NURBN 2024 Module 4: Psychotic Illness and Schizophrenia Overview
VerifiedAdded on 2022/09/06
|14
|2744
|17
Homework Assignment
AI Summary
This document provides a comprehensive overview of psychotic illness and schizophrenia, covering key concepts, symptoms (hallucinations, delusions, thought disorders), precipitating factors, and the stages of psychosis. It defines schizophrenia, its prevalence, causes (genetic, biochemical, and vulnerability/stress), and differentiates between facts and myths. The assignment details the use of antipsychotic medications, including typical and atypical drugs, their mechanisms of action, and adjunct treatments like hospital care, rehabilitation, and psychological therapies (CBT, family therapy, and self-help groups). It also discusses the management of medication side effects and strategies for handling challenging behaviors, including triggers and risk assessments. The document emphasizes the importance of understanding and addressing challenging behaviors, which can be triggered by intrinsic and extrinsic factors, and provides guidance on how nurses can help clients manage medication side effects and challenging behaviors, focusing on de-escalation techniques, risk assessment and the importance of a calm approach.
NURBN 2024 Module 4
Week 4 - psychotic illness and schizophrenia
Mark as done
Introductio
Intended learning outcomes
On completion of this unit, participants will be able to:
Have an understanding of psychotic illness & schizophrenia
Discuss the use of anti-psychotic medication & management of side-effects
Explore the care & support for a client with a psychotic illness
Understand the issues around challenging behaviour / aggression
Understand solution focused therapy interventions
What is psychosis?
Key Concept
Psychosis is a syndrome or group of symptoms that may be associated with
schizophrenia and other mental illnesses including depression, bipolar disorder,
dementia and borderline personality disorder. Psychosis may also be caused by a
brain injury, neurological problem, or other health problem.
Major Symptoms:
Hallucinations
Delusions
Week 4 - psychotic illness and schizophrenia
Mark as done
Introductio
Intended learning outcomes
On completion of this unit, participants will be able to:
Have an understanding of psychotic illness & schizophrenia
Discuss the use of anti-psychotic medication & management of side-effects
Explore the care & support for a client with a psychotic illness
Understand the issues around challenging behaviour / aggression
Understand solution focused therapy interventions
What is psychosis?
Key Concept
Psychosis is a syndrome or group of symptoms that may be associated with
schizophrenia and other mental illnesses including depression, bipolar disorder,
dementia and borderline personality disorder. Psychosis may also be caused by a
brain injury, neurological problem, or other health problem.
Major Symptoms:
Hallucinations
Delusions
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Other Symptoms:
Difficulties concentrating, completing tasks, or making decisions
Thoughts may feel ‘jumbled’ or confused.
Difficulty following conversations or speaking clearly.
May affect physical movement and emotional expression.
Precipitating Factors
Extreme stress,
Severe lack of sleep, or trauma
Using or withdrawing from certain drugs or medications
Stages of psychosis - usually experienced in schizophrenia
Premorbid – no signs or symptoms
Prodrome – a period of pre-psychotic disturbance with changes in feelings, thoughts
and perceptions - it tends to develop earlier in males e.g. late teens and later in
females - in mid 20's
Acute – characterised by positive psychotic symptoms
Recovery and Late Recovery – acute symptoms remit and later functional recovery
occurs
Relapse – often occurs within five years of the onset of the acute phase
What is schizophrenia?
Schizophrenia - is a psychotic illness & the focus of our study in this module
•Schizophrenia (s’a) is not defined as a single illness but is thought of as a group
of severe, disabling psychotic disorders marked by withdrawal from reality,
illogical thinking, possible delusions and hallucinations and other emotional,
behavioural or intellectual disturbances (it is important to understand this
definition)
•There is currently no physical or laboratory test that can definitively diagnose
schizophrenia – diagnosis is arrived at by a psychiatrist, based on clinical symptoms.
•Disturbances may affect everything from speech, affect, psycho-motor behaviour,
interpersonal relationships and sense of self
•Prevalence is 1% of the population & affects men & women equally
•Onset between 15 – 25 years of age (usually for males) and 25 years onwards (for
females)
•Incidence and lifetime prevalence is roughly the same world-wide
Facts and myths about schizophrenia
Difficulties concentrating, completing tasks, or making decisions
Thoughts may feel ‘jumbled’ or confused.
