stopped.
critical evaluation of Mr Smith
The nursing intervention given to the Mr Smith focus on to quit smoking and provide effective
teaching regarding the impact of disease in his health. The expected outcome by the nurse after
giving such intervention is, patient can effectively manage his illness by maintaining healthy diet
and exercise. In order to evaluate that whether he has quit smoking or not, nurse need to take
blood test in every 15 day of period. If the level of nicotine in blood is at low level, then nurse
can predict that the patient has stopped smoking. Nurse needs to make a regular record of his
signs and symptoms to check the effectiveness of nursing intervention. In next visit, nurse can
do a test to check oxygen saturation level to know whether the medicine given to the patient
has effectively worked. If the oxygen level gets maintained for the period of 2 months, nurse can
expect that the medicine has proven to be effective (Calvo et al. 2014). If he is still facing the
problem in breathing and his oxygen level is still low, nurse in consultation with the doctor can
make changes in nursing intervention for better recovery. Thus, by continuous monitoring of his
healthy habits and diet, nurse assume that care given is being practical for his health. The
progress is seen for 3 months of continuous visit, proves that nursing teaching and education given to the
patient has been worked.
2. The outcome of the evaluation will be reported to the concerned physician who undertook the case
and responsibility of patient.
3. Specific documentation the will be completed after visiting to Mr Jones and Mr Smith is
medical briefing file highlighting his current sign and symptoms along with an information form
on the situation of the patient.
Reference
Augustin, M., Brocatti, L.K., Rustenbach, S.J., Schäfer, I. and Herberger, K., 2014. Cost of illness‐ ‐
of leg ulcers in the community. International wound journal, 11(3), pp.283-292.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Calvo, G.S., Gómez-Suárez, C., Soriano, J.B., Zamora, E., Gónzalez-Gamarra, A., González-Béjar,
M., Jordán, A., Tadeo, E., Sebastián, A., Fernández, G. and Ancochea, J., 2014. A home telehealth
program for patients with severe COPD: the PROMETE study. Respiratory medicine, 108(3),
pp.453-462.
Chamanga, E., Christie, J. and McKeown, E., 2014. Community nurses' experiences of treating
patients with leg ulcers. Journal of community nursing, 28(6), pp.27-34.
Chamanga, E., Christie, J. and McKeown, E., 2014. Community nurses' experiences of treating
patients with leg ulcers. Journal of community nursing, 28(6), pp.27-34.
Dumville, J.C., Land, L., Evans, D. and Peinemann, F., 2015. Negative pressure wound therapy for
treating leg ulcers. Cochrane Database of Systematic Reviews, (7).
Edwards, H., Finlayson, K., Skerman, H., Alexander, K., Miaskowski, C., Aouizerat, B. and Gibb,
M., 2014. Identification of symptom clusters in patients with chronic venous leg ulcers. Journal
of pain and symptom management, 47(5), pp.867-875.
Fletcher, M.J. and Dahl, B.H., 2013. Expanding nurse practice in COPD: is it key to providing high
quality, effective and safe patient care?. Primary Care Respiratory Journal, 22(2), p.230.
Garvey, C., Spruit, M.A., Hill, K., Pitta, F. and Shioya, T., 2013. International COPD Coalition
Column: pulmonary rehabilitation-reaching out to our international community. Journal of
thoracic disease, 5(3), p.343.
Heslop, K., Newton, J., Baker, C., Burns, G., Carrick-Sen, D. and De Soyza, A., 2013. Effectiveness
of cognitive behavioural therapy (CBT) interventions for anxiety in patients with chronic
obstructive pulmonary disease (COPD) undertaken by respiratory nurses: the COPD CBT CARE
study:(ISRCTN55206395). BMC pulmonary medicine, 13(1), p.62.
Kapp, S., Miller, C. and Donohue, L., 2013. The clinical effectiveness of two compression stocking
treatments on venous leg ulcer recurrence: a randomized controlled trial. The international
journal of lower extremity wounds, 12(3), pp.189-198.
Kelechi, T.J., Johnson, J.J. and Yates, S., 2015. Chronic venous disease and venous leg ulcers: an
evidence-based update. Journal of Vascular Nursing, 33(2), pp.36-46.
Lazarus, G., Valle, M.F., Malas, M., Qazi, U., Maruthur, N.M., Doggett, D., Fawole, O.A., Bass, E.B.
and Zenilman, J., 2014. Chronic venous leg ulcer treatment: future research needs. Wound
repair and regeneration, 22(1), pp.34-42.
