Principles of Care: Maslow's Theory, Rights & Legislation Analysis
VerifiedAdded on 2023/06/14
|11
|4155
|470
Report
AI Summary
This report delves into the principles of care, emphasizing the importance of dignity, privacy, and effective communication in providing quality care to vulnerable individuals. It applies Maslow's hierarchy of needs to illustrate how care providers can meet patient needs and enhance their well-being. The report also highlights the significance of protecting patient rights and autonomy through relevant legislations and policies, such as the Health and Safety at Work Act 1974, Equality Act 2010, and Care Act 2014. It discusses how these measures promote equality, safety, and person-centered care, while addressing potential ethical dilemmas faced by care providers, stressing the need to uphold organizational policies and procedures to ensure legal compliance and ethical practice.

Principles of Care
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The concept of principle of care is generally defined as a way by which early care
providers behave towards people while providing care. It is an approach by which care providers
can provide care or support to people who significantly requires effective care. While providing
care to vulnerable people, it generally involves various principles through which care providers
can provide an effective care such as dignity, privacy, effective communication and many more.
In this report, it will cover effective care principles and it can be explained by using specific
theory such as Maslow's theory. And, care providers can apply theory in their practice to meet
the needs of each patient so that they can feel satisfied. The report will also cover rights and
autonomy of vulnerable people that is need to be protected with the help of some legislations and
policies through which care professionals can deliver a quality care towards vulnerable people
(Maynard and Williams, 2018).
The care principles are generally based on idea of human rights. It can define care
principles in a way social and health care along with early years care provider should behave
towards vulnerable people in their care. It is quite important to a productive social and health
care practice. In this, care principles generally support care providers to determine as well as
mirror upon position of dignity while providing all care services as well as to commit to
upholding the dignity of those people whom care providers can support. In this, care providers
must treat vulnerable people in a way that they would like to be treated as well as care workers
must work in best interests of people (Principles of Health and Social Care Practice, 2021). The
care providers can easily get to know about their patients as well as involve empathy with them.
Care worker's main aim is to enhance quality life for vulnerable people. In this, having support
principles can aid to provide specific guidelines on how care providers can effectively meet their
patient's needs. The concept of care is quite important in both health and social care as well as it
is what makes it actually successful (Feo, Kitson and Conroy, 2018).
Well-being and social care is essential towards both society and across nation. Well-
being of population is paramount and is important for survival of nation. Therefore, it is the only
reason why government of United Kingdom has invested more funds or money on NHS
(National Health Services). In this, providing social and health care services towards vulnerable
people, maintaining patient's privacy along with communication can specifically pose a barrier
that can develop risk to patient's health. And, to overcome such barriers or reduce the developing
risks, care providers must deliver an effective quality care with help of various skills such as
providers behave towards people while providing care. It is an approach by which care providers
can provide care or support to people who significantly requires effective care. While providing
care to vulnerable people, it generally involves various principles through which care providers
can provide an effective care such as dignity, privacy, effective communication and many more.
In this report, it will cover effective care principles and it can be explained by using specific
theory such as Maslow's theory. And, care providers can apply theory in their practice to meet
the needs of each patient so that they can feel satisfied. The report will also cover rights and
autonomy of vulnerable people that is need to be protected with the help of some legislations and
policies through which care professionals can deliver a quality care towards vulnerable people
(Maynard and Williams, 2018).
The care principles are generally based on idea of human rights. It can define care
principles in a way social and health care along with early years care provider should behave
towards vulnerable people in their care. It is quite important to a productive social and health
care practice. In this, care principles generally support care providers to determine as well as
mirror upon position of dignity while providing all care services as well as to commit to
upholding the dignity of those people whom care providers can support. In this, care providers
must treat vulnerable people in a way that they would like to be treated as well as care workers
must work in best interests of people (Principles of Health and Social Care Practice, 2021). The
care providers can easily get to know about their patients as well as involve empathy with them.
Care worker's main aim is to enhance quality life for vulnerable people. In this, having support
principles can aid to provide specific guidelines on how care providers can effectively meet their
patient's needs. The concept of care is quite important in both health and social care as well as it
is what makes it actually successful (Feo, Kitson and Conroy, 2018).
Well-being and social care is essential towards both society and across nation. Well-
being of population is paramount and is important for survival of nation. Therefore, it is the only
reason why government of United Kingdom has invested more funds or money on NHS
(National Health Services). In this, providing social and health care services towards vulnerable
people, maintaining patient's privacy along with communication can specifically pose a barrier
that can develop risk to patient's health. And, to overcome such barriers or reduce the developing
risks, care providers must deliver an effective quality care with help of various skills such as
having effective communication with patients, privacy, empathy and many other (Van Melle et.
al., 2019). In addition, maintaining confidentiality is also an essential aspect among care
organization, as care providers must keep all data linked with patients private, any of data which
is violated privacy of user will require the consent of patients. The care providers must involve
empathy that decisions about their patients are informed choice of them. In this, these such are
specific principles which apply to well-being and social care practice to improve patient
outcomes.
