400871 Professional Health Competencies: Osteoarthritis Case Study
VerifiedAdded on 2023/03/29
|8
|1598
|144
Case Study
AI Summary
This case study, completed for the Professional Health Competencies course, focuses on a 50-year-old female, Helen, diagnosed with generalized osteoarthritis stemming from a childhood injury and subsequent failed hip replacement. The study utilizes the ICF framework to detail Helen's impairments, activity limitations, and the impact of environmental factors, including the loss of her job and a divorce that led to depression and eating disorders. The assignment outlines interventions by a healthcare nurse and a mental health counselor, including pain assessment, exercise therapies, and strategies to manage depression, eating, and sleep disorders. It emphasizes effective communication, education, and ethical considerations. Additionally, the case study highlights person-centered strategies such as creating a safe environment and encouraging family engagement to improve patient outcomes. The document includes references to support the interventions and strategies discussed.

400871
PROFESSIONAL HEALTH COMPETENCIES
400871
OSTEOARTHRITIS CASE STUDY
1
PROFESSIONAL HEALTH COMPETENCIES
400871
OSTEOARTHRITIS CASE STUDY
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
400871
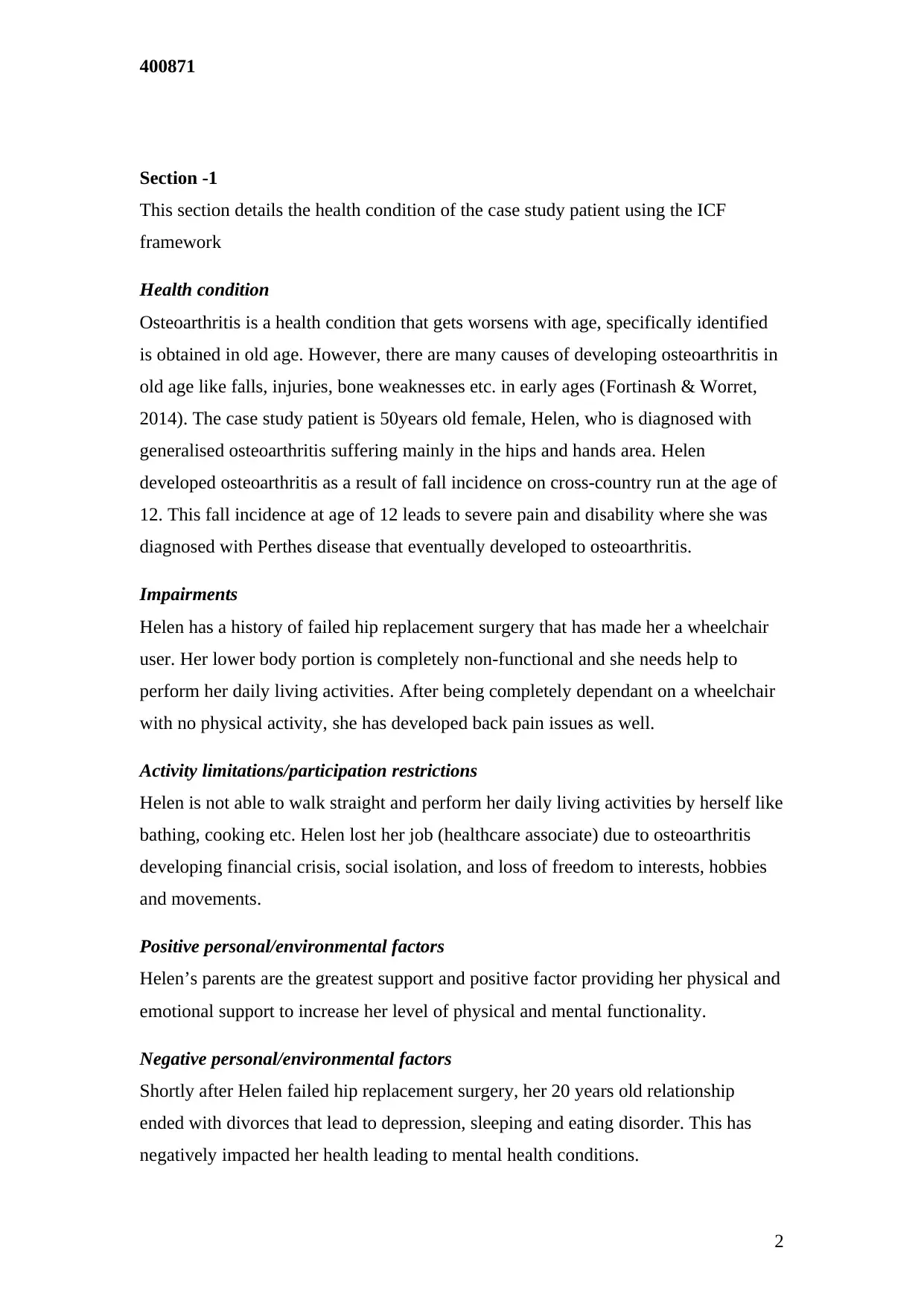
Section -1
This section details the health condition of the case study patient using the ICF
framework
Health condition
Osteoarthritis is a health condition that gets worsens with age, specifically identified
is obtained in old age. However, there are many causes of developing osteoarthritis in
old age like falls, injuries, bone weaknesses etc. in early ages (Fortinash & Worret,
2014). The case study patient is 50years old female, Helen, who is diagnosed with
generalised osteoarthritis suffering mainly in the hips and hands area. Helen
developed osteoarthritis as a result of fall incidence on cross-country run at the age of
12. This fall incidence at age of 12 leads to severe pain and disability where she was
diagnosed with Perthes disease that eventually developed to osteoarthritis.
