University Assignment: Principles of Wound Management in Clinic
VerifiedAdded on 2022/11/19
|26
|6559
|300
Homework Assignment
AI Summary
This assignment comprehensively addresses the principles of wound management within a clinical environment. It covers various aspects, including the stages of wound healing (hemostasis, inflammation, proliferation, and maturation), factors influencing healing (stress, sleep, exudate), and the characteristics of wound tissues (necrotic, sloughy, granulating, and epithelizing). The assignment also details clinical manifestations of wound interventions, strategies for preventing infection, and measures to minimize cross-infection. Furthermore, it explores different types of wound drainage, the importance of wound cleaning, and the principles of wound care, including primary and secondary dressings. Periwound assessment, factors affecting psychosocial impact, wound management considerations (moist environment, pH balance), and the roles of healthcare team members are also discussed. The assignment concludes with instructions for family education, intrinsic factors affecting healing, types of dressings (hydrocolloid and hydrogel), documentation practices, and the classification and management of leg ulcers and pressure injuries.

Running Head: Principles of Wound Management in Clinic
Principles of Wound Management in Clinic
Name of the Student:
Name of the University:
Author Note:
Principles of Wound Management in Clinic
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Principles of Wound Management in Clinic
Table of Contents
Assessment I...............................................................................................................................2
Assessment Task 2- Scenario...................................................................................................12
References................................................................................................................................20
Table of Contents
Assessment I...............................................................................................................................2
Assessment Task 2- Scenario...................................................................................................12
References................................................................................................................................20
2Principles of Wound Management in Clinic
Assessment I
1. The confidentiality and privacy of the patient is maintained by developing a patient
privacy and confidentiality policy. It is ensured that this policy is extended to the
partner. This confidential policy should be in secured systems and the best IT
security policies should be implemented.
2. A. Epidermis
B. Papillary layer
C. Dermis
D. Reticular layer
E. Subcutaneous layer
F. Hair follicle
G. Hair shaft
H. Pore
I. Dermal papillae
J. Melanocytes
K. Hair follicle
L. Blood cell
M. Apocrine Sweat gland
N. Eccrine Sweat gland
O. Pacirial corpuscles
P. Adipose connective tissue
3. The wound healing process has four steps. They are- homeostasis phase,
inflammatory phase, proliferative phase and maturation phase.
Homeostatic phase deals with the closing of the wound by clotting. The platelets
stick to the wound site and takes up an amorphous shape. These activated platelets
Assessment I
1. The confidentiality and privacy of the patient is maintained by developing a patient
privacy and confidentiality policy. It is ensured that this policy is extended to the
partner. This confidential policy should be in secured systems and the best IT
security policies should be implemented.
2. A. Epidermis
B. Papillary layer
C. Dermis
D. Reticular layer
E. Subcutaneous layer
F. Hair follicle
G. Hair shaft
H. Pore
I. Dermal papillae
J. Melanocytes
K. Hair follicle
L. Blood cell
M. Apocrine Sweat gland
N. Eccrine Sweat gland
O. Pacirial corpuscles
P. Adipose connective tissue
3. The wound healing process has four steps. They are- homeostasis phase,
inflammatory phase, proliferative phase and maturation phase.
Homeostatic phase deals with the closing of the wound by clotting. The platelets
stick to the wound site and takes up an amorphous shape. These activated platelets
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Principles of Wound Management in Clinic
secrete chemicals that promote clotting which activates fibrin. Fibrin forms a mesh
like structure that enables the platelets to stick to each other and successfully form
a clot.
Inflammatory phase causes dead and damaged cells are removed from the system
by means of phagocytosis by white blood cells. The platelet derived growth factor
helps in growth and proliferation of cells.
Proliferative phase initiates the growth of new tissues. New blood vessels are
formed by vascular endothelial cells by the process of angiogenesis. Fibroblasts
secrete fibronectin and collagen and forms new extracellular matrix. This stage
ensures wound contraction as well.
Maturation phase realigning of the collagen occurs and cells which are not required
are removed by the process of apoptosis (Harper, Young and McNaught, 2014).
4. Moist environment has a positive impact on wound healing promising a faster
healing than wounds that normally dry out. Three advantages of healing wounds in
a moist environment is:
Ensures faster healing of the wound
Moist wound causes a hypoxic environment that prevents invading of
bacteria and maintains a proper pH ensuring angiogenesis.
