Primary Health Care and Diabetes: An Australian Nursing Perspective
VerifiedAdded on 2022/09/17
|9
|1438
|25
Essay
AI Summary
This essay examines the National Primary Health Care Strategic Framework (NPHCSF) in Australia, specifically focusing on strategic outcome two, which aims to increase access to primary healthcare and reduce health inequalities, particularly in the context of Type 2 Diabetes Mellitus (T2DM). The assignment evaluates the framework's relevance to diabetes management, considering epidemiological factors, social determinants of health like employment, financial stability, and social isolation, as well as health inequalities among Indigenous populations and those in remote areas. The essay also discusses the World Health Organization's (WHO) five principles of primary healthcare, including universal access, health equity, community participation, inter-sectoral approaches, and technology implementation, and how they align with the NPHCSF. The author reflects on how to promote holistic care, improve health literacy, and the importance of multidisciplinary teams in designing person-centered care plans to address the challenges of diabetes management and reduce health disparities, ultimately emphasizing the role of nurses in implementing these strategies.

Running head: NURSING
Nursing
Name of the Student
Name of the University
Author Note
Nursing
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
NURSING
Introduction
The National Primary Health Care Strategic Framework (NPHCSF) is the first
national statement by the Standing Council on Health. It endorses an agreed approach for
developing robust primary health care system in Australia. Research suggests that primary
health care is more efficient in lowering the rate of hospitalisation and reducing health
inequalities (Sanding Council on Health 2013). The following essay will focus on the
strategic outcome two of NPSHCF and its expected outcomes. The outcomes or proposed
goals of NPSHCF will be linked with the management of Type 2 diabetes and reducing the
health inequalities in healthcare access.
Evaluation of the Australian PHC Strategic Framework
The strategic outcome 2 of NPHCSF (2013) deals with increasing the overall access
of primary healthcare by the application of the integrated service system and thereby helping
to reduce health inequity. This strategic outcome is extremely relevant to Type 2 Diabetes
Mellitus which is a national health issue in Australia. During 2015, 16, 400 cases of death in
Australia occurred due to diabetes and nearly 55% of these deaths was due to T2DM. There
were 1 million hospitalizations due to diabetes with majority of the cases being reported from
the remote and very remote areas (Australian Institute of Health and Welfare 2018). Higher
rate of mortality and morbidity in the remote and very remote areas indicate that there is
prevalence of health inequality and thus strategy 2 promotes increase in the primary care
access in remote or very remote areas under the presence of multidisciplinary teams and
proper funding (Sanding Council on Health. 2013). The study conducted by Somerville et al.
(2017) highlighted that due to lack of proper funding in the remote areas, of Australia the
health inequality in diabetes management is higher. Channelization of proper funds will help
to implement advanced-technological based primary healthcare like tele-health, e-health and
NURSING
Introduction
The National Primary Health Care Strategic Framework (NPHCSF) is the first
national statement by the Standing Council on Health. It endorses an agreed approach for
developing robust primary health care system in Australia. Research suggests that primary
health care is more efficient in lowering the rate of hospitalisation and reducing health
inequalities (Sanding Council on Health 2013). The following essay will focus on the
strategic outcome two of NPSHCF and its expected outcomes. The outcomes or proposed
goals of NPSHCF will be linked with the management of Type 2 diabetes and reducing the
health inequalities in healthcare access.
Evaluation of the Australian PHC Strategic Framework
The strategic outcome 2 of NPHCSF (2013) deals with increasing the overall access
of primary healthcare by the application of the integrated service system and thereby helping
to reduce health inequity. This strategic outcome is extremely relevant to Type 2 Diabetes
Mellitus which is a national health issue in Australia. During 2015, 16, 400 cases of death in
Australia occurred due to diabetes and nearly 55% of these deaths was due to T2DM. There
were 1 million hospitalizations due to diabetes with majority of the cases being reported from
the remote and very remote areas (Australian Institute of Health and Welfare 2018). Higher
rate of mortality and morbidity in the remote and very remote areas indicate that there is
prevalence of health inequality and thus strategy 2 promotes increase in the primary care
access in remote or very remote areas under the presence of multidisciplinary teams and
proper funding (Sanding Council on Health. 2013). The study conducted by Somerville et al.