Impairments
Helen has a history of failed hip replacement surgery that has made her a wheelchair
user. Her lower body portion is completely non-functional and she needs help to
perform her daily living activities. After being completely dependant on a wheelchair
with no physical activity, she has developed back pain issues as well.
Activity limitations/participation restrictions
Helen is not able to walk straight and perform her daily living activities by herself like
bathing, cooking etc. Helen lost her job (healthcare associate) due to osteoarthritis
developing financial crisis, social isolation, and loss of freedom to interests, hobbies
and movements.
Positive personal/environmental factors
Helen’s parents are the greatest support and positive factor providing her physical and
emotional support to increase her level of physical and mental functionality.
Negative personal/environmental factors
Shortly after Helen failed hip replacement surgery, her 20 years old relationship
ended with divorces that lead to depression, sleeping and eating disorder. This has
negatively impacted her health leading to mental health conditions.
2
Section -1
This section details the health condition of the case study patient using the ICF
framework
Health condition
Osteoarthritis is a health condition that gets worsens with age, specifically identified
is obtained in old age. However, there are many causes of developing osteoarthritis in
old age like falls, injuries, bone weaknesses etc. in early ages (Fortinash & Worret,
2014). The case study patient is 50years old female, Helen, who is diagnosed with
generalised osteoarthritis suffering mainly in the hips and hands area. Helen
developed osteoarthritis as a result of fall incidence on cross-country run at the age of
12. This fall incidence at age of 12 leads to severe pain and disability where she was
diagnosed with Perthes disease that eventually developed to osteoarthritis.
Impairments
Helen has a history of failed hip replacement surgery that has made her a wheelchair
user. Her lower body portion is completely non-functional and she needs help to
perform her daily living activities. After being completely dependant on a wheelchair
with no physical activity, she has developed back pain issues as well.
Activity limitations/participation restrictions
Helen is not able to walk straight and perform her daily living activities by herself like
bathing, cooking etc. Helen lost her job (healthcare associate) due to osteoarthritis
developing financial crisis, social isolation, and loss of freedom to interests, hobbies
and movements.
Positive personal/environmental factors
Helen’s parents are the greatest support and positive factor providing her physical and
emotional support to increase her level of physical and mental functionality.
Negative personal/environmental factors
Shortly after Helen failed hip replacement surgery, her 20 years old relationship
ended with divorces that lead to depression, sleeping and eating disorder. This has
negatively impacted her health leading to mental health conditions.
