Project Proposal: Revamping HPV Immunization in Bay of Plenty, NZ
VerifiedAdded on 2020/04/29
|12
|2343
|72
Project
AI Summary
This project proposal outlines a plan to revamp the HPV immunization program in New Zealand, focusing on the Bay of Plenty region, which has a high cancer prevalence. The proposal addresses the background of HPV, its link to cervical cancer, and the existing immunization programs. It details strategies to increase immunization rates, including targeting vulnerable populations and addressing public perceptions. The proposal also includes next steps, such as improving awareness, focusing on deprived populations, and implementing government-funded initiatives. References and appendices with supporting data are also included in the project proposal. The project aims to improve public health outcomes and reduce cancer incidence through increased HPV vaccination uptake.
[Organization Name]
[Date]
PROJECT
PROPOSAL
HPV IMMUNIZATION
Prepared for: Management team
Prepared by:
1
[Date]
PROJECT
PROPOSAL
HPV IMMUNIZATION
Prepared for: Management team
Prepared by:
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of contents
Summary
Background
Proposal Details
Next Steps
References
2
Summary
Background
Proposal Details
Next Steps
References
2
1. Summary
Immunization programs in New Zealand exist in a two-fold
set of initiatives including a National Immunization Schedule
that primarily focuses on young children up to 12 years and the
Nationally Recommended and Funded vaccinations. The role of
both programs is to ensure that the population is safe from
vulnerabilities to lethal diseases. There has been a high
prevalence of cancer that forms the hallmark of this project.
The initiative is meant to revamp the approach to
implementation of the HPV immunization program.
HPV is fully understood as the Human Papillomavirus which is
mainly passed through sexual activity. The HPV virus is known
to proliferate other conditions such as cervical cancer in women
and other diseases in men. The HPV immunization program was
initiated in 2008 and was mainly for women. Recently, the
application has been made free for both males and females.
This program is meant to work to increase the level of which the
project may see its success. Some of the strategies include
focusing on the most vulnerable populations such as the
Whanau who are most exposed to the disease. This may involve
public awareness concerning the need for immunization for
both children and young adults.
The relevance for this initiative is based on the little statistics
that keep Bay of Plenty as one of the leading areas affected by
cancers. According to the figures, there is a significantly higher
rate of cancer reports in the field than the rest of nation.
Further, there is a higher prevalence of HPV virus among the
population. Some of the primary issues to address involve the
role of social perceptions concerning the immunization to be
encouraging sexual promiscuity. Also, it is also essential to take
note of the tendency of high poverty levels to be related to the
onset of cancers and effective ways of preventing the
development of the diseases. One of the methods is ensuring
that preventable factors such as HPV are dealt with.
3
Immunization programs in New Zealand exist in a two-fold
set of initiatives including a National Immunization Schedule
that primarily focuses on young children up to 12 years and the
Nationally Recommended and Funded vaccinations. The role of
both programs is to ensure that the population is safe from
vulnerabilities to lethal diseases. There has been a high
prevalence of cancer that forms the hallmark of this project.
The initiative is meant to revamp the approach to
implementation of the HPV immunization program.
HPV is fully understood as the Human Papillomavirus which is
mainly passed through sexual activity. The HPV virus is known
to proliferate other conditions such as cervical cancer in women
and other diseases in men. The HPV immunization program was
initiated in 2008 and was mainly for women. Recently, the
application has been made free for both males and females.
This program is meant to work to increase the level of which the
project may see its success. Some of the strategies include
focusing on the most vulnerable populations such as the
Whanau who are most exposed to the disease. This may involve
public awareness concerning the need for immunization for
both children and young adults.
The relevance for this initiative is based on the little statistics
that keep Bay of Plenty as one of the leading areas affected by
cancers. According to the figures, there is a significantly higher
rate of cancer reports in the field than the rest of nation.
Further, there is a higher prevalence of HPV virus among the
population. Some of the primary issues to address involve the
role of social perceptions concerning the immunization to be
encouraging sexual promiscuity. Also, it is also essential to take
note of the tendency of high poverty levels to be related to the
onset of cancers and effective ways of preventing the
development of the diseases. One of the methods is ensuring
that preventable factors such as HPV are dealt with.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Background
2. The target suggested is the increase in immunizations for
communities in New Zealand. The immunization programs are mainly
facilitated by the locally approved vaccinators. According to Ministry of
Health, (2017) the main vaccinators that are supported for this target
include any local programs specifically recommended by a medical
health officer of the area or the National Immunization Schedule and
nationally endorsed and funded vaccinations for particular groups. The
National Immunization Schedule is usually aimed at providing
vaccinations against diseases for children aged six weeks to 12 years
(Udy, 2008). The rationale for increased immunizations is to ensure the
best possible health protection for children and to reduce the
prevalence of lethal disease among the younger population. Very
young children are usually at most risk of developing diseases since
their body immune systems are not exposed to dangerous infectious
conditions. If there might emerge infectious and lethal diseases that
are likely to affect other groups, the program has allowed funded
vaccinations for particular groups. The coverage of immunization
programs for the National Immunization Schedule has seen significant
success. For instance, in 2017, their immunization of eligible
candidates was well above 80% for most immunization services
(Ministry of Health, 2017). The implication is that there are minimal
changes that should be made to create an improvement in the
immunization prospects.