(2017) highlighted that due to lack of proper funding in the remote areas, of Australia the
health inequality in diabetes management is higher. Channelization of proper funds will help
to implement advanced-technological based primary healthcare like tele-health, e-health and
2
NURSING
thereby helping to improve the health outcome. The strategic outcome two focuses on
channelization of fund along with increase in implementation of Personally Controlled
Electronic Health Record (PCEHR) throughout Australia (Sanding Council on Health. 2013).
Two Determinants of Health
The social factors that promote the development of T2DM include lack of
employment or financial crisis leading to the development of stress and substance abuse that
ultimate increase the vulnerability of diabetes. Depression due to social isolation increase
sedentary behaviour and obesity that leads to T2DM development (Hermanns, Bremmer &
Snoek, 2018). Aboriginals and Torres Strait Islanders are four times more likely to develop
T2DM in comparison to the non-indigenous population of Australia (Diabetes Australia
2019) The statistics also showed that the Aboriginals who have high blood pressure are 9%
more likely to develop T2DM in comparison to the non-indigenous population with
hypertension (Burrow & Ride, 2016). This increased prevalence of diabetes among
indigenous population shows inequity in the prognosis of T2DM and thus require proper
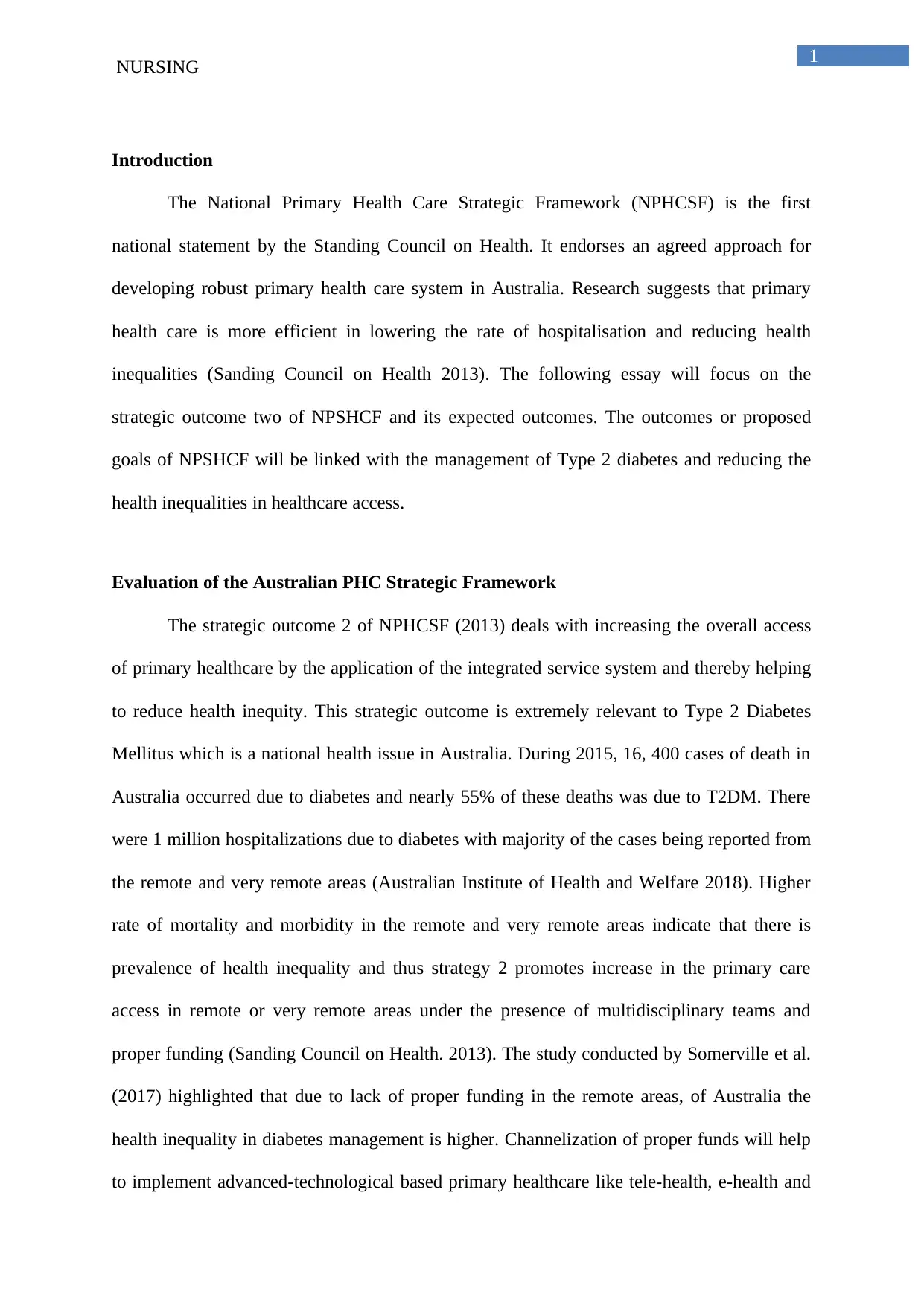
primary healthcare intervention. During 2014 to 15, the prevalence of diabetes among the
adult men were higher than women. This increased probability of T2DM in men is higher
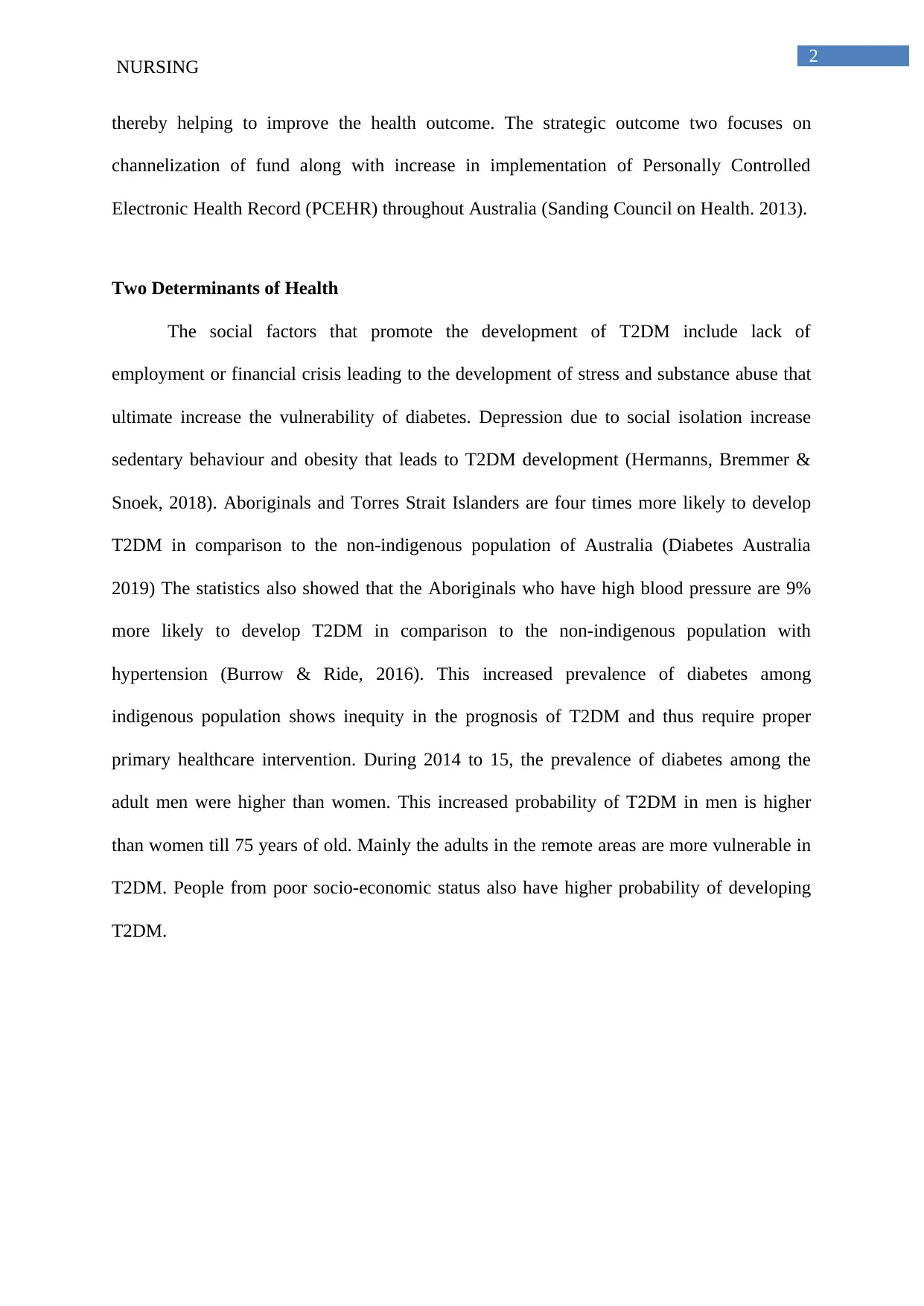
than women till 75 years of old. Mainly the adults in the remote areas are more vulnerable in
T2DM. People from poor socio-economic status also have higher probability of developing
T2DM.
NURSING
thereby helping to improve the health outcome. The strategic outcome two focuses on