2
400871
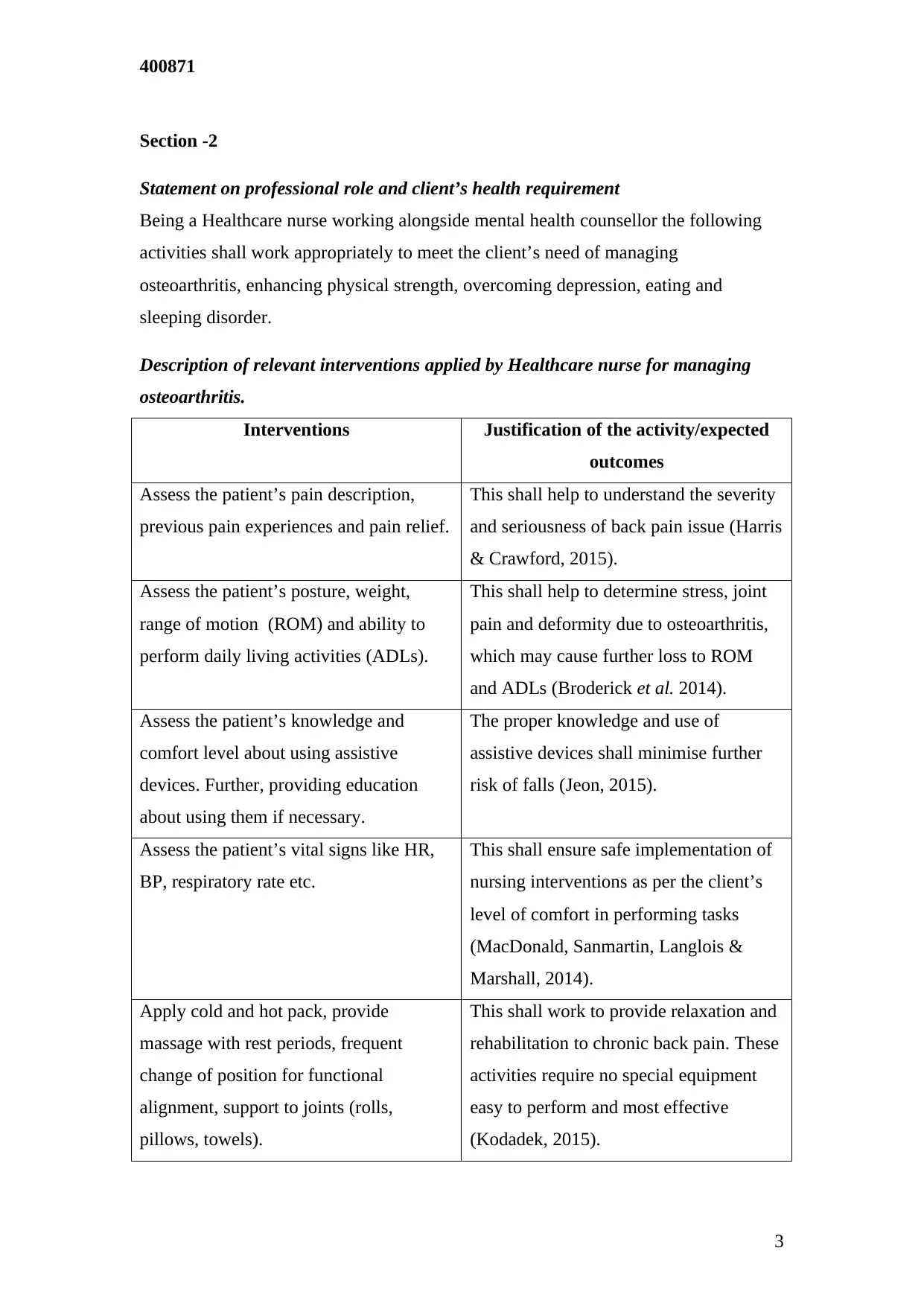
Section -2
Statement on professional role and client’s health requirement
Being a Healthcare nurse working alongside mental health counsellor the following
activities shall work appropriately to meet the client’s need of managing
osteoarthritis, enhancing physical strength, overcoming depression, eating and
sleeping disorder.
Description of relevant interventions applied by Healthcare nurse for managing
osteoarthritis.
Interventions Justification of the activity/expected
outcomes
Assess the patient’s pain description,
previous pain experiences and pain relief.
This shall help to understand the severity
and seriousness of back pain issue (Harris
& Crawford, 2015).
Assess the patient’s posture, weight,
range of motion (ROM) and ability to
perform daily living activities (ADLs).
This shall help to determine stress, joint
pain and deformity due to osteoarthritis,
which may cause further loss to ROM
and ADLs (Broderick et al. 2014).
Assess the patient’s knowledge and
comfort level about using assistive
devices. Further, providing education
about using them if necessary.
The proper knowledge and use of
assistive devices shall minimise further
risk of falls (Jeon, 2015).
Assess the patient’s vital signs like HR,
BP, respiratory rate etc.
This shall ensure safe implementation of
nursing interventions as per the client’s
level of comfort in performing tasks
(MacDonald, Sanmartin, Langlois &
Marshall, 2014).
Apply cold and hot pack, provide
massage with rest periods, frequent
change of position for functional
alignment, support to joints (rolls,
pillows, towels).
This shall work to provide relaxation and
rehabilitation to chronic back pain. These
activities require no special equipment
easy to perform and most effective
(Kodadek, 2015).