While working with their responsibilities or duties, care providers have to face various
difficulties or challenges that can lead to provide ineffective care to patients and resulting in
unmet needs of their patients. In order to deliver an efficient or effective care to vulnerable
people, here is a theory that can help to improve care practices so that it can improve patient's
outcome. With help of Maslow's theory, care providers can provide cost effective care to their
patients so that it can enhance their well-being (Adapting Maslow’s Hierarchy of Needs to
Nursing Communication, 2018). In Maslow's theory on hierarchy of needs, it generally posits
that human beings are mainly motivated by various intrinsic needs for self-actualization. It
explains that requirements must be met in a hierarchical way, where meeting of one's need can
motivate the person to desire meeting higher needs. The theory is mainly predicted on basic five
requirements and are as mentioned below:
Physiological Needs, in this, Physiological are needs which must be met before patients
can worry about them. In order to begin with, care provider's must require breaks to feel easy, to
eat their stuff or can catch their breaths. They can also require communication tool which can
enable them to interconnect as well as collaborate more effectively. In addition, care worker's
capability to work can effectively up the levels of hierarchy, to fulfil more complex requirements
is significantly based on accomplish the Physiological needs. Furthermore, while providing
Physiological needs to patients, care workers must have some skills such as problem solving,
good communication, self-awareness and confidence. Through assessing such skills, care
workers can able to fulfil basic needs of their patients (Kitson, 2018).
Safety Needs, in this, all human involves some of its basic requirement to feel secure. In
context with health and social care, care workers consist specific tools with the help of which
they can protect their patients when their physical safety is at risk or harm.
al., 2019). In addition, maintaining confidentiality is also an essential aspect among care
organization, as care providers must keep all data linked with patients private, any of data which
is violated privacy of user will require the consent of patients. The care providers must involve
empathy that decisions about their patients are informed choice of them. In this, these such are
specific principles which apply to well-being and social care practice to improve patient
outcomes.
While working with their responsibilities or duties, care providers have to face various
difficulties or challenges that can lead to provide ineffective care to patients and resulting in
unmet needs of their patients. In order to deliver an efficient or effective care to vulnerable
people, here is a theory that can help to improve care practices so that it can improve patient's
outcome. With help of Maslow's theory, care providers can provide cost effective care to their
patients so that it can enhance their well-being (Adapting Maslow’s Hierarchy of Needs to
Nursing Communication, 2018). In Maslow's theory on hierarchy of needs, it generally posits
that human beings are mainly motivated by various intrinsic needs for self-actualization. It
explains that requirements must be met in a hierarchical way, where meeting of one's need can
motivate the person to desire meeting higher needs. The theory is mainly predicted on basic five
requirements and are as mentioned below:
Physiological Needs, in this, Physiological are needs which must be met before patients
can worry about them. In order to begin with, care provider's must require breaks to feel easy, to
eat their stuff or can catch their breaths. They can also require communication tool which can
enable them to interconnect as well as collaborate more effectively. In addition, care worker's
capability to work can effectively up the levels of hierarchy, to fulfil more complex requirements
is significantly based on accomplish the Physiological needs. Furthermore, while providing
Physiological needs to patients, care workers must have some skills such as problem solving,
good communication, self-awareness and confidence. Through assessing such skills, care
workers can able to fulfil basic needs of their patients (Kitson, 2018).
Safety Needs, in this, all human involves some of its basic requirement to feel secure. In
context with health and social care, care workers consist specific tools with the help of which
they can protect their patients when their physical safety is at risk or harm.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Belonging Needs, the needs are quite essential for patients while delivering care. It
generally involves to feel that both care providers and service users belong to same social group.
The needs can importantly include both feeling loved as well as feeling love to other people. It is
essential for care workers also to effectively know about feelings of their patients and this can be
done with help of effective communication. Through good communication, care workers can
build strong relationships with their patients, which can influence patient's outcome. Having an
effective communication among them can make patients to share their feelings or emotions with
care workers so that they can provide treatment or care as per their needs (Weeks, et. al., 2019).
Esteem needs, in this, mainly define the need for respect and appreciation as well. When
requirements of the above levels have been met or satisfied, esteem needs begin to play a large
role such as motivating the behavior of vulnerable people. In context with health and social care,
these such needs are the most basic desires of humans that they want as all humans have to be
accepted as well as valued by other people also. It is important for both the care provider and
service user, through the needs, care providers are effectively able to protect their patient's
privacy and dignity as well. Both service users and care provider can use their rights in suitable
situations when they feel insecure or not safe.
Self-actualization: In this, it is a process of development and growth through which a
person can attain their potential. In context with health and social care practice, having self-
actualization, care workers or providers can positively create an environment in which they can
feel energized by their care work. It can be met by having an effective communication with other
people, self-confidence, as well as having a capability to fix every ongoing or upcoming
problems while delivering care towards service user. As having an effective communication with
other care workers or with patients can help to develop an effective relationship with them. This
can improve better quality care and enhances outcomes of care organization. Having a problem-
solving skill among care workers can also help them to overcome any challenging or difficult
situations which can affect patient care (Lin, Lin and Chen, 2019).