channelization of fund along with increase in implementation of Personally Controlled
Electronic Health Record (PCEHR) throughout Australia (Sanding Council on Health. 2013).
Two Determinants of Health
The social factors that promote the development of T2DM include lack of
employment or financial crisis leading to the development of stress and substance abuse that
ultimate increase the vulnerability of diabetes. Depression due to social isolation increase
sedentary behaviour and obesity that leads to T2DM development (Hermanns, Bremmer &
Snoek, 2018). Aboriginals and Torres Strait Islanders are four times more likely to develop
T2DM in comparison to the non-indigenous population of Australia (Diabetes Australia
2019) The statistics also showed that the Aboriginals who have high blood pressure are 9%
more likely to develop T2DM in comparison to the non-indigenous population with
hypertension (Burrow & Ride, 2016). This increased prevalence of diabetes among
indigenous population shows inequity in the prognosis of T2DM and thus require proper
primary healthcare intervention. During 2014 to 15, the prevalence of diabetes among the
adult men were higher than women. This increased probability of T2DM in men is higher
than women till 75 years of old. Mainly the adults in the remote areas are more vulnerable in
T2DM. People from poor socio-economic status also have higher probability of developing
T2DM.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
NURSING
Figure: Prevalence of Diabetes among adults who are aged 18 years and above (2014 to
2015)
(Source: Australian Institute of Health and Welfare, 2015)
Figure: Prevalence of Diabetes based on the Social Determinates of Health
NURSING
Figure: Prevalence of Diabetes among adults who are aged 18 years and above (2014 to
2015)
(Source: Australian Institute of Health and Welfare, 2015)
Figure: Prevalence of Diabetes based on the Social Determinates of Health