Some of the current HPV related health initiatives in Bay of Plenty area
include the Pasifika HPV promotion that focuses on Pacific Islander
females using incentives to encourage HPV immunizations. For this
target, we focus on a health initiative that is inclusive of children
vaccinated under the National Immunization Schedule and older
populations. The HPV immunization is government funded and is
provided for children at the age of 8 years to 26-year-old young adults.
The HPV Immunization Program was initiated as early as 2008. The
HPV began as an initiative to help prevent cancer causing HPV
infections. The effort started through evaluation of similar strategies
that were already commenced overseas. The currently available HPV
vaccination is approved by Medsafe to be safe for use on humans. Also
up to 125 other countries are using the same immunization and have
established that the prevention is long lasting. According to New
Zealand Herald, (2011), there are still up to 150 cases of cervical
cancer among older women in the entire nation every year. The
perception is that the prevalence of disease-causing infections is
always relatively high and requires the attention of governmental
programs. The main idea behind the HPV virus is to introduce to the
body, a non-infectious version of the HPV virus to trigger preventive
antibodies that can keep the patient immune from infection.
4
2. The target suggested is the increase in immunizations for
communities in New Zealand. The immunization programs are mainly
facilitated by the locally approved vaccinators. According to Ministry of
Health, (2017) the main vaccinators that are supported for this target
include any local programs specifically recommended by a medical
health officer of the area or the National Immunization Schedule and
nationally endorsed and funded vaccinations for particular groups. The
National Immunization Schedule is usually aimed at providing
vaccinations against diseases for children aged six weeks to 12 years
(Udy, 2008). The rationale for increased immunizations is to ensure the
best possible health protection for children and to reduce the
prevalence of lethal disease among the younger population. Very
young children are usually at most risk of developing diseases since
their body immune systems are not exposed to dangerous infectious
conditions. If there might emerge infectious and lethal diseases that
are likely to affect other groups, the program has allowed funded
vaccinations for particular groups. The coverage of immunization
programs for the National Immunization Schedule has seen significant
success. For instance, in 2017, their immunization of eligible
candidates was well above 80% for most immunization services
(Ministry of Health, 2017). The implication is that there are minimal
changes that should be made to create an improvement in the
immunization prospects.
Some of the current HPV related health initiatives in Bay of Plenty area
include the Pasifika HPV promotion that focuses on Pacific Islander
females using incentives to encourage HPV immunizations. For this
target, we focus on a health initiative that is inclusive of children
vaccinated under the National Immunization Schedule and older
populations. The HPV immunization is government funded and is
provided for children at the age of 8 years to 26-year-old young adults.
The HPV Immunization Program was initiated as early as 2008. The
HPV began as an initiative to help prevent cancer causing HPV
infections. The effort started through evaluation of similar strategies
that were already commenced overseas. The currently available HPV
vaccination is approved by Medsafe to be safe for use on humans. Also
up to 125 other countries are using the same immunization and have
established that the prevention is long lasting. According to New
Zealand Herald, (2011), there are still up to 150 cases of cervical
cancer among older women in the entire nation every year. The
perception is that the prevalence of disease-causing infections is
always relatively high and requires the attention of governmental
programs. The main idea behind the HPV virus is to introduce to the
body, a non-infectious version of the HPV virus to trigger preventive
antibodies that can keep the patient immune from infection.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Proposal details
The relevance for an increased investment into the
implementation of vaccination programs for HPV is that there
is a need for most families to understand the reality of
cervical cancer and other conditions that the young adult
may risk in the event of HPV infection. According to Cancer
Society, (2017) HPV is behind 70% of cervical cancer cases
and is therefore essential for girls. In fact, the program in
2008 offered free vaccination for girls. However, there is still
a high risk of developing other cancers among women and
men who contract the virus. This explains the place of
controversies against the vaccination with a focus on
medications such as Gardasil. New Zealand Herald, (2017)
reports that in 2016, the government invested an extra $124
million in HPV vaccinations to increase access to further
medication. Even with the progress that the government has
made in availing the injection for HPV, there is a need for
public education which forms part of the program to
implement HPV vaccination correctly. Some of the primary
concerns are the public perception of the immunization to be
promoting promiscuity and the scepticism that is associated
with the cervical smear (Dursun et al., 2009). The approval
age for the HPV vaccination requires girls to acquire the
immunization as early as possible when their immune
systems are stronger than when they get older.