Moist wound healing reduces pain and this reduces stress followed up by
lesser fatigue in the patient promoting faster healing and mobility of the
patient (Junker et al, 2013).
The key factors that affect wound healing includes-
Stress and negative mood that may cause social isolation
Sleep disturbances
The exudates from the wound and the pain (Upton & South, 2011).
secrete chemicals that promote clotting which activates fibrin. Fibrin forms a mesh
like structure that enables the platelets to stick to each other and successfully form
a clot.
Inflammatory phase causes dead and damaged cells are removed from the system
by means of phagocytosis by white blood cells. The platelet derived growth factor
helps in growth and proliferation of cells.
Proliferative phase initiates the growth of new tissues. New blood vessels are
formed by vascular endothelial cells by the process of angiogenesis. Fibroblasts
secrete fibronectin and collagen and forms new extracellular matrix. This stage
ensures wound contraction as well.
Maturation phase realigning of the collagen occurs and cells which are not required
are removed by the process of apoptosis (Harper, Young and McNaught, 2014).
4. Moist environment has a positive impact on wound healing promising a faster
healing than wounds that normally dry out. Three advantages of healing wounds in
a moist environment is:
Ensures faster healing of the wound
Moist wound causes a hypoxic environment that prevents invading of
bacteria and maintains a proper pH ensuring angiogenesis.
Moist wound healing reduces pain and this reduces stress followed up by
lesser fatigue in the patient promoting faster healing and mobility of the
patient (Junker et al, 2013).
The key factors that affect wound healing includes-
Stress and negative mood that may cause social isolation
Sleep disturbances
The exudates from the wound and the pain (Upton & South, 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Principles of Wound Management in Clinic
It has been evident in the research studies that living with wound has psychological
impact. Research studies has demonstrated that the patient with wound suffers from
anxiety and depression as result of continuous pain. In addition to this, they sometime
feel themselves as burden on their family members (Pereira, Figueiredo-Braga, &
Carvalho, 2016).
5. The characteristic wound tissues discussed are as follows:
Necrotic tissues indicate dead tissues in the wound area due to lack of
oxygen supply. It causes cells to be acidic which releases enzymes that
break the cell.
Sloughy tissue is categorised under necrotic tissue and it separates itself
from the site of the wound. Tissues become fibrous in nature.
Granulating tissue is new connective tissue growing at the wound surface.
This indicates a sign of healing.
Epithelizing tissue forms a barrier between the wound and the
environment. This tissue is formed during the re-epithelialization phase in
the process of the wound healing.
6. a) The clinical manifestations of wound interventions if wound infection is
Purulent drainage- This is a milky white discharge from the wound which
indicates infection.
Serous drainage- this is a thin watery discharge from the wound that
consists of blood cells, proteins and other cells that heat the body.
b) Three strategies to prevent wound infection includes:
The wound should be washed with antiseptic or at least soap immediately.
After applying ointment, it should be covered with bandages or gauze.
It has been evident in the research studies that living with wound has psychological
impact. Research studies has demonstrated that the patient with wound suffers from
anxiety and depression as result of continuous pain. In addition to this, they sometime
feel themselves as burden on their family members (Pereira, Figueiredo-Braga, &
Carvalho, 2016).
5. The characteristic wound tissues discussed are as follows:
Necrotic tissues indicate dead tissues in the wound area due to lack of
oxygen supply. It causes cells to be acidic which releases enzymes that
break the cell.
Sloughy tissue is categorised under necrotic tissue and it separates itself
from the site of the wound. Tissues become fibrous in nature.
Granulating tissue is new connective tissue growing at the wound surface.
This indicates a sign of healing.
Epithelizing tissue forms a barrier between the wound and the
environment. This tissue is formed during the re-epithelialization phase in
the process of the wound healing.
6. a) The clinical manifestations of wound interventions if wound infection is
Purulent drainage- This is a milky white discharge from the wound which
indicates infection.
Serous drainage- this is a thin watery discharge from the wound that
consists of blood cells, proteins and other cells that heat the body.
b) Three strategies to prevent wound infection includes:
The wound should be washed with antiseptic or at least soap immediately.
After applying ointment, it should be covered with bandages or gauze.