3
Section -2
Statement on professional role and client’s health requirement
Being a Healthcare nurse working alongside mental health counsellor the following
activities shall work appropriately to meet the client’s need of managing
osteoarthritis, enhancing physical strength, overcoming depression, eating and
sleeping disorder.
Description of relevant interventions applied by Healthcare nurse for managing
osteoarthritis.
Interventions Justification of the activity/expected
outcomes
Assess the patient’s pain description,
previous pain experiences and pain relief.
This shall help to understand the severity
and seriousness of back pain issue (Harris
& Crawford, 2015).
Assess the patient’s posture, weight,
range of motion (ROM) and ability to
perform daily living activities (ADLs).
This shall help to determine stress, joint
pain and deformity due to osteoarthritis,
which may cause further loss to ROM
and ADLs (Broderick et al. 2014).
Assess the patient’s knowledge and
comfort level about using assistive
devices. Further, providing education
about using them if necessary.
The proper knowledge and use of
assistive devices shall minimise further
risk of falls (Jeon, 2015).
Assess the patient’s vital signs like HR,
BP, respiratory rate etc.
This shall ensure safe implementation of
nursing interventions as per the client’s
level of comfort in performing tasks
(MacDonald, Sanmartin, Langlois &
Marshall, 2014).
Apply cold and hot pack, provide
massage with rest periods, frequent
change of position for functional
alignment, support to joints (rolls,
pillows, towels).
This shall work to provide relaxation and
rehabilitation to chronic back pain. These
activities require no special equipment
easy to perform and most effective
(Kodadek, 2015).
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
400871
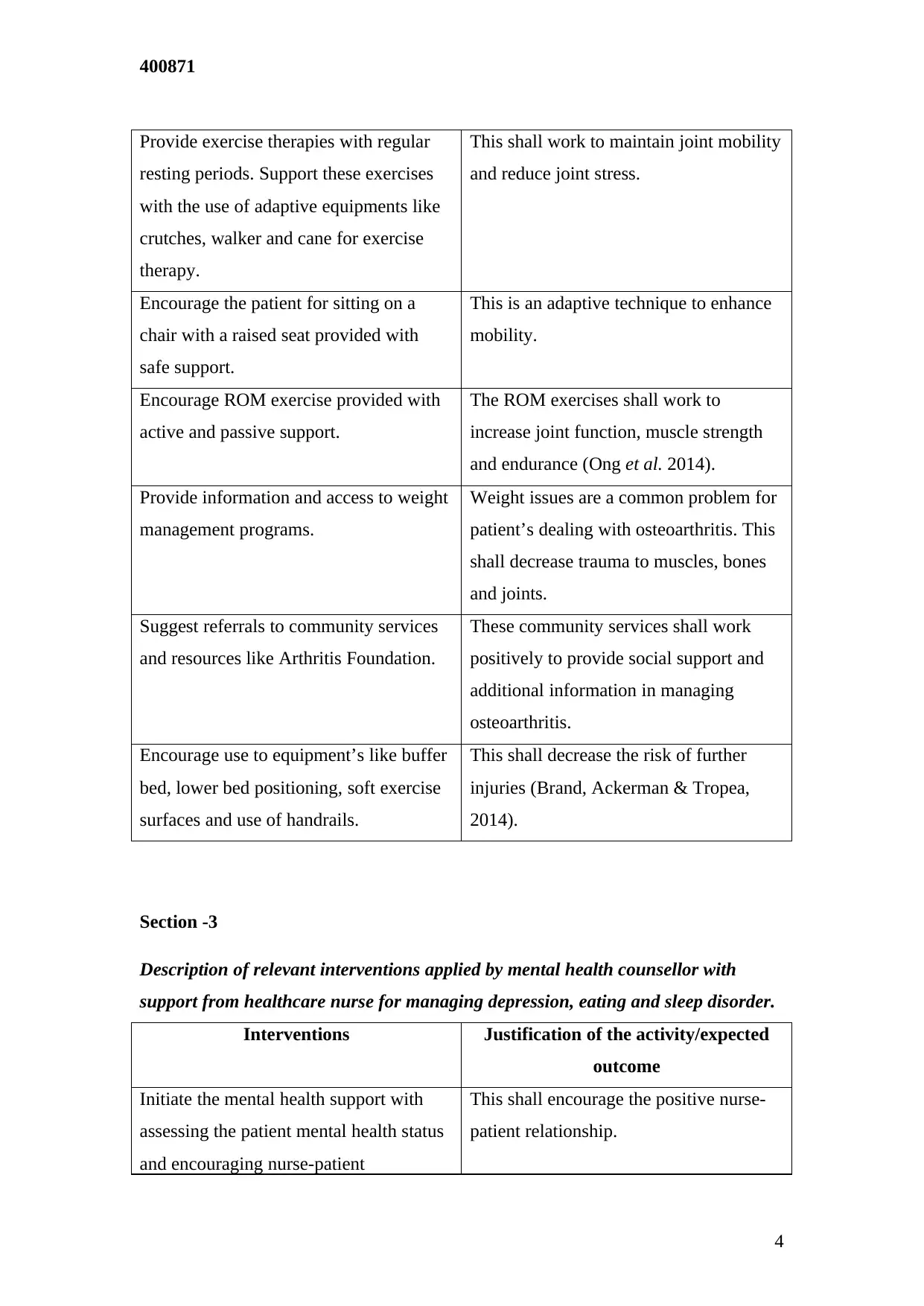
Provide exercise therapies with regular
resting periods. Support these exercises
with the use of adaptive equipments like
crutches, walker and cane for exercise
therapy.