Difficulty following conversations or speaking clearly.
May affect physical movement and emotional expression.
Precipitating Factors
Extreme stress,
Severe lack of sleep, or trauma
Using or withdrawing from certain drugs or medications
Stages of psychosis - usually experienced in schizophrenia
Premorbid – no signs or symptoms
Prodrome – a period of pre-psychotic disturbance with changes in feelings, thoughts
and perceptions - it tends to develop earlier in males e.g. late teens and later in
females - in mid 20's
Acute – characterised by positive psychotic symptoms
Recovery and Late Recovery – acute symptoms remit and later functional recovery
occurs
Relapse – often occurs within five years of the onset of the acute phase
What is schizophrenia?
Schizophrenia - is a psychotic illness & the focus of our study in this module
•Schizophrenia (s’a) is not defined as a single illness but is thought of as a group
of severe, disabling psychotic disorders marked by withdrawal from reality,
illogical thinking, possible delusions and hallucinations and other emotional,
behavioural or intellectual disturbances (it is important to understand this
definition)
•There is currently no physical or laboratory test that can definitively diagnose
schizophrenia – diagnosis is arrived at by a psychiatrist, based on clinical symptoms.
•Disturbances may affect everything from speech, affect, psycho-motor behaviour,
interpersonal relationships and sense of self
•Prevalence is 1% of the population & affects men & women equally
•Onset between 15 – 25 years of age (usually for males) and 25 years onwards (for
females)
•Incidence and lifetime prevalence is roughly the same world-wide
Facts and myths about schizophrenia
Facts and myths about schizophrenia
Schizophrenia is not caused by bad parenting, childhood trauma, poverty or
alcohol
Schizophrenia is not contagious
Although people with schizophrenia sometimes hear “voices” that others can’t
hear, this illness does not mean that you have “split” or “multiple” personalities
Schizophrenia is not a person’s fault; it is a chemical brain disorder caused by a
combination of biological and genetic factors, and often triggered by
environmental stressors
Schizophrenia is not a developmental disability or intellectual disability
Those with a diagnosis of schizophrenia who are undergoing treatment are no
more violent or aggressive than those who do not have schizophrenia
There is no cure for schizophrenia
Aggression may occur among a minority of patients during an untreated
acute episode. However, this is uncommon and often unfairly portrayed in
the media. People with schizophrenia are more likely to be victims of
violence rather than perpetrators.
Possible causes of schizophrenia are:-
Genetic factors - (runs in families, a person with a first degree relative with the
disease stands a 15% chance of developing it themselves compared to the 1%
amongst the general population)
•Biochemical – abnormalities in the neuro-transmitters dopamine and
glutamate e.g. dopamine theory. This theory proposes that dopamine is
overactive in the brain thereby explaining hallucinations, agitation, delusional
thoughts & grandiosity
•Vulnerability / stress – a biologically susceptible person experiencing a
stressful event can trigger symptoms of schizophrenia
What is psychosis?
Symptoms of schizophrenia
Symptoms include:
• Hallucinations
• Delusions
• Thought disorder
• Social withdrawal
Schizophrenia is not caused by bad parenting, childhood trauma, poverty or
alcohol
Schizophrenia is not contagious
Although people with schizophrenia sometimes hear “voices” that others can’t
hear, this illness does not mean that you have “split” or “multiple” personalities
Schizophrenia is not a person’s fault; it is a chemical brain disorder caused by a
combination of biological and genetic factors, and often triggered by
environmental stressors
Schizophrenia is not a developmental disability or intellectual disability
Those with a diagnosis of schizophrenia who are undergoing treatment are no
more violent or aggressive than those who do not have schizophrenia
There is no cure for schizophrenia
Aggression may occur among a minority of patients during an untreated
acute episode. However, this is uncommon and often unfairly portrayed in
the media. People with schizophrenia are more likely to be victims of
violence rather than perpetrators.