In this, support in health and social care generally involves five basic principles which
are needed to be met such as safety, independence, good communication, dignity and privacy.
These all are necessarily required while providing care to vulnerable patients. Among all, having
positive communication among healthcare organization can develop patient's outcomes as well
as provide confidence to protect the rights and dignity of patients as well. These all can be
generally involves to feel that both care providers and service users belong to same social group.
The needs can importantly include both feeling loved as well as feeling love to other people. It is
essential for care workers also to effectively know about feelings of their patients and this can be
done with help of effective communication. Through good communication, care workers can
build strong relationships with their patients, which can influence patient's outcome. Having an
effective communication among them can make patients to share their feelings or emotions with
care workers so that they can provide treatment or care as per their needs (Weeks, et. al., 2019).
Esteem needs, in this, mainly define the need for respect and appreciation as well. When
requirements of the above levels have been met or satisfied, esteem needs begin to play a large
role such as motivating the behavior of vulnerable people. In context with health and social care,
these such needs are the most basic desires of humans that they want as all humans have to be
accepted as well as valued by other people also. It is important for both the care provider and
service user, through the needs, care providers are effectively able to protect their patient's
privacy and dignity as well. Both service users and care provider can use their rights in suitable
situations when they feel insecure or not safe.
Self-actualization: In this, it is a process of development and growth through which a
person can attain their potential. In context with health and social care practice, having self-
actualization, care workers or providers can positively create an environment in which they can
feel energized by their care work. It can be met by having an effective communication with other
people, self-confidence, as well as having a capability to fix every ongoing or upcoming
problems while delivering care towards service user. As having an effective communication with
other care workers or with patients can help to develop an effective relationship with them. This
can improve better quality care and enhances outcomes of care organization. Having a problem-
solving skill among care workers can also help them to overcome any challenging or difficult
situations which can affect patient care (Lin, Lin and Chen, 2019).
In this, support in health and social care generally involves five basic principles which
are needed to be met such as safety, independence, good communication, dignity and privacy.
These all are necessarily required while providing care to vulnerable patients. Among all, having
positive communication among healthcare organization can develop patient's outcomes as well
as provide confidence to protect the rights and dignity of patients as well. These all can be
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
protected by having positive communication among care workers and service users, making
patients more independent. These all can be done with help of active legislations, policies,
regulations as well as code of conducts on health and social care practice. It is essential for care
providers to be aware of these such legislations and code of conduct which are relevant to their
practice. The code of practice generally set particular standards of conduct expected of care
providers and can positively outlines attitudes and behaviours that are expected from them. In
this, code of practice can effectively guide care providers to be responsible by making sure that
they can answer for their activities, promote as well as maintain dignity, privacy, and rights of
vulnerable people who generally use care services, can work in association with other care
providers to ensure delivery of quality and safe care along with support and can communicate in
an open and effective manner to promote health and safety of vulnerable people. Other aspects in
this are esteem the rights of vulnerable people and maintaining their dignity and confidentiality
at every possible time. In addition, care practices are necessary in order to promote dignity of
care. There are various legislative measures along with regulations that can positively encourage
health and safety of vulnerable people at care organization. In this, some pieces of legislations
are as detailed below (Workplace health and safety standards, 2013):
Health and Safety at Work Act 1974: It is piece of legislation that can provide legal
framework to stimulate, promote as well as support increased standards of well-being and safety
in care organizations. The legislation can protect care workers as well as vulnerable people from
developing risks or harms.
Equality Act 2010: In health and social care, legislation generally protects those people
who receives care and care providers that can effectively provide care services from being
treated unfairly because of any particular characteristics. It mainly covers some protected
characteristics such as Gender reassignment, Sexual orientation, Disability, Religion, Marriage
and civil partnership, Race and many other. Any of mentioned practice to counter discrimination
and can positively promote equality by introducing anti-discrimination policy in care
organization. In addition, care providers have to maintain such standards set by healthcare
professionals or higher authorities, as it can help with consistency as standards can positively
ensures that working in health and care sectors meet a better-quality care level when giving care
along with support to vulnerable people (Guglielmin et. al., 2018).
patients more independent. These all can be done with help of active legislations, policies,
regulations as well as code of conducts on health and social care practice. It is essential for care
providers to be aware of these such legislations and code of conduct which are relevant to their
practice. The code of practice generally set particular standards of conduct expected of care
providers and can positively outlines attitudes and behaviours that are expected from them. In
this, code of practice can effectively guide care providers to be responsible by making sure that
they can answer for their activities, promote as well as maintain dignity, privacy, and rights of
vulnerable people who generally use care services, can work in association with other care
providers to ensure delivery of quality and safe care along with support and can communicate in
an open and effective manner to promote health and safety of vulnerable people. Other aspects in
this are esteem the rights of vulnerable people and maintaining their dignity and confidentiality
at every possible time. In addition, care practices are necessary in order to promote dignity of
care. There are various legislative measures along with regulations that can positively encourage
health and safety of vulnerable people at care organization. In this, some pieces of legislations
are as detailed below (Workplace health and safety standards, 2013):
Health and Safety at Work Act 1974: It is piece of legislation that can provide legal
framework to stimulate, promote as well as support increased standards of well-being and safety
in care organizations. The legislation can protect care workers as well as vulnerable people from
developing risks or harms.