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
NURSING
(Source: Australian Institute of Health and Welfare, 2015)
WHO 5 principles
WHO’s has five principles for the promotion of primary healthcare. First principle is
universal access to healthcare and healthcare coverage on basis of need of the patient (World
Health Organization 2003). The NPHCSF strategic outcome two, aims is to reduce equity and
increase the healthcare access. In order to increase the comprehensive healthcare access,
long-term relationship with the consumers and healthcare practitioner is established and this
healthy relationship helps in understanding of the clinical priority and basic needs and
thereby helping to improve the healthcare access. The second principle of WHO emphasize
on ccommitment towards healthcare equity as a part of the developmental oriented process
for promoting social justice. The objective of the strategic planning 2 of NPHCF, promotes
working of the primary healthcare professionals in unison as multidisciplinary team in order
develop the approach of care. Improving service delivery approach under the presence of
multidisciplinary team like nurse, occupational therapists, psychologist and dieticians will
help to increase the access of diabetes care. The third and fourth principle of WHO include
community based participation in defining and implementing proper agenda in healthcare and
inter-sectoral approaches towards health (World Health Organization 2003). Towards
improving inter-sectoral approaches, exploration of funding initiatives is selected as one of
the agenda behind strategic outcome 2. Increasing the level of funding will help to earn
collaboration from different healthcare bodies to develop effective yet person-centred
treatment plan. WHO’ last principle is proper implementation of the healthcare technology
and is also supported by strategic outcome two in promotion of eHealth and other electronic
records (NPHCF, 2013).