However, there are more disparaging statistics that point
towards the need to implement vaccination that may work
towards improving future healthfully. The Bay of Plenty faces
the highest numbers of cancer cases and therefore requires
all mechanisms to be undertaken to ensure that the
possibility of developing cancer through contracted HPV are
reduced. Some of the main issues surrounding the perception
include a report that Bay of Plenty shows cancer cases
significantly higher than the national mean. The cancer
mortality rate is at 140 per 100,000 making it the seventh
highest in the nation (New Zealand Herald, 2011). It is thus
an imperative to look at the population outlook of cancer
cases. According to New Zealand Herald, (2011) the Maori
population who are the most deprived report more cases. The
implication is that there is a higher correlation between low
income and the possibility of developing cancer.
Government-funded initiatives to counter cancer and cancer-
causing diseases such as HPV, therefore, do not cease in
their importance.
5
The relevance for an increased investment into the
implementation of vaccination programs for HPV is that there
is a need for most families to understand the reality of
cervical cancer and other conditions that the young adult
may risk in the event of HPV infection. According to Cancer
Society, (2017) HPV is behind 70% of cervical cancer cases
and is therefore essential for girls. In fact, the program in
2008 offered free vaccination for girls. However, there is still
a high risk of developing other cancers among women and
men who contract the virus. This explains the place of
controversies against the vaccination with a focus on
medications such as Gardasil. New Zealand Herald, (2017)
reports that in 2016, the government invested an extra $124
million in HPV vaccinations to increase access to further
medication. Even with the progress that the government has
made in availing the injection for HPV, there is a need for
public education which forms part of the program to
implement HPV vaccination correctly. Some of the primary
concerns are the public perception of the immunization to be
promoting promiscuity and the scepticism that is associated
with the cervical smear (Dursun et al., 2009). The approval
age for the HPV vaccination requires girls to acquire the
immunization as early as possible when their immune
systems are stronger than when they get older.
However, there are more disparaging statistics that point
towards the need to implement vaccination that may work
towards improving future healthfully. The Bay of Plenty faces
the highest numbers of cancer cases and therefore requires
all mechanisms to be undertaken to ensure that the
possibility of developing cancer through contracted HPV are
reduced. Some of the main issues surrounding the perception
include a report that Bay of Plenty shows cancer cases
significantly higher than the national mean. The cancer
mortality rate is at 140 per 100,000 making it the seventh
highest in the nation (New Zealand Herald, 2011). It is thus
an imperative to look at the population outlook of cancer
cases. According to New Zealand Herald, (2011) the Maori
population who are the most deprived report more cases. The
implication is that there is a higher correlation between low
income and the possibility of developing cancer.
Government-funded initiatives to counter cancer and cancer-
causing diseases such as HPV, therefore, do not cease in
their importance.
5
3. Next Steps
At the bay of plenty, some of the leading programs should be
aimed at improving awareness concerning HPV immunization
and its importance. Some of the factors to address are the
perceptions concerning sexual behaviour about HPV
immunization (Dursun et al., 2009). This may involve
encouraging safe sexual conduct alongside the promotion of
healthy options such as the immunization.
Other strategies may involve focusing on the most deprived
populations in the Bay of Plenty. For instance, Ministry of
Health, (2017) suggests a move to lobby for the DHB to include
cancer component in the whanau long-term contracts. Such
policy implementations should work towards ensuring that the
government is accountable for reducing the cancer prospects at
the Bay of Plenty.
An important strategy is to fund and implement a provision of
HPV immunization freely for both the males and females
alongside the promotion of nurse knowledge framework to
assist with the efficient implementation of the project (Parkin &
Bray, 2006). The Bay of Plenty may work towards encouraging
funds for initiatives to work on nursing hospices and practitioner
training to improve the patient experiences at healthcare
centres.
Further, there should be an improvement of palliative care and
innovation of various prevention plans to deal with HPV and HPV
related conditions (Kang et al., 2015). There should be
implemented more effective tumour review technology that may
help in treating cancers in time.
6
At the bay of plenty, some of the leading programs should be
aimed at improving awareness concerning HPV immunization
and its importance. Some of the factors to address are the
perceptions concerning sexual behaviour about HPV
immunization (Dursun et al., 2009). This may involve
encouraging safe sexual conduct alongside the promotion of
healthy options such as the immunization.
Other strategies may involve focusing on the most deprived
populations in the Bay of Plenty. For instance, Ministry of
Health, (2017) suggests a move to lobby for the DHB to include
cancer component in the whanau long-term contracts. Such
policy implementations should work towards ensuring that the
government is accountable for reducing the cancer prospects at
the Bay of Plenty.
An important strategy is to fund and implement a provision of
HPV immunization freely for both the males and females
alongside the promotion of nurse knowledge framework to
assist with the efficient implementation of the project (Parkin &
Bray, 2006). The Bay of Plenty may work towards encouraging
funds for initiatives to work on nursing hospices and practitioner
training to improve the patient experiences at healthcare
centres.
Further, there should be an improvement of palliative care and
innovation of various prevention plans to deal with HPV and HPV
related conditions (Kang et al., 2015). There should be
implemented more effective tumour review technology that may
help in treating cancers in time.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Ministry of Health. (2017) “HPV Vaccine” Retrieved from
http://www.health.govt.nz/our-work/preventative-health-
wellness/immunisation/hpv-immunisation-programme/hpv-
vaccine
Ministry of Health. (2017). “National and DHB Immunization data.”