Equality Act 2010: In health and social care, legislation generally protects those people
who receives care and care providers that can effectively provide care services from being
treated unfairly because of any particular characteristics. It mainly covers some protected
characteristics such as Gender reassignment, Sexual orientation, Disability, Religion, Marriage
and civil partnership, Race and many other. Any of mentioned practice to counter discrimination
and can positively promote equality by introducing anti-discrimination policy in care
organization. In addition, care providers have to maintain such standards set by healthcare
professionals or higher authorities, as it can help with consistency as standards can positively
ensures that working in health and care sectors meet a better-quality care level when giving care
along with support to vulnerable people (Guglielmin et. al., 2018).
Care Act 2014: In this, it effectively places both cares along with support legislations into
a single law. Having such legislation can support care providers to take specific person-centred
approach when they are safeguarding or protecting vulnerable people. It can help care providers
to directly involve people who need care as well as put forward the people who can aid reach
decisions that are best in interest of vulnerable people, when protecting their concerns and care
plans as well. In addition, risk assessment is also shown by care team to mitigate against chances
of misshapen. Care team contain a duty to report any risk which is linked with their role to care
administration. Furthermore, it can stress on prevention as well as manage the developing risks
that concentrates on strengths as well as abilities of vulnerable patients and encourage them to
live more autonomously for long duration. In addition, the legislation will make support and care
fairer and clearer as well for those who actually need it (Revell and Elton-Chalcraft, 2021).
In this, care providers are most of the times faced with some ethical dilemma that is quite
contradictory to them. Therefore, it is quite crucial that care providers can uphold policies as
well as procedures of care organization to avoid unnecessary legal difficulties or challenges.
Vulnerable people involve various unique beliefs, values, cultures and orientations as well as
these such factors are sometimes what forms their decisions or opinions. Sometimes, difficulties
may arises in culture, beliefs or values among care provider as well as vulnerable people. In
some cases, people can think of not to take drugs as it is against their belief or religions and it is
necessary to take drugs on time as it can help them to get their health better. Similarly,
vulnerable people contain right to take their own decisions but, most of the times people make
decisions that actually make no sense and which reduces their health, thus care provider is faced
with such type of ethical dilemma. Care providers cannot force vulnerable people to do things
against their will, but they also involve a obligation to take care of vulnerable people even if they
refuse their medications. Moreover, management of healthcare organization have to decide in
most severe situations about what is best suitable care for vulnerable people to better their well-
being. In addition, a method of dealing with such ethical dilemma is capability to express
empathy as well as emotions, even in situation where people refuse to obey, it is value
substantial them with warm heart that care providers are always there to shield their well-being
interest as well as can make their health much better (Paillé, and Halilem, 2019).
From above discussion, it is concluded that well-being and social care play an essential role
within community. Care provider is mainly responsible for furnishing effective care services to
a single law. Having such legislation can support care providers to take specific person-centred
approach when they are safeguarding or protecting vulnerable people. It can help care providers
to directly involve people who need care as well as put forward the people who can aid reach
decisions that are best in interest of vulnerable people, when protecting their concerns and care
plans as well. In addition, risk assessment is also shown by care team to mitigate against chances
of misshapen. Care team contain a duty to report any risk which is linked with their role to care
administration. Furthermore, it can stress on prevention as well as manage the developing risks
that concentrates on strengths as well as abilities of vulnerable patients and encourage them to
live more autonomously for long duration. In addition, the legislation will make support and care
fairer and clearer as well for those who actually need it (Revell and Elton-Chalcraft, 2021).
In this, care providers are most of the times faced with some ethical dilemma that is quite
contradictory to them. Therefore, it is quite crucial that care providers can uphold policies as
well as procedures of care organization to avoid unnecessary legal difficulties or challenges.
Vulnerable people involve various unique beliefs, values, cultures and orientations as well as
these such factors are sometimes what forms their decisions or opinions. Sometimes, difficulties
may arises in culture, beliefs or values among care provider as well as vulnerable people. In
some cases, people can think of not to take drugs as it is against their belief or religions and it is
necessary to take drugs on time as it can help them to get their health better. Similarly,
vulnerable people contain right to take their own decisions but, most of the times people make
decisions that actually make no sense and which reduces their health, thus care provider is faced
with such type of ethical dilemma. Care providers cannot force vulnerable people to do things
against their will, but they also involve a obligation to take care of vulnerable people even if they
refuse their medications. Moreover, management of healthcare organization have to decide in
most severe situations about what is best suitable care for vulnerable people to better their well-
being. In addition, a method of dealing with such ethical dilemma is capability to express
empathy as well as emotions, even in situation where people refuse to obey, it is value
substantial them with warm heart that care providers are always there to shield their well-being
interest as well as can make their health much better (Paillé, and Halilem, 2019).