This shall work to maintain joint mobility
and reduce joint stress.
Encourage the patient for sitting on a
chair with a raised seat provided with
safe support.
This is an adaptive technique to enhance
mobility.
Encourage ROM exercise provided with
active and passive support.
The ROM exercises shall work to
increase joint function, muscle strength
and endurance (Ong et al. 2014).
Provide information and access to weight
management programs.
Weight issues are a common problem for
patient’s dealing with osteoarthritis. This
shall decrease trauma to muscles, bones
and joints.
Suggest referrals to community services
and resources like Arthritis Foundation.
These community services shall work
positively to provide social support and
additional information in managing
osteoarthritis.
Encourage use to equipment’s like buffer
bed, lower bed positioning, soft exercise
surfaces and use of handrails.
This shall decrease the risk of further
injuries (Brand, Ackerman & Tropea,
2014).
Section -3
Description of relevant interventions applied by mental health counsellor with
support from healthcare nurse for managing depression, eating and sleep disorder.
Interventions Justification of the activity/expected
outcome
Initiate the mental health support with
assessing the patient mental health status
and encouraging nurse-patient
This shall encourage the positive nurse-
patient relationship.
4
Provide exercise therapies with regular
resting periods. Support these exercises
with the use of adaptive equipments like
crutches, walker and cane for exercise
therapy.
This shall work to maintain joint mobility
and reduce joint stress.
Encourage the patient for sitting on a
chair with a raised seat provided with
safe support.
This is an adaptive technique to enhance
mobility.
Encourage ROM exercise provided with
active and passive support.
The ROM exercises shall work to
increase joint function, muscle strength
and endurance (Ong et al. 2014).
Provide information and access to weight
management programs.
Weight issues are a common problem for
patient’s dealing with osteoarthritis. This
shall decrease trauma to muscles, bones
and joints.
Suggest referrals to community services
and resources like Arthritis Foundation.
These community services shall work
positively to provide social support and
additional information in managing
osteoarthritis.
Encourage use to equipment’s like buffer
bed, lower bed positioning, soft exercise
surfaces and use of handrails.
This shall decrease the risk of further
injuries (Brand, Ackerman & Tropea,
2014).
Section -3
Description of relevant interventions applied by mental health counsellor with
support from healthcare nurse for managing depression, eating and sleep disorder.