NURSING
(Source: Australian Institute of Health and Welfare, 2015)
WHO 5 principles
WHO’s has five principles for the promotion of primary healthcare. First principle is
universal access to healthcare and healthcare coverage on basis of need of the patient (World
Health Organization 2003). The NPHCSF strategic outcome two, aims is to reduce equity and
increase the healthcare access. In order to increase the comprehensive healthcare access,
long-term relationship with the consumers and healthcare practitioner is established and this
healthy relationship helps in understanding of the clinical priority and basic needs and
thereby helping to improve the healthcare access. The second principle of WHO emphasize
on ccommitment towards healthcare equity as a part of the developmental oriented process
for promoting social justice. The objective of the strategic planning 2 of NPHCF, promotes
working of the primary healthcare professionals in unison as multidisciplinary team in order
develop the approach of care. Improving service delivery approach under the presence of
multidisciplinary team like nurse, occupational therapists, psychologist and dieticians will
help to increase the access of diabetes care. The third and fourth principle of WHO include
community based participation in defining and implementing proper agenda in healthcare and
inter-sectoral approaches towards health (World Health Organization 2003). Towards
improving inter-sectoral approaches, exploration of funding initiatives is selected as one of
the agenda behind strategic outcome 2. Increasing the level of funding will help to earn
collaboration from different healthcare bodies to develop effective yet person-centred
treatment plan. WHO’ last principle is proper implementation of the healthcare technology
and is also supported by strategic outcome two in promotion of eHealth and other electronic
records (NPHCF, 2013).
5
NURSING
Self-Reflection
In order to promote holistic care practice under primary healthcare settings, I will first
focus on the level of health awareness and health literacy for people in remote and in very
remote areas. Increase in the level of health literacy will help to increase the level of
healthcare access. In order to design the care plan with a holistic approach that is covering
both physical (obesity, blood pressure and high glucose) and mental well-being (depression
and stress), I will take help from the multidisciplinary team (Moffat & Mercer, 2015).
Understanding proper clinical priority will help to widen the probability of delivering person
centred act.
Conclusion
Thus from the above discussion, it can be concluded that health inequalities exists in
effective management of diabetes of the people in the remote or remote areas and aboriginals.
The health inequalities can be addressed by proper implementation of the WHO’s 5 principle
of the primary healthcare and aligning the same with the strategic outcome 2 of the NPHCF.
It is the duty of the healthcare professional to abide by the guidelines of WHO and NPHCF in
order to design holistic care.
NURSING
Self-Reflection
In order to promote holistic care practice under primary healthcare settings, I will first
focus on the level of health awareness and health literacy for people in remote and in very
remote areas. Increase in the level of health literacy will help to increase the level of
healthcare access. In order to design the care plan with a holistic approach that is covering
both physical (obesity, blood pressure and high glucose) and mental well-being (depression
and stress), I will take help from the multidisciplinary team (Moffat & Mercer, 2015).
Understanding proper clinical priority will help to widen the probability of delivering person
centred act.
Conclusion
Thus from the above discussion, it can be concluded that health inequalities exists in
effective management of diabetes of the people in the remote or remote areas and aboriginals.
The health inequalities can be addressed by proper implementation of the WHO’s 5 principle
of the primary healthcare and aligning the same with the strategic outcome 2 of the NPHCF.