Possible causes of schizophrenia are:-
Genetic factors - (runs in families, a person with a first degree relative with the
disease stands a 15% chance of developing it themselves compared to the 1%
amongst the general population)
•Biochemical – abnormalities in the neuro-transmitters dopamine and
glutamate e.g. dopamine theory. This theory proposes that dopamine is
overactive in the brain thereby explaining hallucinations, agitation, delusional
thoughts & grandiosity
•Vulnerability / stress – a biologically susceptible person experiencing a
stressful event can trigger symptoms of schizophrenia
What is psychosis?
Symptoms of schizophrenia
Symptoms include:
• Hallucinations
• Delusions
• Thought disorder
• Social withdrawal
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
• Lack of motivation
• ‘Blunted’ emotions
• Inappropriate responses
• Impaired thinking and memory
• Lack of insight
• Grossly disorganised or abnormal motor behaviour including catatonia
What are positive symptoms? (make sure you know what this means)
What are negative symptoms? (make sure you know what this means)
Below is a brief overview for you
• ‘Blunted’ emotions
• Inappropriate responses
• Impaired thinking and memory
• Lack of insight
• Grossly disorganised or abnormal motor behaviour including catatonia
What are positive symptoms? (make sure you know what this means)
What are negative symptoms? (make sure you know what this means)
Below is a brief overview for you
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
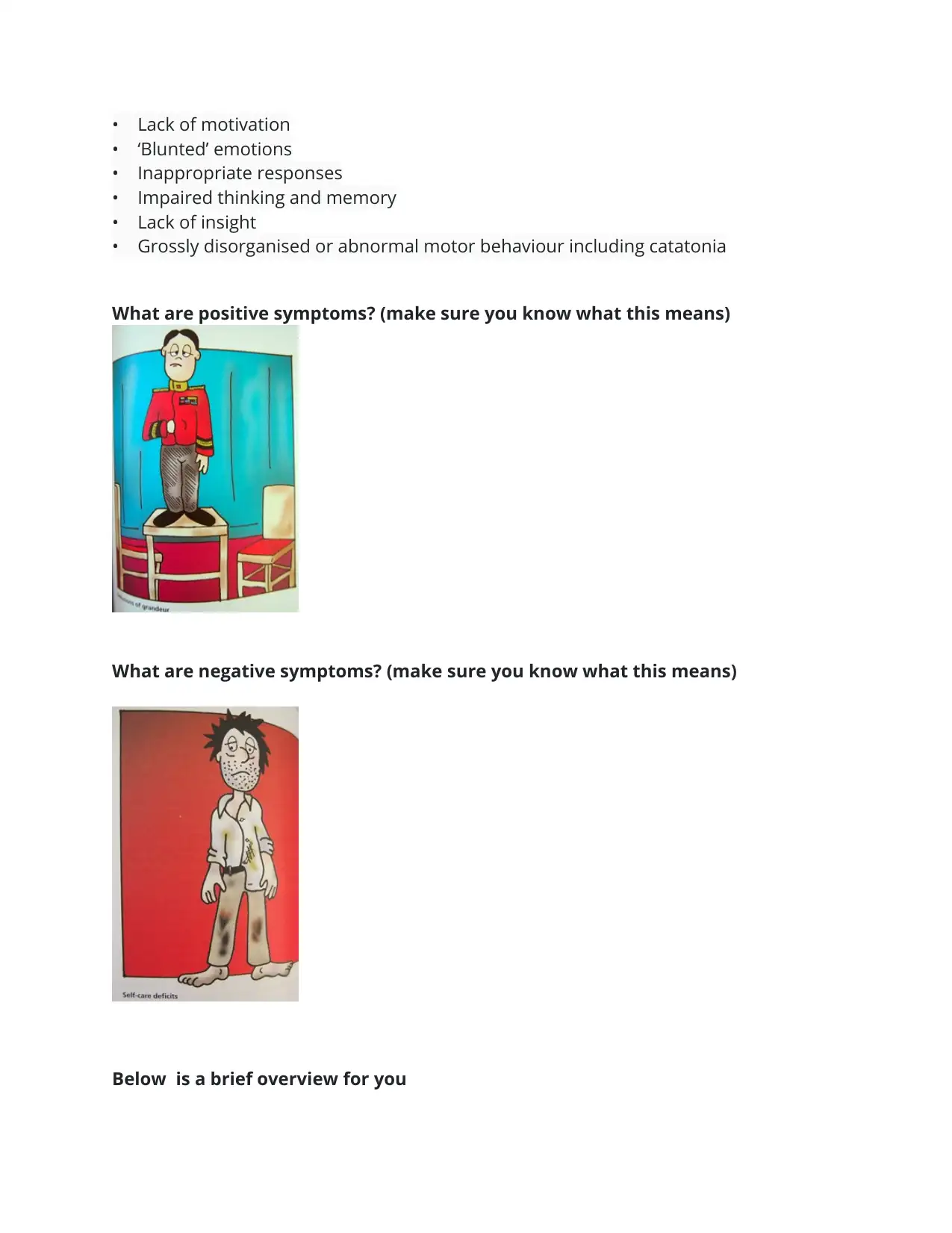
Positive Symptoms Negative Symptoms Cognitive Symptoms
- Hallucinations
- Delusions
- Racing &
disorganised thoughts
(expressed through
speech)
Apathy(avolution)
Lack of emotion
Poor or non-existent
social functioning
Poor self care
Difficulty concentrating
and/or following instructions
Difficulty completing tasks
Memory problems
Anti-psychotic medication
Anti-psychotic medication
To date, the best way to treat the symptoms of schizophrenia is with a combination of
medication, support and recovery-focused rehabilitation.
Taking medication as it is prescribed makes it five times less likely that a client will
experience a relapse.