5Principles of Wound Management in Clinic
The dressings should be changed every day and the wound should be kept
dry.
c) Measures to minimise cross infection are:
Early diagnosis of infection prevents the spreading of it.
Healthy wound care practices: Sanitary wound bed preparation,
debridement and maintenance of moist environment and appropriate on
time dressings.
d) Educating patients to prevent infection of wound includes:
Daily dressing of the infected area and keeping the wound covered.
Pain management training should be done to avoid pain as it restricts the
flow of blood.
Non adhesive dressing tapes should be used and wound should be dry.
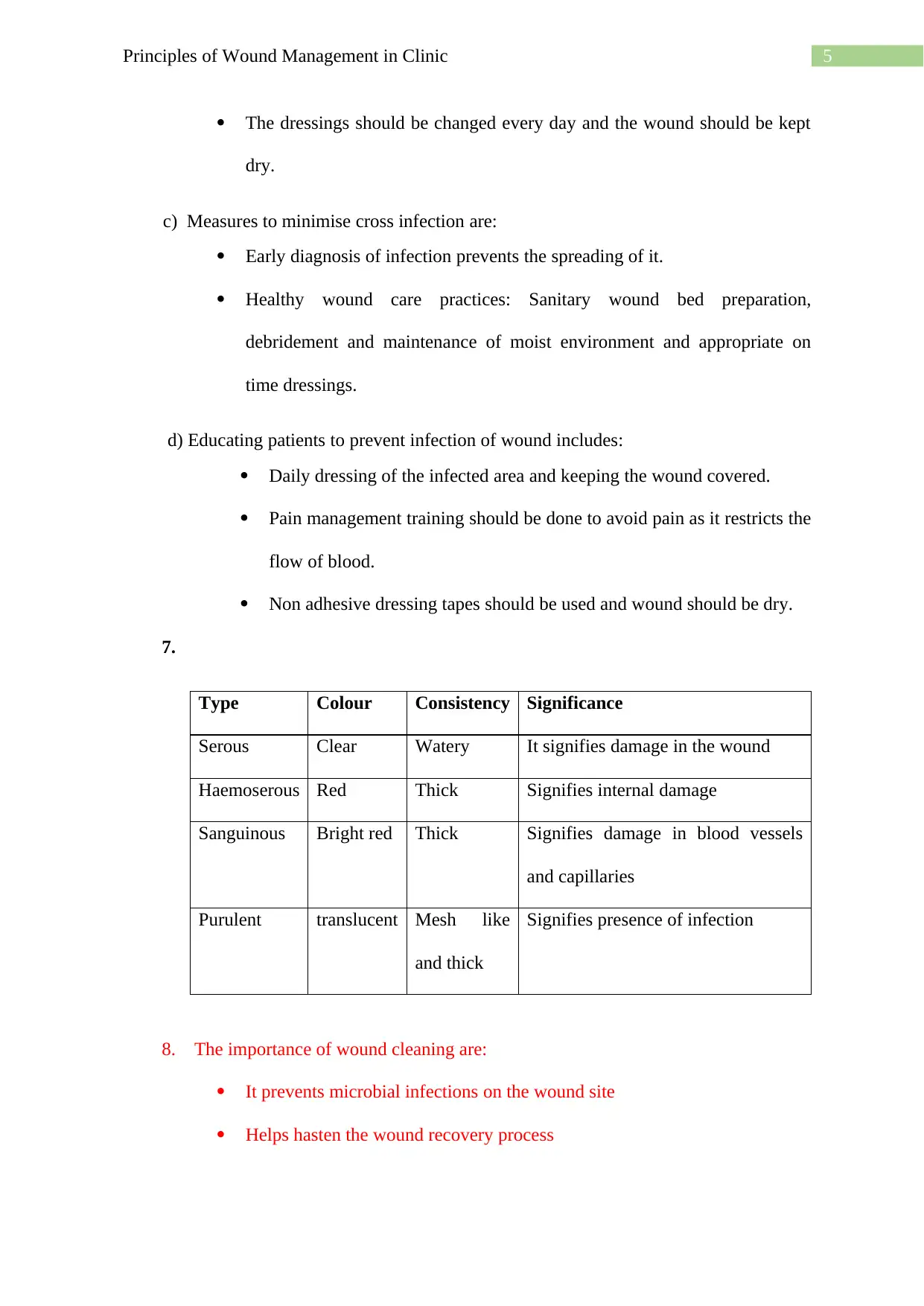
7.