Interventions Justification of the activity/expected
outcome
Initiate the mental health support with
assessing the patient mental health status
and encouraging nurse-patient
This shall encourage the positive nurse-
patient relationship.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
400871
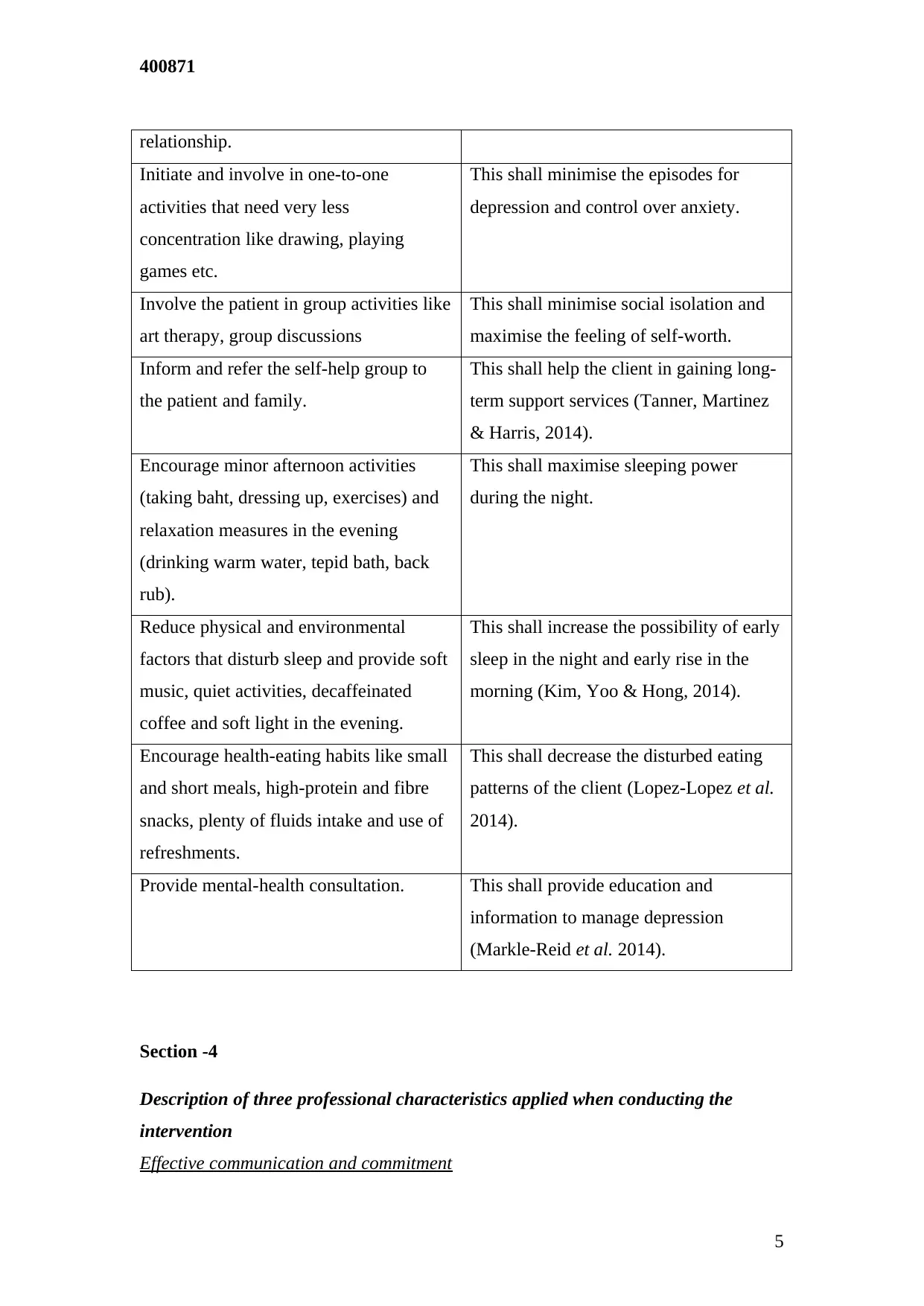
relationship.
Initiate and involve in one-to-one
activities that need very less
concentration like drawing, playing
games etc.
This shall minimise the episodes for
depression and control over anxiety.
Involve the patient in group activities like
art therapy, group discussions
This shall minimise social isolation and
maximise the feeling of self-worth.
Inform and refer the self-help group to
the patient and family.
This shall help the client in gaining long-
term support services (Tanner, Martinez
& Harris, 2014).
Encourage minor afternoon activities
(taking baht, dressing up, exercises) and
relaxation measures in the evening
(drinking warm water, tepid bath, back
rub).
This shall maximise sleeping power
during the night.
Reduce physical and environmental
factors that disturb sleep and provide soft
music, quiet activities, decaffeinated
coffee and soft light in the evening.
This shall increase the possibility of early
sleep in the night and early rise in the
morning (Kim, Yoo & Hong, 2014).
Encourage health-eating habits like small
and short meals, high-protein and fibre
snacks, plenty of fluids intake and use of
refreshments.
This shall decrease the disturbed eating
patterns of the client (Lopez-Lopez et al.
2014).
Provide mental-health consultation. This shall provide education and
information to manage depression
(Markle-Reid et al. 2014).
Section -4
Description of three professional characteristics applied when conducting the
intervention
Effective communication and commitment
5
relationship.
Initiate and involve in one-to-one
activities that need very less
concentration like drawing, playing
games etc.
This shall minimise the episodes for
depression and control over anxiety.
Involve the patient in group activities like
art therapy, group discussions
This shall minimise social isolation and
maximise the feeling of self-worth.