There are two groups of anti-psychotics:-
The older group are called ‘typical’ antipsychotics' and include:
Chlorpromazine (Largactil)
Flupenthixol Decanoate (Fluanxol)
Haloperidol (Serenace)
Zuclopenthixol Decanoate (Clopixol)
- Hallucinations
- Delusions
- Racing &
disorganised thoughts
(expressed through
speech)
Apathy(avolution)
Lack of emotion
Poor or non-existent
social functioning
Poor self care
Difficulty concentrating
and/or following instructions
Difficulty completing tasks
Memory problems
Anti-psychotic medication
Anti-psychotic medication
To date, the best way to treat the symptoms of schizophrenia is with a combination of
medication, support and recovery-focused rehabilitation.
Taking medication as it is prescribed makes it five times less likely that a client will
experience a relapse.
There are two groups of anti-psychotics:-
The older group are called ‘typical’ antipsychotics' and include:
Chlorpromazine (Largactil)
Flupenthixol Decanoate (Fluanxol)
Haloperidol (Serenace)
Zuclopenthixol Decanoate (Clopixol)
The newer group are called ‘atypical’ antipsychotics' and examples of these include:
Amisulpride (Solian)
Aripiprazole (Abilify)
Clozapine (Clozaril, Clopine)
Olanzapine (Zyprexa)
Quetiapine (Seroquel)
Risperidone (Risperdal
How do these drugs work?
Anti-psychotics reduce or eliminate delusions, hallucinations, abnormal mood and
thought disorder. They also reduce the likelihood of further episodes of psychosis.
Their mode of action is blockage of dopamine and 5-HT2A receptors within the central
nervous system.
Anti-psychotic medication
Adjunct treatments for schizophrenia
Adjunct treatments for schizophrenia
To date, the best way to treat the symptoms of schizophrenia is with a
combination of medication, support and recovery-focused rehabilitation
Amisulpride (Solian)
Aripiprazole (Abilify)
Clozapine (Clozaril, Clopine)
Olanzapine (Zyprexa)
Quetiapine (Seroquel)
Risperidone (Risperdal
How do these drugs work?
Anti-psychotics reduce or eliminate delusions, hallucinations, abnormal mood and
thought disorder. They also reduce the likelihood of further episodes of psychosis.
Their mode of action is blockage of dopamine and 5-HT2A receptors within the central
nervous system.