Type Colour Consistency Significance
Serous Clear Watery It signifies damage in the wound
Haemoserous Red Thick Signifies internal damage
Sanguinous Bright red Thick Signifies damage in blood vessels
and capillaries
Purulent translucent Mesh like
and thick
Signifies presence of infection
8. The importance of wound cleaning are:
It prevents microbial infections on the wound site
Helps hasten the wound recovery process
The dressings should be changed every day and the wound should be kept
dry.
c) Measures to minimise cross infection are:
Early diagnosis of infection prevents the spreading of it.
Healthy wound care practices: Sanitary wound bed preparation,
debridement and maintenance of moist environment and appropriate on
time dressings.
d) Educating patients to prevent infection of wound includes:
Daily dressing of the infected area and keeping the wound covered.
Pain management training should be done to avoid pain as it restricts the
flow of blood.
Non adhesive dressing tapes should be used and wound should be dry.
7.
Type Colour Consistency Significance
Serous Clear Watery It signifies damage in the wound
Haemoserous Red Thick Signifies internal damage
Sanguinous Bright red Thick Signifies damage in blood vessels
and capillaries
Purulent translucent Mesh like
and thick
Signifies presence of infection
8. The importance of wound cleaning are:
It prevents microbial infections on the wound site
Helps hasten the wound recovery process
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Principles of Wound Management in Clinic
Prevents further deterioration such as spread and formation necrotic tissue
in wound site (Pegram & Bloomfield, 2010)
The wound care is fragile and has complications. The principle of wound care
involves preserve the function of the cells and tissues affect and to prevent
complications. Any deviations from the care can lead to non-healing of the chronic
wounds.
Primary dressing is the initial dressing of the wound which involves application of
ointment and covering of the wound with tape to prevent bleeding or oozing of any
liquid. It is in direct contact of the wound. The wound is non-adhering and acts as
an absorbent.
Secondary dressing covers the primary dressing of the wound. The main purpose
of secondary dressing is to keep primary dressing in place. It includes gauze and
tapes. They do not directly come in contact with the wound but covers the wound
fully (Dhivya, Padma & Santhini, 2015).
9. Periwound are good indicators for identifying the wound type, moisture imbalance,
intruding infections and for managing the plan of care.
Periwound assessment involves:
Abscess- A painful compressible tender mass of tissues which is warm to touch.
This occurs due to collection of fluid within the tissue. This mainly occurs due to
acute or chronic localized infection.
Hyperkeratosis- inflammation due to the wound may trigger excessive keratin
secretion. As a result, the person’s skin becomes thicker than usual. This causes
callous-like tissue formation at the edges of the wound.
10. Wound pain can occur due to various issues like skin damage, blood vessel injury
or nerve damage and ischaemia. Ischaemia is a syndrome that prevents the supply
Prevents further deterioration such as spread and formation necrotic tissue
in wound site (Pegram & Bloomfield, 2010)
The wound care is fragile and has complications. The principle of wound care
involves preserve the function of the cells and tissues affect and to prevent
complications. Any deviations from the care can lead to non-healing of the chronic
wounds.
Primary dressing is the initial dressing of the wound which involves application of
ointment and covering of the wound with tape to prevent bleeding or oozing of any
liquid. It is in direct contact of the wound. The wound is non-adhering and acts as
an absorbent.
Secondary dressing covers the primary dressing of the wound. The main purpose
of secondary dressing is to keep primary dressing in place. It includes gauze and
tapes. They do not directly come in contact with the wound but covers the wound
fully (Dhivya, Padma & Santhini, 2015).
9. Periwound are good indicators for identifying the wound type, moisture imbalance,
intruding infections and for managing the plan of care.
Periwound assessment involves:
Abscess- A painful compressible tender mass of tissues which is warm to touch.
This occurs due to collection of fluid within the tissue. This mainly occurs due to
acute or chronic localized infection.
Hyperkeratosis- inflammation due to the wound may trigger excessive keratin
secretion. As a result, the person’s skin becomes thicker than usual. This causes
callous-like tissue formation at the edges of the wound.