From above discussion, it is concluded that well-being and social care play an essential role
within community. Care provider is mainly responsible for furnishing effective care services to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
patients as well as aid them in treating and preventing specific illnesses. In this, without
delivering an effective care within well-bieng and social care practice, it is quite impossible to
overcome or cope with specific illnesses. This can increase rates of hospitalization, increased
morbidity and mortality rates also. Moreover, it is important that care organizations must involve
an effective working relationship as it can positively enhances delivery rates.
delivering an effective care within well-bieng and social care practice, it is quite impossible to
overcome or cope with specific illnesses. This can increase rates of hospitalization, increased
morbidity and mortality rates also. Moreover, it is important that care organizations must involve
an effective working relationship as it can positively enhances delivery rates.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFLECTIVE ACCOUNT.
Reflection model such as Gibbs reflection model involve six stages and these are as
mentioned below:
Description:
I have described above that having principle of care among health and social care sectors
are quite important towards productive well-being and social care sectors. In this, it can consist a
goal to effectively support acre providers to easily determine as well as can mirror the dignity of
vulnerable people while providing care services and can also commit to keep their dignity while
encouraging them. I have illustrated that principles generally means moral rule that simply guide
specific behavior's and sometimes consistence with regulations associated with moral law. In
this, there is also a discussion about care providers must follow legislations such as Health and
Safety Act 1974, Equality Act 2010, conduct of risk assessment as well as determine how to
work against such risks. An effective care can give suitable well-being and empowerment which
will be right for vulnerable people. To protect vulnerable people from such abuses or
discrimination among care organization, some pieces of legislations are made so that people can
feel free or independent and can effectively improve their health (Truong et. al., 2021).
Feelings:
Through this, I feel that while providing care to vulnerable people, I lack in some of the
skills such as lack of communication, integrity, does not know more about legislations or policies
and many more. With the help of care team or care managers, I effectively develop my skills and
this can help me to improve my care towards vulnerable people, and resulting in better outcomes.
Evaluation:
While providing care to vulnerable people, I have learned that effective communication
skills, empathy, dignity and respect can play an important role to improve their health. With help
of communication, I can able to develop positive relationship with patients and make them share
their feelings with me so that I can deliver quality care as per their requirement. With help of
legislations, I can get to know that how rights of vulnerable people are protected so that I can
improve the well-being of patients (Ratima, 2019).
Reflection model such as Gibbs reflection model involve six stages and these are as
mentioned below:
Description:
I have described above that having principle of care among health and social care sectors
are quite important towards productive well-being and social care sectors. In this, it can consist a
goal to effectively support acre providers to easily determine as well as can mirror the dignity of
vulnerable people while providing care services and can also commit to keep their dignity while
encouraging them. I have illustrated that principles generally means moral rule that simply guide
specific behavior's and sometimes consistence with regulations associated with moral law. In
this, there is also a discussion about care providers must follow legislations such as Health and
Safety Act 1974, Equality Act 2010, conduct of risk assessment as well as determine how to
work against such risks. An effective care can give suitable well-being and empowerment which
will be right for vulnerable people. To protect vulnerable people from such abuses or
discrimination among care organization, some pieces of legislations are made so that people can
feel free or independent and can effectively improve their health (Truong et. al., 2021).
Feelings:
Through this, I feel that while providing care to vulnerable people, I lack in some of the
skills such as lack of communication, integrity, does not know more about legislations or policies
and many more. With the help of care team or care managers, I effectively develop my skills and
this can help me to improve my care towards vulnerable people, and resulting in better outcomes.
Evaluation:
While providing care to vulnerable people, I have learned that effective communication
skills, empathy, dignity and respect can play an important role to improve their health. With help
of communication, I can able to develop positive relationship with patients and make them share
their feelings with me so that I can deliver quality care as per their requirement. With help of
legislations, I can get to know that how rights of vulnerable people are protected so that I can
improve the well-being of patients (Ratima, 2019).
Analysis:
From all the above, I have analysed that in order to improve patient care or well-being,
care provider must have active skills through which they can able to provide a care which their
patients need to improve their health. Having communication skills are most important among
care organizations as it can help to develop as well as maintain an effective relationship with
patients to increase their well-being.
Conclusion:
From all my study, it is positively concluded that having principles of care among care
organization generally influence outcomes of care sector. It is quite necessary among care
sectors. Along with this, care providers must involve specific skills through which they can
provide quality care to their patients. It is also concluded that legislations or policies also play an
important role in care sectors as through which care providers can positively protects the rights
of vulnerable people. This can make people to feel secured or safe (Lillo-Crespo and Sierras-
Davó, 2019).