Anti-psychotic medication
Adjunct treatments for schizophrenia
Adjunct treatments for schizophrenia
To date, the best way to treat the symptoms of schizophrenia is with a
combination of medication, support and recovery-focused rehabilitation
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Treatments include:
Effective antipsychotic medications provide many people with schizophrenia the
opportunity to lead full and productive lives. Antipsychotics help stabilise
some symptoms, but do not cure the disease and are frequently associated
with side effects. Most people with schizophrenia need to stay on medication to
prevent relapse (more on this later)
Hospital care – hospital admission is necessary only during periods of crises. As
soon as symptoms subside clients should be encouraged to return to normal
living.
Rehabilitation in the context of significant cognitive decline
All treatments / therapies have a recovery focus & aim to support and
assist a client on their journey back to functional wellness
Psychological treatment
Psychological treatment may help reduce the intensity of psychotic symptoms, and
anxiety caused by psychosis. Some possible psychological treatments are discussed
below.
Cognitive behavioural therapy
Cognitive behavioural therapy (CBT) for psychosis is based on an understanding
of how people make sense of their experiences and why some people become
distressed by them.
The aim of CBT is to identify unhelpful thinking patterns and emotions that may
be causing unwanted feelings and behaviours. It's then possible to learn to
replace this thinking with more realistic and balanced thoughts.
CBT encourage people to consider different ways of understanding specific
sitations. The aim is to help you achieve goals that are meaningful and
important to you, such as reducing your distress, returning to work or university,
or regaining a sense of control.
Family therapy
Family psycho-education (FPE) interventions have been shown to reduce relapse rates
and symptom levels and improve the social participation of people living with severe
and persistent psychotic disorders. FPE has a well-established evidence base that
predates that of CBT for psychosis! Surprisingly, despite the strong evidence, FPE
interventions are not routinely available for Australians living with psychosis and their
families.
Effective antipsychotic medications provide many people with schizophrenia the
opportunity to lead full and productive lives. Antipsychotics help stabilise
some symptoms, but do not cure the disease and are frequently associated
with side effects. Most people with schizophrenia need to stay on medication to
prevent relapse (more on this later)
Hospital care – hospital admission is necessary only during periods of crises. As
soon as symptoms subside clients should be encouraged to return to normal
living.
Rehabilitation in the context of significant cognitive decline
All treatments / therapies have a recovery focus & aim to support and
assist a client on their journey back to functional wellness
Psychological treatment
Psychological treatment may help reduce the intensity of psychotic symptoms, and
anxiety caused by psychosis. Some possible psychological treatments are discussed
below.
Cognitive behavioural therapy
Cognitive behavioural therapy (CBT) for psychosis is based on an understanding
of how people make sense of their experiences and why some people become
distressed by them.
The aim of CBT is to identify unhelpful thinking patterns and emotions that may
be causing unwanted feelings and behaviours. It's then possible to learn to
replace this thinking with more realistic and balanced thoughts.
CBT encourage people to consider different ways of understanding specific
sitations. The aim is to help you achieve goals that are meaningful and
important to you, such as reducing your distress, returning to work or university,
or regaining a sense of control.
Family therapy
Family psycho-education (FPE) interventions have been shown to reduce relapse rates
and symptom levels and improve the social participation of people living with severe
and persistent psychotic disorders. FPE has a well-established evidence base that
predates that of CBT for psychosis! Surprisingly, despite the strong evidence, FPE
interventions are not routinely available for Australians living with psychosis and their
families.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Aims to improve knowledge and coping skills in families and clients, to enable
them to work together more effectively to address the challenges of living with
psychosis.
Goal setting
Information sharing about the disorder, early warning signs and relapse
prevention
Practical skills training in coping, communication, problem solving and goal
setting.
Sessions can be conducted with single families or in a multi-family setting
Self-help groups
People who experience episodes of psychosis, may benefit from connecting with
other people who have had similar experiences.
Eg. Mind Australia, Sane Australia, Grow.org.au.
How can nurses help clients manage medication side-effects
How can we help our client manage unwanted side-effects of medication?