10. Wound pain can occur due to various issues like skin damage, blood vessel injury
or nerve damage and ischaemia. Ischaemia is a syndrome that prevents the supply
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Principles of Wound Management in Clinic
of blood to tissues resulting in lack of oxygen to carry out cellular metabolism.
These situations create a condition of hypoxia and delays wound healing subjecting
the wound to infections.
11. One of the clinical feature that impact the psychosocial life of the patient suffering
from chronic wound is anxiety. An individual with chronic wound suffers from
loss of low self- esteem, pain and social isolation. All of these negative emotions
impacts the individual emotionally and hampers the mental state of the individual.
This impacts the quality of life of the individual. Anxiety prevents the individuals
from participating wholly in their social and daily life activities leading to social
isolation and depression. These cumulative approach causes anxiety in the patient
due to chronic wound that impacts the psychosocial life of the patient.(Platsidaki,
Kouris, & Christodoulou, 2017).
12. Factors to be considered for wound management are-
Maintaining moist environment for fast healing- The moisture content helps
in healing the wound three to four times faster than the normal conditions.
Maintaining stable wound temperature. Prevent wound exposure or
avoiding cold solutions.
Maintain an acidic or neutral pH to prevent wound infections. This is
because the pH plays an important role in cellular processes. It also
prevents formation of biofilms that affect the process of wound healing.
Allow flow of drainage if there is extensive drainage flow. This is because
exudates play a major role in allowing migration of the cells across the
wound bed. This ensures distribution of growth and immune factors that
play a crucial role in healing.
of blood to tissues resulting in lack of oxygen to carry out cellular metabolism.
These situations create a condition of hypoxia and delays wound healing subjecting
the wound to infections.
11. One of the clinical feature that impact the psychosocial life of the patient suffering
from chronic wound is anxiety. An individual with chronic wound suffers from
loss of low self- esteem, pain and social isolation. All of these negative emotions
impacts the individual emotionally and hampers the mental state of the individual.
This impacts the quality of life of the individual. Anxiety prevents the individuals
from participating wholly in their social and daily life activities leading to social
isolation and depression. These cumulative approach causes anxiety in the patient
due to chronic wound that impacts the psychosocial life of the patient.(Platsidaki,
Kouris, & Christodoulou, 2017).
12. Factors to be considered for wound management are-
Maintaining moist environment for fast healing- The moisture content helps
in healing the wound three to four times faster than the normal conditions.
Maintaining stable wound temperature. Prevent wound exposure or
avoiding cold solutions.
Maintain an acidic or neutral pH to prevent wound infections. This is
because the pH plays an important role in cellular processes. It also
prevents formation of biofilms that affect the process of wound healing.
Allow flow of drainage if there is extensive drainage flow. This is because
exudates play a major role in allowing migration of the cells across the
wound bed. This ensures distribution of growth and immune factors that
play a crucial role in healing.
8Principles of Wound Management in Clinic
13. The five members of a health care plan for wound management involves:
Physician
Nurse
Radiologist
Psychiatrist
Physiotherapist
14. The instructions to be provided to the family to prevent wound damage is given
below:
The family should be educated on prevention of wound drying. Ensuring
presence of moist environment as it promotes faster healing of the wounds.
Moist environment ensures better and faster healing of the wound.
Maintenance of moist environment ensures new cell and tissue formation.
It enhances the skin renewal power.
To maintain a pH balance to prevent infections in the wound ensuring the
wound is dry and the dressing are done at regular intervals. The formation
of biofilms is essentially prevented by maintaining low pH and improves
the cellular processes.
15. Intrinsic factors that affect wound healing-
Age
Nutrition
Obesity
Repeated trauma
16. The two types of dressing are:
13. The five members of a health care plan for wound management involves:
Physician
Nurse
Radiologist
Psychiatrist
Physiotherapist
14. The instructions to be provided to the family to prevent wound damage is given
below:
The family should be educated on prevention of wound drying. Ensuring
presence of moist environment as it promotes faster healing of the wounds.
Moist environment ensures better and faster healing of the wound.
Maintenance of moist environment ensures new cell and tissue formation.
It enhances the skin renewal power.
To maintain a pH balance to prevent infections in the wound ensuring the
wound is dry and the dressing are done at regular intervals. The formation
of biofilms is essentially prevented by maintaining low pH and improves
the cellular processes.