Inform and refer the self-help group to
the patient and family.
This shall help the client in gaining long-
term support services (Tanner, Martinez
& Harris, 2014).
Encourage minor afternoon activities
(taking baht, dressing up, exercises) and
relaxation measures in the evening
(drinking warm water, tepid bath, back
rub).
This shall maximise sleeping power
during the night.
Reduce physical and environmental
factors that disturb sleep and provide soft
music, quiet activities, decaffeinated
coffee and soft light in the evening.
This shall increase the possibility of early
sleep in the night and early rise in the
morning (Kim, Yoo & Hong, 2014).
Encourage health-eating habits like small
and short meals, high-protein and fibre
snacks, plenty of fluids intake and use of
refreshments.
This shall decrease the disturbed eating
patterns of the client (Lopez-Lopez et al.
2014).
Provide mental-health consultation. This shall provide education and
information to manage depression
(Markle-Reid et al. 2014).
Section -4
Description of three professional characteristics applied when conducting the
intervention
Effective communication and commitment
5
400871
An effective communication and commitment approach shall be applied in this case
because Helen is dealing with both physical and mental health issues, an effective
nurse-patient relation shall help in the recovery process (Fortinash & Worret, 2014).
Long-term and regular education
As osteoarthritis is a long-term condition that has no quick treatment, the long-term
and regular education from care nurse shall ensure proper and effective treatment with
these interventions (Kim, Yoo & Hong, 2014).
Ethical foundation
A proper ethical foundation shall be established while performing interventions.
Firstly, informed consent shall be obtained from the patient before implementing the
treatment process followed by providing patient with non-maleficence, respect to
autonomy and beneficence in nursing services (Fortinash & Worret, 2014).
Section - 5
Description and justification of two person-centred strategies applicable in this case
Creating a safe patient care environment
As a case study patient, Helen is a sufferer of osteoarthritis a safe care environment is
a must requirement to ensure minimum risk of further injury or fall. Any further
injury or fall can make this case more complicated, therefore, providing a safe care
environment is a must person-centred care strategy in this case.
Encouraging caregiver and family engagement
According to Kodadek (2015) studies, any extra eye or ear can help a lot in patient
care services. The family and care provider engaged together in care process add a
double commitment to patient safety. As Helen is suffering osteoarthritis and she
holds positive support from her parents, this means involving her parents in care
intervention process shall ensure enhanced patient safety.
6
An effective communication and commitment approach shall be applied in this case
because Helen is dealing with both physical and mental health issues, an effective
nurse-patient relation shall help in the recovery process (Fortinash & Worret, 2014).
Long-term and regular education
As osteoarthritis is a long-term condition that has no quick treatment, the long-term
and regular education from care nurse shall ensure proper and effective treatment with
these interventions (Kim, Yoo & Hong, 2014).
Ethical foundation
A proper ethical foundation shall be established while performing interventions.
Firstly, informed consent shall be obtained from the patient before implementing the
treatment process followed by providing patient with non-maleficence, respect to
autonomy and beneficence in nursing services (Fortinash & Worret, 2014).
Section - 5
Description and justification of two person-centred strategies applicable in this case
Creating a safe patient care environment
As a case study patient, Helen is a sufferer of osteoarthritis a safe care environment is
a must requirement to ensure minimum risk of further injury or fall. Any further
injury or fall can make this case more complicated, therefore, providing a safe care
environment is a must person-centred care strategy in this case.
Encouraging caregiver and family engagement
According to Kodadek (2015) studies, any extra eye or ear can help a lot in patient
care services. The family and care provider engaged together in care process add a
double commitment to patient safety. As Helen is suffering osteoarthritis and she
holds positive support from her parents, this means involving her parents in care
intervention process shall ensure enhanced patient safety.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
400871
References
References
Books
MacDonald, K. V., Sanmartin, C., Langlois, K., & Marshall, D. A. (2014). Symptom
onset, diagnosis and management of osteoarthritis. Canada :Statistics Canada.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-
Book. Australia: Elsevier Health Sciences.
Journals
Brand, C. A., Ackerman, I. N., & Tropea, J. (2014). Chronic disease management:
improving care for people with osteoarthritis. Best Practice & Research Clinical
Rheumatology, 28(1), 119-142.
Broderick, J. E., Keefe, F. J., Bruckenthal, P., Junghaenel, D. U., Schneider, S.,
Schwartz, J. E., ... & Gould, E. (2014). Nurse practitioners can effectively deliver
pain coping skills training to osteoarthritis patients with chronic pain: a
randomized, controlled trial. PAIN®, 155(9), 1743-1754.