It is the duty of the healthcare professional to abide by the guidelines of WHO and NPHCF in
order to design holistic care.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
NURSING
References
Australian Institute of Health and Welfare. (2015). Diabetes snapshot. Access date: 21st
August 2019. Retrieved from: https://www.aihw.gov.au/reports/diabetes/diabetes-
snapshot/contents/how-many-australians-have-diabetes
Australian Institute of Health and Welfare. (2018). Diabetes snapshot. Access date: 21st
August 2019. Retrieved from: https://www.aihw.gov.au/reports/diabetes/diabetes-
snapshot/contents/how-many-australians-have-diabetes/type-2-diabetes
Burrow, S., & Ride, K. (2016). Review of diabetes among Aboriginal and Torres Strait
Islander people. Access date:
https://pdfs.semanticscholar.org/7a8b/458d7864e1cfa7eb8e5b0ae8b2bfbb5ab9a4.pdf
Diabetes Australia. 2019. Aboriginal and Torres Strait Islanders. Access date: 21st August
2019. Retrieved from: https://www.diabetesaustralia.com.au/aboriginal-and-torres-
strait-islanders
Hermanns, N., Bremmer, M. A., & Snoek, F. J. (2018). Diabetes distress. Depression and
Type 2 Diabetes.
Moffat, K., & Mercer, S. W. (2015). Challenges of managing people with multimorbidity in
today’s healthcare systems. BMC family practice, 16(1), 129.
Sanding Council on Health. 2013. National Primary Health Care Strategic Framework
(NPHCSF). Access date: 21st August 2019. Retrieved from:
https://www.health.qld.gov.au/__data/assets/pdf_file/0027/434853/nphc_strategic_fra
mework_final.pdf
NURSING
References
Australian Institute of Health and Welfare. (2015). Diabetes snapshot. Access date: 21st
August 2019. Retrieved from: https://www.aihw.gov.au/reports/diabetes/diabetes-
snapshot/contents/how-many-australians-have-diabetes
Australian Institute of Health and Welfare. (2018). Diabetes snapshot. Access date: 21st
August 2019. Retrieved from: https://www.aihw.gov.au/reports/diabetes/diabetes-
snapshot/contents/how-many-australians-have-diabetes/type-2-diabetes
Burrow, S., & Ride, K. (2016). Review of diabetes among Aboriginal and Torres Strait
Islander people. Access date:
https://pdfs.semanticscholar.org/7a8b/458d7864e1cfa7eb8e5b0ae8b2bfbb5ab9a4.pdf
Diabetes Australia. 2019. Aboriginal and Torres Strait Islanders. Access date: 21st August
2019. Retrieved from: https://www.diabetesaustralia.com.au/aboriginal-and-torres-
strait-islanders
Hermanns, N., Bremmer, M. A., & Snoek, F. J. (2018). Diabetes distress. Depression and
Type 2 Diabetes.
Moffat, K., & Mercer, S. W. (2015). Challenges of managing people with multimorbidity in
today’s healthcare systems. BMC family practice, 16(1), 129.
Sanding Council on Health. 2013. National Primary Health Care Strategic Framework
(NPHCSF). Access date: 21st August 2019. Retrieved from:
https://www.health.qld.gov.au/__data/assets/pdf_file/0027/434853/nphc_strategic_fra
mework_final.pdf
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING
Somerville, R., Cullen, J., McIntyre, M., Townsend, C., & Pope, S. (2017). Engaging
Aboriginal and Torres Strait Islander peoples in the ‘Proper Way’. Newparadigm: the
Australian Journal on Psychosocial Rehabilitation, 14, 1-4.
World Health Organization. 2003. Chapter 7: Health Systems: principled integrated care.
Access date: 21st August 2019. Retrieved from:
https://www.who.int/whr/2003/chapter7/en/index1.html
NURSING
Somerville, R., Cullen, J., McIntyre, M., Townsend, C., & Pope, S. (2017). Engaging
Aboriginal and Torres Strait Islander peoples in the ‘Proper Way’. Newparadigm: the
Australian Journal on Psychosocial Rehabilitation, 14, 1-4.
World Health Organization. 2003. Chapter 7: Health Systems: principled integrated care.
Access date: 21st August 2019. Retrieved from:
https://www.who.int/whr/2003/chapter7/en/index1.html

8
NURSING
NURSING
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