15. Intrinsic factors that affect wound healing-
Age
Nutrition
Obesity
Repeated trauma
16. The two types of dressing are:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Principles of Wound Management in Clinic
Hydrocolloid dressing- This type of dressing is usually done on burns. It
involves too much of oozing out of liquid and necrotic wounds. These are
non-adhesive in nature and non-breathable. It is self-adhesive, easy to apply
and biodegradable. It prevents the bacterial infections as it is impermeable
to bacteria. Example include Duoderm, Medihoney.
Hydrogel dressing- This type of dressing is used for wounds with less
drainage and necrotic wounds. This type of dressing maximizes patient
comfort and reduces pain. The cooling effect of the gel promotes pain
reduction. Example include Aquaform, Intrasite.
17. Five observations that a nurse should document about a patient having a wound
with staples in situ:
The patient’s medical history
Details of the wound and extent of cut should be examined
The sterility of the environment should be checked
Check the wound for any redness, drainage or accumulation of dead
tissues
Remove any dead cells from the surface of the wound and ensure moist
environment for fast healing.
18. Wound drainage can be normal as well as abnormal. Normal drainage from wound
is watery, odourless and having a clear consistency. Minimal amount of blood loss
may be observed. It shows less redness and swelling indicating a sign of healing.
Serous and serosanguinous drainage can be considered as examples of normal
wound drain.
Purulent drainage is not a characteristic of normal healthy wound healing. The
exudates can be thick, milky that may turn yellowish, tan, grey ensuring the
Hydrocolloid dressing- This type of dressing is usually done on burns. It
involves too much of oozing out of liquid and necrotic wounds. These are
non-adhesive in nature and non-breathable. It is self-adhesive, easy to apply
and biodegradable. It prevents the bacterial infections as it is impermeable
to bacteria. Example include Duoderm, Medihoney.
Hydrogel dressing- This type of dressing is used for wounds with less
drainage and necrotic wounds. This type of dressing maximizes patient
comfort and reduces pain. The cooling effect of the gel promotes pain
reduction. Example include Aquaform, Intrasite.
17. Five observations that a nurse should document about a patient having a wound
with staples in situ:
The patient’s medical history
Details of the wound and extent of cut should be examined
The sterility of the environment should be checked
Check the wound for any redness, drainage or accumulation of dead
tissues
Remove any dead cells from the surface of the wound and ensure moist
environment for fast healing.
18. Wound drainage can be normal as well as abnormal. Normal drainage from wound
is watery, odourless and having a clear consistency. Minimal amount of blood loss
may be observed. It shows less redness and swelling indicating a sign of healing.
Serous and serosanguinous drainage can be considered as examples of normal
wound drain.
Purulent drainage is not a characteristic of normal healthy wound healing. The
exudates can be thick, milky that may turn yellowish, tan, grey ensuring the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10Principles of Wound Management in Clinic
presence of infection in the wound site. Abnormal wound drainage shows
excessive oozing of blood. The area is soft and tender indicating pain in the area.
The consistency is also thicker and may sometimes have bad odour. The examples
are haemorrhage and sanguinous drain.
19. The cost related factors of wound management include nursing staff for monitoring
and dressing the wound. In case of delayed healing surgical intervention and
hospitalisation may impact the expenses. Prevention, monitoring and interventions
in the wound are important cost related treatments. Psychiatrist may also help the
patient to deal with the stress factor and enable faster healing.
20. Leg ulcers can be categorised into three types. They are venous ulcers, ischemic
ulcer and neurotrophic ulcer.
Venous ulcers occur due to damage in the underlying veins of the foot. It can be
treated by keeping the legs at elevated heights and by compression therapy.
Neurotrophic ulcer occurs when an individual has sensation impairment in their
foot due to nerve disorders (Sacchetti & Lambiase, 2014). It attacks the pressure
points of the foot and are difficult to heal. It requires wound debridement to ensure
successful healing.
Ischemic ulcer is seen in patients who have cardiovascular disease and the arteries
are affected. These ulcers are painful but bleeding of the ulcers is not frequent
(Yotsu et al, 2014).
21. Pressure injuries occur on the skin or tissue over a bone due to shear pressure. The
stages involve
Stage I- Non-blanchable erythema which indicates redness of the region
which might be warmer than the surrounding, tender and painful to touch.
presence of infection in the wound site. Abnormal wound drainage shows
excessive oozing of blood. The area is soft and tender indicating pain in the area.