Retrieved from http://www.health.govt.nz/our-work/preventative-
health-wellness/immunisation/immunisation-coverage/national-
and-dhb-immunisation-data
Udy, Carly. (2008 May 2nd). “TOP STORY: Cancer Vaccine for Bay
Children.” New Zealand Herald. Retrieved from
http://www.nzherald.co.nz/bay-of-plenty-times/news/article.cfm?
c_id=1503343&objectid=10969360
New Zealand Herald. (2017 Jan 31st). “Awareness Campaign launched
as HPV immunization is extended to year 8 boys.” New Zealand
Herald. Retrieved from
http://www.nzherald.co.nz/nz/news/article.cfm?
c_id=1&objectid=11792001
New Zealand Herald. (2011, Sep 10th). “Bay has the highest cancer
rate in NZ.” New Zealand Herald. Retrieved from
http://www.nzherald.co.nz/bay-of-plenty-times/news/article.cfm?
c_id=1503343&objectid=11040619
Waikato DHB. (2017). “Regional Services Plan 2016/19” Retrieved from
http://waikatodhb-ebooks.co.nz/midlandregional/MidlandDHBsRe
gionalServicesPlan/files/basic-html/page31.html
Toi Te Ora. (2017, April 3rd). “Young people urged to get free HPV
immunization.” Scoop. Retrieved from
http://www.scoop.co.nz/stories/GE1704/S00009/young-people-
urged-to-get-free-hpv-immunisation.htm
Cancer Society. (2017). “Cervical Cancer.” Retrieved from
https://cancernz.org.nz/cancer-information/cancer-types/cervical-
cancer/
Kang, Y. J., Lewis, H., Smith, M. A., Simonella, L., Neal, H., Bromhead,
C., & Canfell, K. (2015). Pre-vaccination type-specific HPV
prevalence in confirmed cervical high grade lesions in the Māori
and non-Māori populations in New Zealand. BMC infectious
diseases, 15(1), 365.
Carter, J. R., Ding, Z., & Rose, B. R. (2011). HPV infection and cervical
disease: a review. Australian and New Zealand Journal of
Obstetrics and Gynaecology, 51(2), 103-108.
7
Ministry of Health. (2017) “HPV Vaccine” Retrieved from
http://www.health.govt.nz/our-work/preventative-health-
wellness/immunisation/hpv-immunisation-programme/hpv-
vaccine
Ministry of Health. (2017). “National and DHB Immunization data.”
Retrieved from http://www.health.govt.nz/our-work/preventative-
health-wellness/immunisation/immunisation-coverage/national-
and-dhb-immunisation-data
Udy, Carly. (2008 May 2nd). “TOP STORY: Cancer Vaccine for Bay
Children.” New Zealand Herald. Retrieved from
http://www.nzherald.co.nz/bay-of-plenty-times/news/article.cfm?
c_id=1503343&objectid=10969360
New Zealand Herald. (2017 Jan 31st). “Awareness Campaign launched
as HPV immunization is extended to year 8 boys.” New Zealand
Herald. Retrieved from
http://www.nzherald.co.nz/nz/news/article.cfm?
c_id=1&objectid=11792001
New Zealand Herald. (2011, Sep 10th). “Bay has the highest cancer
rate in NZ.” New Zealand Herald. Retrieved from
http://www.nzherald.co.nz/bay-of-plenty-times/news/article.cfm?
c_id=1503343&objectid=11040619
Waikato DHB. (2017). “Regional Services Plan 2016/19” Retrieved from
http://waikatodhb-ebooks.co.nz/midlandregional/MidlandDHBsRe
gionalServicesPlan/files/basic-html/page31.html
Toi Te Ora. (2017, April 3rd). “Young people urged to get free HPV
immunization.” Scoop. Retrieved from
http://www.scoop.co.nz/stories/GE1704/S00009/young-people-
urged-to-get-free-hpv-immunisation.htm
Cancer Society. (2017). “Cervical Cancer.” Retrieved from
https://cancernz.org.nz/cancer-information/cancer-types/cervical-
cancer/
Kang, Y. J., Lewis, H., Smith, M. A., Simonella, L., Neal, H., Bromhead,
C., & Canfell, K. (2015). Pre-vaccination type-specific HPV
prevalence in confirmed cervical high grade lesions in the Māori
and non-Māori populations in New Zealand. BMC infectious
diseases, 15(1), 365.
Carter, J. R., Ding, Z., & Rose, B. R. (2011). HPV infection and cervical
disease: a review. Australian and New Zealand Journal of
Obstetrics and Gynaecology, 51(2), 103-108.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Parkin, D. M., & Bray, F. (2006). The burden of HPV-related cancers.
Vaccine, 24, S11-S25.
Dursun, P., Altuntas, B., Kuscu, E., & Ayhan, A. (2009). Women's
knowledge about human papillomavirus and their acceptance of
HPV vaccine. Australian and New Zealand Journal of Obstetrics
and Gynaecology, 49(2), 202-206.