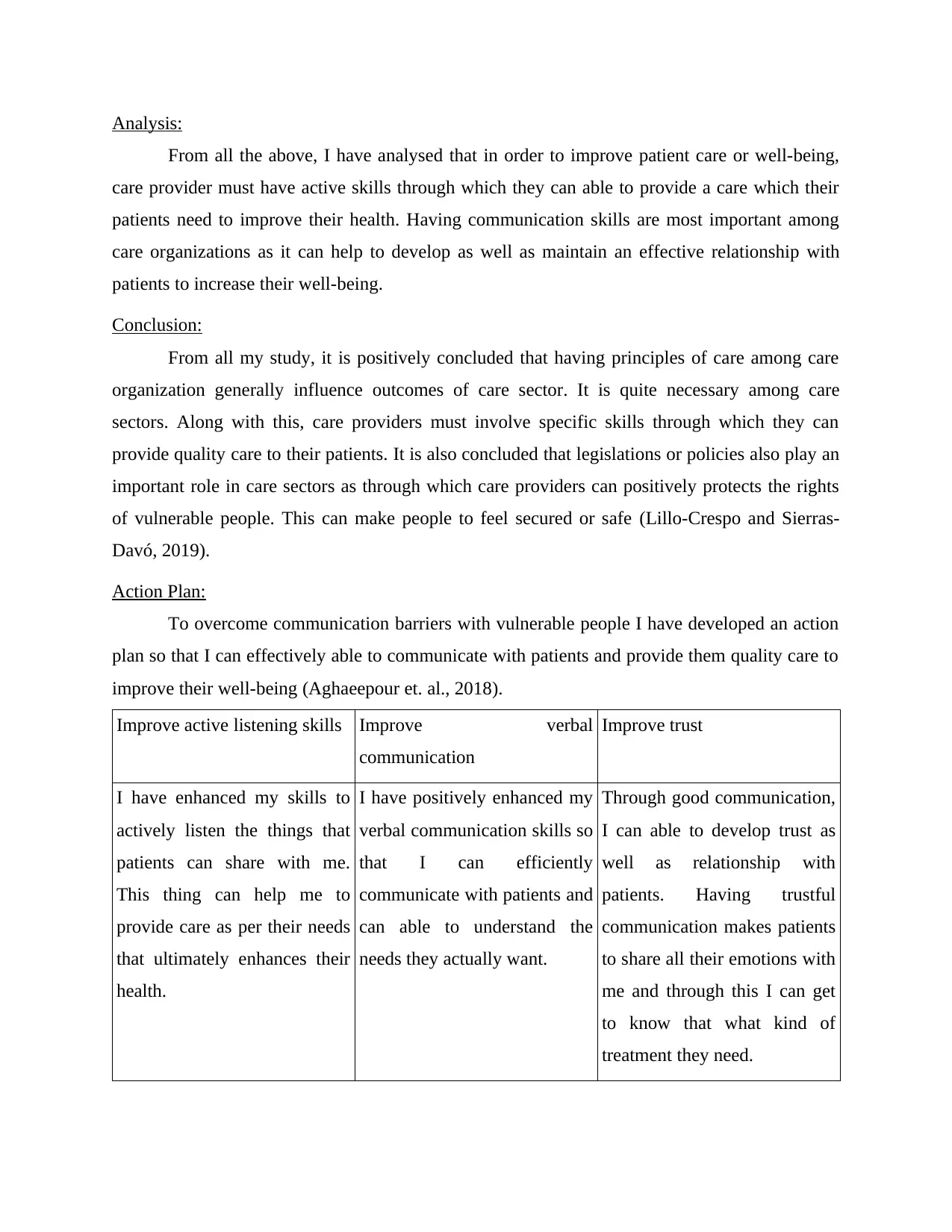
Action Plan:
To overcome communication barriers with vulnerable people I have developed an action
plan so that I can effectively able to communicate with patients and provide them quality care to
improve their well-being (Aghaeepour et. al., 2018).
Improve active listening skills Improve verbal
communication
Improve trust
I have enhanced my skills to
actively listen the things that
patients can share with me.
This thing can help me to
provide care as per their needs
that ultimately enhances their
health.
I have positively enhanced my
verbal communication skills so
that I can efficiently
communicate with patients and
can able to understand the
needs they actually want.
Through good communication,
I can able to develop trust as
well as relationship with
patients. Having trustful
communication makes patients
to share all their emotions with
me and through this I can get
to know that what kind of
treatment they need.
From all the above, I have analysed that in order to improve patient care or well-being,
care provider must have active skills through which they can able to provide a care which their
patients need to improve their health. Having communication skills are most important among
care organizations as it can help to develop as well as maintain an effective relationship with
patients to increase their well-being.
Conclusion:
From all my study, it is positively concluded that having principles of care among care
organization generally influence outcomes of care sector. It is quite necessary among care
sectors. Along with this, care providers must involve specific skills through which they can
provide quality care to their patients. It is also concluded that legislations or policies also play an
important role in care sectors as through which care providers can positively protects the rights
of vulnerable people. This can make people to feel secured or safe (Lillo-Crespo and Sierras-
Davó, 2019).