The consistency is also thicker and may sometimes have bad odour. The examples
are haemorrhage and sanguinous drain.
19. The cost related factors of wound management include nursing staff for monitoring
and dressing the wound. In case of delayed healing surgical intervention and
hospitalisation may impact the expenses. Prevention, monitoring and interventions
in the wound are important cost related treatments. Psychiatrist may also help the
patient to deal with the stress factor and enable faster healing.
20. Leg ulcers can be categorised into three types. They are venous ulcers, ischemic
ulcer and neurotrophic ulcer.
Venous ulcers occur due to damage in the underlying veins of the foot. It can be
treated by keeping the legs at elevated heights and by compression therapy.
Neurotrophic ulcer occurs when an individual has sensation impairment in their
foot due to nerve disorders (Sacchetti & Lambiase, 2014). It attacks the pressure
points of the foot and are difficult to heal. It requires wound debridement to ensure
successful healing.
Ischemic ulcer is seen in patients who have cardiovascular disease and the arteries
are affected. These ulcers are painful but bleeding of the ulcers is not frequent
(Yotsu et al, 2014).
21. Pressure injuries occur on the skin or tissue over a bone due to shear pressure. The
stages involve
Stage I- Non-blanchable erythema which indicates redness of the region
which might be warmer than the surrounding, tender and painful to touch.
11Principles of Wound Management in Clinic
Stage II- Partial thickness skin loss has no bruising indicating a primary
shallow open ulcer which is dry. Change in consistency of the tissue,
tenderness, heat and pain observed (Stankiewicz et al., 2016).
Stage III- Full thickness skin loss suffers loss of subcutaneous fat but
tendons and bones are not exposed. Slough is also observed.
Stage IV- Full thickness tissue loss exhibits exposure of tendons, bones,
ligaments due to loss of subcutaneous fat. Slough with tunnelling may also
be observed.
Stage V- Depth unknown and deep tissue injury involves purple or maroon
localized area. This discoloration occurs due to damage of the tissues in
that area (Skórkowska et al., 2013).
22. The major causes of pressure injuries involve-
Pressure- A prolonged pressure on a particular part of the body reduce the
flow of blood to that region. Blood flow is very important for the cells to
receive the required oxygen and nutrients. Cells depleted of nutrients can
get damaged and eventually die which leads to the development of pressure
injury.
Friction- When there is rubbing skin rubbing observed against bed sheets or
any clothing it leads to friction. This action makes the skin in contact with
clothing or bed sheets fragile and it becomes vulnerable for pressure injury.
Shear- When two surfaces move in direction opposite to each other it
results in shear. When shear occurs, the skin over the bone in our body
might stay in same place which is essentially pulls the skin in opposite
direction. If this process occurs continuously, then this two opposite
direction force develops into pressure injury.
Stage II- Partial thickness skin loss has no bruising indicating a primary
shallow open ulcer which is dry. Change in consistency of the tissue,
tenderness, heat and pain observed (Stankiewicz et al., 2016).
Stage III- Full thickness skin loss suffers loss of subcutaneous fat but
tendons and bones are not exposed. Slough is also observed.
Stage IV- Full thickness tissue loss exhibits exposure of tendons, bones,
ligaments due to loss of subcutaneous fat. Slough with tunnelling may also
be observed.
Stage V- Depth unknown and deep tissue injury involves purple or maroon
localized area. This discoloration occurs due to damage of the tissues in
that area (Skórkowska et al., 2013).
22. The major causes of pressure injuries involve-
Pressure- A prolonged pressure on a particular part of the body reduce the
flow of blood to that region. Blood flow is very important for the cells to
receive the required oxygen and nutrients. Cells depleted of nutrients can
get damaged and eventually die which leads to the development of pressure
injury.
Friction- When there is rubbing skin rubbing observed against bed sheets or
any clothing it leads to friction. This action makes the skin in contact with
clothing or bed sheets fragile and it becomes vulnerable for pressure injury.
Shear- When two surfaces move in direction opposite to each other it
results in shear. When shear occurs, the skin over the bone in our body
might stay in same place which is essentially pulls the skin in opposite
direction. If this process occurs continuously, then this two opposite
direction force develops into pressure injury.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