Increased appetite/weight gain/obesity - Regular exercise, avoid sweet and fatty
foods, low GI foods, avoid high carb diet
It's hard to avoid fast food when you can't cope ....but we can help clients by choosing
healthy alternatives
Nausea - Take meds with food or before sleeping
Constipation - Increase water intake, eat high fibre diet, fibre supplements
Postural hypotension (low BP) - Get up slowly after lying or sitting, avoid hot showers
& baths, avoid caffeine, alcohol
them to work together more effectively to address the challenges of living with
psychosis.
Goal setting
Information sharing about the disorder, early warning signs and relapse
prevention
Practical skills training in coping, communication, problem solving and goal
setting.
Sessions can be conducted with single families or in a multi-family setting
Self-help groups
People who experience episodes of psychosis, may benefit from connecting with
other people who have had similar experiences.
Eg. Mind Australia, Sane Australia, Grow.org.au.
How can nurses help clients manage medication side-effects
How can we help our client manage unwanted side-effects of medication?
Increased appetite/weight gain/obesity - Regular exercise, avoid sweet and fatty
foods, low GI foods, avoid high carb diet
It's hard to avoid fast food when you can't cope ....but we can help clients by choosing
healthy alternatives
Nausea - Take meds with food or before sleeping
Constipation - Increase water intake, eat high fibre diet, fibre supplements
Postural hypotension (low BP) - Get up slowly after lying or sitting, avoid hot showers
& baths, avoid caffeine, alcohol
Drowsiness (somnolence) = Divided doses of medication, negotiate a smaller doses
with Dr, use a Webster pack to keep on track if memory problems due to somnolence
Dry mouth = Regular fluids, suck on ice cubes, use sugarless gum or lollies, limit
alcohol & caffeine, artificial saliva (Biotin)
Sensitivity to sunburn = Avoid strong sun, wear hat and long sleeves
Managing challenging behaviour
Managing challenging behaviour
Key Concept
Challenging behaviour
Challenging behaviour can be defined as any behaviour of an individual which has the
potential to cause physical or psychological harm to themselves, another person, or to
property around them. It does not have to be deliberate acts – some patients who
suffer from mental health conditions can express challenging behaviour
unintentionally.
Such behaviour, whether intentional or not, can act as a barrier between the patient
and healthcare providers attempting to deliver care and support. Such behaviour can
also compromise the safety of staff and other patients in an in-patient setting (2)
What triggers challenging behaviour in mental health patients?
To better understand how to deal with challenging behaviours, healthcare providers
should appreciate the factors which trigger such actions in their patients. Research
with Dr, use a Webster pack to keep on track if memory problems due to somnolence
Dry mouth = Regular fluids, suck on ice cubes, use sugarless gum or lollies, limit
alcohol & caffeine, artificial saliva (Biotin)
Sensitivity to sunburn = Avoid strong sun, wear hat and long sleeves
Managing challenging behaviour
Managing challenging behaviour
Key Concept
Challenging behaviour
Challenging behaviour can be defined as any behaviour of an individual which has the
potential to cause physical or psychological harm to themselves, another person, or to
property around them. It does not have to be deliberate acts – some patients who
suffer from mental health conditions can express challenging behaviour
unintentionally.
Such behaviour, whether intentional or not, can act as a barrier between the patient
and healthcare providers attempting to deliver care and support. Such behaviour can
also compromise the safety of staff and other patients in an in-patient setting (2)
What triggers challenging behaviour in mental health patients?
To better understand how to deal with challenging behaviours, healthcare providers
should appreciate the factors which trigger such actions in their patients. Research
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
suggests that patients will express challenging behaviour as a result of either intrinsic
or extrinsic factors (2);
Intrinsic factors can be personal feelings, thoughts, emotions and health status
- both mental and physical.
Extrinsic factors will be the environment and people around them who can
trigger a behavioural response.
Remember - challenging behaviour does not lie exclusively in
the mental health ward alone. You will have to deal with challenging behaviour in all
areas of the hospital. Behaviour from a client that is challenging is a clear indication the
client is in distress.
Why does behaviour escalate?
Conflict - potentially harmful events such as:
aggression
perceived rule breaking (by the client)
Substance / alcohol use
Absconding / missing
Medication refusal
Self-harm / suicide
Coerced intra-muscular injection
Seclusion
Restraint
Over-use of PRN medication
How do we recognise escalating behaviour?