Action Plan:
To overcome communication barriers with vulnerable people I have developed an action
plan so that I can effectively able to communicate with patients and provide them quality care to
improve their well-being (Aghaeepour et. al., 2018).
Improve active listening skills Improve verbal
communication
Improve trust
I have enhanced my skills to
actively listen the things that
patients can share with me.
This thing can help me to
provide care as per their needs
that ultimately enhances their
health.
I have positively enhanced my
verbal communication skills so
that I can efficiently
communicate with patients and
can able to understand the
needs they actually want.
Through good communication,
I can able to develop trust as
well as relationship with
patients. Having trustful
communication makes patients
to share all their emotions with
me and through this I can get
to know that what kind of
treatment they need.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals:
Aghaeepour, N. et. al., 2018. A proteomic clock of human pregnancy. American journal of
obstetrics and gynecology, 218(3), pp.347-e1.
Aveyard, H., 2018. Doing a literature review in health and social care: A practical guide.
Bowman, M., 2021. A framework for scaffolding academic reflective writing in
dentistry. European Journal of Dental Education, 25(1), pp.35-49.
Caveney, N. et. al., 2020. Police reform, austerity and ‘cop culture’: time to change the
record?. Policing and society, 30(10), pp.1210-1225.
Crosby, S.D., Howell, P. and Thomas, S., 2018. Social justice education through trauma-
informed teaching. Middle School Journal, 49(4), pp.15-23.
Dee, M. and Hanson, V.L., 2019. Effectively including the voice of residents in care home
design. Design for Health, 3(2), pp.283-304.
Eaves, T. et. al., 2020. The Professional Is the Personal: A Qualitative Exploration of Self-Care
Practices in Clinical Infant Mental Health Practitioners. Journal of Social Service
Research, 47(3), pp.369-387.
Feo, R., Kitson, A. and Conroy, T., 2018. How fundamental aspects of nursing care are defined
in the literature: A scoping review. Journal of Clinical Nursing, 27(11-12), pp.2189-
2229.
Guglielmin, M. et. al., 2018. A scoping review of the implementation of health in all policies at
the local level. Health policy, 122(3), pp.284-292.
Kitson, A.L., 2018. The fundamentals of care framework as a point-of-care nursing
theory. Nursing Research, 67(2), pp.99-107.
Lillo-Crespo, M. and Sierras-Davó, M.C., 2019. Quality Improvement with Compassion:
Developing Healthcare Improvement Science in the European Health Professions’
Education. In Values of the University in a Time of Uncertainty (pp. 231-240). Springer,
Cham.
Lin, Y.K., Lin, M. and Chen, H., 2019. Do electronic health records affect quality of care?
Evidence from the HITECH Act. Information Systems Research, 30(1), pp.306-318.
Maroun, W., 2020. A conceptual model for understanding corporate social responsibility
assurance practice. Journal of Business Ethics, 161(1), pp.187-209.
Maynard, A. and Williams, A., 2018. Privatisation and the National Health Service.
In Privatisation and the welfare state (pp. 95-110). Routledge.
Paillé, P. and Halilem, N., 2019. Systematic review on environmental innovativeness: A
knowledge-based resource view. Journal of cleaner production, 211, pp.1088-1099.
Ratima, T., 2019. Retrospection of a Maori Tutor Educator's Bi-Cultural Teaching Discourse in
Te Wananga o Aotearoa (TWoA): A Narrative Portfolio. In Handbook of Research on
Indigenous Knowledge and Bi-Culturalism in a Global Context (pp. 136-148). IGI
Global.
Revell, L. and Elton-Chalcraft, S., 2021. Extremism, values, and education in policy and
practice. In Oxford Research Encyclopedia of Education.
Steele, L. et. al., 2020. Ending confinement and segregation: Barriers to realising human rights in
the everyday lives of people living with dementia in residential aged care. Australian
Journal of Human Rights, 26(2), pp.308-328.
Books and Journals:
Aghaeepour, N. et. al., 2018. A proteomic clock of human pregnancy. American journal of
obstetrics and gynecology, 218(3), pp.347-e1.
Aveyard, H., 2018. Doing a literature review in health and social care: A practical guide.
Bowman, M., 2021. A framework for scaffolding academic reflective writing in
dentistry. European Journal of Dental Education, 25(1), pp.35-49.
Caveney, N. et. al., 2020. Police reform, austerity and ‘cop culture’: time to change the
record?. Policing and society, 30(10), pp.1210-1225.
Crosby, S.D., Howell, P. and Thomas, S., 2018. Social justice education through trauma-
informed teaching. Middle School Journal, 49(4), pp.15-23.
Dee, M. and Hanson, V.L., 2019. Effectively including the voice of residents in care home
design. Design for Health, 3(2), pp.283-304.
Eaves, T. et. al., 2020. The Professional Is the Personal: A Qualitative Exploration of Self-Care
Practices in Clinical Infant Mental Health Practitioners. Journal of Social Service
Research, 47(3), pp.369-387.