Lowey, S.E., Norton, S.A., Quinn, J.R. and Quill, T.E., 2013. Living with advanced heart failure or
COPD: experiences and goals of individuals nearing the end of life. Research in nursing &
health, 36(4), pp.349-358.
Moriyama, M., Takeshita, Y., Haruta, Y., Hattori, N. and Ezenwaka, C.E., 2015. Effects of a 6‐
Month Nurse Led Self Management Program on Comprehensive Pulmonary Rehabilitation for‐ ‐
Patients with COPD Receiving Home Oxygen Therapy. Rehabilitation Nursing, 40(1), pp.40-51.
Phillips, J., 2013. Care of the bariatric patient in acute care. Journal of Radiology Nursing, 32(1),
pp.21-31.
Sears, N., Baker, G.R., Barnsley, J. and Shortt, S., 2013. The incidence of adverse events among
home care patients. International Journal for Quality in Health Care, 25(1), pp.16-28.
Sorknaes, A.D., Bech, M., Madsen, H., Titlestad, I.L., Hounsgaard, L., Hansen-Nord, M., Jest, P.,
Olesen, F., Lauridsen, J. and Østergaard, B., 2013. The effect of real-time teleconsultations
between hospital-based nurses and patients with severe COPD discharged after an
exacerbation. Journal of telemedicine and telecare, 19(8), pp.466-474.
Stoilkova, A., Janssen, D.J. and Wouters, E.F., 2013. Educational programmes in COPD
management interventions: a systematic review. Respiratory medicine, 107(11), pp.1637-1650.
Thomas, D., Abramson, M.J., Bonevski, B., Taylor, S., Poole, S.G., Weeks, G.R., Dooley, M.J. and
George, J., 2015. Quitting experiences and preferences for a future quit attempt: a study among
inpatient smokers. BMJ open, 5(4), p.e006959.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 11
M., Jordán, A., Tadeo, E., Sebastián, A., Fernández, G. and Ancochea, J., 2014. A home telehealth
program for patients with severe COPD: the PROMETE study. Respiratory medicine, 108(3),
pp.453-462.
Chamanga, E., Christie, J. and McKeown, E., 2014. Community nurses' experiences of treating
patients with leg ulcers. Journal of community nursing, 28(6), pp.27-34.
Chamanga, E., Christie, J. and McKeown, E., 2014. Community nurses' experiences of treating
patients with leg ulcers. Journal of community nursing, 28(6), pp.27-34.
Dumville, J.C., Land, L., Evans, D. and Peinemann, F., 2015. Negative pressure wound therapy for
treating leg ulcers. Cochrane Database of Systematic Reviews, (7).
Edwards, H., Finlayson, K., Skerman, H., Alexander, K., Miaskowski, C., Aouizerat, B. and Gibb,
M., 2014. Identification of symptom clusters in patients with chronic venous leg ulcers. Journal
of pain and symptom management, 47(5), pp.867-875.
Fletcher, M.J. and Dahl, B.H., 2013. Expanding nurse practice in COPD: is it key to providing high
quality, effective and safe patient care?. Primary Care Respiratory Journal, 22(2), p.230.
Garvey, C., Spruit, M.A., Hill, K., Pitta, F. and Shioya, T., 2013. International COPD Coalition
Column: pulmonary rehabilitation-reaching out to our international community. Journal of
thoracic disease, 5(3), p.343.
Heslop, K., Newton, J., Baker, C., Burns, G., Carrick-Sen, D. and De Soyza, A., 2013. Effectiveness
of cognitive behavioural therapy (CBT) interventions for anxiety in patients with chronic
obstructive pulmonary disease (COPD) undertaken by respiratory nurses: the COPD CBT CARE
study:(ISRCTN55206395). BMC pulmonary medicine, 13(1), p.62.
Kapp, S., Miller, C. and Donohue, L., 2013. The clinical effectiveness of two compression stocking
treatments on venous leg ulcer recurrence: a randomized controlled trial. The international
journal of lower extremity wounds, 12(3), pp.189-198.
Kelechi, T.J., Johnson, J.J. and Yates, S., 2015. Chronic venous disease and venous leg ulcers: an
evidence-based update. Journal of Vascular Nursing, 33(2), pp.36-46.