Male
or extrinsic factors (2);
Intrinsic factors can be personal feelings, thoughts, emotions and health status
- both mental and physical.
Extrinsic factors will be the environment and people around them who can
trigger a behavioural response.
Remember - challenging behaviour does not lie exclusively in
the mental health ward alone. You will have to deal with challenging behaviour in all
areas of the hospital. Behaviour from a client that is challenging is a clear indication the
client is in distress.
Why does behaviour escalate?
Conflict - potentially harmful events such as:
aggression
perceived rule breaking (by the client)
Substance / alcohol use
Absconding / missing
Medication refusal
Self-harm / suicide
Coerced intra-muscular injection
Seclusion
Restraint
Over-use of PRN medication
How do we recognise escalating behaviour?
Male
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
pacing
internally preoccupied / responding to unseen others / muttering /
physical gesturing / punching the air / etc etc
yelling at self and others
isolative / fearful / paranoid / withdrawn / hard to engage
aggressive or abusive responses to others
Female
demanding
claiming
self-destructive
dependent
When challenging behaviour happens
1. Keep calm.
2. Back off where possible
3. Call for help.
4. Leave the person to calm down, if possible.
5. Remove others from the environment, if possible.
6. Be aware of body language and tone of voice used to the person.
The importance of risk assessment / risk factors when assessing challenging
behaviour
When addressing challenging behaviours, it is important to know the reasons
behind the behaviour as this can help identify the problem that needs to be
addressed.
Managing challenging behaviour
Managing challenging behaviour
Key Concept
internally preoccupied / responding to unseen others / muttering /
physical gesturing / punching the air / etc etc
yelling at self and others
isolative / fearful / paranoid / withdrawn / hard to engage
aggressive or abusive responses to others
Female
demanding
claiming
self-destructive
dependent
When challenging behaviour happens
1. Keep calm.
2. Back off where possible
3. Call for help.
4. Leave the person to calm down, if possible.
5. Remove others from the environment, if possible.
6. Be aware of body language and tone of voice used to the person.
The importance of risk assessment / risk factors when assessing challenging
behaviour
When addressing challenging behaviours, it is important to know the reasons
behind the behaviour as this can help identify the problem that needs to be
addressed.
Managing challenging behaviour
Managing challenging behaviour
Key Concept
Challenging behaviour
Challenging behaviour can be defined as any behaviour of an individual which has the
potential to cause physical or psychological harm to themselves, another person, or to
property around them. It does not have to be deliberate acts – some patients who
suffer from mental health conditions can express challenging behaviour
unintentionally.
Such behaviour, whether intentional or not, can act as a barrier between the patient
and healthcare providers attempting to deliver care and support. Such behaviour can
also compromise the safety of staff and other patients in an in-patient setting (2)
What triggers challenging behaviour in mental health patients?
To better understand how to deal with challenging behaviours, healthcare providers
should appreciate the factors which trigger such actions in their patients. Research
suggests that patients will express challenging behaviour as a result of either intrinsic
or extrinsic factors (2);
Intrinsic factors can be personal feelings, thoughts, emotions and health status
- both mental and physical.
Extrinsic factors will be the environment and people around them who can
trigger a behavioural response.
Important
Challenging behaviour can be defined as any behaviour of an individual which has the
potential to cause physical or psychological harm to themselves, another person, or to
property around them. It does not have to be deliberate acts – some patients who
suffer from mental health conditions can express challenging behaviour
unintentionally.
Such behaviour, whether intentional or not, can act as a barrier between the patient
and healthcare providers attempting to deliver care and support. Such behaviour can
also compromise the safety of staff and other patients in an in-patient setting (2)
What triggers challenging behaviour in mental health patients?
To better understand how to deal with challenging behaviours, healthcare providers
should appreciate the factors which trigger such actions in their patients. Research
suggests that patients will express challenging behaviour as a result of either intrinsic
or extrinsic factors (2);
Intrinsic factors can be personal feelings, thoughts, emotions and health status
- both mental and physical.
Extrinsic factors will be the environment and people around them who can
trigger a behavioural response.
Important
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