Feo, R., Kitson, A. and Conroy, T., 2018. How fundamental aspects of nursing care are defined
in the literature: A scoping review. Journal of Clinical Nursing, 27(11-12), pp.2189-
2229.
Guglielmin, M. et. al., 2018. A scoping review of the implementation of health in all policies at
the local level. Health policy, 122(3), pp.284-292.
Kitson, A.L., 2018. The fundamentals of care framework as a point-of-care nursing
theory. Nursing Research, 67(2), pp.99-107.
Lillo-Crespo, M. and Sierras-Davó, M.C., 2019. Quality Improvement with Compassion:
Developing Healthcare Improvement Science in the European Health Professions’
Education. In Values of the University in a Time of Uncertainty (pp. 231-240). Springer,
Cham.
Lin, Y.K., Lin, M. and Chen, H., 2019. Do electronic health records affect quality of care?
Evidence from the HITECH Act. Information Systems Research, 30(1), pp.306-318.
Maroun, W., 2020. A conceptual model for understanding corporate social responsibility
assurance practice. Journal of Business Ethics, 161(1), pp.187-209.
Maynard, A. and Williams, A., 2018. Privatisation and the National Health Service.
In Privatisation and the welfare state (pp. 95-110). Routledge.
Paillé, P. and Halilem, N., 2019. Systematic review on environmental innovativeness: A
knowledge-based resource view. Journal of cleaner production, 211, pp.1088-1099.
Ratima, T., 2019. Retrospection of a Maori Tutor Educator's Bi-Cultural Teaching Discourse in
Te Wananga o Aotearoa (TWoA): A Narrative Portfolio. In Handbook of Research on
Indigenous Knowledge and Bi-Culturalism in a Global Context (pp. 136-148). IGI
Global.
Revell, L. and Elton-Chalcraft, S., 2021. Extremism, values, and education in policy and
practice. In Oxford Research Encyclopedia of Education.
Steele, L. et. al., 2020. Ending confinement and segregation: Barriers to realising human rights in
the everyday lives of people living with dementia in residential aged care. Australian
Journal of Human Rights, 26(2), pp.308-328.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Truong, M. et. al., 2021. Equity in clinical practice requires organisational and system-level
change–The role of nurse leaders. Collegian, 28(3), pp.346-350.
Van Melle, E and et. al., 2019. A core components framework for evaluating implementation of
competency-based medical education programs. Academic Medicine, 94(7), pp.1002-
1009.
Veugelers, W., 2021. How globalisation influences perspectives on citizenship education: from
the social and political to the cultural and moral. Compare: A Journal of Comparative
and International Education, 51(8), pp.1174-1189.
Weeks, K.W. and et. al., 2019. Developing and integrating nursing competence through
authentic technology-enhanced clinical simulation education: Pedagogies for
reconceptualising the theory-practice gap. Nurse education in practice, 37, pp.29-38.
Zachariadis, M., Hileman, G. and Scott, S.V., 2019. Governance and control in distributed
ledgers: Understanding the challenges facing blockchain technology in financial
services. Information and Organization, 29(2), pp.105-117.
Online:
Adapting Maslow’s Hierarchy of Needs to Nursing Communication, 2018 [Online]
Available through: <https://www.healthitanswers.net/adapting-maslows-hierarchy-needs-
nursing-communication/>
Principles of Health and Social Care Practice, 2021 [Online]
Available through: <https://ukdiss.com/examples/health-and-social-care-principles.php>
Workplace health and safety standards, 2013 [Online]
Available through: <https://www.nhsemployers.org/sites/default/files/2021-08/workplace-health-
safety-standards.pdf>
change–The role of nurse leaders. Collegian, 28(3), pp.346-350.
Van Melle, E and et. al., 2019. A core components framework for evaluating implementation of
competency-based medical education programs. Academic Medicine, 94(7), pp.1002-
1009.
Veugelers, W., 2021. How globalisation influences perspectives on citizenship education: from
the social and political to the cultural and moral. Compare: A Journal of Comparative
and International Education, 51(8), pp.1174-1189.
Weeks, K.W. and et. al., 2019. Developing and integrating nursing competence through
authentic technology-enhanced clinical simulation education: Pedagogies for
reconceptualising the theory-practice gap. Nurse education in practice, 37, pp.29-38.
Zachariadis, M., Hileman, G. and Scott, S.V., 2019. Governance and control in distributed
ledgers: Understanding the challenges facing blockchain technology in financial
services. Information and Organization, 29(2), pp.105-117.
Online:
Adapting Maslow’s Hierarchy of Needs to Nursing Communication, 2018 [Online]
Available through: <https://www.healthitanswers.net/adapting-maslows-hierarchy-needs-
nursing-communication/>
Principles of Health and Social Care Practice, 2021 [Online]
Available through: <https://ukdiss.com/examples/health-and-social-care-principles.php>
Workplace health and safety standards, 2013 [Online]
Available through: <https://www.nhsemployers.org/sites/default/files/2021-08/workplace-health-
safety-standards.pdf>
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