8
Vaccine, 24, S11-S25.
Dursun, P., Altuntas, B., Kuscu, E., & Ayhan, A. (2009). Women's
knowledge about human papillomavirus and their acceptance of
HPV vaccine. Australian and New Zealand Journal of Obstetrics
and Gynaecology, 49(2), 202-206.
8
Appendices
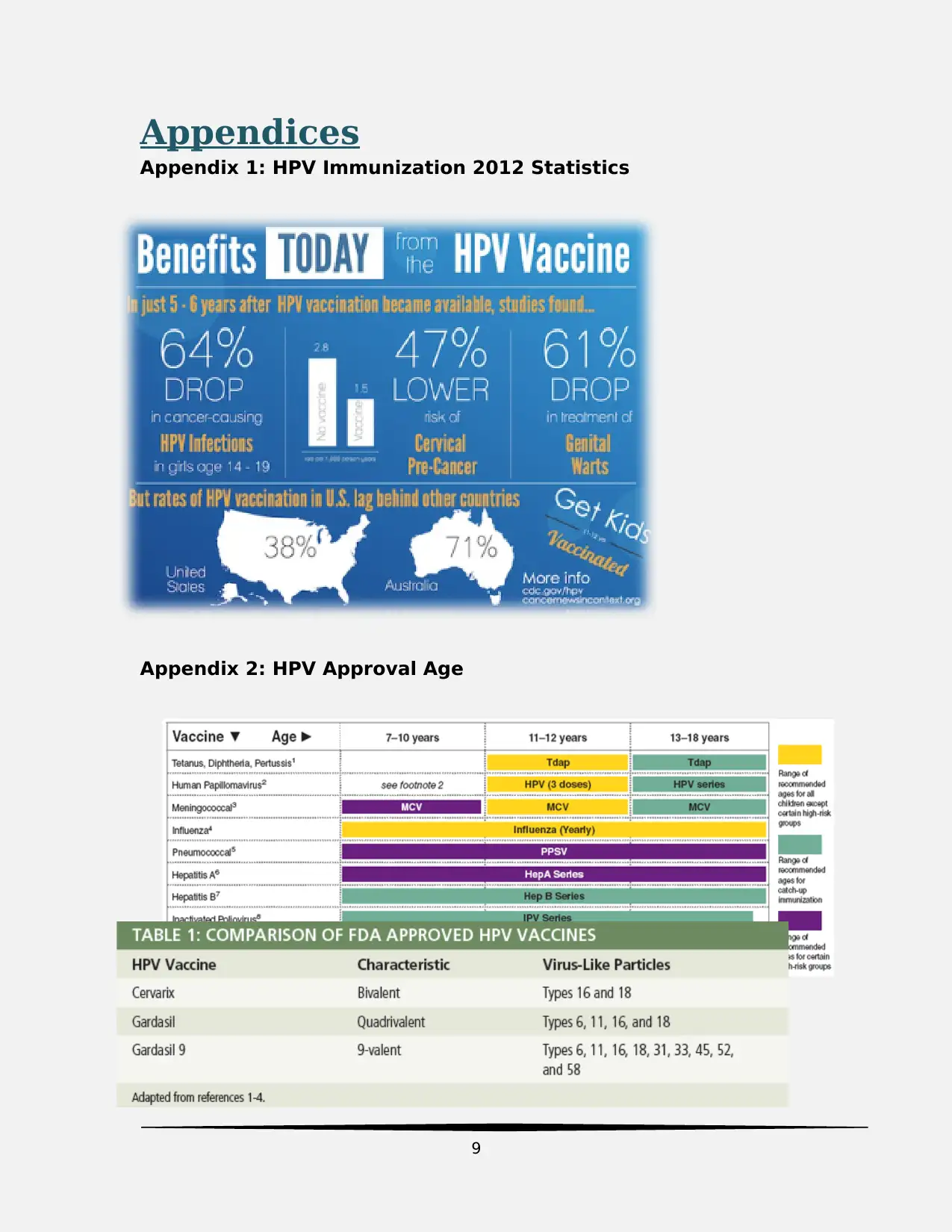
Appendix 1: HPV Immunization 2012 Statistics
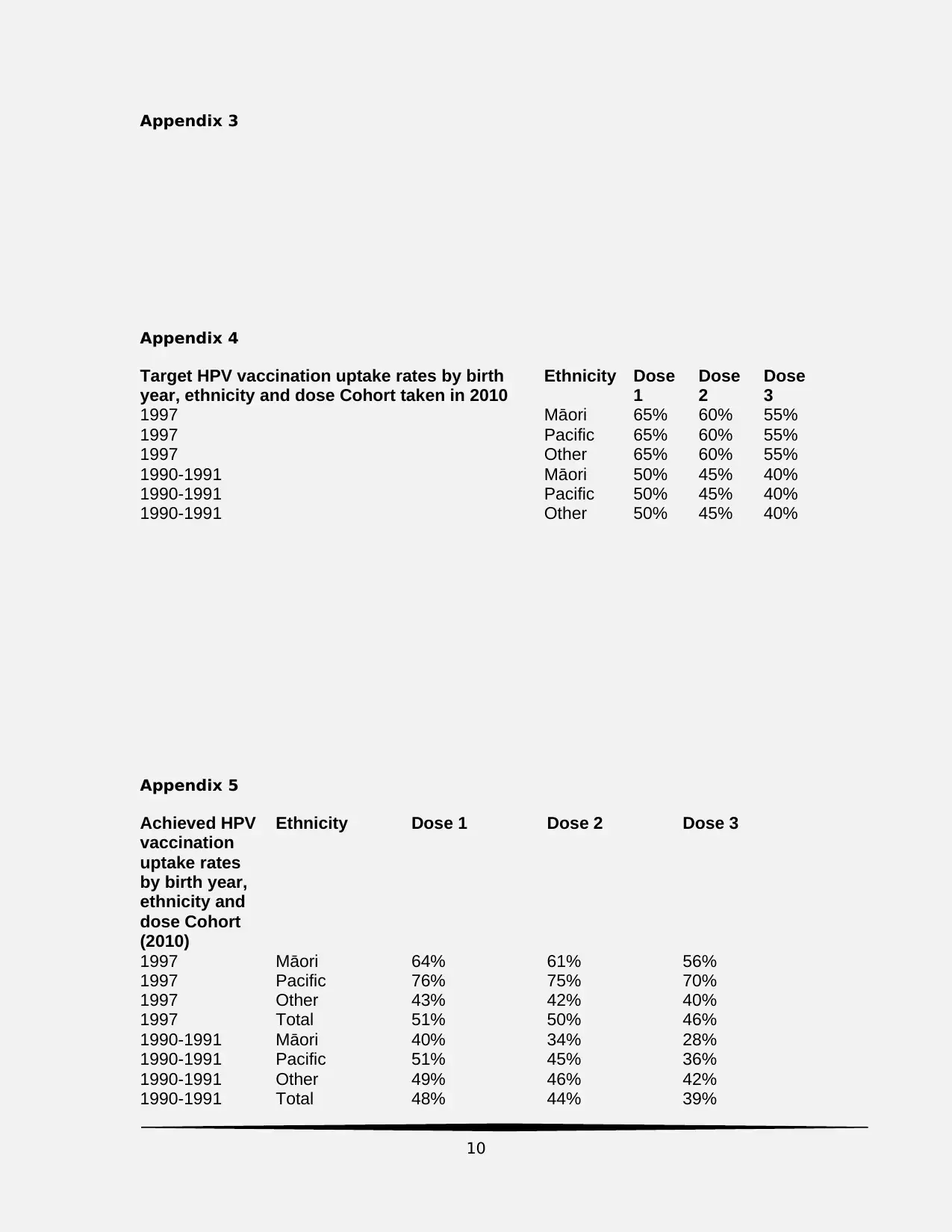
Appendix 2: HPV Approval Age
9
Appendix 1: HPV Immunization 2012 Statistics
Appendix 2: HPV Approval Age
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Appendix 3
Appendix 4
Target HPV vaccination uptake rates by birth
year, ethnicity and dose Cohort taken in 2010
Ethnicity Dose
1
Dose
2
Dose
3
1997 Māori 65% 60% 55%
1997 Pacific 65% 60% 55%
1997 Other 65% 60% 55%
1990-1991 Māori 50% 45% 40%
1990-1991 Pacific 50% 45% 40%
1990-1991 Other 50% 45% 40%
Appendix 5
Achieved HPV
vaccination
uptake rates
by birth year,
ethnicity and
dose Cohort
(2010)