Harris, H., & Crawford, A. (2015). Recognizing and managing
osteoarthritis. Nursing2018, 45(1), 36-42.
Jeon, E. (2015). Health behaviors of the elderly with osteoarthritis across gender
groups. Journal of the Korean Data and Information Science Society, 26(6), 1453-
1463.
Kim, C. S., Yoo, K. S., & Hong, S. H. (2014). The Effects of Foot Reflexology on
Arthralgia, Ankylosis, Depression, and Sleep in Community-dwelling Elderly
Women with Osteoarthritis. Journal of Korean Academy of Community Health
Nursing, 25(3), 207-216.
Kodadek, M. (2015). Managing osteoarthritis. Nursing for women's health, 19(1), 71-
76.
Lopez-Lopez, A., Gonzalez, J. L., Alonso-Fernández, M., Cuidad, N., & Matías, B.
(2014). Pain and symptoms of depression in older adults living in community and
in nursing homes: the role of activity restriction as a potential mediator and
moderator. International psychogeriatrics, 26(10), 1679-1691.
Markle-Reid, M., McAiney, C., Forbes, D., Thabane, L., Gibson, M., Browne, G., ...
7
References
References
Books
MacDonald, K. V., Sanmartin, C., Langlois, K., & Marshall, D. A. (2014). Symptom
onset, diagnosis and management of osteoarthritis. Canada :Statistics Canada.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-
Book. Australia: Elsevier Health Sciences.
Journals
Brand, C. A., Ackerman, I. N., & Tropea, J. (2014). Chronic disease management:
improving care for people with osteoarthritis. Best Practice & Research Clinical
Rheumatology, 28(1), 119-142.
Broderick, J. E., Keefe, F. J., Bruckenthal, P., Junghaenel, D. U., Schneider, S.,
Schwartz, J. E., ... & Gould, E. (2014). Nurse practitioners can effectively deliver
pain coping skills training to osteoarthritis patients with chronic pain: a
randomized, controlled trial. PAIN®, 155(9), 1743-1754.
Harris, H., & Crawford, A. (2015). Recognizing and managing
osteoarthritis. Nursing2018, 45(1), 36-42.
Jeon, E. (2015). Health behaviors of the elderly with osteoarthritis across gender
groups. Journal of the Korean Data and Information Science Society, 26(6), 1453-
1463.
Kim, C. S., Yoo, K. S., & Hong, S. H. (2014). The Effects of Foot Reflexology on
Arthralgia, Ankylosis, Depression, and Sleep in Community-dwelling Elderly
Women with Osteoarthritis. Journal of Korean Academy of Community Health
Nursing, 25(3), 207-216.
Kodadek, M. (2015). Managing osteoarthritis. Nursing for women's health, 19(1), 71-
76.
Lopez-Lopez, A., Gonzalez, J. L., Alonso-Fernández, M., Cuidad, N., & Matías, B.
(2014). Pain and symptoms of depression in older adults living in community and
in nursing homes: the role of activity restriction as a potential mediator and
moderator. International psychogeriatrics, 26(10), 1679-1691.
Markle-Reid, M., McAiney, C., Forbes, D., Thabane, L., Gibson, M., Browne, G., ...
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

400871
& Busing, B. (2014). An interprofessional nurse-led mental health promotion
intervention for older home care clients with depressive symptoms. BMC
geriatrics, 14(1), 62.
Ong, B. N., Morden, A., Brooks, L., Porcheret, M., Edwards, J. J., Sanders, T., ... &
Dziedzic, K. (2014). Changing policy and practice: making sense of national
guidelines for osteoarthritis. Social Science & Medicine, 106, 101-109.
Tanner, E. K., Martinez, I. L., & Harris, M. (2014). Examining functional and social
determinants of depression in community-dwelling older adults: Implications for
practice. Geriatric Nursing, 35(3), 236-240.
8
& Busing, B. (2014). An interprofessional nurse-led mental health promotion
intervention for older home care clients with depressive symptoms. BMC
geriatrics, 14(1), 62.
Ong, B. N., Morden, A., Brooks, L., Porcheret, M., Edwards, J. J., Sanders, T., ... &
Dziedzic, K. (2014). Changing policy and practice: making sense of national
guidelines for osteoarthritis. Social Science & Medicine, 106, 101-109.
Tanner, E. K., Martinez, I. L., & Harris, M. (2014). Examining functional and social
determinants of depression in community-dwelling older adults: Implications for
practice. Geriatric Nursing, 35(3), 236-240.
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