Lazarus, G., Valle, M.F., Malas, M., Qazi, U., Maruthur, N.M., Doggett, D., Fawole, O.A., Bass, E.B.
and Zenilman, J., 2014. Chronic venous leg ulcer treatment: future research needs. Wound
repair and regeneration, 22(1), pp.34-42.
Lowey, S.E., Norton, S.A., Quinn, J.R. and Quill, T.E., 2013. Living with advanced heart failure or
COPD: experiences and goals of individuals nearing the end of life. Research in nursing &
health, 36(4), pp.349-358.
Moriyama, M., Takeshita, Y., Haruta, Y., Hattori, N. and Ezenwaka, C.E., 2015. Effects of a 6‐
Month Nurse Led Self Management Program on Comprehensive Pulmonary Rehabilitation for‐ ‐
Patients with COPD Receiving Home Oxygen Therapy. Rehabilitation Nursing, 40(1), pp.40-51.
Phillips, J., 2013. Care of the bariatric patient in acute care. Journal of Radiology Nursing, 32(1),
pp.21-31.
Sears, N., Baker, G.R., Barnsley, J. and Shortt, S., 2013. The incidence of adverse events among
home care patients. International Journal for Quality in Health Care, 25(1), pp.16-28.
Sorknaes, A.D., Bech, M., Madsen, H., Titlestad, I.L., Hounsgaard, L., Hansen-Nord, M., Jest, P.,
Olesen, F., Lauridsen, J. and Østergaard, B., 2013. The effect of real-time teleconsultations
between hospital-based nurses and patients with severe COPD discharged after an
exacerbation. Journal of telemedicine and telecare, 19(8), pp.466-474.
Stoilkova, A., Janssen, D.J. and Wouters, E.F., 2013. Educational programmes in COPD
management interventions: a systematic review. Respiratory medicine, 107(11), pp.1637-1650.
Thomas, D., Abramson, M.J., Bonevski, B., Taylor, S., Poole, S.G., Weeks, G.R., Dooley, M.J. and
George, J., 2015. Quitting experiences and preferences for a future quit attempt: a study among
inpatient smokers. BMJ open, 5(4), p.e006959.
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 11
Thoroddsen, A., Sigurjónsdóttir, G., Ehnfors, M. and Ehrenberg, A., 2013. Accuracy,
completeness and comprehensiveness of information on pressure ulcers recorded in the patient
record. Scandinavian journal of caring sciences, 27(1), pp.84-91.
Weller, C.D., Buchbinder, R. and Johnston, R.V., 2016. Interventions for helping people adhere to
compression treatments for venous leg ulceration. Cochrane database of systematic reviews,
(3).
White-Chu, E.F. and Conner-Kerr, T.A., 2014. Overview of guidelines for the prevention and
treatment of venous leg ulcers: a US perspective. Journal of multidisciplinary healthcare, 7,
p.111.
Ylönen, M., Stolt, M., Leino Kilpi, H. and Suhonen, R., 2014. Nurses' knowledge about venous leg‐
ulcer care: a literature review. International nursing review, 61(2), pp.194-202.
Zarchi, K. and Jemec, G.B., 2014. Delivery of compression therapy for venous leg ulcers. JAMA
dermatology, 150(7), pp.730-736.
Outcome S ☐ NS ☐
Result: _______/50
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 12
completeness and comprehensiveness of information on pressure ulcers recorded in the patient
record. Scandinavian journal of caring sciences, 27(1), pp.84-91.
Weller, C.D., Buchbinder, R. and Johnston, R.V., 2016. Interventions for helping people adhere to
compression treatments for venous leg ulceration. Cochrane database of systematic reviews,
(3).
White-Chu, E.F. and Conner-Kerr, T.A., 2014. Overview of guidelines for the prevention and
treatment of venous leg ulcers: a US perspective. Journal of multidisciplinary healthcare, 7,
p.111.
Ylönen, M., Stolt, M., Leino Kilpi, H. and Suhonen, R., 2014. Nurses' knowledge about venous leg‐
ulcer care: a literature review. International nursing review, 61(2), pp.194-202.
Zarchi, K. and Jemec, G.B., 2014. Delivery of compression therapy for venous leg ulcers. JAMA
dermatology, 150(7), pp.730-736.
Outcome S ☐ NS ☐
Result: _______/50
Skills Training Australia Quality Controlled Document │ Version 2018.0.0 │ 4 April 2018 │HLT54115 │ CS_HLTENN015 Page 12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