Ethnicity Dose 1 Dose 2 Dose 3
1997 Māori 64% 61% 56%
1997 Pacific 76% 75% 70%
1997 Other 43% 42% 40%
1997 Total 51% 50% 46%
1990-1991 Māori 40% 34% 28%
1990-1991 Pacific 51% 45% 36%
1990-1991 Other 49% 46% 42%
1990-1991 Total 48% 44% 39%
10
Appendix 4
Target HPV vaccination uptake rates by birth
year, ethnicity and dose Cohort taken in 2010
Ethnicity Dose
1
Dose
2
Dose
3
1997 Māori 65% 60% 55%
1997 Pacific 65% 60% 55%
1997 Other 65% 60% 55%
1990-1991 Māori 50% 45% 40%
1990-1991 Pacific 50% 45% 40%
1990-1991 Other 50% 45% 40%
Appendix 5
Achieved HPV
vaccination
uptake rates
by birth year,
ethnicity and
dose Cohort
(2010)
Ethnicity Dose 1 Dose 2 Dose 3
1997 Māori 64% 61% 56%
1997 Pacific 76% 75% 70%
1997 Other 43% 42% 40%
1997 Total 51% 50% 46%
1990-1991 Māori 40% 34% 28%
1990-1991 Pacific 51% 45% 36%
1990-1991 Other 49% 46% 42%
1990-1991 Total 48% 44% 39%
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
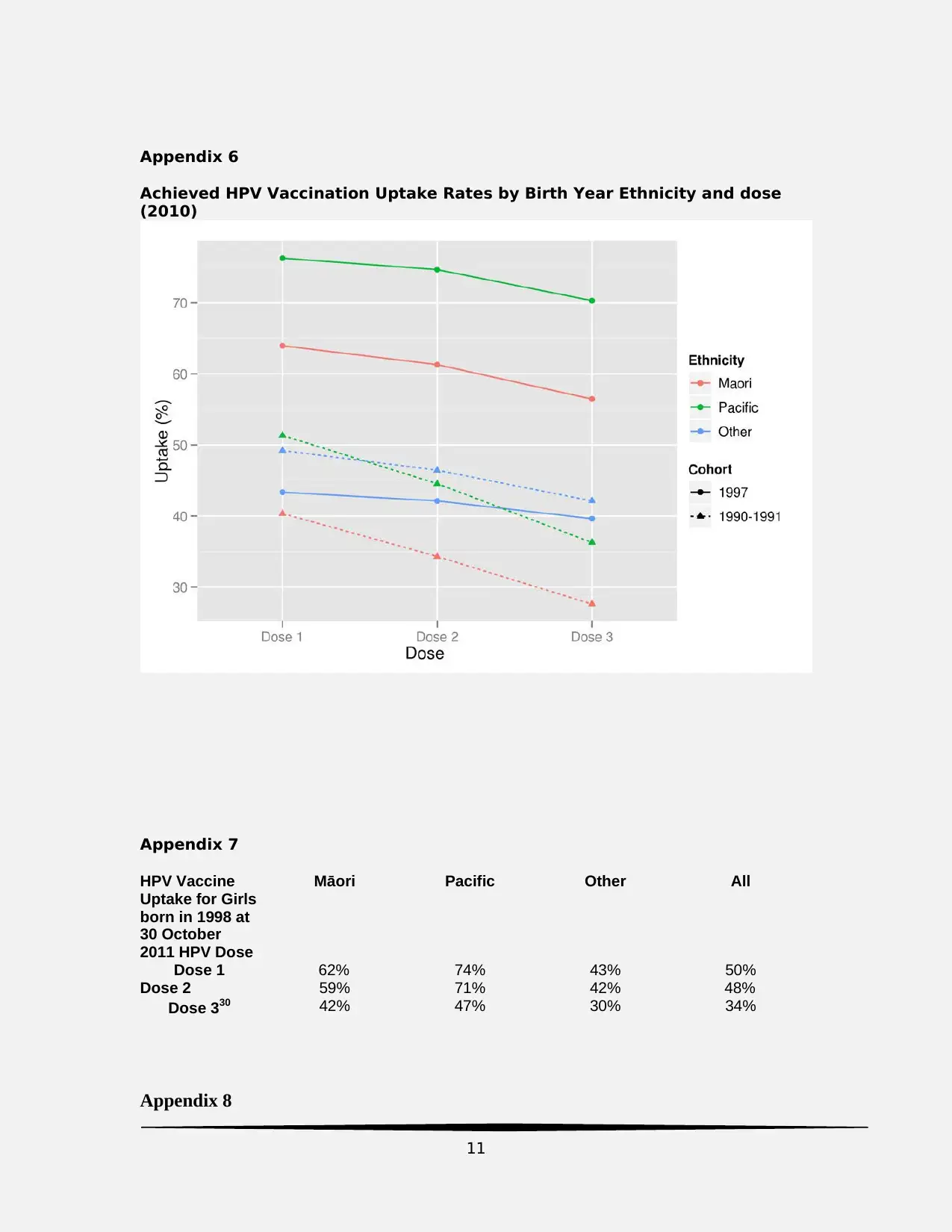
Appendix 6
Achieved HPV Vaccination Uptake Rates by Birth Year Ethnicity and dose
(2010)
Appendix 7
HPV Vaccine
Uptake for Girls
born in 1998 at
30 October
2011 HPV Dose
Māori Pacific Other All
Dose 1 62% 74% 43% 50%
Dose 2 59% 71% 42% 48%
Dose 330 42% 47% 30% 34%
Appendix 8
11
Achieved HPV Vaccination Uptake Rates by Birth Year Ethnicity and dose
(2010)
Appendix 7
HPV Vaccine
Uptake for Girls
born in 1998 at
30 October
2011 HPV Dose
Māori Pacific Other All
Dose 1 62% 74% 43% 50%
Dose 2 59% 71% 42% 48%
Dose 330 42% 47% 30% 34%
Appendix 8
11
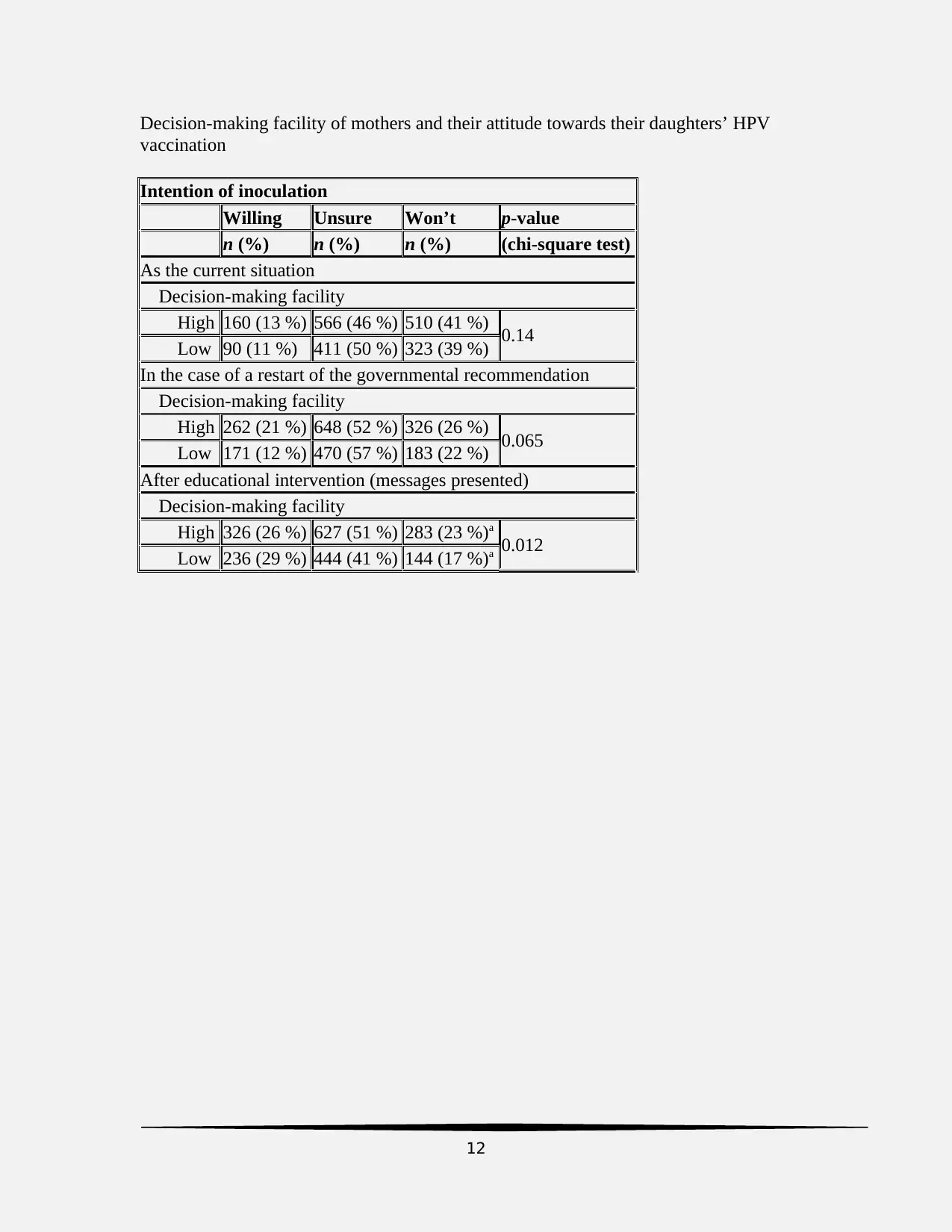
Decision-making facility of mothers and their attitude towards their daughters’ HPV
vaccination
Intention of inoculation
Willing Unsure Won’t p-value
n (%) n (%) n (%) (chi-square test)
As the current situation
Decision-making facility
High 160 (13 %) 566 (46 %) 510 (41 %) 0.14
Low 90 (11 %) 411 (50 %) 323 (39 %)
In the case of a restart of the governmental recommendation
Decision-making facility
High 262 (21 %) 648 (52 %) 326 (26 %) 0.065
Low 171 (12 %) 470 (57 %) 183 (22 %)
After educational intervention (messages presented)
Decision-making facility
High 326 (26 %) 627 (51 %) 283 (23 %)a
0.012
Low 236 (29 %) 444 (41 %) 144 (17 %)a
12
vaccination
Intention of inoculation
Willing Unsure Won’t p-value
n (%) n (%) n (%) (chi-square test)
As the current situation
Decision-making facility
High 160 (13 %) 566 (46 %) 510 (41 %) 0.14
Low 90 (11 %) 411 (50 %) 323 (39 %)
In the case of a restart of the governmental recommendation
Decision-making facility
High 262 (21 %) 648 (52 %) 326 (26 %) 0.065
Low 171 (12 %) 470 (57 %) 183 (22 %)
After educational intervention (messages presented)
Decision-making facility
High 326 (26 %) 627 (51 %) 283 (23 %)a
0.012
Low 236 (29 %) 444 (41 %) 144 (17 %)a
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





